Abstract
The diagnosis of a genetic disorder in a child impacts all family members with respect to potential risks for those biologically related and the psychosocial impact associated with the disorder. The advent of new genetic technologies including microarray and whole genome sequencing poses additional challenges for genetic counselling; some relevant challenges include the volume of data obtained from these testing modalities, the interpretative uncertainty of some test results, and the possibility of incidental findings unrelated to the reason for testing. Given this, how will personalized medicine be implemented in the paediatric setting? In this chapter, we will discuss genetic counselling in the context of patient-centred and family-centred care and whether patient-centred care is just a point on the family-centred care spectrum.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Genetic counselling
- Genes
- Genome
- DNA
- Karyotype
- Microarray testing
- Whole exome/genome sequencing
- Predictive genetic testing
- Informed consent
- Respect for autonomy
The diagnosis of a genetic disorder in a child has rippling effects throughout the family. Much of the impact mirrors the psychosocial adaptation and pragmatic issues that arise any time a child falls ill; however, when there is an underlying genetic contribution to the disorder, additional issues typically emerge. Initially the genetic contributions to a disorder may not be recognized or acknowledged, nevertheless, genetic factors are estimated to account for 96 % of chronic paediatric disorders in children and prompt 71 % of paediatric hospital admissions (McCandless et al. 2004) . Therefore, concerns related to a genetic diagnosis are likely to surface more often than might otherwise have been anticipated.
Key issues inherent to the diagnosis of a genetic disorder in a child include communicating and addressing potential risks to family members. By its very nature, genetic medicine and genetic counselling involve the family unit. Whereas in previous years family members might have been offered empiric information regarding their own potential risks, our increasing ability to define the etiology of genetic disorders via genetic testing now also offers them more actionable options. The increasing availability of genetic testing may prompt some families impacted by the diagnosis of a genetic disorder to reframe their notion of family. That is, families may need to consider communicating genetic information to more than just first degree relatives (e.g., nuclear family members). The intricacies involved in the provision of genetic counselling as applied to patient-centred and family centred care models will form the basis of this chapter.
The advent of new genetic/genomic testing technologies, such as microarray and whole genome/exome sequencing (described below), holds tremendous promise for resolving the diagnostic odyssey encountered by many families when a specific diagnosis and etiology cannot be determined. These technologies are also contributing to our understanding of chronic, multigenic, and multifactorial conditions, such as autism spectrum disorder and diabetes, where the cause of these complex diseases is thought to involve an interaction of both genetic and environmental factors. Current thinking holds that genomic testing will be transformative in predicting and managing healthcare for children and their family members. In fact, many propose that genomic testing, specifically whole genome sequencing, will be offered widely to individuals including perhaps all newborn babies, to identify genetic alterations before the development of symptomatology; the results of such testing would then be used for anticipatory medical management with the intended goals of improving overall health and well-being, and reducing healthcare costs. At present, the utilization of genetic and genomic testing by non-genetics healthcare providers indicates that this testing has already transitioned into mainstream medicine.
Genomic testing, as with the implementation of many new testing modalities, presents a number of ethical and practical challenges. Some of these are not entirely new nor even unique to the field of genetics. Examples of challenges associated with genomic testing include managing the volume of data generated, interpreting multiple results of uncertain or unknown clinical significance, disclosing incidental findings (i.e., findings detected that are not related to the original indication for testing), and recontacting patients/families as re-interpretation and new information become available (Tabor et al. 2011; Sijmons et al. 2011; Ormond et al. 2010) . The landscape of genetic medicine is changing dramatically and the provision of care to children and their families in this new context merits thoughtful consideration and planning involving all stakeholders.
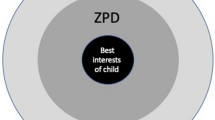
When genetic information becomes available on a child, by way of a clinical diagnosis or through the use of genetic testing, can either of the two health care delivery models, i.e., (i) paediatric patient centred care and (ii) family centred care inform clinicians in terms of providing optimal care? How do clinicians balance what might be in the best interest of the child when the child’s diagnosis and/or test results have implications for other family members? Is one health care delivery model more relevant to paediatric genetic medicine than the other? This chapter will discuss the application of these models in the context of genetic counseling and genetic testing, using whole genome sequencing as an example in a paediatric setting.
For the purposes of this chapter, patient-centred care is defined as focusing on the needs of the patient and his/her world. The clinician-patient relationship is viewed as a collaborative partnership where the patient is encouraged to be actively involved in decisions involving his/her own medical care (Epstein and Street 2011) . In contrast, the family-centred perspective values the needs of the patient’s family in that it respects “the family’s values, environment, culture, resources, needs and strengths, as well as viewing these characteristics as assets for patient care and treatment plans” (Hernandez et al. 2006) . In a paediatric genetic medicine setting, it can be difficult to disentangle the needs of the child from that of his/her family, especially given the potential implications of genetic alterations to the personal health of other family members. In order to clarify some of the concepts presented, we begin with a brief review of basic genetics and testing terminology.
1 Background—Genetic Concepts
Genes determine the instructions for how our bodies develop, grow and function. It is currently recognized that environmental factors can influence the expression of genes and this has become an important area of study but will not be addressed in this chapter. Each gene comprises a specific stretch of DNA (deoxyribonucleic acid) and is encoded by four bases: adenine (A), guanine (G), cytosine (C) and thymine (T). Simply put, the specific sequence of these bases is critical for the correct cellular instruction. Genetic errors such as the replacement of one base with another or having too few or too many copies of genes can result in a problem with development (birth defects, developmental delay, etc.) or the functioning of our cells and bodies (cancer, diabetes, etc.). Such errors are typically referred to as mutations. However, many changes in the sequence can represent benign variants that contribute to each of us being a unique individual. The term “genome” refers collectively to all of the genes in an individual.
It is currently estimated that humans have approximately 25,000 genes which are ‘lined up’ on structures called chromosomes. We typically have 23 pairs of chromosomes, or 46 chromosomes in total, and these pairs are numbered from the largest (1) to the smallest (22). The first 22 pairs are the same in males and females, while the 23rd pair is the sex chromosomes; females usually have two X chromosomes (i.e., 46, XX) and males usually have one X and one Y chromosome (i.e., 46, XY).
2 Background—Genetic Testing
When a child is suspected of having a genetic condition, genetic testing may be undertaken to determine or to confirm a diagnosis based on clinical presentation. Such testing would be considered diagnostic and may include targeted genetic testing looking for mutation(s) or change(s) in the specific gene responsible for the genetic condition in question.
Diagnostic testing approaches include chromosome analysis to screen for extra or missing chromosomal material. This testing would report an individual’s chromosomal make-up or karyotype ; an example of a relatively common karyotype alteration is trisomy 21 Down syndrome, where instead of the usual two copies of chromosome number 21, there are three copies. A far more sensitive approach currently utilized for the detection of extra or missing chromosomal material is microarray testing , also known as array-based comparative genomic hybridization (aCGH). This testing scans the whole genome to detect changes in the dosage of genetic material at a much higher resolution than conventional karyotype analysis. Such alterations are referred to as copy number variants (CNV). Another method to detect even more subtle genomic variations (single nucleotide polymorphisms or SNPs) either in the clinical or research arena is a SNP array. Detecting such alterations (i.e., CNVs and SNPs) may assist in determining the cause or possible contributors to an individual’s physical and/or intellectual disability. However, these testing modalities may also reveal incidental genetic alterations which could have reproductive or health implications not only for the child, but also for other family members. Incidental findings may not align with one’s clinical presentation; that is to say, the testing result may suggest that the individual has a condition which s/he clearly does not. The interpretive expertise of the clinician is critical for contextualizing any findings detected on testing.
As the cost continues to decrease, even newer genetic testing technologies such as exome or whole genome sequencing are transitioning from the research to the clinical arena, such that they are now becoming incorporated into testing algorithms. These tests allow for the analysis of all of the gene coding regions (exome sequencing) or of the entire genome (whole genome sequencing) for an individual, rather than the evaluation of one or a limited number of genes known to be associated with a specific disorder. Such testing not only generates huge volumes of data requiring sophisticated bioinformatics analysis for interpretation, but is likely to reveal incidental or secondary findings, and with increased frequency in comparison to microarray testing . Some of these findings may have potential health implications for which current medical management in childhood may or may not exist. Additionally, whole genome or exome sequencing undertaken on a child may unintentionally reveal genetic alteration(s) associated with adult-onset disorders; this issue of predictive testing is discussed further in the case example below. When should such unanticipated findings be disclosed and to whom? Parents can consent to testing for their children, but there are inherent ethical challenges when considering disclosure of such results to the parents, including preserving the child’s autonomy and privacy.
Another issue related to genetic testing involves changes that may be detected in a chromosomal region involving a gene(s) not previously reported (i.e., not published or catalogued in one of the databases curated and accessed by scientists and clinicians) and therefore classified as being of unknown or uncertain clinical significance. In such situations, the information available for dissemination is limited. Family studies (i.e., potentially obtaining DNA from biological parents, sibs, and other family members) are often recommended to ascertain if other family members, especially those not affected with the disorder under investigation, may have the same alteration. This can assist with determining if the change(s) identified is pathogenic (i.e., disease causing).
Genetic testing implications for family members also arise when a pathogenic mutation(s) is identified in a child as the clinician may recommend cascade testing for other family members. This would require that the parents inform other family members of both the diagnosis in their child, and the availability of genetic testing for the familial mutation. Such testing may be informative for diagnostic purposes since the condition may be present in other family members but with a milder presentation. This information may also provide relevant information for future reproductive risks (e.g., carrier status) depending on the inheritance pattern. Communication of this information to other relatives may pose challenges for some families, both logistically (e.g., may not have any contact) and psychosocially (e.g., stigmatization). Furthermore, consideration must be given to providing such information to unsuspecting relatives who, if given the choice to know, may have chosen otherwise.
In addition to pursuing genetic testing for the purposes of a diagnosis, additional genetic testing categories include predictive genetic testing , carrier testing and population screening. Predictive testing may be undertaken for individuals at increased risk for developing a disorder based on their family history. Ideally, testing is first initiated on the individual(s) in the family diagnosed with the disorder in question. If a genetic mutation were identified in that individual, then this would facilitate predictive testing for other interested but as yet asymptomatic family members. The absence of the familial mutation would allow the clinician to offer reassurance to the asymptomatic family member about not being at increased risk to develop the condition. Predictive genetic tests are often undertaken in adult patients for adult onset conditions (familial forms of breast and/or ovarian cancer, Huntington disease, early onset Alzheimer disease, etc.). In contrast, predictive testing in children may be considered for conditions where anticipatory medical management may be possible (e.g., cancer syndromes such as Li Fraumeni or von Hippel Lindau, cardiac disorders such as hypertrophic cardiomyopathy or long QT syndrome [arrhythmia], etc.). Generally, predictive testing for adult onset disorders is not undertaken in childhood unless there are medical management recommendations that might improve outcome. If no such medical management exists, testing is typically postponed until such time as the child has the capacity to participate in the decision-making process about the test and to provide informed consent (Clarke 1994; ASHG Social Issues Committees 1995; Arbour and Bioethics Committee of the Canadian Paediatric Society 2003; Borry et al. 2009) . Along the same continuum, direct to consumer (DTC) testing could impact the provision of medical care if parents were to ask for testing of their children based on their own desire for such information.
Carrier testing is primarily relevant for reproductive planning and therefore the same principles for predictive testing for adult onset disorders would apply for carrier testing of children. However, if carrier testing results might impact medical interventions, exceptions to these guidelines would be entertained. One notable exception pertains to carrier or premutation testing for fragile X syndrome, a common cause of intellectual disability in males. Given that some premutation carriers can have learning and psychological challenges and for which early intervention may be of benefit, testing for premutation status in these cases may be undertaken under the auspices of medical management.
3 Ethical Issues and Care Models
When undertaking genetic testing in a child, consideration must be given to key ethical tenets such as respect for autonomy (Beauchamp and Childress 2001a) . However, with the integration of whole genome/exome sequencing in the clinical arena , and the potential amplification of ethical issues in general, a guiding medical ethics framework is necessary. Challenges in developing such a framework include balancing parents’ desire/rationale for testing and the child’s right to autonomy and privacy. As well disclosure of results would necessitate consideration of what information specifically to provide, to whom and when; and the implications of testing results for extended family members.
The guiding principles of paediatric patient-centred care and family-centred care have been articulated previously. At first glance, one might assume that a paediatric patient-centred care model would not resonate in a specialty where the potential for familial transmission is a key concept, however, elements of this model are in fact highly applicable. In the family-centred care model, the family and healthcare provider are meant to work in partnership to make decisions that ideally should be in the best interests of the child. Difficulties with this model can arise, however, when there are competing interests of different family members, whether or not articulated, which can interfere with the child’s best interests. As well, family members may align in their stated interests and decisions but these may differ from the recommendations of the clinician(s). Is it possible to draw on the strengths of both models, i.e., an integrated approach, to guide best clinical practice? We present a case, involving whole genome sequencing, to facilitate the above discussion with a focus on disclosure of incidental findings.
3.1 Case 1
An eight-year-old child, Lisa, was referred for genetic assessment and genetic counselling because she was born with a cleft palate (opening in the roof of her mouth) and was also recently diagnosed with a mild intellectual disability. She attends the initial assessment with both of her parents, who are reportedly healthy and have no similar learning or physical issues. Lisa’s mother is 35 years of age and her father is 38 years of age. As well, Lisa has two brothers, one of whom is 12 years old the other 5 years old; neither brother attends the appointment and the parents note that they are both healthy and without similar issues. The family history is non-contributory, with both parents having healthy sibs, all of whom are younger than themselves. The maternal grandparents are alive and in relatively good health but the paternal grandparents died in a motor vehicle accident a number of years ago. After obtaining informed consent from the parents, whole genome sequencing is undertaken on Lisa and a genetic alteration is identified which would account for her clinical presentation; specifically, the report notes a submicroscopic deletion of chromosome 22. This is a well-documented finding in the literature and referred to as 22q11.2 deletion syndrome. Incidentally, a different genetic change associated with an increased risk for breast and ovarian cancer in adulthood is also found, that is a deletion at chromosome region 13q13.1. This region houses the BrCa2 gene, and mutations of this gene can result in a significantly increased risk for breast and ovarian cancer. If this deletion at chromosome region 13q13.1 were inherited from one of Lisa’s parents, this could confer an increased risk for that parent to develop cancer.
3.2 Case Discussion
The utilization of whole genome sequencing in the above case was undertaken for the purpose of establishing a diagnosis. Testing did in fact reveal a pathogenic change (i.e., deletion of 22q11.2), and provided a diagnosis consistent with Lisa’s clinical findings. Unexpectedly, the report also noted the detection of an incidental, predictive finding associated with a potential increased risk of an adult onset condition (i.e., breast and ovarian cancer) in an eight-year-old child. In the current climate, parents seeking testing for a BrCa1 or BrCa2 mutation in their young child because of a positive family history of breast and/or ovarian cancer would be engaged in a discussion about deferring this request until such time as the child is old enough to participate in the decision-making process regarding the pros and cons of testing. This approach is based upon an extensive review process with consensus being reached by a number of professional organizations and resulting in the published guidelines noted earlier in this chapter. These policy statements stipulate that when there is no medical benefit to be gained from testing for an adult-onset condition in childhood, testing of minors should be deferred. Although the deletion on chromosome 13 involving the BrCa2 gene would not lead to revised medical management in childhood, it could pose significant health implications for one of Lisa’s parents and, potentially, their extended relatives. Screening and surgical options exist for adults with a BrCa1 or BrCa2 mutation and these interventions can significantly impact health outcomes.
Disclosure to Lisa’s parents of the pathogenic deletion of 22q11.2 would be undertaken, but should the incidental finding of the potential increased risk for breast and ovarian cancer also be disclosed? In considering this question, one might first look to published guidelines regarding the informed consent process and the delineation of such issues, including the plan for results disclosure (Canadian Institutes of Health Research 2010; Thorogood et al. 2012; Clayton and McGuire 2012) . In the case of offering whole genome sequencing in a research context, the research and clinical teams would develop a plan regarding disclosure of test results including incidental findings. The clinicians/researchers involved would then review the possible outcomes with the family, prior to initiation of testing, and ask them to consider what they would prefer to learn and the potential implications of categories or ‘bins’ of information (Berg et al. 2011) . The informed consent process in such research protocols can serve to guide the transition of whole genome sequencing from the research realm to the clinical arena; however, of equal importance would be to look at established healthcare models, as these might inform clinical practice. What follows next is a discussion of the practical applications of the paediatric patient-centred and family-centred healthcare delivery models in trying to address the health and ethical constructs that might inform best clinical practice given the issues inherent in our case.
4 Healthcare Delivery Models and Genetic Care
4.1 Paediatric Patient-Centred Care Model
As mentioned previously in this chapter, the premise of the patient-centred care model involves the active participation of the patient in decisions involving his/her health and medical care. In the adult healthcare world, active participation of the patient is plausible but even in this setting, additional implications arise in genetic/genomic medicine given the potential relevance of pathogenic alterations to one’s family members. Nonetheless, such issues would be discussed with the individual presenting for consultation and testing, and while s/he would be encouraged to discuss these implications, his/her autonomy need not be breached. Issues regarding discretion vs. healthcare providers’ duty to warn at-risk relatives have been considered in the genetic/genomic context, and generally the privacy of the patient is maintained (Knoppers et al. 1998; Lacroix et al. 2008) .
In the paediatric healthcare setting, we considered two potential approaches regarding disclosure of testing results pertaining to incidental findings which are medically actionable in adulthood. Firstly, one could infer that the patient-centred care model would entail communicating relevant information to children, at their level of understanding, encouraging children to participate in medical decision-making and seeking their assent. Obtaining assent vs. consent from children pertains to their having some capacity for decision-making but this can vary even between children of the same age. As such, healthcare providers would need to ascertain the particular capacity of each child. Therefore, to invoke the patient-centred care model when the patient is a young child/an infant with no decision making capacity or where the child does not have the intellectual capacity to engage in such a discussion is simply not feasible.
Another approach would be to not disclose the incidental finding(s) but rather to ‘lock’ them away in the child’s medical record until such time as the child has the intellectual and emotional maturity to decide whether or not to receive them (i.e., capable minor or adult). In this regard, the parents might be viewed solely as a proxy for safeguarding undisclosed information on behalf of their child. This would imply that the parents would not be engaged in any decision-making regarding the incidental test result(s) for their child.
In the case scenario posed above, one would need to work out the practical issues of locking away Lisa’s incidental genetic testing information and construct a plan for future contact and communication. Given the basic tenets of the paediatric patient-centred care model, locking away Lisa’s test results regarding the incidental finding would maintain her privacy and autonomy but might this negatively impact the health and well-being of her parents and other family members? Moreover, one might anticipate that negative health sequelae in one of Lisa’s parents could subsequently impact her own well-being.
Our case is further compounded by Lisa’s young age and her intellectual disability, as she may have a very limited understanding, or none at all, of the testing process and results. Given this, perhaps the risks inherent in disclosure of incidental test results to Lisa’s parents can be rationalized, i.e., breaching her privacy and autonomy. Implicit in the discussion regarding the deletion involving the BrCa2 gene is the potential increased risk of cancer in one of her parents and possibly their extended family members. Although the paediatric patient-centred care model advocates that the role of the healthcare provider is to respect the patient and his/her needs, genetic test results transcend beyond the individual patient. Key ethical tenets of beneficence and non-malificence can easily be extended to preserving the child’s well-being by having both parents remain in good health (Beauchamp and Childress 2001b) . Contextualizing the incidental finding for the parents with respect to their own health could have the unintended benefit of invoking anticipatory healthcare for one of them. These significant health benefits can also be extended to other family members. Potential discord arises in the genetic/genomic medicine setting when one tries to isolate the genetic test results and ignores the potential benefits to other family members.
4.2 Family-Centred Care Model
In contrast to the paediatric patient-centred care model where the primary focus is the child or patient, the family-centred care model views the child within the context of his/her family. The family, with its own goals, values and belief systems is seen as a source of strength for the child and integral to promoting the child’s health and medical care. In other words, the family-centred care model “recognizes the family as central to the child’s life (and) accepts parental expertise as an information resource for a child and an important component of health care delivery” (Brown et al. 2008) .
Defining what constitutes “the family” is fundamental to extrapolating this model to genetics/genomic medicine. The definition of family can vary from a two-parent household to one where the child is cared for and raised in an extended family (aunts, uncles, grandparents, etc…). How the family is defined in this model has relevance to its application to the case scenario involving Lisa. In a two-parent family, the family-centred care model would look to Lisa’s parents for their expertise as they would know their daughter and her needs best. This family-centred care model would support disclosure of the incidental findings to Lisa’s parents given their involvement in decision-making for her and in facilitating interventions. What is not so clear is how this model would inform practice with regards to communicating genetic test results to other family members (outside of the two-parent household) who might also be at risk. With regards to their extended family, one can hypothesize that if the extended family is seen as the expert in Lisa’s care, then communication of the incidental findings would occur in their presence, and by so doing, would accomplish the goal of sharing test results with at-risk relatives. Given that some family members have the “right not to know,” disclosure to the extended family would have implications for breach of individual family member’s right to autonomy and privacy. Additional complexities pertaining to communication and decision-making can arise when dyadic coalitions are formed that include any two of the following stakeholders: capable minor, parents, extended family members, healthcare providers (Gilbar 2005) . These discussion points are beyond the scope of this chapter but are important issues to touch upon. Equally possible with the extended family version of the family-centred care model is differing expert views on what is in the best interest of the child and divided consensus with regards to disclosure of incidental findings. Granted this could also occur with the two-parent version of family; however, the likelihood is greater when more family members are involved.
5 Summary
Overall, the principles guiding the paediatric patient-centred and family-centred care models satisfy specific requisites and appear to be somewhat independent in their applicability to our case example with Lisa. Neither model adequately guides best clinical practice where genetic/genomic medicine is concerned, given that genetic disorders affect not only the child but also have implications for the extended family. Perhaps the designations of paediatric patient-centred and family-centred care are somewhat arbitrary distinctions in the discipline of genetics/genetic counselling . The American Academy of Pediatrics (AAP) recently issued a Policy Statement (Pediatrics 2012) which advocates for the involvement of the family, as well as the need to work in partnership with paediatric patients themselves in decision-making about their own medical care where developmentally appropriate. Recommendations outlined in this policy statement include “respect for families’ unique insights into and understanding of their child’s behavior and needs….and [to] appropriately incorporate family preferences into the care plan” (Pediatrics 2012). Additionally, paediatric healthcare providers should actively involve children, including children with physical and/or intellectual disabilities in decision-making about their own health by adapting the information to their level of understanding (Pediatrics 2012).
Although the AAP patient and family-centred care model integrates a number of highly relevant constructs of the two models (i.e., the paediatric patient-centred care model and the family-centred care model) discussed in this chapter, the issues inherent in caring for a young child with a genetic condition and his/her family continue to pose challenges not addressed by any of these healthcare delivery models. Perhaps it is unrealistic to assume that existing healthcare delivery models will address all of the underlying nuances specific to each medical specialty and, conceivably, it is not necessary to have a “one size fits all” model. However, with the genomic era of personalized medicine upon us, there is a pressing need to develop a model that will help shape best clinical practice guidelines for optimal patient and family care in genetics.
References
Arbour, L., and Bioethics Committee of the Canadian Paediatric Society. 2003. Position statement (B 2003-01): Guidelines for genetic testing of healthy children. Paediatric Child Health 8 (1): 42–45.
ASHG Social Issues Committees. 1995. ASHG/ACMG REPORT: Points to consider: Ethical, legal, and psychosocial implications of genetic testing in children and adolescents. American Journal of Human Genetics 57:1233–1241.
Beauchamp, T., and J. Childress. 2001a. Principles of biomedical ethics. 5th ed. 57–103. New York: Oxford University Press.
Beauchamp, T., and J. Childress. 2001b. Principles of biomedical ethics. 5th ed. 113–214. New York: Oxford University Press.
Berg, J. S., M. J. Khoury, and J. P. Evans. 2011. Deploying whole genome sequencing in clinical practice and public health: meeting the challenge one bin at a time. Genetics in medicine: official journal of the American College of Medical Genetics 13 (6): 499–504. doi:10.1097/GIM.0b013e318220aaba.
Borry, P., G. Evers-Kiebooms, M. C. Cornel, A. Clarke, and K. Dierickx. 2009. On behalf of the Public and Professional Policy Committee (PPPC) of the European Society of Human Genetics (ESHG). Genetic testing in asymptomatic minors Background considerations towards ESHG Recommendations. European journal of human genetics: EJHG 17 (6): 711–719. doi:10.1038/ejhg.2009.25.
Brown, K., S. E. Mace, A. M. Dietrich, S. Knazik, N. E. Schamban. 2008. Patient and family-centred care for pediatric patients in the emergency department. CJEM: Canadian Journal of Emergency Medical Care 10 (1): 38–43.
Canadian Institutes of Health Research. 2010. Tri-Council policy statement: Ethical conduct for research involving humans. Ottawa, Canada.
Clarke, A. 1994, Oct. The genetic testing of children. Working party of the clinical genetics society (UK). Journal of medical genetics 31 (10): 785–797.
Clayton, E. W., and A. L. McGuire. 2012. The legal risks of returning results of genomics research. Genetics in Medicine: Official Journal of the American College of Medical Genetics 14 (4): 473–477. doi:10.1038/gim.2012.10.
Epstein, R., and R. Street Jr. 2011. The values and value of patient-centered care. Annals of Family Medicine 9:100–103. doi:10.1370/afm.1239.
Gilbar, R. 2005. The status of the family in law and bioethics: The genetic c ontext, 185. England: Ashgate Publishing Limited.
Hernandez, V. R., K. Selber, and M. S. Tijerina. 2006. Visioning family-centered care in genetics: What parents and providers have to say. Journal of Genetic Counseling 350. doi:10.1007/s10897–006-9032–9.
Knoppers, B. M., C. Strom, E. Wright Clayton, T. Murray, W. Fibison, L. Luther, P. R. Billings, L. Godmilow, and B. Handelin. 1998. Professional disclosure of familial genetic information. American Journal of Human Genetics 62:474–483.
Lacroix, M., G. Nycum, B. Godard, and B. M. Knoppers. 2008, Feb. 26. Should physicians warn patients’ relatives of genetic risks? CMAJ 178(5). doi:10.1503/cmaj.070956.
McCandless, S. E., J. W. Brunger, and S. B. Cassidy. 2004. The burden of genetic disease on inpatient care in a children’s hospital. American Journal of Human Genetics 74 (1): 121–127.
Ormond, K. E., M. T. Wheeler, L. Hudgins, T. E. Klein, A. J. Butte, R. B. Altman, E. A. Ashley, and H. T. Greely. 2010. Challenges in the clinical application of whole-genome sequencing. Lancet. doi:10.1016/S0140–6736(10)60599–5.
Pediatrics. 2012. Patient- and family-centered care and the pediatrician’s role. American Academy of Pediatrics 129:394–404.
Sijmons, R. H., I. M. Van Langen, J. G. Sijmons. 2011. A clinical perspective on ethical issues in genetic testing. Accountability in Research 18 (3): 148–162. doi:10.1080/08989621.2011.575033.
Tabor, H. K., B. E. Berkman, S. C. Hull, and M. J. Bamshad. 2011. Genomics really gets personal: How exome and whole genome sequencing challenge the ethical framework of human genetics research. American Journal of Medical Genetics Part A 155:2916–2924.
Thorogood, A., B. M. Knoppers, W. J. Dondorp, and G. M. W. R. de Wert. 2012. Whole-genome sequencing and the physician. Clinical Genetics 81:511–513. doi:10.1111/j.1399–0004.2012.01868.x.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer Science+Business Media Dordrecht
About this chapter
Cite this chapter
Shuman, C., Babul-Hirji, R. (2014). Clinical Genetics Practice: Integrating Paediatric Patient and Family-Centred Care. In: Zlotnik Shaul, R. (eds) Paediatric Patient and Family-Centred Care: Ethical and Legal Issues. International Library of Ethics, Law, and the New Medicine, vol 57. Springer, New York, NY. https://doi.org/10.1007/978-1-4939-0323-8_13
Download citation
DOI: https://doi.org/10.1007/978-1-4939-0323-8_13
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4939-0322-1
Online ISBN: 978-1-4939-0323-8
eBook Packages: MedicineMedicine (R0)