Abstract
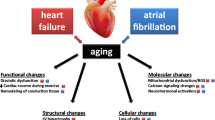
Age per se is the major risk factor for cardiovascular disease. Elucidation of the age-associated alterations in cardiac and arterial structure and function at both the cellular and molecular levels provides valuable clues that may assist in the development of effective therapies to prevent, to delay, or to attenuate the cardiovascular changes that accompany aging and contribute to the clinical manifestations of chronic heart failure. Changes in cardiac cell phenotype that occur with normal aging, as well as in HF associated with aging, include deficits in β-adrenergic receptor (β-AR) signaling, increased generation of reactive oxygen species (ROS), and altered excitation–contraction (EC) coupling that involves prolongation of the action potential (AP), intracellular Ca2+ (Cai 2+) transient and contraction, and blunted force and relaxation-frequency responses. Evidence suggests that altered sarcoplasmic reticulum (SR) Ca2+ uptake, storage, and release play central role in these changes, which also involve sarcolemmal L-type Ca2+ channel (LCC), Na+−Ca2+ exchanger (NCX), and K + channels.
In spite of the interest in the physiology of the age-associated changes in cardiovascular structure and function, however, cardiovascular aging has remained, for the most part, outside of mainstream clinical medicine. This is largely because the pathophysiologic implications of these age-associated changes are largely underappreciated and are not well disseminated in the medical community. In fact, age has traditionally been considered a nonmodifiable risk factor. Policy makers, researchers, and clinicians need to intensify their efforts toward identification of novel pathways that could be targeted for interventions aiming at retardation or attenuation of these age-associated alterations that occur in the heart and arteries, particularly in individuals in whom these alterations are accelerated. Translational studies would then examine whether these strategies (i.e., those targeting cardiovascular aging) can have a salutary impact on the adverse cardiovascular effects of accelerated cardiovascular aging. As such, cardiovascular aging is a promising frontier in preventive cardiology.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Ventricular Myocytes
- Action Potential Duration
- Left Ventricle Wall
- Cardiovascular Aging
- Action Potential Prolongation
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Introduction
Hypertension, atherosclerosis, and resultant chronic heart failure (HF) reach epidemic proportions among older persons, and the clinical manifestations and the prognoses of these maladies worsen with increasing age (Fig. 21.1).
A steady stream of incremental knowledge, derived from both animal and human studies, has established that several of the aging-associated changes in the heart and in the walls of the central arteries are, themselves, potent and independent risk factors for cardiovascular diseases. This suggests that these age-associated alterations in arterial and cardiac structure and function may link aging to the risk for these disease states. Thus, one way to conceptualize why the clinical manifestations and the prognosis of CV diseases worsen with age is that in older individuals, the specific pathophysiologic mechanisms that cause clinical disorders are superimposed on heart and vascular substrates that are modified by aging (Fig. 21.2).
Schematic of cardiovascular factors as they relate to clinical practice threshold [Adapted from Najjar SS, Lakatta EG, Gerstenblith G. Cardiovascular Aging: The Next Frontier in Cardiovascular Prevention. In Blumenthal R, Foody J, Wong NA (editors), Prevention of Cardiovascular Disease: Companion to Braunwald’s Heart Disease. Philadelphia: Saunders, 2011:415–432]
Imagine that age increases as one moves from the lower to the upper part of Fig. 21.2 and that the line bisecting the top and bottom parts represents the clinical practice “threshold” for disease recognition. Entities above the line are presently classified as “diseases,” and lead to heart and brain failure.
Arterial and cardiac changes presently thought to occur as a result of the “normal aging process” are depicted below the line. These age-associated changes in cardiac and vascular properties alter the substrate on which cardiovascular disease becomes superimposed in several ways. First, they lower the extent of disease severity required to cross the threshold that results in clinically significant signs and symptoms. Aging should no longer be viewed as an immutable risk factor. In one sense, those processes below the line in Fig. 21.2 ought not to be considered to reflect normal aging, because these are specific risk factors for the diseases that they relate to, and thus might be targets of interventions designed to decrease the occurrence or manifestations of cardiovascular disease at later ages.
Because many of the age-associated alterations in cardiovascular structure and function, at both the cellular and molecular levels, have already been identified as specific risk factors for cardiovascular diseases, there is an urgency to incorporate cardiovascular aging into clinical medicine. Such a strategy would be aimed at treatment (preventative measures) to retard what is now considered to be normal aging.
Cardiac Aging in Humans
A unified interpretation of identified cardiac changes that accompany advancing age in otherwise healthy persons suggests that at least in part, these are adaptive, occurring to some extent in response to arterial changes that occur with aging (Fig. 21.3) [1].
Arterial and cardiac changes that occur with aging in normotensives and at any age in hypertensives are shown. One interpretation of the constellation (flow of arrows) is that vascular changes lead to cardiac structural and functional alterations that maintain cardiac function. LV left ventricular (Modified from Lakatta EG. Normal Changes of Aging. In: Abrams WB, Berkow R (Eds), Merck Manual of Geriatrics, Rahway, N.J.: Merck Sharp & Dohme Research Laboratories, 1990, pp. 310–325)
With advancing age, the walls of the left ventricle (LV) increase in thickness, in part, resulting from an increase in arterial impedance in ventricular myocyte size and increase in size and increase in LV wall thickness; this helps to moderate the increase in LV wall tension. Modest increases in collagen levels also occur with aging.
Prolonged contraction of myocytes within the thickened LV wall maintains a normal ejection time in the presence of the late augmentation of aortic impedance. This preserves the systolic cardiac pumping function at rest. One disadvantage of prolonged contraction is that, at the time of the mitral valve opening, myocardial relaxation is relatively more incomplete in older than in younger individuals, and this causes the early LV filling rate to be reduced in older individuals.
Structural changes and functional heterogeneity occurring within the left ventricle with aging may also contribute to this reduction in peak LV filling rate. However, concomitant adaptations—left atrial enlargement and an enhanced atrial contribution to ventricular filling—compensate for the reduced early filling and prevent a reduction of the end-diastolic volume. Age-associated changes in the tissue levels of or responses to growth factors (catecholamines, angiotensin II, endothelin, TGF-β, or fibroblast growth factor) and cytokines that influence myocardial or vascular cells or their extracellular matrices (see below) likely have a role in the schema depicted in Fig. 21.3.
Biologic sex is a well-recognized factor in the physiology and pathophysiology of the cardiovascular system, including the aging heart (reviewed in [2, 3]). Postmortem morphometric assessments in non-failing human hearts have shown extensive age-related myocyte loss and hypertrophy of the surviving myocytes in male hearts but preserved ventricular myocardial mass and average cell diameter and volume in aging female hearts. These sex differences may stem, in part, from differences in the replicative potential of cardiac myocytes. Analysis of gene expression differences by sex and age in samples of the left ventricle from patients with dilated cardiomyopathy has identified more than 1,800 genes displaying sexual dimorphism in the heart. A significant number of these genes were highly represented in gene ontology pathways involved in ion transport and G protein-coupled receptor signaling [4].
Cardiovascular Reserve in Humans
Impaired heart rate acceleration and impaired augmentation of blood ejection from the left ventricle, accompanied by an acute modest increase in LV end-diastolic volume in males, are the most dramatic changes in cardiac reserve capacity that occur during aging in healthy, community-dwelling persons (Table 21.1).
Mechanisms that underlie the age-associated reduction in maximum ejection fraction are multifactorial and include a reduction in intrinsic myocardial contractility, an increase in vascular afterload, and an arterial–ventricular load mismatch.
Ventricular load is the opposition to myocardial contraction and the ejection of blood; afterload is the component of load that pertains to the time after excitation, as opposed to preload, before excitation. Although these age-associated changes in cardiovascular reserve are insufficient to produce clinical heart failure, they do affect its clinical presentation, that is, the threshold for symptoms and signs or the severity and prognosis of heart failure secondary to any level of disease burden (e.g., chronic hypertension that causes either systolic or diastolic heart failure).
A sizeable component of the age-associated deficit in cardiovascular reserve is composed of diminished effectiveness of the autonomic modulation of heart rate, LV contractility, and arterial afterload. The essence of sympathetic modulation of the cardiovascular system is to ensure that the heart beats faster; to ensure that it retains a small size, by reducing the diastolic filling period, reducing LV afterload; to augment myocardial contractility and relaxation; and to redistribute blood to working muscles and to skin to dissipate heat. Each of the deficient components of cardiovascular regulation with aging, that is, heart rate (and thus filling time), afterload (both cardiac and vascular), myocardial contractility, and redistribution of blood flow, exhibits a deficient sympathetic modulation [1].
Multiple lines of evidence support the idea that the efficiency of postsynaptic β-adrenergic signaling declines with aging [1]. One line of evidence stems from the observation that cardiovascular responses to β-adrenergic agonist infusions at rest decrease with age [1]. A second type of evidence for a diminished efficacy of postsynaptic β-adrenergic receptor (β-AR) signaling is that acute β-adrenergic receptor blockade changes the exercise hemodynamic profile of younger persons to make it resemble that of older individuals. Significant beta blockade-induced LV dilation occurs only in younger subjects [5]. The heart rate reduction during exercise in the presence of acute β-adrenergic blockade is greater in younger vs. older subjects [5], as are the age-associated deficits in LV early diastolic filling rate, both at rest and during exercise [5]. It has also been observed in older dogs that the age-associated increase in aortic impedance during exercise is abolished by acute β-adrenergic blockade [6].
Apparent deficits in sympathetic modulation of cardiac and arterial functions with aging occur in the presence of exaggerated neurotransmitter levels. Plasma levels of norepinephrine and epinephrine, during any perturbation from the supine basal state, increase to a greater extent in older compared with younger healthy humans. The age-associated increase in plasma levels of norepinephrine results from an increased spillover into the circulation and, to a lesser extent, reduced plasma clearance. The degree of norepinephrine spillover into the circulation differs among body organs; increased spillover occurs within the heart. Deficient norepinephrine reuptake at nerve endings is a primary mechanism for increased spillover during acute graded exercise. During prolonged exercise, however, diminished neurotransmitter reuptake might also be associated with depletion and reduced release and spillover. Cardiac muscarinic receptor density and function are also diminished with increasing age and might contribute to the decrease in baroreflex activity observed in aged subjects [7].
Age-Associated Cell and Molecular Changes in Heart Cells
Cellular and molecular mechanisms implicated in age-associated changes in myocardial structure and function in humans have been studied largely in rodents (Table 21.2).
The altered cardiac structural phenotype that evolves with aging in rodents includes an increase in LV mass due to an enlargement of myocyte size [8] and focal proliferation of the matrix in which the myocytes reside, which may be linked to an altered cardiac fibroblast number or function. The number of cardiac myocytes becomes reduced because of necrosis and apoptosis, with the former predominating [9]. Putative stimuli for cardiac cell enlargement with aging in rodents include an age-associated increase in vascular load due to arterial stiffening and stretching of cells caused by dropout of neighboring myocytes [10]. Stretch of cardiac myocytes and fibroblasts initiates growth factor signaling (e.g., angiotensin II/TGF-β) that, in addition to modulating cell growth and matrix production, leads to apoptosis [11]. The expression of atrial natriuretic [12] and opioid [13] peptides, molecules that are usually produced in response to chronic stress, is increased in the senescent rodent heart.
Excitation–Contraction Coupling in the Aging Heart
Ca2+ influx via L-type calcium channels (LCC) has a dual role in cardiac EC coupling: peak L-type Ca2+ current (ICaL) provides the primary “trigger” for sarcoplasmic reticulum (SR) Ca2+ release, while the integrated Ca2+ entry replenishes the SR Ca2+ content available for release. The SR Ca2+ release and uptake play key roles in the regulation of cardiac contraction and relaxation. The SR Ca2+-transporting proteins include the sarcoplasmic reticular Ca2+-ATPase (SERCA2), its inhibitory protein phospholamban (PLB), the Ca2+-storage protein calsequestrin (CSQ), and the SR Ca2+ release channel (ryanodine receptor; RyR). The SR Ca2+ cycling is further modulated by Ca2+ influx through LCC and by Ca2+ transport via Na+–Ca2+ exchanger (NCX) (Fig. 21.4).
Coordinated changes in the expression and function of proteins that regulate several key steps of the cardiac EC coupling process (Fig. 21.4) occur in the rodent heart with aging. Prolonged time to peak and slower relaxation of contraction (Fig. 21.5), typical for aged myocardium [14–19], are attributable to changes in both the αMHC and βMHC protein ratio (Table 21.2) [1] and in the configuration of the Ca2+ transient. A slower decay of the Cai 2+ transient is a hallmark of the aged cardiac myocyte (Fig. 21.4 and Table 21.1) (Fig. 21.5).
Action potential (a), isometric contraction (b), and cytosolic Ca2+ (Cai) transient (c), measured via aequorin luminescence, in isometric right ventricular papillar muscles isolated from the hearts of young adult and senescent Wistar rats, are shown. (Inset) Time course of the Cai transient (1) relative to that of contraction (2). (d) Effect of age on Ca2+ accumulation velocity by sarcoplasmic reticulum (SR) isolated from senescent and adult Wistar rat hearts. (a) and (b): Reprinted from Spurgeon HA, Steinbach MF, Lakatta EG. Chronic exercise prevents characteristic age-related changes in rat cardiac contraction. Am J Physiol 1983; 244:H513–H518. With permission from American Physiological Society. (c): Reprinted from Orchard CH, Lakatta EG. Intracellular calcium transients and developed tensions in rat heart muscle. A mechanism for the negative interval–strength relationship. J Gen Physiol 1985; 86: 637–651. With permission Rockefeller University Press. (d): Reprinted from Froehlich JP, Lakatta EG, Beard E, Spurgeon HA, Weisfeldt ML, Gerstenblith G. Studies of sarcoplasmic reticulum function and contraction duration in young adult and aged rat myocardium. J Mol Cell Cardiol 1978; 10:427–438. With permission from Elsevier
Action Potential Prolongation
L-Type Ca2+ Channel
Age-associated prolongation of the action potential (AP) (Fig. 21.5) [20–23] is thought to stem, in part at least, from changes in L-type Ca2+ channel characteristics [20, 22, 24]. Perspectives on how age affects ICaL characteristics differ among studies, depending upon species, stress, and age range studied. Peak density of ICaL in ventricular myocytes from senescent (21–25 months) does not differ from that of young (2–3 months) male Wistar rats [22, 25] and does not differ between 20–22 and 10- to 12-month-old male FVB mice [26]. ICaL inactivates more slowly in myocytes from older vs. younger Wistar rats [22, 24], and this might partially account for prolongation of the AP reported in senescent Wistar and Fisher 344 rat hearts [22, 23]. In contrast, in ventricular myocytes isolated from young adult (6 months) and aged (27 months) Fischer 344 or Long–Evans rats, however, an age-associated decrease in peak density of ICaL was observed and was accompanied by a slower inactivation and a greater amplitude of transient outward current (ITO) [27]. Compared to young myocytes, AP duration in these myocytes from aged rats was longer at 90 % of repolarization but shorter at 20 and 75 % of repolarization [27].
In ventricular myocytes isolated from young (2 months) and senescent (20–27 months) C57/BL6 mice (sex unspecified), peak ICaL density was similar at stimulation rates of 2–8 Hz but higher in myocytes of the older group at 0.4 and 1 Hz [28]. The ICaL time integral (a function of peak amplitude and inactivation rate) normalized to cell capacitance did not differ with age during 6 Hz stimulation. Compared to young cells, ICaL time integral in aged myocytes was significantly smaller at 8 Hz and larger at 0.4 Hz [28]. In ventricular myocytes isolated from young adult (~7 months) and aged (~24 months) male and female B6SJLF1/J mice [14] stimulated at 2 Hz, a significant reduction in peak ICaL density, accompanied by a significantly slower inactivation, occurred in aged vs. young adult myocytes from males. No age-associated changes in ICaL characteristics were identified in the females. In myocytes isolated from the hearts of young (18 months) and aged (8 years) female sheep, the AP duration and both the peak ICaL and integrated Ca2+ entry were significantly greater in aged cells [20].
Ca2+ influx via LCC is a complex function of several interdependent mechanisms: voltage-dependent modulation; Ca2+-dependent modulation via direct binding to LCC of Ca2+–calmodulin and via calmodulin-dependent protein kinase II (CaMKII); and β-adrenergic modulation via protein kinase A (PKA) signaling. Voltage-dependent changes may be consequent to prolongation of the AP duration that accompanies advancing age and manifested by reduced peak amplitude accompanied by slower inactivation/larger time integral of ICaL (e.g., [29]). Ca2+-mediated effects may contribute to frequency-dependent reduction in the amplitude and time integral of ICaL [28] due to rate-dependent diastolic Ca2+ accumulation, which slows the rate of LCC recovery from inactivation in both normal and failing cardiac myocytes (reviewed in [30]). In addition, Ca2+-dependent cross talk between LCC and RyR [30] may facilitate Ca2+ influx via LCC in the presence of slower and/or smaller SR Ca2+ release in aging myocardium. For instance, buffering of Cai 2+ with EGTA eliminated age-related differences in the AP configuration and the time course of ICaL inactivation in myocytes from senescent and young rats [22].
Reductions in outward K+ currents [22] also contribute to the prolonged AP in cardiocytes of the aged heart. Of particular interest is the role of ITO as an indirect modulator of EC coupling in cardiac cells (reviewed in [31]). Specifically, recent studies have provided evidence that the early repolarization phase may considerably influence the entire AP waveform and that ITO is the main current responsible for this phase. Decreased ITO density is observed in immature and aging myocardium, as well as during several types of cardiomyopathy and HF, i.e., under conditions in which SR function is depressed.
The AP prolongation that evolves during aging and accompanies heart failure favors Ca2+ influx during the depolarization and limits voltage-dependent Ca2+ efflux via NCX and thus may be adaptive since it provides partial compensation for SR deficiency, although possibly at the cost of asynchronous SR Ca2+ release and greater propensity to triggered arrhythmias [31].
SR Ca2+ Pump
The development of the Cai 2+ transient is dependent primarily on the amount and the rate of Ca2+ release from the SR, and the decline of the Cai 2+ transient and the amount of Ca2+ available for subsequent release are dependent primarily on Ca2+ sequestration by the SR. Sequestration of Ca2+ by the SERCA2 pump serves a dual function: (1) to cause muscle relaxation by lowering the cytosolic Ca2+ and (2) to restore SR Ca2+ content necessary for subsequent muscle contraction.
An age-associated reduction in the rate of rise and the amplitude of the Cai 2+ transient (systolic dysfunction), as well as the rate of decline of the Cai 2+ transient (diastolic dysfunction), appears to result, in large part, from impaired Ca2+ pumping by SERCA2. These changes have been extensively documented in biochemical and functional studies [32–36]. At the molecular level, they are attributable to a reduced protein expression of SERCA2 or its ratio to PLB and/or reduced phosphorylation of the SERCA2–PLB complex by PKA and CaMK [36–38]. A shift of SERCA2b distribution to the subsarcolemmal space has also been suggested [28].
The age-associated reduction in SERCA2 mRNA levels is well documented (Table 21.2). The majority of studies in aging vs. younger rats have shown a significant reduction in protein levels of SERCA2 [19, 34, 35, 39]. In contrast, most studies in aging mice have shown unchanged levels of SERCA2 [16, 28, 40]. Apart from the phosphorylation status of SERCA2–PLB complex, discussed later, SR Ca2+ uptake is dependent on the relative levels of both proteins, i.e., reduced at lower SERCA2/PLB ratio [41].
The majority of studies reporting expression levels of both SERCA2 and PLB showed reduced SERCA2/PLB ratios in aging rodent hearts. Increasing SERCA/PLB ratio through in vivo gene transfer of SERCA2a markedly improved rate-dependent contractility and diastolic function in 26-month-old rat hearts [34]. Functional improvement consequent to increasing SERCA/PLB ratio by PLB suppression was also reported in human failing myocytes [42]. On the other hand, PLB ablation in transgenic mouse models of HF was beneficial only in some models (reviewed in [41, 43]).
Age-associated decline in the Ca2+-sequestering activity of SERCA2 in rodent myocardium has been well documented both by biochemical studies in isolated SR vesicles and by biophysical studies in cardiac preparations [32–36].
In addition to a reduced content of SERCA2 or SERCA2/PLB ratio, discussed earlier, lower pumping activity of SERCA2 in aging myocardium may result from reduced phosphorylation of the SERCA2–PLB complex. Specifically, in its unphosphorylated state, PLB interacts with SERCA2 exerting an inhibitory effect manifested largely through a decrease in the enzyme’s affinity for Ca2+.
Phosphorylation of PLB by PKA and/or Ca2+/CaMK is thought to disrupt this interaction resulting in enhanced affinity of the ATPase for Ca2+ and stimulation of Ca2+ pump activity [41]. In addition to PLB, CaMK has been suggested to modulate the SR Ca2+ uptake and release through direct phosphorylation of SERCA2 [38]. Recent studies have also shown that significant age-associated decrements occur in (1) the amount of CaMK (δ-isoform) in the rat heart, (2) the endogenous CaMK-mediated phosphorylation of SERCA and PLB, and (3) the phosphorylation-dependent stimulation of SR Ca2+ sequestration [36]. Increased activity of the SR-associated phosphatase PP1, which dephosphorylates PLB, had already been reported, and overexpression of PP1 in transgenic mice resulted in HF. PP1 activity was further shown to be regulated by the inhibitor I-1, and I-1 was found to be reduced in human HF (reviewed in [44]). However, potential age-related changes in the activity of cardiac phosphatases have yet to be examined.
Age-related alterations in the gating properties of RyR [19, 45], resulting in an increased SR Ca2+ leak, may also contribute to both diastolic and systolic dysfunction of the aging myocardium by limiting the net rate of SR Ca2+ sequestration and SR Ca2+ loading, respectively. Finally, a slower rate of development/longer time to peak of the Cai 2+ transient in aging myocytes is likely to result from reduced SR Ca2+ loading but may be also consequent to a longer time to peak ICaL [22], which synchronizes SR Ca2+ release.
SR Ca2+ Release Channel
In addition to Ca2+ pumping by SERCA2, RyR characteristics are regulated by its protein expression and gating properties, a major determinant of the SR Ca2+ release, triggered by Ca2+ influx through LCC, as well as during cardiac relaxation and diastole. Accordingly, alterations in the expression or function of RyR have been implicated in both systolic and diastolic dysfunction of the aging heart. Reduced protein expression of cardiac RyR has been reported in aging Wistar rats [39], but not Fisher 344 rats [19, 34, 36]. The RYR is phosphorylated by PKA and CaMK, and a significant reduction in the CaMK-mediated phosphorylation of the RyR has been shown to occur in the aged compared with adult Fisher 344 rats [36].
Single-channel properties of RyR and unitary SR Ca2+ release events (Ca2+ sparks) in ventricular cardiomyocytes were recently examined in hearts from 6- to 24-month-old Fisher 344 rats [19]. Senescent myocytes displayed a decreased Cai 2+ transient amplitude and an increased time constant of the Cai 2+ transient decay, both of which correlated with a reduced Ca2+ content of the SR. Senescent cardiomyocytes also had an increased frequency of spontaneous Ca2+ sparks and a slight but statistically significant decrease in their average amplitude, full-width-at half-maximum and full-duration-at-half-maximum.
Single-channel recordings of RyR demonstrated that in aging hearts, the open probability of RYR was increased but the mean open time was shorter, providing a molecular correlate for the increased frequency of Ca2+ sparks and decreased size of sparks, respectively [19]. These results suggest modifications of normal RyR gating properties associated with increased sensitivity of RyR to resting and activating Ca2+ that may play a role in the altered Ca2+ homeostasis observed in senescent myocytes. Another recent study [45] examined the effects of aging on whole cell electrically stimulated Ca2+ transients and Ca2+ sparks at 37 °C in ventricular myocytes isolated from young adult (~5 months) and aged (~24 months) B6SJLF1/J mice of both sexes. A reduced amplitude and abbreviated rise time of the Cai 2+ transient in aged cells stimulated at 8 Hz and a markedly higher incidence and frequency of spontaneous Ca2+ sparks were observed in aged vs. young adult cells. Spark amplitudes and spatial widths were similar in both age groups. However, spark half-rise times and half-decay times were abbreviated in aged cells compared with younger cells. Neither resting Cai 2+ levels nor SR Ca2+ content differed between young adult and aged cells, indicating that increased spark frequency in aging cells was not attributable to increased SR Ca2+ stores and that a decrease in the Cai 2+ transient amplitude was not due to a decrease in SR Ca2+ load. These results suggest that alterations in SR Ca2+ release units occur in aging ventricular myocytes and raise the possibility that alterations in Ca2+ release may reflect age-related changes in fundamental release events rather than changes in SR Ca2+ stores and/or diastolic Cai 2+ levels. Differences in the characteristics of Ca2+ sparks (and the SR Ca2+ content) reported in these experiments [19, 45] might be partly related to differences in species and experimental conditions (e.g., temperature) employed.
Consistent with previous findings [45], both studies discussed above [19, 45] have shown increased frequency of spontaneous Ca2+ sparks in aging ventricular myocytes. The resulting increased Ca2+ leak from the SR may reduce the net rate of SR Ca2+ sequestration. Functional consequences of the latter include a slower decline of the Cai 2+ transient and increased diastolic Cai 2+ (diastolic dysfunction), a reduced SR Ca2+ load available for release (systolic dysfunction), and a reduced threshold for myocardial cell Ca2+ intolerance [46, 47]. PKA-dependent hyperphosphorylation of RYR, resulting in abnormal SR Ca2+ leak through the RyR, has been implicated in both diastolic and systolic dysfunction of the failing heart [48]. However, more recent evidence points to CaMKII site phosphorylation of RYR in normal cardiac tissue [49, 50], and a potential role and mechanism for PKA modulation of this process in the pathophysiology of HF associated with aging remains lacking.
Na+–Ca2+ Exchanger
The NCX serves as the main transsarcolemmal Ca2+ extrusion mechanism and is centrally involved in the beat-to-beat regulation of cellular Ca2+ content and cardiac contractile force, including regulation of the AP configuration in the late repolarization phase and the later Ca2+ clearance phase of the Cai 2+ transient. Thus, alterations in NCX activity may contribute to the prolongation of both the AP duration and relaxation in aging myocardium [1]. An age-associated increase in the NCX expression has been demonstrated at the transcriptional level, but protein levels of NCX reported in aging rodent hearts were unchanged [21, 34, 51] or reduced compared to younger adults [16, 39, 52].
Results of experiments using enriched sarcolemmal vesicles or muscle strips isolated from rats were also inconsistent, i.e., the NCX activity in aged myocardium was observed to be decreased [52, 53], increased [54], or unchanged [55]. More recent functional assessments of NCX activity in cardiac myocytes isolated from young (14–15 months) and aged (27–31 months) male Fischer Brown Norway rats [21] showed that under conditions where membrane potential and intracellular [Na+] and [Ca2+] could be controlled, “forward” NCX activity was increased in aged vs. young cells. The increased “forward” NCX activity was interpreted as a factor contributing to the late AP prolongation in aging myocardium [21]. An increased Ca2+ efflux via NCX would compensate for increased Ca2+ influx via LCC [20, 22, 24]. Prolongation of the AP consequent to reduced ITO [22] may temporarily limit “forward” NCX during relaxation, allowing better SR Ca2+ reuptake by SERCA2 [29].
The imposition of a shorter AP to myocytes from the old rat heart reduces the amplitude and the rate of decline of the steady-state Ca2+ transient and Cai 2+ transient [29]. This is attributable to a reduction in the SR Ca2+ uptake and loading, which, in the presence of a reduced rate of Ca2+ sequestration by SERCA2, is presumably due to a reduced ICaL time integral and likely also to an increased net Ca2+ extrusion via NCX [29].
Response to Action Potentials of an Increased Frequency
Reduction in the amplitude of the Cai 2+ transient in myocytes from aged hearts, compared to younger counterparts, has been reported in some studies already at low (<2 Hz) stimulation rates [14, 19]. Studies that have employed a range of stimulation rates [15, 28] typically showed blunted force and relaxation-frequency responses in myocytes from old vs. young hearts (Fig. 21.6). Thus, while the age-related differences in the amplitude and the rate of decay of the Cai 2+ transients (and diastolic Cai 2+ levels) were small or absent at low stimulation rates, they became apparent and progressively larger at pacing rates approximating those in vivo [15, 28].
Likewise, abrupt changes in the stimulation rate reveal an impaired SR Ca2+ release in ventricular myocytes isolated from senescent vs. young rats (Fig. 21.6). Specifically, in the presence of similar kinetics of ICaL recovery, reduction in the amplitude of the Cai 2+ transients and the gain of ICaL-dependent Ca2+ release during premature depolarizations is attributable to a slower rate of SR Ca2+ reuptake in older myocytes (Fig. 21.7).
Recovery of the L-type Ca2+ current (ICaL) and the intracellular Ca2+ (Cai 2+) transient following a prior depolarization. (a) Recordings of Cai 2+ transients (top) and ICaL (middle), induced by voltage clamp depolarizations (bottom) from −75 to 0 mV (with Na+ current, K+ currents, and “reverse” Na+–Ca2+ exchange blocked) in a representative ventricular myocyte isolated from young adult (6 months) Wistar rat. Test pulse intervals of 75–300 ms duration were applied following a train of nine conditioning voltage pulses (50 ms, from −75 to 0 mV at 0.5 Hz). (b) Averaged data from these experiments in myocytes from young (n = 5) and old (24 months; n = 7) rats show slower rate of Cai 2+ decline during the last conditioning pulse and similar kinetics of ICaL recovery but prolonged recovery time of the Cai 2+ transient and “gain” of ICaL-dependent Ca2+ release (Cai 2+/ICaL) during premature depolarizations in old vs. young myocytes (courtesy of Andzej M. Janczewski and Edward G. Lakatta)
Consistent with the major role of SERCA2 in these effects, studies in rat-isolated cardiac muscle preparations have shown that exercise training reverses age-associated slowing of contraction and relaxation [17, 18]. This was associated with increased Ca2+ transport by SERCA2 but not myosin ATPase activity in cardiac homogenates [18]. Likewise, overexpression of SERCA2 markedly improved rate-dependent contractility and contractile function in senescent rat hearts [34]. Clearly, the latter underlies impaired frequency-dependent inotropic and lusitropic responses [14–16, 34] that largely contribute to the systolic and diastolic dysfunction of the aging heart.
Reduced Acute Response of Myocardial Cells from Older Hearts to Acute β-Adrenergic Receptor Stimulation
Age-associated deficits in the myocardial β-AR signaling cascade also occur with aging in rats. The richly documented age-associated reduction in the postsynaptic response of myocardial cells to β-adrenergic stimulation seems to be due to multiple changes in the molecular and biochemical steps that couple the receptor to postreceptor effectors. However, the major limiting modification of this signaling pathway that occurs with advancing age in rodents seems to be the coupling of the β-AR to adenylyl cyclase via the Gs protein and changes in adenylyl cyclase protein, which lead to a reduction in the ability to sufficiently augment cell cAMP and to activate PKA to drive the phosphorylation of key proteins that are required to augment cardiac contractility [37, 56]. In contrast, the apparent desensitization of β-adrenergic signaling that occurs with aging does not seem to be mediated via increased β-AR kinase or increased Gi activity [57]. A blunted response to β-adrenergic stimulation of the cells within older myocardium can, in one sense, be viewed as adaptive with respect to its effect to limit the risk of Ca2+ overload and cell death in these cells in response to stress (Table 21.3), including reduced augmentation of the ICaL (Fig. 21.8) [25] through PKA-mediated changes in the availability and gating properties of LCC. The well-established deficits in β-AR signaling that occur in aging humans and animals [1] include significantly lower PKA-dependent phosphorylation of PLB in aged vs. adult rat ventricular myocardium [37]. A reduced myocardial contractile response to either β1AR or β2AR stimulation is observed with aging [25, 57, 58]. This is due to failure of β-adrenergic stimulation to augment Cai 2+ to the same extent in cells of senescent hearts that it does in those from younger adult hearts (Fig. 21.8), an effect attributable to a deficient increase of L-type sarcolemmal Ca2+ channel availability (Fig. 21.8), which leads to a lesser increase in Ca2+ influx [25].
Effects of norepinephrine (10−7 M) on contraction and Ca2+ transient amplitudes and kinetics. (a) Tracings obtained in the presence and absence of NE in the same myocyte are superimposed. (b) Peak current–voltage relationship of L-type Ca2+ channel activation for young (2 months), adult (8 months), and senescent (24 months) ventricular myocytes from Wistar rats, before and after NE 10−7 M. (c) Maximum rate of rise of calcium transient indexed by INDO-1 fluorescence in presence of increasing dose of NE in three ages of rat. (d) Average contractile amplitude responses to norepinephrine in 3 age groups. (Adapted from Xiao R-P, Tomhave ED, Wang DJ, Ji X, Boluyt MO, Cheng H, Lakatta EG, Koch WJ. Age-associated reductions in cardiac β1- and β2-adrenoceptor responses without changes in inhibitory G proteins or receptor kinases. J Clin Invest 1998; 101:1273–1282)
Markers of Chronic Stress in the Aged Heart Suggest That It “Operates on the Edge of Disease”
Acute excess myocardial Ca2+ loading leads to dysregulation of Ca2+ homeostasis, impaired diastolic and systolic function, arrhythmias, and cell death [47]. The cell Ca2+ load is determined by membrane structure and permeability characteristics, the intensity of stimuli that modulate Ca2+ influx or efflux via their impact on regulatory function of proteins within membranes, and ROS, which affect both membrane structure and function. Excessive cytosolic Ca2+ loading occurs during physiological and pharmacological scenarios that increase Ca2+ influx (e.g., neurotransmitters, postischemic reperfusion, or oxidative stress) [46, 59]. In hearts or myocytes from the older heart, enhanced Ca2+ influx, impaired relaxation, and increased diastolic tone occur during pacing at an increased frequency [15, 18, 60, 61]. This is a “downside” of the age-associated adaptations that occur within the cells of senescent heart and also of young animals chronically exposed to arterial pressure overload (Table 21.4). Causes of reduced Ca2+ tolerance of the older heart include changes in the amounts of proteins that regulate Ca2+ handling, caused in part by altered gene expression (Tables 21.3 and 21.4), and an age-associated alteration in the composition of membranes in which Ca2+ regulatory proteins reside, which includes an increase in membrane ω6:ω3 polyunsaturated fatty acids (PUFAs) [62]. ω3 PUFAs are protective of cardiac Ca2+ regulation. An additional potential cause of the reduced threshold of senescent myocytes for Ca2+ overload is an enhanced likelihood for intracellular generation of ROS [59, 63] in cells from the senescent vs. the younger adult heart during stress. In this regard, the older cardiac myocyte and endothelial cells [64] share common “risks” with aging.
Myocyte Progenitors in the Aging Heart
There are two opposing views regarding cardiomyocyte renewal within the heart: One proposes that the number of myocytes is fixed around birth and remains static; the other purports that the heart is a self-renewing organ containing a pool of progenitor cells (PCs) that dictate cell turnover, organ homeostasis, and myocardial aging. Observations in both humans and animals suggest that myocyte maturation and aging are characterized by loss of replicative potential, telomeric shortening, and the expression of the senescence-associated protein/cell cycle inhibitor p16INK4a [65–69]. Telomeric shortening in PCs leads to generation of progeny that rapidly acquire the senescent phenotype involving a progressive increase in the size of the cell (up to a critical volume beyond which myocyte hypertrophy is no longer possible), deficits in the electrical, Ca2+ cycling, and mechanical properties, and cell death. Cardiac myocytes with senescent and nonsenescent phenotypes already coexist at young age [69]. However, aging limits the growth and differentiation potential of PCs, thus interfering not only with their ability to sustain physiological cell turnover but also with their capacity to adapt to increases in pressure and volume loads [65, 68].
A loss of PC function can result in an imbalance between factors enhancing oxidative stress, telomere attrition, and death and factors promoting growth, migration, and survival. Recent findings suggest a preeminent position of insulin-like growth factor-1 (IGF-1) among factors that can partly overcome cardiac cellular senescence. Specifically, cardiac-restricted overexpression of IGF-1 in transgenic mice has been shown to delay the aging myopathy and the manifestations of HF [26] and to restore SERCA2a expression and rescue age-associated impairment of cardiac myocyte contractile function [51]. The latter effect was also partly mimicked by short-term in vitro treatment with recombinant IGF-1 [51]. Furthermore, intramyocardial delivery of IGF-1 improved senescent heart phenotype in male Fisher 344 rats [67], including increased proliferation of functionally competent PCs and diminished angiotensin II-induced apoptosis. Myocardial regeneration mediated by PC activation attenuated ventricular dilation and the decrease in ventricular mass-to-chamber volume ratio, resulting in improvement of in vivo cardiac function in animals at 28–29 months of age [67].
More recent studies employing the 14C retrospective dating of myocytes in the human heart are controversial and have been interpreted to indicate that the cell renewal rate is very low [70] or, conversely, becomes substantially higher with advancing age [71]. The latter result suggests that factors that cause excessive cell death, and not a reduced stem cell renewal rate, per se, are the predominant cause of a reduced myocyte number in the aged heart.
Summary
In summary, age per se is the major risk factor for cardiovascular disease. Elucidation of the age-associated alterations in cardiac and arterial structure and function at both the cellular and molecular levels provides valuable clues that may assist in the development of effective therapies to prevent, to delay, or to attenuate the cardiovascular changes that accompany aging and contribute to the clinical manifestations of chronic heart failure. Changes in cardiac cell phenotype that occur with normal aging, as well as in HF associated with aging, include deficits in β-adrenergic receptor signaling, increased generation of reactive oxygen species, and altered excitation–contraction (EC) coupling that involves prolongation of the action potential, intracellular Ca2+ transient and contraction, and blunted force and relaxation-frequency responses. Evidence suggests that altered sarcoplasmic reticulum Ca2+ uptake, storage, and release play central role in these changes, which also involve sarcolemmal L-type Ca2+ channel (LCC), Na+–Ca2+ exchanger, and K+ channels.
In spite of the interest in the physiology of the age-associated changes in cardiovascular structure and function, however, cardiovascular aging has remained, for the most part, outside of mainstream clinical medicine. This is largely because the pathophysiologic implications of these age-associated changes are largely underappreciated and are not well disseminated in the medical community. In fact, age has traditionally been considered a nonmodifiable risk factor. Policy makers, researchers, and clinicians need to intensify their efforts toward identification of novel pathways that could be targeted for interventions aiming at retardation or attenuation of these age-associated alterations that occur in the heart and arteries, particularly in individuals in whom these alterations are accelerated. Translational studies would then examine whether these strategies (i.e., those targeting cardiovascular aging) can have a salutary impact on the adverse cardiovascular effects of accelerated cardiovascular aging. As such, cardiovascular aging is a promising frontier in preventive cardiology.
References
Lakatta EG. Cardiovascular regulatory mechanisms in advanced age. Physiol Rev. 1993;73:413.
Leinwand LA. Sex is a potent modifier of the cardiovascular system. J Clin Invest. 2003;112:302.
Konhilas JP, Leinwand LA. The effects of biological sex and diet on the development of heart failure. Circulation. 2007;116:2747.
Fermin DR, Barac A, Lee S, et al. Sex and age dimorphism of myocardial gene expression in nonischemic human heart failure. Circ Cardiovasc Genet. 2008;1:117–25.
Fleg JL, Schulman S, O’Connor FC, Becker LC, Gerstenblith G, Clulow JF, Renlund DG, Lakatta EG. Effects of acute β-adrenergic receptor blockade on age-associated changes in cardiovascular performance during dynamic exercise. Circulation. 1994;90:2333–41.
Yin FCP, Weisfeldt ML, Milnor WR. Role of aortic input impedance in the decreased cardiovascular response to exercise with aging in dogs. J Clin Invest. 1981;68:28–38.
Brodde OE, Konschak U, Becker K, et al. Cardiac muscarinic receptors decrease with age. In vitro and in vivo studies. J Clin Invest. 1998;101:471.
Fraticelli A, Josephson R, Danziger R, Lakatta E, Spurgeon H. Morphological and contractile characteristics of rat cardiac myocytes from maturation to senescence. Am J Physiol. 1989;257:H259–65.
Anversa P, Palackal T, Sonnenblick EH, Olivetti G, Meggs LG, Capasso JM. Myocyte cell loss and myocyte cellular hyperplasia in the hypertrophied aging rat heart. Circ Res. 1990;67:871–85.
Lakatta EG. Cardiovascular aging research: the next horizons. J Am Geriatr Soc. 1999;47:613–25.
Cigola E, Kastura J, Li B, Meggs LG, Anversa P. Angiotensin II activates programmed myocyte cell death in vitro. Exp Cell Res. 1997;231:363–71.
Younes A, Boluyt MO, O’Neill L, Meredith AL, Crow MT, Lakatta EG. Age-associated increase in rat ventricular ANP gene expression correlates with cardiac hypertrophy. Am J Physiol. 1995;38:H1003–8.
Caffrey JL, Boluyt MO, Younes A, Barron BA, O’Neill L, Crow MT, Lakatta EG. Aging, cardiac proenkephalin mRNA and enkephalin peptides in the Fisher 344 rat. J Mol Cell Cardiol. 1994;26:701–11.
Grandy SA, Howlett SE. Cardiac excitation-contraction coupling is altered in myocytes from aged male mice but not in cells from aged female mice. Am J Physiol. 2006;291:H2362–70.
Lim CC, Apstein CS, Colucci WS, Liao R. Impaired cell shortening and relengthening with increased pacing frequency are intrinsic to the senescent mouse cardiomyocyte. J Mol Cell Cardiol. 2000;32:2075–82.
Lim CC, Liao R, Varma N, Apstein CS. Impaired lusitropy-frequency in the aging mouse: role of Ca2+ handling proteins and effects of isoproterenol. Am J Physiol. 1999;277:H2083–90.
Spurgeon HA, Steinbach MF, Lakatta EG. Chronic exercise prevents characteristic age-related changes in rat cardiac contraction. Am J Physiol. 1983;244:H513–8.
Tate CA, Taffet GE, Hudson EK, Blaylock SL, McBride RP, Michael LH. Enhanced calcium uptake of cardiac sarcoplasmic reticulum in exercise-trained old rats. Am J Physiol. 1990;258:H431–5.
Zhu X, Altschafl BA, Hajjar RJ, Valdivia HH, Schmidt U. Altered Ca2+ sparks and gating properties of ryanodine receptors in aging cardiomyocytes. Cell Calcium. 2005;37:583–91.
Dibb K, Rueckschloss U, Eisner D, Insberg G, Trafford A. Mechanisms underlying enhanced excitation contraction coupling observed in the senescent sheep myocardium. J Mol Cell Cardiol. 2004;37:1171–81.
Mace LC, Palmer BM, Brown DA, Jew KN, Lynch JM, Glunt JM, Parsons TA, Cheung JY, Moore RL. Influence of age and run training on cardiac Na+/Ca2+ exchange. J Appl Physiol. 2003;95:1994–2003.
Walker KE, Lakatta EG, Houser SR. Age associated changes in membrane currents in rat ventricular myocytes. Cardiovasc Res. 1993;27:1968–77.
Wei JY, Spurgeon A, Lakatta EG. Excitation-contraction in rat myocardium: alterations with adult aging. Am J Physiol. 1984;246:H784–91.
Josephson IR, Guia A, Stern MD, Lakatta EG. Alterations in properties of L-type Ca channels in aging rat heart. J Mol Cell Cardiol. 2002;34:297–308.
Xiao RP, Spurgeon HA, O’Connor F, Lakatta EG. Age-associated changes in beta-adrenergic modulation on rat cardiac excitation-contraction coupling. J Clin Invest. 1994;94:2051–9.
Torella D, Rota M, Nurzynska D, Musso E, Monsen A, Shiraishi I, Zias E, Walsh K, Rosenzweig A, Sussman MA, Urbanek K, Nadal-Ginard B, Kajstura J, Anversa P, Leri A. Cardiac stem cell and myocyte aging, heart failure, and insulin-like growth factor-1 overexpression. Circ Res. 2004;94:514–24.
Liu SJ, Wyeth RP, Melchert RB, Kennedy RH. Aging-associated changes in whole cell K+ and L-type Ca2+ currents in rat ventricular myocytes. Am J Physiol. 2000;279:H889–900.
Isenberg G, Borschke B, Rueckschloss U. Ca2+ transients in cardiomyocytes from senescent mice peak late and decay slowly. Cell Calcium. 2003;34:271–80.
Janczewski AM, Spurgeon HA, Lakatta EG. Action potential prolongation in cardiac myocytes of old rats is an adaptation to sustain youthful intracellular Ca2+ regulation. J Mol Cell Cardiol. 2002;34:641–8.
Bito V, Heinzel FR, Biesmans L, Antoons G, Sipido KR. Crosstalk between L-type Ca2+ channels and the sarcoplasmic reticulum: alterations during cardiac remodeling. Cardiovasc Res. 2008;77:315–24.
Bassani RA. Transient outward potassium current and Ca2+ homeostasis in the heart: beyond the action potential. Braz J Med Biol Res. 2006;39:393–403.
Froehlich JP, Lakatta EG, Beard E, Spurgeon HA, Weisfeldt ML, Gerstenblith G. Studies of sarcoplasmic reticulum function and contraction duration in young and aged rat myocardium. J Mol Cell Cardiol. 1978;10:427–38.
Kaplan P, Jurkovicova D, Babusikova E, Hudecova S, Racay P, Sirova M, Lehotsky J, Drgova A, Dobrota D, Krizanova O. Effect of aging on the expression of intracellular Ca2+ transport proteins in a rat heart. Mol Cell Biochem. 2007;301:219–26.
Schmidt U, del Monte F, Miyamoto MI, Matsui T, Gwathmey JK, Rosenzweig A, Hajjar RJ. Restoration of diastolic function in senescent rat hearts through adenoviral gene transfer of sarcoplasmic reticulum Ca2+-ATPase. Circulation. 2000;101:790–6.
Taffet GE, Tate CA. CaATPase content is lower in cardiac sarcoplasmic reticulum isolated from old rats. Am J Physiol. 1993;264:H1609–14.
Xu A, Narayanan N. Effects of aging on sarcoplasmic reticulum Ca2+-cycling proteins and their phosphorylation in rat myocardium. Am J Physiol. 1998;275:H2087–94.
Jiang MT, Moffat MP, Narayanan N. Age-related alterations in the phosphorylation of sarcoplasmic reticulum and myofibrillar proteins and diminished contractile response to isoproterenol in intact rat ventricle. Circ Res. 1993;72:102–11.
Xu A, Hawkins C, Narayanan N. Phosphorylation and activation of the Ca2+-ATPase of cardiac sarcoplasmic reticulum by Ca2+/calmodulin-dependent protein kinase. J Biol Chem. 1993;268:8394–7.
Assayag P, Charlemagne D, Marty I, de Leiris J, Lompre AM, Boucher F, Valere PE, Lortet S, Swynghedauw B, Besse S. Effects of sustained low-flow ischemia on myocardial function and calcium-regulating proteins in adult and senescent rat hearts. Cardiovasc Res. 1998;38:169–80.
Slack JP, Grupp IL, Dash R, Holder D, Schmidt A, Gerst MJ, Tamura T, Tilgmann C, James PF, Johnson R, Gerdes AM, Kranias EG. The enhanced contractility of the phospholamban-deficient mouse heart persists with aging. J Mol Cell Cardiol. 2001;33:1031–40.
MacLennan DH, Kranias EG. Phospholamban: a crucial regulator of cardiac contractility. Nat Rev Mol Cell Biol. 2003;4:566–77.
del Monte F, Harding SE, Dec GW, Gwathmey JK, Hajjar RJ. Targeting phospholamban by gene transfer in human heart failure. Circulation. 2002;105:904–7.
Armand A-S, De Windt LJ. Calcium cycling in heart failure: how the fast became too furious. Cardiovasc Res. 2004;62:439–41.
Sipido KR, Eisner D. Something old, something new: changing views on the cellular mechanisms of heart failure. Cardiovasc Res. 2005;68:167–74.
Howlett SE, Grandy SA, Ferrier GR. Calcium spark properties in ventricular myocytes are altered in aged mice. Am J Physiol. 2006;290:H1566–74.
Hano O, Bogdanov KY, Sakai M, Danziger RG, Spurgeon HA, Lakatta EG. Reduced threshold for myocardial cell calcium intolerance in the rat heart with aging. Am J Physiol. 1995;269:H1607–12.
Lakatta EG. Functional implications of spontaneous sarcoplasmic reticulum Ca2+ release in the heart. Cardiovasc Res. 1992;26:193–214.
Marks AR. Cardiac intracellular calcium release channels: role in heart failure. Circ Res. 2000;87:8–11.
Guo T, Zhang T, Mestril R, Bers DM. Ca/calmodulin-dependent protein kinase II phosphorylation of ryanodine receptor does affect calcium sparks in mouse ventricular myocytes. Circ Res. 2006;99:398–406.
Li Y, Kranias EG, Mignery GA, Bers DM. Protein kinase a phosphorylation of the ryanodine receptor does not affect calcium sparks in mouse ventricular myocytes. Circ Res. 2002;90:309–16.
Li Q, Wu S, Li S-Y, Lopez FL, Du M, Kajstura J, Anversa P, Ren J. Cardiac-specific overexpression of insulin-like growth factor 1 attenuates aging-associated cardiac diastolic contractile dysfunction and protein damage. Am J Physiol. 2007;292:H1398–403.
Janapati V, Wu A, Davis N, Derrico CA, Levengood J, Schummers J, Colvin RA. Post-transcriptional regulation of the Na+/Ca2+ exchanger in aging rat heart. Mech Ageing Dev. 1995;84:195–208.
Heyliger C, Prakash A, McNeill J. Alterations in membrane Na+–Ca2+ exchange in the aging myocardium. Age. 1988;1988:1–6.
Frolkis VV, Frolkis RA, Mkhitarian LS, Shevchuk VG, Fraifeld VE, Vakulenko LG, Syrovy I. Contractile function and Ca2+ transport system of myocardium in ageing. Gerontology. 1988;34:64–74.
Abete P, Ferrara N, Cioppa A, Ferrara P, Bianco S, Calabrese C, Napoli C, Rengo F. The role of aging on the control of contractile force by Na+–Ca2+ exchange in rat papillary muscle. J Gerontol A Biol Sci Med Sci. 1996;51:M251–9.
Schmidt U, Zhu X, Lebeche D, Huq F, Guerrero JL, Hajjar RJ. In vivo gene transfer of parvalbumin improves diastolic function in aged rat hearts. Cardiovasc Res. 2005;66:318–23.
Xiao R-P, Tomhave ED, Wang DJ, Ji X, Boluyt MO, Cheng H, Lakatta EG, Koch WJ. Age-associated reductions in cardiac β1- and β2-adrenoceptor responses without changes in inhibitory G proteins or receptor kinases. J Clin Invest. 1998;101:1273–82.
Sakai M, Danziger RS, Staddon JM, Lakatta EG, Hansford RG. Decrease with senescence in the norepinephrine-induced phosphorylation of myofilament proteins in isolated rat cardiac myocytes. J Mol Cell Cardiol. 1989;21:1327–36.
Lakatta EG, Sollott SJ, Pepe S. The old heart: operating on the edge. In: Bock G, Goode JA, editors. Ageing vulnerability: causes and interventions, Novartis Foundation Symposium, vol. 235. New York, NY: Wiley; 2001. p. 172–201.
Brenner DA, Apstein CS, Saupe KW. Exercise training attenuates age-associated diastolic dysfunction in rats. Circulation. 2001;104:221–6.
Zhang SJ, Zhou YY, Xiao RP, et al. Age-associated reduction in recovery of the equilibrium state of myocyte length during reduced interstimulus intervals at higher stimulation rates. Biophys J. 2000;78:227A (Abstract).
Pepe S, Tsuchiya N, Lakatta EG, Hansford RG. PUFA and aging modulate cardiac mitochondrial membrane lipid composition and Ca2+ activation of PDH. Am J Physiol. 1999;276:H149–58.
Lucas D, Sweda L. Cardiac reperfusion injury, aging, lipid peroxidation, and mitochondrial dysfunction. Proc Natl Acad Sci USA. 1998;95:510–4.
Van der Loo B, Labugger R, Skepper JN, Bachschmid M, Kilo J, Powell JM, Palacios-Callendere M, Erusalimsky JD, Quaschning T, Malinski T, Gygi D, Ullrich V, Luscher TF. Enhanced peroxynitrite formation is associated with vascular aging. J Exp Med. 2000;192:1731–43.
Anversa P, Rota M, Urbanek K, Hosoda T, Sonnenblick EH, Leri A, Kajstura J, Bolli R. Myocardial aging-a stem cell problem. Basic Res Cardiol. 2005;100:482–93.
Chimenti C, Kajstura J, Torella D, Urbanek K, Heleniak H, Colussi C, Di Meglio F, Nadal-Ginard B, Frustaci A, Leri A, Maseri A, Anversa P. Senescence and death of primitive cells and myocytes leads to premature cardiac aging and heart failure. Circ Res. 2003;93:604–13.
Gonzalez A, Rota M, Nurzynska D, Misao Y, Tillmanns J, Ojaimi C, Padin-Iruegas ME, Muller P, Esposito G, Bearzi C, Vitale S, Dawn B, Anganalmath SK, Baker M, Hintze TH, Bolli R, Urbanek K, Hosoda T, Anversa P, Kajstura J, Leri A. Activation of cardiac progenitor cells reverses the failing heart senescent phenotype and prolongs lifespan. Circ Res. 2008;102:597–606.
Kajstura J, Urbanek K, Rota M, Bearzi C, Hosoda T, Bolli R, Anversa P, Leri A. Cardiac stem cells and myocardial disease. J Mol Cell Cardiol. 2008;45:505–13.
Rota M, Hosoda T, De Angelis A, Arcarese ML, Esposito G, Rizzi R, Tillmanns J, Tugal D, Musso E, Rimoldi O, Bearzi C, Urbanek K, Anversa P, Leri A, Kajstura J. The young mouse heart is composed of myocytes heterogeneous in age and function. Circ Res. 2007;101:387–99.
Bergmann O, Bhardwaj RD, Bernard S, Zdunek S, Barnabe-Heider F, Walsh S, Zupicich J, Alkass K, Buchholz BA, Druid H, Jovinge S, Frisen J. Evidence for cardiomyocyte renewal in humans. Science. 2009;324:98–102.
Kajstura J, Rota M, Cappetta D, Ogorek B, Arranto C, Bai Y, Ferreira-Martins J, Signore S, Sanada F, Matsuda A, Kostyla J, Caballero M-V, Fiorini C, D’Alessandro DA, Michler RE, del Monte F, Hosoda T, Perrella MA, Leri A, Buchholz BA, Loscalzo J, Anversa P. Cardiomyogenesis in the aging and failing human heart. Circulation. 2012;126:1869–81.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer Science+Business Media New York
About this chapter
Cite this chapter
Lakatta, E.G., Spurgeon, H.A., Janczewski, A.M. (2014). Changes in the Heart That Accompany Advancing Age: Humans to Molecules. In: Jugdutt, B. (eds) Aging and Heart Failure. Springer, New York, NY. https://doi.org/10.1007/978-1-4939-0268-2_21
Download citation
DOI: https://doi.org/10.1007/978-1-4939-0268-2_21
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4939-0267-5
Online ISBN: 978-1-4939-0268-2
eBook Packages: MedicineMedicine (R0)