Abstract
Pediatric subtrochanteric femur fractures are a challenging subset of fractures to treat, with a relative paucity of literature-based evidence to support specific algorithmic approaches. These fractures are rare, and there is no clear consensus among authors on the definition of a subtrochanteric femur fracture in children. Patient age, weight, femoral canal size, fracture stability, associated injuries, and surgeon experience should all be considered when determining the best treatment option. Infants 0–6 months of age are well treated with a Pavlik harness. Children 6 months to 5 years of age should be treated with a hip spica cast, although internal fixation is a viable alternative if the fracture is unstable. Flexible intramedullary nails, open plating, and submuscular plating are all successful treatment options in children 5–11 years of age, depending on the fracture pattern. Finally, children aged 11 years to skeletal maturity are well treated with rigid intramedullary nailing using a lateral trochanteric entry site. While these overall principles largely mirror trends currently applied for treatment of femoral shaft fractures in children, subtrochanteric fractures are frequently more prone toward displacement, due to the strong, divergent pull of muscular attachments in the peritrochanteric region. Therefore, consideration should be given toward selection of age-based treatment approaches more likely to ensure stability. All treatment methods have associated complications, and these should be discussed with the patient and family during the informed consent process.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Subtrochanteric femur fracture
- Pediatrics
- Fracture treatment
- Titanium elastic nails
- Plating
- Submuscular plating
- Complications
Introduction
Fractures in the subtrochanteric region are a particularly challenging subset of femur fractures to manage. These fractures are rare and account for 4–17 % of pediatric femur fractures [1–3]. The mechanism of injury, treatment, and associated complications are significantly different from femoral shaft and intertrochanteric femur fractures, owing to the strong muscle forces, bending moments, and complex fracture patterns that can occur with subtrochanteric femur fractures. Obtaining and maintaining fracture reduction is challenging secondary to flexion, abduction, and external rotation of the proximal fragment, relative to the distal fragment. Treatment selection is based on patient age, weight, femoral canal size, fracture stability, associated injuries, and surgeon experience. Few studies have evaluated the outcomes and complications of treatment of subtrochanteric femur fractures in children.
Classification
There is no consensus in the literature on the definition of a pediatric subtrochanteric femur fracture. Several definitions exist, including any fracture that is located in the proximal quarter of the femoral shaft or within 3 cm of the lesser trochanter [2, 4]. However, some subtrochanteric femur fractures do not fit perfectly into this classification, with fracture lines extending proximal to the lesser trochanter or distally into the diaphysis. Pombo and Shilt identified a pediatric subtrochanteric femur fracture as a fracture that is located within the proximal 10 % of the total femur length below the lesser trochanter (Fig. 6.1). This formula is a modification of one adult definition of a subtrochanteric femur fracture, which includes any fracture that occurs within 5 cm of the lesser trochanter, based on the average length of the adult femur [5]. Pombo and Shilt’s modification is the authors’ preferred definition, as it takes into account the difference in femur lengths at various ages, as well as the difference in femur lengths among children of the same age.
The authors prefer this method to classify subtrochanteric femur fractures. A full-length anteroposterior femur radiograph is used to determine the total length of the femur (B), which is defined as the distance between the top of the femoral head and the medial femoral condyle. Next, the distance between the inferior aspect of the lesser trochanter and the fracture site is measured (A). If (A/B) × 100 = 10 % or less of the total length of the femur, the fracture is classified as subtrochanteric
Anatomy
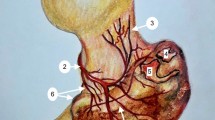
Knowledge of the proximal femoral anatomy is crucial in order to understand the deforming forces that must be overcome to achieve anatomic alignment. The subtrochanteric region of the femoral shaft is almost completely encased in a muscular envelope. The quadriceps and hamstrings span the proximal femur, and contribute to the femoral shortening that occurs after a subtrochanteric femur fracture (Fig. 6.2). The integrity of the trochanters influences fracture deformity. If the majority of the fracture is below the lesser trochanter, the proximal segment typically externally rotates, flexes, and abducts due to the muscular pull of the short external rotators, iliopsoas, and hip abductors, respectively. The hip adductors, in turn, generally medialize the distal shaft of the femur, as shown in Fig. 6.2. In contrast, if the lesser trochanter is involved in the distal fracture fragment , this results in decreased flexion and external rotation deformities of the proximal fragment produced by the psoas muscle. Understanding the pathophysiology of the fracture is crucial to obtain proper reduction, since longitudinal traction alone is unlikely to correct the deformity. The treating surgeon should anticipate the need to utilize several reduction techniques, either through positioning or externally applied forces, to control the fracture segments and obtain proper alignment.
(a) AP and (b) lateral diagrams of the muscle forces in a subtrochanteric femur fracture. The subtrochanteric region of the femoral shaft is almost completely encased in a muscular envelope. The quadriceps and hamstrings span the proximal femur, and contribute to femoral shortening. The integrity of the trochanters influences fracture deformity. If the majority of the fracture is below the lesser trochanter, the proximal segment typically externally rotates, flexes, and abducts due to the muscular pull of the short external rotators, iliopsoas, and hip abductors. The hip adductors medialize the distal shaft of the femur. In contrast, if the lesser trochanter is involved in the fracture, this results in decreased flexion and external rotation deformities of the proximal fragment produced by the psoas muscle
Biomechanics
The majority of the studies evaluating the biomechanics of the subtrochanteric region have been conducted in adult cadaveric and computer models. Although there are many similarities in the stresses seen in the subtrochanteric region, the results of these studies cannot be fully applied to a pediatric model because the primarily cartilaginous skeleton can better distribute stresses. During ambulation, the femur is subjected to high compressive, tensile, and torsional forces as a result of body weight and the multiple deforming muscle forces exerted on the proximal femur. The majority of these forces are concentrated in the subtrochanteric region [6]. In 1917, Koch et al. created a mathematical beam model of a femur, which was represented as a curved beam with a 100-pound force applied at the femoral head. The authors found that the highest stresses in compression occurred just at the base of the medial subtrochanteric region, and in tension, just below the greater trochanter. This work has been further elaborated on and substantiated by several researchers using various methods, ranging from finite element analysis to 3-D CT modeling [7, 8]. In general, the fracture pattern is determined by the magnitude of the applied load, the rate of load application, and the local strength of the femur.
Mechanism of Injury
The incidence of femur fractures has increased in recent decades, which likely correlates with greater participation in organized sports and physical extracurricular activities [9]. The osseous failure in subtrochanteric fractures may be due to pure torsion, or a combination of torsion and bending. These fractures are found across all age groups and are attributable to a number of mechanisms. High-energy trauma is the most common mechanism, such as motor vehicle accidents or falls. There is an asymmetric age- and gender-related distribution of subtrochanteric femur fractures, with these injuries occurring more frequently in younger children [2, 4, 10] and males [2, 4, 11].
Evaluation
History
A complete history is vital to the proper management of a patient with a subtrochanteric femur fracture. This can be obtained from the patient, family members, and emergency medical personnel. The pertinent pieces of information that must be documented are the patient’s age, mechanism of injury, need for extrication, and any comorbid conditions. Nonaccidental trauma should always be considered in a nonambulatory child. Although fractures associated with nonaccidental trauma are more common in the distal femur, the evaluating physician should assess for signs suggestive of child abuse, such as bruises, burns, late presentation, or fractures in various stages of healing [12]. If the subtrochanteric femur fracture resulted from a low-energy mechanism, evaluation for a pathologic bone condition should be conducted.
Physical Examination
The patient with a subtrochanteric femur fracture usually presents with a lower extremity that is shortened, flexed, and externally rotated secondary to the deforming muscles forces. The extremity should be inspected for any skin disruption, which may indicate an open fracture. The circumference of the hip and thigh should be evaluated and monitored for potential compartment syndrome or an expanding deep hematoma. The knee should be assessed for ligamentous injury and a thorough vascular examination should be performed, including the popliteal, dorsalis pedis, and posterior tibial pulses. The sciatic nerve is in close proximity to the subtrochanteric region, and documentation of the motor and sensory function of the tibial and peroneal nerves is required. The contralateral lower extremity can be assessed to evaluate relative leg lengths. It is imperative to perform a detailed evaluation for other sites of discomfort that may be masked by pain from the femur fracture. A methodical examination of all extremities and the pelvis should be performed to assess for associated fractures. Associated injuries are common in young patients with a high-energy mechanism of injury. Ipsilateral noncontiguous pelvic injuries and other ipsilateral fractures can occur.
It is uncommon for patients with isolated femoral fractures to have hemodynamic insufficiency, and aggressive volume support is usually not needed. Further investigation into associated abdominal, thoracic, or cranial etiology is warranted in patients who are hypotensive, hypovolemic, or anemic. A study assessing 149 children who sustained a femur fracture secondary to a motor vehicle accident found that 18.5 % of patients had an associated soft-tissue injury, 5 % had an intra-abdominal injury, and 14 % had a head injury [13].
Radiographic Studies
Radiographic evaluation should begin with an anteroposterior (AP) pelvis radiograph, and full-length AP and lateral radiographs of the entire femur. Traction radiographs may be helpful to delineate subtle fracture lines, although these may be difficult to obtain in the acute injury setting. Fracture pattern, comminution, bone loss, and associated fractures should be assessed. Signs of an underlying pathologic bony process should be noted, such as osteopenia or a radiolucent lesion. If nonaccidental trauma is suspected, a skeletal survey should be obtained to evaluate for additional fractures. This should consist of AP radiographs of the long bones of all four extremities, AP and lateral views of the thoracolumbar spine, and an AP and lateral skull series. A single radiograph of the entire child is not sufficient, as this is likely to miss fractures [14].
Computed tomography (CT) is not usually necessary in the routine evaluation of subtrochanteric femur fractures. Magnetic resonance imaging may be indicated if a pathologic fracture or stress fracture is suspected. If there is concern for vascular compromise, ankle-brachial indices are a quick subjective measurement of limb perfusion that can be obtained in the trauma bay.
Management Principles
The timing of definitive fixation is dictated by the patient’s hemodynamic stability and associated injuries. Although the treatment of subtrochanteric femur fractures has been predominantly age-based (Table 6.1), the treating surgeon must take into account the patient’s body habitus and skeletal age. Treatment failures occur when there is a mismatch between the biomechanical demands of the fracture and construct stability. In general, overriding of the fracture segments by 2 cm or more indicates disruption of the periosteal sleeve and can be used as an indicator of fracture stability. The ideal device for stabilization of subtrochanteric fractures is an implant that resists the tendency for shaft medialization, as well as external rotation, flexion, and varus angulation of the proximal fragment [15].
Fracture malalignment is a commonly reported complication from subtrochanteric femur fractures [16–21]. The majority of the criteria used for acceptable shortening and angulation at the fracture site originate from the femoral shaft literature. Caution should be used when applying these principles to the assessment of subtrochanteric femur fractures because functional outcome studies assessing proximal femur angular deformities are lacking. In general, fracture shortening is tolerated in children younger than 10 years of age because of the physiologic growth stimulation that occurs during fracture healing and subsequent femoral overgrowth following such fractures [2, 4, 22–24]. Therefore, 1.0–1.5 cm of shortening is considered acceptable in this young age group.
Due to the remodeling potential of the femur, coronal and sagittal malalignment can be tolerated up to 20–25° before abductor function becomes compromised [2, 4, 22, 25–27]. Jeng et al. followed 15 children treated with 90–90 traction for a subtrochanteric femur fracture for approximately 6.5 years. Remodeling of coronal angulation was 50 % or more in all cases. However, the average age of patients in the study was 4.5 years, making it difficult to extrapolate the results to adolescents who have decreased growth and remodeling potential [2].
Unlike coronal or sagittal angular deformities , torsional deformities have been found to have less remodeling potential but are generally well compensated by patients [28]. The treating surgeon should carefully scrutinize preoperative and intraoperative imaging, which may include the relationship of the lesser and greater trochanters of the contralateral side, or that of one or both of the trochanters to the distal femoral condyles, to accurately assess the rotational deformity and attempt to correct this during treatment.
Nonoperative Management
Pavlik Harness
The Pavlik harness is the preferred treatment for femoral shaft fractures in children 6 months of age and younger. Notably, however, there are no published reports of pediatric subtrochanteric femur fractures treated with a Pavlik harness. The thick periosteum in this age group results in relative fracture stability. Several authors have reported excellent functional outcomes after Pavlik harness treatment of femoral shaft fractures due to the robust fracture remodeling potential in the infant and toddler [29, 30]. Podeszwa et al. assessed the radiographic and functional results of 40 children under 1 year who had sustained a femur fracture; 24 patients were treated with a Pavlik harness, while 16 patients were treated in a spica cast. They found no difference in radiographic outcomes between the two groups. Approximately one-third of the spica cast patients had a skin complication, which was not seen in the Pavlik harness group [29, 31]. Although a similar study has not been performed in subtrochanteric fractures, we recommend a Pavlik harness for children 0–6 months of age (Table 6.2) .
Hip Spica Cast
There is a paucity of data regarding the use of spica casting in the treatment of pediatric subtrochanteric femur fractures. Similar to femoral shaft fractures, children 6 months to 5 years of age can be considered for spica cast treatment. However, because unstable femoral shaft fractures have been shown to displace with spica cast treatment [31, 32], determination of fracture stability is equally, if not more, important when determining the optimal treatment for subtrochanteric femur fractures. The majority of subtrochanteric fractures are difficult to manage with closed means, secondary to the strong deforming muscle forces and high-energy mechanism of injury. Jarvis et al. evaluated 13 skeletally immature adolescents who had undergone treatment of a subtrochanteric femur fracture. Ten patients were treated operatively with a variety of different techniques, while three patients were treated nonoperatively with a spica cast. At final follow-up, all of the patients who were treated nonoperatively had unsatisfactory outcomes, with fracture malalignment ranging from 8 to 16° and subsequent leg length inequalities. The authors concluded that internal fixation was more effective than nonoperative treatment of subtrochanteric femur fractures in skeletally immature adolescents [33]. Although children younger than 5 years have increased remodeling potential compared with adolescents, and are more likely to have a good outcome when managed in a spica cast, we advise careful assessment of fracture stability when deciding between spica cast versus operative management of a subtrochanteric femur fracture in this age group. Close radiographic and clinical follow-up is necessary if cast treatment is undertaken (Fig. 6.3a, b), as skin-related complications are also common with spica casting (Table 6.3).
(a) Standing AP lower extremity radiographi of a 3-year-old female who sustained a subtrochanteric femur fracture after jumping from a bed. The patient was treated in a spica cast for 8 weeks at an outside facility and was seen as a second opinion for a leg length discrepancy 6 months later. (b) Patient 15 months following a subtrochanteric osteotomy
Operative Management
External Fixation
External fixation for treatment of subtrochanteric fractures is generally reserved for open fractures, fractures with associated neurovascular injury, and polytrauma patients [34]. One advantage of external fixation is the ability to perform serial adjustments if the reduction is inadequate. In uniplanar constructs, lateral half-pin frames allow for control of the fracture, as well as mobilization of adjacent joints. Multiplanar external fixators allow the adjustment to occur in three planes. With the advent of flexible nails, external fixation is now more commonly used as an initial temporizing measure, rather than for definitive fixation. Although external fixation allows for potential adjustment of fracture position after original operation, better functional outcomes have been demonstrated with femoral shaft fractures treated with flexible nails, with decreased time to full-weight bearing, return to full range of motion, and return to school [34, 35]. No studies have specifically compared external fixation and flexible nailing of pediatric subtrochanteric femur fractures. Refracture after frame removal and pin tract infections are potential complications of external fixation. Wani et al. treated 45 displaced femur fractures in children with external fixation and reported pin tract infections in 47 % (Table 6.4) [36].
Flexible Intramedullary Nailing
Flexible intramedullary nailing is currently the most widely used technique for treatment of femoral shaft fractures in children 5–11 years of age, and remains highly applicable to subtrochanteric fractures as well. This is a minimally invasive, simple, economical, and safe technique. Titanium elastic nailing has demonstrated the best outcomes in patients with length-stable femur fractures in the middle 60 % of the diaphysis who weigh less than 49 kg [16–20, 37–39]. There are only a few reports in the literature on the treatment of pediatric subtrochanteric femur fractures with flexible intramedullary nailing [16–19, 21, 38, 39]. Pombo and Shilt examined 13 patients with an average age of 8.7 years, with subtrochanteric femur fractures treated with titanium elastic nails [5]. They classified their results according to the Titanium Elastic Nails Outcome Scoring system [16]. There were no poor results. The only complications were leg length inequalities of 1.6 cm or less in two patients, which were attributed to physiologic overgrowth. The authors recommended advancing the lateral nail into or just distal to the greater trochanter apophysis, and advancing the medial nail into the femoral neck just short of the proximal femoral physis (Fig. 6.4a, b). This modification in technique may increase rotational and angular stability by decreasing the forces across the fracture site. The authors also suggested intraoperative stressing of the fracture after fixation to determine whether postoperative immobilization is necessary [5].
Stainless steel flexible intramedullary nails may be an alternative to titanium elastic nails for treatment of pediatric subtrochanteric femur fractures [19, 40]. Unlike titanium elastic nails , which are not optimal for length-unstable fractures, stainless steel nails have demonstrated good results in the treatment of length-stable and length-unstable pediatric femoral shaft fractures [40]. Distal locking of the stainless steel nail increases rotational control, and may prevent fracture shortening with a subsequent reduction in complications in length-unstable fractures [41]. Stainless steel nails have not been specifically studied in pediatric subtrochanteric femur fractures. The authors’ technical tips in flexible intramedullary nailing of pediatric subtrochanteric femur fractures can be found in Table 6.5.
Plating
Plate fixation is an alternative method of fixation in children 5–11 years of age with length-unstable femur fractures, children who weigh more than 49 kg, and children over 11 years who have a femoral canal that is too narrow for rigid intramedullary nailing. Traditional open plating and submuscular plating have been described for the treatment of pediatric subtrochanteric femur fractures [42, 43]. Traditional open plating requires more extensive soft tissue dissection, longer operating times, greater blood loss, and potential disruption of periosteal blood flood, thereby increasing the risk of delayed union or nonunion. In cases where proximal fixation is limited, long oblique fracture patterns or patient-specific anatomic constraints, locking plates allow fixation into the femoral neck, optimizing surgical fixation.
Alternatively, submuscular plating uses a minimally invasive insertion technique. Submuscular plates may function as internal “external fixators.” Indirect fracture reduction and increased biomechanical stability can be obtained with longer plates and fewer screws. The increased working length of a long plate leads to decreased strain on the construct and reduced pull-out force on the screws. Similar to placement of an external fixator, one screw should be placed just proximal and one screw should be placed just distal to the fracture. The remaining screws should be spread wide apart for maximum stability. For subtrochanteric femur fractures, the plate is inserted through a proximal incision over the lateral thigh. The plate is then advanced extraperiosteally between the lateral femur and vastus lateralis in a proximal-to-distal direction. Subtrochanteric femur fractures may be better stabilized with a locking plate. There is biomechanical evidence that locking plates provide more stable fixation than titanium elastic nails in femur fractures (Fig. 6.5a, b) [44, 45].
Kanlic et al. evaluated 51 pediatric femur fractures treated with submuscular plating , 24 % of which were in the subtrochanteric region. No postoperative immobilization was used. All of the fractures healed. No wound healing problems or infections were found. Eight percent of patients had a leg length inequality with the affected limb ranging from 23 mm shorter to 10 mm longer. However, none of the patients with subtrochanteric femur fractures experienced significant complications (Table 6.6) [46].
Rigid Intramedullary Nailing
Subtrochanteric femur fractures have been treated successfully with rigid intramedullary nailing in the adult population. These fractures may also be managed in adolescents using nails with a trochanteric entry point or lateral trochanteric entry point. Subtrochanteric femoral fractures have a short proximal fragment with a wide medullary canal, making standard locking techniques potentially inadequate to secure the short proximal fracture fragment. The wide medullary canal in the proximal femur increases the risk of the nail toggling due to lack of screw purchase; therefore, when appropriate a cephalomedullary nail should be used, because its screws engage the bone in the femoral neck. Malalignment of the proximal fragment may occur despite placement of the nail, which may be avoided by assuring an anatomic alignment and control of the proximal fragment during the procedure. The reconstruction femoral nail has a widened proximal section that incorporates one or more interlocking screws, designed to be placed into the femoral neck. While not directly applicable to the pediatric population, a Cochrane Database review of 189 adults with subtrochanteric femur fractures found that intramedullary nails were associated with fewer fracture fixation complications and higher healing rates than fixed angle plates [47]. Rigid intramedullary nailing can be safely performed in children 11 years to skeletal maturity with a subtrochanteric femur fracture using a trochanteric or a lateral trochanteric entry point, provided the femoral canal is large enough to accommodate the nail [48–50]. A more recent study suggests that children aged 7–12 years may also be acceptable candidates for such newer lateral-entry nailing techniques [51]. The main technical difference between pediatric and adult rigid intramedullary nailing is in the starting point of the femoral nail. A piriformis starting point in a skeletally immature patient places the posteriorly based medial femoral circumflex vessels at risk, injuries to which could lead to avascular necrosis of the femoral head, a rare, but serious, complication. MacNeil et al. performed a systematic review of 19 articles and found an avascular necrosis rate of 2 % when the nail was inserted from the piriformis fossa, compared to 1.4 % from the tip of the greater trochanter, and no reported cases from the lateral aspect of the greater trochanter (Fig. 6.6a, b) [52] (Table 6.7).
Outcomes and Complications
There are few reports in the literature on the outcomes and complications of treatment of pediatric subtrochanteric femur fractures. Complications are related to the strong deforming muscle forces acting at the fracture site and the treatment method. The risk of various complications for each treatment method is listed in Table 6.8.
Flexible Intramedullary Nailing
Titanium elastic nails are currently accepted as the preferred treatment for femoral shaft fractures in children 5–11 years of age; however, they have also been shown to be associated with a number of complications with fractures in the subtrochanteric region [16, 19, 20]. In fact, it was shown that almost a quarter of patients with proximal third femur fractures treated in such a way experienced complications [19]. Typically, those complications resulted from fracture displacement, and include leg-length differences, malunion, or irritating hardware [16–20, 53]. A need for additional surgery has been identified as a complication in children and adolescents with length-unstable fractures managed with titanium elastic nails [17, 18].
Narayanan et al. demonstrated that comminuted fractures had a five times greater risk of loss of reduction leading to reoperation or malunion. Pediatric subtrochanteric femur fractures usually result from a high-energy mechanism of injury, which is more likely to produce an unstable fracture pattern. If titanium elastic nailing is selected as the treatment method, the lateral nail should be advanced into or just distal to the greater trochanter apophysis, and the medial nail should be advanced into the femoral neck just short of the proximal femoral physis. Pombo and Shilt reported no major complications and no poor results in their series of 13 pediatric patients with subtrochanteric femur fractures treated using this technique [5]. However, fracture stability should be assessed intraoperatively after fixation, and postoperative immobilization with a single-leg spica cast, hip-knee-ankle-foot orthosis, or knee immobilizer should be considered if residual instability is found.
Plating
Caird et al. reviewed 60 pediatric patients with femoral shaft fractures treated with open plating. Twenty-five percent of the fractures were in the proximal third of the femur. The overall complication rate was 10 %, which included one early implant failure, two refractures after the plate was removed, two symptomatic leg length inequalities, and one hypertrophic scar. Four of these patients required unplanned surgery. Three of the six complications occurred in fractures of the proximal third of the femur [54].
In a multicenter retrospective study, Li et al. compared titanium elastic nailing with plating for the treatment of subtrochanteric femur fractures in 54 school-aged children. The authors found that patients treated with titanium elastic nails had a significantly higher overall complication rate than patients treated with plating (48 % versus 14 %), but the major complication rate was similar (Table 6.9). Outcome scores were also significantly better in the plating group than in the nail group, but both groups had high rates of excellent and satisfactory results (97 % and 92 % respectively). Length of hospitalization and time to radiographic union were comparable between the two groups. Plating technique did not appear to influence the complication rate and outcome, as the open plating and submuscular plating groups demonstrated similar results [20].
Conclusion
Subtrochanteric femur fractures are rare in the pediatric population, and are a challenge to treat. There is a lack of agreement on the definition of a subtronchanteric fracture in this age subset, and a dearth of literature evaluating treatment outcomes. Despite the lack of definitive treatment algorithms, there are some guidelines that should be followed. It is important to keep age and body size in mind when choosing a treatment option. The unique biomechanics around the subtrochanteric region and the torsion forces leading to injury are different than those seen in mid-shaft fractures, so must be taken into consideration. Corresponding injuries, fracture pattern, and rotational deformity are also important in determining the best course of care, and can be assessed through history and radiological examination. Pavlik harnesses are recommended for use in children 0–6 months of age. Spica casting is an acceptable form of treatment in children 6 months to 5 years of age with stable fractures. If the fracture is deemed too unstable, operative measures may be reasonable to pursue in this younger age group. The method of treatment in patients aged 5–11 years old is dependent upon stability, with flexible intramedullary nailing acceptable for stable fractures and open or submuscular plating viable options for more unstable fractures. Children aged 11 years to skeletal maturity are usually treated with rigid intramedullary nailing using a trochanteric or lateral trochanteric entry site. Finally, external fixation should be reserved for children with open fractures, polytrauma patients, and fractures with associated neurovascular injuries. There are complications and risks associated with all treatments, which should be discussed with the patient and family when considering the various care options.
References
Daum R, Jungbluth KH, Metzger E, Hecker WC. Results of treatment of subtrochanteric and supracondylous femoral fractures in children. Chirurg. 1969;40(5):217–20.
Jeng C, Sponseller PD, Yates A, Paletta G. Subtrochanteric femoral fractures in children. Alignment after 90 degrees-90 degrees traction and cast application. Clin Orthop Relat Res. 1997;341:170–4.
Blount WP, Schaefer A, Fox GW. Fractures of the femur in children. South Med J. 1944;37(9):481–93.
Ireland DC, Fisher RL. Subtrochanteric fractures of the femur in children. Clin Orthop Relat Res. 1975;110:157–66.
Pombo MW, Shilt JS. The definition and treatment of pediatric subtrochanteric femur fractures with titanium elastic nails. J Pediatr Orthop. 2006;26(3):364–70.
Paul JP. Force actions transmitted by joints in the human body. Proc R Soc Lond B Biol Sci. 1976;192(1107):163–72.
Rybicki EF, Simonen FA, Weis Jr EB. On the mathematical analysis of stress in the human femur. J Biomech. 1972;5(2):203–15.
Toridis TG. Stress analysis of the femur. J Biomech. 1969;2(2):163–74.
Galano GJ, Vitale MA, Kessler MW, Hyman JE, Vitale MG. The most frequent traumatic orthopaedic injuries from a national pediatric inpatient population. J Pediatr Orthop. 2005;25(1):39–44.
Theologis TN, Cole WG. Management of subtrochanteric fractures of the femur in children. J Pediatr Orthop. 1998;18(1):22–5.
Alho A, Ekeland A, Stromsoe K. Subtrochanteric femoral fractures treated with locked intramedullary nails. Experience from 31 cases. Acta Orthop Scand. 1991;62(6):573–6.
Rewers A, Hedegaard H, Lezotte D, Meng K, Battan FK, Emery K, et al. Childhood femur fractures, associated injuries, and sociodemographic risk factors: a population-based study. Pediatrics. 2005;115(5):e543–52.
Jawadi AH, Letts M. Injuries associated with fracture of the femur secondary to motor vehicle accidents in children. Am J Orthop (Belle Mead NJ). 2003;32(9):459–62. discussion 62.
Merten DF, Carpenter BL. Radiologic imaging of inflicted injury in the child abuse syndrome. Pediatr Clin North Am. 1990;37(4):815–37.
Kuzyk PR, Bhandari M, McKee MD, Russell TA, Schemitsch EH. Intramedullary versus extramedullary fixation for subtrochanteric femur fractures. J Orthop Trauma. 2009;23(6):465–70.
Flynn JM, Hresko T, Reynolds RA, Blasier RD, Davidson R, Kasser J. Titanium elastic nails for pediatric femur fractures: a multicenter study of early results with analysis of complications. J Pediatr Orthop. 2001;21(1):4–8.
Narayanan UG, Hyman JE, Wainwright AM, Rang M, Alman BA. Complications of elastic stable intramedullary nail fixation of pediatric femoral fractures, and how to avoid them. J Pediatr Orthop. 2004;24(4):363–9.
Sink EL, Gralla J, Repine M. Complications of pediatric femur fractures treated with titanium elastic nails: a comparison of fracture types. J Pediatr Orthop. 2005;25(5):577–80.
Ho CA, Skaggs DL, Tang CW, Kay RM. Use of flexible intramedullary nails in pediatric femur fractures. J Pediatr Orthop. 2006;26(4):497–504.
Li Y, Heyworth BE, Glotzbecker M, Seeley M, Suppan CA, Gagnier J, et al. Comparison of titanium elastic nail and plate fixation of pediatric subtrochanteric femur fractures. J Pediatr Orthop. 2013;33(3):232–8.
Moroz LA, Launay F, Kocher MS, Newton PO, Frick SL, Sponseller PD, et al. Titanium elastic nailing of fractures of the femur in children. Predictors of complications and poor outcome. J Bone Joint Surg Br. 2006;88(10):1361–6.
Barfod B, Christensen J. Fractures of the femoral shaft in children with special reference to subsequent overgrowth. Acta Chir Scand. 1959;116(3):235–50.
Park SS, Noh H, Kam M. Risk factors for overgrowth after flexible intramedullary nailing for fractures of the femoral shaft in children. Bone Joint J. 2013;95-B(2):254–8.
Staheli LT. Femoral and tibial growth following femoral shaft fracture in childhood. Clin Orthop Relat Res. 1967;55:159–63.
Blount WP. Fractures in children. Postgrad Med. 1954;16(3):209–16.
Griffin PP, Green WT. Fractures of the shaft of the femur in children: treatment and results. Orthop Clin North Am. 1972;3(1):213–24.
Wallace ME, Hoffman EB. Remodelling of angular deformity after femoral shaft fractures in children. J Bone Joint Surg Br. 1992;74(5):765–9.
Davids JR. Rotational deformity and remodeling after fracture of the femur in children. Clin Orthop Relat Res. 1994;302:27–35.
Podeszwa DA, Mooney III JF, Cramer KE, Mendelow MJ. Comparison of Pavlik harness application and immediate spica casting for femur fractures in infants. J Pediatr Orthop. 2004;24(5):460–2.
Rush JK, Kelly DM, Sawyer JR, Beaty JH, Warner Jr WC. Treatment of pediatric femur fractures with the Pavlik harness: multiyear clinical and radiographic outcomes. J Pediatr Orthop. 2013;33(6):614–7.
Epps HR, Molenaar E, O’Connor DP. Immediate single-leg spica cast for pediatric femoral diaphysis fractures. J Pediatr Orthop. 2006;26(4):491–6.
Pollak AN, Cooperman DR, Thompson GH. Spica cast treatment of femoral shaft fractures in children—the prognostic value of the mechanism of injury. J Trauma. 1994;37(2):223–9.
Jarvis J, Davidson D, Letts M. Management of subtrochanteric fractures in skeletally immature adolescents. J Trauma. 2006;60(3):613–9.
Barlas K, George B, Hashmi F, Bagga T. Open medial placement of Kirschner wires for supracondylar humeral fractures in children. J Orthop Surg (Hong Kong). 2006;14(1):53–7.
Bar-On E, Sagiv S, Porat S. External fixation or flexible intramedullary nailing for femoral shaft fractures in children. A prospective, randomised study. J Bone Joint Surg Br. 1997;79(6):975–8.
Wani MM, Dar RA, Latoo IA, Malik T, Sultan A, Halwai MA. External fixation of pediatric femoral shaft fractures: a consecutive study based on 45 fractures. J Pediatr Orthop B. 2013;22(6):563–70.
Ligier JN, Metaizeau JP, Prevot J, Lascombes P. Elastic stable intramedullary nailing of femoral shaft fractures in children. J Bone Joint Surg Br. 1988;70(1):74–7.
Flynn JM, Luedtke L, Ganley TJ, Pill SG. Titanium elastic nails for pediatric femur fractures: lessons from the learning curve. Am J Orthop. 2002;31(2):71–4.
Luhmann SJ, Schootman M, Schoenecker PL, Dobbs MB, Gordon JE. Complications of titanium elastic nails for pediatric femoral shaft fractures. J Pediatr Orthop. 2003;23(4):443–7.
Rathjen KE, Riccio AI, De La Garza D. Stainless steel flexible intramedullary fixation of unstable femoral shaft fractures in children. J Pediatr Orthop. 2007;27(4):432–41.
Ellis HB, Ho CA, Podeszwa DA, Wilson PL. A comparison of locked versus nonlocked Enders rods for length unstable pediatric femoral shaft fractures. J Pediatr Orthop. 2011;31(8):825–33.
Cortes LE, Triana M, Vallejo F, Slongo TF, Streubel PN. Adult proximal humerus locking plate for the treatment of a pediatric subtrochanteric femoral nonunion: a case report. J Orthop Trauma. 2011;25(7):e63–7.
Sanders S, Egol KA. Adult periarticular locking plates for the treatment of pediatric and adolescent subtrochanteric hip fractures. Bull NYU Hosp Jt Dis. 2009;67(4):370–3.
Li Y, Stabile KJ, Shilt JS. Biomechanical analysis of titanium elastic nail fixation in a pediatric femur fracture model. J Pediatr Orthop. 2008;28(8):874–8.
Porter SE, Booker GR, Parsell DE, Weber MD, Russell GV, Woodall Jr J, et al. Biomechanical analysis comparing titanium elastic nails with locked plating in two simulated pediatric femur fracture models. J Pediatr Orthop. 2012;32(6):587–93.
Kanlic EM, Anglen JO, Smith DG, Morgan SJ, Pesantez RF. Advantages of submuscular bridge plating for complex pediatric femur fractures. Clin Orthop Relat Res. 2004;426:244–51.
Parker MJ, Handoll HH. Gamma and other cephalocondylic intramedullary nails versus extramedullary implants for extracapsular hip fractures in adults. Cochrane Database Syst Rev. 2010;9, CD000093.
Keeler KA, Dart B, Luhmann SJ, Schoenecker PL, Ortman MR, Dobbs MB, et al. Antegrade intramedullary nailing of pediatric femoral fractures using an interlocking pediatric femoral nail and a lateral trochanteric entry point. J Pediatr Orthop. 2009;29(4):345–51.
Kanellopoulos AD, Yiannakopoulos CK, Soucacos PN. Closed, locked intramedullary nailing of pediatric femoral shaft fractures through the tip of the greater trochanter. J Trauma. 2006;60(1):217–22. discussion 22–3.
Gordon JE, Khanna N, Luhmann SJ, Dobbs MB, Ortman MR, Schoenecker PL. Intramedullary nailing of femoral fractures in children through the lateral aspect of the greater trochanter using a modified rigid humeral intramedullary nail: preliminary results of a new technique in 15 children. J Orthop Trauma. 2004;18(7):416–22. discussion 23–4.
Miller DJ, Kelly DM, Spence DD, Beaty JH, Warner Jr WC, Sawyer JR. Locked intramedullary nailing in the treatment of femoral shaft fractures in children younger than 12 years of age: indications and preliminary report of outcomes. J Pediatr Orthop. 2012;32(8):777–80.
MacNeil JA, Francis A, El-Hawary R. A systematic review of rigid, locked, intramedullary nail insertion sites and avascular necrosis of the femoral head in the skeletally immature. J Pediatr Orthop. 2011;31(4):377–80.
Sink EL, Faro F, Polousky J, Flynn K, Gralla J. Decreased complications of pediatric femur fractures with a change in management. J Pediatr Orthop. 2010;30(7):633–7.
Caird MS, Mueller KA, Puryear A, Farley FA. Compression plating of pediatric femoral shaft fractures. J Pediatr Orthop. 2003;23(4):448–52.
Davids JR, Frick SL, Skewes E, Blackhurst DW. Skin surface pressure beneath an above-the-knee cast: plaster casts compared with fiberglass casts. J Bone Joint Surg Am. 1997;79(4):565–9.
Heyworth BE, Hedequist DJ, Nasreddine AY, Stamoulis C, Hresko MT, Yen YM. Distal femoral valgus deformity following plate fixation of pediatric femoral shaft fractures. J Bone Joint Surg Am. 2013;95(6):526–33.
Hajek PD, Bicknell Jr HR, Bronson WE, Albright JA, Saha S. The use of one compared with two distal screws in the treatment of femoral shaft fractures with interlocking intramedullary nailing. A clinical and biomechanical analysis. J Bone Joint Surg Am. 1993;75(4):519–25.
Ricci WM, Gallagher B, Haidukewych GJ. Intramedullary nailing of femoral shaft fractures: current concepts. J Am Acad Orthop Surg. 2009;17(5):296–305.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer Science+Business Media New York
About this chapter
Cite this chapter
Seeley, M., Caird, M.S., Li, Y. (2016). Subtrochanteric Femur Fractures in Children. In: Hedequist, D., Heyworth, B. (eds) Pediatric Femur Fractures. Springer, Boston, MA. https://doi.org/10.1007/978-1-4899-7986-5_6
Download citation
DOI: https://doi.org/10.1007/978-1-4899-7986-5_6
Published:
Publisher Name: Springer, Boston, MA
Print ISBN: 978-1-4899-7984-1
Online ISBN: 978-1-4899-7986-5
eBook Packages: MedicineMedicine (R0)