Abstract
Rubella virus typically causes only a mild febrile illness with a rash. In childhood the infection is usually trivial, but in a pregnant woman infected during the first trimester serious sequelae may include miscarriage, fetal death or a range of birth defects known as congenital rubella syndrome (CRS). Beginning in 1969 the introduction of rubella virus vaccines to prevent infection steadily reduced the incidence of CRS and has all but eliminated it in countries where vaccine is in wide use. Of lower priority in the developing world, rubella vaccine was not adopted more widely until the 1990s when CRS was still occurring in infants at an estimated incidence of more than 100,000 annually. The World Health Organization (WHO) issued a position paper on rubella vaccine in 2000 to guide countries toward effective incorporation of vaccine into their schedules for childhood immunization. In 2009 WHO highlighted the need for both routine and supplemental immunization activities in order to reach the target ≥80% coverage in childhood as a key step toward global elimination of CRS. It was also recognized that this ambitious goal needed to be coupled with a focus on immunizing women of childbearing age. More recently, key national and international organizations have embraced a Measles and Rubella Initiative representing an even more coordinated partnership aimed at significant reduction of CRS worldwide and elimination in multiple WHO regions by 2020.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Introduction
Rubella (German measles) is usually a mild febrile viral rash illness in children and adults. However, infection early in pregnancy, particularly during the first 16 weeks, can result in miscarriage, stillbirth, or an infant born with birth defects known as congenital rubella syndrome.
2 Historical Background
German physicians, in the mid-eighteenth century, were the first researchers to distinguish the rubella disease from other exanthems. Even though they named it Rotheln, rubella is recognized today by its common English language eponym German measles [1]. In 1841, a British physician reported an outbreak in a boys’ school in India and coined the term rubella, a Latin diminutive meaning “little red” [2]. Even though, in the late nineteenth century, rubella was considered different from measles or scarlet fever [3], not until 1941 the significance of rubella was noted. In 1941, Norman McAlister Gregg, an Australian ophthalmologist, linked congenital cataracts to maternal rubella. In his practice, Gregg had noticed an unusual number of infants with cataracts [4]. It is noted that a crucial clue was a conversation he overheard in his waiting room between 2 mothers who were discussing the rubella they both had sustained in pregnancy during the Australian outbreak of 1940 [5]. Gregg’s original observation was followed by reports of Australian [6], Swedish [7], American [8], and British [9] epidemiologists and teratologists confirming his observations and also noting infants presented with heart disease and deafness. Thus, the characteristic congenital rubella triad was established.
After Gregg’s discovery, it was 20 years before the isolation of the causative agent, rubella virus. During this time, various estimates of the risk of fetal disease after maternal rubella were made. However, the wide range of estimates stemmed from the absence of a definitive diagnostic test and consequent misdiagnosis of rubella in the mother. In late 1962, the rubella virus was isolated by two different groups: Weller and Neva [10] in Boston and by Parkman, Beuscher, and Artenstein [11] in Washington, DC.
In 1962–1965 a worldwide rubella epidemic started in Europe and spread to the United States. In the United States an estimated 12.5 million cases of rubella occurred in the United States, resulting in 2,000 cases of encephalitis, 11,250 fetal deaths, 2,100 neonatal deaths, and 20,000 infants born with CRS, a constellation of birth defects that often includes blindness, deafness, and congenital heart defects. The economic impact of this epidemic in the United States was estimated at $1.5 billion [12, 13]. The pandemic led to the recognition of an expanded congenital rubella syndrome (CRS), which added hepatitis, splenomegaly, thrombocytopenia, encephalitis, mental retardation, and numerous other anomalies to the already described deafness, cataracts, and heart disease [14, 15]. The pandemic also made it obvious that a vaccine was needed, and many groups set to work.
The global epidemic spurred development of rubella vaccines and emphasized the need to develop and implement strategies for using these vaccines to prevent this devastating health burden [3]. Between 1965 and 1967, several attenuated rubella strains were developed and reached clinical trials [16–18]. In 1969 and 1970, rubella vaccine was introduced in Europe and North America. Since the late 1970s, vaccination has had a major impact on the epidemiology of rubella and CRS resulting in the interruption of endemic rubella virus transmission in 2001 [19].
3 Methodology
3.1 Mortality Data
Deaths associated with rubella are rare enough that they have no impact on the epidemiology of the rubella.
3.2 Morbidity Data
In the United States, rubella and CRS became nationally reportable to the National Notifiable Disease Surveillance System (NNDSS) in 1966. In 1969, Centers for Disease Control and Prevention established the National Congenital Rubella Syndrome Registry (NCRSR). The reporting efficiency for clinical cases is estimated to be only 10–20 %. As part of the process for documenting the elimination of rubella and CRS in 2004, the adequacy of surveillance was evaluated by reviewing five different sources. The conclusion was that the surveillance system was adequate and was able to support the elimination of endemic rubella transmission [20].
3.3 Serological Surveys
Serological surveys of healthy population groups have been of major importance for understanding the pre-vaccine rubella epidemiology including age specific to identify the target age groups and strategy for vaccine introduction [21]. In addition, serosurveys are used to monitor the impact of the vaccination program, provide evidence for modifying the vaccination strategy, and support the documentation of elimination of rubella/CRS [22].
Prior to the licensure and introduction of the rubella vaccine, the World Health Organization sponsored collaborative serosurveys in 1967–1968 assessing the rubella seropositivity in five continents; however, most of the studies were conducted in the Americas and Europe. In 12 of the 25 studies conducted, the seropositivity rate was 80 % or greater among women aged 17–22 years of age [23]. In the United States, serological surveys conducted in the pre-vaccine era showed seropositivity ranging between 80 and 92 %.
In some regions and countries, post-vaccination serosurveys are used to monitor the vaccination program. However, interpretation of serological studies can be complicated due to variations in the sensitivity of the assays. In the European Region, European Sero-epidemiology Network, the aim is to standardize the serological survey of eight vaccine preventable diseases in 22 countries [24]. By standardizing the methodology, international comparisons can be made to allow to evaluate the effectiveness of different immunization programs and to coordinate vaccine policy to ensure that adequate levels of immunity exist throughout Europe.
In the United States, the most recent use of post-vaccination serosurveys was to support the documentation of elimination of rubella and CRS [25]. Two nationwide seroprevalence studies were conducted through the population-based National Health and Nutrition Examination Survey. Sera were tested for rubella immunoglobulin G antibodies during 1988–1994 and 1999–2004. From the earlier to the later period, the overall age-adjusted rubella seroprevalence in the US population 6–49 years of age rose from 88.1 to 91.3 % was statistically a significant increase. Additional analyses showed that seroprevalence either remained at the same level or higher for the groups (i.e., children of both sexes, women of childbearing age) that were targeted for vaccination.
3.4 Laboratory Methods
3.4.1 Virus Isolation/Detection
In persons with acquired rubella, the rubella virus can be isolated from the blood and nasopharynx during the prodromal period and from the nasopharynx for as long as 2 weeks after eruption. However, the likelihood of virus recovery is sharply reduced by 4 days after the rash. Rubella virus can be isolated using several different cell lines: Vero cell line, primary African green monkey kidney cells, or the RK13 cell line. Through the World Health Organization Global Laboratory Network, laboratories are trained to use either Vero/SLAM cells or Vero cells to isolate rubella virus [26, 27]. The method for detection of the rubella E1 glycoprotein is by using monoclonal antibodies in either an immunofluorescent or an immunocolorimetric assay.
Another recently developed method for virus detection is the polymerase chain reaction (PCR). The most important roles of RT-PCR in rubella control are to characterize the virus genetically and to detect inactivated virus. RT-PCR can be used to detect virus before the IgM is positive and used to detect inactivated particles when the person is shedding only small amounts of virus. The polymerase chain reaction (PCR) has been adapted to the detection of rubella RNA by reverse transcription and amplification.
3.4.2 Antibody Tests
3.4.2.1 Sera
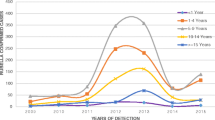
After the isolation of the rubella, laboratory confirmation of rubella infection was available. Over the last 40 years, several different testing methodologies were developed (Fig. 31.1). These include the following: neutralization assays (NT), hemagglutination-inhibition (HI) assays, enzyme immunoassay (EIA), single radial hemolysis (SRH), and latex agglutination. NT assays were the first to be developed [28], but they are seldom used today, as they are demanding and require use of cell cultures. HI assays were developed in 1967 [29] and results were shown to correlate well with NT. However, HI is also labor intensive. HI is no longer recommended for routine testing; however, the HI is used as a reference method to establish a calibration standard for other rubella assays. Other more recent assays developed included enzyme immunoassay (EIA), single radial hemolysis (SRH), and latex agglutination, which have been used extensively for rubella antibody screening [30].
Nowadays, EIA is the most frequently used test for rubella antibody screening and diagnosis, as it is a sensitive and an adaptable technique and is readily automated. EIA can also be adapted to detect class-specific antibodies (e.g., IgM, IgG1, IgG3, IgA) and is the method of choice for detection of rubella-specific IgM [31–33]. Indirect and M-antibody capture EIAs are available commercially for detection of rubella IgM. Another adaptation of EIAs is the IgG1 avidity assay. The avidity assays are useful for diagnostic purposes, particularly to distinguish primary rubella from rubella reinfection and to identify persistent IgM responses and nonspecific IgM [34]. The most common diagnostic method employs a denaturating agent (6–8 M urea or DEA) to elute low avidity antibody from antigen-antibody complexes in an EIA (reviewed by Thomas et al. [34]; Best and Enders [30]). Depending upon the strength of this binding, the complex formed may or may not be easily dissociated. Antibody avidity is low after primary antigenic challenge, becomes higher with time, and usually involves IgG antibodies [51, 52]. However, IgG avidity assays can be difficult to establish, standardize, quality control, and interpret; they are therefore recommended only for laboratories experienced in using these assays [35].
3.4.2.2 Oral Fluids
Since the early 1990s, the use of oral fluid sampling has been used successfully for the detection of rubella antibodies as part of the surveillance system in the United Kingdom [35] Oral fluid sampling can also be used for detecting RNA. In a recent study, the use of oral fluids for detection of RNA was superior to testing of sera or oral fluid for rubella IgM within the first few days after rash onset [36]. Oral fluid samples are easy to collect, noninvasive, and more acceptable to the population. Its use enables field workers to obtain more complete sampling of suspected cases.
4 Biological Characteristics of the Vaccine
Rubella virus is a member of the Togaviridae family and the genus Rubivirus. Rubella virus is a single-stranded enveloped RNA with a single antigenic type. It measures 50–70 nm in diameter and has two envelope proteins (E1,E2) and a core protein (c). The core protein is surrounded by a single-layer lipoprotein enveloped with spike-like projections that contain the two glycoproteins, E1 and E2. Humans are the only known reservoir.
The rubella virus is relatively temperature labile but is more heat stable than measles virus; it is inactivated after 30 min at 56 °C, 4 min at 70 °C, and 2 min at 100 °C. It degrades rapidly with conventional freezing at −20°, but the virus is stable at −60 °C and below and when freeze-dried with stabilizers. When stabilized with protein it can be repeatedly frozen and thawed without loss of titer. Lipid solvents, weak acids and alkalis, and UV light inactivate the rubella virus. It is also susceptible to a wide range of disinfectants and is inactivated by 1 % sodium hypochlorite, 70 % ethanol, and formaldehyde [37].
Over the last 15–20 years, the study of molecular epidemiology has evolved. In 2005, a systematic nomenclature was adopted by the WHO [38, 39]. The genetic characterization of rubella virus has identified two clades that differ by 8–10 % at the nucleotide level. Clade 1 is divided into 10 genotypes (1a, 1B, 1C, 1D, 1E, 1 F, 1G, 1 h, 1i, and 1j), of which 6 are recognized and 4 are provisional (designated by lowercase letters). Clade 2 contains 3 genotypes (2A, 2B, and 2C) [40]. For rubella isolates collected before 2000, isolates from North America, Europe, and Japan are closely related to each other and form clade I, whereas clade II comprises some strains from China, Korea, and India [41]. However, in China between 2001 and 2007, there was a shift of genotypes toward predominance of IE and 1F [42]. Of rubella isolates collected between 2005 and 2010, three genotypes (1E, 1G, 2B) had wide geographic distribution whereas others occurred sporadically or were geographically restricted [40].
The genetic differences between clades do not appear to translate into antigenic differences, despite amino acid changes of 3–6 % in viral proteins. Isolates from CRS cases are not genetically distinct from isolates from acquired rubella.
5 Descriptive Epidemiology
5.1 Incidence and Prevalence
Our understanding of pre-vaccine era epidemiology of rubella in the United States is from surveillance conducted from 1928 to 1983 in 10 selected areas in the United States. During the 1962–1965 the United States experienced an epidemic with an estimated 12.5 million cases of rubella, resulting in 2,000 cases of encephalitis, 11,250 fetal deaths, 2,100 neonatal deaths, and 20,000 infants born with CRS, a constellation of birth defects that often includes blindness, deafness, and congenital heart defects.
In 1969, live-attenuated rubella vaccines were first licensed in the United States [43], and a vaccination program was established with the goal of preventing congenital infections, including CRS. Before the introduction of vaccine, rubella incidence was highest among children aged <9 years [44]. The new rubella vaccination program targeted a dose of vaccine to children aged 1 year to puberty [45]. To increase coverage among school-aged children rapidly, mass campaigns were conducted, particularly in schools. By 1977, reported vaccination levels were approximately 60 % for children aged 1–4 years, 71 % for those aged 5–9 years, and 64 % for those aged 10–14 years [46]. The number of reported rubella cases declined 78 %, from 57,686 cases in 1969 to 12,491 cases in 1976. As anticipated, the greatest decreases in rubella occurred among persons aged <15 years; however, incidence declined in all age groups, including adults. This decrease in rubella also resulted in a decline in the number of reported CRS cases, from 68 cases reported in 1970 to 23 reported in 1976 [47]. The total number of rubella cases continued to decline overall during the late 1970s; however, in subsequent years a resurgence of rubella occurred among older adolescents and young adults, with outbreaks occurring among students in high schools, colleges, and universities and among persons on military bases and workers in hospitals. Rubella incidence was highest among young adults [48]. In addition, the number of reported CRS cases increased, from 23 in 1976 to 57 in 1979; however, the annual number of CRS cases never reached the level reported during the 1960s in the pre-vaccine era. Serologic studies at that time suggested that 10–20 % of adults remained susceptible to rubella [49].
The resurgence of rubella and its increased incidence among young adults focused attention on the need for additional strategies. In 1978, the changing epidemiology of rubella prompted the Advisory Committee on Immunization Practices (ACIP) to additionally recommend that rubella vaccine be targeted to susceptible postpubertal females, in addition to adolescents, persons in military service, college students, and persons in certain work settings (e.g., hospitals) [50]. Efforts to increase overall childhood vaccination coverage to greater than 90 % for all vaccine-preventable diseases, including rubella, had begun in 1977, with the first National Childhood Immunization Initiative [51]. In 1978, a program was undertaken to eliminate indigenous measles in the United States; the use of combined vaccines, either measles-rubella (MR) vaccine or measles-mumps-rubella (MMR) vaccine, was encouraged. These efforts to increase immunity among selected adults and children resulted in substantial decreases in the numbers of both rubella and CRS cases. During 1977–1981, reported rubella cases declined from 20,395 to 2,077. During 1979–1981, reported CRS cases decreased from 57 to 10 [52]. For the 1981–1982 school year, rubella vaccination coverage was 96 % for children entering school (i.e., into kindergarten or first grade) in the 50 states and the District of Columbia [53]. Efforts to maintain high coverage through enforcement of school immunization laws produced a continuing decrease in reported rubella cases.
In 1979, a new formulation of live-attenuated rubella vaccine (RA 27/3) replaced the previous rubella vaccines in the United States. RA 27/3 vaccine had been determined to induce higher antibody titers and produce an immune response more closely paralleling natural infection than previous vaccines [54].
By 1979, rubella vaccination had eliminated the characteristic 6–9-year epidemic cycle of rubella in the United States [52]. In 1980, national health objectives for 1990 were established for rubella and CRS, calling for reductions in the annual number of rubella cases to fewer than 1,000 and CRS cases to fewer than 10 [55]. During the 1980s, the number of reported rubella cases continued to decline steadily, and overall incidence continued to decrease in all age groups. By 1983, the 1990 objectives already had been achieved, with 970 rubella cases and four CRS cases reported. During the early 1980s, outbreaks continued to be reported in health-care settings, universities, workplaces, and prisons. In 1981, ACIP recommendations increased emphasis on targeting these settings to ensure vaccination coverage among students and staff members [56].
In 1988, state health departments reported an all-time low of 225 cases of rubella; however, in 1989, a total of 396 cases were reported, and in 1990, the number increased to 1,125 [57]. Most cases were associated with outbreaks that occurred in settings where unvaccinated adults congregated, including colleges, workplaces, prisons, and in religious communities that did not accept vaccination. Outbreaks among these populations accounted for 56 % of CRS cases in the 1990s. In 1989, a goal was established to eliminate indigenous rubella transmission and CRS in the United States by 2000 [58]. With establishment of the 1993 Childhood Immunization Initiative, the number of annual rubella cases continued to decline in the mid-1990s. Outbreaks continued to be associated with settings where adults had close contact; however, the demographic characteristics of rubella patients changed. Before 1995, most persons with rubella were non-Hispanic; beginning in 1995, most were Hispanic [59]. Beginning in 1998, data on country of origin were collected for rubella patients. These data revealed that, during 1998 and 1999, approximately 79 and 65 % of patients whose country of origin was known were foreign born. Of these, 91 % in 1998 and 98 % in 1999 were born in the Western Hemisphere, and 43 % in 1998 and 81 % in 1999 were born in Mexico. These persons were either unvaccinated or their vaccination status was unknown. During 1998–2000, a total of 23 CRS cases were reported to CDC. The infants in 22 (96 %) of these cases were born to Hispanic women, and 22 of the mothers with known country of birth were born outside the United States. The countries of origin of these mothers were Mexico (14 mothers), Dominican Republic (four), Honduras (two), Colombia (one), and Philippines (one). Since 2001, the annual numbers of rubella cases have been the lowest ever recorded in the United States: 23 in 2001, 18 in 2002, seven in 2003, and nine in 2004. Approximately half of these cases have occurred among persons born outside the United States, of whom most were born outside the Western Hemisphere. During 2001–2004, four CRS cases were reported to CDC; the mothers of three of the children were born outside the United States. In 2004, the panel convened by CDC concluded that sustained transmission of rubella has been interrupted. Since 2004, the United States has maintained elimination of rubella and CRS. From 2005 to 2011, a median of 11 rubella cases was reported each year in the United States (range: 4–18). In addition, two rubella outbreaks involving three cases, as well as four total CRS cases, were reported [60]. In 2012, as part of the documentation process for PAHO, the United States convened an independent external panel to evaluate if elimination of measles, rubella, and CRS had been maintained.
The incidence of CRS has been evaluated mainly in developed countries over the last 60 years. Initially in the United States, the incidence of CRS roughly paralleled the incidence of rubella in individuals over 15 years; however, with the interruption of endemic rubella virus transmission, CRS cases became very rare and occurred mainly among mothers who are foreign born [61].
In most developing countries, there is little documentation to illuminate the epidemiology of either rubella or CRS. The epidemic pattern for developing countries is similar to the developed countries with cycles 3–7 years. Globally, it is estimated that approximately 103,000 infants with CRS were born in 2010 with the greatest burden in regions where rubella vaccine uptake is limited. A review of worldwide data concerning CRS revealed rates in developing countries varying between 0.6 and 2.2 per 1,000 live births, similar to rates seen in developed countries before universal vaccination [62, 63]. It has been estimated that the incidence of CRS is 0.1–0.2 per 1,000 live births during endemic periods and 1–4 per 1,000 live births during epidemic periods [64]. Where rubella virus is circulating and women of childbearing age are susceptible, CRS cases will continue to occur.
5.2 Epidemic Behavior
Rubella usually occurs in a seasonal pattern, with epidemics every 5–9 years. However, the extent and periodicity of rubella epidemics is highly variable in both industrialized and developing countries. From published literature, epidemics have been reported every 6–7 years in Hong Kong [65] and São Paulo, Brazil [66]; every 4–5 years in Panama [67]; and every 4–7 years in Argentina [68] and Bangkok, Thailand [69–71].
5.3 Geographic Distribution
Prior to the establishment of the rubella and CRS elimination goal in the Region of Americas, rubella had a worldwide distribution. However, in 2009, the last endemic rubella case in the Region of the Americas was documented in Argentina [72]. Rubella continues to circulate in the Eastern Hemisphere. In 2012–2013, rubella epidemics have been documented in several countries (i.e., Romania [73], Poland [74], Japan [75], Ethiopia) in three different continents.
5.4 Temporal Distribution
Prior to the elimination of endemic rubella virus in the United States, the largest number of rubella cases occurred in late winter and spring, in both high and low incidence. Because of the acceleration of measles control, the understanding of rubella seasonality can be documented in developing countries. Using the measles case-based surveillance in African region, rubella seasonality could be detected with variation of seasonality by subregion [76]. In the West subregion, during 2003–2009, marked seasonality of rubella occurred each year with sharp increases in reporting during January with peaks in March–April followed by sharp declines in May, leading to troughs during October– December each year. However, in the South subregion, a distinct annual seasonality was observed with consistently few cases reported during January–June each year, followed by gradual increases in June–July and peaks in September–October.
5.5 Age and Sex
In the pre-vaccine era in the United States, rubella was primarily a disease of school-aged children; however, rubella occurred also in preschool children. In many countries, this is the pattern for rubella infection. However, in other countries such as Caribbean islands and Southeast Asia, young adult females show high susceptibility, which can result in cases among pregnant women with subsequent CRS.
In the pre-vaccine era, there were no differences in attack rates by sex for children. In the post-vaccination era, in countries where adolescent girls were targeted for vaccination, outbreaks among adolescent and adult males have been documented [71]. However, in countries that have not targeted females only in vaccination, attack rates in males and females are similar.
6 Mechanisms and Routes of Transmission
Rubella virus is spread from person to person via respiratory droplets. Individuals with acquired rubella may shed virus from 7 days before rash onset to ~5–7 days thereafter. Both clinical and subclinical infections are considered contagious.
After primary implantation and replication, subsequent viremia occurs, which in pregnant women often results in infection of the placenta. Placental virus replication may lead to infection of fetal organs. Infants with CRS may shed large quantities of virus from bodily secretions, particularly from the throat and in the urine, up to 1 year of age. Outbreaks of rubella, including some in nosocomial settings, have originated with index cases of CRS. Thus only individuals immune to rubella should have contact with infants who have CRS or who are congenitally infected with rubella virus but are not showing signs of CRS.
7 Pathogenesis and Immunity
Although the pathogenesis of postnatal (acquired) rubella has been well documented, data on pathology are limited because of the mildness of the disease. Primary implantation and replication in the nasopharynx are followed by spread to the lymph nodes. This is followed by viremia and shedding of virus from the throat.
For acquired rubella, the rubella virus induces both circulating and cell-mediated immune (CMI) responses. HI and NT antibodies develop very rapidly and may be detectable, while the rash is still specific antibodies, rubella-specific IgM appears first and is closely followed by IgG1, IgG3, and IgA [31]. IgM is transient; it peaks on about day 7 and persists for 4–12 weeks after illness and occasionally for about a year [77].
The role of CMI in protection from rubella has not been determined. Rubella infection induces a fall in total leukocytes, T cells, and neutrophils, and a transient depression in lymphocyte responses to mitogens and antigens (e.g., purified protein derivative, PPD), but the mechanism responsible for the mild immunosuppression has not been elucidated. Studies of cytokine secretion demonstrate the strongest responses in persons with a recent history of rubella [78, 79]. Lymphoproliferative assays show that CMI responses develop a few days after onset of rash and persist at low levels for many years.
The pathology of CRS in the infected fetus is well defined, with almost all organs found to be infected; however, the pathogenesis of CRS is only poorly delineated. In tissue, infections with rubella virus have diverse effects, ranging from no obvious impact to cell destruction. The hallmark of fetal infection is chronicity, with persistence throughout fetal development in utero and for up to 1 year after birth.
The immune response to the intrauterine rubella infection starts while in pregnancy. However, the development of the fetal humoral immune system appears to be too late to limit the effects of the virus. Cells with membrane-bound immunoglobulins of all three major classes—IgM, IgG, and IgA—appear in the fetus as early as 9–11 weeks gestation [80]. However, circulating fetal antibody levels remain low until mid-gestation, despite the presence of high titers of virus. At this time, levels of fetal antibody increase, with IgM antibody predominating [81]. As in the case with other chronic intrauterine infections, congenital rubella infection may lead to an increase in total IgM antibody levels [82]. At the time of delivery of infected infants, levels of IgG rubella antibodies in cord sera are equal to or greater than those in maternal sera, even if the infant is born prematurely. IgG is the dominant antibody present at delivery in rubella-infected infants and is mainly maternal in origin. In contrast, the IgM levels are lower but are totally fetus derived.
8 Patterns of Host Response
In acquired rubella, the ratio of inapparent to apparent infections has been estimated to be from 1:1 to as high as 6:1 [83, 84]. Age probably influences the clinical expression of infection. Children usually develop few or no constitutional symptoms.
8.1 Clinical Manifestations
8.1.1 Acquired Infection
The average incubation period is 14 days with a range of 12–23 days. During the first week after exposure, there are no symptoms. During the second week after exposure, there may be a prodromal illness consisting of low-grade fever (<39.0 °C), malaise, mild coryza, and mild conjunctivitis, which is more common in adults. Postauricular, occipital, and posterior cervical lymphadenopathy is characteristic and typically precedes the rash by 5–10 days. Children usually develop few or no constitutional symptoms. Rarely, rubella may mimic measles in its severity of fever and constitutional symptoms, but Koplik’s spots are absent.
At the end of the incubation period, a maculopapular erythematous rash appears on the face and neck. The rubella rash occurs in 50–80 % of rubella-infected persons and is sometimes misclassified as measles or scarlet fever. The maculopapular erythematous rash of rubella starts on the face and neck and progresses down the body. The rash, which may be pruritic, usually lasts between 1 and 3 days. The rash is fainter than measles rash and does not coalesce, and it may be difficult to detect, particularly on pigmented skin.
Rubella disease is usually mild, resulting in very few complications apart from the serious consequences of congenital rubella infection. Transient joint symptoms (e.g., arthritis, arthralgias) may occur in up to 70 % of adult women with rubella. They usually begin within 1 week after rash onset and typically last for 3–10 days, although occasionally they may last for up to 1 month. Other complications include thrombocytopenic purpura (1 in 3,000 rubella cases) and encephalitis (1 in 6,000 rubella cases). In outbreaks in the Kingdom of Tonga (2002), the Independent State of Samoa (2003), and Tunisia [85], encephalitis was seen more commonly, with an estimated rate of 1 in 300 to 1 in 1,500 cases. Long-term sequelae with such progressive rubella panencephalitis (PRP) are rare. PRP has similarities to subacute sclerosing panencephalitis (SSPE) caused by measles.
8.1.2 Congenital Rubella Infection
The risk of congenital infection is related to the gestational age at the time of maternal infection. The outcome of a primary rubella infection during pregnancy includes the following: spontaneous abortion, stillbirth/fetal death, infant born with CRS, infant born with congenital rubella infection without congenital defects, and birth of a normal infant.
The most common defects of CRS are hearing impairment (unilateral or bilateral sensorineural), eye defects (e.g., cataracts, congenital glaucoma, or pigmentary retinopathy), and cardiac defects (e.g., patent ductus arteriosus or peripheral pulmonic stenosis). Other clinical manifestations may include microcephaly, developmental delay, purpura, meningoencephalitis, hepatosplenomegaly, low birth weight, and radiolucent bone disease (Table 31.1).
Children with CRS may develop late-onset manifestations including endocrine abnormalities (e.g., diabetes mellitus, thyroid dysfunction), visual abnormalities (e.g., glaucoma, keratitic precipitates), and neurological abnormalities (e.g., progressive panencephalitis), in addition to developmental manifestations which include autism [86].
When pregnant women are infected with rubella during the first 11 weeks of gestation, up to 90 % of live-born infants will have CRS; thereafter the rate of CRS declines until 17–18 weeks’ gestation when deafness is the rare and only consequence. Reinfection with rubella may occur, but if this occurs early in pregnancy, transmission to the fetus is rare, and the risk of congenital rubella defects is probably less than 5 %.
8.2 Serological Responses
Antibodies to rubella virus develop promptly and can sometimes be detected on the day of rash onset. The IgM and IgG classes rise rapidly; IgG persists, but IgM begins to wane (see Sect. 7). However, in a small percentage of persons, IgM persists for long period of time [30]. This persistence can be confused with acute infection. To help differentiate IgM associated with acute infection, testing for seroconversion of IgG or avidity testing is recommended.
9 Control
9.1 Vaccine Development
As noted earlier, the development of vaccines was spurred by the 1962–1965 epidemics in Europe and the United States. Shortly after the isolation of rubella virus, investigators attempted to develop an inactivated virus vaccine, but their attempts were unsuccessful. Either the vaccines were not antigenic or if antibodies were produced, it was questionable if the preparation was contaminated with live virus [87].
With the issues of the inactivated vaccine, several groups were interested in developing a live-attenuated vaccine in the 1960s. Parkman and colleagues were the first to successfully attenuate RV with 77 passages in African green monkey kidney cell cultures and to give the attenuated strain HPV77 [88]. Between 1969 and 1970, three vaccines were licensed in the United States, including HPV-77.DK12 (dog kidney), HPV-77.DE5 (duck embryo), and Cendehill (rabbit kidney) [46]. The Cendehill vaccine was licensed in Britain in 1969, and shortly thereafter, the RA 27/3 vaccine (human diploid cells) was licensed in Europe. In Japan, the initial vaccines licensed were the Takahashi (rabbit kidney) and Matsuura (Japanese quail-embryo fibroblasts) vaccines. Three additional vaccines were licensed in Japan: Matsuba (rabbit kidney), DCRB 19 (rabbit kidney), and TO-336 (rabbit kidney) [89].
By 1979, all three of the vaccines licensed in the United States were replaced by RA27/3. RA27/3 vaccine generally induces higher antibody titers and produces an immune response more closely paralleling natural infection than the other vaccines. HPV-77.DK12 was withdrawn due to the higher incidence of side effects as compared to other vaccines.
After the development and licensure of the initial rubella vaccines globally, additional vaccines were licensed in various geographic locations. In 1980, a rubella vaccine (BRD-2) was developed in the People’s Republic of China using a local RV strain from a child, isolated in human diploid cells. In a trial comparing the BRD-2 vaccine and RA 27/3 vaccine, the seroconversion rate and mild side effects were similar [90]. In Japan, currently, five different rubella vaccines are in use, including the TO-366 vaccine [91]. Even though additional vaccines have been licensed and developed, RA27/3 continues to be the most widely used vaccine strain globally.
Rubella-containing vaccine is available as either a single antigen or combined with measles (MR), measles and mumps (MMR), and measles, mumps, and varicella (MMRV).
9.2 Response
9.2.1 Clinical Reactions
Vaccines can develop mild rubella, including rash, lymphadenopathy, fever, sore throat, and headache. However, the incidence of each of these side effects varies directly with age, being almost absent in infants and increasing with age. Fortunately, the minor side effects are seldom severe enough to cause days to be lost from school or work [92–94].
In a double-blind study of vaccination with MMR in twins, there was a 1 % incidence of arthropathy and little evidence of other reactions [95]. In 1991, the Institute of Medicine of the National Academy of Sciences published a committee report on four possible adverse effects of rubella vaccine: acute arthritis, chronic arthritis, neuropathies, and thrombocytopenia [96]. The committee concluded that RA27/3 causes acute arthritis. With regard to chronic arthritis, the committee stated doubtfully, “The evidence is consistent with a causal relation between the currently used rubella vaccine strain (RA27/3) and chronic arthritis in adult women, although the evidence is limited in scope and confined to reports from one institution.” Since that time, large vaccination campaigns conducted in millions of Latin Americans, including women of childbearing age, have not been accompanied by additional reports of significant chronic arthropathy [64].
In 2011, IOM was asked to review adverse events associated with several vaccines. In their report, the IOM concluded that the evidence is inadequate to accept or reject the causal relationship between MMR vaccine and chronic arthralgia or arthritis in women [97].
9.2.2 Shedding of Virus
Because of the risk of spreading of vaccine virus to susceptible persons including pregnant women, considerable effort has been made to detect the spread of vaccine virus to susceptible contacts. Early contact studies documented no evidence of spread to susceptible contacts. However, there was a rare asymptomatic seroconversion that could not be explained fully [98, 99].
Virus has been recovered from breast milk of women vaccinated postpartum. Transmission of the virus to the infant has been documented, but the infection is asymptomatic and transient.
9.2.3 Serological Response
Rubella vaccine is usually administered ≥12 months of age, since maternal antibodies have usually disappeared by that age. The seroconversion rate for children ≥12 months is >95 %. The age at first vaccination does not appear to be as critical for rubella as for measles vaccine. Passively transmitted maternal antibodies to rubella have been found in approximately 5 % of infants from 9 to 12 months and 2 % from 12 to 15 months of age. Studies of rubella-containing vaccine administered at 9–12 months of age has demonstrated a seroconversion rate of >90 %. Rubella vaccine is usually offered to children with measles vaccine (MR) or measles and mumps vaccines (MMR).
9.3 Rubella Vaccination Strategies: Their Impact on Rubella and Congenital Rubella
9.3.1 Epidemiological Approach
The goal of rubella vaccination programs is the prevention of the intrauterine infection that causes CRS. There initially were two basic approaches: the US (indirect protection) (see Sect. 5.1) and the UK (direct protection). However, with over 30 years of experience with introducing rubella vaccine into countries, the strategies have evolved.
In 2000, the WHO convened a meeting to review the worldwide status of CRS and its prevention [100, 101]. Since the previous international meeting on CRS and rubella in 1984, some of the changes included availability of more data on the CRS disease burden in developing countries, an increase in the number of countries with national rubella immunization programs, and advances in laboratory diagnosis. In 1996, only 83 countries/territories used rubella vaccine in their national immunization programs. Since the 2000 meeting, additional countries have introduced rubella-containing vaccine, two WHO regions (Regions of the Americas and Europe) have established rubella elimination goals by 2010 and 2015, respectively, and one WHO region (Western Pacific) has established an accelerated rubella control and CRS prevention goal by 2015. As of 2010, this number had increased to 130 countries.
In 2011, the WHO rubella vaccine recommendations were updated [64]. The WHO recommends that countries that have not introduced rubella vaccination take the opportunity offered by accelerated measles control and elimination to introduce rubella vaccine. The measles vaccine strategy platform provides the opportunity to use combined vaccine and an integrated measles-rubella surveillance system. The preferred strategy for introduction of rubella vaccination is to begin with MR/MMR vaccine in a campaign targeting a wide range of ages together with immediate introduction of MR/MMR vaccine into the routine program. In 2011, GAVI (formerly the Global Alliance for Vaccines and Immunization) opened a window for introduction of rubella-containing vaccine into GAVI eligible countries (for more on GAVI, see Chap. 1. Of the remaining 63 countries that had not introduced rubella vaccine in 2011, 51 (81 %) are GAVI eligible. GAVI funding will support MR vaccine for catchup campaigns targeting children 9 months to 14 years 11 months and introduction grant. It is estimated that 30 countries will have introduced rubella vaccine by the end of 2015, and all GAVI eligible countries will have introduced it by 2018. With GAVI support, the goal of rubella eradication may be within reach.
9.3.2 Vaccination in Pregnancy
Although there is now abundant evidence for the safety of RA 27/3 for the fetus, pregnancy remains a contraindication to rubella vaccination, and women are advised to take precautions against pregnancy for 1 month (28 days) after vaccination. Prior to the efforts to eliminate rubella from Latin America, there was limited data on vaccination of unknowingly pregnant women [102]. To eliminate rubella and CRS in the region of the Americas, countries conducted campaigns in adult. As part of the campaigns in several countries, women who were vaccinated and subsequently learned that they were pregnant at the time of vaccination were followed up. On the basis of serological evaluation, 2,894 (10 %) women were classified as susceptible at the time of vaccination; of their pregnancies, 1980 (90 %) resulted in a live birth. Sera from 70 (3.5 %) of these infants were rubella IgM antibody positive, but none of the infants had features of CRS as a result of rubella vaccination. The maximum theoretical risk for CRS following rubella vaccination of susceptible pregnant women was 0.2 %. In all the available literature on vaccination of pregnant women, approximately 3,000 susceptible women with live births have been followed up and none of the infants had features of CRS.
9.3.3 Persistence of Vaccine-Induced Immunity
Studies on the long- term persistence of antibodies after rubella immunization of susceptible persons have documented that immunity probably persists for life in the majority of vaccines. Although antibody titers fall over time, sometimes to very low levels, immunological memory persists, and a secondary immune response will occur on exposure to rubella.
Follow-up studies have shown that 95–100 % RA27/3 vaccines are seropositive 10–21 years after immunization [103]. The high seroconversion rate, the persistence of antibodies, and an amnestic response when revaccinated do not support the need for a second dose of rubella vaccine. However, based on the indications for a second dose of measles- and mumps-containing vaccine, a second dose of MMR is now offered in most industrialized countries, and this helps to boost low rubella antibody concentrations.
9.3.4 Reinfection
Reinfection is usually subclinical and is more likely to occur in persons with vaccine-induced immunity than in those whose immunity is naturally acquired. It is not due to antigenic variants of rubella virus [104]. Reinfection is defined as a significant rise in antibody concentration in a person with preexisting antibodies. In a clinical situation, preexisting antibodies can be confirmed by testing an earlier stored serum, but if no such serum is available, evidence of preexisting antibody may be accepted if there are at least two previous laboratory reports of antibodies ≥10 iu/ml obtained by reliable techniques (not HI) or a single result of antibodies ≥10 iu/ml obtained after documented rubella vaccination [105].
The concern for reinfection is a pregnant woman as it might lead to fetal infection. Several challenge tests have been conducted with some attempting to document viremia. In one of these studies [106], the viremia was detected in persons with low levels of antibody titers. The risk of congenital infection following reinfection in the first 12 weeks of pregnancy has been estimated in the United Kingdom to be about 8 %, while the risk of congenital rubella defects is probably no more than 5 %, which is considerably less than the >80 % risk of primary rubella during the same period of pregnancy [107]. Thus, it is important to be able to use laboratory tests to distinguish reinfection from primary rubella in pregnancy.
References
Smith JL. Rotheln (epidemic roseola-German measles-hybrid measles, etc.). Arch Dermatol. 1875;1:1–13.
Veale H. History of an epidemic of Rotheln, with observation on its pathology. Edin Med J. 1866;12:404–14.
Smith JL. Contributions to the study of Rötheln. Trans Int Med Congr Phil. 1881;4:14.
Gregg NM. Congenital cataract following German measles in the mother. Trans Ophthalmol Soc Aust. 1941;3:35–46.
Burgess MA. Gregg’s rubella legacy 1941–1991. Med J Aust. 1991;155(6):355–7.
Pitt D, Keir EH. Results of rubella in pregnancy. Med J Aust. 1965;2:647–51.
Lundstrom R. Rubella during pregnancy: a follow-up study of children born after an epidemic of rubella in Sweden, 1951, with additional investigations on prophylaxis and treatment of maternal rubella. Acta Paediatr Scand. 1962;133(Suppl):1–110.
Greenberg M, Pellitteri O, Barton J. Frequency of defects in infants whose mothers had rubella during pregnancy. JAMA. 1957;165:675–8.
Manson MM, Logan WPD, Loy RM. Rubella and other virus infections during pregnancy (Report on Public Health and Mechanical Subjects, No. 101.) London: Her Royal Majesty’s Stationery Office; 1960.
Weller TH, Neva FA. Propagation in tissue culture of cytopathic agents from patients with rubella-like illness. Proc Soc Exp Biol Med. 1962;111:215–25.
Parkman PD, Buescher EL, Artenstein MS. Recovery of rubella virus from army recruits. Proc Soc Exp Biol Med. 1962;111:225–30.
Witte JJ, Karchmer AW. Epidemiology of rubella. Am J Dis Child. 1969;118:107–12.
Plotkin SA, Orenstein W, Offit PA. Rubella surveillance. 1. Bethesda: National Communicable Disease Center, United States Department of Health, Education and Welfare; 1969.
Plotkin SA, Oski FA, Hartnett EM, et al. Some recently recognized manifestations of the rubella syndrome. J Pediatr. 1965;67:182–91.
Cooper LZ, Krugman S. Clinical manifestations of postnatal and congenital rubella. Arch Ophthalmol. 1967;77:434–9.
Meyer HM, Parkman PD, Hobbins TE, et al. Attenuated rubella viruses: laboratory and clinical characteristics. Am J Dis Child. 1969;118:155–69.
Prinzie A, Huygelen C, Gold J, et al. Experimental live attenuated rubella virus vaccine: clinical evaluation of Cendehill strain. Am J Dis Child. 1969;118:172–7.
Plotkin SA, Farquhar J, Katz M, Buser F. Attenuation of RA27/3 rubella virus in WI-38 human diploid cells. Am J Dis Child. 1969;118:178–85.
Reef SE, Redd SB, Abernathy E, Kutty P, Icenogle JP. Evidence used to support the achievement and maintenance of elimination of rubella and congenital rubella syndrome in the United States. J Infect Dis. 2011;204 Suppl 2:S593–7.
Averhoff F, Zucker J, Vellozzi C, Redd S, et al. Adequacy of surveillance to detect endemic rubella transmission in the United States. Clin Infect Dis. 2006;43 Suppl 3:S151–7.
Upreti SR, Thapa K, Pradhan YV, Shakya G, et al. Developing rubella vaccination policy in Nepal–results from rubella surveillance and seroprevalence and congenital rubella syndrome studies. J Infect Dis. 2011;204 Suppl 1:S433–8.
Pebody RG, Edmunds WJ, Conyn-van Spaendonck M, Olin P, et al. The seroepidemiology of rubella in Western Europe. Epidemiol Infect. 2000;125:347–57.
Cockburn WC. World aspects of the epidemiology of rubella. Am J Dis Child. 1969;118(1):112–22.
Nardone A, Miller E, ESEN2 Group. Serological surveillance of rubella in Europe: European Sero-Epidemiology Network (ESEN2). Euro Surveill. 2004;9:5–7.
Hyde TB, Kruszon-Moran D, McQuillan GM, Cossen C, Forghani B, Reef SE. Rubella immunity levels in the United States population: has the threshold of viral elimination been reached? Clin Infect Dis. 2006;43 Suppl 3:S146–50.
World Health Organization. Manual for the laboratory diagnosis of measles and rubella virus infection. 2nd ed. Geneva: World Health Organization; 2007.
Featherstone DA, Rota PA, Icenogle J, Mulders MN, et al. Expansion of the global measles and rubella laboratory network 2005–09. J Infect Dis. 2011;204 Suppl 1:S491–8.
Parkman PD, et al. Studies of rubella. II. Neutralization of the virus. J Immunol. 1964;93:608–17.
Stewart GL, et al. Rubella-virus hemagglutination-inhibition test. N Engl J Med. 1967;276:554–7.
Best JM, Enders G. Laboratory diagnosis of rubella and congenital rubella. In: Banatvala JE, Peckham C, editors. Rubella viruses. London: Elsevier; 2007. p. 39–77.
O’Shea S, Best JM, Banatvala JE, Shepherd WM. Development and persistence of class-specific serum and nasopharyngeal antibodies in rubella vaccines. J Infect Dis. 1985;151:89–98.
Sarnesto A, et al. Proportions of Ig classes and subclasses in rubella antibodies. Scand J Immunol. 1985;21:275–82.
Wilson KM, et al. Humoral immune response to primary rubella virus infection. Clin Vaccine Immunol. 2006;13:380–6.
Thomas HIJ, et al. Persistence of specific IgM and low avidity specific IgG1 following primary rubella. J Virol Methods. 1992;39:149–55.
World Health Organization. Manual for the laboratory diagnosis of measles and rubella virus. 2nd ed. Geneva: World Health Organization; 2007.
Abernathy E, Cabezas C, Sun H. Confirmation of rubella within 4 days of rash onset: comparison of rubella virus RNA detection in oral fluid with immunoglobulin M detection in serum or oral fluid. J Clin Microbiol. 2009;47:182–8.
Wolinsky JS. Rubella. In: Fields BN, Knipe DM, Hawley PM, editors. Fields’ virology. New York: Raven Press; 1996. p. 899–929.
World Health Organization. Standardization of the nomenclature for genetic characteristics of wild- type rubella viruses. Wkly Epidemiol Rec. 2005;80:126–32.
World Health Organization. Update of standard nomenclature for wild-type rubella viruses, 2007. Wkly Epidemiol Rec. 2007;82:216–22.
Abernathy ES, Hubschen JM, Muller CP, et al. Status of global virologic surveillance for rubella viruses. J Infect Dis. 2011;204 Suppl 1:S524–32.
Zheng DP, Frey TK, Icenogle J, et al. Global distribution of rubella virus genotypes. Emerg Infect Dis. 2003;9(12):1523–30.
Zhu Z, Abernathy E, Cui A, et al. Rubella virus genotypes in the People’s Republic of China between 1979 and 2007: a shift in endemic viruses during the 2001 Rubella Epidemic. J Clin Microbiol. 2010;48:1775–81.
Preblud SR, Serdula MK, Frank Jr JA, Hinman AR. From the Center for Disease Control: current status of rubella in the United States, 1969–1979. J Infect Dis. 1980;142:776–9.
Hinman AR, Preblud SR, Brandling-Bennett AD. Rubella: the U.S. experience. Dev Biol Stand. 1978;43:315–26.
CDC. Prelicensing statement on rubella virus vaccine: recommendation of the Public Health Service Advisory Committee on Immunization Practices. MMWR. 1969;18.
Preblud SR, Serdula MK, Frank Jr JA, Brandling-Bennett AD, Hinman AR. Rubella vaccination in the United States: a ten-year review. Epidemiol Rev. 1980;2:171–94.
Williams NM, Preblud SR. Current epidemiology of rubella in the United States. In: Proceedings of 19th National Immunization Conference (Boston, MA). Centers for Disease Control 1984. p. 11–17.
Preblud SR, Hinman AR. Remaining problems with rubella. Infect Dis. 1980;10:1, 3, 6, 7, 22.
CDC. Rubella surveillance, January 1976–December 1978. Atlanta: CDC; 1980.
CDC. Rubella vaccine: recommendation of the Immunization Practices Advisory Committee (ACIP). MMWR. 1978;27:451–4, 459.
Bart KJ, Orenstein WA, Preblud SR, Hinman AR, Lewis Jr FL, Williams NM. Elimination of rubella and congenital rubella from the United States. Pediatr Infect Dis. 1985;4:14–21.
Williams NM, Preblud SR. Rubella and congenital rubella surveillance, 1983. MMWR CDC Surveill Summ. 1984;33(4):1SS–10.
CDC. Rubella—United States, 1979–1982. MMWR. 1982;31:573–5.
Orenstein WA, Bart KJ, Hinman AR, et al. The opportunity and obligation to eliminate rubella from the United States. JAMA. 1984;251:1988–94.
Public Health Service. Promoting health/preventing disease: objectives for the nation. Washington, DC: Public Health Service; 1980.
CDC. Rubella prevention. Recommendation of the Immunization Practices Advisory Committee. MMWR. 1981;30:37–41, 47.
Lindegren ML, Fehrs LJ, Hadler SC, Hinman AR. Update: rubella and congenital rubella syndrome, 1980–1990. Epidemiol Rev. 1991;13:341–8.
Public Health Service. Healthy people 2000: national health promotion and disease prevention objectives—full report, with commentary. Washington, DC: US Department of Health and Human Services, Public Health Service; 1990, DHHS publication no. (PHS) 91–50212.
Reef SE, Frey TK, Theall K, Abernathy E, Burnett CL, Icenogle J, McCauley MM, Wharton M. The changing epidemiology of rubella in the 1990s: on the verge of elimination and new challenges for control and prevention. JAMA. 2002;287:464–72.
Papania M, et al. Elimination of endemic measles, rubella and congenital rubella syndrome from the Western Hemisphere- The United States Experience. JAMA Pediatr. 2014;168(2):148–55.
Centers for Disease Control and Prevention (CDC). Three cases of congenital rubella syndrome in the post-elimination era–Maryland, Alabama, and Illinois, 2012. MMWR Morb Mortal Wkly Rep. 2013;62(12):226–9.
Robertson SE, Featherstone DA, Gacic-Dobo M, Hersh BS. Rubella and congenital rubella syndrome: global update. Rev Panam Salud Publica. 2003;14(5):306–15.
Cutts FT, Robertson SE, Diaz-Ortega JL, Samuel R. Control of rubella and congenital rubella syndrome (CRS) in developing countries, Part 1: Burden of disease from CRS. Bull World Health Organ. 1997;75(1):55–68.
World Health Organization. Rubella vaccines: WHO position paper. Wkly Epidemiol Rec. 2011;86(29):301–16.
Chan CM, Tsang HF. Rubella in Hong Kong. Public health and epidemiology bulletin, Department of Health, Hong Kong. 1995;4(3):17–20.
Schatzmayr HG. Aspects of rubella infection in Brazil. Rev Infect Dis. 1985;7 Suppl 1:S53–5.
Owens CS, Espino RT. Rubella in Panama: still a problem. Pediatr Infect Dis J. 1989;8:110–5.
Marquez A, Zapata MT. Epidemiology of rubella in the province of Cordoba, Argentina. Bol Oficina Sanit Panam. 1984;97(1):14–25 (in Spanish).
Desudchit P, Chatiyanonda K, Bhamornsathit S. Rubella antibody among Thai women of childbearing age. Southeast Asian J Trop Med Public Health. 1978;9(3):312–6.
Intaraprasert S, Prasertsawat PO, Phiromsawat S. Postpartum rubella immunization: Ramathibodi experience in March-April 1986. J Med Assoc Thai. 1988;71 Suppl 1:94–7.
Phiromsawat S, et al. Rubella: a serologic study in pregnant women at Ramathibodi Hospital (1984–1985). J Med Assoc Thai. 1988;71 Suppl 2:26–8.
Castillo-Solórzano C, Marsigli C, Bravo-Alcántara P, et al. Elimination of rubella and congenital rubella syndrome in the Americas. J Infect Dis. 2011;204 Suppl 2:S571–8.
Janta D, Stanescu A, Lupulescu E, Molnar G, Pistol A. Ongoing rubella outbreak among adolescents in Salaj, Romania, September 2011–January 2012. Euro Surveill. 2012;17(7):pii=20089. http://www.eurosurveillance.org/images/dynamic/EE/V17N07/art20089.pdf.
Paradowska-Stankiewicz I, Czarkowski M, Derrough T, Stefanoff P. Ongoing outbreak of rubella among young male adults in Poland: increased risk of congenital rubella infections. Euro Surveill. 2013;18(21):pii=20485. http://www.eurosurveillance.org/ViewArticle.aspx?ArticleId=20485.
Centers for Disease Control and Prevention (CDC). Nationwide rubella epidemic – Japan, 2013. MMWR Morb Mortal Wkly Rep. 2013;62:457–62.
Goodson JL, Masresha B, Dosseh A, Byabamazima C, Nshimirimana D, Cochi S, Reef S. Rubella epidemiology in Africa in the prevaccine era, 2002–2009. J Infect Dis. 2011;204 Suppl 1:S215–25.
Al-Nakib W, Best JM, Banatvala JE. Rubella-specific serum and nasopharyngeal immunoglobulin responses following naturally acquired and vaccine induced infection; prolonged persistence of virus-specific IgM. Lancet. 1975;1(7900):182–5.
Buimovici-Klein E, Cooper LZ. Cell-mediated immune response in rubella infections. Rev Infect Dis. 1985;7 Suppl 1:S123–8.
Buimovici-Klein E, Vesikari T, et al. Study of the lymphocyte in vitro response to rubella antigen and phytohaemagglutinin by a whole blood method. Arch Virol. 1976;52:323–31. 5:182–5.
Lawton AR, et al. Ontogeny of lymphocytes in the human fetus. Clin Immunol Immunopathol. 1972;1:104.
Bellanti JA, et al. Congenital rubella: clinicopathologic, virologic, and immunologic studies. Am J Dis Child. 1965;110:464.
Alford Jr CA. Studies on antibody in congenital rubella infections. I. Physicochemical and immunologic investigations of rubella-neutralizing antibody. Am J Dis Child. 1965;110:455.
Buescher EL. Behavior of rubella virus in adult populations. Arch Gesamte Virusforsch. 1965;16:470–6.
Green RH, Balsamo MR, Giles JP, Krugman S, Mirick GS. Studies of the natural history and prevention of rubella. Am J Dis Child. 1965;110(4):348–65.
Chaari A, Bahloul M, Berrajah L, Kahla SB, Gharbi N, Karray H, Bouaziz M. Childhood rubella encephalitis: diagnosis, management, and outcome. J Child Neurol. 2012.
Cooper LZ. The history and medical consequences of rubella. Rev Infect Dis. 1985;7 Suppl 1:S2–10.
Sever JL, Schiff GM, Huebner RJ. Inactivated rubella virus vaccine. J Lab Clin Med. 1963;62:1015.
Parkman PD, Meyer HM, Kirschstein BL, Hopps HE. Attenuated rubella virus. I. Development and laboratory characterization. N Engl J Med. 1966;275:569–74.
Perkins FT. Licensed vaccines. Rev Infect Dis. 1985;7 Suppl 1:S73–6.
Yaru H, Zhao K, Yinxiang G, Sulan H, Shuzhen W, Changtai W. Rubella vaccine in the People’s Republic of China. Rev Infect Dis. 1985;7 Suppl 1:S79.
Kakizawa J, Nitta Y, Yamashita T, Ushijima H, Katow S. Mutations of rubella virus vaccine TO-336 strain occurred in the attenuation process of wild progenitor virus. Vaccine. 2001;19:2793–2–802.
Bottiger M, Heller L. Experiences from vaccination and revaccination of teenage girls with three different rubella vaccines. J Biol Stand. 1976;4(2):107–14.
Freestone DS, Prydie J, Smith SG, Laurence G. Vaccination of adults with Wistar RA 27/3 rubella vaccine. J Hyg (Lond). 1971;69(3):471–7.
Fogel A, Moshkowitz A, Rannon L, Gerichter CB. Comparative trials of RA 27–3 and Cendehill rubella vaccines in adult and adolescent females. Am J Epidemiol. 1971;93(5):392–8.
Peltola H, Heinonen OP. Frequency of true adverse reactions to measles-mumps-rubella vaccine. A double-blind placebo-controlled trial in twins. Lancet. 1986;1(8487):939–42.
Howson CP, Howe CJ, Fineberg HV. Chronic arthritis. In: Institute of Medicine, Howson CP, Howe CJ, Fineberg HV, editors. Adverse effects of pertussis and rubella vaccines. Washington, DC: National Academy Press; 1991. p. 196.
IOM (Institute of Medicine). Adverse effects of vaccines: evidence and causality. Washington, DC: National Academics Press; 2011. p. 89–210, 574–6.
Meyer Jr HM, Parkman PD. Rubella vaccination. A review of practical experience. JAMA. 1971;215(4):613–9.
Mogabgab WJ, Stowe Jr FR. Evaluation of attenuated rubella virus vaccine in families. Am J Dis Child. 1971;122(2):122–8.
World Health Organization. Rubella vaccines: WHO position paper. Wkly Epidemiol Rec. 2000;75:161–9.
World Health Organization (WHO). Report of a meeting on preventing congenital rubella syndrome: immunization strategies, surveillance needs, vol. 10. Geneva: WHO Departments of Vaccines and Biologicals; 2000. p. 1–77.
Castillo-Solórzano C, Reef SE, Morice A, et al. Rubella vaccination of unknowingly pregnant women during mass campaigns for rubella and congenital rubella syndrome elimination, the Americas 2001–2008. J Infect Dis. 2011;204 Suppl 2:S713–7.
Best JM, Reef SE. Module 11: rubella. The immunological basis for immunization series. Geneva: World Health Organization; 2008.
Bosma TJ, et al. Nucleotide sequence analysis of a major antigenic domain of 22 rubella virus isolates. J Gen Virol. 1996;77:2523–30.
Best JM, et al. Fetal infection after maternal reinfection with rubella: criteria for defining reinfection. Br Med J. 1989;299:773–5.
Balfour HH, et al. Rubella viraemia and antibody responses following rubella vaccination and reimmunization. Lancet. 1981;1:1078–80.
Morgan-Capner P, Crowcroft NS, PHLS Joint Working Party of the Advisory Committees of Virology and Vaccines and Immunization. Guidelines on the management of, and exposure to, rash illness in pregnancy (including consideration of relevant antibody screening programmes in pregnancy). Commun Dis Public Health. 2002;5 Suppl 1:59–71.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer Science+Business Media New York
About this chapter
Cite this chapter
Orenstein, W., Reef, S.E. (2014). Rubella Virus. In: Kaslow, R., Stanberry, L., Le Duc, J. (eds) Viral Infections of Humans. Springer, Boston, MA. https://doi.org/10.1007/978-1-4899-7448-8_31
Download citation
DOI: https://doi.org/10.1007/978-1-4899-7448-8_31
Published:
Publisher Name: Springer, Boston, MA
Print ISBN: 978-1-4899-7447-1
Online ISBN: 978-1-4899-7448-8
eBook Packages: MedicineMedicine (R0)