Abstract
Medical trainees must be able to master large volumes of knowledge quickly to be academically successful and competent to practice clinically. About a third of struggling medical learners have insufficient medical knowledge. In this chapter, through case examples and use of Bloom’s taxonomy as a theoretical framework, the author demonstrates how medical knowledge deficits can be distinguished from other types of academic difficulty. Once a medical knowledge deficit is identified, strategies to address this should be tailored to the etiology of the problem. In the experience of the author, who is the founding director of a comprehensive remediation program serving medical students and residents, the most common predominant underlying causes for a significant medical knowledge deficit in medical students are lack of committed study time, distraction, and anxiety and poor self-confidence. Questions to help the learner clarify the issues contributing to their insufficient working medical knowledge are offered. Specific remediation strategies are described in detail and illustrated with case examples. In addition, a list of study tips and test-taking strategies has been included to assist in remediation of these medical learners.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Attention Deficit Hyperactivity Disorder
- Medical Knowledge
- Remediation Strategy
- Practice Question
- Medial College Admission Test
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Introduction
Learning enormous amounts of information is the sine qua non of medical school. Students struggle with the volume of facts they need to commit to memory. For most, to succeed requires an unprecedented level of sustained concentration and necessitates developing new, more rigorous learning strategies. In one study, when asked for potential solutions to these challenges, preclinical medical students most commonly requested a course on study skills [1]. Across all 4 years of medical school, the most common reasons students request support services are to help with test taking and organization and integration of large amounts of information [2].
Failing finals is often a surprise for the student but not the teacher. [3]
Insufficient medical knowledge is prevalent among students who struggle in medical school. At the University of Colorado School Of Medicine, starting in 2006, we developed a comprehensive remediation program, which serves all levels of medical trainees. Medical students can self-refer to the program or are enrolled if they fail, receive negative comments on evaluations, or are identified by the course director as otherwise performing poorly. Insufficient medical knowledge is the single most common deficit, identified in 38 % of the medical students referred to the program [4].
Interestingly, despite how common it is, our experience is that insufficient medical knowledge is “overdiagnosed” by clinician educators who are sensitive but not specific in identifying remediation issues [5]. After investigation by the remediation committee, it turns out that many students thought by preceptors to “need to read more” actually have adequate foundational knowledge bases but struggle instead with other issues such as application of that knowledge in the context of clinical reasoning, problems with interpersonal communication, performance anxiety, and/or disorganization. Because of this, and in order to effectively address the problem, all students reported to have a medical knowledge deficit should be assessed carefully before they are pressured to “read more.”
2 Distinguishing a Medical Knowledge Deficit from Other Deficits
Nationally standardized examinations, such as the United States Medical Licensing Exams (USMLE) Steps 1, 2, and 3 and the National Board of Medical Examiners (NBME) Subject Exams, are designed to measure medical knowledge [6] with high reliability. Reviewing the student or resident’s academic record or asking a learner if they passed all prior standardized exams may help differentiate medical knowledge problems from other deficiencies. If a learner, for example, passed USMLE Step 1 on her first attempt and scored a 200 or better, then foundational medical knowledge is unlikely the problem, and it would be more fruitful to evaluate her clinical reasoning and related heuristic biases, communication skills, or mental health issues, such as anxiety. If the learner failed the USMLE Step 1 and then passed on retest by one point, there is a better chance that weak foundational medical knowledge is the primary problem.
-
Sam is getting ready to start her third year of medical school, which marks the start of her clinical clerkship rotations. She failed USMLE Step 1 twice and passed it on her third attempt with a 188, the lowest possible passing score that year. She is interested in improving her test scores, as she will have to take USMLE Steps 2 and 3, as well as individual NBME subject examinations.
For students who fail medical knowledge examinations, further investigation will elucidate the cause of the knowledge deficit, so that a targeted and individualized remediation plan can be created. Answers to the following questions will paint a comprehensive picture of the learner’s examination challenges:
-
How did you score on other standardized exams such as the Scholastic Aptitude Test (SAT) for college admissions, Graduate Record Exam (GRE) for graduate school admissions, Medial College Admission Test (MCAT) for medical college admissions, and USMLEs compare with your peers? Was your performance consistent across all components of the exam, or did you score low in one area and high in others?
-
Has your performance on exams throughout medical school been consistent? Can you identify a point in time that performance significantly worsened? If so what was happening in your life at that time, and did your study habits change?
-
Is your knowledge gap global or related to a specific topic or set of topics?
-
What approaches have you been using to study? Can you describe your study habits in detail?
-
Do you have a previously diagnosed learning disability?
-
Upon further questioning, Sam reports getting a 1,400 on her SAT which places her in the 95th percentile of all college-bound high school students in the United States and MCAT scores of 10 in physical science, 11 in biological science, and 10 in verbal reasoning. Her total MCAT school of 31 put places her in the 82nd percentile of US medical school applicants. Her scores are not unlike her high-achieving peers. Sam scored just about average on her first two courses in medical school.
If a learner reports that they have always been a “bad test taker” or had an injury or illness that resulted in a change in performance, neuropsychiatric testing may be informative (see Chap. 9). If the knowledge deficit is limited to one or two topic areas, a successful remediation is more likely. Reviewing the learner’s study skills is also important. If the learner is putting in sufficient time but study strategies are inefficient (e.g., reading the same textbook over many times rather than summarizing the material into briefer study tools), study skills coaching can make a remarkable difference. If the learner has been previously diagnosed with a learning disability, that student’s experience with accommodations (e.g., extra time for exams, use of a calculator for calculations or computer for writing) should provide guidance for what will work in the future.
-
When asked to discuss her study strategies, she admits that because the grading policy is pass/fail, once she was confident that she could pass her courses, she stopped going to class. Instead, she sleeps until noon, attends labs in the afternoon, and watches video recordings of the lectures from home in the evenings, often at double speed. She feels this is a more “healthy” approach since she had more control over her time and energy. She has been cramming before exams. Starting 2 days before the exam, she repeatedly review lecture notes and textbook chapters taking brief breaks to eat and sleep.
-
At the end of the pre-clerkship curriculum, she failed the USMLE Step 1 exam twice. Prior to her third attempt, she enrolled in a review course, and neuropsychological testing did not reveal a learning disability. She has subsequently passed the exam.
Sam’s “pump and dump” (also known as “binge and purge” or “brute force”) study strategy is a problem. This approach is among the least effective in producing future recall of information and application of that information to new problems. Studies of human learning reveal that the most durable learning, with the least “forgetting” or degradation of learning, occurs with: 1) spacing study of a particular content over long periods of time; 2) studying strategies which include frequent testing of recall using short-answer-type questions, rather than multiple choice questions which test recognition rather than recall; and 3) interleaving the studying of a variety of topics rather than “blocking” study time by spending large amounts of time on a single topic and then moving on to the next topic [7]. Despite the weight of the evidence in favor of these strategies, learners often perceive that they are less effective because while these strategies—spacing, testing, and interleaving—produce better long-term impact on learning, this may not be obvious in the short run. Curriculum structures that block the material to be studied and assessment approaches of traditional medical schools, which do not test material cumulatively, reinforced this study behavior.
-
It is often only when durability of knowledge is tested in the longer run that the student may perceive a problem with their study strategies.
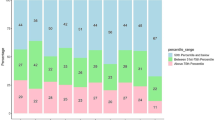
Through direct observation using Bloom’s Taxonomy as modernized by Lorin Anderson, we find students who struggle at the lower two levels benefit from strategies presented in this chapter. In Fig. 3.1 we illustrate how this information can be used to select from among the remediation strategies described later in this chapter.
In 1956, Benjamin Bloom chaired a committee of educators that created a classification system for educational goals [8]. Figure 3.1 represents a modernization of this taxonomy for learning in the cognitive domain [9]. While recent research in learning and neuroscience have revealed that linear hierarchical models such as Bloom’s are unlikely to accurately represent the complexity of human knowledge structures, Bloom’s Taxonomy has stood the test of time because frontline teachers find this model useful conceptually in educational practice. For instance, we find that students who struggle with the tasks of remembering or understanding benefit from remediation strategies focused on expanding their medical knowledge, while students whose struggles are above these levels are more likely to benefit from work on their clinical reasoning skills.
Imagine listening to this presentation from a third-year medical student rounding with you in the hospital. At what level does her deficiency lie on the updated Bloom’s Taxonomy in Fig. 3.1? Why?
Case Example 1: Sam
“Mr. Smith is a 55 year old male who presents with bleeding. This morning he felt nauseated after eating toast and drinking a bottle of beer for breakfast. About 1 h later, he vomited the toast and about one cup of bright red blood. After he vomited, he had a sore throat and metallic taste in his mouth. He came to the hospital because his discharge paperwork from 2 month ago said to return if he had any bleeding. He is not sure what makes it better or worse, though he does relay that doctors keep telling him not to drink alcohol anymore. He also says that his stools have been black and sticky for the past 3–4 days.
Mr. Smith reports nasal congestion with seasonal allergies. The review of systems is otherwise negative.
His past medical history is significant for chronic obstructive pulmonary disease on 2 L of oxygen, fatty liver disease, and alcohol-related cirrhosis. Two months ago he presented to the hospital with hematemesis and was found to have Grade II varices on upper endoscopy and is status post banding.
His medications include ipratropium/albuterol nebulizer four times a day and albuterol nebulizer ever 2 h as needed. He has no known drug allergies.
His family history is significant for liver cancer in his father and brother.
He smokes unfiltered cigarettes at 2 packs per day for a total of 80 pack years and drinks three 40 oz bottles of beer per day. He denies illicits, except for the marijuana he smokes a few times per month.
On physical exam, he is a thin male, has a big belly and appears older than his stated age. His vital signs are T 98.2 °F HR 125 BP 95/62 R 22 Sat 84 % on room air. His sclera are yellow. His heart is regular rate, no murmurs. His lungs are diffusely wheezing with expiration. He has a soft abdomen that is nontender with bowel sounds. His liver is enlarged. He has trace lower extremity edema. His rectal exam reveals black stool.
The only lab back so far is his CBC. His WBC is 3, HCT 24, and platelets of 53.
My differential diagnosis for his bleeding is a posterior nosebleed with vomiting, gastroesophageal reflux disease (GERD), and cancer.
I put nosebleed on the list first because he has had nasal congestion, which he might have mistaken for allergies, GERD because it is so common in our society and cancer because he has a strong family history.
I think we should order imaging to look for cancer and check liver cancer labs, consult ENT to make sure the nose isn’t actively bleeding and an upper endoscopy biopsy for GERD. He also needs two large bore IVs for blood and serial CBCs every 4 h.”
What is the quality and relevance of Sam’s medical knowledge? As the attending physician hearing this case, you would notice immediately that Sam has come to the wrong diagnostic conclusion about this patient, who is likely to be having an emergent, life-threatening GI bleed from esophageal varices rather than a nosebleed and liver cancer. Once you check that the patient is receiving appropriate care, you turn your attention to the learning needs of the student.
Sam is not semantically accurate or competent; she uses the term “hematemesis” and diagnoses “Grade II varices,” but you suspect she does not understand their specific meanings. She is likely repeating terms she heard from supervisors or read in the patient chart. While she has collected a good deal of information, it is not obvious she knows which components of the physical exam are pertinent to assessing a patient with liver disease and gastrointestinal bleeding. For example, she does not comment on orthostatic vital signs, skin pallor or lesions, or tests of ascites. Considering the taxonomy in Fig. 3.1, Sam appears to lack a firm foundational level of factual knowledge. She does not remember to refer to yellow sclera as icterus, liver cancer as hepatocellular carcinoma, or black stool as melena. She doesn’t quantify the size of the liver as would be routine. She does not appear to know which imaging tests are appropriate to assess for hepatocellular carcinoma or to check for alpha-fetoprotein in the serum.
Now compare and contrast this presentation of the same patient by another struggling third-year medical student:
Case Example 2: Jackson
Take 2:
Mr. Smith, our patient, has been very patient, allowing two medical students to interview him. This time, Jackson presents to the team:
“Mr. Smith is a 55 year old male who presents with bleeding. He felt nauseated this morning after eating toast and drinking 12 oz of beer. About 1 h later, he vomited the toast and had about one cup of bright red hematemesis. After he vomited, he had a sore throat and metallic taste in his mouth. He came to hospital because his discharge paperwork from 2 month ago said to return if he had any bleeding. He is not sure what makes it better or worse. He has had melena for the past 3–4 days and said that doctors keep telling him not to drink alcohol anymore.
Mr. Smith reports nasal congestion with seasonal allergies. The review of systems is otherwise negative.
His past medical history is significant for chronic obstructive pulmonary disease on 2 L of oxygen, fatty liver disease and alcohol-related cirrhosis. Two months ago he presented to the hospital with hematemesis and was found to have Grade II varices on upper endoscopy and is status post banding.
His medications include ipratropium/albuterol nebulizer four times a day and albuterol nebulizer ever 2 h as needed. He has no known drug allergies.
His family history is significant for hepatocellular carcinoma in his father and brother.
He smokes unfiltered cigarettes at 2 packs per day for a total of 80 pack years and drinks three 40 oz bottle of beer per day. He denies illicits, except for the marijuana he smokes a few times per month.
On physical exam, his is a thin male, has a big belly and appears older than his stated age. His vital signs are T 98.2 °F HR 125 BP 95/62 R 22 Sat 84 % on room air. His sclera are icteric. His skin has both telangiectasias and caput medusa. His heart is regular rate, no murmurs. His lungs are diffusely wheezing with expiration. He has a soft abdomen with positive bowel sounds, that is nontender. His liver is enlarged. He has trace lower extremity edema. His rectal exam reveals black sticky melena.
The only lab back so far is his CBC. His WBC is 3, HCT 24, and platelets of 53.
My differential diagnosis for his bleeding is a posterior nosebleed with vomiting, gastroesophageal reflux disease (GERD), and cancer.
I put nosebleed on the list first because he has had nasal congestion which he might be mistaken for allergies, GERD because it is so common in our society and cancer because he has a strong family history.
I think we should order a right upper quadrant ultrasound to look for cancer and check an AFP, consult ENT to make sure the nose isn’t actively bleeding and an upper endoscopy biopsy for GERD. He also needs two large bore IVs for blood and serial CBCs every 4 h. Oh, and a bone marrow biopsy to find out why his platelets are so low.”
In response to this type of presentation, we have heard colleagues exclaim, “This student, Jackson doesn’t know anything. He needs to read more!” For comparison, this presentation, unlike Sam’s, conveys that he has at least some medical knowledge in this content domain. Jackson is semantically savvy, able to use terminology like melena, telangiectasias, and icterus accurately. He demonstrates that he knows what to look for in a patient with liver disease. He also knows the appropriate diagnostic tests for each of the diagnoses on his differential. In contrast, he seems to be missing the most likely unifying explanation for this patient’s presentation. He is not recognizing the pattern (also referred to by psychologists as a schema or script) which is immediately recognized by more experienced clinicians. For Jackson, reading more and memorizing more will not remediate his clinical reasoning deficit the way that work to increase his clinical experience and explicit work on his clinical reasoning will (see Chap. 6).
Both these students “didn’t get” a life-threatening diagnosis. To help Sam it is important to understand if the primary underlying issue is lack of medical knowledge and or a clinical reasoning deficit. To do this her attending asks her the following question:
Sam, how would a patient with a variceal bleed present?
If Sam is unable to answer this fact-based question, then we can assume her medical knowledge is limited. If she is able to answer this and other similar questions correctly, medical knowledge is unlikely her deficit in this content domain, but rather she struggles with synthesis of information and pattern recognition. Other examples of fact-based questions include:
-
What are the most common signs and symptoms of gastritis?
-
What physical exam findings would you expect to see in a patient with cirrhosis? How does cirrhosis cause thrombocytopenia?
-
Sam is unable to answer basic fact-based questions. The residents supervising her on the clerkship clinical team report that her knowledge deficits are global and not related to any one disease, organ system, or specialty of medicine. Sam reports that she hasn’t had as much time as she would like to study on this rotation and has not yet purchased the text recommended by the clerkship director. In the past week, her attending suggested she read about the presentation and diagnosis of pancreatitis and to look up the differential of upper gastrointestinal bleeding, but she has not done so yet.
-
3 Remediation Strategies
Since many struggling students believe putting more time into familiar study strategies will improve their performance, external input to help them master new, more efficient strategies is usually required [10–12]. We illustrate this by describing remediation tailored to three commonly encountered types of student issues that interfere with knowledge gain: lack of committed study time, distraction, and anxiety with low self-confidence. Consider using the algorithm in Fig. 3.2 to identify the problem and the best remediation strategy. In tailoring remediation programs, we seek to create opportunities for students to develop study strategy expertise and improve lifelong learning of medical knowledge by taking them through cycles of effortful practice, tailored feedback, and self-reflection. These are the key components of deliberate practice critical to developing expertise [13, 14] (see Chap. 1).
3.1 Remediation Strategy A: Lack of Committed Study Time (Sam)
We have found it critical to create a highly structured remediation process with students such as Sam who need explicit guidance toward high-yield material and the appropriate depth of learning. It is especially important to make specific recommendations with strict time lines and clearly state that the process will take an extended amount of time and frequent and regular meetings with a supervisor. We give specific reading assignments with source and page numbers (e.g., “Internal Medicine Essentials for Clerkship Students, pages 75–99”), rather than leaving this up to the student by saying, “read about cirrhosis.” Initially, we are careful to choose material that is directly related to course or clerkship objectives and is of manageable length to be completed during the time available.
We work with the student to develop a specific study schedule including both the number of pages to be read and short-answer practice questions to be completed per day and week. If possible, we correlate the reading with clinical activities and make specific assignments for the student to do before, during, or after an educational experience. In this way, we model effective ways to blend background and just-in-time reading with experiential learning.
For students who routinely cram for exams, a strategy that may work in the short run, it is important to encourage them to actively learn material in depth to facilitate long-term retention and clinical application. As they read about a patient case, learners should be encouraged to go beyond answering the “what and how” questions and ask “why” questions. For example, if the student is reading about a patient with a flare of Crohn’s disease, the student should prepare to discuss not only that steroids are indicated and how to administer them but also why treatment with steroids is the best strategy.
3.1.1 Importance of Individual Characteristics
Individual characteristics have been found to be determinants of learning and performance, apart from one’s cognitive abilities [15]. Personal characteristics associated with achievement include openness, conscientiousness, dependability, curiosity, intellectual engagement, and mastery orientation—seeking to master the material rather than merely score well on an exam [16–18].
Millions saw the apple fall, but Newton was the one who asked why. —Bernard Baruch
Those who procrastinate and work to avoid appearing incompetent—a performance orientation—are most likely to underachieve [19]. Making students aware of this and asking them to reflect on their own characteristics may help motivate them to change their behavior around and attitude toward learning. Engaging a student in a dialogue about the need for physicians to develop lifelong learning skills and a mastery orientation will help motivate them to put effort into changing ineffective study habits (see Chap. 13).
To take advantage of the “learning through testing” effect mentioned above, the student should be expected to take weekly quizzes based on her required reading, to both encourage her to adhere to the study schedule and focus her studying on identified gaps in knowledge rather than simply restating or rereading material. If practical, the quizzes should require students to provide short answers (e.g., fill in the blank to stimulate recall) rather than MCQ-type questions which rely on recognition of the correct answer. This can be created efficiently by asking students to answer MCQ questions before looking at the answer options. This is often called the “cover the options” approach.
Lastly, give the student the opportunity to reflect on new study methods. What have been the pros and the cons of having such a strict study schedule with weekly quizzes? What has she noticed about how this has affected her performance in the clinical setting? Does she now have more to add to patient or education discussions? Is she better able to follow these discussions? Ideally, in this metacognitive way (Chap. 13), you can facilitate the student making positive links between greater effort on her part and the greater level of commitment in her achievement from faculty [20].
3.2 Remediation Strategy B: Distracted Student (ADHD) with Chronic Low-Test Scores (Raj)
-
While he enjoyed his rotations in obstetrics and gynecology and internal medicine, Raj failed the NBME subject tests in his first two clinical clerkships, and he is not surprised. He reports that he has always been a “bad test taker” but is adamant that his medical knowledge is as good as his peers as demonstrated on his clinical performance evaluations.
-
All three subscores of his MCAT as well as his preclinical exam scores were consistently in the bottom quintile of his class. Raj spends 2 h every evening reading the review textbook recommended by the clerkship, plus completing practice questions. He desperately wants to address this situation. When asked for more detail, he admits to only being able to complete two to five pages of reading per night and about two or three practice questions. He finally admits that he carries the diagnosis of Attention Deficit Hyperactivity Disorder (ADHD) and that because he feared being stigmatized, he has not requested testing accommodations or sought treatment.
Attention deficit hyperactivity disorder is one of the most common learning disorders seen in medical schools, and it is associated with poor attention, impulsivity, distractibility, restlessness, impaired organization and time management, and procrastination [21, 22]. These features impact both the acquisition of knowledge and test taking. While both male and females are affected by ADHD, girls are diagnosed at a lower rate [23, 24] (see Chaps. 9 and 12).
Without support, these students are unable to get through an adequate proportion of the material during their study time and retain less of it compared to their peers. With earlier diagnosis of learning difficulties and more effective interventions for people with ADHD, increasingly students arrive in medical school with a much more sophisticated understanding of their situation and are better prepared to strategize effectively and advocate for their own learning needs. The prognosis for students like Raj is good if competent study skills coaching is available. This includes focus on organizing study material, transforming from passive to active study strategies, and learning strict time management techniques. Referral to determine if medication treatment is appropriate is also important (see Chap. 12).
3.2.1 Study Skills Coaching
Study skills coaching is readily available in most academic communities. Even if the individual coach has no prior experience working with professional school students, in our experience most are able to work effectively with medical students in consultation with an experienced clinician educator.
Strategies that help students become active studiers include requiring students to maintain and follow a detailed study calendar, which includes both exact material to cover in a time period and regular breaks (e.g., “joy breaks”). A student should be coached to take written notes as he reads and advised to keep a list of the challenging content. He should create his own mnemonics, visual maps, charts, pictures, and algorithms from the extracted material. Students should summarize each section or teaching session in writing, identifying the major themes, important facts, the take-home points of figures, tables, and cases, and write down any questions they still may have about the material [20]. Their self-generated questions can then be discussed with their mentor, supervising residents, supervising or course faculty, and in study groups with their peers. Innovative technology is available to assist students with difficulty “capturing” information in writing (see Chap. 9).
3.2.2 Time Management
Time management is essential to remediation and improves exam scores [25]. Many students with ADHD struggle to manage their time during an exam: either they rush through questions due to their underlying impulsivity or get distracted and don’t have enough time to finish. For test taking itself, there are numerous helpful strategies. Getting to know the test, including its format, the number of sections and the number of questions per section, the types of questions being asked, and how much time they will have for each section, is critical. For some tests, a breakdown of topics is also helpful as it will direct the learner to study the highest-yield topics first. Direct students to practice exams or sample questions such as USMLE World questions or even Kaplan flash cards on the 200 most likely diagnoses, Diagnosis, and Pharmacology and Treatment [26, 27].
3.2.3 Training for Test Taking
Practice answering questions has been shown to directly improve testing performance [28–33]. The practice test environment should simulate the level and type of distractions of the actual testing environment and accurately mimic the exam, with the same number of questions and allotted time. Students should practice answering the easiest questions first, then complete the remaining questions, rather than answering questions in order and be encouraged not to rush as they will be more likely to make careless errors. On the other hand, if a question is taking more than 4–5 min, they should move along to the next question. During the final 2 min of the time period, have the learner fill in answers to the unanswered questions. They should not leave any questions blank [26, 27]. As a benchmark, for performing well on the USMLE steps, the average student needs to read one review book series, completely from start to finish, at least once, then study their note and complete 1,500 questions. An alternative focused strategy is to complete 2,500 questions and thoroughly review the explanations for each answer and look up topics that they do not know well [34].
For case-based or long-format questions, the student with ADHD should read the question at the end of the passage first, then go back and read through the body of the questions. This way the distracted reader is not trying to remember all of the details by the time they get to the question. The more efficient student is better able to focus on the important data, rather than trying to manage all of the information from the question in their working memory. This capacity to decide on and attend to the most critical elements of the situation is referred to as salience determination [35]. Starting with the question first trains learners with ADHD to improve his or her salience determination capacity.
Another technique involves helping learners to switch perspectives on a question. Some learners prefer to view the world through a big picture lens and others tend to initially see each tree first rather than the forest. Both are necessary. If the learner is struggling with a question or concept, have him or her try looking at it from both views. Likewise, some learners place more weight on concrete information, details and facts, while other learners work better with abstract concepts and theories. It is important for learners to understand their own preferred approach and be able to switch perspectives; this perspective switching may help distracted learner attend longer and therefore improve performance (see Chap. 13).
For MCQ test questions, be sure to instruct the student to look at all of the answer choices, eliminating the incorrect choices and choosing from the remaining [26, 27]. If a learner narrows the answers down to two choices but consistently gets stuck, the learner lacks specificity of knowledge and needs to go back and focus more on the details during study, as well as the big picture. Statistically speaking, if this occurs during the test, the student should choose the answer furthest down on the answer choice list. For example, if a, c, and d have been eliminated, leaving b and e, the learner should choose e [26].
Using these techniques on practice questions and exams will help provide the learner with feedback on the progression of their knowledge, the effectiveness of different study and test-taking strategies, and optimal pacing for studying and completely exam questions. Practice test data should be monitored to provide feedback on the effectiveness of study and testing strategies. Such learning should be noted and reinforced until better strategies become routine.
3.2.4 Self-Regulation
Students should identify their most productive time of day for studying and monitor such relevant issues such as how much sleep they receive and require; use of caffeine, over-the-counter medications, and prescription medications; and the role of exercise and study location (e.g., students with ADHD paradoxically prefer public locations such as coffeehouses rather than being isolated) in helping them with attention to study. A medical evaluation or psychiatric evaluation may be warranted for medication recommendations and sleep problems. Sleep and poorly treated or untreated mental illness affect alertness and efficient use of time. Specific distracters and interruptions should be identified and eliminated to make study time more efficient and more productive [20]. The student may need advice on confronting their family members’ and friends’ wishes and expectations to preserve the necessary amount of protected study time.
3.3 Remediation Strategy C: Anxiety, Confidence, and Chronic Low-Test Scores (Juan)
-
Juan admits that taking tests is extremely anxiety provoking, and when he gets anxious, it slows him down and he starts thinking in his native language, Spanish. Juan calls the school’s education specialist to help him get ready for taking USMLE Step 1, though he isn’t sure he will ever pass the test or graduate from medical school. In the past, Juan consistently scored in the bottom 10 % on exams and has had to repeat one course each of the past 2 years. Juan has been reading and re-reading the suggested board preparation text and bank of questions for the past year, as the sections correlated to his classroom courses. He has never been evaluated for a learning disability and has never sought testing accommodations. Although he lives with his family to reduce the cost of his education, they are extremely supportive of his study time and proud that he is the first member of his family to attend graduate school.
Chronic anxiety has been consistently associated with poor performance on cognitive assessments [36, 37]. However, the nature of this correlation is not well delineated. While people that are worried tend to perform poorly [38], the data do not explicitly demonstrate that anxiety significantly influences exam scores. Instead, it may be that text anxiety is the result of the deficit, not the cause [39]. Either students with less aptitude report higher levels of anxiety or poor study skills result in poor performance and increased anxiety [40].
In the United States, performance on academic subjects and achievement exam performance are negatively correlated with being black or Hispanic, lower socioeconomic status and parental education level, crowdedness of the home, and renting rather than owning a home. All this contributes to the finding that exam scores are lower for those who do not belong to the Anglo-middle-class culture [41] (see Chap. 8).
It is also known that students with higher confidence ratings perform better on tests [42]. Students and residents who view themselves as outside of the normative culture are more likely to struggle with confidence. Students and residents who consistently score at the bottom of their class will also lack confidence. The cycle continues as learners who lack confidence avoid challenging situations, such as course study groups and higher-level discussions [43].
The main remediation strategies for learners with anxiety, low confidence levels, and chronic low scores include fine-tuning study skills, increasing preparation for exams, and repetition. As mentioned earlier, the student should take written notes in English as he reads and attends teaching sessions. While note-taking in the prior case was encouraged to increase the student’s engagement, in this case, it is to help the learner build confidence in using both the English language and the new medical vocabulary. Native English speakers who do not learn languages easily may also struggle with acquiring the language of medicine. As with learning a new language, discussing medical terms and concepts is best practiced with those with fluency; therefore, the novice needs to seek out opportunities to engage in discussions rather than avoiding them.
3.3.1 Taking Advantage of Aural and Visual Learning
In addition to all the strategies mentioned above, this type of student should audio record a summary of their notes and listen to the recordings on their way to work, while walking the dog, or while working out at the gym. The repetition involved in making and listening to such recordings takes advantage of the multimedia effect of processing information using dual channels, both aurally (words) and visually (pictures) [44], and helps the student solidify and retain the material in a retrievable form. Greater comfort with the material will help decrease anxiety and increase confidence walking into writing exams and other evaluative assessments.
3.3.2 Slow Reading Rate
For learners for whom English is a second language, either having immigrated to seek a medical education or having grown up in the United States in non-English-speaking households or communities, often notice that it takes them longer to complete exams and to read and process information than their peers. This slow reading rate may also be seen in native English speakers (“slow processors”). Often such students have been tested and have received time accommodations on written tests. Students with a slow reading rate can partially overcome this deficit through training by completing large volumes of practice test questions under timed conditions. It may be helpful for students with similar struggles to share their experiences, or even with faculty members who experienced similar challenges.
Such students need to become highly self-aware and develop a repertoire of strategies to ensure that they achieve their goals and meet competency standards. In addition to all the study and test-taking strategies discussed above, the student or resident may need a mentor’s support to establish boundaries with others or give up other nonacademic tasks and responsibilities to preserve the necessary amount of protected study time.
3.3.3 A Good Use of the Medical Educator’s Time
Much of what we have covered in this chapter can and should be done by the student working with a study skills coach or if one is available or competent peers who can function as tutors. The medical teacher’s role should usually be in identifying students who need help, structuring and monitoring the remediation process, and participating in making summary judgments about a student’s success in remediation.
As content experts, the medical educator must lend a hand when content is an issue. We recommend content experts avoid telling information to students who struggle and instead facilitate the student’s learning through reviewing the practice questions the learner got wrong. This is a practical and focused way for the medical educator to directly assist in the remediation of the student with insufficient medical knowledge. It allows the expert to focus on filling specific knowledge gaps and coaching active learning strategies.
The faculty coach should ask the student to rephrase the question to demonstrate understanding of the concept being assessed. Have the learner explain why the given answer is correct and the incorrect answers are wrong to ensure factual knowledge is learned. Then work with the learner to identify keywords to help him or her develop the ability to distinguish salient information from distracting facts. Encouraging the learner to write their own multiple choice question on a challenging topic actively engages the student in encoding, retrieving, and applying information to authentic scenarios [45]. Some course directors routinely have students write test questions as a study strategy.
3.3.4 Determining When Medical or Neuropsychological Testing Is Indicated
All along the way, and especially if above recommended remediation methods are not successful, consider cognitive or neuropsychiatric testing to look for new or undiagnosed learning disabilities from physical or mental illness. Signs of an underlying learning disability include prior difficulties in school; uneven strengths such as scoring high on physical science and biological science but low on verbal reasoning; difficulty understanding and following instructions; trouble remembering what someone just told him or her; difficulty distinguishing right from left; difficulty identifying words or a tendency to reverse letters, words, or numbers; lack in physical coordination; frequent loss or misplacement of items; or difficulty understanding the concept of time [46]. Other clues that neuropsychiatric testing would be helpful include head trauma; failure to achieve developmental milestones as a child, such as delayed language development; exposure to drugs, alcohol, or maternal illness in utero; exposure to chemicals, toxins, or heavy metals; tics; seizure disorders; substance abuse; strokes; and psychiatric disorders (see Chap. 9).
4 Summing Up
Sam’s Story
-
Sam works closely with a mentor who helps her design a study schedule. She is disgruntled that she must take weekly quizzes, until she notices that her overall performance is improving and that her improved knowledge base allows her to be more engaged on rounds, with patient care and in working with the resident teams. She even received the second highest score on her Internal Medicine NBME subject exams.
Raj’s Story
-
With advice and support from his attending physician, Raj sought counseling and pharmacologic treatment for his ADHD. His studying has become much more efficient and interactive, as he has begun creating visual maps and algorithms for everything he reads. He no longer needs to stay up all night to get through the required material and is able to wake up early in the morning to run for 45 min before work. Overall he is feeling less burnt out, and he has passed the remaining shelf exams.
Juan’s Story
-
Juan is frustrated that he must study more than his peers. However, the time and repetition are paying off. For Juan, taking notes, recording his own voice explaining concepts, and listening to the recordings on his way to work have been most helpful. He has begun sharing his struggles with a few of his classmates and has found them to be very supportive. They have been available to discuss concepts with him to reinforce what he is learning, and he has found the confidence to engage more with the resident and faculty members on his teams. Juan took a month off of clinical rotations to concentrate on practice questions prior to USMLE Step 2, and it paid off. He was able to complete all of the questions and received an average score.
We have illustrated road-tested effective remediation strategies for the most common types of medical students presenting to our program with concerns about their medical knowledge. We describe an approach, which is tailored to individual learners, closely supervised and includes deliberate practice, which is effortful, challenging, and supported with multiple sources of feedback and requires metacognitive awareness through self-reflection.
5 Recommendations for Preventing and Addressing Medical Knowledge Deficits
5.1 At the Program Level
-
Consider proactive introductory classes on study, cognitive, and metacognitive skills [47, 48].
-
Encourage use of the school’s academic support to identify resources locally [49].
-
Provide a list of the most appropriate reading material and access to question banks.
-
Identify a pool of students, residents, and faculty who are skillful tutors and good role models.
5.2 At the Individual Student Level
-
Help the students develop a study schedule.
-
Encourage openness, conscientiousness, dependability, individual curiosity, intellectual engagement, and mastery of material.
-
Warn against procrastination and effort and time invested in appearing competent.
-
Instruct the students to focus on learning and understanding rather than just remembering or memorizing.
-
Encourage the student to take written notes on reading and attend teaching and group study sessions.
-
Consider having the student audio record their notes or a summary of their notes and listen to the recordings.
-
Encourage students to learn the language and vocabulary of medicine by discussing questions that arise while studying with a knowledgeable other.
-
Find efficient protected time to study.
-
Identify most productive time of day for studying.
-
Get at least 6 h of sleep per night.
-
Limit caffeine and use medication appropriately.
5.3 Test Preparation Advice
-
Make liberal use of practice tests and practice questions.
-
When studying from practice questions:
-
If you find you consistently narrow the answers down to two choices, you lack specificity of knowledge in that domain. Read more.
-
Make sure you are able to rephrase questions, explain why the given answer is correct and the incorrect answers wrong, and identify the keywords.
-
Analyze and monitor the reasons why you get practice questions wrong. A knowledge deficit? Why didn’t you know this material? Not enough time spent? Did you misread the question? Get discouraged or anxious? Document lessons learned.
-
Track practice scores and document lessons learned.
-
Learn to manage time during exams.
-
Take practice tests in an environment that simulates the testing environment.
-
Review lessons learned about test taking before the exam.
-
5.4 Test-Taking Tips
-
Be familiar with the test format and content.
-
Keep track of how long it takes to complete a certain number of questions.
-
Practice answering the easiest questions first.
-
Do not to rush through any one question.
-
If a question is taking more than 4–5 min, move on.
-
During the final 2 min of the time period, fill in answers to the unanswered questions.
-
For long-format questions read the question at the end of the passage first.
-
Try looking at questions from both the big picture view and the detailed view.
5.5 Faculty Development Objectives
-
1.
Differentiate the presentation of medical knowledge deficits from other types of deficits.
-
2.
Be able to interview learners to obtain information relevant to designing a remediation plan.
-
3.
Be able to implement the three remediation plans for learners who fit into those categories.
-
4.
Construct and implement a remediation plan from the study tip and test-taking tip lists for learners.
References
Olmesdahl PJ. The establishment of student needs: an important internal factor affecting course outcomes. Med Teach. 1999;21(2):174–9. doi:10.1080/01421599979824.
Hinman PG, Dottl S, Passon J. Academic development: a survey of academic difficulties experienced by medical students and support services provided. Teach Learn Med. 2009;21(3):254–60. doi:10.1080/10401330903021041.
Cleland J, Arnold R, Chesser A. Failing finals is often a surprise for the student but not the teacher: identifying difficulties and supporting students with academic difficulties. Med Teach. 2005;27(6):504–8. PMID: 16199356.
Guerrasio J. Remediation program successes. Poster session presented at federation of states physician health programs, Fort Worth, TX; 2012.
Wiese JG. Strong as our weakest link. Presentation. San Francisco, CA: UCSF Grand Rounds; 2005.
Hoffman KI. The USMLE, the NBME subject examinations, and assessment of individual academic achievement. Acad Med. 1993;68(10):740–7. PMID: 8397598.
Rohrer D, Pashler H. Recent research on human learning challenges conventional instructional strategies. Educ Res. 2010;39(5):406–12. doi:10.3102/0013189X10374770.
Bloom BS, Engelhart MD, Furst EJ, Hill WH, Krathwohl DR. Taxonomy of educational objectives: the classification of educational goals/handbook I: cognitive domain. New York, NY: Longmans; 1956. p. 206.
Anderson LW, Sosniak LA, Bloom BS. National society for the study of education. Bloom’s taxonomy: a forty-year retrospective. Chicago, IL: National Society for the Study of Education (NSSE); 1994. p. 214.
Loyens SMM, Rikers RMJP, Schmidt HG. The impact of students’ conceptions of constructivist assumptions on academic achievement and drop-out. Stud High Educ. 2007;32(5):581–602.
Sayer M, Chaput De Saintonge M, Evans D, Wood D. Support for students with academic difficulties. Med Educ. 2002;36(7):643–50. PMID: 12109986.
Mattick K, Knight L. High-quality learning: harder to achieve than we think? Med Educ. 2007;41(7):638–44. PMID: 17614883.
Hauer KE, Ciccone A, Henzel TR, Katsufrakis P, Miller SH, Norcross WA, Papadakis MA, Irby DM. Remediation of the deficiencies of physicians across the continuum from medical school to practice: a thematic review of the literature. Acad Med. 2009;84(12):1822–32. doi:10.1097/ACM.0b013e3181bf3170.
Gladwell M. Outliers: the story of success. New York, NY: Little, Brown and Company; 2008. p. 309.
Beier ME, Campbell M, Crook AE. Developing and demonstrating knowledge: ability and non-ability determinants of learning and performance. Intelligence. 2010;38(1):179–86. doi:10.1016/j.intell.2009.09.007.
Barrick MR, Mount MK. The big five personality dimensions and job performance: a meta-analysis. Pers Psychol. 1991;44(1):1–26. doi:10.1111/j.1744-6570.1991.tb00688.x.
Beier ME, Ackerman PL. Current events knowledge in adults: an investigation of age, intelligence, and nonability determinants. Psychol Aging. 2001;16(4):615–28. PMID: 11766916.
Colquitt JA, LePine JA, Noe RA. Toward an integrative theory of training motivation: a meta-analytic path analysis of 20 years of research. J Appl Psychol. 2000;85(5):678–707. PMID: 11055143.
Artino Jr AR, Dong T, DeZee KJ, Gilliland WR, Waechter DM, Cruess D, Durning SJ. Achievement goal structures and self-regulated learning: relationships and changes in medical school. Acad Med. 2012;87(10):1375–81. PMID: 22914521.
Connelly J, Forsyth PB. The study skills guide: essential strategies for smart students. Philadelphia, PA: Kogan Page; 2010. p. 166.
Hosterman JA, Shannnon DP, Sondheimer HM. American association of American medical colleges. Medical students with disabilities: resources to enhance accessibility. Washington, DC: Association of American Medical Colleges; 2010. p. 104.
American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM-IV. 4th ed. Washington DC: American Psychiatric Association; 1994. p. 886.
Arnold LE. Sex differences in ADHD: conference summary. J Abnorm Child Psychol. 1996;24(5):555–69. PMID: 8956084.
Gaub M, Carlson CL. Gender differences in ADHD: a meta-analysis and critical review. J Am Acad Child Adolesc Psychiatry. 1997;36(8):1036–45. PMID: 9256583.
Vrugt A, Oort FJ. Metacognition, achievement goals, study strategies and academic achievement: pathways to achievement. Metacogn Learn. 2008;3(2):123–46. doi:10.1007/s11409-008-9022-4.
Cutts J, Campbell M, Gotlib L, Oman D, Oman R, Wallace JS. MCAT. New York, NY: Barron’s; 2011. p. 983.
Magliore K. Cracking the AP biology exam. 2011th ed. New York, NY: Random House, Inc.; 2010. p. 360.
Thalheimer W. The learning benefits of questions; 2003. http://www.learningadvantage.co.za/pdfs/questionmark/LearningBenefitsOfQuestions.pdf
Gibbs G, Simpson C. Conditions under which assessment supports student learning. Learn Teach High Educ. 2004;1:3–31.
Sivagnanam G, Sarawathi S, Rajasekaran A. Student-led objective tutorial (SLOT) in medical education. Med Educ Online. 2006;11(7):1–10. http://med-ed-online.net/index.php/meo/article/view/4610/4789 doi:10.3402/meo.v11i.4610.
Pashler H, Bain PM, Bottge BA, Graesser A, Koedinger K, McDaniel M, Metcalfe J. Organizing instruction and study to improve student learning (NCER 2007-2004). Washington, DC: National Center for Education Research, Institute of Education Sciences, US Department of Education; 2007. http://ies.ed.gov/ncee/wwc/pdf/practiceguides/20072004.pdf
Larsen DP, Butler AC, Roediger 3rd HL. Test-enhanced learning in medical education. Med Educ. 2008;42(10):959–66. doi:10.1111/j.1365-2923.2008.03124.x.
Marcell M. Effectiveness of regular online quizzing in increasing class participation and preparation. Int J Scholarsh Teach Learn. 2008;2(1):1–9.
Guerrasio J. Remediation of the Struggling Medical Learner. Irwin, PA: Association for Hospital Medical Education; 2013.
Kelly DP, Levine MD. A neurodevelopmental approach to differences in learning. In: Fine AH, Kotkin R, editors. Therapist’s guide to learning and attention disorders. San Diego, CA: Elsevier Science; 2003. p. 87–108.
Ackerman PL, Heggestad ED. Intelligence, personality and intelligence: evidence for overlapping traits. Psychol Bull. 1997;121(2):219–45. PMID: 9100487.
Hembree R. Correlates, causes, effects, and treatment of test anxiety. Rev Educ Res. 1988;58(1):47–77.
Eysenck HJ, Eysenck MK. Personality and individual differences: a natural science approach. New York, NY: Plenum; 1985. p. 424.
Covington MV, Omelich CL. “I knew it was cold before the exam”: a test of the anxiety blockage hypothesis. J Educ Psychol. 1987;79(4):393–400. doi:10.1037/0022-0663.79.4.393.
Zeidner M. Test anxiety: the state of the art. New York, NY: Plenum; 1998. p. 440.
Elliott R. Tests, abilities, race and conflict. Intelligence. 1988;12(4):333–50.
Stankov L, Crawford JD. Self-confidence and performance on tests of cognitive abilities. Intelligence. 1997;25(2):93–109.
Fenollar P, Roman S, Cuestas PJ. University students’ academic performance: an integrative conceptual framework and empirical analysis. Br J Educ Psychol. 2007;77(Pt 4):873–91. PMID: 17535509.
Mayer RE. Cognitive theory of multimedia learning. In: Mayer RE, editor. The Cambridge handbook of multimedia learning. New York, NY: Cambridge University Press; 2005. p. 31–48.
Winston KA, Van der Vleuten CP, Scherpbier AJ. An investigation into the design and effectiveness of a mandatory cognitive skills programme for at-risk medical students. Med Teach. 2010;32(3):236–43. doi:10.3109/01421590903197035.
American Academy of Child and Adolescent Psychiatry. Children with learning disabilities. Facts for Families. 2011;16:2. http://www.aacap.org/AACAP/AACAP/Families_and_Youth/Facts_for_Families/Facts_for_Families_Pages/Children_With_Learning_Disabilities_16.aspx
Flavell JH. Metacognition and cognitive monitoring: a new area of cognitive-developmental inquiry. Am Psychol. 1979;34(10):906–11.
Mevarech ZR, Amrany C. Immediate and delayed effects of metacognitive instruction on regulation of cognition and mathematics achievement. Metacogn Learn. 2008;3(2):147–57. doi:10.1007/s11409-008-9023-3.
Saks NS, Karl S. Academic support services in U.S. and Canadian medical schools. Med Educ Online. 2004;9(6):1–8. doi:10.3402/meo.v9i.4348.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer Science+Business Media New York
About this chapter
Cite this chapter
Guerrasio, J. (2014). “She Needs to Read More”: Helping Trainees Who Struggle with Medical Knowledge. In: Kalet, A., Chou, C. (eds) Remediation in Medical Education. Springer, New York, NY. https://doi.org/10.1007/978-1-4614-9025-8_3
Download citation
DOI: https://doi.org/10.1007/978-1-4614-9025-8_3
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4614-9024-1
Online ISBN: 978-1-4614-9025-8
eBook Packages: MedicineMedicine (R0)