Abstract
Sex/gender plays an important role when it comes to health and illness or health care utilization. It is well known that women and men differ in regard to their well-being, their morbidity and also in their longevity. In most countries of the world, the life expectancy of women exceeds the life expectancy of men. These differences depend on a country’s context and are smallest in low-income countries with 1–2 years, and highest in so-called transitioning countries with 8–10 years. In Europe, the gender differences in life expectancies range from 4–7 years; in Germany, women currently reach an average of 82.5 years and men 77.5 years (gender difference = 5 years) (reference period 2008/2010; Statistisches Bundesamt 2012).
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Mental Health Care
- Health Care Utilization
- Disease Management Program
- Statutory Health Insurance
- Integrate Health Care
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Sex/gender plays an important role when it comes to health and illness or health care utilization. It is well known that women and men differ in regard to their well-being, their morbidity and also in their longevity. In most countries of the world, the life expectancy of women exceeds the life expectancy of men. These differences depend on a country’s context and are smallest in low-income countries with 1–2 years, and highest in so-called transitioning countries with 8–10 years. In Europe, the gender differences in life expectancies range from 4–7 years; in Germany, women currently reach an average of 82.5 years and men 77.5 years (gender difference = 5 years) (reference period 2008/2010; Statistisches Bundesamt 2012).
There are many reasons for this so-called gender gap . Verbrugge (1985), one of the first authors who provided a comprehensive list of explanatory factors, differentiated these as follows:
-
1.
Biological risks, defined as sex-related intrinsic differences in women and men due to their genes or reproductive physiology.
-
2.
Acquired risks specified as gender differences in living conditions, life styles and health behaviour.
-
3.
Psychosocial aspects of symptoms and care defined as gender differences in the “perception of symptom severity, readiness to tale curative action, and ability to do so” (p. 165).
-
4.
Health-reporting behaviour specified as gender differences in the openness and the ability to talk about health problems with other persons or professionals.
-
5.
Prior health care and caretakers as causes covers gender differences in the utilization (including made experiences) and satisfaction with the health care system.
This explanatory framework has proved to be a valuable tool in describing gender differences within and between countries. Taking current research findings into account (Luy 2011), it seems that environmental risks and therein health behaviour contribute most to the observed gender gap.
Interestingly, in Verbrugge’s framework , two of the risks factor categories are directly related to the health care system and to health care utilization. There are few studies showing that women and men differ in number of physician contacts and in their health-reporting behaviour. It seems that women are more likely to talk about their well-being and their health status with other people and with health professionals than men. This can be partly explained by gender differences in subjective health concepts where women include well-being as an important component of health, whereas men describe their health more in the sense of functioning.
That the health care system is not gender neutral has been shown in many studies. Older studies have identified a medicalisation of women’s body, especially with regard to their reproductive health (see for overview: Maschewsky-Schneider 1997; Kuhlmann & Kolip 2005; Babitsch, Ducki & Maschewsky-Schneider 2011). At that time, the grassroots women’s health movement and feminist scholars worked together to simultaneously provide evidence designed to emphasize the need for changing the health care system into a more women-friendly one. Current studies have focused mainly on gender bias in the health care system and have identified many problems in regard to diagnosis and therapy, with women being more often disadvantaged compared to men (Rieder & Lohff 2008). One reason, besides many others, is that gender stereotypes on the side of the health care providers, as well as on the side of patients, could lead to a false interpretation of symptoms, as some experimental studies have shown (von dem Knesebeck et al. 2008, 2010). Examples are the diagnoses of myocardial infarction in younger women or depression in men.
The aim of this chapter is to identify gender differences in health care utilization . Due to the huge differences in living circumstances, as well as in health care systems around the world, this chapter will focus on the situation in Europe, and Germany will serve as a case study. Given the complexity of sex/gender influences on health and health care utilization, the explanatory model provided by Verbrugge (1985) will be used as an analytic framework for exploring sex/gender differences in the use of health services. Furthermore, to describe the process of health care utilization, the behavioural model of health care use developed by Andersen and colleagues (Andersen 1995; Anderson & Davidson 2001) will be used (see, for details, 2 by von Lengerke et al.) and, based on that concept, enabling, predisposing and need factors will be identified. Accordingly, this chapter includes: (1) a brief description of women and men’s health in Europe with a particular focus on Germany, (2) the results of a systematic review, (3) an exemplary description of health care utilization in Germany, and (4) a summary and a discussion of gender differences in health care utilization.
Women and Men’s Health in Europe
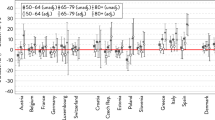
Compared to other regions of the world, the life expectancy in Europe is high, although huge differences can be observed between European countries (see Fig. 7.1). Women in France have the highest average life expectancy with 84.4 years, while the lowest can be found in women in Turkey with 75.3 years (difference = 9.1 years). The findings are different in men, where men in Switzerland have the highest life expectancy with 79.1 years and Lithuanian men the lowest with 65.1 years (difference = 14 years). The European average life expectancy is 80.8 years in women and 74.3 years in men. Due to its relatively high life expectancy in both genders, Germany ranks in the upper third among European countries.
Highest and lowest life expectancy at birth in Europe, by gender, 2005–2007. (OECD 2010)
The total mortality rates match with the presented life expectancy and highlight the huge differences between European countries. The average total mortality rate in Europe is 696 per 100,000 inhabitants, whereas the gender-specific average rates are 534 per 100,000 inhabitants in women and 912 per 100,000 inhabitants in men. The lowest total mortality rate can be found in Switzerland and the highest in Lithuania. The smallest gender difference exists in Iceland and the biggest in Lithuania, where the total mortality rate is nearly double in men compared to women. The main causes of death in Europe are cardiovascular diseases and cancer (see Fig. 7.2). The death rates in men are higher in all presented diseases. In Germany, the death rates attributable to these diseases are lower compared to the European average.
An important indicator for health is the self-reported health status. In general, Europeans perceive their health status as being fairly good (OECD 2010), but again with huge differences between countries. Two-thirds of the European population stated that their health is good or very good and one-third indicated that they have a long-standing illness or health problem. In regard to the self-reported health status, Switzerland ranks first and Latvia ranks last. Germany is slightly below the European average, with 65 % of its inhabitants reporting their health to be good or very good.
Results of a Systematic Review on Gender Differences in Health Care Utilization in Europe
A systematic review was conducted to investigate gender differences in health care utilization in Europe. The literature search was conducted in July 2011 (last search on 27 July 2011) and updated on 24 January 2012. The search strategy (see Fig. 7.3) aimed at retrieving articles reporting on gender and health care utilization in the European context between 2009 and 2012. Due to the huge number of hits the initially defined time frame from 1998 to 2011 was reduced respectively. PubMed was used as the research database.
The selection of eligible articles was conducted in three steps: firstly, based on the title, secondly, based on abstracts and thirdly, based on the full-text publication. In all steps, two researchers (BB and DG) independently screened the publication and included/excluded articles according to a catalogue of a priori set criteria. In cases of disagreement, the selection was discussed and finally a concerted decision was met. In the first round (selection by title), 22 potentially relevant studies were identified.
The following criteria were applied:
Inclusion criteria:
-
Studies related to health care utilization or access to care and gender.
-
Studies published between 2009 and 2012.
-
Studies on adults.
Exclusion criteria:
-
Studies not primarily related to health care, health care utilization, or access to care.
-
Focus on health system research, intervention studies, medical/therapy study, screening, etc.
-
Focus on specific health problems or areas such as human immunodeficiency virus (HIV), cancer, dental health, etc.
-
Specific study population (e.g., disabled, aging people, military personnel, gardeners).
-
Studies not conducted in Europe.
-
Studies on children.
In the second step (selection by abstract), eight potentially relevant studies were selected. At this stage, further exclusion criteria were introduced since some studies appeared to be too specific and not comparable to other contexts or target groups.
Additional exclusion criteria:
-
Focus on ethnicity, financing, health politics, and social support.
-
Focus on a specific health care sector (out-of-hours service, walk-in centre).
-
Studies on the long-term care of elderly people.
Finally, four studies were selected after reading the fulltext. These articles made up the database for the results section.
Results
An overview of the selected publications is presented in Table 7.1. The studies were published in 2008 (ten Have et al. 2008), 2009 (Gerritsen & Devillé 2009) and in 2010 (Doherty & Kartalova-O’Doherty 2010; Gudmundsdottir & Vilhjalmsson 2010). The countries covered were Ireland (Doherty & Kartalova-O’Doherty 2010), the Netherlands (Gerritsen & Devillé 2009), Iceland (Gudmundsdottir & Vilhjalmsson 2010), and one study referred to the situation in more than one European country (ten Have et al. 2008). All publications included a representative sample of the general population; in addition, one article (Doherty & Kartalova-O’Doherty 2010) included subsamples of the four largest immigrant population groups. All studies included both women and men, and all study participants were older than 18 years. In regard to the health care system, two of the selected publications (Doherty & Kartalova-O’Doherty 2010; Gudmundsdottir & Vilhjalmsson 2010) focused on ambulatory care; one (Gerritsen & Devillé 2009) considered all sectors and the other did not specify any sector of the health care system (ten Have et al. 2008). Three of the publications deal with mental health problems (Doherty & Kartalova-O’Doherty 2010; Gudmundsdottir & Vilhjalmsson 2010; 4) and one focused explicitly on gender and ethnicity in health care utilization. All articles are based on nationally representative studies and applied quantitative methods. In one study (Gudmundsdottir & Vilhjalmsson 2010), Andersen’s behavioural model of health service use was adopted as theoretical background.
Gender differences in health care utilization were found in all studies, indicating higher rates of use in women compared to men (Doherty & Kartalova-O’Doherty 2010; Gerritsen & Devillé 2009; Gudmundsdottir & Vilhjalmsson 2010; ten Have et al 2008). Against the background of Andersen’s behavioural model of health services utilization , Gudmundsdottir and Vilhjalmsson (2010) investigated predictors of outpatient help seeking for psychological distress. They used a random national sample of Icelandic adults and focused on four different forms of distress. Besides gender, other socio-demographic variables such as age and marital status were included. health care utilization was more frequent in women compared to men. In detail, the findings showed a greater total utilization rate in women, as well as more visits to physicians and complementary and alternative medicine (CAM) providers. After controlling for symptoms, the observed gender differences were reduced, but still significant.
Doherty & Kartalova-O’Doherty (2010) showed that the prevalence of self-reported mental health problems was higher in women than in men (59.4 % vs. 40.6 %) and women were more likely to have contacted their general practitioner (GP) for such problems in the previous year compared to men (63.2 % vs. 54.2 %). Additionally, in this study, socio-demographic and psychosocial variables were used as predictors of seeking help from GPs. More of the variables included in the regression model became significant in men than in women. Limitations in social activities were the only significant predictor that increased the probability of help seeking in women. In men, self-reported embarrassment was the strongest predictor. Also, some limitations in physical activities and being married/cohabitating increased men’s help-seeking behaviour, whereas secondary education decreased their likelihood to contact a GP. These findings demonstrate that different reasons for seeking help are effective in women and men, seemingly in close connection to societal gender roles.
Reasons for mental health care seeking were also investigated by ten Have et al. (2008). Based on the European Study of Epidemiology of Mental Disorders (ESEMeD), representative data from six European countries (Belgium, France, Germany, Italy, the Netherlands and Spain) were analysed. Female gender increased the probability of accessing mental health care. Other significant predictors were being younger than 65 years of age, higher income and living in Spain or Italy. Women indicated more often than men that they would feel comfortable talking about personal problems. Participants who already had experience with using mental health services were more likely to seek help when faced with a serious health problem and they believed more often that professional help is effective compared to participants without any experiences. These attitudes are significantly associated with health services use. General health care was more likely to be utilized by participants who were open to using professional help in case of a serious emotional problem (ARR = 1.34) and who felt comfortable talking about personal problems (ARR = 1.22). These two attitudes also showed the strongest association to mental health care use (ARR = 2.97 and ARR = 1.88, respectively). Furthermore, the adjusted relative risk ratio was 1.62 for the perceived effectiveness of professional help and 1.31 for feeling embarrassed if friends knew about one receiving professional help. Unfortunately, no gender differentiation of these findings was provided.
The only selected study which is not related to mental health was published by Gerritsen and Devillé (2009). They analysed gender and ethnic differences in health and health care utilization based on data from the second Dutch National Survey of General Practice . Compared to native men, native women reported a poorer health status and consequently used general practice services, physiotherapy, ambulatory mental health care and over-the-counter medication more often. No gender differences were found in this group regarding outpatient medical specialist visits, hospitalization and the use of prescribed medication. However, use of these health services differed between men and women in the four selected immigrant groups (Morocco, Netherlands Antilles, Turkey and Surinam). Although immigrant women assessed their health status similarly to native women (except Netherlands Antilles), a higher utilization among the former group was only found for few health services. Moroccan and Antillean women visited GPs more often than their male counterparts. Turkish women were more often hospitalized than Turkish men and Moroccan women had more contacts to ambulatory mental health care than Moroccan men.
Summary
Against the background of Andersen’s behavioural model, the presented studies included mainly predisposing factors (see Table 7.2). As indicated by our search strategy, gender was considered as a horizontal dimension influencing all factors specified in the model. Only one publication (Gudmundsdottir &Vilhjalmsson 2010) explicitly used the Andersen model as its explanatory framework.
The presented studies showed influences in help seeking and health care utilization taking the above-mentioned variables into account. All studies showed a higher utilization rate in women compared to men, which can only partly explained by gender differences in morbidity (need factors) and also by the predisposing and enabling factors. Most commonly used variables were age, marital status and education as predisposing factors and income as an enabling factor. Interestingly, the study conducted by Doherty & Kartalova-O’Doherty (2010) revealed more influencing factors in men compared to women. Referring back to the Verbrugges’ explanatory framework it seems very likely that on the one side health-reporting behaviour (ten Have et al. 2008) and on the other side former experiences with the health care system (Doherty & Kartalova O’Doherty 2010) contribute to the observed gender differences in health care utilization (see also Gudmundsdottir & Vilhjalmsson 2010).
As three of four articles focused on mental health, the generalization of these findings is limited. However, the frequent focus on mental health care illustrated in our chapter might point to an area of increased gender differences in health service utilization.
Health Care Utilization in Germany—Selected Examples Regarding Contextual Factors
A special focus is put in the following section on Germany, which serves as a case sample to highlight the influence of sex/gender on the process of health care utilization. This allows—as having a defined context—a deeper insight into existing gender differences and similarities. Exemplified on three different areas of the health care system, disease management programmes (DMPs) including guidelines, managed care and cardiovascular diagnostic procedures (intracardiac catheter), the inclusion of gender into political considerations and into decision-making is considered. It will be worked out, if the decisions met influence health care utilization and contribute to a reduction of gender inequality in health care or are provoking the contrary. Other areas of health care delivery where gender differences have been explored intensively, such as preventive programmes, were not taken into account (see, for further details, Chap. 16).
Gender and Health Care Utilization: Current Findings
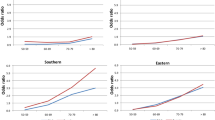
Representative data on health and health care utilization were provided in health reports published by the Robert Koch Institute (RKI). In outpatient care the current data from the German Health Update (GEDA) survey 2010 confirmed—as shown in previous studies—a higher utilization of outpatient health care in women compared to men (RKI 2012; see Fig. 7.4). Overall, the percentage of women who had a physicians’ appointment (GP or specialist) in the last year was higher(91.9 %)than men (84.9 %). The observed gender differences are decreasing with age and are consequently most pronounced in the younger age groups (18–44 years; difference around 10 %).The authors argue that probably one reason for the larger gender differences in the younger groups is the routine consultation of a gynaecologist. However, Thode et al. (2005) revealed in a detailed analysis of representative data, that even taking differences in morbidity as well as the utilization of gynaecologist into account, gender differences were reduced but still remain.
Gender differences in physician contacts during last year. (GEDA 2010; RKI 2012)
Gender Differences in Health Care Utilization: Three Examples
Disease Management Programs (DMP)
In 2000, national disease management programs for selected chronic diseases were introduced into the German health care system. The aim was to improve the quality and effectiveness of outpatient care for chronic ill persons. DMPs are structured and integrated health care programs, in which 1) therapeutic decisions are based on evidence-based clinical practice and treatment guidelines, 2) cooperation among the involved health care professionals (not only medical doctors) are strengthened and 3) patients are educated and involved in the therapeutic process. The participation of health insurance beneficiaries is voluntary. The evaluation and monitoring of DMPs is required by law and hence an obligatory part of the program (BVA 2011). Sex/gender is one of the evaluation criteria referring to participants in the program. As a consequence, the database only allows comparisons between the programs offered by different statutory health insurances, but not between patients enrolled in DMP programs and patients continuing their treatment in regular outpatient care. This would require additional studies. To date, DMP programs are implemented for: type 1 and 2 diabetes, breast cancer, coronary heart disease, asthma bronchiale and chronic obstructive pulmonary disease (COPD). In September 2011, 10893 programmes with more than 5.9 mio. enrolled health insurance beneficiaries or 6.8 mio. participants were accredited (BVA 2011). The data from one statutory health insurance (AOK) show the following participation rates in women and men (Lente 2011):
DMP | Women (%) | men (%) |
|---|---|---|
Diabetes mellitus Type 2 | 56.5 | 43.4 |
Coronary heart disease | 41.3 | 58.7 |
The interpretation of these data, as well as drawing conclusions on the adequacy and gender-equity of the health care system is difficult due to the following reasons:
-
The data focus on all DMP participants and therefore they do not recognize differences in prevalence rates, nor in indication-specific need;
-
No statement can be made regarding the appropriateness and effectiveness of these programs from a gender perspective in the absence of a comparison to regular treatment;
-
No research has been conducted on reasons for different participations rates, e.g. interventions provided by the attending physician or by the statutory health insurance;
-
It has to be examined whether key components of DMPs such as evidence-based guidelines, training programs, etc., are equally appropriate for women and men, and thus developed and implemented in a gender-sensitive manner (Kuhlmann & Kolip 2005).
Some of these issues were addressed in additional studies, such as ELSID or the KORA study (see Chap. 12). In the ELSID study (Evaluation of a large scale implementation of disease management programs for patients with type 2 diabetes) on diabetic patients insured by the AOK Saxony-Anhalt and Rhineland-Palatinate, DMP was compared with regular care. The analysis showed that the 2-year mortality rate was lower in DMP participants compared to non-participants and the prescription rates for antihypertensives and antilipemics were higher in DMP participants; in contrast, differences in health-related quality of life between participants and non-participants were not clear (Lente 2011, p. 74-77). All in all, the authors came to the conclusion that DMPs have a positive effect. However, the question if this kind of treatment leads to the provision of appropriate and gender-equitable health care for women and men was not assessed based on the available data and remains unanswered.
Integrated health care and medical centers
To reduce problems which often occur in Germany at the transition between health care sectors, e.g. between outpatient and inpatient care, the establishment of integrated care and medical centers (MVZ) was facilitated by the law on the modernization of statutory health insurance, which was passed in 2004. The implementation process has since been continuously evaluated by the National Association of Statutory Health Insurance Physicians (KBV) through MVZ-surveys. The results of these surveys refer mainly to the numbers of newly founded MVZ and involved physicians with their respective sub-specialities and regional aspects, the participation of other health care providers, financial budgets and means of quality assurance (KBV 2009). Only very limited information is available regarding the users and also the effectiveness of such programs. The KBV conducted one survey with health insurance beneficiaries (KBV 2011). The data analysis was stratified by sex/gender, but the general focus lies only on physician consults rather than on the use of medical centers (KBV 2011). Furthermore, the study conducted by the Gemeinsame Registrierungsstelle (2009) only provides estimations regarding the utilization rate of integrated health care without any gender differentiation.
Participation in ‘Gesundes Kinzigtal Integrated Care’ (GKIC), a regional project of integrated health care developed by two statutory health insurances, is higher in women compared to men: 3,882 men and 4,605 women were enrolled in this program in 2011 (personal communication, Head Office Manager, Nov. 11th, 2011). Only general data are published regarding the participation rates in the provided DMPs, showing that 10.6% of all enrolled participants take part in the DMP for type 2 diabetes, 3.7% in the DMP for coronary heart disease, 1.4% in the DMP for asthma bronchiale and 2.0% in the DMP for COPD (EKIV-Newsletter 3/2011). No information is available for gender. Hence, it has not been investigated so far if both genders profit in the same way from such a project. Such gender-sensitive analyses are not easy to perform and would require considerable additional effort.
Left heart catheterization (coronary angiography)
With the reunification of Germany, the federal government aimed to ensure a uniform health care provision in the old and new federal states. Among other measures, this lead to increased funding for the establishment of left heart catheterization laboratories. The number of such facilities increased by 120% from 1990 to 1999 (SVR-Gesundheit 2001). In 2009, Germany had 830 left heart catheterization laboratories, in which 864,858 left heart catheterizations were performed (Bruckenberg 2010). The advisory council on the assessment of developments in the health care system thus concluded that there was an oversupply of left heart catheterization in Germany compared to other European countries. Moreover, the high number of procedures does not match with the cardiovascular mortality rates in Germany.
In 2009, 65.7% of all cardiac procedures with extracorporeal circulation (ECC) were performed in men and 34.3% in women (Bruckenberg 2010). Minimally invasive diagnostic procedures of the heart carry risks, potential complications being myocardial infarction, cardiac arrhythmias or stroke. Further potential risks are allergic reactions caused by the administration of contrast medium or persistent the puncture site bleeding. Taking these potential complications into account, an oversupply should be avoided. With regard to gender differences many open questions remain, such as:
-
Is there an oversupply of cardiac care in men and, if so, why?
-
Is the higher rate of minimally invasive diagnostic procedures in men legitimate given the 10-year earlier onset of myocardial infarction in men compared to women?
-
Is the provision of cardiac care for women sufficient and adequate?
Conclusion
The concept of gender mainstreaming requires the recognition of gender in all policy aspects and consequences, with the aim of establishing gender equality. Although the federal government adopted gender mainstreaming as a key principle in 1998, the above-mentioned examples showed that gender is not always appropriately considered. Therefore, gender mainstreaming needs to be systematically applied in the health care system, in the provision of health care and in health policy-making. It is problematic when new programs such as DMP consider the patient gender-neutral.
Generally, there are major research gaps in this area, especially on how to ensure that gender is systematically considered in newly developed and implemented health care services.
Summary and Discussion
Although there is enough evidence that women and men differ in health care utilization, it is hardly possible to explain the observed findings. It is quite obvious that health and health care utilization are by itself intricate matters taking sex/gender into account the picture becomes more complex. There are more questions open than answered as shown in both parts of the chapter. Surprisingly, the number of studies explicitly analyzing sex/gender differences in health care utilization is low. In the beginning of the systematic review, we expected much higher number of papers covering this topic. Although we had to reduce the search period due to the overall amount of hits, the number of eligible was rather low.
One main problem which also has been revealed in the examples from Germany is that sex/gender is often treated as a simple variable and, by doing this, the connectedness with other variables, such as education, employment status, income or health beliefs, body awareness and social support, is being disregarded.
Taking this assumption as a prerequisite for doing research there is a huge need for further studies and the (re)-development of theoretical frameworks. As shown for the Andersen’s behavioural model , gender is explicitly regarded as a predisposing factor. Whereas sex can indeed be regarded mainly as a predisposing factor, such a restriction in regard to gender is considered too narrow. Given its association with many other elements of the model, gender should rather be integrated in this explanatory framework as a horizontal dimension.
There is no room in this chapter to illustrate an entire research agenda in this area. But along the main topics most relevant research questions will be presented in the following:
-
1.
Help seeking: How do women and men enter the system of professional health care services? How are the processes of help seeking triggered in women and men? What role do the social and societal network play? How are the gender differences influenced by other diversity attributes?
-
2.
Health care utilization: How can the observed gender differences in health care utilization be explained? Are the existent theoretical frameworks sufficient where are potential shortcomings? How is health care utilization influenced by the gender-related structures and roles in a given society?
-
3.
Experiences with the health care system: How do women and men experience and evaluate the utilized (medical) treatments? How are prior experiences linked with further help seeking and health care utilization in women and men?
Many studies in this field are based on the analysis of secondary data which is in our opinion too restricted to elaborate qualitative differences in health care utilization in women and men. To answer these questions preferential primary studies are required.
References
Andersen, R.M. (1995) Revisiting the behavioral model and access to medical care: does it matter? Journal of Health and Social behavior 36:1–10.
Andersen, R.M., Davidson, P.L. (2001) Improving access to care in America: individual and contextual indicators. In: Andersen RM, Rice TH, Kominski EF, editors. Changing the U.S. health care system: key issues in health services, policy, and management. San Francisco, CA: Jossey-Bass. pp. 3–30.
Babitsch, B., Ducki, A., Maschewsky-Schneider, U. (2011). Geschlecht und Gesundheit. In: Hurrelmann, K., Razum, O., Laaser, U. (Hrsg.): Handbuch für Gesundheitswissenschaften, S. 639–660.
Bruckenberger, E. (2010). Herzbericht 2009. 22. Bericht sektorübergreifende Versorgungsanalyse zur Kardiologie und Herzchirurgie in Deutschland sowie vergleichende Daten aus Österreich und den Schweiz, Hannover.
Bundesversicherungsamt (BVA) (2011). Zulassung der Disease Management Programme (DMP) durch das Bundesversicherungsamt. Bonn.
Doherty, D.T., Kartalova-O’Doherty, Y. (2010). Gender and self-reported mental health problems: Predictors of help seeking from a general practitioner. British Journal of Health Psychology 15:213–228.
Evaluation der Integrierten Versorgung Gesundes Kinzigtal. EKIV-Newsletter 3/2011.
Gemeinsame Registrierungsstelle zur Unterstützung der Umsetzung des § 140d SBG V (2009). Entwicklung der integrierten Versorgung in der Bundesrepublik Deutschland 2004–2008. o.O.
Gerritsen, A.A.M., Devillé, W.L. (2009). Gender differences in health and health care utilisation in various ethnic groups in the Netherlands: a cross-sectional study. BMC Public Health 9:109.
Gudmundsdottir, G., Vilhjalmsson, R. (2010). Group differences in outpatient help-seeking for psychological distress: Results from a national prospective study of Icelanders. Scandinavian Journal of Public Health 38:160–167.
Kassenärztliche Bundesvereinigung (KBV) (2009). MVZ-Survey 2008. Die Strategische Positionierung Medizinischer Versorgungszentren. Berlin.
Kassenärztliche Bundesvereinigung (KBV) (2011). Versichertenbefragung der Kassenärztlichen Bundesvereinigung 2011. Berlin.
Kuhlmann, E. (2010). Gender im Mainstream der Medizin. Wohin geht die Reise? In: Kolip, P., Lademann, J. (Hrsg.). Frauenblicke auf das Gesundheitssystem. Frauengerechte Gesundheitsversorgung zwischen Marketing und Ignoranz (S. 239–255). Weinheim und München: Juventa.
Kuhlmann, E., Kolip, P. (2005). Gender und Public Health. Grundlegende Orientierungen für Forschung, Praxis und Politik. Weinheim und München: Juventa.
Lente, E. J. van (2011). Erfahrungen mit strukturierten Behandlungsprogrammen (DMPs) in Deutschland. In: Günster, C., Klose, J., Schmacke, N. (Hrsg.) Versorgungs-Report 2011. Schwerpunkt: Chronische Erkrankungen (S. 55–83). Stuttgart: Schattauer.
Luy, M. (2011) Ursachen der Geschlechterdifferenz in der Lebenserwartung. Erkenntnisse aus der Klosterstudie [Causes of sex differences in life expectancy. Insights from the cloister study], Swiss Medical Forum (Schweizerisches Medizin-Forum) 11:580–583.
Maschewsky-Schneider, U. (1997): Frauen sind anders krank. Zur gesundheitlichen Lage der Frauen in Deutschland. Weinheim, München: Juventa Verlag.
OECD (2010) Health at a Glance: Europe 2010, OECD Publishing. http://dx.doi.org/10.1787/health_glance-2010-en.
Rieder, A., Lohff, B. (2008). Gender Medizin: Geschlechtsspezifische Aspekte für die klinische Praxis. Wien: Springer Verlag.
RKI—Robert Koch-Institut (Hrsg.) (2012). Daten und Fakten: Ergebnisse der Studie »Gesundheit in Deutschland aktuell 2010«. Beiträge zur Gesundheitsberichterstattung des Bundes. RKI, Berlin.
Sachverständigenrat für die Konzertierte Aktion im Gesundheitswesen (SVR-Gesundheit) (2001). Bedarfsgerechtigkeit und Wirtschaftlichkeit. Band III: Über-, Unter- und Fehlversorgung. Gutachten 2000/2001. Bonn.
Statistisches Bundesamt (2012). https://www.destatis.de/. Accessed: 24. September 2012.
ten Have, M., de Graaf, R., Ormel, J., Vilagut, G., Kovess, V., Alonso, J.—the ESEMeD/MHEDEA 2000 Investigators (2008). Are attitudes towards mental health help-seeking associated with service use? Results from the European Study of Epidemiology of Mental Disorders. Soc Psychiat Epdeimiol 45:153–163.
Thode, N., Bergmann, E., Kamtsiuris, P. et al. (2005) Einflussfaktoren auf die ambulante Inanspruchnahme in Deutschland. Bundesgesundheitsbl—Gesundheitsforsch—Gesundheitsschutz 48:296–306.
Verbrugge, L.M. (1985): Gender and Health: An Update on Hypotheses and Evidence. Journal of Health and Social Behavior 26:156–182.
von dem Knesebeck, O., Bönte, M., Siegrist, J., Marceau, L., Link, C., Arber, S., Adams, A., McKinlay, J. (2008) Country differences in the diagnosis and management of coronary heart disease—a comparison between the US, the UK and Germany. BMC Health Serv Res 8:198.
von dem Knesebeck, O., Gerstenberger, E., Link, C., Marceau, L., Roland, M., Campbell, S., Siegrist, J., de Cruppé, W., McKinlay, J. (2010) Differences in the diagnosis and management of type 2 diabetes in 3 countries (US, UK, and Germany): results from a factorial experiment. Med Care 48:321–6.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer Science+Business Media New York
About this chapter
Cite this chapter
Babitsch, B., Bormann, C., Gohl, D., Ciupitu-Plath, C. (2014). Gender and Utilization of Health Care. In: Janssen, C., Swart, E., von Lengerke, T. (eds) Health Care Utilization in Germany. Springer, New York, NY. https://doi.org/10.1007/978-1-4614-9191-0_7
Download citation
DOI: https://doi.org/10.1007/978-1-4614-9191-0_7
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4614-9190-3
Online ISBN: 978-1-4614-9191-0
eBook Packages: MedicineMedicine (R0)