Abstract
This chapter is intended to provide the reader with a perceptive of how resiliency plays a role in youth’s adjustment and management of chronic medical conditions. We will draw upon theory and empirical research to build a case for the need for psychological evaluations and interventions to incorporate an individual and family resiliency perspective to aid youth and their families in having more positive outcomes, such as better disease control, healthier interpersonal relationships, and greater self-confidence in their own abilities. Further, youth with chronic illnesses are at particular risk for difficulties in school. Thus, we will also highlight strategies that may work to promote better school functioning. In order to demonstrate these connections, we will draw upon case examples and present data from a study focused on integrating medical, mental health, and school psychological services for adolescents with diabetes.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Attention Deficit Hyperactivity Disorder
- Chronic Illness
- Sickle Cell Disease
- Family Functioning
- Juvenile Rheumatoid Arthritis
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
This chapter examines chronic illnesses in children and how factors associated with resiliency serve as a buffer against the negative outcomes associated with these conditions. An estimated 15–18 % of children suffer from a chronic illness (Ferro & Boyle, 2013; Woods, Mayes, Bartley, Fedele, & Ryan, 2013). Chronic illness can be defined as a medical condition existing longer than 3 months that interferes with an individual’s daily function. It must be managed by hospitalizations, treatment at home, and attendance at multiple physician appointments (Compas, Jaser, Dunn, & Rodriguez, 2012). This definition includes diseases such as diabetes, epilepsy, cancer, juvenile arthritis (JA), and asthma. There have been many changes in the medical field over the past several decades. Through these advances, illnesses that were previously considered to be life threatening are now treatable. Children who would previously not have survived are able to recover from or manage their illnesses. As a consequence, there has been an increase in children living with chronic illnesses (Newacheck & Taylor, 1992). Many of the illnesses have been shown to cause high stress in individuals, especially when they have to monitor their daily care activities regarding their illness (Guo, Whittemore, & He, 2011). Thus, when considering the impact of the chronic illness, it is important to consider the degree of behavioral self-management involved (Fournier, de Ridder, & Bensing, 2002). For instance, conditions such as diabetes and asthma entail significant self-care efforts to prevent serious medical situations that can occur at a moment’s notice, such as a spike in blood sugar or an asthmatic attack. It is often the role of the child, depending on age, to act in these situations that entail a high level of responsiveness and responsibility. Other chronic illnesses also necessitate self-care, but to varying degrees. Juvenile arthritis is somewhat controllable by self-care with the proper use of medication, a strict diet, and prescribed exercise. However, diseases like epilepsy do not entail much self-care as the symptoms are variable and the onset of seizures can be unpredictable.
Children with chronic illnesses experience a wide variety of challenges associated with their particular medical conditions. The initial diagnosis of a chronic condition is often a stressful and confusing time for children and parents (Compas et al., 2012). Many children with these conditions experience ongoing symptoms during or following treatment. Physical symptoms include pain, fatigue, and seizures. Additionally, there may be many unwanted side effects and stress associated with the medications and treatments that children receive for their respective conditions.
The parents of children with chronic illnesses, or the children themselves, must be prepared to administer medication immediately for diseases such as diabetes or asthma. This requires knowledge of the disease and how to manage the symptoms. In addition to the physical effects of these diseases, children with chronic illnesses also experience unwanted interruptions in their daily lives. For many children this includes missing school, being excluded from activities, and having to undergo frequent medical treatments. These activities can lead to significant stress for children with chronic illness and their caregivers. Another source of stress for students is the transition from the hospital or a prolonged period of time out of school back into the classroom (Shaw & McCabe, 2008). Although the transition itself is often stressful, returning to school includes deciding what information to share with the administration and fellow students. Additionally, if the disease requires treatment during the school day, the teacher and school nurse must be educated on how to provide treatment and handle situations such as the onset of a seizure or asthma attack. Research suggests that many children with chronic illness are also coping with significant psychological stress (Compas et al., 2012). This stress can lead to multiple psychological consequences such as low self-esteem, depression, and anxiety. However, children with such diseases often exhibit notable resiliency against these negative effects. To that end, this chapter will examine how resiliency plays a role in outcomes for children with chronic illnesses. First, we will review the literature on resiliency with regard to the family and school environment. Next, we provide information on chronic illnesses in the pediatric population and highlight two case examples of youth with similar levels of distress, but differing levels of resiliency. Finally, we close by discussing how to promote resiliency in children with chronic illnesses.
Resiliency Research
First we begin with our definition of resiliency. Resiliency is the capacity to recuperate from challenges or trauma to be successful across domains of functioning, such as self-perceptions, interpersonal relationships, and performance at school or work (Yi, Vitaliano, Smith, Yi, & Weinger, 2008). The concept of resiliency involves both the occurrence of stressors and the capacity within the child to respond, to endure, or to develop and master, in spite of the impact of the stressors (Richmond & Beardslee, 1988). Resiliency may be assessed by individuals’ self-perceptions of their own capacity and their interpersonal relationships (Prince-Embury, 2008). The targeted individual characteristics have varied across studies; however, these qualities often include perceived self-mastery, optimism, assertiveness, adaptability, effective emotional control, the ability to relate, trust, and feel supported by others, acceptance of differences in others, and perceived controllability of the situation. With regard to mental health, it is important to consider that although measures of psychopathology often inversely relate to measures of resiliency, the constructs are not necessarily on the same or opposing dimensions. Rather, it is possible to have moderate levels of distress and still evidence resiliency. Thus, a resilient individual is not necessarily someone who is characterized by the absence of distress, but also possesses positive qualities and strengths to be able to function well despite the distress (Masten, Herbers, Cutuli & Lafavor, 2008). Consequently, having resilient characteristics may serve to mitigate the negative outcomes that may have otherwise been associated with depression, anxiety, or disruptive behaviors in children. The research on chronic illness has indicated that resiliency factors can be protective against some of the negative effects associated with these diseases. Although individual or personal resiliency is an important construct, two other areas are particularly relevant for youth with chronic medical conditions: family and school.
People rarely exist in complete isolation. Instead, their experiences are shared with the people around them. When considering the factors that influence resiliency, it is important to explore the familial context in which the individual is embedded (Long & Marsland, 2011). Family resiliency is a growing body of literature that views resilience as a combination of multidimensional factors that promote the ability to adapt and overcome hardships as a functional unit (Walsh, 2003). Families contribute to the buffering elements that protect individuals from negative outcomes, such as those associated with chronic illnesses. It is clear that nearly all chronic illnesses disrupt family functioning due to the emotional, psychological, and financial stresses of caring for and treating a person with a disease. The different ways in which families are impacted by someone in the family having a chronic illness will be discussed later in the chapter. Despite these obstacles, many families do not experience problems within the family and instead adapt and adjust to the demands of the situation and emerge stronger (Walsh, 2003). The goal of a family resiliency model is to recognize and strengthen the processes that occur within interpersonal relationships that allow the family to endure and recover from negative life events. These processes include a sense of understanding that the crisis is manageable (coherence), a positive outlook (optimism), connectedness between family members (social support), ability to express feelings and concerns openly (emotional expression), and openness to change and ability to adapt (flexibility). This viewpoint focuses on seeing the family as an asset in need of repair as opposed to a hindrance contributing to the problem (Walsh, 2003).
The influences of family on well-being point to possible interventions aimed at improving outcomes for children with chronic illness by enhancing family resiliency. Rolland and Walsh (2006) reviewed present use of a family resiliency model in improving outcomes for the families with children facing childhood illnesses. The review showed that facilitating resilience factors such as coping and the ability to adapt enhanced overall quality of life for the family. Promising results suggest that enhancing family resiliency can be an effective intervention for children with chronic illnesses and highlight the need for research in this area.
Schools are a natural context to promote resiliency as youth spend one-third of their waking hours in the classroom. Students who possess resilient characteristics, such as academic and social competence, high expectations for oneself, and feelings of connectedness, are less likely to drop out of school and demonstrate higher levels of academic achievement (Brooks, 2006). Nonetheless, the literature on resiliency in schools is scarce as many studies emphasize a deficit model of functioning. However, a few reviews and studies support the benefit of emphasizing resiliency to promote school performance. The first consideration is assessment of resiliency within the school context. Prince-Embury (2008) described the methodological and practical challenges associated with conducting such a screening, but noted many benefits of ongoing monitoring of resilient characteristics. In this regard, a school system may wish to administer a measure of resiliency, such as the Resiliency Scales for Children and Adolescents (RSCA), to all children. Data obtained from this screening would identify students who are considered to be vulnerable to stressors or at risk for mental health difficulties. It would also identify strengths in each student that could be highlighted and fostered further. School personnel could use these findings to tailor classroom-wide or individual interventions. With regard to interventions within the school setting, several preliminary studies have yielded positive outcomes (Prince-Embury, 2008). Doll, Zucker, and Brehm (2004) emphasized the importance of establishing resilient classrooms so that all students have the opportunity to reach their full potential and are psychologically healthy. The authors promoted modifying the classroom environment rather than solely targeting individuals. Masten and colleagues, (2008) recommended simple resilience-enhancing strategies for school mental health professionals. Specifically, they suggested that all student-related objectives be written in positive language (i.e., what the student should be doing rather than what the student should be doing less of) and that monitoring of the outcomes should focus on strengths. Classroom-wide efforts should be proactive and preventative in nature rather than reactive and crisis-intervention oriented.
With regard to chronic illness, Wideman-Johnston (2011) reviewed literature focused on building resiliency for educational success for youth with chronic medical conditions. Qualitative findings suggest that effective management of health among youth with chronic health illnesses was characterized by three qualities: a positive self-image, adaptability, and relatedness to others. Consequently, resilience-enhancing strategies may include helping youth to understand the nature of their disease, having open communication with others, and promoting their confidence in their ability to manage their condition and its associated morbidities. A school-wide systemic approach involves school personnel ensuring that youth with chronic illnesses have the same educational opportunities as their otherwise healthy peers (Wideman-Johnston, 2011). Educators should avoid excluding these youth from traditional classrooms and have plans for the smooth transition back to school following hospitalizations or prolonged absences (Shaw & McCabe, 2008; Wideman-Johnston, 2011). Such plans may include allowing attendance for partial days until the child is fully recovered or provision of home-based instruction (Shaw & McCabe, 2008). Further, school personnel should consider and accommodate for physical limitations, isolation from others, academic challenges associated with the condition or its treatment, and the possibility that the youth with a chronic illness may experience feelings of being different than their peers (Wideman-Johnston, 2011). At the classroom level, teachers can provide a balance of autonomy and support as a way to strengthen the student–teacher relationship, foster acceptance and understanding within the classroom, provide appropriate supports to address unique instructional needs, and welcome them back into the classroom giving these youth an opportunity to make up missed assignments (Downey, 2008; Shaw & McCabe, 2008; Wideman-Johnston, 2011). One example may be identifying a classroom buddy or other peers with whom the child feels comfortable (Wideman-Johnston, 2011). To foster autonomy, a teacher should offer assistance and options, but allow the students to make decisions regarding their limitations or needs. Simply listening to the students’ needs can help to support their transition back to the classroom (Shaw & McCabe, 2008). Individual supports or interventions should promote problem solving abilities, instill hope, and help youth understand their own self-worth (Perfect & Jaramillo, 2012; Prince-Embury, 2007; Wideman-Johnston, 2011).
Pediatric Chronic Medical Conditions
As noted previously, each chronic medical condition is unique and varies in its prevalence, etiology, outcomes, and degree of self-management needed to avoid exacerbation of the condition. To some extent, certain conditions are more managed through behaviors of the patient, whereas other conditions are more likely to be less controllable and unpredictable. There are numerous medical conditions in the pediatric population and variable levels of severity within each of those conditions. Nonetheless, we selected epilepsy, juvenile arthritis, asthma, cancer, sickle cell disease, and diabetes given their prevalence in and impact on children (Sansom-Daly, Peate, Wakefield, Bryant, & Cohn, 2012). Under each condition, we present the estimated prevalence, the nature of the illness and its management, family and school outcomes associated with the disorder, research on resiliency or resilient characteristics within the population, and select findings related to interventions targeting youth diagnosed with that condition. Please see Table 19.1 for a summary of research findings related to (1) studies published examining personal strengths/resiliency with outcomes; (2) studies published examining family resilience and outcome; and (3) psychosocial interventions aimed at enhancing coping or resiliency as a way to enhance outcome.
Epilepsy
Epilepsy, or seizure disorders, includes a group of disorders that involve recurring seizures caused by unusual brain activity. It affects approximately 1 % of all children and has a higher incidence in lower income families (Russ, Larson, & Halfon, 2012). Seizures are the most common symptom of epilepsy and, when uncontrolled, can cause serious disruptions in the child’s life and put the child at risk for injuring himself or herself. There are many types of seizures but the defining characteristic is the presence of involuntary movements that can last seconds to several minutes. The type of seizures, age of onset, and brain activity during the seizures are used to determine what type of epilepsy the child is experiencing. The onset of the seizures generally must be spontaneous in order to be considered a seizure disorder; however, some types have triggers. This means that, for most children, a seizure may occur at any time. These children are at risk for having episodes during class time and interrupting their learning. A child is essentially incapacitated at the time of a seizure which often leaves the teacher responsible for ensuring the safety of the child and others in the room. Preparation for this might include the parents and child discussing the condition with the teacher and suggesting procedures in the event that the child suffers from a seizure. This can be uncomfortable for a child to reveal sensitive medical information with others and might cause the child to feel stigmatized for being different and requiring special accommodations. The most common treatment for epilepsy is medication to control the seizures. Unfortunately, many people with epilepsy do not get relief from seizure even with medication. The uncertainty associated with when the child will experience symptoms and lack of medical relief contribute to the negative psychological affects that children with epilepsy may experience. Outcomes associated with epilepsy are increased risk for attention deficit hyperactivity disorder (ADHD), conduct disorder, autism, and psychological problems such as anxiety and depression. In school, these risks increase the need for special services as epilepsy is highly comorbid with learning disabilities (56 % prevalence) and developmental delay (50 % prevalence) and overall a significantly increased risk for poor academic achievement (Russ et al., 2012). Parents of a child with epilepsy have been shown to experience uncertainty about familiar roles while providing care to the child. There might be uncertainty within the family surrounding the duties of a child in the household, which can lead to an over or underestimate of their abilities. Parents might also question whether the child feels psychologically excluded and, therefore, overcompensate for this perceived deficit and compound the problem. Unclear perceptions about the role of each family member can lead to negative effects for the child and family as a whole (Mu, Kuo, & Chang, 2005). The resiliency of youth with epilepsy is not well studied. However, two studies have emphasized family resiliency. One study found that factors such as family cohesion and fewer negative perceptions of epilepsy helped fathers feel they could respond to the unpredictable nature of their child’s illness (Mu, 2005). One qualitative study found that parents exhibited resiliency by maintaining hope for successful medical treatment and minimizing medical complications, seeking out resources to be informed, and maintaining flexibility so they could adapt to their child’s medical needs (Mu, 2008).
Some interventions have been developed to improve psychosocial outcomes for adolescents with epilepsy. One intervention was developed to improve self-concept, social confidence, and quality of life through participation in a karate course. Over the 10 weeks, the children reported an increase in their self-esteem and overall confidence in social situations. Parent reports indicated an increase in health-related quality of life for their children. The results suggest that similar activities might have a positive impact on youth with epilepsy in avoiding some of the negative social–emotional risks associated with the disease (Conant, Morgan, Muzykewicz, Clark, & Thiele, 2008). For families, Mu (2005) recommended that interventions should include psychoeducation about the illness to help families deal with uncertainty, targeting family cohesiveness by involving fathers, and frequent and open communication with families by medical professionals. Mu and Chang (2010) developed and examined a program designed to reduce ambiguity in the roles of families with children being treated for epilepsy. The mothers of children with epilepsy were asked to complete the boundary ambiguity scale, depression scale, and parental needs checklist as well as an initial in-person interview. Using the collected information, the needs of the family were assessed and they were offered one to two in-depth sessions to explore issues surrounding role ambiguity. The parents and child were made aware of the importance of defining roles and how they could improve this within their own family. Additionally, they were given information about epilepsy and how to care for a child with epilepsy. After the sessions, the family was given a parental education handbook and other materials about the disease itself. The results of a posttest 3 months after the intervention showed that the program decreased role ambiguity and, therefore, promoted resiliency in families caring for a child with epilepsy by increasing the child’s control over his or her own vulnerability (mastery; Mu & Chang, 2010).
Juvenile Arthritis (JA)
Juvenile arthritis is an umbrella term that encompasses the types of arthritis that affect children and adolescents. Nearly 1 in 250 children under the age of 18 is diagnosed with a form of childhood arthritis, making it one of the most prevalent chronic illnesses in children (Sacks, Helmick, Luo, Ilowite, & Bowyer, 2007). Arthritis is an autoimmune disease generally defined by inflamed joints lasting more than 6 months. The classification of arthritis is largely dependent on the type and number of joints affected. Youth with arthritis typically experience stiffness of the joints that can range from discomfort to severe pain impeding all physical movements. Fatigue is also very commonly associated with arthritis, especially when the joints are inflamed. Other effects of the disease can be vision problems related to inflammation of the optic nerve and the premature end of growth. The symptoms of the disease are controlled largely through pharmaceuticals. Many of these drugs are very hard on the system as they are designed to stop the body from attacking the joints. Therefore, children on these medications experience a depreciated immune system and must undergo frequent blood tests to ensure proper liver and kidney functioning. Another common treatment for juvenile arthritis is a series of cortisone shots injected directly into the affected joints. These shots can be extremely painful and frightening for young children. However, there is also evidence that restricted diets and exercise targeting muscles surrounding the afflicted joints can reduce symptoms. For children in school, this means limited physical activity, increased absences, tiredness during class time, etc. all of which can lead to negative social–emotional outcomes and poor school performance (Sanzo, 2008).
Families can be affected by the stress and financial impact of the disease (Gerhardt et al., 2003). One study examined family functions and parental distress in families of children with juvenile rheumatoid arthritis (JRA). The results indicated that the families exhibited considerable resilience as defined by the ability to adapt to the difficulties of caring for a child with JRA. In comparison to families without a child with a chronic illness, these families reported similar levels of family functioning, parental distress, and supportiveness indicating that families are able to adapt to the challenges presented by the disease (Gerhardt et al., 2003). A study on adults with arthritis found that increases in positive affect and positive interactions correlated with resiliency when confronted with the stresses of the disease (Smith & Zautra, 2008). In this particular study, the resilience factor comprised measures of optimism, coping, positive reinforcement, and purpose in life. These findings suggest that the factors of resilience can influence how patients cope with psychological effects of the disease. With regard to interventions, Stinson et al. (2010) evaluated a program aimed at improving outcomes for adolescents with juvenile arthritis and their families. The intervention was delivered through internet modules to the adolescent and one parent over 12 weeks that provided information about the disease itself and self-management techniques. The results indicated that the adolescents with arthritis and their parents’ knowledge of the disease increased and the youth saw a significant overall decrease in pain intensity by the end of the intervention. Although not specifically examined, the increased knowledge may have led to increased disease care and, therefore, contributed to decreases in pain intensity. Interventions aimed at increasing self-management that include the family have the potential to serve as an effect invention tool to improve outcomes for children with juvenile arthritis.
Asthma
Asthma affects approximately 9 % of children in the United States. It is one of the more prevalent childhood illnesses affecting more than seven million children as of 2010 (Centers for Disease Control and Prevention, 2012b). Asthma is a chronic illness involving the lungs and airways that become inflamed and make breathing difficult. Children with asthma experience difficulty breathing, chest tightness, coughing or wheezing, etc. An asthma attack can be bought on suddenly during exercise, stress, or allergens, and is frightening and potentially life threatening for the child. Children with asthma are often responsible for managing their disease through the use of an inhaler and by avoiding situations likely to provoke an attack. Managing asthma can be stressful for a young child and also alienating at school. Children with asthma might be excluded from activities, such as outdoor sports, due to their illness. Additionally, the need for regularly scheduled doctor appointments may require children with asthma to miss school frequently. Additionally, during an attack or following one, other students might not have an understanding of what asthma is or why the student is having problems breathing. This discomfort with the illness may result in avoidance or rejection. Such negative peer interactions can lead to feelings of depression in addition to other psychological distress of which children with asthma are at risk (Petteway, Valerio, & Patel, 2011).
Childhood asthma is associated with poor psychological adjustment for both the child and parents. Family functioning can be disrupted by the burden of caring for a child with asthma. Holm (2008) asserted that parents of children, specifically mothers, with asthma are at risk for psychological symptoms related to uncertainty about the disease and the impact on the child. However, the psychological well-being of these parents is impacted by how resilient the family is. Hardiness has been described as a component of or synonymous with resiliency. From a family resiliency perspective, it refers to how the family copes with stressful life outcomes by viewing change as growth rather than burdensome and feeling control over such life changes. Svavarsdottir and Rayens (2005) measured family hardiness using the Family Hardiness Index, which comprised questions about the family’s current situation on a four-point Likert scale. Higher scores reflected greater family hardiness. Data supported that in families with asthmatic children, sense of coherence (feeling that life is predictable and manageable), level of depression, and well-being related to the level of family hardiness. This finding suggests that interventions aimed at improving the well-being of the family may increase family resiliency and, therefore, improve outcomes for children with asthma by being better able to adapt to caring for a child with a chronic illness (Svavarsdottir & Rayens 2005).
Asthma also impacts how the child functions in an educational setting. Specifically, children with asthma are at risk for poor school outcomes due to increased absences, side effects from medication, stress, as well as perceptions by the teacher or parents that the child cannot perform due to weaknesses related to the disease (Celano & Geller, 1993). Many of the negative school outcomes that children with asthma are at risk for can be minimized with proper disease management. As mentioned previously, asthma is a highly manageable disease through self-care. To promote positive school outcomes, children can be taught disease management techniques for home and school with the support of family members and supportive teachers. This includes how to properly use an inhaler and the ability to monitor symptoms and take steps to prevent asthmatic attacks.
Koinis Mitchell, Murdock, and McQuaid (2004) examined if the individual characteristics of perceived control and adaptability predicted asthma management behaviors in the context of neighborhood and disease characteristics. Adaptability and self-management behaviors were measured using the Behavioral Assessment Scale for Children (BASC) and the Asthma Behavioral Assessment Questionnaire (ABAQ), respectively; they were administered at the beginning of the study and at a 1-year follow-up. Adaptability was defined as how quickly and easily the child was able to adapt to new situations. The authors found that higher levels of adaptability enhanced self-management behaviors for children with high levels of neighborhood disadvantage at the 1-year follow-up. Therefore, resiliency characteristics associated with adaptability may operate as protective factors for urban children and help them manage their asthma symptoms within a disadvantaged setting. Another study examining Korean children with asthma found that resiliency associated inversely with levels of depression (Kim & Yoo, 2007). The resiliency of the children was measured using a scale developed by the authors that measured coping and intrapersonal and interpersonal aspects of children with chronic illnesses. The findings indicate that factors associated with resiliency are important for buffering children against the psychological effects of asthma. Additionally, a systematic review reported that several interventions have been developed to decrease asthmatic symptoms through improving interpersonal relationships and family functioning. Family therapy has been shown to improve airway inflammation and decrease wheezing symptoms in children with severe asthma. These results suggest that family resiliency can provide physical relief to children with asthma by addressing emotional aspects and promoting family evolvement in managing the disease (Ritz, Meuret, Trueba, Fritzsche, & von Leupoldt, 2013).
Cancer
Cancer is the overproduction of cells in the body that creates abnormal cells by damaging the DNA. The reproduction of these cells often results in the creation of tumors that grow and spread to other parts of the body, creating more damaged cells. The primary types of cancer encountered in the pediatric population are leukemia (34 %), brain and nervous system tumors (27 %), lymphoma (8 %), bone cancer (osteosarcomas), extracranial tumors (neuroblastoma; 7 %), Wilms tumor (5 %), and cancer of the eye (retinoblastoma; 3 %). Cancer in children has been rising in the last several decades and roughly 11,500 children are projected to be diagnosed this year (American Cancer Society, 2012). Although the rate of cancer in children is lower than other chronic illnesses, the mortality rate is much higher. Cancer is the second leading cause of death in children under the age of 15. Childhood cancers are often different from the kinds of cancer that affect adults in that they are relatively unrelated to lifestyle choices or environmental factors. Most of the DNA damage that leads to cancer in children occurs very early on in a child’s life and can even begin prenatally (American Cancer Society, 2012).
Although treatment for different types of cancer varies, the most common treatments, based on severity and type, include chemotherapy, surgery, radiation, and medication. The treatments for cancer are accompanied by severe side effects such as weight loss, extreme nausea, hair loss, and many others. Depending on the stage of cancer and the frequency of the treatments, hospitalizations may be required which removes the child from the home and school environment for long periods of time. Some cancers, such as bone cancer, may require intensive rehabilitation (Smorti, 2012).
Family functioning is also impacted by the demands of treating childhood cancer. The parents and youth must adapt to intense treatment regimes that may be time-consuming and financially burdensome. In addition to disruptions in daily life, the family must also cope with the unpredictability of the disease which may in turn increases the risk for negative family interactions. Children with cancer might feel that their parents are being overbearing due to an increased presence in the child’s life and decision making for the child (Heiney, Ruffin, Ettinger, & Ettinger, 1988). A review of the literature done by Long and Marsland (2011) indicated that families of children undergoing treatment for cancer experience considerable variability in family functioning. Many families report role reorganization, shifting of responsibilities, financial uncertainty, etc. However, the degree to which the family experiences disruption is dependent on a host of factors including the mental health of the parents, marital distress, and family closeness.
Upon release from the hospital, children with cancer may experience a difficult school reentry period. Because the side effects of the cancer and treatment are so taxing on the body, children with cancer often have notable physical characteristics that bring attention to their illness. Other students might be afraid of catching the disease from the child or that the child will die soon. These morbid thoughts create distance between the child and his or her peers. In addition to social and psychological stress associated with childhood cancer, children also experience school problems related to absences, fatigue during school, etc. (Henning & Fritz, 1983).
Kim and Yoo (2010) found that several factors related to resiliency in school age children with cancer. The authors defined resiliency as utilizing personal strengths and abilities to overcome difficulties and adapt to challenging situations. Children who reported higher family functioning, positive friendships, and good teacher relationships showed higher resiliency than their counterparts. These findings suggest that positive relationships with teachers and friends and cohesive and adaptive families serve as important resiliency factors that can protect children from some of the negative psychosocial morbidities associated with cancer. Another study examined predictors of resiliency in adolescents being treated for cancer. Resiliency was assessed using the Haase Adolescent Resilience in Illness Scale which measures how the children think and feel about managing their illness. The study reported positive correlations between resiliency and the coping strategies of cognitive coping and problem-orientated coping in dealing with the worry associated with undergoing cancer treatments (Wu, Sheen, Shu, Chang, & Hsiao, 2013). A study of adolescents diagnosed with bone cancer examined the resilient characteristics of optimism and adaptability (Smorti, 2012). The author found that scores on measures of impulse control and optimism were higher for adolescents who had experienced remission from bone cancer compared to those without cancer. However, compared to those without cancer, those diagnosed with bone cancer had lower ego-resiliency and were less welcoming of unfamiliar situations. When reviewing the data more carefully, Smorti (2012) noted that since scores on the measure of optimism were so high for the adolescents with cancer, there was the potential for these youth holding unrealistic expectations. These findings support the need for practitioners to evaluate whether what appears to be an optimistic viewpoint is based on facts or a reflection of an unrealistic outlook on the situation. In another qualitative study of self-image among female adolescent cancer survivors, researchers concluded that cancer and its treatment impact self-esteem. Interestingly, following treatment, the participants’ views on appearance changed in that it became less important and there was an increase in satisfactions with their own self-image (Wallace, Harcourt, Rumsey, & Foot, 2007). In describing a conceptual model of resiliency among childhood cancer survivors, Wills and Bantum (2012) asserted that resiliency relates to self-control in that good regulation results from social support and poor self-control is related to interpersonal conflict. The authors also reviewed findings relevant to resiliency in cancer survivors. Specifically, the review discussed how optimism, self-control, and social support are related to improvements in quality of life and overall psychological functioning in cancer patients. These resiliency factors work together to reduce the risk of negative outcomes related to cancer.
There are a wide variety of interventions for children with cancer that target improving social, academic, and psychological outcomes. One study investigated the use of group therapy to increase social functioning of children with cancer. Descriptive data suggested that the adolescents were better able to cope with the stress associated with parental overbearingness and peer isolation following group therapy (Heiney et al., 1988). Additionally, several studies have aimed to increase treatment adherence among adolescents with cancer. One study utilized a video game as an intervention. Adolescents with cancer who were randomly assigned to the experimental condition were asked to play a single player video game across several weeks, which included “missions” related to cancer treatments. Participants in the control condition did not play the video game. Participants were asked to defeat cancer cells, deliver antibiotics, and other tasks that represent real life needs for youth with cancer. At the end of the intervention, the adolescents who played the video game showed better treatment adherence as well as increased knowledge about the treatment and self-efficacy. This increased knowledge about the treatment and self-efficacy served as mediators for improvements in patient’s adherence (Kato, Cole, Bradlyn, & Pollock, 2008). We highlighted just a few of the interventions that have been conducted with children being treated for cancer. Using technology that is appealing to youth such as video games may be both well received and effective.
Sickle Cell Disease
Sickle cell anemia is a blood disorder characterized by abnormally shaped red blood cells that can cause various complications. The disease is hereditary and is passed from parents to offspring. It is more common among African Americans and people originating from areas where malaria is common. The Centers for Disease Control and Prevention report that sickle cell disease occurs in 1 of every 500 African American births. People with sickle cell often have anemia, or a shortage of red blood cells, and may appear pale or jaundiced. The most common side effect of the disease is chronic pain associated with blood cells becoming stuck in various parts of the body which deprives that area of oxygen. The onset and duration of these episodes are relatively unpredictable. Pain management is an important component to treating this disease as episodes can last anywhere from a few hours to several days and require hospitalization. Blockages caused by the rigid blood cells can also compromise organs and make the body more vulnerable. Therefore, most children with sickle cell are prescribed a regime of antibiotics to fight off infections. This disease can also slow development that leads to slower growth and delayed puberty for affected youth (Centers for Disease Control and Prevention, 2011).
The physical pain associated with this disease can be accompanied by psychological distress. The unpredictability of symptoms may cause disruptions in the daily life or the child’s ability to function at and attend school. Managing symptoms of the disease also puts strain on family functioning by interfering with the parent’s ability to attend work as well as the emotional stress of caring for an ill child. However, not all children with sickle cell experience negative social and psychological outcomes associated with the disease. Studies have found that acceptance, self-encouragement, and hope are related to better adjustment and lower pain intensity in youth and adults with sickle cell disease (Bediako & Neblett, 2011; Ziadni, Patterson, Pulgarón, Robinson, & Barakat, 2011). Using case reviews and focus groups, Barbarin (1994) concluded that personal resiliency factors such as optimism and hope as well as positive family functioning (parental involvement, supportive relationships, etc.) played a crucial role in mitigating the negative outcomes associated with sickle cell disease. Additionally, the author article discussed how illness severity does not necessarily determine the extent to which a child will suffer from negative psychological outcomes or the degree to which the disease will serve as an interruption. This factor was mediated by the child and family’s view of the illness. Therefore, the better the family copes with the disease as a whole, the better the child’s adjustment will be across all domains (Barbarin, 1994).
Diabetes
Diabetes is a group of metabolic disorders that affects blood sugars (glucose) in the body. A hormone in the body, insulin, serves to regulate glucose. Two primary types of diabetes, type 1 diabetes mellitus (T1DM) and type 2 diabetes mellitus (T2DM), are characterized by the body’s inability or ineffectiveness to produce insulin, respectively. Over 13,000 youth are newly diagnosed with T1DM annually in the United States, with approximately 1 in 500 children and adolescents having the disorder (Centers for Disease Control and Prevention, 2012a; Wodrich, Hasan, & Parent, 2011). Physicians monitor diabetic health through a blood test that yields a value for hemoglobin A1c (HbA1c), which is an estimate of glucose levels over a 3-month time period (Hilliard, Wu, Rausch, Dolan, & Hood, 2013; Yi-Frazier, Hilliard, Cochrane, & Hood, 2012). Excessively high amounts of blood sugars (hyperglycemia) for long durations may lead to long-term complications with the kidneys, vision, or nerves, whereas extremely low blood sugars (hypoglycemia) may result in seizures, coma, or even death. Management of T1DM involves administration of exogenous insulin via a pump or injections, adjustment of those doses based on diet or physical activity, and frequent check of blood sugars to determine a patient’s degree of glycemic control. These multiple daily blood checks require pricking the finger to extract a small amount of blood, which can be very burdensome and uncomfortable to patients (Kucera & Sullivan, 2011; Perfect & Jaramillo, 2012).
Compliance with diabetes self-care significantly declines in adolescence. The diagnosis and management of diabetes place a high level of stress on individuals and families (Rearick, Sullivan-Bolyai, Bova, & Knafl, 2011). Research has supported that high levels of parental–child conflict and parenting stress interfere with the execution of behaviors necessary to manage diabetes (Hilliard et al., 2013; Monaghan, Horn, Alvarez, Cogen, & Streisand, 2012; Streisand, Swift, Wickmark, Chen, & Holmes, 2005; Yi-Frazier et al., 2012). Conversely, higher levels of parental involvement and monitoring and family cohesion are associated with better management and control (Grabill et al., 2010; Hilliard et al., 2013; Mackey et al., 2011).
With regard to school functioning, studies have found that youth with T1DM often struggle in the areas of writing and math (Naguib, Kulinskaya, Lomax, & Garralda, 2009), establishing and maintaining peer relationships, performance in school, high school completion, and post-secondary educational pursuits (Kucera & Sullivan, 2011; Wodrich et al., 2011). However, one study found that students with diabetes who reported the ability to adapt to current situations and had stronger family relations were less likely to evidence lower school performance (Erkolahti & Ilonen, 2005). Perfect and Jaramillo (2012) found that self-mastery and optimism predicted higher parental-reported school grades. Given the amount of self-care activities involved, managing diabetes is a family process. Caregivers often have to provide frequent reminders to their children to take their medication or check their sugars. They may also experience sleep disruption due to checking levels in the middle of the night (Monaghan, Hilliard, Cogen, & Streisand, 2009).
A few studies have examined resiliency among adults with diabetes. Yi et al. (2008) found that resilient adults were less likely to have increases in HbA1c relative to adults characterized by low levels of resiliency. In our research, we found that to achieve better glucose control, adolescents need to feel competent in their problem solving skills in general (Perfect & Jaramillo, 2012). In one review, authors only identified 22 studies that focused on resilience, well-being, or positive emotions. The authors found that all three factors were associated with self-management of diabetes and diabetic health (Robertson, Stanley, Cully, & Naik, 2012). Mackey et al. (2011) examined the interrelations between positive attributes in young adolescents with T1DM. Findings supported that both individual qualities and family cohesion predicted better diabetes management, which, in turn, related to better glucose control. Thus, resiliency within the individual as well as families may serve to buffer adolescents from lapsing in their diabetes management.
Very few interventions for youth with T1DM have focused on enhancing resiliency. Youth with effective coping skills, such as actively engaging in tasks to manage a disease, are able to adjust to their chronic illness and feel more competent (Jaser & White, 2010; Lee, Kim, & Choi, 2013). Some researchers have focused on coping skills training to increase patients’ abilities to manage stressful situations and gain greater self-confidence (Thorpe et al., 2013). One review examined interventions that promoted “healthy coping,” which the authors defined as emphasizing “positive attitudes toward diabetes and its treatment, positive relationships with others, and high perceived quality of life” (Thorpe et al., 2013, p. 34). Based on their review, Robertson et al. (2012) concluded that interventions should target these areas rather than taking a deficit approach. Family therapy interventions for youth with T1DM have also yielded positive effects, with benefits being shown in improving family resiliency factors such as cohesion, communication, and efficacy in solving problems (Hillard, Harris, & Weissberg-Benchell, 2012; Thorpe et al., 2013).
Case Examples
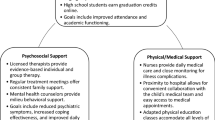
In this next section, we highlight two case examples to underscore the potential protective factor of resiliency for youth with T1DM. The data were collected as part of a study aimed at integrating medical, mental health, and school-based services for youth with diabetes. Recruitment occurred in a diabetes clinic where research team members described the study to families who provided permission to be approached by the team members. There were a minimum of two face-to-face visits, followed by phone feedback to families. The primary measures were administered at the initial screening visit which lasted no more than 20 min. This included the Diabetes Quality of Life-Youth (DQOL-Y) and the Brief Symptoms Inventory (BSI). Parents completed the Pediatric Symptoms Checklist (PSC) about their child. At the assessment visit, which occurred regardless of screening results and lasted approximately 90 min, youth completed the Beck Youth Inventory-2nd Edition (BY-II), RSCA, and select modules from the National Institutes of Mental Health-Diagnostic Interview Schedule for Children (NIMH-DISC-IV-TR). The criteria for referral included the following: (1) cutoff raw score on the PSC was 28; (2) a T-score ≥ 60 on the Global Severity Index of the BSI, T-score ≥ 60 on more than one subscale, or a T-score ≥ 70 in any one domain; (3) a T-score ≥ 60 on any one of the Depression, Anxiety, Disruptive Behavior, and Anger BY-II scales, and a positive diagnosis on the NIMH-DISC-IV-TR (whether the adolescents reported enough symptoms to warrant receiving a particular disorder based on the DSM-IV-TR). The feedback included a recommendation to participate in a third phase that involved a referral to a mental health professional and monitoring by our team for up to 3 months. Although a positive diagnosis was used for the NIMH-DISC-IV-TR to make a referral, subthreshold symptoms or symptoms that are not endorsed for a long enough duration are identified as an intermediate diagnosis. Further, although the DQOL-Y was not used for a referral, we considered it in our feedback and recommendations.
To summarize our overall findings from the study (Perfect & Jaramillo, 2012; Perfect, Levine-Donnerstein, Swartz, Wheeler, & Amaya, 2011), we first pre-tested variables to determine if they related to the outcome. Multiple regression analyses were conducted to predict self-reported GPA, parental-reported school problems, blood glucose monitoring, and HbA1c. When measures of psychopathology (Global Severity Index of the BSI and BY-II subscales) were entered into the same model as the RSCA scales of Self-Mastery and Emotional Reactivity to predict grades, they no longer contributed their own variation to the model. Self-mastery predicted all three of our targeted outcomes: self-reported grades, parent-reported school-related problems, and HbA1c. A complex picture emerged. Different aspects of resiliency related to the different outcomes. Children who perceived better interpersonal relationships characterized by trust and support were more likely to monitor their glucose levels. These interpersonal qualities did not significantly correlate with HbA1c. However, sense of relatedness related to blood glucose monitoring, which, in turn, related to HbA1c. Factors that associated with HbA1c were self-mastery and an optimistic outlook as well as low emotional reactivity including reduced sensitivity and improved recovery time from stressful experiences related directly to HbA1c (please see Perfect & Jaramillo, 2012 for more data and information regarding these relations). Although more research is needed to expand on the interrelations among the different dimensions of resiliency and outcomes such as adherence to treatment and optimal glucose control, examining specific cases provides exemplars for a strength-based approach to assessment and linking assessment with intervention.
Case example #1. One of our participants, “Sal,” came into the diabetes clinic with his mother. He was 13 years 4 months old and had T1DM for 2 years. After agreeing to participate in the study and completing the assent/consent process, Sal completed the BSI, the DQOL-Y, and questions regarding his perception of the screening process. His mother filled out the PSC and questions about her perceptions of the screening process. Scores on the BSI were within the Average range. A score of 29 on the PSC was above the clinical cutoff suggesting his mother had significant concerns regarding his psychological adjustment and behaviors. On the DQOL-Y, Sal’s scores suggested moderate-to-high life satisfaction, low diabetes-related worries, and moderate-low disease burden. At the assessment visit, Sal completed the BY-II, RSCA, and the NIMH-DISC-IV-TR. Although the BY-II and NIMH-DISC-IV-TR did not meet the clinical cutoffs, Sal’s responses to the NIMH-DISC-IV-TR did reveal a positive diagnosis for ADHD. With regard to resiliency, the T-score on the RSCA Resource Index was a 64, with his score on the Interpersonal Relatedness scale in the Above Average range. Based on subscale scores in the Above Average to Superior range, he self-reported a positive outlook on the future, an ability to adapt to different situations, trust in others, feelings of being supported by others, comfort in his social relationships, and a high tolerance for differences in others. With regard to outcomes, Sal reported that his grades consisted of mostly Bs and the most recent HbA1c value was 8.5 indicating he did fairly well in school, but his glucose levels were not well controlled, which the American Diabetes Association defines as a HbA1c < 7.5 % for this age group. Although above the recommended target (Silverstein et al., 2005), his levels were still below the mean of the sample (9.56 %). His medical record also showed that he checked his blood sugars an average of 2.9 times per day.
Case example #2. “Peter,” a 13-year-10-month-old male, agreed to participate in the study while waiting for his appointment in the diabetes clinic. He was diagnosed with diabetes when he was 11½ years old. The score on the BY-II Anger scale was 63, suggesting he harbored considerable anger. His mother also reported that he experienced emotional and behavioral problems as evidenced by a score of 29 on the PSC. On the DQOL-Y Peter’s scores suggest moderate life satisfaction, low levels of diabetes-related worries, and moderate-high disease burden. In his case, he endorsed items on the DQOL-Y Disease Burden subscale such as missing school because of diabetes, having to explain diabetes, eating something he should not because he does not want to tell someone about diabetes, and diabetes preventing his participation in some activities. Assessment results indicated an intermediate diagnosis of Generalized Anxiety Disorder, Major Depressive Disorder, Mania, and Oppositional Defiant Disorder on the NIMH-DISC-IV-TR. Thus, he endorsed subthreshold mental health symptoms in a number of areas. T-scores on the Resiliency Resource and Vulnerability Indexes of the RSCA were 40 and 62, respectively. Such a profile suggests that Peter perceived himself as lower in resiliency defined as protective resources, and a large discrepancy between his emotional reactivity and resources with which to cope effectively when encountering stressful situations. Specifically, he reported lower-than-average self-mastery and higher-than-average emotional reactivity. A further examination of the subscales showed a very negative outlook for the future (i.e., Optimism subscale scaled score = 4), that his trust in others was not as developed as his same age peers, that he was easily triggered by emotional situations, and he had difficulty managing when emotionally aroused. In contrast to Sal, Peter’s grades consisted of some Cs and some Ds and the medical record showed that his most recent HbA1c value was 10.8 %, indicating he struggled with both his performance in school and his diabetic health. However, downloaded meter data showed that he did test his blood sugars an average of 4.3 times per day.
As was the case with the majority of the sample (less than 10 % had HbA1c < 7.5 %), both of these two male adolescents were in suboptimal control. Despite some levels of distress, Sal appeared to be doing well in school and was closer to achieving optimal glycemic control than Peter. Since research has shown that adherence to diabetes management, often reflected in frequent blood glucose monitoring, improves blood sugars (as reflected by meeting the target HbA1c), intervention would want to start with increasing Sal’s blood glucose checks. Since our overall findings suggested that the RSCA Relatedness scale positively related to blood glucose monitoring, recommendations would be to capitalize on Sal’s sense of trust, support, and comfort in his relationships to promote better adherence. A school-specific intervention might include building relationships at school with the school nurse or teachers. They should encourage Sal to engage in more frequent testing while trying to minimize missing important instruction. Further, a family approach to diabetes management also has a high likelihood of better diabetes management and control. Thus, intervention should emphasize promoting collaboration and open communication among Sal’s family members (Hillard et al., 2012; Yi-Frazier et al., 2012), particularly since his mother had some concerns about his behaviors.
Resilience enhancement for Peter would involve assisting him to establish positive, yet realistic, expectations by helping him to establish reasonable goals (Fournier et al., 2002; Perfect & Jaramillo, 2012). He could be encouraged to produce positive self-statements rather than relying on praise by others. An intervention could include an out-of-session assignment, such as having him maintain a journal in which he records situations that he felt proud as well as share these statements with school professionals (Perfect & Jaramillo, 2012; Prince-Embury, 2007). In school, he would benefit from case management services to ensure that both his educational and his health needs are met (Engelke, Guttu, Warren, & Swanson, 2008).
Summary and Conclusions
This chapter reviewed research related to personal and family resiliency in the face of chronic illness. The etiology and outcomes vary according to the particular medical condition. Nonetheless, the commonality for each of them is the impact of chronic illness on psychological, family, and school functioning. We underscored that personal resiliency must be considered in the context of family and school. As part of our review, we highlighted some of the most prevalent chronic medical conditions experienced in the pediatric population. In many cases, there were only single studies and in no case is there an evidence-based or empirically supported treatment focused on enhancing resiliency in youth with any chronic medical conditions. Data from our study underscore the importance of assessing the multidimensional components of resiliency. The contrasting case studies further elucidate the importance of examining strengths as part of the evaluation process for youth with chronic illnesses. In this chapter, we were able to identify some interventions that target individuals and families facing different health conditions. We applied findings from the literature when suggesting strategies to enhance resiliency in the two adolescents with T1DM from our case examples. However, more empirical data are needed to add to the evidence base for resilience-enhancing interventions to improve outcomes for children with chronic illness.
References
American Cancer Society. (2012). Cancer in children. Retrieved June 8, 2013, from www.cancer.org/acs/groups/cid/documents/webcontent/002287-pdf.pdf
Barbarin, O. A. (1994). Risk and resilience in adjustment to sickle cell disease: Integrating focus groups, case reviews, and quantitative methods. Journal of Health & Social Policy, 5, 97–121. doi:10.1300/J045v05n03_07.
Bediako, S. M., & Neblett, E. R. (2011). Optimism and perceived stress in sickle-cell disease: The role of an afrocultural social ethos. Journal of Black Psychology, 37, 234–253. doi:10.1177/0095798410385681.
Brooks, J. E. (2006). Strengthening resilience in children and youths: Maximizing opportunities through the schools. Children & Schools, 28, 69–76.
Celano, M. P., & Geller, R. J. (1993). Learning, school performance, and children with asthma: How much at risk? Journal of Learning Disabilities, 26, 23–32. doi:10.1177/002221949302600103.
Centers for Disease Control and Prevention. (2011). Sickle cell disease, data, and statistics. Retrieved June 8, 2013, from http://www.cdc.gov/ncbddd/sicklecell/data.html
Centers for Disease Control and Prevention. (2012a). Children and diabetes—More information. Retrieved June 15, 2013, from http://www.cdc.gov/diabetes/projects/cda2.htm
Centers for Disease Control and Prevention. (2012b). Trends in asthma prevalence, health care use, and mortality in the United States, 2001–2010. Retrieved June 7, 2013, from http://www.cdc.gov/nchs/data/databriefs/db94.htm
Compas, B. E., Jaser, S. S., Dunn, M. J., & Rodriguez, E. M. (2012). Coping with chronic illness in childhood and adolescence. Annual Review of Clinical Psychology, 8, 455–480.
Conant, K. D., Morgan, A. K., Muzykewicz, D., Clark, D. C., & Thiele, E. A. (2008). A karate program for improving self-concept and quality of life in childhood epilepsy: Results of a pilot study. Epilepsy & Behavior, 12, 61–65. doi:10.1016/j.yebeh.2007.08.011.
Doll, B., Zucker, S., & Brehm, K. (2004). Resilient classrooms: Creating healthy environments for learning. New York: Guilford Press.
Downey, J. (2008). Recommendations for fostering educational resilience in the classroom. Preventing School Failure, 53, 56–64. http://dx.doi.org/10.3200/PSFL.53.1.56-64.
Engelke, M. K., Guttu, M., Warren, M. B., & Swanson, M. (2008). School nurse case management for children with chronic illness: Health, academic, and quality of life outcomes. The Journal of School Nursing, 24, 205–214. doi:10.1177/1059840508319929.
Erkolahti, R., & Ilonen, T. (2005). Academic achievement and the self-image of adolescents with diabetes mellitus type-1 and rheumatoid arthritis. Journal of Youth and Adolescence, 34, 199–205. doi:10.1007/s10964-005-4301-8.
Ferro, M. A., & Boyle, M. H. (2013). Self-concept among youth with a chronic Illness: A meta-analytic review. Health Psychology, 32, 839–848. doi:10.1037/a0031861.
Fournier, M., de Ridder, D., & Bensing, J. (2002). Optimism and adaptation to chronic disease: The role of optimism in relation to self-care options of type 1 diabetes mellitus, rheumatoid arthritis and multiple sclerosis. British Journal of Health Psychology, 7, 409–432. doi:10.1348/135910702320645390.
Gerhardt, C. A., Vannatta, K., McKellop, J., Zeller, M., Taylor, J., Passo, M., et al. (2003). Comparing parental distress, family functioning, and the role of social support for caregivers with and without a child with juvenile rheumatoid arthritis. Journal of Pediatric Psychology, 28, 5–15. doi:10.1093/jpepsy/28.1.5.
Grabill, K. M., Geffken, G. R., Duke, D., Lewin, A., Williams, L., Storch, E., et al. (2010). Family functioning and adherence in youth with type 1 diabetes: A latent growth model of glycemic control. Children’s Health Care, 39, 279–295.
Guo, J., Whittemore, R., & He, G. (2011). The relationship between self-management and metabolic control in youth with type 1 diabetes: An integrative review. Journal of Advanced Nursing, 67, 2294–2310.
Heiney, S. P., Ruffin, J., Ettinger, R. S., & Ettinger, S. (1988). The effects of group therapy on adolescents with cancer. Journal of Pediatric Oncology Nursing, 5, 20–24.
Henning, J., & Fritz, G. K. (1983). School reentry in childhood cancer. Psychosomatics, 24, 261–269.
Hilliard, M. E., Harris, M. A., & Weissberg-Benchell, J. (2012). Diabetes resilience: A model of risk and protection in type 1 diabetes. Current Diabetes Reports, 12, 739–748.
Hilliard, M. E., Wu, Y. P., Rausch, J., Dolan, L. M., & Hood, K. K. (2013). Predictors of deteriorations in diabetes management and control in adolescents with type 1 diabetes. Journal of Adolescent Health, 52, 28–34.
Holm, K. E. (2008). The impact of uncertainty associated with a child’s chronic health condition on parents’ health. Families, Systems & Health, 26, 282.
Jaser, S. S., & White, L. E. (2010). Coping and resilience in adolescents with type 1 diabetes. Child: Care, Health and Development, 37, 335–342.
Kato, P. M., Cole, S. W., Bradlyn, A. S., & Pollock, B. H. (2008). A video game improves behavioral outcomes in adolescents and young adults with cancer: A randomized trial. Pediatrics, 122, e305–e317.
Kim, D., & Yoo, I. (2007). Factors associated with depression and resilience in asthmatic children. Journal of Asthma, 44, 423–427. doi:10.1080/02770900701421823.
Kim, D. H., & Yoo, I. Y. (2010). Factors associated with resilience of school age children with cancer. Journal of Paediatrics and Child Health, 46, 431–436.
Koinis Mitchell, D., Klein Murdock, K., & McQuaid, E. L. (2004). Risk and resilience in urban children with asthma: A conceptual model and exploratory study. Children’s Health Care, 33, 275–297.
Kucera, M., & Sullivan, A. (2011). The educational implications of type I diabetes mellitus: A review of research and recommendations for school psychological practice. Psychology in the Schools, 48, 587–603. doi:10.1002/pits.20573.
Lee, S., Kim, S., & Choi, J. W. (2013). Coping and resilience of adolescents with congenital heart disease. Journal of Cardiovascular Nursing (Epub ahead of print).
Long, K. A., & Marsland, A. L. (2011). Family adjustment to childhood cancer: A systematic review. Clinical Child and Family Psychology Review, 14, 57–88. doi:10.1007/s10567-010-0082-z.
Mackey, E. R., Hilliard, M. E., Berger, S. S., Streisand, R., Chen, R., & Holmes, C. (2011). Individual and family strengths: An examination of the relation to disease management and metabolic control in youth with type 1 diabetes. Families, Systems & Health, 29, 314–326.
Masten, A. S., Herbers, J. E., Cutuli, J. J., & Lafavor, T. L. (2008). Promoting competence and resilience in the school context. Professional School Counseling, 12, 76–84.
Monaghan, M. C., Hilliard, M. E., Cogen, F. R., & Streisand, R. (2009). Nighttime caregiving behaviors among parents of young children with type 1 diabetes: Associations with illness characteristics and parent functioning. Families, Systems & Health, 27, 28–38.
Monaghan, M., Horn, I. B., Alvarez, V., Cogen, F. R., & Streisand, R. (2012). Authoritative parenting, parenting stress, and self-care in pre-adolescents with type 1 diabetes. Journal of Clinical Psychology in Medical Settings, 19, 255–261.
Mu, P. F. (2005). Paternal reactions to a child with epilepsy: Uncertainty, coping strategies, and depression. Journal of Advanced Nursing, 49, 367–376.
Mu, P. F. (2008). Transition experience of parents caring of children with epilepsy: A phenomenological study. International Journal of Nursing Studies, 45, 543–551.
Mu, P., & Chang, K. (2010). The effectiveness of a programme of enhancing resiliency by reducing family boundary ambiguity among children with epilepsy. Journal of Clinical Nursing, 19, 1443–1453. doi:10.1111/j.1365-2702.2009.03075.x.
Mu, P. F., Kuo, H. C., & Chang, K. P. (2005). Boundary ambiguity, coping patterns and depression in mothers caring for children with epilepsy in Taiwan. International Journal of Nursing Studies, 42, 273–282.
Naguib, J. M., Kulinskaya, E., Lomax, C. L., & Garralda, M. E. (2009). Neurocognitive performance in children with type 1 diabetes: A meta analysis. Journal of Pediatric Psychology, 34, 271–282. doi:10.1093/jpepsy/jsn074.
Newacheck, P. W., & Taylor, W. R. (1992). Childhood chronic illness: Prevalence, severity, and impact. American Journal of Public Health, 82, 364–371.
Perfect, M. M., & Jaramillo, E. (2012). Relations between resiliency, diabetes-related quality of life, and disease markers to school-related outcomes in adolescents with diabetes. School Psychology Quarterly, 27, 29–40. doi:10.1037/a0027984.
Perfect, M. M., Levine-Donnerstein, D., Swartz, N. E., Wheeler, L., & Amaya, G. (2011). Parents’ and diabetic adolescents’ perceptions of mental health screening, assessment, and feedback. Administration and Policy in Mental Health and Mental Health Services Research, 38, 181–192. doi:10.1007/s10488-010-0312-1.
Petteway, R. J., Valerio, M. A., & Patel, M. R. (2011). What about your friends? Exploring asthma-related peer interactions. Journal of Asthma, 48, 393–399. doi:10.3109/02770903.2011.563807.
Prince-Embury, S. (2007). Resiliency scales for children and adolescents: Profiles of personal strengths. San Antonio, TX: Harcourt Assessments.
Prince-Embury, S. (2008). The resiliency scales for children and adolescents, psychological symptoms and clinical status in adolescents. Canadian Journal of School Psychology, 23, 41–56. doi:10.1177/0829573508316592.
Rearick, E. M., Sullivan-Bolyai, S., Bova, C., & Knafl, K. A. (2011). Parents of children newly diagnosed with type 1 diabetes: Experiences with social support and family management. The Diabetes Educator, 37, 508–518.
Richmond, J. B., & Beardslee, W. R. (1988). Resiliency: Research and practical implications for pediatricians. Journal of Developmental and Behavioral Pediatrics, 9, 157–163. doi:10.1097/00004703-198806000-00007.
Ritz, T., Meuret, A. E., Trueba, A. F., Fritzsche, A., & von Leupoldt, A. (2013). Psychosocial factors and behavioral medicine interventions in asthma. Journal of Consulting and Clinical Psychology, 81, 231–250. doi:10.1037/a0030187.
Robertson, S. M., Stanley, M. A., Cully, J. A., & Naik, A. D. (2012). Positive emotional health and diabetes care: Concepts, measurement, and clinical implications. Psychosomatics, 53, 1–12.
Rolland, J. S., & Walsh, F. (2006). Facilitating family resilience with childhood illness and disability. Current Opinion in Pediatrics, 18, 527–538.
Russ, S. A., Larson, K., & Halfon, N. (2012). A national profile of childhood epilepsy and seizure disorder. Pediatrics, 129, 256–264.
Sacks, J., Helmick, C., Luo, Y., Ilowite, N., & Bowyer, S. (2007). Prevalence of and annual ambulatory health care visits for pediatric arthritis and other rheumatologic conditions in the United States in 2001–2004. Arthritis & Rheumatism, 57, 1439–1445.
Sansom-Daly, U. M., Peate, M., Wakefield, C. E., Bryant, R. A., & Cohn, R. J. (2012). A systematic review of psychological interventions for adolescents and young adults living with chronic illness. Health Psychology, 31(3), 380–393.
Sanzo, M. (2008). The child with arthritis in the school setting. Journal of School Nursing, 24, 190–196.
Shaw, S. R., & McCabe, P. C. (2008). Hospital-to-school transition for children with chronic illness: Meeting the new challenges of an evolving health care system. Psychology in the Schools, 45, 74–87.
Silverstein, J., Klingensmith, G., Copeland, K., Plotnick, L., Kaufman, F., Laffel, L., et al. (2005). Care of children and adolescents with type 1 diabetes: A statement of the American Diabetes Association. Diabetes Care, 28, 186.
Smith, B. W., & Zautra, A. J. (2008). Vulnerability and resilience in women with arthritis: Test of a two-factor model. Journal of Consulting and Clinical Psychology, 76, 799–810. doi:10.1037/0022-006X.76.5.799.
Smorti, M. (2012). Adolescents’ struggle against bone cancer: An explorative study on optimistic expectations of the future, resiliency and coping strategies. European Journal of Cancer Care, 21, 251–258.
Stinson, J. N., McGrath, P. J., Hodnett, E. D., Feldman, B. M., Duffy, C. M., Huber, A. M., et al. (2010). An internet-based self-management program with telephone support for adolescents with arthritis: A pilot randomized controlled trial. The Journal of Rheumatology, 37, 1944–1952.
Streisand, R., Swift, E., Wickmark, T., Chen, R. S., & Holmes, C. S. (2005). Pediatric parenting stress among parents of children with type 1 diabetes. Journal of Pediatric Psychology, 30, 513–521.
Svavarsdottir, E. K., & Rayens, M. K. (2005). Hardiness in families of young children with asthma. Journal of Advanced Nursing, 50, 381–390.
Thorpe, C. T., Fahey, L. E., Johnson, H., Deshpande, M., Thorpe, J. M., & Fisher, E. B. (2013). Facilitating healthy coping in patients with diabetes: A systematic review. The Diabetes Educator, 39, 33–52.
Wallace, M. L., Harcourt, D., Rumsey, N., & Foot, A. (2007). Managing appearance changes resulting from cancer treatment: Resilience in adolescent females. Psycho-Oncology, 16, 1019–1027. doi:10.1002/pon.1176.
Walsh, F. (2003). Family resilience: A framework for clinical practice. Family Process, 42, 1–18. doi:10.1111/j.1545-5300.2003.00001.x.
Wideman-Johnston, T. (2011). Resilience and students with chronic illness: A literature review of fostering resilience into the lives of students with chronic illness. Journal of Educational and Developmental Psychology, 1, 127–132.
Wills, T. A., & Bantum, E. (2012). Social support, self-regulation, and resilience in two populations: General-population adolescents and adult cancer survivors. Journal of Social and Clinical Psychology, 31, 568–592. doi:10.1521/jscp.2012.31.6.568.
Wodrich, D. L., Hasan, K., & Parent, K. B. (2011). Type 1 diabetes mellitus and school: A review. Pediatric Diabetes, 12, 63–70. doi:10.1111/j.1399-5448.2010.00654.x.
Woods, K., Mayes, S., Bartley, E., Fedele, D., & Ryan, J. (2013). An evaluation of psychosocial outcomes for children and adolescents attending a summer camp for youth with chronic illness. Children’s Health Care, 42, 85–98. doi:10.1080/02739615.2013.753822.
Wu, L. M., Sheen, J. M., Shu, H. L., Chang, S. C., & Hsiao, C. C. (2013). Predictors of anxiety and resilience in adolescents undergoing cancer treatment. Journal of Advanced Nursing, 69, 158–166.
Yi, J. P., Vitaliano, P. P., Smith, R. E., Yi, J. C., & Weinger, K. (2008). The role of resilience on psychological adjustment and physical health in patients with diabetes. British Journal of Health Psychology, 13, 311–325. doi:10.1348/135910707X186994.
Yi-Frazier, J. P., Hilliard, M. E., Cochrane, K., & Hood, K. K. (2012). The impact of positive psychology on diabetes outcomes: A review. Psychology, 3, 1116–1124.
Ziadni, M. S., Patterson, C. A., Pulgarón, E. R., Robinson, M., & Barakat, L. P. (2011). Health-related quality of life and adaptive behaviors of adolescents with sickle cell disease: Stress processing moderators. Journal of Clinical Psychology in Medical Settings, 18, 335–344. doi:10.1007/s10880-011-9254-3.
Acknowledgements
The data presented in this chapter were derived from funding provided by the Institute for Mental Health Research (#2008PM803) to Michelle M. Perfect, Ph.D.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer Science+Business Media New York
About this chapter
Cite this chapter
Perfect, M.M., Frye, S.S. (2014). Resiliency in Pediatric Chronic Illness: Assisting Youth at School and Home. In: Prince-Embury, S., Saklofske, D. (eds) Resilience Interventions for Youth in Diverse Populations. The Springer Series on Human Exceptionality. Springer, New York, NY. https://doi.org/10.1007/978-1-4939-0542-3_19
Download citation
DOI: https://doi.org/10.1007/978-1-4939-0542-3_19
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4939-0541-6
Online ISBN: 978-1-4939-0542-3
eBook Packages: Behavioral ScienceBehavioral Science and Psychology (R0)