Abstract
Fifty-two percent of all surgical patients will experience postoperative nausea and vomiting (PONV) when no antiemetics are used. Risk factors include female sex, nonsmoker, having a history of motion sickness, or PONV. Anesthetic risk factors include not receiving a total intravenous anesthetic (TIVA), receiving opioids, exposure to nitrous oxide, and the length of the anesthetic. Class/type of antiemetic or not using a triggering anesthetic technique was associated with the same decrease in PONV, and to each was attributed a 26 % decrease in PONV. Additionally, patients are willing to pay between $56 and $100 out of pocket to receive an antiemetic that is completely effective. Neostigmine has been found to be a triggering agent at a dose above 2.5 mg in some studies, but other studies have failed to show any correlation between neostigmine and PONV. A recent meta-analysis showed that inhaled isopropyl alcohol was more effective than placebo, but less effective than standard antiemetics.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Motion Sickness
- Postoperative Nausea
- Serotonin Receptor Antagonist
- Chemoreceptor Trigger Zone
- Favorable Side Effect Profile
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Introduction
Fifty-two percent of all surgical patients will experience postoperative nausea and vomiting (PONV) when no antiemetics are used. Risk factors include female sex, nonsmoker, having a history of motion sickness, or PONV. Anesthetic risk factors include not receiving a total intravenous anesthetic (TIVA), receiving opioids, exposure to nitrous oxide, and the length of the anesthetic. Class/type of antiemetic or not using a triggering anesthetic technique was associated with the same decrease in PONV, and to each was attributed a 26 % decrease in PONV [1]. Additionally, patients are willing to pay between $56 and $100 out of pocket to receive an antiemetic that is completely effective [2]. Neostigmine has been found to be a triggering agent at a dose above 2.5 mg in some studies, but other studies have failed to show any correlation between neostigmine and PONV [3]. A recent meta-analysis showed that inhaled isopropyl alcohol was more effective than placebo, but less effective than standard antiemetics [4].
The chemoreceptor trigger zone is located outside the blood-brain barrier in the medulla and is responsible for beginning the emesis process. Lesions of the area do not prevent emesis due to vagal stimulation or motion [5]. The CTZ is rich in chemical receptors, and antagonists to these receptors have become the mainstay of PONV prevention. While not well studied, PONV in diabetic patients with gastroparesis can be treated with metoclopramide.
Drug Class and Mechanism of Action
Serotonin Receptor Antagonists (see Fig. 28.1)
5-hydroxytryptamine3 (5-HT3) receptor antagonists Thompson [22]
Serotonin released from enterochromaffin cells of the small intestinal mucosa binds to the 5-hydroxytryptamine type 3 (5-HT3) in the CTZ. Most of the 5-HT3 blockers (ondansetron, granisetron) competitively antagonize these receptors and receptors in the gut [6]. The newest 5-HT3 antagonist (palonosetron) allosterically binds and causes downregulation of this type of serotonin receptor, possibly contributing to its long half-life [7]. It may also inhibit the emetic response caused by substance P, a characteristic shared by the NK1 receptor antagonists [8]. In a recent study, it was shown to be as effective as other 5-HT3 blockers plus dexamethasone and more effective than the others alone [9].
Corticosteroids
Dexamethasone and other corticosteroids stabilize liposomal membranes and interfere with the synthesis of prostaglandins [10].
Anticholinergics
Scopolamine
While there are many anticholinergic agents, only scopolamine is used in the prevention of PONV by inhibiting the binding of acetylcholine in the vestibular system [11] and the cortex and pons [12]. It is available in IV or transdermal formulations. It has been shown to be effective across a wide range of surgery times as a preventative agent as opposed to a rescue medication. Additionally, patients receiving this antiemetic reported much higher satisfaction scores than those in other treatment groups despite a high incidence of side effects [13].
Substance P Receptor (NK1) Antagonists
Aprepitant has been found to be more effective than ondansetron at preventing PONV in the perioperative period [14]. It has been found to exert its effects via a final, more common pathway of the emetic centers after crossing the blood-brain barrier [15]. In fact, there were no improved outcomes when scopolamine and aprepitant were combined [16]. However, it has not led to complete abolishment of nausea, so other mechanisms may be involved.
Dopamine Antagonists
Droperidol and promethazine block the effects of dopamine on the CTZ, and promethazine has additional histamine-blocking properties [17].
Indications/Clinical Pearls
-
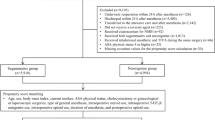
Le and Gan have developed an algorithm for the prevention of PONV based on risk factors. Risk factors include female sex, nonsmoker, having a history of motion sickness or PONV, and the use of opioids. For 0–1 risk factors, no antiemetics are recommended. For 2–3 risk factors, give one or two antiemetics, and if four or more risk factors are present, consider two or more antiemetics. TIVA can be used in place of one antiemetic [18] (See Fig. 28.2).
Fig. 28.2 A clinical decision algorithm for the prevention and treatment of postoperative nausea and vomiting (PONV) Le and Gan [18]
-
As mentioned, alcohol has been shown to be effective in the clinical setting. Owing to its parasympathetic mediation, nausea can be rapidly treated successfully with two alcohol pads in each nostril with four deep breaths through the nose. The mechanism is believed to be the noxious smell creating a sympathetic overdrive response, and it should be seen within 30 s to a minute.
Dosing Options [17]
Ondansetron should be given in 4 mg doses. Dexamethasone should be administered at a dose of 8 mg [17] and it should be given at least 2 h prior to the end of surgery [19]. Scopolamine transdermal patch (1.5 mg) should be applied the night before surgery and removed 24 h after surgery. Aprepitant should be given in a dose of 40 mg [14]. Droperidol should be administered in a dose of 0.625 mg.
Drug Interactions (Package Inserts)
Ondansetron should not be given with apomorphine or any agent that prolongs QTc. Dexamethasone has no interaction with commonly used operating room drugs. Scopolamine levels may be increased by ipratropium, magnesium sulfate, and droperidol. Aprepitant may increase the levels of corticosteroids. Droperidol should not be given with MAO inhibitors or other agents that prolong the QTc.
Side Effects/Black Box Warnings
Headaches and constipation are the most common side effects associated with ondansetron, and it has a black box warning for QTc prolongation, most commonly associated with high doses. Dexamethasone has many side effects, but rarely are any of them a concern with a single injection with the exception of perineal burning after rapid IV injection [20]. Aprepitant is associated with fatigue, constipation, weakness, and hiccups. Droperidol was issued a block box warning for prolonged QT syndrome. However, this is rarely seen in the low doses used to prevent PONV [21].
Summary
PONV is a frequent problem that rarely leads to hospital admission. Most of the antiemetics today are inexpensive and have a very favorable side effect profile. All classes of antiemetics have been shown to be somewhat efficacious, but much of the data is contradictory given the complex nature of PONV. Nausea and emesis are multifactorial, and, therefore, no one agent is likely to prevent PONV in all patients. A large number of patients need to be studied to best sort out individual variables. Identifying patients who are at high risk and giving appropriate preventative antiemetics can decrease PACU stays and increase patient comfort.
References
Apfel CC, Korttila K, Abdalla M, et al. A factorial trial of six interventions for the prevention of postoperative nausea and vomiting. N Engl J Med. 2004;350(24):2441–51.
Gan T, Sloan F, Dear Gde L, et al. How much are patients willing to pay to avoid postoperative nausea and vomiting? Anesth Analg. 2001;92(2):393–400.
Cheng CR, Sessler DI, Apfel CC. Does neostigmine administration produce a clinically important increase in postoperative nausea and vomiting? Anesth Analg. 2005;101:1349–55.
Hines S, Steels E, Chang A, et al. Aromatherapy for treatment of postoperative nausea and vomiting. Cochrane Database Syst Rev. 2012;4:CD007598.
Miller AD, Leslie RA. The area postrema and vomiting. Front Neuroendocrinol. 1994;15(4):301–20.
Andrews P, Rapeport W, Sanger G. Neuropharmacology of emesis induced by anti-cancer therapy. Trends Pharmacol Sci. 1988;9:334–41.
Rojas C, Stathis M, Thomas AG, et al. Palonosetron exhibits unique molecular interactions with the 5-HT3 receptor. Anesth Analg. 2008;107:469–78.
Rojas C, Li Y, Zhang J, et al. The antiemetic 5-HT3 receptor antagonist palonosetron inhibits substance P-mediated responses in vitro and in vivo. J Pharmacol Exp Ther. 2010;335:362–8.
Moon YE, Joo J, Kim JE, Lee Y. Anti-emetic effect of ondansetron and palonosetron in thyroidectomy: a prospective, randomized, double-blind study. Br J Anaesth. 2012;108:417–22.
Rich W, Abdulhayoglu G, Di Saia PJ. Methylprednisolone as antiemetic during cancer chemotherapy: a pilot study. Gynecol Oncol. 1980;9:193–8.
Pergolizzi JV, Philip BK, Leslie JB, Taylor R, Raffa RB. Perspectives on transdermal scopolamine for the treatment of postoperative nausea and vomiting. J Clin Anesth. 2012;24(4):334–45.
McCarthy BG, Peroutka SJ. Differentiation of muscarinic cholinergic receptor subtypes in human cortex and pons: implications for anti-motion sickness therapy. Aviat Space Environ Med. 1988;59(1):63–6.
Kranke P, Morin A, Roewer N, et al. The efficacy and safety of transdermal scopolamine for the prevention of postoperative nausea and vomiting: a quantitative systematic review. Anesth Analg. 2002;95:133–43.
Diemunsch P, Apfel C, Gan TJ, et al. Preventing postoperative nausea and vomiting: post hoc analysis of pooled data from two randomized active-controlled trials of aprepitant. Curr Med Res Opin. 2007;23(10):2559–65.
Minami M, Endo T, Kikuchi K, et al. Antiemetic effects of sendide, a peptide tachykinin NK1 receptor antagonist, in the ferret. Eur J Pharmacol. 1998;363:49–55.
Green MS, Green P, Malayaman SN, et al. Randomized, double-blind comparison of oral aprepitant alone compared with aprepitant and transdermal scopolamine for prevention of postoperative nausea and vomiting. Br J Anaesth. 2012;109(5):716–22.
Scuderi PE. Pharmacology of antiemetics. Int Anesthesiol Clin. 2003;41(4):41–66.
Le TP, Gan TJ. Update on the management of postoperative nausea and vomiting and postdischarge nausea and vomiting in ambulatory surgery. Anesthesiol Clin. 2010;28(2):225–49.
Elhakim M, Nafie M, Mahmoud K, et al. Dexamethasone 8 mg in combination with ondansetron 4 mg appears to be the optimal dose for the prevention of nausea and vomiting after laparoscopic cholecystectomy. Can J Anaesth. 2002;49:922–6.
Wang JJ, Ho ST, Tzeng JI, et al. The effect of timing of dexamethasone administration on its efficacy as a prophylactic antiemetic for postoperative nausea and vomiting. Anesth Analg. 2000;91(1):136–9.
White PF. Droperidol: a cost-effective antiemetic for over thirty years. Anesth Analg. 2002;95(4):789–90.
Thompson AJ. Recent developments in 5-HT3 receptor pharmacology. Trends Pharmacol Sci. 2013;34(2):100–9. doi:10.1016/j.tips.2012.12.002. ISSN 0165-6147.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Additional information
Disclosure
The opinions expressed in this manuscript are the opinions of the author and do not necessarily reflect the opinions of the US Air Force, Army, or government.
Chemical Structures
Chemical Structure 28.1
Dexamethasone
Chemical Structure 28.2
Scopolamine
Rights and permissions
Copyright information
© 2015 Springer Science+Business Media New York
About this chapter
Cite this chapter
Fields, A.M. (2015). Antiemetic Agents. In: Kaye, A., Kaye, A., Urman, R. (eds) Essentials of Pharmacology for Anesthesia, Pain Medicine, and Critical Care. Springer, New York, NY. https://doi.org/10.1007/978-1-4614-8948-1_28
Download citation
DOI: https://doi.org/10.1007/978-1-4614-8948-1_28
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4614-8947-4
Online ISBN: 978-1-4614-8948-1
eBook Packages: MedicineMedicine (R0)