Abstract
The anatomy of neck arteries, normal variations, and anastomoses between different arteries is discussed in this chapter. All major arteries of the neck originate from the aortic arch via three main vessels: the brachiocephalic trunk, left common carotid (CCA), and left subclavian arteries. The CCA courses superiorly in the neck, anteromedial to the jugular vein and alongside the vagus nerve. CCA typically divides at the level of C3 or C4 vertebral body into internal and external carotid arteries. The cervical segment of the internal carotid artery (ICA) usually does not have branches in the neck, unless there is remnant of carotid-basilar anastomoses such as the hypoglossal artery or proatlantal artery type I. The external carotid artery (ECA) is the smaller branch of the CCA and runs anteromedial to ICA. It has six branches in the neck before entering the parotid gland and divides into two terminal branches: superficial temporal artery and internal maxillary artery. The ECA supplies most of the neck structures, scalp, and meninges. The vertebral artery is usually the first branch of the subclavian artery, running superiorly in the transverse foramen of C6 to C1 with no cervical branches. It then courses between the C1 and foramen magnum and enters intracranial space. There are extensive anastomoses between carotid and vertebral arteries, the knowledge of which is essential to prevent disastrous complications during interventions.
Access provided by Autonomous University of Puebla. Download reference work entry PDF
Similar content being viewed by others
Keywords
- Aortic arch
- Common carotid artery
- Internal carotid artery
- External carotid artery
- Vertebral artery
- External-internal carotid artery anastomoses
- Embryonic carotid-basilar system anastomoses
- Superior thyroid artery
- Ascending pharyngeal artery
- Lingual artery
- Facial artery
- Occipital artery
- Posterior auricular artery
- Superficial temporal artery
- Internal maxillary artery
1 Introduction
In this chapter, the anatomy of the aortic arch and neck arteries is described. The aortic arch configuration and its common variations are reviewed as well as the anatomy of CCA, ECA, cervical ICA, and vertebral artery. The normal variations and anastomoses between different arteries, the knowledge of which is crucial for performing safe catheter angiography, are also discussed. The aim of this chapter is to illustrate the application of anatomical knowledge in clinical practice.
2 Aortic Arch
All major arteries of the neck originate directly or indirectly from the aortic arch. In the standard configuration, the aortic arch gives rise to three great vessels: the brachiocephalic trunk (also termed brachiocephalic or innominate artery), the left common carotid artery, and the left subclavian artery. The brachiocephalic trunk then bifurcates at the level of the right sternoclavicular joint into the right common carotid and the right subclavian arteries (Fig. 1a). This standard branching pattern occurs in approximately 70 % of patients [1, 2].
Branching patterns of the aortic arch. (a) Standard configuration. (b) Common origin of the brachiocephalic trunk and the left common carotid artery. (c) Origin of the left common carotid artery from the brachiocephalic trunk. (d) Arch origin of the left vertebral artery. (e) Bi-innominate artery. (f) Bicarotid trunk. (g) Separate origins of subclavian, common carotid, and vertebral arteries. (h) Aberrant right subclavian artery. R/L-SA right/left subclavian artery, R/L-VA right/left vertebral artery, R/L-CCA right/left common carotid artery
There are many possible anatomical configurations of the aortic arch and its branches. Description of all these variations is beyond the scope of this chapter; in particular, developmental anomalies leading to the formation of right or double aortic arches will be omitted here. The most common anatomical variants, knowledge of which is of paramount importance for performing safe catheter angiography, deserve a brief mention however.
The most frequent anatomical variants are the common origin of the brachiocephalic trunk and the left common carotid artery seen on average in 13 % of population and the origin of the left common carotid artery from the brachiocephalic trunk encountered in 9 % of patients [3, 4]. Both of these variants are more common in blacks (25 % and 10 %, respectively). Instead of arising separately, the left common carotid artery shares the aortic arch origin with the brachiocephalic trunk (Fig. 1b) or arises from the brachiocephalic trunk slightly more cranially (1–2.5 cm distal to its ostium) (Fig. 1c). As a result, only two major vessels ascend from the aortic arch. The common trunk variant, or sometimes both of the above variants, has been referred to as “bovine” arch implying high frequency of such configuration in cattle. In fact, the aortic arch in cows more often gives rise to a single common vessel, and these branching patterns are not specific on any species. Thus, “bovine-type” aortic arch should be avoided as a misnomer and replaced with an anatomical terminology [3, 4].
The arch origin of the left vertebral artery as a fourth separate arch vessel is seen in 0.5 % of patients; in such cases the left vertebral artery most commonly arises between the left common carotid and the left subclavian artery (Fig. 1d) and sometimes distal to the left subclavian artery. Rare variants include the bi-innominate artery (symmetrical right and left innominate arteries each bifurcating into the common carotid and subclavian vessels, Fig. 1e) and bicarotid trunk (bifurcating into the right and left common carotid vessels, with separate origins of subclavian arteries, Fig. 1f). Different combinations in which the neck vessels arise separately from the aortic arch are also encountered, in extreme case giving rise to six aortic arch branches (separate right and left subclavian, common carotid, and vertebral arteries, Fig. 1g) [1, 2].
The most frequent anomaly of the aortic arch seen in 0.4–2 % of population is the aberrant right subclavian artery (Fig. 1h) arising distal to the left subclavian artery and passing to the right side of the mediastinum behind the esophagus causing its typical posterior indentation and dysphagia lusoria [2].
3 Common Carotid Artery
The right and left common carotid arteries (CCA) course superiorly on both sides of the neck lying within the respective carotid space, anteromedial to the internal jugular veins and accompanied by the vagus nerve. The common carotid artery typically divides at the level of C3 or C4 vertebral body into the external carotid artery (ECA) and the internal carotid artery (ICA); this corresponds approximately to the superior border of the thyroid cartilage. Bifurcation can occur as low as T2 and as high as C2. Normally CCA does not have any named cervical branches, but occasionally the vertebral artery or proximal ECA branches can arise from it (Fig. 2) [1].
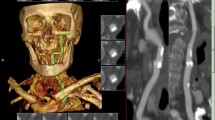
(a) Volume rendering demonstrating the cervical arteries. Common carotid artery (CCA) bifurcates into the internal (ICA) and external (ECA) carotid artery at the level of C4 vertebral body. Note the variant origin of the left common carotid artery from the brachiocephalic trunk. The vertebral artery (VA) enters the transverse canal at C6 level. Note a dominant left vertebral artery with hypoplastic right vertebral artery. (b) Posterolateral view. Distal to the CCA bifurcation, the ICA lies posterior and lateral to the ECA
4 Cervical Internal Carotid Artery
The cervical segment of the ICA (C1) extends from the carotid bifurcation to the skull base where the artery enters the carotid canal transitioning into the petrous (C2) segment. At the bifurcation, the ICA most frequently arises posterolaterally to ECA; its medial origin from CCA is seen in 10–15 % of the population. The most proximal part of the ICA shows a focal dilatation termed the carotid bulb or carotid sinus. Reversal of flow and turbulent flow pattern in this region predispose it to atherosclerotic plaque formation. Ascending cranially, the ICA passes medial to the ECA and lies medial to the internal jugular vein and anterior to the transverse processes of the upper cervical vertebrae. Usually there are no major named branches of the C1 segment of the ICA. Important exceptions include remnants of the carotid-basilar system anastomoses such as persistent hypoglossal artery (arising from the cervical ICA between C1 and C3 and passing through the hypoglossal canal to join the basilar artery) and persistent proatlantal artery type I (proatlantal intersegmental artery, joining the vertebrobasilar system after passing through the foramen magnum) [1].
5 External Carotid Artery
The ECA is the second branch of the CCA, which unlike the ICA has multiple branches in the neck and supplies most of the neck structures. The ECA extends from the carotid bifurcation, usually at the level of the upper border of the thyroid cartilage, and curves anteriorly before inclining backward behind the neck of the mandible. The ECA is anteromedial to the ICA [1]. It gives six main branches in the neck and, after entering the parotid gland, divides into its two terminal branches. In comparison to ICA, it has smaller caliber and rapidly tapers along its course as it gives multiple branches.
The following structures cross the ECA anteriorly: the hypoglossal nerve (CN XII), posterior belly of digastric muscle, stylohyoid muscle and ligament, and facial nerve (CN VII) within the parotid gland, while the pharyngeal wall, superior laryngeal branch of the vagus nerve (CN X), and deep lobe of the parotid gland are posterior to ECA. The pharyngeal branch of the vagus nerve (CN X) and glossopharyngeal nerve (CN IX) are between the ECA and ICA [5].
Branches of ECA
-
1.
The superior thyroid artery is the first branch of ECA, which arises anteriorly and descends to the apex of the thyroid. It supplies the larynx and superior thyroid and anastomoses with the inferior thyroid artery which is a branch of the thyrocervical trunk. The superior thyroid artery may arise from CCA bifurcation (20 %) or have common origin with the lingual artery as thyrolingual trunk (2.5 %) or with both lingual and facial arteries as the thyrolinguofacial trunk (2.5 %). Its main branches are the hyoid artery, sternocleidomastoid branches, superior laryngeal artery, and cricothyroid branch [1, 5].
-
2.
The ascending pharyngeal artery is the smallest branch of the ECA which arises posteriorly near the carotid bifurcation. It is a long vessel that ascends superiorly between the ICA and ECA deeply in the neck [5]. After a short common trunk, it divides into two major branches: anteriorly, the pharyngeal trunk, which is extracranial, and, posteriorly, the neuromeningeal trunk, which is intracranial. The other branches are inferior tympanic and musculospinal arteries. The pharyngeal trunk supplies the nasopharynx, oropharynx, and eustachian tube. The neuromeningeal branches supply the dura, CN IX–XII, and first, second, and third cervical roots. Inferior tympanic and musculospinal branches supply the middle ear and prevertebral muscles, respectively [6]. The ascending pharyngeal artery has several important and potentially dangerous anastomoses with internal carotid, internal maxillary, vertebral, and occipital arteries [6, 7].
-
3.
The lingual artery is the second anterior branch of the ECA. Initially it runs obliquely upward to the hyoid bone. Then it curves downward and forward, forming a loop, which is crossed by the hypoglossal nerve [1]. It passes beneath the digastric and stylohyoid muscles and ascends and courses forward underneath the tongue. It supplies the tongue, oral cavity, and submandibular gland and has four branches: suprahyoid, dorsal lingual, deep lingual, and sublingual arteries. The lingual artery may have common origin with the facial artery (10–20 %) [5].
-
4.
The facial artery originates above the lingual artery. It is sheltered by the ramus of the mandible and courses above the submandibular gland, then curves upward over the body of the mandible, and passes anterosuperiorly across the cheek to the angle of the mouth and nasolabial fold. It then runs toward the inner canthus of the eye and terminates as the angular artery. The facial artery is a very tortuous vessel and supplies the face, lip, palate, and superficial neck [1, 5]. Its cervical branches are the ascending palatine artery, tonsillar, submental, and glandular branches. Branches in the face include inferior and superior labial arteries, inferior alar artery, and lateral nasal branch [8]. The facial artery has anastomoses with the ophthalmic artery, branch of the ICA, and other ECA branches [7, 8].
-
5.
The occipital artery originates from the posterior aspect of the ECA opposite to the facial artery, at the level of the posterior belly of the digastric muscle [1, 5]. It ascends posterosuperiorly between the occiput and C1 in the occipital groove toward the superior nuchal line and then becomes subgaleal and extends up to the vertex. It supplies the scalp, upper cervical musculature, and posterior fossa meninges. Branches of the occipital artery are sternocleidomastoid, auricular, mastoid, descending, and occipital [9]. The occipital artery is a remnant of the embryologic type I and type II proatlantal arteries. It corresponds to C1 and C2 segmental arteries and, therefore, retains extensive connection to the vertebral artery in adulthood [10]. It is critical to understand the type and pattern of anastomoses between occipital and vertebral arteries to avoid any disastrous complications during embolization.
-
6.
The posterior auricular artery arises from the posterior ECA above the occipital artery and opposite to the apex of the styloid process [1]. It ascends posteriorly beneath the parotid and along the styloid process toward the ear. It supplies the pinna, scalp, external auditory canal, and chorda tympani. Common origin of occipital and posterior auricular arteries is seen in 12.5 % [5].
-
7.
The superficial temporal artery is the smaller of the two terminal branches of the ECA. It arises in the parotid gland behind the neck of the mandible and runs superiorly between the deep and superficial lobes of the parotid gland [1]. The transverse facial artery comes off the superficial temporal artery before it leaves the parotid gland. Then the superficial temporal artery passes superficially over the zygomatic process and divides into two branches: frontal and parietal. It supplies the scalp and some parts of the face [11].
-
8.
The internal maxillary artery arises within the substance of the parotid gland behind the mandibular neck. It then runs forward between the ramus of the mandible and sphenomandibular ligament and courses along the pterygoid muscle to the pterygopalatine fossa [5]. The internal maxillary artery is divided into three major parts based on its relationship to the external (lateral) pterygoid muscle. The first (mandibular) section is posterior to the external pterygoid muscle and courses along its lower border giving rise to five branches: the deep auricular artery, anterior tympanic artery, middle meningeal artery, accessory meningeal artery, and inferior alveolar artery. The second (pterygoid or muscular) section is within the pterygoid muscle and runs obliquely forward and upward as well as medially through the infratemporal fossa. Branches arising from this section are entirely muscular including: anterior and posterior deep temporal branches, pterygoid branches, masseteric artery, and buccinator artery. The third section (pterygopalatine) is anterior to the external pterygoid muscle and enters the pterygopalatine fossa. It terminates by sending off six branches to deep facial structures: the posterior superior alveolar artery, infraorbital artery, artery of pterygoid canal, pharyngeal artery, greater palatine artery, and sphenopalatine artery [12].
There are several potential anastomoses between the internal maxillary artery and ICA: in the orbital region, potential collateral route from both proximal and distal internal maxillary arteries to the ophthalmic branch of ICA. In the cavernous-petrous region, the major anastomotic route is between the middle and accessory meningeal arteries and inferolateral trunk of the cavernous ICA [7].
6 External Carotid Artery Anastomoses
There are three main regions of anastomoses between the ECA and ICA and vertebral arteries:
-
1.
Anterior or orbital region: ECA anastomoses through internal maxillary and facial arteries with ophthalmic branch of ICA.
-
2.
Middle or petrocavernous: ECA connects with petrocavernous branches of the ICA via internal maxillary and ascending pharyngeal branches.
-
3.
Posterior or cervical: anastomoses between the ECA and vertebral artery via occipital or ascending pharyngeal arteries [7]. Persistent embryonic connection between the ECA and vertebrobasilar system is called type II proatlantal artery [1, 10].
7 Vertebral Artery
The vertebral artery usually arises as the first branch of the subclavian artery, proximal to the thyrocervical trunk. Less frequent anatomical variations include the vertebral artery originating together with the thyrocervical trunk, from the thyrocervical trunk, from the subclavian artery distal to the thyrocervical trunk, or from the common carotid artery. In its typical course, the vertebral artery courses superiorly and medially to enter the transverse foramen of C6; this part of the vertebral artery is termed an extraosseous segment (V1). The foraminal (V2) segment of the vertebral artery ascends through the transverse foramina of C6 to C1 vertebrae. At the level of the axis, the artery makes a sharp superolateral turn to pass through its obliquely positioned transverse foramen. In the extraspinal (V3) segment between the C1 transverse foramen and foramen magnum, the artery courses medially and posteriorly lying superior to the arch of C1. In the last intracranial segment (V4), the artery pierces the dura and courses superomedially over the clivus to unite with its contralateral counterpart into the basilar artery (Fig. 3) [1].
Volume rendering demonstrating the typical course of the vertebral artery. The segment proximal to the transverse foramen of C6 is termed V1; the segment coursing through the transverse canal from C6 to C1 is termed V2; note a sharp superolateral turn at the C2 transverse foramen. Extraspinal V3 segment stretches from the transverse foramen of C1 to the site at which the artery pierces the dura and enters the cranium
The level at which the vertebral artery enters the transverse foramen is variable and dependent on which embryonic intersegmental artery persists to form the vertebral artery during development. Vertebral arteries often demonstrate variation in size with unilateral (usually left sided) dominance [1]. Cervical branches of the vertebral artery include segmental muscular and spinal branches, often with a single branch to brachial widening of the cervical cord (which can also arise from the thyrocervical or costocervical trunk or superior thyroid artery). In the presence of carotid-basilar anastomoses (persistent hypoglossal artery or proatlantal artery type I from the ICA or proatlantal artery type II from the ECA), the vertebral artery proximal to anastomosis may be hypoplastic or absent.
8 Summary
All major neck arteries originate from the aortic arch. In the standard configuration the aortic arch gives rise to three great vessels: the brachiocephalic trunk, the left common carotid artery, and the left subclavian artery. The most frequent anatomical variants are the common origin of the brachiocephalic trunk and the left common carotid artery (13 %). The common carotid arteries course superiorly on both sides of the neck and divide at the level of C3 or C4 vertebral body into the ECA and ICA. The cervical segment of ICA (C1) extends from the carotid bifurcation to the skull base. At the bifurcation, the ICA most frequently arises posterolaterally to the ECA and then passes medially. Usually there are no major named branches of the C1 segment of the ICA. Important exceptions are persistent hypoglossal artery and proatlantal artery type I as the remnants of the carotid-basilar system anastomoses. The ECA is the smaller branch of the CCA which has six branches in the neck before entering the parotid gland and divides into two terminal branches: superficial temporal artery and internal maxillary artery. The ECA supplies most of the neck structures, scalp, and meninges. The vertebral artery is usually the first branch of the subclavian artery, running superiorly in the transverse foramen of C6 to C1 with no cervical branches. It then courses between the C1 and foramen magnum and enters intracranial space.
There are three main regions of anastomoses between the ECA with ICA and vertebral artery: (1) anterior or orbital region, (2) middle or petrocavernous, and (3) posterior or cervical. Persistent embryonic connection between the ECA and vertebrobasilar system is called type II proatlantal artery. It is very crucial to identify these anastomoses or embryological remnants to prevent disastrous complications during interventions.
References
Harnsberger HR, Macdonald AJ (2006) Diagnostic and surgical imaging anatomy, 1st edn, Brain, head and neck, spine. Amirsys, Salt Lake City
Lippert H, Pabst R (1985) Arterial variations in man: classification and frequency. J F Bergmann, Munchen
Katz JC, Chakravarti S, Ko HH, Lytrivi ID, Srivastava S, Lai WW et al (2006) Common origin of the innominate and carotid arteries: prevalence, nomenclature, and surgical implications. J Am Soc Echocardiogr 19(12):1446–1448
Layton KF, Kallmes DF, Cloft HJ, Lindell EP, Cox VS (2006) Bovine aortic arch variant in humans: clarification of a common misnomer. AJNR Am J Neuroradiol 27(7):1541–1542
Standring S (2011) Gray’s anatomy, 39th edn. Livingstone, Churchill
Hacein-Bey L, Daniels DL, Ulmer JL, Mark LP et al (2002) The ascending pharyngeal artery: branches, anastomoses, and clinical significance. Am J Neuroradiol 23:1246–1256
Geibprasert S, Pongpech S, Armstrong D, Krings T (2009) Dangerous extracranial–intracranial anastomoses and supply to the cranial nerves: vessels the neurointerventionalist needs to know. Am J Neuroradiol 30:1459–1468
Lohn JWG, Penn JW, Norton J, Butler PEM (2011) The course and variation of the facial artery and vein, implications for facial transplantation and facial surgery. Ann Plast Surg 67:184–188
Alvernia JE, Fraser K, Lanzino G (2006) The occipital artery: a microanatomical study. Neurosurgery 58(1 Suppl):114–122
Chen PR, Siddiqui AH, Chen PR (2011) Intracranial arterial collateralization: relevance in neuro-endovascular procedures In: Peres JFP (ed) Neuroimaging for clinicians- combining research and practice. InTech Europe, Rijeka, p 175–202
Pinar YA, Govsa F (2006) Anatomy of superficial temporal artery and its branches: its importance for surgery. Surg Radiol Anat 28:248–253
Kashiwagi N, Nakanishi K, Kozuka T, Sato Y et al (2010) Vascular supply with angio-CT for superselective intra-arterial chemotherapy in advanced maxillary sinus cancer. Brit J Radiol 83:171–178
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer Science+Business Media New York
About this entry
Cite this entry
Sheikh-Bahaei, N., Matys, T., Gillard, J.H. (2016). Anatomy of the Neck Arteries. In: Saba, L., Raz, E. (eds) Neurovascular Imaging. Springer, New York, NY. https://doi.org/10.1007/978-1-4614-9029-6_2
Download citation
DOI: https://doi.org/10.1007/978-1-4614-9029-6_2
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4614-9028-9
Online ISBN: 978-1-4614-9029-6
eBook Packages: MedicineReference Module Medicine