Abstract
Astrocytes provide the structural and functional interface between the cerebral circulation and neuronal networks. They enwrap all intracerebral arterioles and capillaries, control the flux of nutrients as well as the ionic and metabolic environment of the neuropil. Astrocytes have the ability to adjust cerebral blood flow to maintain constant PO2 and PCO2 of the brain parenchyma. Release of ATP in the brainstem, presumably by local astrocytes, helps to maintain breathing and counteract hypoxia-induced depression of the respiratory network. Astrocytes also appear to be involved in mediating hypoxia-evoked changes in blood–brain barrier permeability, brain inflammation, and neuroprotection against ischaemic injury. Thus, astrocytes appear to play a fundamental role in supporting neuronal function not only in normal conditions but also in pathophysiological states when supply of oxygen to the brain is compromised.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
The central nervous system is hig hly vulnerable to changes in energy supply. Permanent damage to the human brain occurs when oxygen delivery is interrupted for more than several minutes. However, brain cells differ significantly in terms of their susceptibility to the effects of energy depletion. For example, in vitro studies have shown that glucose deprivation affects ionic gradients associated with decreases in cellular levels of ATP, ADP, phosphocreatinine and creatinine in both major types of brain cells—neurons and astrocytes. However, these changes are more pronounced and occur faster in neurons than in astrocytes [30]. Similarly, in conditions of hypoxia, neurons show a substantial decrease in both ATP and phosphocreatinine, whilst astrocytes remain largely unaffected if glucose is available [1].
Cerebral microcirculation in spec ific brain regions is regulated by mechanisms that match local blood flow to the levels of neuronal activity and metabolism. When neuronal activity increases local microvasculature dilates in order to divert more oxygenated blood to the active area. This neurovascular coupling mechanism is termed functional hyperaemia. When the brain is exposed to hypoxic conditions, adaptive molecular mechanisms are rapidly activated in order to limit the damage and to protect the viability and function of the brain cells. In this brief report, we focus on the possible role(s) played by astroglial cells in maintaining brain function under conditions when oxygen supply is compromised.
2 Astrocytes and Neurovascular Coupling
Astrocytes are the most abundant type of brai n glial cells. Their functions are versatile and have attracted considerable interest over the last few years. The traditional view of the functional role played by astroglial cells was limited to providing neurons with structural and nutritional support. Indeed, they enwrap all penetrating and intracerebral arterioles and capillaries, control the traffic of nutrients and other chemicals from and into the blood stream, and regulate the ionic and metabolic environment of the neuropil. Astrocytic processes surround neuronal bodies and make contacts with thousands of individual synapses and thus can “sense” the level of neuronal activity by responding to neurotransmitter spillover from the synaptic clefts [4, 14]. On the other hand, pial arteries rest on the underlying glia limitans, while all the penetrating arterioles are surrounded by astrocytic end-feet. Therefore, astrocytes can affect the activity of vascular smooth muscle cells [23].
There is significant evidence supporting the idea that brain astrocytes provide a neurovascular coupling interface. Several in vitro studies have demonstrated that astrocytic activation by Ca2+ uncaging changes the diameter of associated arterioles [2, 10, 21]. Multiple mechanisms underlying astrocyte-mediated neurovascular coupling have been proposed. One of these putative mechanisms is believed to be via release of potassium ions from astrocytic endfeet onto the arterioles in response to neuronal activity [8, 24]. Increases in extracellular K+ concentration could hyperpolarize smooth muscle cells resulting in dilation of cerebral vasculature [18]. Another mechanism whereby astrocytes control the local blood flow in brain areas involves the products of arachidonic acid (AA) metabolism. Increased synaptic activity is detected by astrocytes when glutamate is released by presynaptic nerve terminals. Glutamate activates astrocytic metabotropic glutamate receptors, leading to increases in [Ca2+]i and activation of phospholipase A2, which generates AA from membrane phospholipids. AA is then converted to prostaglandins (PGEs) and epoxyeicosatrienoic acids (EETs). Astroglial release of both, PGEs and EETs has vasodilator effects [10, 21, 36] whilst another AA product 20-hydroxy-eicosatetraenoic acid (20-HETE) produced in vascular smooth muscle cells promotes vasoconstriction [21, 22]. The main prostaglandin involved in neurovascular coupling is believed to be PGE2 whose vasodilator effect involves decreased phosphorylation of the myosin light chain and the activation of the K+ channels in arteriole vascular smooth muscle cells [29, 32].
In vitro slice studies have shown that activation of astrocytes can produce either dilation or constriction of brain arterioles. The precise contribution of glial control over the cerebral vasculature appears to depend on the pre-existing tone of the vessel [2] and most importantly, on tissue O2 concentration [10]. Activation of perivascular astrocytes through stimulation of metabotropic glutamate receptors or via Ca2+ uncaging produces arteriolar constriction when the preparation is exposed to hyperoxic conditions. However, activation of astrocytes under lower O2 conditions leads to vasodilation [10]. This suggests that tissue PO2 level is one of the main factors that determines the cerebrovascular responses to astroglial activation. These differential effects appear to be produced by changes in the synthesis of astrocytic messengers involved in neurovascular coupling. When PO2 is high, low levels of extracellular lactate facilitate clearance of PGE2 (in exchange for intracellular lactate) by prostaglandin transporters. In conditions of low extracellular PGE2 levels, vasoconstrictor effects of 20-HETE produced by vascular smooth muscle cells dominate [22]. In contrast, low PO2 promotes astrocytic glycolysis resulting in increased lactate release. Increased level of extracellular lactate reduces the activity of prostaglandin transporters leading to accumulation of extracellular PGE2, which dilates cerebral arterioles [10]. In additi on, cellular hypoxia triggers release of adenosine , which binds to adenosine A2A receptors on vascular smooth muscle cells to promote vasodilation [11].
3 Astrocytes as Hypo xia Sensors
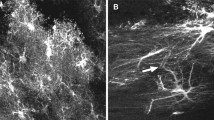
Recent studies from our laboratory have shown that astrocytes show robust increases in [Ca2+]i when PO2 is reduced below ~17 mmHg. Our previous studies in anesthetized, artificially ventilated and peripherally chemodenervated rats demonstrated that systemic hypoxia (10 % O2 in the inspired air; 5 min) elicits release of ATP (a key gliotransmitter) in the brainstem areas responsible for generation and patterning of the respiratory rhythm. Blockade of ATP receptors in the same brainstem areas facilitates hypoxia-evoked respiratory depression [13]. Further experiments in slice preparations confirmed that ATP release in response to hypoxia occurs within the anatomical regions corresponding to the location of the medullary respiratory networks and immediately ventral to it [13]. These data suggest that ATP is released within (and in close proximity to) the respiratory network and plays an important role in maintaining breathing in conditions when hypoxia-induced slowing of respiration occurs. Astrocytes are likely to be the source of ATP released in the brainstem during hypoxia and the mechanism(s) of ATP release include vesicular exocytosis. Interestingly, in our earlier study we showed that ventral brainstem astrocytes also respond to increases in the inspired levels of CO2 in vivo as well acidification of the extracellular medium in vitro with elevations in intracellular Ca2+ leading to exocytotic release of ATP [12]. ATP propagates astrocytic Ca2+ excitation within the astroglial network and activates local chemoreceptor neurons resulting in adaptive increases in breathing. These data obtained in various brainstem preparations demonstrate that astrocytes are capable of sensing both decreases in PO2 and increases in PCO2 and respond to these chemosensory challenges with increases in intracellular [Ca2+]. These results suggest that ATP released as a result of chemosensory activation contributes to the development of the ventilatory response to CO2 and helps to maintain breathing in face of the hypoxia-evoked depression of the respiratory network.
4 Astrocytes and Inflammation
Glial cells are capable of releasi ng chemokines while hypoxia is associated with upregulation of a number of inflammatory mediators, including interleukin (IL)-1β (IL-1β), IL-8, monocyte chemoattractant protein, intercellular adhesion molecule-1 (ICAM-1) and others [31, 34]. In human fetal astrocytes, hypoxia has been shown to evoke a marked upregulation of NF-kappaB—a crucial transcription factor necessary for synthesis of many inflammatory mediators [31]. There is evidence that NF-kappaB upregulates the expression of astrocytic IL-1β and IL-8 in response to hypoxia followed by amplification through autocrine IL-1β-induced NF-kappaB activation during reoxygenation [31]. It is not yet clear whether glial-derived cytokines have a protective or harmful effect on neurons exposed to hypoxic conditions, although the inflammatory process may contribute to brain repair following a hypoxic event. Removal of the damaged cells may be facilitated by macrophage infiltration, whilst neurogenesis may be promoted in response to increased cytokine production [7, 27, 35].
5 Astrocytes and Blood–Brain Barrier During Hypoxia
The blood–brain barrier (BBB) separates the circulating blood and the brain parenchyma. The BBB is composed of endothelial cells and astrocytic end-feet. Tight junctions between adjacent cells and sparse pinocytic vesicular transport are the landmarks of cerebral endothelium which under normal physiological conditions limit the permeability of microorganisms, T lymphocytes and hydrophilic molecules from the arterial blood into the brain. Efficacy of this barrier also relies on astrocytic end-feet which cumulatively circumscribe all cerebral blood vessels.
During hypoxia the BBB may become disrupted, leading to vasogenic edema [15, 19]. Astrocytes m ay increase BBB permeability through the release of a range of cytokines and chemical mediators [31, 34]. Glial-derived chemokines can upregulate the synthesis of the other factors such as IL-8, ICAM-1, E-selectin, IL-1β, TNF-α, and MCP-1 by the cerebrovascular endothelial cells [33], facilitating infiltration of leukocytes across the BBB. This triggers further signal transduction cascades leading to increased phosphotyrosine production, loss of tight junction proteins (occludin and zonula occludens-1), and redistribution of vinculin [3]. These events result in junctional disorganization and increased BBB permeability.
There is also evidence that astrocytes can protect the integrity of the BBB during hypoxia. It was demonstrated using an in vitro model that hypoxia-induced paracellular hyperpermeability is significantly decreased if astrocytes or astrocytic-conditioned medium are present [9]. These effects are associated with inhibition of hypoxia-induced vascular endothelial growth factor synthesis which enhances transcytosis in endothelial cells [6] and induces endothelium fenestrations [26].
6 Astrocytes and Neuroprotection During Hypoxia
In the last dec ade it has also become clear that astrocytes are capable of protecting neurons under conditions of hypoxia. One of the possible mechanisms is related to the phenomenon called “hypoxic preconditioning” where an initial brief period of mild hypoxia confers neuroprotection to subsequent, normally lethal to neurons, ischemic events. Mild hypoxia stimulates the production of various protective astrocytic factors that enhance neuronal viability [16]. Hypoxia upregulates the expression of certain proteins that may mediate egress of ATP/adenosine into the extracellular compartment like connexin 43 [17]. In response to hypoxia [20] astrocytes have been found to produce another factor with potent neuroprotective effect—erythropoietin [25]. Erythropoietin expression in astrocytes is upregulated following activation of hypoxia inducible factors—HIF-1α and HIF-2α [5, 28].
7 Summary
Astrocytes appear to play an important role in maintaining neurophysiological function under conditions when oxygen supply to the brain is compromised. At the system level, release of ATP by the brainstem astrocytes helps to maintain breathing and counteract hypoxia-induced depression of the respiratory network. At the tissue level, astrocytes appear to be involved in mediating hypoxia-evoked changes in BBB permeability, brain inflammation and neuroprotection against ischaemic injury. Under normal physiological conditions astrocytes mediate neurovascular coupling and have the ability to “sense” increased neuronal activity to trigger dilation of local microvasculature and divert oxygenated blood to brain areas with increased activity.
References
Alves PM, Fonseca LL, Peixoto CC, Almeida AC, Carrondo MJ, Santos H. NMR studies on energy metabolism of immobilized primary neurons and astrocytes during hypoxia, ischemia and hypoglycemia. NMR Biomed. 2000;13:438–48.
Blanco VM, Stern JE, Filosa JA. Tone-dependent vascular responses to astrocyte-derived signals. Am J Physiol Heart Circ Physiol. 2008;294:H2855–63.
Bolton SJ, Anthony DC, Perry VH. Loss of the tight junction proteins occludin and zonula occludens-1 from cerebral vascular endothelium during neutrophil-induced blood–brain barrier breakdown in vivo. Neuroscience. 1998;86:1245–57.
Bushong EA, Martone ME, Jones YZ, Ellisman MH. Protoplasmic astrocytes in CA1 stratum radiatum occupy separate anatomical domains. J Neurosci. 2002;22:183–92.
Chavez JC, Baranova O, Lin J, Pichiule P. The transcriptional activator hypoxia inducible factor 2 (HIF-2/EPAS-1) regulates the oxygen-dependent expression of erythropoietin in cortical astrocytes. J Neurosci. 2006;26:9471–81.
Collins PD, Connolly DT, Williams TJ. Characterization of the increase in vascular permeability induced by vascular permeability factor in vivo. Br J Pharmacol. 1993;109:195–9.
Feuerstein GZ, Wang X, Barone FC. The role of cytokines in the neuropathology of stroke and neurotrauma. Neuroimmunomodulation. 1998;5:143–59.
Filosa JA, Bonev AD, Straub SV, Meredith AL, Wilkerson MK, Aldrich RW, Nelson MT. Local potassium signaling couples neuronal activity to vasodilation in the brain. Nat Neurosci. 2006;9:1397–403.
Fischer S, Wobben M, Marti HH, Renz D, Schaper W. Hypoxia-induced hyperpermeability in brain microvessel endothelial cells involves VEGF-mediated changes in the expression of zonula occludens-1. Microvasc Res. 2002;63:70–80.
Gordon GR, Choi HB, Rungta RL, Ellis-Davies GC, Macvicar BA. Brain metabolism dictates the polarity of astrocyte control over arterioles. Nature. 2008;456:745–9.
Gordon GR, Mulligan SJ, Macvicar BA. Astrocyte control of the cerebrovasculature. Glia. 2007;55:1214–21.
Gourine AV, Kasymov V, Marina N, Tang F, Figueiredo MF, Lane S, Teschemacher AG, Spyer KM, Deisseroth K, Kasparov S. Astrocytes control breathing through pH-dependent release of ATP. Science. 2010;329:571–5.
Gourine AV, Llaudet E, Dale N, Spyer KM. Release of ATP in the ventral medulla during hypoxia in rats: role in hypoxic ventilatory response. J Neurosci. 2005;25:1211–8.
Halassa MM, Fellin T, Takano H, Dong JH, Haydon PG. Synaptic islands defined by the territory of a single astrocyte. J Neurosci. 2007;27:6473–7.
Hayashi K, Nakao S, Nakaoke R, Nakagawa S, Kitagawa N, Niwa M. Effects of hypoxia on endothelial/pericytic co-culture model of the blood–brain barrier. Regul Pept. 2004;123:77–83.
Heurteaux C, Lauritzen I, Widmann C, Lazdunski M. Essential role of adenosine, adenosine A1 receptors, and ATP-sensitive K+ channels in cerebral ischemic preconditioning. Proc Natl Acad Sci U S A. 1995;92:4666–70.
Kang J, Kang N, Lovatt D, Torres A, Zhao Z, Lin J, Nedergaard M. Connexin 43 hemichannels are permeable to ATP. J Neurosci. 2008;28:4702–11.
Knot HJ, Zimmermann PA, Nelson MT. Extracellular K(+)-induced hyperpolarizations and dilatations of rat coronary and cerebral arteries involve inward rectifier K(+) channels. J Physiol. 1996;492:419–30.
Mark KS, Davis TP. Cerebral microvascular changes in permeability and tight junctions induced by hypoxia-reoxygenation. Am J Physiol Heart Circ Physiol. 2002;282:H1485–94.
Masuda S, Okano M, Yamagishi K, Nagao M, Ueda M, Sasaki R. A novel site of erythropoietin production. Oxygen-dependent production in cultured rat astrocytes. J Biol Chem. 1994;269:19488–93.
Metea MR, Newman EA. Glial cells dilate and constrict blood vessels: a mechanism of neurovascular coupling. J Neurosci. 2006;26:2862–70.
Mulligan SJ, Macvicar BA. Calcium transients in astrocyte endfeet cause cerebrovascular constrictions. Nature. 2004;431:195–9.
Nedergaard M, Ransom B, Goldman SA. New roles for astrocytes: redefining the functional architecture of the brain. Trends Neurosci. 2003;26:523–30.
Paulson OB, Newman EA. Does the release of potassium from astrocyte endfeet regulate cerebral blood flow? Science. 1987;237:896–8.
Prass K, Scharff A, Ruscher K, Lowl D, Muselmann C, Victorov I, Kapinya K, Dirnagl U, Meisel A. Hypoxia-induced stroke tolerance in the mouse is mediated by erythropoietin. Stroke. 2003;34:1981–6.
Roberts WG, Palade GE. Increased microvascular permeability and endothelial fenestration induced by vascular endothelial growth factor. J Cell Sci. 1995;108:2369–79.
Sakurai-Yamashita Y, Shigematsu K, Yamashita K, Niwa M. Expression of MCP-1 in the hippocampus of SHRSP with ischemia-related delayed neuronal death. Cell Mol Neurobiol. 2006;26:823–31.
Semenza GL, Agani F, Booth G, Forsythe J, Iyer N, Jiang BH, Leung S, Roe R, Wiener C, Yu A. Structural and functional analysis of hypoxia-inducible factor 1. Kidney Int. 1997;51:553–5.
Serebryakov V, Zakharenko S, Snetkov V, Takeda K. Effects of prostaglandins E1 and E2 on cultured smooth muscle cells and strips of rat aorta. Prostaglandins. 1994;47:353–65.
Silver IA, Deas J, Erecinska M. Ion homeostasis in brain cells: differences in intracellular ion responses to energy limitation between cultured neurons and glial cells. Neuroscience. 1997;78:589–601.
Stanimirovic D, Zhang W, Howlett C, Lemieux P, Smith C. Inflammatory gene transcription in human astrocytes exposed to hypoxia: roles of the nuclear factor-kappaB and autocrine stimulation. J Neuroimmunol. 2001;119:365–76.
Takata F, Dohgu S, Nishioku T, Takahashi H, Harada E, Makino I, Nakashima M, Yamauchi A, Kataoka Y. Adrenomedullin-induced relaxation of rat brain pericytes is related to the reduced phosphorylation of myosin light chain through the cAMP/PKA signaling pathway. Neurosci Lett. 2009;449:71–5.
Zhang W, Smith C, Howlett C, Stanimirovic D. Inflammatory activation of human brain endothelial cells by hypoxic astrocytes in vitro is mediated by IL-1beta. J Cereb Blood Flow Metab. 2000;20:967–78.
Zhang W, Smith C, Shapiro A, Monette R, Hutchison J, Stanimirovic D. Increased expression of bioactive chemokines in human cerebromicrovascular endothelial cells and astrocytes subjected to simulated ischemia in vitro. J Neuroimmunol. 1999;101:148–60.
Zhang W, Stanimirovic D. Current and future therapeutic strategies to target inflammation in stroke. Curr Drug Targets Inflamm Allergy. 2002;1:151–66.
Zonta M, Angulo MC, Gobbo S, Rosengarten B, Hossmann KA, Pozzan T, Carmignoto G. Neuron-to-astrocyte signaling is central to the dynamic control of brain microcirculation. Nat Neurosci. 2003;6:43–50.
Acknowledgments
The research in our laboratories referred to in this report was funded by The Wellcome Trust and British Heart Foundation. A.V.G. is a Wellcome Trust Senior Research Fellow (ref. 079040); G.L.A. is an Academy of Medical Sciences/Health Foundation Clinician Scientist.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer Science+Business Media New York
About this chapter
Cite this chapter
Marina, N., Kasymov, V., Ackland, G.L., Kasparov, S., Gourine, A.V. (2016). Astrocytes and Brain Hypoxia. In: Roach, R., Hackett, P., Wagner, P. (eds) Hypoxia. Advances in Experimental Medicine and Biology, vol 903. Springer, Boston, MA. https://doi.org/10.1007/978-1-4899-7678-9_14
Download citation
DOI: https://doi.org/10.1007/978-1-4899-7678-9_14
Published:
Publisher Name: Springer, Boston, MA
Print ISBN: 978-1-4899-7676-5
Online ISBN: 978-1-4899-7678-9
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)