Abstract
Nasal dermoid cysts are the commonest midline nasal defect. Histologicaly they contain both ectodermal and embryonal elements. Complete surgical excision is the recommended treatment. If left untreated there is potential for infection and consequent significant morbidity: brain abscess, meningitis, and frontal osteomyelitis.
Preoperative imaging is mandatory in order to assess the extent of lesion including whether intracranial extension is present. Magnetic resonance imaging (MRI) and computerized tomography (CT) provide complementary information. The optimum surgical approach for each patient depends upon the site and extent of the dermoid cyst, as determined by both clinical and radiological factors.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
First reported in 1817 by Cruvelier, congenital dermoid cysts contain ectodermal and embryonal elements, as opposed to teratomas, which contain elements from all three embryonal layers. Nasal dermoids account for 1–3 % of all dermoid cysts and approximately 10 % of all head and neck dermoid cysts [1, 2]. These benign lesions are the commonest diagnosis in a child who presents with a midline nasal defect. The differential diagnoses are nasal glioma or encephalocele.
Key Points
-
Commonest congenital midline nasal defect [3].
-
Potential for significant morbidity if becomes infected; brain abscess, meningitis and frontal osteomyelitis [4].
-
Complete surgical excision including excision of any intracranial extension is recommended.
-
The optimum surgical approach differs for each patient, depending on the site and extension of the lesion.
Biology and Epidemiology
Nasal dermoids are frontonasal inclusion cysts or tracts related to embryologic errors localized to the anterior neuropore . Grunwald described in 1910 the prenasal theory for the embryogenesis of a nasal dermoid cyst or tract. This theory was subsequently illustrated by Pratt in 1965 [5, 6].
Pathogenesis
-
At 8 weeks gestation, a dural diverticulum protrudes through the nasal and frontal bones, entering the space between the nasal bones and nasal capsule.
-
This diverticulum is subsequently surrounded by the frontal process of the nasal bones, hence separating the dura from the skin. Under normal circumstances, this diverticulum involutes, but incomplete closure results in a persistent attachment of the dura to the dermis.
-
As the dura recedes, dermis is pulled superiorly resulting in trapped epithelium along the diverticulum path.
-
These trapped elements result in a sinus tract and/ or cyst containing glands and hair follicles, located anywhere along the course of the diverticulum, from the columella to the anterior cranial fossa.
-
As a consequence, the cyst may be extranasal, intranasal, or a combination of the two. Intracranial extension usually communicates through the foramen cecum or the cribriform plate with extradural adherence to the falx cerebri.
Molecular/Genetic Pathology
-
Majority of dermoid cysts appear to occur spontaneously .
-
Familial tendency has been suggested but no genetic cause identified [7].
-
Nasal dermoids have been reported in a mother and identical twin daughters—suggesting an autosomal dominant inheritance in some rare patients [8].
Incidence and Prevalence
-
Uncommon lesion: estimated to occur in 1 in every 20,000–40,000 live births [9].
Age Distribution
-
Generally present at birth or in early childhood.
-
Mean age at presentation is 14–34 months [10].
-
Late presentation in adulthood does rarely occur [11].
Sex Predilection
-
Slight male predominance [10].
Risk Factors—Environmental, Life Style
-
None reported.
Relationships to Other Disease States, Syndromes
-
Nasal dermoids are not associated with any named syndrome .
-
However, other congenital anomalies have been reported in up to 41 % of cases, including cleft palate, aural atresia, hydrocephalus, craniosynostosis, hemifacial microsomia, lacrimal duct cysts, and hypertelorism [2, 12].
-
In the presence of other congenital anomalies the incidence of intracranial extension of the dermoid cyst is said to increase [12].
Presentation
Nasal dermoids present in early childhood as a midline mass, anywhere from the base of the columella to the nasoglabellar region. The reported incidence of intracranial extension varies widely from 5–45 % [6].
The mass is typically noncompressible and does not enlarge with compression of the jugular vein (negative Furstenberg sign). The mass may cause broadening of the nasal dorsum. The cyst may first present when it becomes infected with pain, tenderness and erythema.
Sixty percent are located on the lower nasal dorsum, 30 % are intranasal, and 10 % are combined intra- and extranasal.
A sinus opening is best appreciated by examining the nose with magnification. The opening may express sebaceous material. The presence of a hair follicle in the sinus opening is pathognomonic for a nasal dermoid .
Rarely, a nasal dermoid may present with local extension of infection such as a recurrent septal abscess, osteomyelitis, meningitis, or brain abscess.
Differential Diagnosis
The differential diagnosis of a midline nasal mass includes nasal dermoid, glioma, and encephaloceles (Table 15.1) . Differentiation between these entities relies upon clinical examination and radiological findings. Clinically, encephaloceles often transilluminate whilst nasal dermoids do not. Furthermore, encephaloceles tend to enlarge with straining, crying, or jugular vein compression (Furstenburg sign), whilst lesions that do not communicate intracranially (dermoids or gliomas) do not.
Diagnosis and Evaluation
Physical Examination
-
Noncompressible mass between columella and glabella.
-
Does not transilluminate.
-
Negative Furstenberg sign.
-
Broadening of nasal dorsum.
-
Widening of the anterior nasal septum.
-
Sinus opening may be difficult to see unless it contains sebaceous material or a hair follicle.
Imaging Evaluation
Preoperative imaging is mandatory in order to assess for intracranial extension as well as the extent of the cyst, with computerized tomography (CT) and magnetic resonance imaging (MRI) giving complimentary information. CT provides information on boney anatomy, whilst MRI determines the soft tissue characteristics. Traditionally, many centers have performed both investigations. However, with a heightened awareness of the potential long-term complications from the radiation exposure in CT, MRI is being increasingly utilized as a solitary investigation [13].
Computerized Tomography
-
Fine-cut CT (1–3 mm) of the anterior skull base is suggestive of intracranial extension if there is widening of the foramen cecum, a bifid crista galli, or a boney defect in the skull base. However, a fibrous attachment to the dura, without intracranial extension of the cyst may result in a widened foramen cecum and bifid crista galli, therefore mimicking intracranial extension on CT [14].
-
Images should include the entire nasal, ethmoid, and orbital region from the tip of the nose through the anterior cranial fossa. Contrast should be used in cases of infection and to differentiate a boney defect from enhancing cartilage as well as to differentiate between enhancing nasal mucosa and nonenhancing dermoids.
Magnetic Resonance Imaging
-
Multiplanar, high-resolution MRI using T1 images, fat-suppressed T2, fast-spin echo inversion recovery pulse sequences as gadolinium-enhanced, fat suppressed T1 images are used to deliver improved soft tissue resolution, particularly in patients who are suspected of having intracranial extension (Fig. 15.1).
-
Gadolinium contrast helps differentiate dermoids from other enhancing masses such as hemangiomas or teratomas.
Pathology
Macroscopic examination reveals a well-defined cyst lined by squamous epithelium of ectodermal origin with adnexal structures (i.e., hair follicle, sebaceous glands, and sweat glands) of mesodermal origin. These adnexal structures allow differentiation of dermoid cysts from epidermoid cysts . Furthermore, unlike teratomas, nasal dermoids do not contain tissue of endodermal origin (Fig. 15.2).
Treatment
Treatment entails complete surgical excision. Conservative procedures such as incision and drainage, aspiration, curettage, and subtotal excision fail to eradicate the cyst, with consequent high rates of recurrence [15, 16].
Surgical Therapy
A wide array of surgical approaches have been described. The optimum approach for each individual patient is determined by the site of the cyst, the site of any tract opening, the presence or absence of intracranial extension, and the surgeon’s experience.
Excision is performed under general anesthesia with a thorough examination of the nasal skin performed under magnification (prior to injection of local anesthesia), as a sinus tract opening may be visible that may not have been appreciated in the office.
-
In the absence of intracranial extension, the external rhinoplasty approach, a vertical incision over the cyst, a horizontal incision over the cyst, facial degloving approach, endoscopic transnasal approach, and a medial canthal incision have all been described [10].
-
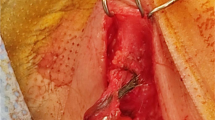
Excision of any sinus tract opening necessitates an incision on the nasal dorsum. Excision of the underlying cyst and tract via a vertical extension of this has remained the most traditional approach. The sinus tract opening is excised using a small elliptical incision and attempts are made to confine the vertical incision to the skin overlying the cartilaginous nose, as it is the senior author’s experience that skin in this area heals more satisfactorily than the skin overlying the boney nasal skeleton. Depending on the location of the cyst, this incision may be in continuity or separate from the elliptical incision around the sinus tract opening. This approach has been suggested to have superior cosmetic outcomes to lateral rhinotomy and horizontal incisions [17, 18] (Fig. 15.3).
Fig. 15.3 Examples of nasal dermoids in two separate patients. a Small cyst that was adjacent to the sinus opening, amenable to excision via a single elliptical incision. b Sinus tract opening at the nasal tip, with a sinus tract extending to a more cranially located cyst. In this patient two separate incisions were necessary
-
Cysts located near the nasal tip can be successfully approached via an external rhinoplasty incision, dissection being aided by otologic dissecting instruments and the use of a 0° sinus telescope. This approach has been suggested to have better cosmetic outcomes [19]. However, this approach is of limited utility if an external opening exists which needs to be excised via a separate incision and only gives limited access to the superior nasal dorsum.
-
If the sinus tract or cyst extends deep to the nasal bones, a nasal osteotomy is performed to improve access to the entirety of the cyst. The nasal bones are fractured and separated vertically over the dorsum of the nose at the nasofrontal suture. Meticulous care is required in following the entire tract and assessing for intracranial extension.
-
In some cases the preoperative imaging will suggest a sinus tract extending to the skull base, widening of the crista galli but no intracranial cyst. This may represent a vestigial fibrous tract rather than an epithelial tract. Faced with this situation, it is recommended to confirm the absence of epithelial components with a frozen section biopsy prior to suture ligation of the fibrous tract [1].
-
Definitive intracranial disease requires either a combined approach with neurosurgery utilizing a bifrontal craniotomy, or more recently a transglabellar sub cranial approach has also been described, which may obviate the need for a nasal dorsum incision [20] (Fig. 15.4).
Outcomes
Complete surgical resection is curative, however, recurrence and complicated infections can occur if epithelial tissue remains in situ following an incomplete resection. A recurrence rate of 12 % has been reported, with a mean time to recurrence of 3.6 years [10].
Follow-up
Due to the potential for recurrence years after resection, prolonged annual follow-up is recommended.
References
Sessions RB. Nasal dermal sinuses—new concepts and explanations. Laryngoscope. 1982;92:1–28.
Denoyelle F, Ducroz V, Roger G, Garabedian EN. Nasal dermoid sinus cysts in children. Laryngoscope. 1997;107:795–800.
Bloom DC, Carvalho DS, Dory C, Brewster DF, Wickersham JK, Kearns DB. Imaging and surgical approach of nasal dermoids. Int J Pediatr Otorhinolaryngol. 2002;62:111–22.
Blake WE, Chow CW, Holmes AD, Meara JG. Nasal dermoid sinus cysts: a retrospective review and discussion of investigation and management. Ann Plast Surg. 2006;57:535–40.
Pratt LW. Midline cysts of the nasal dorsum: embryologic origin and treatment. Laryngoscope. 1965;75:968–80.
Zapata S, Kearns DB. Nasal dermoids. Curr Opin Otolaryngol Head Neck Surg. 2006;14:406–11.
Anderson PJ, Dobson C, Berry RB. Nasal dermoid cysts in siblings. Int J Pediatr Otorhinolaryngol. 1998;44:155–9.
Bratton C, Suskind DL, Thomas T, Kluka EA. Autosomal dominant familial frontonasal dermoid cysts: a mother and her identical twin daughters. Int J Pediatr Otorhinolaryngol. 2001;57:249–53.
Szeremeta W, Parikh TD, Widelitz JS. Congenital nasal malformations. Otolaryngol Clin North Am. 2007;40:97–112, vi–vii.
Rahbar R, Shah P, Mulliken JB, et al. The presentation and management of nasal dermoid: a 30-year experience. Arch Otolaryngol Head Neck Surg. 2003;129:464–71.
Hacker DC, Freeman JL. Intracranial extension of a nasal dermoid sinus cyst in a 56-year-old man. Head Neck. 1994;16:366–71.
Wardinsky TD, Pagon RA, Kropp RJ, Hayden PW, Clarren SK. Nasal dermoid sinus cysts: association with intracranial extension and multiple malformations. Cleft Palate Craniofac J. 1991;28:87–95.
Lusk RP, Lee PC. Magnetic resonance imaging of congenital midline nasal masses. Otolaryngol Head Neck Surg. 1986;95:303–6.
Pensler JM, Bauer BS, Naidich TP. Craniofacial dermoids. Plast Reconstr Surg. 1988;82:953–8.
Yavuzer R, Bier U, Jackson IT. Be careful: it might be a nasal dermoid cyst. Plast Reconstr Surg. 1999;103:2082–3.
Vibe P, Lontoft E. Congenital nasal dermoid cysts and fistulas. Scand J Plast Reconstr Surg. 1985;19:105–7.
Kelly JH, Strome M, Hall B. Surgical update on nasal dermoids. Arch Otolaryngol. 1982;108:239–42.
Posnick JC, Clokie CM, Goldstein JA. Maxillofacial considerations for diagnosis and treatment in Gorlin’s syndrome: access osteotomies for cyst removal and orthognathic surgery. Ann Plast Surg. 1994;32:512–8.
Locke R, Rakhra J, Kubba H. A comparative study of two techniques for excision of midline nasal dermoids: how we do it. Clin Otolaryngol. 2011;36:252–5.
Goyal P, Kellman RM. Tatum SA, 3rd. Transglabellar subcranial approach for the management of nasal masses with intracranial extension in pediatric patients. Arch Facial Plast Surg. 2007;9:314–7.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer Science+Business Media New York
About this chapter
Cite this chapter
Kieran, S., Meara, J., Proctor, M., Rahbar, R. (2014). Dermoid: Nasal. In: Rahbar, R., Rodriguez-Galindo, C., Meara, J., Smith, E., Perez-Atayde, A. (eds) Pediatric Head and Neck Tumors. Springer, New York, NY. https://doi.org/10.1007/978-1-4614-8755-5_15
Download citation
DOI: https://doi.org/10.1007/978-1-4614-8755-5_15
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4614-8754-8
Online ISBN: 978-1-4614-8755-5
eBook Packages: MedicineMedicine (R0)