Abstract
Our understanding of what happens in working muscle and at the whole-body level at sea level and at high altitude is different from that a few years ago. If dietary CHO and nutrition are adequate, at sea level metabolism shifts from a mix of lipid and CHO-derived fuels toward carbohydrate (glycogen, glucose, and lactate) oxidation at moderate and greater exercise intensities. As given by the Crossover Concept, a percentage to total energy expenditure, lipid oxidation is greatest at exercise power outputs eliciting 45–50 % of VO2max with greater intensities requiring relatively more CHO and lesser lipid oxidation. At altitude, a given exercise power output is achieved at a greater relative intensity expressed as % VO2max. Hence, exercise under conditions of hypoxia requires greater glycolytic flux, and lactate production than does the same effort at sea level, normoxic conditions. Glycolytic flux is further augmented at altitude by the effect of hypoxemia on sympathetic nervous system activity. Hence, augmented lactate production during exercise is adaptive. Over the short term, accelerated lactate flux provides ATP supporting muscle contraction and balances cytosolic redox. As well, lactate provides and energy substrate and gluconeogenic precursor. Over a longer term, via redox and ROS-generating mechanisms, lactate may affect adaptations in mitochondrial biogenesis and solute (glucose and lactate) transport. While important, the energy substrate, gluconeogenic, and signaling qualities of lactate production and disposal at altitude need to be considered within the context of overall dietary energy intake and expenditure during exercise at sea level and high altitude.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Background
1.1 Historical Perspective
Questions related to the balance of oxidative and glycolytic energy flux are traceable to the beginnings of modern biology. Working from the perspective of nineteenth century fermentation technologists who observed acid byproducts to accumulate in cultured yeast and bacteria cultured in the absence of oxygen, in the early twentieth century investigators working with non-perfused and deoxygenated frog muscle preparations readily concluded that lactic acidosis was attributable to oxygen lack [1]. However, it is now apparent that the Warburg Effect of aerobic glycolysis is not specific to tumor cells, but that glycolysis leading to lactate production is characteristic of mammalian cells whether studied in vitro or in vivo. Since the 1920s, interest in understanding the control of lactate production has been common to such disparate fields as exercise physiology, neuroscience, and tumor biology. More recently, focus has been on the Lactate Shuttle Mechanism to understand the pathways, controls, and physiological roles of lactate production and disposal. Based on simultaneous determinations of glucose and lactate flux rates in laboratory rodents [2, 3], as originally conceived, the Lactate Shuttle was hypothesized to be a mechanism to support glycolytic and aerobic energy production via oxidation and glucose homeostasis via gluconeogenesis [4]. However, via redox, ROS, and other mechanisms, lactate is being investigated for its role as a signaling molecule, i.e., as a “Lactormone.” In the contemporary literature in the field of neurobiology contains many investigations on Lactate Shuttling for neuron metabolism, glutaminergic signaling, peripheral energy store sensing, and appetite regulation [5] (Fig. 29.1). Not surprisingly, Larsen et al. [6] have shown that when arterial lactate rises during exercise, lactate is taken up and oxidized such that it substitutes, in part, for glucose. This very same effect has been demonstrated by Miller et al. [7] using lactate-clamp technology. Broad acceptance of the Lactate Shuttle Concept was demonstrated by investigators who have sought to disrupt the Lactate Shuttle as a mechanism for killing tumor cells [8]. In sum, while the field has been, and remains, controversial, there is widespread interest in lactate as is it obvious to many that critically important stress and strain mechanisms involve lactate formation and disposal.
A schematic illustration of the brain glycolytic pathway under aerobic conditions . A schematic illustration of the brain glycolytic pathway under aerobic conditions in which glucose is broken down to the glycolytic end-product lactate. Lactate, in turn, becomes the mitochondrial substrate, via its conversion to pyruvate, for the tricarboxylic acid cycle. At maximal work load, as measured in the study of Larsen et al. [6], most of the lactate that is utilized by brain mitochondria is muscular in origin and thus exogenous. Under resting conditions, most of the lactate used by brain mitochondria originates from glucose that is metabolized glycolytically in neurons and glia. From Schurr [5]
1.2 Early Studies at Altitude
Not to be inattentive or otherwise neglectful of then contemporary science, as described by Reeves [9], pioneer workers such as Dill et al. [10] and Edwards et al. [11] took an early interest in the lactate response at altitude. In the 1929 expeditions to Leadville, CO [10] and the Andes in Chile [11] observed in unacclimatized sojourners that during rest and exercise, blood lactate concentrations were evaluated at altitude above those seen at sea level. The conclusion at that time regarding the elevation in blood lactate was classic and based on the Pasteur Effect , glycolytic flux was increased because oxidative metabolism was limited. However, the pioneer investigators observed that after acclimatization to altitude, resting, and exercise, blood lactate levels declined despite the persistence of hypoxemia. And, moreover, other paradoxical observations, such as an inverse relationship between altitude and blood lactate levels, at the end of maximal exertion while blood lactate is elevated during submaximal exertion have been of interest [12]. Like the pioneers, we and others (e.g., [14]) have continued to be perplexed by the original and subsequent observations. In all of this could invocation of the term “paradox” simply mean that our understanding is inadequate?
Certainly there are many complications in studying metabolic responses to stress, but prominent in the field of carbohydrate metabolism at altitude are factors of ambient hypoxia, cachexia and malnutrition, changes in body mass and composition, changes in temperature, humidity, and photoperiod. Superimposed on those, sometimes also are factors associated with gender and racial differences , the stresses of travel, change of season, and hemisphere. And to complicate things more has to be recognition that acclimatization occurs and that experience at altitude and exposure to hypoxia affect outcomes. Hence, it is the position of this writer that the seemingly incongruent results obtained by diverse researchers are all appropriate for the conditions studied. However, with my colleagues at the USARIEM and inspired by J.T. Reeves and colleagues at the UCHSC, we have tried to dissect out and describe the effects of acute and chronic exposure hypoxia on energy substrate partitioning. Over the course of almost a decade, most of it before and subsequent to my participation in the effort, many contributions have been made in describing the metabolic responses of men and women to high altitude. I will try to do justice to this work, but at the outset I need to identify the key and essential contribution of Gail Butterfield to our efforts. Describing her seminal contribution provides insight into what we did, how we interpret the results, and how we read and interpret the literature.
From working with my colleagues on Pikes Peak, and now after almost four decades of studying intermediary metabolism, I have come to ask beginning students the following question: “What are the boundaries between nutrition and biochemistry, and between biochemistry and physiology?” Then, after hearing that the boundaries are hard to identify, I sometimes ask as second question: “What is the difference between stress and strain.” Ultimately, we end up in a continuing discussion about the interrelatedness of biological processes and conclude with increasing admiration for the complicated beauty of regulatory processes.
1.3 Dietary Controls
Because Gail Butterfield anticipated that the stress of altitude could affect metabolic rate, but that hypoxemia would cause a cachexia such that together the two effects of acute altitude exposure would cause an energy deficit that would affect metabolism, body mass, and body composition. She also knew that changes in the latter two (body mass and composition) would further affect metabolism. Hence, Gail insisted on tight dietary controls at lea level and at altitude. The following figures for the 1988 Pikes Peak Study illustrate what happens. Indeed, she and colleagues showed that BMR is elevated at 4300 m altitude and the increase persists over 3-weeks acclimatization [16] (Fig. 29.2). As well, because of the stress of altitude and the resulting energy deficit nitrogen balance is negative. The problem with nitrogen balance was corrected by the addition of ≈500 kcal/day depending on the subject’s response, so weight loss at altitude was minimized, though not prevented in two of seven subjects. And finally, in the same study it was shown that catecholamines are elevated on arrival at altitude, and while the epinephrine response diminishes over time, if anything circulating norepinephrine rises showing adrenal medullary activation at altitude [17]. Consequently, in subsequent investigations, investigators revisited issues related to sympathetic influences in the acute and chronic responses to altitude exposure.
Basal oxygen consumption at sea level and at 4300 m. Values are mean ± SEM for seven males. * Significant difference from sea level throughout. The elevation at day 6 was associated with the addition of ≈500 kcal/day to cover in increase in basal energy expenditure. From Butterfield et al. [16]
With adequate controls of macronutrient and energy nutrition in two studies on Pikes Peak, we [18, 19] saw increased glucose utilization during rest and a given absolute intensity of exercise (e.g., 100 W); effects on glucose flux and oxidation are greatest in men on arrival, but persists for 3 weeks at least even with best attempts at insuring dietary energy balance. With regard to hypoxia increasing glucose use, this observation is typical of tissues and cells in vitro [20], and nonhuman mammals [21]. However, what appears to be clear for the effect of hypoxia on metabolism is, in fact, not clear at all because according to the Crossover Concept [2], substrate flux and energy substrate partitioning are geared to relative exercise intensity. This effect of a given task being relatively more difficult at altitude than sea level was addressed by Braun et al. [23] who studied women at sea level at a power output eliciting 50 % VO2peak as was done previously for men [18, 19], but they determined also the glucose flux at 65 % VO2peak at SL in order to make a relative comparison to what happens at 4300 m. What Braun et al. found was that women responded differently from men, and when normalized to total energy expenditure (kcal/min), glucose flux was normalized over altitude and exercise intensity in women and 10 days after exposure to 4300 m.
1.4 The Fatty Acid Paradox
In the past, weight loss has been part of the tradition of altitude exposure, but the ritualistic hypophagia and dehydration dietary practices are not conducive to determining the effects of hypoxia on metabolism. And, the data obtained in the 1991 Pikes Peak study in which half the subjects were β-blocked reveals yet another, and relatively uninvestigated phenomenon; this is the “Fatty Acid Paradox.” Whether rest or exercise, β-blocked or not, arterial [FFA] rises during exercise [24] (Fig. 29.3). However, in contrast to what is typical at sea level, a rise in [FFA] during exercise at altitude reflects not increased, but decreased use as the net FFA uptake [limb blood flow (a-v)] for working limb muscle declines to zero as the RQ approaches unity [24]. Clearly, within the context of energy balance and appropriate CHO nutrition working muscle uses little lipid as a substrate. In fact, we [25, 26] have recently shown that little lipid is used in working limb muscle at sea level. In the light of these data showing the dominance of CHO fuel energy use in working muscle, if it occurs inadequate total and CHO nutrition at altitude deprives muscle of it’s preferred substrate, forces use of less preferred fatty- and amino acids and results in the loss of body mass. That mountaineers reach great heights while malnourished and dehydrated is sheer testament to their inner and physical strength.
Mean free fatty acid and glycerol exchanges across the lets (mean ± SEM) in five control and six β-blocked men at rest and during exercise at sea level, upon acute exposure to 4300 m altitude, and after 3 weeks at 4300 m. Data from Roberts et al. [24]
2 What People Do Determines What They See
2.1 The Lactate Faux Pas
It is historic that much of the discussion of metabolism at high altitude has centered on lactate. In a broader sense, this focus on but one aspect of CHO metabolism has been to ignore effects of hypoxia and environment on the possibilities of fatty acid and amino acid paradoxes. With regard to the historic interest and discussion of a “Lactate Paradox,” the dialogue is useful to the extent that it furthers our understanding of what happens at altitude and during exercise at altitude. Hence, while the pioneers and more recent investigators have observed phenomena descriptive of a “paradox,” others have not. To reiterate, because I believe all the data to be valid, variability in the results means, to me, that different studies were done on different persons, at different times in different places. Time and space are limited so the discussion is compressed to CHO nutrition, gender, and mechanism.
2.2 Macronutrient Nutrition and Exercise Metabolism
In the early 1980s, we [27] and Heigenhauser et al. [28] independently studied the effects of glycogen depletion on ventilatory and blood lactate responses to graded exercises. The two studies showed glycogen-depleted subjects the ventilatory threshold came at a lower exercise power output than when the same subjects were not glycogen depleted. In contrast to the VT is displaced left, the lactate response and hence, the Lactate Threshold (LT) is right-shifted and appears at a higher power output. Therefore, we can reasonably expect to see that in subjects who have lost body weight at altitude, the tendency for glycolysis to be accelerated will be counterbalanced by the effect of glycogen depletion.
2.3 Gender
In his recent review appearing in MSSE, Braun [29] addressed the mechanism of increased metabolic efficiency at altitude and produced an interpretation similar to that presented here. Using some of data previously shown above, Braun compared metabolic responses at altitude in partially acclimatized men and women at altitude. In an altitude-induced shift to increased glucose use is evident, whereas this shift is not evident in women. Indeed, in a series of investigations by Braun and colleagues have shown a greater metabolic resilience in women compared to men at altitude. As well, independently we have shown differences in fatty acid [30] and glucose metabolism [31] in men and women during exercise and recovery from exercise at sea level.
2.4 Mechanism
Greater glucose disposal rates , but unchanged insulin levels imply increased insulin sensitivity at altitude [18, 19]. In subjects studied with dietary controls, Braun (ref) demonstrated increased insulin sensitivity in subjects 10 days after arrival on Pikes Peak (4300 m). However, by stimulating epinephrine, altitude exposure has the possibility to elicit insulin resistance. Such an effect may have been observed by Larsen et al. on Monte Rosa (4559 m) [32] in subjects studied 2 days after arrival at altitude exposure. Limited data are available on mechanism of hypoxia-stimulated muscle glucose uptake, but it appears that AMPKα2 is upregulated in hypoxia as it is during normoxic exercise [33].
Glycogenolysis , and hence lactate production during rest and exercise, is influenced by the sympathetic response to hypoxia. Epinephrine rises on exposure and is associated with increments in muscle glucose uptake [18] and lactate flux and accumulation [17] (Fig. 29.4). In our experience, the rise in epinephrine wanes with exposure, but it is apparent also that sensitivity to epinephrine rises over time with exposure to altitude. This effect of acclimatization was revealed in studies on Pikes Peak using β-blockade that increased glucose and decreased fatty acid uptake [18, 19]. In contrast to epinephrine, norepinephrine rises with acclimatization [17]. Hence, it is apparent that the changes in substrate utilization that occur over time correspond to epinephrine. It needs to be noted, however, that while the pattern of catecholamine response to altitude was similar in men and women, metabolic responses to altitude were less perturbed in women than men.
Mean blood lactate rate of appearance (Ra) [±SEM] as a function of mean epinephrine concentration [±SEM] in men at sea level (open squares), upon acute exposure to 4300 m altitude (diamonds), and after 3 weeks of acclimatization to 4300 m (triangles). From Brooks et al. [46]
3 Why Lactate?
3.1 The Oxygen Deficit Shortfall
The conventional view that an oxygen deficit is responsible for lactate production and accumulation during rest or exercise is unsupported in the literature. As well, there is confusion equating lactate “accumulation” and “production,” the mistake reflecting the assumption that lactate is a “dead end,” as opposed to dynamic metabolic intermediate that servers multiple functions. And, even associating lactate production and accumulation, the conclusion that either or both are attributable to oxygen limitations is not supportable. Numerous times we [12, 34–38] and others have shown lactate production in resting individuals at sea level. Importantly, we have shown that the decline in blood [lactate] that accompanies exercise after training is largely attributable to enhanced clearance, and secondarily to better matching of glycolytic flux to energy demand. Whether at rest or during exercise, whether at sea level or 4300 m altitude, or during submaximal exercise at altitude with or without β-blockade, the circulation transports sufficient oxygen to maintain working muscle oxygen consumption [24, 38].
With regard to the state of tissue oxygenation as causal to working muscle lactate accumulation and net release, our results and interpretations are entirely consistent with those of Richardson, Wagner and associates who studied the effect of breathing gas containing 12 and 21 % O2 at 1 ATM ambient pressure on c irculating epinephrine and muscle oxygenation and lactate net release (efflux) during graded exercise [40]. The hypoxemia of breathing 12 % O2 increased muscle lactate efflux while having a minimal effect on oxygenation which was 3–4 Torr and well above the critical mitochondrial PO2 of ≈1.0 Torr. Instead of a deficiency in O2 supply or muscle oxygenation, hypoxemia left shifted relationships between arterial epinephrine and working leg muscle VO2, and between muscle lactate efflux and working leg muscle VO2. As a result, net muscle lactate efflux was related to arterial epinephrine level.
In gaining an appreciation for the magnitude of lactate flux at rest, and the effects of exercise, acute hypoxia, and altitude acclimatization on it, it is useful to compare glucose and lactate fluxes determined simultaneously using dual tracers. From our first study on Pikes Peak, the resting 12-h glucose flux at sea level was ≈ 2 mg/kg/min, and the lactate flux about a third of the glucose value. On acute exposure, both fluxes rose significantly, but not the lactate and glucose fluxes were approximately equal. And, after a 3-weeks sojourn at 4300 m, the lactate flux declined somewhat, as did epinephrine, but the glucose flux rose still further [36]. During 100 W leg cycle ergometer exercise at SL, glucose flux doubled over rest, and lactate flux approximated the glucose flux. On acute exposure to altitude, glucose flux increased over that at sea level, but the lactate flux increased many times more. With acclimatization, the glucose flux during exercise increased over that on initial exposure, while the lactate flux declin ed.
3.2 Stainsby and Other Effects
Our operating hypothesis is that of the Lactate Shuttle which now has Cell-Cell and Intracellular components . We and others have observed net release by particular tissues (e.g., working muscle at the onset of exercise) and net consumption by others (e.g., the heart) [41]. We know also that tissues such as a working muscle bed can switch from net consumption to release and that simultaneous production and utilization always occurs, thus obscuring the extent of turnover within cells and tissues. A prime example of this “Stainsby Effect” where by working muscle switches from lactate net release to uptake was seen in men studied at SL on Pikes Peak both before and after acclimatization (39 Brooks). The results are to be contrasted with the corresponding arterial blood levels, and example of which is found in observations that stable blood lactate levels were achieved during exercise with the lowest values being observed at SL, the highest on acute exposure, and with intermediate blood lactate levels after the 3-weeks acclimatization period. However, as seen in, regardless of altitude condition, lactate release is a feature after 5 min of exercise, with highest net release on acute exposure but declining net release transitioning in some cases to net uptake all the while arterial lactate concentration is elevated and pulmonary and working limb rates of oxygen consumption elevated over rest, but not different due to condition during exercise. That so many cells and tissues can produce and exchange lactate makes the task of understanding lactate from blood concentration (a-v) difference, biopsy, or flux measurements far more difficult than understanding glucose flux that under postabsorptive conditions is by the liver with one point of entry into the circulation.
4 A Different View of the Role of Lactate
4.1 The Lactate Shuttle Mechanism
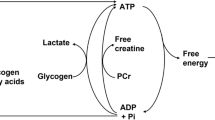
The lactate shuttle works because lactate, the product of glycolysis, is the substrate for oxidative metabolism. Further, because MCTs are ubiquitous, lactate can shuttle down concentration and H+ gradients, fluxing between cellular organelles (e.g., cytosol and mitochondria, and cytosol and peroxisomes), between cells in the same tissue (e.g., white Type 2b(x) and red Type 1 fibers), and between tissues and organs via vascular conductance (e.g., working muscle and heart). As mentioned earlier, there is utility in the formation and lactate exchange because lactate is an important energy source, the most important gluconeogenic precursor, and a lactormone [4]. The realization that lactate shuttles as it does lead to discovery that membrane permeation is via facilitated transport involving characteristics of saturation, stereo-specificity, competition, hydrogen ion co-transport, bi-directionality, and inhibition by specific molecules. These lactate transport proteins are now recognized to be products of a gene superfamily of solute transporters (SLC16), of which the first four (monocarboxylate transporters 1–4 (i.e., MCT1–MCT4)) are lactate-pyruvate transporters. Of these, MCT1 appears to be most ubiquitously expressed, but there being cell type and cell domain differences in MCT expression.
Having participated in discovery of the proteins now called MCTs and having also helped demonstrate their tissue and cell type expression and compartmentation, my bias is that lactate/pyruvate transporters are important. However, it is important to know that while they are lactate anion-proton symporters, MCTs are not the only means for cells to extrude protons. Further, so far as solute transport is concerned, the MCTs support facilitated exchange down concentration and pH gradients. More important, therefore, are the processes that establish the concentration gradients; here I speak of the circulation and mitochondrial respiration. The circulation is essential because it delivers oxygen for mitochondrial respiration and also because it is responsible fo r bulk flow delivery of lactate from cells and tissues of production to disposal sites.
4.2 Muscle Lactate Oxidation, the Mitochondrial Lactate Oxidation Complex, and Mitochondrial Dynamics
To reiterate, there are at least three biological functions of lactate (substrate oxidation, gluconeogenic precursor, and signaling molecule) [4]. Unfortunately, working muscle and whole-body lactate oxidation rates are less well worked out at altitude, but there are very good data for sea level. From Bergman et al. [33], Stanley et al. [34], Mazzeo et al. [35], and Brooks et al. [12], we know that lactate oxidation tracks disposal rate, and that working muscle, resting or working in the range of 45–65 % of VO2max accounts for 50–60 % of lactate Rd. At altitude, we have as yet to measure pulmonary and working muscle 13CO2 production following vascular infusion of 13C-lactate tracer, but from efforts on Pikes Peak we know that arterial lactate concentration, tracer-measured lactate production and disposal, circulating epinephrine are highly correlated [36]. As well, from tracer-measured lactate fractional extraction during rest and during exercise at SL and after acute and chronic exposures to 4300 m we know that lactate extraction is concentration dependent [37].
4.3 The Mitochondrial Lactate Oxidation Complex (mLOC)
That working muscles and heart oxidize lactate raises the question as to how. Some have concluded that lactate is oxidized to pyruvate in working muscle, but cytosolic lactate oxidation is unlikely, and contrary to data available on humans and dogs as studied by Zinker et al. [21]. With dogs made hypoxic by breathing 11 % O2 gas, they observed net lactate exchange and net and tracer-measure glucose uptake. They found that hypoxia increased glucose flux and working limb glucose and lactate uptake. More importantly, from carbon-labeled glucose they observed that half the glucose uptake observed was released as lactate. Hence, as with our experience with humans, the data of Zinker et al. are consistent with cytosolic glycolysis and contrary to cytosolic lactate oxidation. However, the data on running dogs is extraordinary showing simultaneous glycolysis to lactate and net lactate uptake.
Given our results and those of others, we took the obvious steps to investigate direct mitochondrial oxidation of lactate. We took several approaches to the problem. First, we [42] respired mitochondria from rat liver, heart, and skeletal muscle and found that respiration with each preparation was greater with lactate + malate than with pyruvate + malate. These findings were taken to mean that mitochondria require a lactate/pyruvate transporter and lactate dehydrogenase (LDH). To evaluate the potential role of LDH in mitochondrial lactate oxidation, we treated mitochondria with oxamate, and inhibitor of LDH, and found that lactate oxidation was inhibited whereas pyruvate oxidation was increased. To evaluate the potential role of MCT1, we treated mitochondria with cinnamate, a known MCT inhibitor, and respiration with both lactate and pyruvate was blocked. However, with the addition of either succinate or glutamate, the blockage to MCT inhibition was bypassed. Subsequently, a more careful reading of the literature revealed that these effects had been demonstrated previously, but the results were overlooked.
To demonstrate the presence of mitochondrial LDH (mLDH) and MCT1 (mMCT1), we isolated mitochondria and probed for the presence of mLDH and mMCT1 obtaining positive results. And when others failed to replicate our results, we sought to demonstrate mLDH and mMCT1 by electron microscopy (for LDH) and confocal laser scanning microscopy (LDH, MCT1 and other proteins). In both adult cells and cultured myocytes, mMCT1 and mLDH (Fig. 29.5) are clearly visible [43, 44]. Further, because the results were suggestive of the presence of a mitochondrial lactate oxidation complex (mLOC) comprised minimally of MCT1, LDH, Basigin, and cytochrome oxidase (COX). And, using combinations of cell fractionation, differential centrifugation and Western blotting, as well as immunocoprecipitation, we have verified presence of the mLOC in cultured myocytes and adult limb skeletal muscle. Realizing generality of our findings on muscle, we collaborated with Daniela Kaufer, an acclaimed neurobiologist and demonstrated the mLOC in primary neuronal cell cultures and adult rat brains [45]. Bolstered by publication of the MitoCarta [46] that contains the purported four mLOC proteins , at present we are utilizing muscle cell culture, pulse-chase tracer technology, and the most advanced techniques of proteomics to independently verify the existence of mLOC proteins, and to identify the factors responsible for mitochondrial biogenesis and protein turnover rates.
Immunohistochemical images demonstrating some components of the lactate oxidation complex in L6, cultured rat muscle cells . This complex involves the mitochondrial constituent cytochrome oxidase, the lactate transport protein, lactate dehydrogenase (LDH), and other constituents. (a) Co-localization of the lactate transport protein (MCT1) and the mitochondrial reticulum. MCT1 was detected at both sarcolemmal and intracellular domains (A-1). The mitochondrial reticulum was extensively elaborated and detected at intracellular domains throughout L6 cells (A-2). When signals from probes for the lactate transporter (MCT1, green, A-1) and mitochondria (red, A-2) were merged, superposition of the signals (yellow) showed co-localization of MCT1 and components of the mitochondrial reticulum, particularly at perinuclear cell domains (A-3). In panel (b), Lactate dehydrogenase (LDH) (B-1) and mitochondrial cytochrome oxidase (COX) where most oxygen is actually used in cells (B-2) are imaged. Superposition of signals for LDH (red, B-1) and COX (green, B-2) shows co-localization of LDH in the mitochondrial reticulum (yellow) of cultured L6 rat muscle cells (B-3). Depth of field ~1 μm, scale bar = 10 μm. From Hashimoto et al. [44]
Getting close to closing, it is essential to mention a new field in which we are returning to an old theme that has been reinvigorated by new technology and discoveries. Today, it is passé to use terminology “mitochondrion” and “mitochondria” as terms mitochondrial “reticulum,” “network,” and “dynamics” have come into use.
The exploding field of mitochondrial dynamics has shown that structure of the mitochondrial reticulum constantly undergoes turnover. Fission involves the transmembrane protein fission-1 (Fis1) and dynamin-related (like) protein (Drp1 or DLP1 ). The mechanism has been reviewed by Yoon [47] who summarizes his work and that of others in this exciting and emerging field. Drp1 is a large GTPase (80–85 kDa, with multiple splicing variants) that assemble onto the outer surface of mitochondria during mitochondrial fission and sever the mitochondrial membrane via the GTP hydrolysis-mediated mechanical pinching. Mitochondrial scission appears to involve Fis1, a small helix-rich mitochondrial outer membrane protein [48]. The Drp1-Fis1 complex apparently acts as a molecular noose pinching off sections of the mitochondrial reticulum in effect causing fission. A “normal,” but as yet unknown rate of mitochondrial turnover is apparently necessary because Yoon [47] has shown mitochondrial dysfunction in cells overexpressing Fis1. In contrast, in recent case study [49], it was reported on the lethal effect in a newborn of a defect in Drp1 as rendering the protein ineffective. Significant current research includes our own focuses on Drp1 as it is the only mGTPase known to be regulated by phosphorylation (51). Following their lead, we are following up with studies of the effects of lactate, other ROS generators, and putative regulators of mitochondrial biogenesis.
5 Summary
This portrayal of what happens in working muscle and at the whole-body level is different from what might have been rendered a few years ago. If dietary CHO and nutrition are adequate, metabolism shifts toward glucose and total CHO oxidation. As given by the Crossover Concept, a percentage to total energy expenditure, lipid oxidation is greatest at exercise power outputs eliciting 45–50 % of VO2max with greater intensities requiring relatively more CHO, and lesser lipid oxidation. At altitude, a given exercise power output is achieved at a greater relative intensity expressed as % VO2max. Hence, exercise under conditions of hypoxia requires greater glycolytic flux, and lactate production than does the same effort at sea level, normoxic conditions. Glycolytic flux is further augmented at altitude by the effect of hypoxemia on sympathetic nervous system activity. Hence, augmented lactate production during exercise is adaptive. Over the short term, accelerated lactate flux provides ATP supporting muscle contraction and balances cytosolic redox. As well, lactate provides an energy substrate and gluconeogenic precursor. Over a longer term, via redox and ROS-generating mechanisms, lactate may affect adaptations in mitochondrial biogenesis and solute (glucose and lactate) transport.
References
Brooks GA, Gladden LB. Metabolic systems: non-oxidative (Glycolytic and Phosphagen). In: Tipton CM, editor. Exercise physiology: people and ideas. Bethesda, MD: American Physiological Society; 2003. p. 322–60.
Brooks GA, Donovan CM. Effect of training on glucose kinetics during exercise. Am J Physiol. 1983;244:E505–12.
Donovan CM, Brooks GA. Endurance training affects lactate clearance, not lactate production. Am J Physiol. 1983;244:E83–92.
Brooks GA. Mammalian fuel utilization during sustained exercise. Comp Biochem Physiol B. 1998;120:89–107.
Schurr A. Lactate: the ultimate cerebral oxidative energy substrate? J Cereb Blood Flow Metab. 2006;26:142–52.
Larsen TS, Rasmussen P, Overgaard M, Secher NH, Nielsen HB. Non-selective beta-adrenergic blockade prevents reduction of the cerebral metabolic ratio during exhaustive exercise in humans. J Physiol. 2008;586:2807–15.
Miller BF, Fattor JA, Jacobs KA, Horning MA, Suh S-H, Navazio F, Brooks GA. Lactate-glucose interaction in men during rest and exercising using lactate clamp procedure. J Physiol. 2002;544:963–75.
Sonveaux P, Végran F, Schroeder T, Wergin MC, Verrax J, Rabbani ZN, De Saedeleer CJ, Kennedy KM, Diepart C, Jordan BF, Kelley MJ, Gallez B, Wahl ML, Feron O, Dewhirst MW. Targeting lactate-fueled respiration selectively kills hypoxic tumor cells in mice. J Clin Invest. 2008;118:3930–42.
Reeves JT, Wolfel EE, Green HJ, Mazzeo RS, Young AJ, Sutton JR, Brooks GA. Oxygen transport during exercise at high altitude and the lactate paradox: lessons from Operation Everest II and Pikes Peak. In: Exercise and sport science reviews, vol. 20. Baltimore, MD: Williams and Wikins; 1992. p. 275–96.
Dill DB, Edwards HT, Fölling A, Oberg SA, Pappenheimer AM, Talbott JH. Adaptations of the organism to changes in oxygen pressure. J Physiol. 1931;71:47–63.
Edwards HT. Lactic acid in rest and work at high altitudes. Am J Physiol. 1936;116:367–75.
Brooks GA, Butterfield GE, Wolfe RR, Groves BM, Mazzeo RS, Sutton JR, Wolfel EE, Reeves JT. Decreased reliance on lactate during exercise after acclimatization to 4,300m. J Appl Physiol. 1991;71:333–41.
Sutton JR, Reeves JT, Wagner PD, Groves BM, Cymerman A, Malconian MK, Rock PB, Young PM, Walter SD, Houston CS. Operation Everest II: oxygen transport during exercise at extreme simulated altitude. J Appl Physiol. 1988;64:1309–21.
Lundby C, Van Hall G. Substrate utilization in sea level residents during exercise in acute hypoxia and after 4 weeks of acclimatization to 4100 m. Acta Physiol Scand. 2002;176:195–201.
Butterfield GE, Gates J, Brooks GA, Groves BM, Mazzeo RS, Sutton JR, Reeves JT. Energy balance and weight loss during three weeks at 4,300m. J Appl Physiol. 1992;72:1741–8.
Mazzeo RS, Brooks GA, Butterfield GE, Cymerman A, Roberts AC, Selland M, Wolfel EE, Reeves JT. β-adrenergic blockade does not prevent lactate response to exercise after acclimatization to high altitude. J Appl Physiol. 1994;76:610–5.
Brooks GA, Butterfield GE, Wolfe RR, Groves BM, Mazzeo RS, Sutton JR, Wolfel EE, Reeves JT. Increased dependence on blood glucose after acclimatization to 4,300m. J Appl Physiol. 1991;70:919–27.
Roberts AC, Reeves JT, Butterfield GE, Mazzeo RS, Sutton JR, Wolfel EE, Brooks GA. Altitude and ß-Blockade augment glucose utilization during exercise. J Appl Physiol. 1996;80:605–15.
Cartee GD, Douen AG, Ramlal T, Klip A, Holloszy JO. Stimulation of glucose transport in skeletal muscle by hypoxia. J Appl Physiol. 1999;70:1593–600.
Zinker BA, Wilson RD, Wasserman DH. Interaction of decreased arterial PO2 and exercise on carbohydrate metabolism in the dog. Am J Physiol. 1995;269:E409–17.
Brooks GA, Mercier J. The balance of carbohydrate and lipid utilization during exercise: the ‘crossover’ concept. Brief review. J Appl Physiol. 1994;76:2253–61.
Braun B, Mawson JT, Muza SR, Dominick S, Brooks GA, Horning MA, Rock PB, Moore LG, Mazzeo RS, Ezeji-Okoye SC, Butterfield GE. Women at altitude: carbohydrate utilization during rest and exercise at 4300 m elevation and across the menstrual cycle. J Appl Physiol. 2000;88:246–56.
Roberts AC, Butterfield GE, Reeves JT, Wolfel EE, Brooks GA. Acclimatization to 4,300 m altitude decreases reliance on fat as substrate. J Appl Physiol. 1996;81:1762–71.
Friedlander AL, Jacobs KA, Fattor JA, Horning MA, Hagobian TA, Bauer TA, Wolfel EE, Brooks GA. Contributions of working muscle to whole body lipid metabolism vary with exercise intensity and training. Am J Physiol Endocrinol Metab. 2007;292:E107–16.
Wallis GA, Friedlander AL, Jacobs KA, Horning MA, Fattor JA, Wolfel EE, Lopaschuk GD, Brooks GA. Substantial working muscle glycerol turnover during two-legged cycle ergometry. Am J Physiol Endocrinol Metab. 2007;293:E950–7.
Hughes EF, Turner SC, Brooks GA. Effects of glycogen depletion and pedaling speed on the “anaerobic threshold”. J Appl Physiol. 1982;52:1598–607.
Heigenhauser GJ, Sutton JR, Jones NL. Effect of glycogen depletion on the ventilatory response to exercise. J Appl Physiol. 1983;54:470–4.
Braun B. Effects of high altitude on substrate use and metabolic economy: cause and effect? Med Sci Sports Exerc. 2008;40:1495–500.
Henderson GC, Fattor JA, Horning MA, Faghihnia N, Johnson ML, Mau TL, Luke-Zeitoun M, Brooks GA. Lipolysis and free fatty acid metabolism during the post-exercise recovery period. J Physiol. 2007;584:963–81.
Henderson GC, Fattor JA, Horning MA, Faghihnia N, Johnson ML, Luke-Zeitoun M, Brooks GA. More precise postexercise glucoregulation in women than men. Am J Clin Nutr. 2008;87:1686–94.
Larsen JJ, Hansen JM, Olsen NV, Galbo H, Dela F. The effect of altitude hypoxia on glucose homeostasis in men. J Physiol. 1997;504:241–9.
Wadley GD, Lee-Young RS, Canny BJ, Wasuntarawat C, Chen ZP, Hargreaves M, Kemp BE, McConell GK. Effect of exercise intensity and hypoxia on skeletal muscle AMPK signaling and substrate metabolism in humans. Am J Physiol Endocrinol Metab. 2006;290:E694–702.
Bergman BC, Wolfel EE, Butterfield GE, Lopaschuk G, Casazza GA, Horning MA, Brooks GA. Active muscle and whole body lactate kinetics after endurance training in men. J Appl Physiol. 1999;87:1684–96.
Stanley WC, Gertz EW, Wisneski JA, Morris DL, Neese R, Brooks GA. Systemic lactate turnover during graded exercise in man. Am J Physiol. 1985;249:E595–602.
Mazzeo RS, Brooks GA, Schoeller DA, Budinger TF. Disposal of [1-13C]-lactate during rest and exercise. J Appl Physiol. 1986;60:232–41.
Brooks GA, Wolfel EE, Groves BM, Bender PR, Butterfield GE, Cymerman A, Mazzeo RS, Sutton JR, Wolfe RR, Reeves JT. Muscle accounts for glucose disposal but not lactate release during exercise after acclimatization to 4,300 m. J Appl Physiol. 1992;72:2435–45.
Brooks GA, Wolfel EE, Butterfield GE, Cymerman A, Roberts AC, Mazzeo RS, Reeves JT. Poor relationship between arterial [lactate] and leg net release during steady-rate exercise at 4,300 m altitude. Am J Physiol. 1998;275:R1192–201.
Wolfel EE, Bender PR, Brooks GA, Butterfield GE, Groves BM, Mazzeo RS, Sutton JR, Reeves JT. Oxygen transport during steady state, submaximal exercise in chronic hypoxia. J Appl Physiol. 1991;70:1129–36.
Richardson RS, Noyszewski EA, Leigh JS, Wagner PD. Lactate efflux from exercising human skeletal muscle: role of intracellular PO2. J Appl Physiol. 1998;85:627–34.
Gertz EW, Wisneski JA, Stanley WC, Neese RA. Myocardial substrate utilization during exercise in humans. Dual carbon-labeled carbohydrate isotope experiments. J Clin Invest. 1988;82:2017–25.
Brooks GA, Dubouchaud H, Brown M, Sicurello JP, Butz CE. Role of mitochondrial lactate dehydrogenase and lactate oxidation in the ‘intra-cellular lactate shuttle’. Proc Natl Acad Sci U S A. 1999;96:1129–34.
Hashimoto T, Masuda S, Taguchi S, Brooks GA. Immunohistochemical analysis of MCT1, MCT2 and MCT4 expression in rat plantaris muscle. J Physiol. 2005;567:121–9.
Hashimoto T, Hussien R, Brooks GA. Colocalization of MCT1, CD147 and LDH in mitochondrial inner membrane of L6 cells: evidence of a mitochondrial lactate oxidation complex. Am J Physiol Endocrinol Metab. 2006;290:1237–44.
Hashimoto T, Hussien R, Cho H-S, Kaufer D, Brooks GA. Evidence for a mitochondrial lactate oxidation complex in rat neurons: a crucial component for a brain lactate shuttle. PLoS One. 2008;3(8):e2915.
Pagliarini DJ, Calvo SE, Chang B, Sheth SA, Vafai SB, Ong SE, Walford GA, Sugiana C, Boneh A, Chen WK, Hill DE, Vidal M, Evans JG, Thorburn DR, Carr SA, Mootha VK. A mitochondrial protein compendium elucidates complex I disease biology. Cell. 2008;134:112–23.
Yoon Y. Sharpening the scissors: mitochondrial fission with aid. Cell Biochem Biophys. 2004;41:193–206.
James DI, Parone PA, Mattenberger Y, Martinou JC. hFis1, a novel component of the mammalian mitochondrial fission machinery. J Biol Chem. 2003;278:36373–9.
Waterham HR, Koster J, Roermund CW, Mooyer PA, Wanders RJ, Leonard JV. A lethal defect of mitochondrial and peroxisomal fission. N Engl J Med. 2007;356:1736–41.
Cribbs JT, Strack S. Reversible phosphorylation of Drp1 by cyclic AMP-dependent protein kinase and calcineurin regulates mitochondrial fission and cell death. EMBO Rep. 2007;8:939–69.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer Science+Business Media New York
About this chapter
Cite this chapter
Brooks, G.A. (2016). Energy Flux, Lactate Shuttling, Mitochondrial Dynamics, and Hypoxia. In: Roach, R., Hackett, P., Wagner, P. (eds) Hypoxia. Advances in Experimental Medicine and Biology, vol 903. Springer, Boston, MA. https://doi.org/10.1007/978-1-4899-7678-9_29
Download citation
DOI: https://doi.org/10.1007/978-1-4899-7678-9_29
Published:
Publisher Name: Springer, Boston, MA
Print ISBN: 978-1-4899-7676-5
Online ISBN: 978-1-4899-7678-9
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)