Abstract
Trainees must have excellent clinical reasoning skills to practice medicine safely and effectively. Even when a trainee has an impressive knowledge base, he or she can have difficulty applying that knowledge to patient problems. In this chapter, the authors discuss how the cognitive processes involved in decision-making apply in medicine. They propose a framework for how educators can teach and model decision-making to medical trainees based on the literature and their extensive experience with novice clinicians. They propose that learners should manifest progress of clinical reasoning in four ways: (1) an improved ability to develop and share a concise verbal or written problem representation; (2) an increasing and consistent use of semantic qualifiers; (3) the ability to state, seek, identify, and recall the defining and discriminating features of a patient’s history and physical exam and link this to their knowledge base of “illness scripts” and (4) demonstrate an increasing metacognitive awareness which reduces cognitive biases in patient evaluations. They provide detailed descriptions of an array of strategies to address immature clinical reasoning.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Introduction
Physicians must have sound clinical reasoning that consistently leads to accurate diagnosis. Ensuring that trainees develop this complex skill is a foundational focus of medical education. Students begin by accumulating a medical science knowledge base, through a curriculum, which at most US medical schools is organized in organ- or system-based modules. However, patients present with symptoms and complaints, not organ- or system-based diseases. Clinical students must synthesize and interpret this problem-based information gathered from patients and learn to make a diagnosis. As medical educators we have a responsibility to our trainees and our patients to teach and assess clinical reasoning and be equipped with remediation strategies for use when the need arises.
The 1999 Institute of Medicine report To Err is Human estimated that up to 98,000 preventable deaths of hospitalized patients occur annually [1]. Initially, it was concluded that the majority of medical errors responsible for bad outcomes were the result of “faulty systems, processes, and conditions that lead people to make mistakes or fail to prevent them.” Of late, diagnostic failure and misdiagnosis harm has been considered the next frontier of patient safety. Recent data have shown that 40,000–80,000 deaths related to misdiagnosis occur annually in the USA, and an estimated 5 % of autopsies demonstrate errors for which expedient diagnosis and treatment might have saved the patient. It is therefore imperative that diagnostic decision-making must be explicitly taught and modeled for physician trainees—in order to minimize these errors and enhance the safety of our patients [2].
In this chapter we will first selectively review research-informed conceptual models relevant to teaching, assessing, and remediating clinical decision-making. These will touch on the predominant human cognitive process related to reasoning and problem solving, how medical knowledge is organized, and common cognitive dispositions to respond (CDR’s) which can trip up even the most experienced clinicians. Then we will propose criteria to assess normal development of clinical reasoning, describe two of the most common ways novices tend to struggle and share road-tested strategies to work with these learners to get them back on course.
2 How Humans Think: Dual Process Theory
There has been much interest in human information processing and decision-making. While clearly complex, decades of cognitive psychology research have given us some models, theories, and basic principles to guide us in teaching and assessing the reasoning of our trainees [3].
To start off, this work has demonstrated two distinct systems involved in decision-making—the fast, unconscious, highly efficient, yet error prone System 1 and the slow, effortful, analytical, less efficient, yet more reliable System 2.
To understand how this works, consider the following problem and work to solve it as fast as you can:
-
A bat and ball together cost $1.10.
-
The bat costs $1.00 more than the ball.
-
How much does the ball cost? [4]
Chances are at least half of you answered 10 cents. At first glance, the answer 10 cents certainly makes intuitive sense, however, on closer inspection the math just doesn’t add up. If the ball cost 10 cents and the bat was $1 more, then it alone would cost $1.10 and together the items would cost $1.20. In order to satisfy the stipulations of the question, the ball must cost 5 cents. The bat would then cost $1.05 and together they cost $1.10. Kahnemann and Frederick delivered this question and two others as part of a Cognitive Reflection Test (CRT) to thousands of subjects—many of whom were students at elite US universities. Fewer than 50 % of those subjects answered the questions correctly. Why? Because System 1 operates quickly and unconsciously, relies on patterns or shortcuts—and is often wrong.
Now, consider and solve the following problem:
Likely, for this problem you set down to crunch some numbers. Perhaps you began with a rough estimate—less than 1,000 but more than 250—and then settled into some mental effort to arrive at the answer, 408. This process illustrates the work of System 2, which allocates attention to effortful mental activities—such as calculations. System 2 processes can be painstaking and time-consuming, but it’s a highly reliable system and less error-prone than its counterpart System 1. An awareness of these two systems and their interplay is helpful when discussing cognitive models of clinical reasoning.
The dual-process theory blends hypothetico-deductive strategies (described below) and intuitive reasoning and implies that both systems are jointly involved in clinical reasoning at all levels of expertise. Valences shift toward one approach or the other based on a number of factors that relate to the particular problem encountered. Intuitive, or System 1, processes prevail when time is constrained and problems are routine, certain, and easily recognized. Analytic, or System 2, processes dominate when time permits, stakes are high, and problems are complex or unfamiliar. There is some evidence to show that novices primed to employ both System 1 and System 2 in their diagnostic decision-making may achieve the greatest diagnostic accuracy [5].
3 Models of Clinical Diagnostic Reasoning
The past 35 years has seen an evolution in the understanding of clinical reasoning and the way doctors think [6]. Elstein, Shulman, and Sprafka’s original work through the Medical Inquiry Project described a hypothetico-deductive or analytic process of clinical reasoning [7]. This method relies upon cycles of data acquisition and the development and testing of hypotheses. The accuracy and quality of this reasoning process is dependent on the amount and organization of prior knowledge and highly influenced by the experience of the clinician or trainee as well as the context in which the patient is being seen. Bowen has lucidly mapped out this process [8] (Fig. 6.1).
Key elements of the clinical diagnostic reasoning process. Reproduced with permission from N Engl J Med, Bowen JL, Educational strategies to promote clinical diagnostic reasoning, 335(21):2217–2225. Copyright © 2006 Massachusetts Medical Society. Reprinted with permission from Massachusetts Medical Society
In order to illustrate Bowen’s model of the clinical diagnostic reasoning process, consider the following case:
-
A 15-month-old male presents during the winter, with a 3-day history of low-grade fever and runny nose. He has now developed a cough and trouble breathing. His mother states that over the past day, he has had episodes of fast breathing, and she notices his belly moving more than usual. He has had one episode of vomiting after a coughing attack and no diarrhea. His immunizations are up to date. He has a 3-year-old sibling who is in daycare. There is no rash. There has been no travel or new exposures.
-
On PE, temperature was 100°F and RR 40/min. Heart rate and BP are within normal range. Oxygen saturation is 91 % on room air. The toddler is quiet in his mother’s arms. There are intercostal retractions. HEENT exam is normal. The heart rhythm is normal, and there are no murmurs. There is good air exchange and wheezing with occasional crackles on lung exam. The abdomen is soft and non-tender. Tone is normal, and there are no focal neurologic findings.
As the patient’s story unfolds, first through the chief complaint and subsequently through history and physical, a clinician forms impressions. The challenge for all clinicians, from novices to experts, is to synthesize the gathered data into a cohesive and accurate abstraction of the case that represents the overall clinical picture. This is referred to as the “problem representation.” Problem representations are summaries or “bullets” that encapsulate and succinctly organize the information about the patient’s presentation and guide clinical reasoning in the development of diagnostic possibilities.
Problem representations for the above case might take myriad forms. The novice may have difficulty in making editorial choices around key elements of the history and physical and not appreciate pertinent positive and negatives associated with the case. What might follow is an overlong problem representation that will merely rehash the history and physical. More experienced trainees will begin to separate wheat from chaff and hone in on elements that will suggest specific disease entities.
An accurate problem representation of this case scenario is as follows:
“A toddler with acute onset of moderate respiratory distress and low-grade fever with diffuse lower respiratory findings on chest exam”
Key for the development of an accurate abstraction of the case is the judicious use of semantic qualifiers or axes. Semantic qualifiers are “paired, opposing descriptors that can be used to compare and contrast diagnostic considerations” [8] (Table 6.1). In this case, “3-day history” became “acute-onset” the respiratory parameters were transformed to “moderate respiratory distress” and the chest exam findings of “good air exchange and wheezing with occasional crackles” became “diffuse lower respiratory findings.”
In this way, the problem representation can ignite clinical memory and activate a search for stored experiential or book knowledge in the form of illness scripts [9, 10]. Illness scripts are mental representations comprised of the following three key elements of a medical condition—first, the enabling conditions or predisposing, epidemiologic features; second, the fault or the relevant pathophysiologic process; and third, the consequences of the fault or the clinical features and sequelae.
The broad features of this case scenario might activate the particular illness scripts of bronchiolitis, croup, and foreign body—all conditions being associated with toddlers in respiratory distress. Clinicians then test this array of diagnostic considerations based on defining or discriminating features (Fig. 6.2). While bronchiolitis, croup, and foreign body aspiration might all produce respiratory distress (defining features), of these three diagnostic possibilities, only bronchiolitis produces respiratory distress with diffuse lower respiratory findings on auscultation (discriminating features).
This clinical reasoning model is an analytic or hypothetico-deductive process. It might also be described as a largely System 2 operation.
In addition to this analytic model of clinical reasoning, there are alternate cognitive functions in play that are non-analytic, rapid, and intuitive.
Consider the following case:
-
A 50-year-old man presents after the eruption of a rash on his chest. The appearance of the rash was preceded by 2–3 days of burning and tingling over the affected area. There has been no fever or associated systemic signs and no new exposures. His exam is notable for an erythematous, vesicular rash in a horizontal, band-like distribution across his left torso over an area that corresponds to the T6 dermatome.
For many physicians, this pattern is immediately recognized and a diagnosis of shingles is rapidly made. The need to consciously develop a problem representation or analyze the case in an iterative process is bypassed and minimal conscious effort is expended. This is a typical System 1 process—rapid, unconscious, efficient, and accurate. Undoubtedly, the ability to recognize this pattern relies on prior experience with similar cases. One might conclude that novices do not have access or rights to this cognitive domain and are bound to the hypothetico-deductive model. Actually, it has been shown that both novices and experts use non-analytic processes to solve clinical problems. In fact, both groups toggle between analytic and non-analytic approaches and, as Eva states, “…the strategy employed by even the most junior medical students is qualitatively indistinguishable from that employed by experienced doctors—both groups generate hypotheses very quickly, presumably based in part on non-analytic reference to past experiences” [11]. The difference between novice and expert, beyond the amount of knowledge and experience, is in the extent to which their knowledge is organized into detailed and accurate illness scripts.
4 Knowledge Organization and Clinical Reasoning
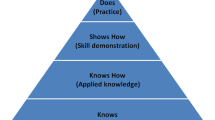
Bordage [12] described four types of knowledge organization in physicians and trainees—reduced, dispersed, elaborated, and compiled, each with its own characteristics and impact on making an accurate diagnosis. For practical reasons, the four levels of organization may be considered as stages of development within a content domain. Learners with:
-
Reduced knowledge have either very limited or inaccessible illness scripts. They are often unable to translate relevant information from a patient’s presentation into meaningful diagnostic categories.
-
Learners with dispersed knowledge possess more abundant illness scripts, but these still tend to be formulaic or static and thus remain difficult to adapt to the dynamic, multisystem presentations of patient care.
-
Elaborated knowledge features improved use of structural semantics and use these relationships to hypothesis test against various diagnoses in their existing, more robust knowledge bases.
-
Compiled learners, often considered expert clinicians, are able to quickly sift through clinical data based on their diversified set of semantics and deep knowledge base. These clinicians often demonstrate rapid pattern recognition and the unique ability to seek missing elements in the case.
Physicians with expert clinical reasoning and compiled knowledge should expend effort with novice learners to discuss how they think through a case - i.e. toggling between System 1 and System 2 - thereby demonstrating both the necessary knowledge and the cognitive connections one needs to become an accurate diagnostician.
It is important to remember that expertise in this domain is influenced more by prior knowledge and clinical experience in the specific domain than by training level. For example, a medical student who has had extensive experience with respiratory illnesses in children may demonstrate compiled knowledge and the ability to reason non-analytically and intuitively with accuracy in this domain but not in others. Critical thinking is the distinguishing characteristic of clinicians who are expert in clinical reasoning across content domains. Such individuals have a habit of being aware of their own thinking and therefore avoid common, dangerous cognitive biases.
5 Metacognition and Cognitive Bias
“Awareness of [cognitive psychology] might accomplish three things. First, it might broaden the list of pitfalls that a clinician can anticipate and possibly avoid. Second, it can provide a language and logic for understanding repeated mistakes. Third, it may encourage greater circumspection in daily practice…”
—Redelmeier et al. [13]
With an understanding of our own thinking, students, residents, and fellows might better invoke and utilize analytic processes (System 2) appropriately, while confidently employing intuitive routes (System 1) in the proper context. Elder and Paul [14] define critical thinking as “the ability and disposition to improve one’s thinking by systematically subjecting it to intellectual self-assessment.” Their theory describes elements of excellent reasoning and intellectual standards and traits that characterize the “well cultivated critical thinker.” Croskerry states, “The various approaches that have been taken toward decision-making have two implicit purposes: first, to explain the ways in which we think and, second, to generate a practical approach to decision-making that has important clinical utilization” [15]. This deliberate, heightened awareness of the processes and systems that govern our reasoning is referred to as metacognition. Quirk describes this as “thinking about one’s own and another’s thinking and feeling” [16] (see also Chaps. 13 and 14). Although limited evidence exists, there remains hope that metacognition might act as a powerful forcing strategy to help students and physicians slow down their thinking when necessary and avoid making diagnostic errors that result from biases and fallacies typically produced from System 1 processes. These cognitive biases have been collectively termed cognitive dispositions to respond (CDRs). Although Croskerry has compiled and described over 30 CDRs, a select few common cognitive biases deserve mention [17].
Premature closure: the tendency to accept a diagnosis before it has been fully verified. The consequences of the bias are reflected in the maxim: “When the diagnosis is made, the thinking stops.”
Anchoring: this is the tendency to lock onto salient features in the patient’s initial presentation too early in the diagnostic process and failing to adjust this initial impression in the light of later information. This CDR may be severely compounded by the confirmation bias.
Confirmation bias: the tendency to look for confirming evidence to support a diagnosis rather than look for disconfirming evidence to refute it, despite the latter often being more persuasive and definitive.
Availability: the disposition to judge things as being more likely, or frequently occurring, if they readily come to mind. Thus, recent experience with a disease may inflate the likelihood of its being diagnosed. Conversely, if a disease has not been seen for a long time (is less available), it may be underdiagnosed.
Diagnosis momentum: once diagnostic labels are attached to patients they tend to become stickier and stickier. Through intermediaries (patients, paramedics, nurses, physicians), what might have started as a possibility gathers increasing momentum until it becomes definite, and all other possibilities are excluded.
6 The Development of Clinical Reasoning Competency
How do you know if your students are moving through the appropriate stages on their way to becoming efficient and accurate diagnostic thinkers? Although medical educators have not embraced a single predominant model for assessing clinical reasoning, we propose that trainees should demonstrate progressive mastery in:
-
Developing and sharing a concise verbal or written problem representation of the patient case which communicates their assessment of the problem.
-
Consistently using semantic qualifiers in their problem representations (see Table 6.1).
-
Seeking, identifying, and recalling the defining and discriminating features (“pertinent positives and negatives”) of a patient’s history and physical exam and linking this to appropriate illness scripts.
-
Demonstrating an explicit metacognitive approach to patient evaluations with fewer examples of bias (availability, anchoring).
7 Strategies for Assessing Clinical Reasoning
Many studies of how health professionals think employ a technique known as “think aloud” [18], wherein subjects speak about how they are thinking about a case or a clinical problem. This is the best available strategy in the day-to-day activities of teaching in a clinical setting to assess how our medical learners are thinking about and solving clinical problems. In the next section we list some examples of these opportunities.
7.1 Direct Observation of Clinical Skills
You can observe a lot just by watching
—Yogi Berra
While it may be resource- and time-intensive, direct observation of trainees in the clinical setting is invaluable. Doing so allows for insight into the learner’s ability to actively generate hypotheses and ask appropriate follow-up questions as well as their ability to consider, search for, and elicit relevant findings on the physical exam. Some of the more common frameworks for direct observation include:
-
1.
The Structured Clinical Observations (SCOs) described by Lane and Gottlieb [19] highlights three major domains of the encounter: history taking, physical examination, and information giving. SCOs can be tailored to unique assessment needs [20] and have been shown to be useful for learner self-evaluation [21].
-
2.
The Mini-Clinical Examination (Mini-CEX) instrument has been broadly applied to inpatient and outpatient in-training assessments (ITAs) (see also Chap. 19) and has been widely adopted in clerkships and residency training programs. A single faculty or resident observer typically completes the instrument, which is a single nine-point Likert scale for each of seven domains: Medical Interviewing Skills, Physical Examination Skills, Humanistic Qualities/Professionalism, Clinical Judgment, Counseling Skills, Organization/Efficiency, Overall Clinical Competency. The total time invested for the observation is approximately 20 min, and the tool is intended for the direct observation of a focused history and physical examination. Of all the direct observation tools, the mini-CEX has been shown to have the strongest inter-rater reliability and validity [22–26].
-
3.
The Brief Structured Clinical Observation (BSCO) [27] can be useful in very busy clinics in which one preceptor is working with multiple learners. The preceptor focuses on a segment or a portion of the patient history in any one episode. Ideally in a longitudinal preceptor–student relationship, there are a number of BSCOs of a single learner performing multiple parts of the history (HPI, family history, sexual history, etc.) so that feedback can be given on each skill and summarized into a comprehensive evaluation at the end of a rotation. There are four phases of the BSCO as follows:
-
Observe and record—the observer writes down the learner’s history gathering questions verbatim categorizing them as open-ended and leading or closed-ended questions.
-
Debrief the learner—the preceptor asks the learner “What did you find out with that question?” and “What else might be important?”
-
Review the script—the preceptor and the learner discuss what questions led to useful information and what additional questions might be needed.
-
Conclude—the preceptor points out 1–2 strengths and 1–2 things to improve upon.
The BSCO can also be adapted to the specific aspects of the physical exam.
-
-
4.
Oral case presentations: The prepared preceptor can use the clinical setting to assess and coach student clinical reasoning by listening to presentations and exploring the student’s ability to gather relevant data and synthesize information in the form of a problem representation which then leads to a differential diagnosis. Novices may struggle with determining what information is diagnostically salient. After they state their patient assessment, ask them to “repeat it, but this time a little shorter.” Coaching them to use more semantic qualifiers and identify pertinent defining and discriminating features (“pertinent positives and negatives”). Doing this once or twice allows them to efficiently flex their “salience determination” muscles.
7.2 The One Minute Preceptor
The One-Minute Preceptor, or the 5 microskills model, is widely used because it is adaptable to many clinical teaching settings [28]. In precepting the learner, the faculty member structures the session by doing the following:
-
1.
Asks for a commitment from the learner regarding the patient’s likely diagnoses
-
2.
Probes the learners’ thinking about “supporting evidence” for their decision
-
3.
Teaches general rules about the patient/topic
-
4.
Reinforces with the learner’s reasoning strengths
-
5.
Corrects any errors in knowledge and reasoning
7.3 Small Group Case Presentations
Small group case presentations such as teaching rounds, morning report, or didactic attending rounds allow for multiple pauses to discuss reasoning as a clinical case unfolds. Facilitators can probe the thinking of a number of learners of varying levels, from students to seasoned residents. Allowing for peer-to-peer facilitation in these settings can also lend insight into the teaching and reasoning skills of trainees.
7.4 Reading and Giving Feedback on Patient Notes in the Setting of Clinical Care
Many medical educators are concerned about the potential negative impact of electronic medical records on learners’ clinical reasoning. This is due to the tendency to “copy forward” information and, as a result, not slow down and “think the case through” (a metacognitive strategy) [29]. Health profession students should be challenged to “force” themselves to generate updated problem representations on a daily basis. In this way—“A toddler with acute-onset of moderate respiratory distress and low-grade fever with diffuse lower respiratory findings on chest exam” might ultimately give way to, “a toddler with acute bronchiolitis.” By reading progress notes with sensitivity to this type of progression in thinking, faculty members can assess a learner’s clinical reasoning and give feedback aimed at developing the trainee’s critical thinking.
7.5 Computer Cases with Diagnostic Frameworks
Instructional cases such as those available in Med U (http://www.med-u.org/) require that students list potential diagnoses and rank them in degree of likelihood.
7.6 Comprehensive Clinical Skills Exams
In June 2012, the USMLE Step II CS examination adopted modifications to the patient note, which require examinees to create a reasoned, focused differential, listed in order of likelihood, and supported with data from the history and physical examination. This extends the SOAP (Subjective, Objective, Assessment, Plan) note format, which only reflected the student’s data gathering and initial diagnostic reasoning. Many medical schools have adopted a similar framework for their internal comprehensive clinical skills examinations or observed structured clinical examinations (OSCE). This framework explicitly asks students to share their illness scripts and therefore can serve as a measure of a student’s clinical reasoning skills.
8 Remediation of Common Clinical Reasoning Problems
According to the literature and our extensive experience with medical students and residents the two most common clinical reasoning problems are [30]
-
1.
Inadequate problem representation
-
2.
Ineffective development or storage of illness scripts
These deficiencies may manifest individually or together, and both can contribute to trouble in developing a differential diagnosis. Of course, weak foundational knowledge (“reduced”) is common among trainees; however, we caution clinical teachers against simply advising the trainee to “read more” (see Chap. 3) without also providing them with support in organizing their knowledge into useful illness scripts as part of active clinical reasoning practice. What follows are detailed descriptions of strategies we have found useful and effective (Fig. 6.3).
8.1 Difficulty with Problem Representation
8.1.1 Major Symptoms
Students who experience difficulty developing a problem representation may limit or completely eliminate their assessment—or commitment to what they believe the differential diagnosis is—from a case presentation. This results in what some refer to as SOP (Subjective, Objective, Plan) or SOSOP (Subjective, Objective, Subjective, Objective, Plan) presentations [31]. For instance:
-
SOP: “This is a 15-month-old male with a 3-day history of low-grade fever, runny nose, cough and trouble breathing. There is good air exchange and wheezing with occasional crackles on lung exam. I would like to get a CXR and give a trial of a bronchodilator.”
-
SOSOP: “This is a 15-month-old male with a 3-day history of low-grade fever, runny nose, cough and trouble breathing. On lung exam there is good air exchange and wheezing with occasional crackles. So my assessment is a 15-month-old male with a 3-day history of low-grade fever, runny nose, cough and trouble breathing whose exam reveals wheezing with occasional crackles. I would like to get a CXR and give a trial of a bronchodilator.”
Since an accurate problem representation serves as a launching off point for creating a relevant differential diagnosis, even students with well-developed knowledge compiled as illness scripts may struggle with developing a differential diagnosis if they cannot first articulate an accurate case summary. As a result, these students may give a “silo-ed” differential (a separate set of diagnoses for related symptoms), or a poorly prioritized differential diagnosis.
-
Silo DDx: “This is a 15-month-old male who presents with a 3-day history of fever, rhinorrhea, cough and trouble breathing with respiratory distress and crackles on pulmonary exam. The differential diagnosis of fever includes viral infections, bacterial infections, connective tissue diseases and drug fever. The differential diagnosis of cough includes foreign body, tracheomalacia, etc.”
For the case above, a student with a poorly prioritized differential diagnosis might mention aspiration pneumonia (e.g., very unlikely in this scenario) at the top of his or her list of diagnostic possibilities.
8.1.2 Remediation and Practice Strategies
Strategies that help a student who is knowledgeable enough with the expected breadth and sophistication in his or her illness scripts but cannot develop a problem representation include (1) reverse presentations, (2) practicing the use of semantic qualifiers (“Buy a qualifier game”), and (3) analyzing students’ presentations using SNAPPS [32] or IDEA [33] precepting models.
-
1.
Reverse presentation (ASOAP): Ask the learner to start the patient presentation with their assessment. The preceptor then carefully listens to determine if the proper positive and negative supporting data are reported which make the assessment credible. As an example, the student would start with the following assessment:
“This is a 15 month old male with bronchiolitis versus viral pneumonia and hypoxia. I believe he should be admitted to the hospital for supportive care with oxygen and IV fluids.”
The preceptor then listens carefully and coaches the student to include in the presentation elements that support the diagnosis and management plan.
-
2.
Practice with semantic qualifier (“Buy a qualifier”): When the student presents the case like this:
“15 month-old male with a 3-day history of low-grade fever, runny nose, cough and trouble breathing. On exam there is good air exchange and wheezing with occasional crackles on lung exam”
The preceptor should display a list of useful semantic qualifiers (see Table 6.1) and ask the student to “buy two.” The student then, with playful coaching, gets a chance to analyze their assessment and rework it, hopefully toward a presentation that sounds more like this:
“A 15 month-old with acute onset of moderate respiratory distress and low-grade fever with diffuse lower respiratory findings on chest exam.”
-
3.
Precepting models: Formal student presentations in the clinical setting can limit the opportunity to judge a student’s reasoning. There are a number of precepting models, which focus on a student’s reasoning. Such models as the One Minute Preceptor described above [27] are faculty-driven, with faculty providing the questions which prompt reasoning (“What do you think is going on with this patient? Why?”). Other models, such as SNAPPS and IDEA, are learner-driven and are useful for oral presentations and patient notes. Many video demonstrations of these models exist on the Internet.
SNAPPS: This model is structured explicitly to force the learner to articulate their clinical reasoning process. Originally described as a model for ambulatory teaching, the SNAPPS model is also easily adaptable to inpatient teaching—especially when rounds are hurried and need to be focused! The learner is provided with this six-step framework for the case presentation:
-
S—Summarize briefly the history and physical
-
N—Narrow the differential to 2 or 3 relevant possibilities
-
A—Analyze the differential by comparing and contrasting the possibilities
-
P—Probe the preceptor by asking questions regarding uncertainties
-
P—Plan management for the patient
-
S—Select an issue for self-directed study
The SNAPPS model has been shown to facilitate development of students’ diagnostic reasoning in the ambulatory setting [31].
Let’s listen to what a dialogue might sound like between a preceptor and a learner using the SNAPPS format:
Preceptor to John, medical student:
“Thanks for going to see that 15 month with respiratory issues John. Remember at the start of the clinic session, we discussed the SNAPPS framework. I’d like you to try to present the patient to me using SNAPPS.
John: “OK, I will give it a try.”
(S) I just finished seeing a 15 month-old male named Kevin. He was brought in by his father due to a 3-day history of low-grade fever, runny nose, and cough. He also developed some trouble breathing this morning described by his dad as fast breathing rate, using extra muscles to breathe and making some noises with breathing. There is no history of foreign body ingestion or aspiration. He’s had sick contacts in daycare. He’s fully vaccinated and he’s had no recent travel out of the country or exposure to people with chronic cough. The rest of his systems review is negative for GI symptoms such as vomiting or diarrhea, as well as for rash, or growth problems. His father says that Kevin’s primary care physician doesn’t have any ongoing health concerns about Kevin. Kevin takes no medications. On exam he’s a happy appearing child in mild to moderate respiratory distress as demonstrated by his respiratory rate of 45. He’s using some accessory muscles to breathe and demonstrates suprasternal retractions and some nasal flaring. He has a prolonged expiratory phase. On his lung exam, there is good air exchange and I hear wheezing with occasional crackles in his bilateral mid to lower lung fields.
(N): I think this child most likely has bronchiolitis, asthma or perhaps bacterial pneumonia.
(A): The reason I think he has bronchiolitis is that he is in the right age group (less than age 2), he has sick contacts in daycare who are probably sharing the same viral infection, and he has a bilaterally symmetric exam with wheezing. He also has other signs of a viral infection such as rhinorrhea. I thought about asthma, but there is no family history of asthma and the father says the child has never been sick like this before. I guess it could be the child’s first asthma exacerbation, triggered by a viral infection, but I think this is less likely—especially given how common bronchiolitis is. Lastly, I thought about bacterial pneumonia based on the crackles on exam and the fact that he developed respiratory distress 3 days into a viral upper respiratory infection, suggesting maybe bacterial superinfection. But Kevin is not that ill appearing and his exam demonstrates bilateral crackles with wheezing which would be less common in bacterial pneumonia.
(P) I also thought about atypical organism infection—such as Mycoplasma, but I don’t know how those present in children or even if they are pathogens in this age group. Can you tell me about that? Come to think of it, I also can’t recall the most common viral causes of bronchiolitis.
(P) I would like to get a chest X ray given that it’s Kevin’s first episode of respiratory distress and also because there is an outside consideration of bacterial pneumonia. I would also like to give a bronchodilator and perhaps send some viral studies.
(S) Before sending any tests, I am going to quickly find out which viruses we might test for and how long it takes for the results to return, in order to see if any testing at all would be useful.
IDEA: The IDEA framework was developed to enable a clinical teacher’s assessment of a student’s clinical reasoning based on the written note. Students are encouraged to organize the assessment section of their write-up using the following anchor points:
-
I: Interpretive summary—a summary of the patient with the use of semantic qualifiers
-
D: Differential diagnosis with commitment to the most likely diagnosis
-
E: Explanation of reasoning for selecting the most likely diagnosis
-
A: Alternative diagnoses with an explanation of reasoning
An example of a written patient assessment in IDEA format might look like the following:
(I): This is a 15 month-old with acute onset fever and upper respiratory symptoms, progressing to moderate respiratory distress, accompanied by diffuse lower respiratory findings on chest exam.”
(D): Diagnostic possibilities include (in descending likelihood) bronchiolitis, asthma, bacterial pneumonia.
(E): Bronchiolitis seems most likely given the child’s age, sick contacts in daycare and his bilaterally symmetric exam with wheezing. Asthma is a possibility but less likely due to no family history of asthma and no previous episodes. Lastly, there is a small consideration for bacterial pneumonia given the crackles on his exam and the progression of his illness.
(A): Other less likely diagnoses would include aspiration pneumonia, foreign body aspiration, cystic fibrosis but there are no specific factors of the history or physical which support these strongly.
The strategies listed above provide a remediation coach with the data needed to assess whether the struggling student has made progress. All remediation activities should be documented (see Chap. 20).
8.2 Problem with “Illness Scripts” (See Fig. 6.3)
As mentioned earlier in this chapter, the problem representation step allows for ignition of clinical memory that in turn leads to a search for stored illness scripts. Students with limitations in the quantity or organization of their illness scripts may be able to gather some data, but it will not typically have the proper attention to those key features that can help to generate, confirm, or refute hypotheses. As a result, these students may also struggle to generate a differential diagnosis.
8.2.1 Major Symptoms
Students with illness script problems miss relevant data on the history or examination due to their inability to test diagnostic hypotheses in real time, a process known as co-selection. Students may also focus unnecessarily on items of little relevance, or gather and report back information in their “comfort zone,” for example, the social history, even if this is not particularly relevant. This has been described as the “unfiltered data dump” [30].
In addition to data gathering problems, students with deficient illness scripts may also have challenges creating differential diagnoses. Some differential diagnoses may be frankly inaccurate or can have other characteristics, often referred to as “frozen” or “zebra” differentials.
-
Frozen differential diagnosis ignores relevant data, in this case a normal chest X ray: “This is a 15-month-old male who presents with a 3-day history of fever, rhinorrhea, cough and trouble breathing with respiratory distress and crackles on pulmonary exam. The differential diagnosis includes viral upper respiratory tract infection, viral or bacterial lower respiratory tract infection, foreign body aspiration and gastroesophageal reflux with aspiration. His CXR is negative. Given the fever and respiratory distress, I think the child most likely has bacterial pneumonia.”
-
Zebra differential diagnosis includes highly unlikely or rare diagnoses “This is a 15-month-old male who presents with a 3-day history of fever, rhinorrhea, cough and trouble breathing with respiratory distress and crackles on pulmonary exam. The differential diagnosis includes viral upper respiratory tract infection, atypical infection such as Legionella or gram negative pneumonia.”
8.2.2 Remediation and Practice Strategies
Strategies to remediate problems with illness scripts generally fall into two categories. The first can be considered “asynchronous,” in that the learner can, with guidance from the teacher, work on remediation on his or her own time. Asynchronous techniques focus on building knowledge and interconnecting illness scripts. The other, synchronous or just-in-time strategies, involves teachers more actively as a coach and facilitator. Which strategies are used depends on time and other resources. In a busy clinical setting, it may not be practical to spend an additional 10 min per patient probing and remediating the reasoning around every case. In those cases, identifying the learning needs and giving the student an assignment to be reported on at a later time can be a more efficient strategy.
8.2.2.1 Asynchronous Strategies
Horizontal reading allows a student to transform a knowledge base that is organized in organ systems into one that applies more readily to patients’ presenting symptoms. With a symptom as a starting point, for example, a toddler presenting with a limp, a student is asked to read about features of specific, common, and “can’t miss” diagnoses. Such an exercise will promote the development of illness scripts with defining and discriminating features as well as encourage a more purposeful retrieval of their knowledge base. Figure 6.4 illustrates a typical grid for horizontal reading. This can be given to a student as a nightly assignment.
Script sorting: This technique is also based on the concept of discriminating and defining features as shown in Fig. 6.5. This process can allow students to compare and contrast certain signs and symptoms across a differential diagnosis, ascribing positive value to those signs or symptoms that speak strongly for a diagnosis and negative values to those that speak against a diagnosis. The end result demonstrates a representation of the relative likelihoods of various diagnoses given certain diagnostic features. A typical grid, again using the example of a toddler with limp, may look like the following, with (++) speaking strongly for the diagnosis, (+) speaking for diagnosis, (0) neutral, (−) speaking against diagnosis, and (− −) speaking strongly against.
8.2.2.2 Synchronous/Just in Time Strategies
Diagnostic reframe: When students first learn the concept of differential diagnosis, mnemonics are often taught (e.g., VINDICATE), which prime the student to consider all known possible causes for particular patient’s presentation. While this can be a useful exercise, many of the items are often disembodied from the case at hand. It is more effective to challenge students to first generate a relevant list of diagnoses based on the presenting complaint, and then revisit the comprehensive VINDICATE list. In revisiting the comprehensive list, students should be encouraged to focus on committing only to what they can justify are the most likely diagnoses and indicate which diagnoses may be rare or “can’t miss.” In this way the teacher coaches the student to reason through the initial list generated by the mnemonic.
Highlighter exercise: This highly effective strategy, as described by Stuart et al. [31] can be used with single or multiple learners. Starting with a written case presentation (a note from the electronic health record, case report from journal, etc.), learners are asked to highlight relevant information in the history they feel will help them discriminate among diagnostic possibilities. In general, when this is done with multiple levels of learners, the more novice learners highlight a great deal while the more expert clinicians highlight only a few high-yield items. Comparing and contrasting different results can lead to effective peer-to-peer teaching. Teaching faculty can debrief with one or many learners and discuss the clinical relevance of certain history and physical examination findings (for example, see Fig. 6.6).
Persuade the MD: This role-play scenario has the learner assume the role of a patient. The learner’s challenge is to, in limited time, convince the preceptor that the “patient” has a certain diagnosis by giving a highly relevant medical history. For example, the preceptor might say to the student, “Let’s assume you have a chronic cough: convince me in 30 seconds or less that you have tuberculosis.” The novice learner, in playing the role of patient, may begin to wander in the presentation, talking about a long-lasting cough while forgetting to include defining features. The more seasoned learner would immediately use semantics such as progressive cough with fever, hemoptysis, and night sweats as well as include the relevant travel or exposure history. This demonstrates the seasoned learners’ awareness of the key features (illness script) for this diagnosis. This type of exercise can be used to analyze the reasoning in a student’s previous case presentation. For example, a teacher–learner dyad discussing a case may take one item on the student’s differential diagnosis. “Let’s say for example that you were this patient and you indeed have cholecystitis. Convince me in 20 seconds that this is your diagnosis.” <student responds> “Now, how did your presentation compare to the one of the patient we are seeing?”
9 Summary
A primary goal of medicine is to make accurate diagnoses in order to improve health outcomes and reduce costs. To that purpose, the importance of this information to clinical teachers and their students cannot be overstated. There have been great advances in the past 40 years in understanding the processes that govern how people reason and, by extension, how physicians make decisions and diagnoses. Medical teachers should be attuned to the relevant body of knowledge from the field of cognitive psychology. These theories themselves—and not just the teaching strategies—are also relevant to students. With this in mind, we recommend instructing trainees in the principles of diagnostic decision-making. Teach them about hypothetico-deductive reasoning and pattern recognition. Explicitly point out when they are engaged in one, the other, or toggling between both. Notice when they take shortcuts and comment on whether they do so wisely or not. Help your learners understand how their reasoning connects with their stored knowledge and illness scripts. Of the thousands of medical students that we have worked with over the past 10 years, virtually all have expressed the goal of becoming master clinicians. In our role as educators, we can best aid our students in this quest by demonstrating a keen awareness of the process of diagnostic decision-making they engage in, rather than focus solely on their ability to get the right answer.
In our experience, most students who have challenges in clinical reasoning can be remediated with attention paid to their knowledge base and their thinking patterns. Students with the greatest difficulty are those who struggle to engage in reflective practice (see Chaps. 13 and 14). Although some of these students may ultimately not succeed, the more we are able to promote the value of metacognition and reflection, the more we may be building upon the foundational guideposts that will allow all students to map their course to clinical excellence and expertise.
References
Kohn LT, Corrigan JM, Donaldson MS. To err is human: building a safer health system. Washington, DC: National Academy Press; 2000.
Newman-Toker DE, Pronovost PJ. Diagnostic errors—the next frontier for patient safety. JAMA. 2009;301(10):1060–2.
Kahnemann D. Thinking fast and slow. New York: Farrar, Straus, and Giroux; 2011.
Frederick S. Cognitive reflection and decision making. J Econ Perspect. 2005;19(4):25–42.
Ark T, Brooks LR, Eva KW. Giving learners the best of both worlds: do clinical teachers need to guard against teaching pattern recognition to novices? Acad Med. 2006;81:405–9.
Groopman J. How doctors think. Boston: Houghton Mifflin; 2007.
Elstein A. Thinking about diagnostic thinking: a 30-year perspective. Adv Health Sci Educ. 2009;14:7–18.
Bowen JL. Educational strategies to promote clinical diagnostic reasoning. N Engl J Med. 2006;335(21):2217–25.
Charlin B, Boshuizen H, Custers EJ, Feltovich P. Scripts and clinical reasoning. Med Educ. 2007;41:1178–84.
Charlin B, Tardif J, Boshuizen H. Scripts and medical diagnostic knowledge: theory and applications for clinical reasoning instruction and research. Acad Med. 2000;75:182–90.
Eva K. What every teacher needs to know about clinical reasoning. Med Educ. 2004;39:98–106.
Bordage G. Elaborated knowledge: a key to successful diagnostic thinking. Acad Med. 1994;69(11):883–5.
Redelmeier DA, et al. Problems for clinical judgment: introducing cognitive psychology as one more basic science. CMAJ. 2001;164:358–60.
Elder L, Paul R. Critical thinking development: a stage theory. http://www.criticalthinking.org/pages/critical-thinking-development-a-stage-theory/483. Accessed 12 Nov 2012.
Croskerry P. A universal model of diagnostic reasoning. Acad Med. 2009;84(8):1022–8.
Quirk M. Intuition and metacognition in medical education: keys to developing expertise. New York, NY: Springer; 2006.
Croskerry P. The importance of cognitive errors in diagnosis and strategies to minimize them. Acad Med. 2003;78(8):775–80.
Fonteyn ME, Kuipers B, Grobe SJ. A description of think aloud method and protocol analysis. Qual Health Res. 1993;3(4):430–41.
Lane JL, Gottlieb RP. Structured clinical observations: a method to teach clinical skills with limited time and financial resources. Pediatrics. 2000;105(4 Pt II):973–7.
Hamburger EK, Cuzzi S, Coddington DA, Allevi AM, Lopreiato J, Moon R, Yu C, Lane JL. Observation of resident clinical skills: outcomes of a program of direct observation in the continuity clinic setting. Acad Pediatr. 2011;11(5):394–402.
Zimmer KP, Solomon BS, Siberry GK, Serwint JR. Continuity-structured clinical observations: assessing the multiple-observer evaluation in a pediatric resident continuity clinic. Pediatrics. 2008;121(6):e1633–45.
Norcini JJ, Blank LL, Arnold GK, Kimball HR. The mini-CEX (clinical evaluation exercise): a preliminary investigation. Ann Intern Med. 1995;123(10):795–9.
Norcini JJ, Blank LL, Duffy FD, Fortna GS. The mini-CEX: a method for assessing clinical skills. Ann Intern Med. 2003;138(6):476–81.
Durning SJ, Cation LJ, Markert RJ, Pangaro LN. Assessing the reliability and validity of the mini-clinical evaluation exercise for internal medicine residency training. Acad Med. 2002;77(9):900–4.
Kogan JR, Bellini LM, Shea JA. Implementation of the mini-CEX to evaluate medical students’ clinical skills. Acad Med. 2002;77(11):1156–7.
Kogan JR, Holmboe ES, Hauer KE. Tools for direct observation and assessment of clinical skills of medical trainees: a systematic review. JAMA. 2009;302(12):1316–26.
Pituch K, Harris M, Bogdewic S. The brief structured observation—a tool for focused feedback. Acad Med. 1999;74(5):599.
Neher JO, Gordon KC, Meyer B, Stevens N. A five-step “microskills” model of clinical teaching. J Am Board Fam Pract. 1992;5(4):419–24.
Schenarts PJ, Schenarts KD. Educational impact of the electronic medical record. J Surg Educ. 2012;69(1):105–12.
Wolpaw TM, Wolpaw DR, Papp KK. SNAPPS: a learner-centered model for outpatient education. Acad Med. 2003;78(9):893–8.
Stuart E, Slavin S, Blankenburg R, Butani L, Konopasek L. Clinical reasoning. In: Morgenstern B, editor. Guidebook for clerkship directors. 4th ed. Syracuse, NY: Gegensatz Press; 2012.
Baker E, Ledford C, Liston B. Teaching, evaluating, and remediating clinical reasoning. Acad Intern Med Insight. 2010;8(1):12–3, 17.
Wolpaw T, Papp KK, Bordage G. Using SNAPPS to facilitate the expression of clinical reasoning and uncertainties: a randomized comparison group trial. Acad Med. 2009;84(4):517–24.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer Science+Business Media New York
About this chapter
Cite this chapter
Mutnick, A., Barone, M. (2014). Assessing and Remediating Clinical Reasoning. In: Kalet, A., Chou, C. (eds) Remediation in Medical Education. Springer, New York, NY. https://doi.org/10.1007/978-1-4614-9025-8_6
Download citation
DOI: https://doi.org/10.1007/978-1-4614-9025-8_6
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4614-9024-1
Online ISBN: 978-1-4614-9025-8
eBook Packages: MedicineMedicine (R0)