Abstract
Adult neurogenesis in the dentate gyrus is profoundly disrupted by seizure activity in experimental models. The relationship between this disruption, seizure-induced plasticity, and the pathogenesis of epilepsy is complex and not well understood, but there is great interest in the therapeutic potential of modulating the effects of seizures on dentate granule cell (DGC) neurogenesis. In this chapter, we discuss how seizure activity or epileptic insults influence DGC neurogenesis, as well as the potential effects of altered neurogenesis on epilepsy development, a process known as epileptogenesis. Where possible, data are included that provide insight into potential underlying mechanisms, or to highlight specific areas where more work is needed to better understand the relationship between seizure activity and aberrant neurogenesis.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
5.1 Introduction
Epilepsy is a complex and diverse neurological disorder characterized by spontaneous recurrent seizures. Of the large variety of epilepsy syndromes, temporal lobe epilepsy (TLE) is the most common in adults. It is also one of the most intractable: in more than 30 % of persons with TLE, seizure activity is not controlled by pharmacotherapy (Engel and Pedley 1998). In many TLE patients, removal of the seizure focus, which includes the hippocampus and other anteromedial temporal lobe structures, alleviates seizures. These resected tissues, along with postmortem tissues, often display hippocampal sclerosis, which includes pyramidal cell death, astrogliosis, and structural reorganization within the dentate gyrus (Engel and Pedley 1998). Pathology in the dentate gyrus is of particular relevance to those interested in adult neurogenesis, because the dentate is a well-established region of ongoing neurogenesis in the adult human brain (Eriksson et al. 1998).
The causes of TLE are largely unknown and probably vary across patients. In many cases, the onset of spontaneous seizures is preceded by an initial precipitating injury, which is believed to play a causal role in the development of epilepsy. Precipitating injuries are different from patient to patient, ranging from prolonged febrile seizures, to nervous system infections like bacterial meningitis, to traumatic brain injury and others. However, most people who experience these insults will not go on to develop epilepsy (Harvey et al. 1997). For those that do, the latent period (time between the injury and onset of seizures) is highly variable. All of these factors contribute to the difficulty of understanding the process of epileptogenesis, which involves cellular and molecular changes leading to the generation of spontaneous recurrent seizures.
Because surgical tissue from patients with epilepsy is typically obtained during late disease stages, this tissue has limited utility for understanding epileptogenesis. Therefore, animal models have been developed to study this process. The most common models use status epilepticus (SE), a prolonged period of continuous seizures, as the initial precipitating injury to produce spontaneous seizures in rodents. In these models, SE is induced by chemoconvulsants (usually pilocarpine or kainic acid) or electrical stimulation, and then spontaneous seizures develop after a latent period lasting days to weeks. Structural changes in the hippocampi of these animals arise within days of SE, and after weeks to months, much of the hippocampal histopathology resembles that seen in hippocampal tissue from human TLE patients (Buckmaster 2004). Within the dentate gyrus, this histopathology includes hilar and pyramidal cell death, dentate granule cell (DGC) layer dispersion, sprouting of mossy fibers, and ectopic locations of DGC bodies (Dudek and Sutula 2007; Houser 1992).
In the late 1990s two reports showed that seizure activity potently stimulates dentate gyrus neural stem cell (NSC) proliferation in rodent models of TLE (Bengzon et al. 1997; Parent et al. 1997). Over the past 15 years, this finding has been replicated in nearly every rodent TLE model (Scharfman and McCloskey 2009), and understanding the relationship between altered NSC behavior and epileptogenesis has become a large focus of the field. The data that emerged have led to a paradigm shift in our understanding of epilepsy-related pathology and strong interest in the potential for targeting NSCs for therapeutic intervention in TLE. In this chapter we will cover the prominent findings related to how seizures affect proliferation, survival, and development of DGC progenitors and their progeny. Although the impact of epileptic insults on DGC development and its subsequent contribution to epilepsy progression remains uncertain, we will describe recent work aimed at understanding these processes and offer suggestions for future directions. Recent data suggest subtle, but important, differences between levels and functionality of neurogenesis between rats and mice (Snyder et al. 2009). We will present pertinent data both from species and from a variety of models, while trying to highlight instances where discrepancies in the reported data may relate to the use of different species or models.
5.2 Cell Proliferation
Under basal laboratory conditions, about 9,000 new DGCs are generated daily in the young adult rat (Cameron and McKay 2001). Typically, 25–40 % of newly generated DGCs survive and functionally integrate into the dentate gyrus network (Kempermann et al. 2003; Tashiro et al. 2007). However, the number of cells generated and the proportion that survive into maturity are dynamically regulated and can be influenced by external stimuli at many different stages. For example, traumatic brain injury appears to stimulate cell division of a subset of dentate NSCs (Yu et al. 2008). Environmental enrichment tends to affect survival of newly generated DGCs more than the number of cells that are born (Kempermann et al. 1997; van Praag et al. 1999). Seizures, however, probably influence adult dentate gyrus neurogenesis at all stages in the neurogenic process, including proliferation of multiple NSC types, survival, maturation, and integration of adult-generated DGCs.
5.2.1 Response of Progenitor Populations to Seizures
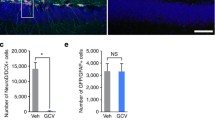
The population of NSCs in the adult dentate gyrus is complex and heterogeneous, and this heterogeneity is not well understood. This has recently been comprehensively reviewed (Duan et al. 2008; Faigle and Song 2013). Determining the responses of the different subsets of NSCs to seizure activity requires a nuanced approach to identifying NSC subpopulations that has not yet been undertaken in TLE models. However, many studies have distinguished the responses of at least two different progenitor populations to seizure activity. Radial glia-like stem cells are multipotent NSCs which are typically quiescent but participate in the early proliferative response to SE in the rodent dentate gyrus (Fig. 5.1) (Huttmann et al. 2003; Kronenberg et al. 2003; Lugert et al. 2010; Seri et al. 2004; Suh et al. 2007). Doublecortin (DCX)-expressing neural progenitors substantially increase in number several days after the initial SE episode and, depending on the severity and duration of SE, continue to accumulate for up to 4 weeks afterward (Jessberger et al. 2005; Jessberger et al. 2007b; Parent et al. 1997, 1999). DCX-expressing cells are committed to a neuronal fate (Francis et al. 1999); thus, most of the proliferating progenitor cells generate new neurons after SE. The survival of these post-SE-generated cells, however, is closely tied to seizure severity and duration (Mohapel et al. 2004). Interestingly, proliferation can be dramatically increased even with a mild seizure stimulus. In fact a single, discrete electrical stimulation-induced discharge is sufficient to increase neurogenesis several weeks later (Bengzon et al. 1997).
Schematic images of NSC and DGC organization within the intact (a) or representative epileptic (b) adult dentate gyrus. Purple structure represents a radial glia-like stem cell, blue represents amplifying neural progenitors, red represents immature DGCs, and green represents mature DGCs. OML = outer molecular layer, MML = middle molecular layer, IML = inner molecular layer, GCL = granule cell layer, SGZ = subgranular zone. (a) In an intact animal, the radial glia-like stem cell and amplifying progenitors are present in the SGZ. Radial glia-like cells are relatively quiescent and unlikely to be dividing at any given time. Amplifying progenitors are a relatively proliferative population and more likely to be dividing. Immature neurons are beginning to develop processes and may have a transient hilar basal dendrite, but it does not receive synaptic input. Mature DGCs, including those born in adulthood, have fully arborized dendritic trees that extend to the outer molecular layer and mossy fiber axons that branch in the hilus and extend out to area CA3. (b). In an animal with epilepsy, radial glia-like stem cells may be activated early after SE in some models, but still generally remain quiescent. Amplifying progenitors, however, are commonly upregulated by seizure activity in many models. Immature neurons develop more rapidly, showing longer processes and more dendritic spines. Some immature neurons migrate ectopically into the hilus, where they remain throughout maturity. Once the cells mature, they may retain hilar basal dendrites, be ectopically located in the hilus, or sprout mossy fiber axons into the inner molecular layer
5.2.2 Effects of Chronic Seizures and Aging
Fewer studies have focused on neurogenesis in the chronic phase of epilepsy. Although it is well known that basal levels of neurogenesis decline with age in the rodent dentate gyrus (Kuhn et al. 1996), it is unclear how chronic epilepsy influences this age-related decline. Recent work suggests that 5 months after chemoconvulsant-induced SE, rats have dramatically reduced basal neurogenesis compared to same-aged controls (Hattiangady et al. 2004). Although the mechanism for this reduction is unknown, it may result from impaired NSC function in the epileptic brain, or perhaps from a reduction in the available “NSC pool.” However, others have found that 6 months after electrically induced SE, epileptic animals do not show a decrease in basal neurogenesis compared to age-matched controls (Bonde et al. 2006), highlighting the variability between models and the importance of understanding how different models relate to human disease.
The age of an animal at the onset of SE is also an important factor in the NSC response. Typically, epilepsy is induced in juvenile/young adult rodents (1–4 months of age). Animals within this age range have equivalent levels of post-SE neurogenesis, despite slight decreases in basal neurogenesis (Gray et al. 2002). However, 24-month-old animals, and in some experiments even those as young as 12 months, do not show increased neurogenesis in response to an epileptogenic insult (Hattiangady and Shetty 2008; Rao et al. 2008). Importantly, this finding is not the result of a general unresponsiveness of NSCs in aged animals, since increased neurogenesis in response to voluntary exercise is maintained in senescent animals (van Praag et al. 2005). Instead, the differential response suggests a specific reduction in NSC activation by seizures in the aged brain.
5.2.3 Possible Mechanisms of Proliferative Response to Seizures
Clues as to why the NSC response differs among models or between the young and old brain may come from a better understanding of the molecular mechanisms that lead to enhanced proliferation after an epileptogenic insult. Part of the difficulty in studying this phenomenon is the fact that molecular mechanisms mediating adult neurogenesis in the intact dentate gyrus are not completely understood. Recent evidence suggests that many of the same processes involved in neurogenesis during brain development also regulate adult neurogenesis (Faigle and Song 2013). Some of these molecular pathways are also stimulated by SE (Elliott and Lowenstein 2004). For example, data indicate that SE alters Notch1 and Sonic hedgehog signaling in a manner that would promote cell proliferation (Banerjee et al. 2005; Sibbe et al. 2012). Trophic factors such as brain-derived neurotrophic factor (BDNF), fibroblast growth factor 2 (FGF-2), and vascular endothelial growth factor (VEGF) are increased in hippocampal tissue after SE (Gall 1993; Isackson et al. 1991; Newton et al. 2003; Warner-Schmidt and Duman 2007) and are also known regulators of adult neurogenesis (Faigle and Song 2013). An important consideration, however, is that changes observed in these signaling cascades after epileptic insults may be incidental to the fact that proliferation has been stimulated, rather than the direct mechanism of stimulation.
Importantly, neuronal activity itself can modulate NSC proliferation (Deisseroth et al. 2004). This effect is mediated through calcium channels, NMDA receptors, and possibly GABA-A receptors expressed by NSCs (Deisseroth et al. 2004; Tozuka et al. 2005). In the dentate gyrus, zinc is an additional potential link between neural activity and NSC proliferation. Zinc is normally released from DGC axon terminals, and zinc chelation after SE reduces NSC proliferation (Kim et al. 2012). Activity-dependent epigenetic modifications are also associated with altered NSC proliferation after single electroconvulsive seizures or chemoconvulsant-induced SE (Jessberger et al. 2007a; Ma et al. 2009), although in one of these settings, neurogenesis is modulated indirectly through epigenetic changes in mature DGCs (Ma et al. 2009). The myriad of diverse signals that have been reported to mediate NSC proliferation after discrete seizures or SE cannot be explained by studies using different epilepsy models because the same models are often used in a number of different studies. Rather, because seizures elicit a variety of changes in neural tissue, it is likely that within any given model, many different signals converge to produce a robust seizure-induced neurogenic response.
5.3 Cell Maturation and Integration
The percentage of adult-generated DGCs that survive the initial activity-dependent selection process is highly variable, even under baseline conditions. Some studies have reported as much as 75 % survival, others as little as 30 %, likely reflective of species and strain differences (Dayer et al. 2003; Kempermann et al. 2003; Snyder et al. 2009; Tashiro et al. 2007). In SE models, the percentage of post-SE-generated cells that survive and mature seems to be, in part, a function of the severity of SE (Mohapel et al. 2004) and a consequence of inflammation in the epileptic hippocampus (Ekdahl et al. 2003). The environmental changes that take place during epileptogenesis, as well as in the setting of chronic epilepsy, affect the maturation and integration of the surviving, seizure-generated DGCs. Moreover, whether these changes influence DGC progenitors to develop in a pro- or antiepileptic fashion may itself be a function of model severity.
5.3.1 Seizures Affect the Rate of DGC Maturation
In intact animals, adult-born DGCs progress through distinct maturation stages over a period of 3–4 months, after which they are fully integrated into the preexisting network and are indistinguishable from perinatally generated DGCs (Esposito et al. 2005; Laplagne et al. 2006; Piatti et al. 2006; Toni et al. 2008; van Praag et al. 2002; Zhao et al. 2006). Each stage of maturation is regulated by both intrinsic and extrinsic mechanisms. GABA plays an important role at many stages (Ge et al. 2007). Because of the high internal chloride concentration of adult neural progenitors and immature neurons, GABA depolarizes the membrane and elicits an excitatory response that is necessary for proper development (Ge et al. 2006; Overstreet Wadiche et al. 2005; Tozuka et al. 2005). Since the developing cells do not respond to glutamatergic inputs until they are about 2 weeks postmitotic (Piatti et al. 2006), tonic and synaptic GABA inputs drive much of the early activity-related development. This effect is, in part, mediated by the basic helix-loop-helix transcription factor NeuroD1, which is activated by GABA-driven activity and is required for survival and maturation of DGCs (Gao et al. 2009; Tozuka et al. 2005). Many SE models show profound changes to GABAergic activity in the dentate gyrus, due to the death of inhibitory interneurons and changes in the structure and function of the remaining interneurons (Dudek and Sutula 2007; Thind et al. 2010; Zhang et al. 2009). A direct relationship between altered GABA signaling and altered neurogenesis has not been explored in the context of TLE models, but this is a promising area for future research. Changes in network activity and in levels of growth factor expression also affect the rate of maturation and integration of adult-born DGCs (Piatti et al. 2011; Waterhouse et al. 2012). Not surprisingly, seizures also strongly affect the rate of DGC development. Under baseline conditions, DGC dendrites do not reach the outer molecular layer until about 21 days after birth (Toni et al. 2007). However, some DGCs born after or near the time of SE develop extensive dendritic arbors almost a week sooner and receive excitatory inputs well before their counterparts in control brains (Overstreet-Wadiche et al. 2006).
5.3.2 Aberrant DGC Migration in Epilepsy
In addition to speeding up maturation and integration, alterations in the local environment of the dentate gyrus after SE lead to abnormal DGC morphological features and physiology. Adult-born DGCs are generated in the subgranular zone (SGZ), between the granule cell layer (GCL) and the hilus. Normally, as they mature, they migrate into the GCL where their dendrites receive excitatory inputs from perforant path fibers. After SE, a subset of the newly generated DGCs migrates aberrantly into the hilus where they are innervated by mossy fiber axons (Jessberger et al. 2007b; Kron et al. 2010; Parent et al. 2006; Pierce et al. 2005). Newborn DGCs continue to migrate ectopically even in chronic epilepsy after the level of neurogenesis has returned to baseline (Bonde et al. 2006), suggesting that permanent changes to the epileptic network underlie the aberrant migration. Although the causes of aberrant migration are not well understood, reelin, a migratory signal that is involved in embryonic development, is one interesting candidate. Reelin signaling is important for proper migration of early postnatal and adult-born neurons in the dentate gyrus (Gong et al. 2007; Teixeira et al. 2012) and is potently disrupted by SE (Gong et al. 2007). Importantly, the loss of reelin signaling within individual DGCs in an otherwise normal animal is sufficient to induce ectopic migration of the affected cells (Teixeira et al. 2012).
Loss of reelin signaling has also been linked to aberrant locations of mature DGCs in the intra-hippocampal kainate model of SE (Heinrich et al. 2006). In this model, the chemoconvulsant kainic acid (KA) is delivered directly into the hippocampus of one hemisphere. This induces SE and robust cellular pathology, including dispersion of the granule cell body layer in the ipsilateral (injected) hippocampus. This dispersion, which can be observed rapidly following the KA injection, is not associated with an increase in neurogenesis (Fahrner et al. 2007), likely due to disruption of the dentate NSC niche from severe injury. Thus, work from different animal models indicates that dispersion of the normally compact granule cell body layer may result both from acute changes to the structure of mature DGCs and from chronic changes that impair migration of developing DGCs.
Due to their aberrant location and inputs, hilar ectopic granule cells (HEGCs) are thought to play an important role in the formation of a recurrent excitatory network after SE (Parent and Lowenstein 2002; Scharfman and Gray 2007). In addition to being innervated by mossy fiber axons, HEGCs send their axon collaterals to the molecular layer to form aberrant synapses onto DGC apical dendrites (Scharfman et al. 2000). Functionally, they receive more excitatory inputs than DGCs located in the GCL (Zhan et al. 2010; Zhang et al. 2012), and they become partially synchronized with pyramidal cells in area CA3 (Scharfman et al. 2000). However, HEGCs are probably not the only drivers of aberrant excitatory activity in the epileptic dentate gyrus. Many, perhaps most, other DGCs participate to some extent in the formation of the abnormal epileptic network. A major difficulty in defining the net effects of altered DGC neurogenesis on epileptogenesis, however, is that the DGCs in the granule cell layer, even those only generated after SE, are likely to be a heterogeneous population, with some contributing to excess excitability, others having a more neutral response, and still others perhaps playing a compensatory role by developing reduced excitability.
5.3.3 Aberrant Dendritic Morphology in Epilepsy
One subpopulation that is believed to contribute to the recurrent network is DGCs with hilar basal dendrites (HBDs) (Dashtipour et al. 2003; Ribak et al. 2000; Shapiro et al. 2005; Shapiro and Ribak 2006; Thind et al. 2008). Normally, basal dendrites are transient structures on immature DGCs of rodents that do not become synaptically integrated (Seress and Pokorny 1981). After SE, however, synapses rapidly develop onto HBDs (Shapiro et al. 2007), leading to spine formation (Jessberger et al. 2007b; Walter et al. 2007) and an overall increase in primarily excitatory inputs onto the cell (Thind et al. 2008). These HBDs persist once the cell has reached maturity (Ribak et al. 2000; Walter et al. 2007). Recent work also indicates that DGCs with a prominent HBD are more likely to have a very high spine density on their apical dendrites when compared with other DGCs born at the same time (Murphy et al. 2011). The mechanism for the increased presence of DGCs with HBDs after SE is not entirely understood, although the fact that HBDs are part of a normal developmental stage for DGCs may be a clue. Only DGCs that are in the process of developing at the onset of SE, or those that are born afterward, show increased rates of HBD persistence (Jessberger et al. 2007b; Kron et al. 2010; Walter et al. 2007). Thus, it seems more likely that DGCs developing in this abnormal environment are for some reason unable to retract their HBDs, than DGCs that regrow HBDs after they have been retracted. Importantly, HBDs have been linked not only to anatomical measures of excitability but to increased physiological excitation as well (Austin and Buckmaster 2004).
Despite the fact that HEGCs and those with HBDs comprise a minority of the total population, the degree to which they are hyper-innervated suggests that they may have a powerful influence on overall network excitability. Two studies suggest that pro-excitatory changes in a relatively small subset of DGCs are sufficient to induce epileptic activity. In one study, computational modeling of an epileptic dentate gyrus showed that the configuration of synaptic connectivity that most reliably produced seizure-like activity was one in which a small subset of DGCs (5 %) were highly interconnected (Morgan and Soltesz 2008). By keeping constant the total number of synapses in the network, and changing only the distribution of the recurrent DGC inputs, Morgan and Soltesz found that a network containing the highly interconnected DGC “hubs” was strongly activated by a relatively mild input. In a separate study, Pun and colleagues used a conditional transgenic mouse to alter the development of a subset of adult-born DGCs in the context of an otherwise normal brain. The genetically altered DGCs displayed HBDs, increased spine density, and ectopic migration into the hilus, similar to DGCs present in models of epilepsy. Remarkably, although only 9–24 % of DGCs developed these abnormal features, animals subsequently developed spontaneous recurrent seizures (Pun et al. 2012). Together, these studies indicate that small populations of DGCs can play a pivotal role in the development of seizure activity, and they highlight the need for a better understanding of individual DGC abnormalities in the context of TLE.
5.3.4 Axon Reorganization in Epilepsy
Mossy fiber sprouting (MFS) is another important feature of the recurrent epileptic network, but it has been difficult to determine whether specific subpopulations of DGCs selectively participate in this abnormality. Initially, the hypothesis was put forward that adult-generated DGCs developing after an epileptogenic insult are responsible for MFS (Parent and Lowenstein 1997); however, a study using irradiation to suppress neurogenesis provided evidence that ablating DGCs born after SE failed to prevent MFS within 4 weeks after SE (Parent et al. 1999). With the use of the more precise retrovirus birthdating methods, subsequent work suggested that only cells that were developing during SE or born afterward contributed to MFS (Kron et al. 2010). Recently, with an even more refined retrovirus, which targets yellow fluorescent protein to axon terminals by conjugating it to the synaptic vesicle protein synaptophysin (Umemori et al. 2004), we have found that neonatally generated DGCs that are mature at the time of SE do participate in MFS, along with those born during adulthood (unpublished data). Nevertheless, the role of MFS, at least in the supragranular inner molecular layer, in epileptogenesis remains controversial.
5.3.5 Potential Compensatory Role for New DGCs in Epilepsy
As mentioned earlier, some DGCs generated after SE appear to show decreased excitability, perhaps as a means of compensating for the overall hyperexcitability within the network. Several recent studies have used fluorescent reporter labeling using retroviruses or transgenic mice to identify DGCs born after SE in order to characterize the morphological and physiological characteristics of this population. On one extreme, nearly all of the adult-born DGCs examined in an adult rat electrical stimulation-induced SE model displayed strongly reduced excitation and increased inhibition (Jakubs et al. 2006), suggesting an anti-epileptogenic role for this population as a whole. In other studies of rodent chemoconvulsant TLE models, many of the adult-born DGCs display pro-excitatory features and receive increased excitatory inputs (Kron et al. 2010; Walter et al. 2007; Wood et al. 2011). Still others report a more mixed population, in which some cells clearly display pro-excitatory features (Jessberger et al. 2007b), while others have features that are consistent with reduced excitation (Murphy et al. 2011). The variability in the proportion of cells that might be “pro-excitatory” as opposed to “pro-inhibitory” in these models may reflect the use of different SE induction protocols. The type of induction protocol can have a dramatic effect on the development of chronic epilepsy, influencing the number and severity of spontaneous seizures. Moreover, post-SE-generated DGCs that are continuously exposed to seizures during their development show increased excitatory activity, even without a dramatic increase in aberrant morphology (Wood et al. 2011).
5.4 Functional Significance
The structural and functional heterogeneity of DGCs born after SE is one major challenge when considering the best way to target these cells for therapeutic intervention. Certainly aberrant integration of and increased excitatory inputs onto some of these cells seems to indicate that they play a pathological role in the development of spontaneous seizures. Supporting this idea is the fact that as little as 9 % of aberrantly connected DGCs in an otherwise normal animal is sufficient to induce spontaneous seizures (Pun et al. 2012). However, the subset of cells in this same population that display pro-inhibitory features in some epilepsy models may be an important part of the brain’s attempt to balance excess network excitability.
5.4.1 Neurogenesis Ablation Studies
Experimental efforts to eliminate the entire population of DGCs that are born in response to SE as a means of understanding the overall impact of this population on seizure development yield mixed results. For example, treatment with an antimitotic agent after chemoconvulsant-induced SE results in reduced seizure frequency (Jung et al. 2004; Jung et al. 2006), suggesting a net excitatory effect of this population on the network. However, focal brain irradiation to suppress neurogenesis in a kindling model increased seizure activity (Raedt et al. 2007), a finding that may indicate a net inhibitory effect of post-SE neurogenesis. Despite the differences in SE models and means of reducing neurogenesis in these experiments, taken together the results suggest that a targeted approach that can address aberrant integration of this cell population without interfering with the development of compensatory mechanisms may be the most effective strategy.
5.4.1.1 Neurogenesis and Human Temporal Lobe Epilepsy
Another, perhaps larger, challenge is to understand how the findings in rodent models relate to the human disease. When considering this question, it is important to note that TLE manifestations in patients are even more diverse than in animal models. Thus, it is perhaps incorrect to try to identify a model that “most closely” resembles the human disease. Instead, it seems most relevant to focus on the salient features in the different models.
Increased neurogenesis, per se, has not been demonstrated in human tissue from adult TLE patients (Fahrner et al. 2007), but there is evidence for increased numbers of neural progenitors in the dentate gyrus of some patients (Crespel et al. 2005). However, one must be cautious when drawing conclusions from postmortem human tissue or specimens obtained from epilepsy surgery to treat drug-resistant seizures. Often, this tissue comes from patients who have had seizures for many years and therefore may not reflect the same structural changes that initially led to epilepsy development. Because experimental tissue from patients in early stages of TLE is largely unavailable, it has been difficult to determine whether hippocampal neurogenesis is affected early in the disease. Interestingly, there is some evidence of increased neurogenesis in very young children after an epileptogenic insult (Blumcke et al. 2001).
The presence of HEGCs in human TLE tissue is well documented, but is not found in every patient (Parent et al. 2006; Parent and Murphy 2008; Scharfman and Gray 2007). Although lack of HEGCs in some tissues could be due to a number of factors, the same issues related to early versus late stage disease course apply when comparing findings in human tissue to experimental models. In addition to this caveat, another potential difficulty is the fact that the method for identifying cell types based on expression of endogenous markers identified in rodent cells may not be completely effective in human tissue. Thus, the presence of HEGCs could be missed if investigators only use one method for detection (Scharfman and Gray 2007). Nonetheless, HEGCs are present and functionally integrated in tissue from at least some patients with TLE (Parent et al. 2006; Parent and Murphy 2008). No obvious differences in intrinsic measures of excitability or perforant path connectivity are apparent between HEGCs and those in the GCL in human surgical TLE tissue (Parent and Murphy 2008; A. Althaus, G. Murphy and J. Parent, unpublished data). However, this finding is also largely true in animal models (Scharfman et al. 2003) and does not necessarily mean HEGCs do not play important roles in the network-level changes in excitability. Other electrophysiological studies of HEGCs in animal models have not yet been replicated in human tissue. Reasons include the reduced availability of living tissue and the difficulty in controlling for factors like slice angle and location within the rostro-caudal axis within the hippocampus when making acute slices from human tissue.
Although the increased presence of HBDs on developing and newborn DGCs after SE is a feature of many different models and represents an important opportunity for increased recurrent input between DGCs, the relevance of this finding to human TLE is also unclear. While mature DGCs in rodent tissue rarely (<6 %) have HBDs (Kron et al. 2010; Walter et al. 2007), they are more common on DGCs in non-epileptic humans (10 %) and nonhuman primates (25 %) (Seress 1992). However, several studies suggest that the number of cells with HBDs is increased in human TLE (Franck et al. 1995; von Campe et al. 1997), raising the possibility that HBDs contribute to increased recurrent innervation. It is unknown whether inputs to these structures are altered in TLE patients, and more work is needed to understand the potential importance of HBDs in human TLE.
In addition to contributing to seizure generation or spread, the aberrant integration of post-SE born DGCs may have other adverse effects on the epileptic brain. Great interest exists in understanding the normal function of adult neurogenesis, and though there are no definitive answers yet, a number of studies have found links between disrupted neurogenesis and disruptions in learning and memory (Deng et al. 2010). Although seizures in human TLE and in animal models affect many other structures besides the dentate gyrus, the potential relationship between aberrant neurogenesis and cognitive impairments in epileptic animals and human patients is intriguing. Also of interest is the reduction of neurogenesis that occurs in some animals in later stages of chronic TLE (Hattiangady et al. 2004) and the increased incidence of major depression in patients with TLE (Hermann et al. 2000). Because the presence of DGC neurogenesis appears to be a critical aspect of the effect of antidepressants, at least in some mouse strains (Santarelli et al. 2003), patients with TLE and comorbid major depression may benefit doubly from a therapeutic target that corrects aberrant neurogenesis or stimulates normal neurogenesis.
5.5 Conclusions
Seizure activity has such profound and widespread effects on all aspects of neurogenesis in the dentate gyrus that it may not be possible to understand the implications of any single aberrant feature on its own. Similarly, nearly all TLE models disrupt the normal function of many brain regions, making it extremely difficult to determine the “net” contribution of aberrant neurogenesis to epilepsy-related pathophysiology in animal models as well as human disease. However, the robust and reproducible nature of the data implicating aberrant DGC neurogenesis in the pathogenesis of TLE indicates the need for a more comprehensive understanding of how aberrant features develop and highlights the exciting potential for targeting aberrant neurogenesis as a therapeutic strategy. An important consideration going forward is the heterogeneity of DGC responses to seizures. In particular, much more work is needed to determine the potential compensatory or “anti-epileptogenic” function of some subpopulations of DGCs. A better understanding of the factors that influence DGCs to develop either pro- or anti-excitatory features should be useful in developing treatments not only for TLE but also for other neurological conditions that are believed to involve dysregulated neurogenesis.
Abbreviations
- BDNF:
-
Brain-derived neurotrophic factor
- DCX:
-
Doublecortin
- DGC:
-
Dentate granule cell
- FGF-2:
-
Fibroblast growth factor 2
- GCL:
-
Granule cell layer
- HBD:
-
Hilar basal dendrite
- HEGC:
-
Hilar ectopic granule cell
- IML:
-
Inner molecular layer
- KA:
-
Kainic acid
- MFS:
-
Mossy fiber sprouting
- MML:
-
Middle molecular layer
- NSC:
-
Neural stem cell
- OML:
-
Outer molecular layer
- SE:
-
Status epilepticus
- SGZ:
-
Subgranular zone
- TLE:
-
Temporal lobe epilepsy
- VEGF:
-
Vascular endothelial growth factor
References
Austin JE, Buckmaster PS (2004) Recurrent excitation of granule cells with basal dendrites and low interneuron density and inhibitory postsynaptic current frequency in the dentate gyrus of macaque monkeys. J Comp Neurol 476:205–218
Banerjee SB, Rajendran R, Dias BG, Ladiwala U, Tole S, Vaidya VA (2005) Recruitment of the Sonic hedgehog signalling cascade in electroconvulsive seizure-mediated regulation of adult rat hippocampal neurogenesis. Eur J Neurosci 22:1570–1580
Bengzon J, Kokaia Z, Elmer E, Nanobashvili A, Kokaia M, Lindvall O (1997) Apoptosis and proliferation of dentate gyrus neurons after single and intermittent limbic seizures. Proc Natl Acad Sci U S A 94:10432–10437
Blumcke I, Schewe JC, Normann S, Brustle O, Schramm J, Elger CE, Wiestler OD (2001) Increase of nestin-immunoreactive neural precursor cells in the dentate gyrus of pediatric patients with early-onset temporal lobe epilepsy. Hippocampus 11:311–321
Bonde S, Ekdahl CT, Lindvall O (2006) Long-term neuronal replacement in adult rat hippocampus after status epilepticus despite chronic inflammation. Eur J Neurosci 23:965–974
Buckmaster PS (2004) Laboratory animal models of temporal lobe epilepsy. Comp Med 54:473–485
Cameron HA, McKay RD (2001) Adult neurogenesis produces a large pool of new granule cells in the dentate gyrus. J Comp Neurol 435:406–417
Crespel A, Rigau V, Coubes P, Rousset MC, de Bock F, Okano H, Baldy-Moulinier M, Bockaert J, Lerner-Natoli M (2005) Increased number of neural progenitors in human temporal lobe epilepsy. Neurobiol Dis 19:436–450
Dashtipour K, Wong AM, Obenaus A, Spigelman I, Ribak CE (2003) Temporal profile of hilar basal dendrite formation on dentate granule cells after status epilepticus. Epilepsy Res 54:141–151
Dayer AG, Ford AA, Cleaver KM, Yassaee M, Cameron HA (2003) Short-term and long-term survival of new neurons in the rat dentate gyrus. J Comp Neurol 460:563–572
Deisseroth K, Singla S, Toda H, Monje M, Palmer TD, Malenka RC (2004) Excitation-neurogenesis coupling in adult neural stem/progenitor cells. Neuron 42:535–552
Deng W, Aimone JB, Gage FH (2010) New neurons and new memories: how does adult hippocampal neurogenesis affect learning and memory? Nat Rev Neurosci 11:339–350
Duan X, Kang E, Liu CY, Ming GL, Song H (2008) Development of neural stem cell in the adult brain. Curr Opin Neurobiol 18:108–115
Dudek FE, Sutula TP (2007) Epileptogenesis in the dentate gyrus: a critical perspective. Prog Brain Res 163:755–773
Ekdahl CT, Claasen JH, Bonde S, Kokaia Z, Lindvall O (2003) Inflammation is detrimental for neurogenesis in adult brain. Proc Natl Acad Sci U S A 100:13632–13637
Elliott RC, Lowenstein DH (2004) Gene expression profiling of seizure disorders. Neurochem Res 29:1083–1092
Engel J, Pedley TA (1998) Epilepsy : a comprehensive textbook. Lippincott-Raven, Philadelphia
Eriksson PS, Perfilieva E, Bjork-Eriksson T, Alborn AM, Nordborg C, Peterson DA, Gage FH (1998) Neurogenesis in the adult human hippocampus. Nat Med 4:1313–1317
Esposito MS, Piatti VC, Laplagne DA, Morgenstern NA, Ferrari CC, Pitossi FJ, Schinder AF (2005) Neuronal differentiation in the adult hippocampus recapitulates embryonic development. J Neurosci 25:10074–10086
Fahrner A, Kann G, Flubacher A, Heinrich C, Freiman TM, Zentner J, Frotscher M, Haas CA (2007) Granule cell dispersion is not accompanied by enhanced neurogenesis in temporal lobe epilepsy patients. Exp Neurol 203:320–332
Faigle R, Song H (2013) Signaling mechanisms regulating adult neural stem cells and neurogenesis. Biochimica et biophysica acta 1830:2435–2448
Francis F, Koulakoff A, Boucher D, Chafey P, Schaar B, Vinet MC, Friocourt G, McDonnell N, Reiner O, Kahn A et al (1999) Doublecortin is a developmentally regulated, microtubule-associated protein expressed in migrating and differentiating neurons. Neuron 23:247–256
Franck JE, Pokorny J, Kunkel DD, Schwartzkroin PA (1995) Physiologic and morphologic characteristics of granule cell circuitry in human epileptic hippocampus. Epilepsia 36:543–558
Gall CM (1993) Seizure-induced changes in neurotrophin expression: implications for epilepsy. Exp Neurol 124:150–166
Gao Z, Ure K, Ables JL, Lagace DC, Nave KA, Goebbels S, Eisch AJ, Hsieh J (2009) Neurod1 is essential for the survival and maturation of adult-born neurons. Nat Neurosci 12:1090–1092
Ge S, Goh EL, Sailor KA, Kitabatake Y, Ming GL, Song H (2006) GABA regulates synaptic integration of newly generated neurons in the adult brain. Nature 439:589–593
Ge S, Pradhan DA, Ming GL, Song H (2007) GABA sets the tempo for activity-dependent adult neurogenesis. Trends Neurosci 30:1–8
Gong C, Wang TW, Huang HS, Parent JM (2007) Reelin regulates neuronal progenitor migration in intact and epileptic hippocampus. J Neurosci 27:1803–1811
Gray WP, May K, Sundstrom LE (2002) Seizure induced dentate neurogenesis does not diminish with age in rats. Neurosci Lett 330:235–238
Harvey AS, Berkovic SF, Wrennall JA, Hopkins IJ (1997) Temporal lobe epilepsy in childhood: clinical, EEG, and neuroimaging findings and syndrome classification in a cohort with new-onset seizures. Neurology 49:960–968
Hattiangady B, Rao MS, Shetty AK (2004) Chronic temporal lobe epilepsy is associated with severely declined dentate neurogenesis in the adult hippocampus. Neurobiol Dis 17:473–490
Hattiangady B, Shetty AK (2008) Implications of decreased hippocampal neurogenesis in chronic temporal lobe epilepsy. Epilepsia 49(Suppl 5):26–41
Heinrich C, Nitta N, Flubacher A, Muller M, Fahrner A, Kirsch M, Freiman T, Suzuki F, Depaulis A, Frotscher M et al (2006) Reelin deficiency and displacement of mature neurons, but not neurogenesis, underlie the formation of granule cell dispersion in the epileptic hippocampus. J Neurosci 26:4701–4713
Hermann BP, Seidenberg M, Bell B (2000) Psychiatric comorbidity in chronic epilepsy: identification, consequences, and treatment of major depression. Epilepsia 41(Suppl 2):S31–S41
Houser CR (1992) Morphological changes in the dentate gyrus in human temporal lobe epilepsy. Epilepsy Res Suppl 7:223–234
Huttmann K, Sadgrove M, Wallraff A, Hinterkeuser S, Kirchhoff F, Steinhauser C, Gray WP (2003) Seizures preferentially stimulate proliferation of radial glia-like astrocytes in the adult dentate gyrus: functional and immunocytochemical analysis. Eur J Neurosci 18:2769–2778
Isackson PJ, Huntsman MM, Murray KD, Gall CM (1991) BDNF mRNA expression is increased in adult rat forebrain after limbic seizures: temporal patterns of induction distinct from NGF. Neuron 6:937–948
Jakubs K, Nanobashvili A, Bonde S, Ekdahl CT, Kokaia Z, Kokaia M, Lindvall O (2006) Environment matters: synaptic properties of neurons born in the epileptic adult brain develop to reduce excitability. Neuron 52:1047–1059
Jessberger S, Nakashima K, Clemenson GD Jr, Mejia E, Mathews E, Ure K, Ogawa S, Sinton CM, Gage FH, Hsieh J (2007a) Epigenetic modulation of seizure-induced neurogenesis and cognitive decline. J Neurosci 27:5967–5975
Jessberger S, Romer B, Babu H, Kempermann G (2005) Seizures induce proliferation and dispersion of doublecortin-positive hippocampal progenitor cells. Exp Neurol 196:342–351
Jessberger S, Zhao C, Toni N, Clemenson GD Jr, Li Y, Gage FH (2007b) Seizure-associated, aberrant neurogenesis in adult rats characterized with retrovirus-mediated cell labeling. J Neurosci 27:9400–9407
Jung KH, Chu K, Kim M, Jeong SW, Song YM, Lee ST, Kim JY, Lee SK, Roh JK (2004) Continuous cytosine-b-D-arabinofuranoside infusion reduces ectopic granule cells in adult rat hippocampus with attenuation of spontaneous recurrent seizures following pilocarpine-induced status epilepticus. Eur J Neurosci 19:3219–3226
Jung KH, Chu K, Lee ST, Kim J, Sinn DI, Kim JM, Park DK, Lee JJ, Kim SU, Kim M et al (2006) Cyclooxygenase-2 inhibitor, celecoxib, inhibits the altered hippocampal neurogenesis with attenuation of spontaneous recurrent seizures following pilocarpine-induced status epilepticus. Neurobiol Dis 23:237–246
Kempermann G, Gast D, Kronenberg G, Yamaguchi M, Gage FH (2003) Early determination and long-term persistence of adult-generated new neurons in the hippocampus of mice. Development 130:391–399
Kempermann G, Kuhn HG, Gage FH (1997) More hippocampal neurons in adult mice living in an enriched environment. Nature 386:493–495
Kim JH, Jang BG, Choi BY, Kwon LM, Sohn M, Song HK, Suh SW (2012) Zinc chelation reduces hippocampal neurogenesis after pilocarpine-induced seizure. PloS one 7:e48543
Kron MM, Zhang H, Parent JM (2010) The developmental stage of dentate granule cells dictates their contribution to seizure-induced plasticity. J Neurosci 30:2051–2059
Kronenberg G, Reuter K, Steiner B, Brandt MD, Jessberger S, Yamaguchi M, Kempermann G (2003) Subpopulations of proliferating cells of the adult hippocampus respond differently to physiologic neurogenic stimuli. J Comp Neurol 467:455–463
Kuhn HG, Dickinson-Anson H, Gage FH (1996) Neurogenesis in the dentate gyrus of the adult rat: age-related decrease of neuronal progenitor proliferation. J Neurosci 16:2027–2033
Laplagne DA, Esposito MS, Piatti VC, Morgenstern NA, Zhao C, van Praag H, Gage FH, Schinder AF (2006) Functional convergence of neurons generated in the developing and adult hippocampus. PLoS Biol 4:e409
Lugert S, Basak O, Knuckles P, Haussler U, Fabel K, Gotz M, Haas CA, Kempermann G, Taylor V, Giachino C (2010) Quiescent and active hippocampal neural stem cells with distinct morphologies respond selectively to physiological and pathological stimuli and aging. Cell Stem Cell 6:445–456
Ma DK, Jang MH, Guo JU, Kitabatake Y, Chang ML, Pow-Anpongkul N, Flavell RA, Lu B, Ming GL, Song H (2009) Neuronal activity-induced Gadd45b promotes epigenetic DNA demethylation and adult neurogenesis. Science (New YorkNY) 323:1074–1077
Mohapel P, Ekdahl CT, Lindvall O (2004) Status epilepticus severity influences the long-term outcome of neurogenesis in the adult dentate gyrus. Neurobiol Dis 15:196–205
Morgan RJ, Soltesz I (2008) Nonrandom connectivity of the epileptic dentate gyrus predicts a major role for neuronal hubs in seizures. Proc Natl Acad Sci U S A 105:6179–6184
Murphy BL, Pun RY, Yin H, Faulkner CR, Loepke AW, Danzer SC (2011) Heterogeneous integration of adult-generated granule cells into the epileptic brain. J Neurosci 31:105–117
Newton SS, Collier EF, Hunsberger J, Adams D, Terwilliger R, Selvanayagam E, Duman RS (2003) Gene profile of electroconvulsive seizures: induction of neurotrophic and angiogenic factors. J Neurosci 23:10841–10851
Overstreet Wadiche L, Bromberg DA, Bensen AL, Westbrook GL (2005) GABAergic signaling to newborn neurons in dentate gyrus. J Neurophysiol 94:4528–4532
Overstreet-Wadiche LS, Bromberg DA, Bensen AL, Westbrook GL (2006) Seizures accelerate functional integration of adult-generated granule cells. J Neurosci 26:4095–4103
Parent JM, Elliott RC, Pleasure SJ, Barbaro NM, Lowenstein DH (2006) Aberrant seizure-induced neurogenesis in experimental temporal lobe epilepsy. Ann Neurol 59:81–91
Parent JM, Lowenstein DH (1997) Mossy fiber reorganization in the epileptic hippocampus. Curr Opin Neurol 10:103–109
Parent JM, Lowenstein DH (2002) Seizure-induced neurogenesis: are more new neurons good for an adult brain? Prog Brain Res 135:121–131
Parent JM, Murphy GG (2008) Mechanisms and functional significance of aberrant seizure-induced hippocampal neurogenesis. Epilepsia 49(Suppl 5):19–25
Parent JM, Tada E, Fike JR, Lowenstein DH (1999) Inhibition of dentate granule cell neurogenesis with brain irradiation does not prevent seizure-induced mossy fiber synaptic reorganization in the rat. J Neurosci 19:4508–4519
Parent JM, Yu TW, Leibowitz RT, Geschwind DH, Sloviter RS, Lowenstein DH (1997) Dentate granule cell neurogenesis is increased by seizures and contributes to aberrant network reorganization in the adult rat hippocampus. J Neurosci 17:3727–3738
Piatti VC, Davies-Sala MG, Esposito MS, Mongiat LA, Trinchero MF, Schinder AF (2011) The timing for neuronal maturation in the adult hippocampus is modulated by local network activity. J Neurosci 31:7715–7728
Piatti VC, Esposito MS, Schinder AF (2006) The timing of neuronal development in adult hippocampal neurogenesis. Neuroscientist 12:463–468
Pierce JP, Melton J, Punsoni M, McCloskey DP, Scharfman HE (2005) Mossy fibers are the primary source of afferent input to ectopic granule cells that are born after pilocarpine-induced seizures. Exp Neurol 196:316–331
Pun RY, Rolle IJ, Lasarge CL, Hosford BE, Rosen JM, Uhl JD, Schmeltzer SN, Faulkner C, Bronson SL, Murphy BL et al (2012) Excessive activation of mTOR in postnatally generated granule cells is sufficient to cause epilepsy. Neuron 75:1022–1034
Raedt R, Boon P, Persson A, Alborn AM, Boterberg T, Van Dycke A, Linder B, De Smedt T, Wadman WJ, Ben-Menachem E et al (2007) Radiation of the rat brain suppresses seizure-induced neurogenesis and transiently enhances excitability during kindling acquisition. Epilepsia 48:1952–1963
Rao MS, Hattiangady B, Shetty AK (2008) Status epilepticus during old age is not associated with enhanced hippocampal neurogenesis. Hippocampus 18:931–944
Ribak CE, Tran PH, Spigelman I, Okazaki MM, Nadler JV (2000) Status epilepticus-induced hilar basal dendrites on rodent granule cells contribute to recurrent excitatory circuitry. J Comp Neurol 428:240–253
Santarelli L, Saxe M, Gross C, Surget A, Battaglia F, Dulawa S, Weisstaub N, Lee J, Duman R, Arancio O et al (2003) Requirement of hippocampal neurogenesis for the behavioral effects of antidepressants. Science (New York NY) 301:805–809
Scharfman HE, Goodman JH, Sollas AL (2000) Granule-like neurons at the hilar/CA3 border after status epilepticus and their synchrony with area CA3 pyramidal cells: functional implications of seizure-induced neurogenesis. J Neurosci 20:6144–6158
Scharfman HE, Gray WP (2007) Relevance of seizure-induced neurogenesis in animal models of epilepsy to the etiology of temporal lobe epilepsy. Epilepsia 48(Suppl 2):33–41
Scharfman HE, McCloskey DP (2009) Postnatal neurogenesis as a therapeutic target in temporal lobe epilepsy. Epilepsy Res 85:150–161
Scharfman HE, Sollas AE, Berger RE, Goodman JH, Pierce JP (2003) Perforant path activation of ectopic granule cells that are born after pilocarpine-induced seizures. Neuroscience 121:1017–1029
Seress L (1992) Morphological variability and developmental aspects of monkey and human granule cells: differences between the rodent and primate dentate gyrus. Epilepsy Res Suppl 7:3–28
Seress L, Pokorny J (1981) Structure of the granular layer of the rat dentate gyrus. A light microscopic and Golgi study. J Anatomy 133:181–195
Seri B, Garcia-Verdugo JM, Collado-Morente L, McEwen BS, Alvarez-Buylla A (2004) Cell types, lineage, and architecture of the germinal zone in the adult dentate gyrus. J Comp Neurol 478:359–378
Shapiro LA, Figueroa-Aragon S, Ribak CE (2007) Newly generated granule cells show rapid neuroplastic changes in the adult rat dentate gyrus during the first five days following pilocarpine-induced seizures. Eur J Neurosci 26:583–592
Shapiro LA, Korn MJ, Ribak CE (2005) Newly generated dentate granule cells from epileptic rats exhibit elongated hilar basal dendrites that align along GFAP-immunolabeled processes. Neuroscience 136:823–831
Shapiro LA, Ribak CE (2006) Newly born dentate granule neurons after pilocarpine-induced epilepsy have hilar basal dendrites with immature synapses. Epilepsy Res 69:53–66
Sibbe M, Haussler U, Dieni S, Althof D, Haas CA, Frotscher M (2012) Experimental epilepsy affects Notch1 signalling and the stem cell pool in the dentate gyrus. Eur J Neurosci 36:3643–3652
Snyder JS, Choe JS, Clifford MA, Jeurling SI, Hurley P, Brown A, Kamhi JF, Cameron HA (2009) Adult-born hippocampal neurons are more numerous, faster maturing, and more involved in behavior in rats than in mice. J Neurosci 29:14484–14495
Suh H, Consiglio A, Ray J, Sawai T, D'Amour KA, Gage FH (2007) In vivo fate analysis reveals the multipotent and self-renewal capacities of Sox2+ neural stem cells in the adult hippocampus. Cell Stem Cell 1:515–528
Tashiro A, Makino H, Gage FH (2007) Experience-specific functional modification of the dentate gyrus through adult neurogenesis: a critical period during an immature stage. J Neurosci 27:3252–3259
Teixeira CM, Kron MM, Masachs N, Zhang H, Lagace DC, Martinez A, Reillo I, Duan X, Bosch C, Pujadas L et al (2012) Cell-autonomous inactivation of the reelin pathway impairs adult neurogenesis in the hippocampus. J Neurosci 32:12051–12065
Thind KK, Ribak CE, Buckmaster PS (2008) Synaptic input to dentate granule cell basal dendrites in a rat model of temporal lobe epilepsy. J Comp Neurol 509:190–202
Thind KK, Yamawaki R, Phanwar I, Zhang G, Wen X, Buckmaster PS (2010) Initial loss but later excess of GABAergic synapses with dentate granule cells in a rat model of temporal lobe epilepsy. J Comp Neurol 518:647–667
Toni N, Laplagne DA, Zhao C, Lombardi G, Ribak CE, Gage FH, Schinder AF (2008) Neurons born in the adult dentate gyrus form functional synapses with target cells. Nat Neurosci 11:901–907
Toni N, Teng EM, Bushong EA, Aimone JB, Zhao C, Consiglio A, van Praag H, Martone ME, Ellisman MH, Gage FH (2007) Synapse formation on neurons born in the adult hippocampus. Nat Neurosci 10:727–734
Tozuka Y, Fukuda S, Namba T, Seki T, Hisatsune T (2005) GABAergic excitation promotes neuronal differentiation in adult hippocampal progenitor cells. Neuron 47:803–815
Umemori H, Linhoff MW, Ornitz DM, Sanes JR (2004) FGF22 and its close relatives are presynaptic organizing molecules in the mammalian brain. Cell 118:257–270
van Praag H, Christie BR, Sejnowski TJ, Gage FH (1999) Running enhances neurogenesis, learning, and long-term potentiation in mice. Proc Natl Acad Sci U S A 96:13427–13431
van Praag H, Schinder AF, Christie BR, Toni N, Palmer TD, Gage FH (2002) Functional neurogenesis in the adult hippocampus. Nature 415:1030–1034
van Praag H, Shubert T, Zhao C, Gage FH (2005) Exercise enhances learning and hippocampal neurogenesis in aged mice. J Neurosci 25:8680–8685
von Campe G, Spencer DD, de Lanerolle NC (1997) Morphology of dentate granule cells in the human epileptogenic hippocampus. Hippocampus 7:472–488
Walter C, Murphy BL, Pun RY, Spieles-Engemann AL, Danzer SC (2007) Pilocarpine-induced seizures cause selective time-dependent changes to adult-generated hippocampal dentate granule cells. J Neurosci 27:7541–7552
Warner-Schmidt JL, Duman RS (2007) VEGF is an essential mediator of the neurogenic and behavioral actions of antidepressants. Proc Natl Acad Sci U S A 104:4647–4652
Waterhouse EG, An JJ, Orefice LL, Baydyuk M, Liao GY, Zheng K, Lu B, Xu B (2012) BDNF promotes differentiation and maturation of adult-born neurons through GABAergic transmission. J Neurosci 32:14318–14330
Wood JC, Jackson JS, Jakubs K, Chapman KZ, Ekdahl CT, Kokaia Z, Kokaia M, Lindvall O (2011) Functional integration of new hippocampal neurons following insults to the adult brain is determined by characteristics of pathological environment. Exp Neurol 229:484–493
Yu TS, Zhang G, Liebl DJ, Kernie SG (2008) Traumatic brain injury-induced hippocampal neurogenesis requires activation of early nestin-expressing progenitors. J Neurosci 28:12901–12912
Zhan RZ, Timofeeva O, Nadler JV (2010) High ratio of synaptic excitation to synaptic inhibition in hilar ectopic granule cells of pilocarpine-treated rats. J Neurophysiol 104:3293–3304
Zhang W, Huguenard JR, Buckmaster PS (2012) Increased excitatory synaptic input to granule cells from hilar and CA3 regions in a rat model of temporal lobe epilepsy. J Neurosci 32:1183–1196
Zhang W, Yamawaki R, Wen X, Uhl J, Diaz J, Prince DA, Buckmaster PS (2009) Surviving hilar somatostatin interneurons enlarge, sprout axons, and form new synapses with granule cells in a mouse model of temporal lobe epilepsy. J Neurosci 29:14247–14256
Zhao C, Teng EM, Summers RG Jr, Ming GL, Gage FH (2006) Distinct morphological stages of dentate granule neuron maturation in the adult mouse hippocampus. J Neurosci 26:3–11
Author information
Authors and Affiliations
Corresponding authors
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer Science+Business Media New York
About this chapter
Cite this chapter
Althaus, A.L., Parent, J.M. (2014). Role of Adult Neurogenesis in Seizure-Induced Hippocampal Remodeling and Epilepsy. In: Junier, MP., Kernie, S. (eds) Endogenous Stem Cell-Based Brain Remodeling in Mammals. Stem Cell Biology and Regenerative Medicine. Springer, Boston, MA. https://doi.org/10.1007/978-1-4899-7399-3_5
Download citation
DOI: https://doi.org/10.1007/978-1-4899-7399-3_5
Published:
Publisher Name: Springer, Boston, MA
Print ISBN: 978-1-4899-7398-6
Online ISBN: 978-1-4899-7399-3
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)