Abstract
Subarachnoid hemorrhage (SAH) is a devastating type of hemorrhagic stroke. It is characterized by spontaneous or traumatic bleeding in the subarachnoid space and is associated with a high rate of morbidity and mortality. A reproducible animal model of SAH that mimics the acute and delayed brain injury history after SAH will be an invaluable tool for exploring the underlying mechanisms of SAH-induced brain injury and evaluating potential therapeutic interventions. At present, a number of models have been developed, mainly the double injection model and the endovascular puncture model. While different species have been studied, rodents have become the most popular and widely utilized animal subjects. In this summary, we will explore in detail the various models and animal species. We will also introduce the emerging modified model, which was recently developed within the past 5 years, and discuss the prospective study.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Introduction
When healthy persons are suddenly seized with thunder pains in the head, quickly laid down speechless, and breathing with stridor, they die in 7 days. It was the earliest known description of subarachnoid hemorrhage (SAH) from Hippocrates. A World Health Organization report found the annual incidence of aneurismal SAH ranges from 2.0 to 22.5 cases per 100,000 population in age-adjusted adults [1]. Although SAH accounts for only 5 % of all strokes, its burden on society is relevant due to the young age at which it occurs, high mortality and disability, and poor outcomes [2]. Despite obliterating the offending aneurysm and removing the risk of rebleeding, the median mortality rate of SAH in epidemiological studies from the United States is 32 %, although this statistics does not fully account for prehospital deaths from SAH [3]. The hope of improving SAH patient outcomes has not been realized. Hence, further studies on the pathophysiology of SAH remain highly valued.
Recently, the theory that cerebral vasospasm is the only cause of brain injury in SAH patients is being increasingly questioned, and hypotheses of other mechanisms contributing to early or delayed brain damage are being discussed [4]. Delayed vasospasm was regarded as the single most important, treatable cause of mortality and morbidity after SAH. However, disappointing results from an endothelin receptor antagonist treatment, clazosentan, were observed in CONSCIOUS-2 trials [5]. Clazosentan succeeded in steering patients out of vasospasm in a randomized, double-blind, placebo-controlled, phase III trial (CONSCIOUS-3), but failed to reduce mortality [6]. Currently, more attention has been focusing on global cerebral injury within 72 h post-ictus, which was termed early brain injury (EBI) [7]. Multifactorial pathophysiological processes are considered to be the important triggers in SAH-evoked EBI, which involve acute elevated intracranial pressure (ICP), reduction in global cerebral blood flow (CBF), brain edema, oxidative stress, inflammation, and apoptosis [8]. Hence, it is very important to design and utilize a suitable model according to the intended research purpose.
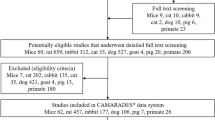
Ideally, studies on the pathogenesis and treatment of SAH should be using human cerebral arteries. However, using live human vessels is clearly not possible in in vivo experimental studies. In addition, only a little information can be obtained from postmortem evaluation of arteries taken from humans that died from SAH [9]. Moreover, there are no naturally occurring animal models of SAH. Hence, animal models of SAH in various species have been developed for this purpose. The first SAH model was invented in 1928. They infused blood into the subarachnoid space of a dog to simulate the lesion occurring in humans, where a small amount of blood escapes into the subarachnoid space. After its introduction, many techniques have been used to deliberately produce SAH in animals that recapitulate this vexing problem in humans [10]. So far, several animal species and SAH models have been developed to better understand SAH pathophysiology, including monkeys, baboons, pigs, rabbits, dogs, cats, rats, and mice [11]. Among those species, the rat is excellent for mimicking SAH because it is relatively inexpensive, easy to manipulate in a laboratory setting, and has been extensively studied. However, no animal model perfectly mimics the phenomenon of EBI and cerebral vasospasm in humans after SAH.
In this review, we will describe both the existing and emerging models and compare their advantages and disadvantages in order to help you choose the most suitable models for your aim.
2 In Vivo Models
In vivo experimental models have been used to investigate diverse aspects of SAH, including its natural history, pathophysiology, diagnosis, and treatment. More than 50 different experimental models have been identified with the aim of reproducing the clinical sequelae after SAH. These models used two major techniques to simulate SAH: (1) an artery was punctured, allowing blood to escape and collect around the artery and neighboring vessels; (2) an artery was surgically exposed and autologous blood, obtained from another site, was placed around the artery.
2.1 Vessel Dissection and Puncture Model
SAH is often elicited by aneurysmal rupture in humans. To closely mimic the human situation after SAH, many different bleeding techniques have been proposed and applied in several species, including mice, rats, rabbits, dogs, primates, cats, pigs, and goats [12].
The vessel avulsion in dogs was the first model used to characterize the biphasic, vasospastic response of large cerebral arteries after SAH [13]. The authors left a suture in the anterior cerebral artery (ACA) by a 4–0 silk loose ligature. Then pulling the suture in the external ear canal produced the ACA rupture. More importantly, they observed a biphasic phenomenon of SAH-induced vasospasm using this experimental technique. The acute phase occurred within minutes of the rupture and lasted no more than 1 h. The chronic phase occurred 3–24 h after the catastrophic hemorrhage and lasted for days. One clear advantage of this model is the biphasic phenomenon occurred repeatedly within the animals as they were awake, which mimics the clinical situation of sudden unconsciousness seen in humans. However, neurological function in this model was highly variable. A similar technique was performed to observe a biphasic vasospasm by Nagai and colleagues [14]. Willis circle was explored after a left subtemporal craniotomy. A threaded needle (~0.33 mm) was left in the posterior communicating artery (PCoA) to induce SAH. Their results suggested rapidly increased ICP seemed to be a crucial factor in producing diffuse early spasm. Asano et al. also performed the internal carotid artery (ICA) avulsion model by withdrawing a needle that was previously inserted into the ICA through a small craniectomy in the lateral base of the skull in dogs [15]. They observed the biphasic ICP pattern, which resulted in reactive hyperemia after the first ICP peak and failure to recover adequate CBF and EEG after the second, prolonged ICP elevation. Thus, they suggest an important role for the no-reflow phenomenon in the acute stage of SAH.
With the development of endoscopic methods, the preferred species in SAH studies changed from dog to murine. Murine became the most commonly used animals for SAH induction. Murine are relatively cheap and convenient for housing care and surgery. They also provoke less opposition from animal rights groups. Several early models that focused on vasospasm involved basilar artery puncture through the midline portion of clivus. In 1979, Barry et al. first tried to induce SAH by developing a lesion around the wall of the basilar artery with a stereotactically controlled tungsten needle, thereby emulating the natural occurrence of SAH. They controlled bleeding under an operating microscope, which is helpful in making a consistent and reproducible model [16]. Most importantly, this study determined the suitability of the rat for SAH models, although there were some deficiencies. The basilar artery puncture method of experimental SAH in rats holds promise for studying the chronic changes in CBF in the telencephalon, but it failed to produce chronic cerebral vasospasm and delayed cerebral ischemia [17]. It is widely accepted that the models utilizing transclival puncture of the basilar artery produce vasospasm 24 and 48 h after surgery and return to baseline after 72 h. However, the model presented several limitations, including the need for craniotomy and arachnoidal dissection or surgical placement of an infusion catheter, small and slow elevations of ICP, and limited blood distribution. To overcome these disadvantages, one new rat SAH model was developed, the endovascular suture technique [18, 19]. The endovascular perforation results in a very rapid and reproducible elevation of ICP, which is detectable from the beginning to 72 h after SAH [20, 21]. The endovascular perforation model exhibits pathological characteristics, such as rupturing of the main cerebral artery with arterial bleeding, and the model produces more profound pathophysiological and histological changes to the brain and cerebral vessels. The surgical procedure involves perforating the ICA near its intracranial bifurcation between the ACA and the middle cerebral artery (MCA) by means of a sharp ended 3–0 or 4–0 monofilament suture inserted through the stump of the external carotid artery (ECA). The suture passes through the common carotid artery (CCA) bifurcation and into the ICA. The filament is advanced distally into the intracranial ICA until resistance is felt and then pushed 2–5 mm farther to perforate the artery. Subsequently, the suture is withdrawn, producing SAH. The endovascular perforation model is able to represent clinical situations because it mimics intracranial aneurysmal rupture with a considerably high mortality ranging between 30 and 50 % after 24 h [22]. The best advantage of this puncture model is it does not require a craniotomy. Recently, the puncture SAH model is believed to better mimic the pathophysiological events after aneurysm rupture with a mortality rate similar to the clinical catastrophe seen in humans (40–50 %). Hence, of all the vessel puncture or avulsion models, the endovascular perforation model is very popular and most widely applied, especially in translational studies, although uncontrollable blood distribution is a well-known weakness of this model. In this approach, the types and sizes of the filament used to perforate a cerebral artery seems to be correlated with the amount of extravasated blood [23–25]. Some researchers tried to control the bleeding by keeping the suture in the artery, but they failed because ischemic development complicated the model.
Numerous transgenic mice have been generated, which are strong research tools. The transgenic mice are able to isolate a single gene product by either nullifying or augmenting gene expression. The transgenic models not only have the potential to provide insights into disease mechanisms but also are useful tools for testing new treatments for SAH. The inherent technical difficulty, however, in establishing a simple, reliable, and reproducible model in mice is the small size of the animal. With the development of microsurgical technology, the puncture technique was also adapted to mice. A mouse SAH model was produced by endovascular arterial rupture in the bifurcation of the ACA and MCA [26]. Recently, the therapeutic effect of some drugs against EBI was examined based on the mouse endovascular puncture model [27, 28]. Overcoming the apparent technical impediments in establishing a mouse model of SAH would be considerably valuable. Increased efforts should been directed toward developing a simple, reliable, and reproducible mouse model of SAH.
Non-human primates are very close in genome, anatomy, and physiology to humans, thus the models of SAH in non-human primates are believed to be the best candidates for replicating clinical SAH. The puncture monkey model through a small anterior craniotomy was first reported in 1968 [29]. A penetrating insult to the wall of a major cerebral vessel is sufficient to induce long-standing constriction in monkeys. Puncturing the ICA in primates can produce acute and delayed vasospasm [30]. However, a craniotomy is needed and delayed vasospasm was found in only 65 % of cases. More importantly, non-human primate models are usually time-consuming and demand complex surgical manipulation, such as anesthesia, angiography, and craniotomy.
Taken together, the endovascular perforation model (a non-craniotomy model) is believed to closely mimic the acute pathophysiological changes of an aneurysmal rupture in humans [25, 31] and was, therefore, selected for the investigation of EBI. However, the lack of control over the hemorrhage volume, resulting in a high morbidity and mortality rate, significantly impacts its use for therapeutic studies.
2.2 Blood Injection Model
The blood injection model, which directly injects blood into the subarachnoid space, is another widely used technique for inducing experimental SAH. This technique is able to elicit early and delayed vasospasm in a variety of species, although its presence depends on the site of injection.
In 1961, autologous blood was injected into the chiasmatic cistern using a small needle, which was the first to report a “one-hemorrhage” SAH experimental model [32]. It appears some animals had severe injuries with SAH symptoms. After 1 year, another new method was introduced to inject blood into the chiasmatic cistern using a needle passed under the zygomatic arch and directed toward the optic foramen. This and subsequent studies using the same model in dogs were used to analyze the effects of dehydrating agents in increased ICP [33, 34]. Also, primate models of SAH utilizing blood injection into the chiasmatic cistern through a transfrontal approach generally have high success rates of inducing cerebral vasospasm and producing high mortality rates, although scarce data have been reported on mortality and neurological scores [35]. Moreover, the prechiasmatic injection model in experimental rats was a suitable candidate to study the acute phase after SAH [36], because it produced a sudden increase in ICP to MABP levels, a significant decrease in CBF, and substantial neuronal death, even when observing the distribution of blood clots in the basal cisterns. Additionally, more than 90 % of SAH cases resulted from rupture of an aneurysm in the anterior circulation [37]. In some studies, however, the biphasic pattern of vasospasm was present only in small subgroups of animals after injecting fresh blood into the chiasmatic cistern through the optic canal following orbital exenteration, and the neurological deficits were none or only lasting a few hours [38].
To overcome the weakness of the chiasmatic cistern infusion model, a pioneering model was performed by means of blood injection into the cisterna magna in a small group of cynomolgus monkeys [39]. In this study, vasospasm seemed more pronounced with whole blood compared with serotonin, which corroborated with Echlin’s opinion that “other factors, not serotonin, in blood cause vasospasm” [40]. The study also demonstrated that introduction of blood into the cisterna magna induced at least as much or more constriction in the MCA than other intracranial arteries. Another line of investigation utilized the injection of autologous erythrocyte hemolysate into the cortex of mice. The arteries in the subarachnoid space were not directly assessed for vasospasm in this study. However, it is noteworthy that the hemolysate did not reach the basal cisterns and the acute mortality rate was 16 % [41]. In addition, vein blood obtained from a dog leg was injected into the cisterna magna, the subarachnoid space over the cerebral hemispheres, and, occasionally, the cerebral ventricles. Dogs with injected blood exhibited an altered clinical course as SAH patients, and pathological changes were observed in stained sections of their brains. The single blood injection model had observed maximal narrowing on days 2–4, but the double injection model had observed maximal narrowing on days 7–10 [12]. To improve the success rate, repeated injections of blood into the basal cisterns in the head-down position after injection was stressed to induce cerebral vasospasm, worsen neurological status, and create dysfunctional autoregulation [42]. In order to increase the precision of blood injections, stereotactic methods and catheter implantations were encouraged [43]. The next major advancement in the development of an SAH model was created by Varsos and collaborators [44]. They performed double-injections of autologous blood into the cisterna magna 48 h apart via small-gauge needles in dogs. The “two-hemorrhage” model was certified for better simulating vasospasm and has been used most frequently in inducing vasospasm after SAH. This double-injection model resulted in cerebral vasospasm development in 100 % of animals. This slight modification is a great step in the field of vasospasm study. This model also demonstrated an acceptable mortality [45]. The simplicity makes it a widely applied technique. However, there are some considerable drawbacks: (1) after injection of blood into the cisterna magna, neurological functioning usually remains intact, and the mortality rate is surprisingly lower than in humans, (2) because leakage of a considerable amount of blood during injection and after removal of the needle leads to an insufficient quantity of subarachnoid blood around the circle of Willis, even with the use of hemostyptic materials, the possibility of excluding animals is high, (3) this model requires two large surgeries to expose the femoral artery and the atlanto-occipital membrane. The second blood injection 24 or 48 h after the initial injection, which is obscured by the discolored and nontransparent dura mater, increases the risk of severe injury to the brain stem or cerebellum [46].
In conclusion, the double hemorrhage model represents a well-established experimental model frequently employed for delayed cerebral vasospasm, mainly defined by proximal vessel narrowing and neurological deterioration observed in the clinic. The great advantage of the SAH injection model is it allows for close control of subarachnoid blood volumes [47] and has a low morbidity and mortality rate, which are criteria for an ideal animal model [45].
3 In Vitro Model
Generally, there are two kinds of compounds that could produce delayed vasospasm after SAH: (1) some compounds or their metabolites found in blood, such as hemoglobin (Hb) and bilirubin oxidation products (BOXes), and (2) compounds regulated or induced from production of blood around blood vessels directly or indirectly from blood itself, blood vessels, or brain, such as endothelin or nitric oxide [48]. Neuron, astrocyte, and vascular smooth muscle cells were grown in culture and exposed to those compounds to mimic an in vitro model of SAH [49]. Vascular smooth muscle was predominantly used from CSF in SAH patients to force generation and reserve oxidative stress for vasospasm, but it is histologically, metabolically, and functionally abnormal in vessel walls. However, there are no good alternatives for in vitro SAH modeling that equal in vivo models.
4 Emerging Modified Models in the Last 5 Years
A CCA-prechiasmal cistern shunt model was established in which the SAH severity could be controlled by changing the bleeding time [50]. However, this model has uncontrolled pressure, is time-consuming, and demands delicate surgical manipulation. Fortunately, a closed-cranium ICP-controlled rabbit SAH model was performed using an extra-intracranial blood shunt from the subclavian artery into the cerebromedullar cistern [51, 52]. The blood shunt rabbit SAH model can mimic both EBI and vasospasm, eliciting acute physiological derangements, provoking marked and consistent early damage to the brain 24 h post-surgery, and triggering a high degree of delayed cerebral vasospasm. These findings make this model a valid tool for investigating pathophysiological mechanisms and novel treatment modalities for SAH. An advantage of this model is the consistent ICP, which is a desirable characteristic in an experimental SAH model. The initial event of increased ICP is considered to be crucial for early physiological derangements that are responsible for acute brain injury in aneurysmal SAH.
Another modification rat SAH model was presented by percutaneous injection of autologous, non-heparinized blood into the intracisternal space [53]. Once anesthetized, rats were fixed in a prone position in a stereotaxic frame. After finding the projection of the occipital bone, the needle is advanced toward the foramen magnum until it punctures through the atlanto-occipital membrane and obtains cerebrospinal fluid. Autologous blood was withdrawn from the tail and injected intracisternally. The average time between obtaining the blood and the start of the injection was very short, so the model did not require treating the blood with heparin to avoid coagulation at the time of injection. It could reduce the effect of Heparin in SAH models, since Heparin can reduce neuroinflammation and neuronal apoptosis [54]. This model is simple to perform, minimally invasive, quick, reproducible, and has low mortality, which makes it suitable for future studies on vasospasm-related delayed SAH complications.
The classical double injection model requires twice large surgeries to expose both the femoral artery and the atlanto-occipital membrane, which induces severe damage. To overcome these weaknesses, Dusick et al. set out to refine a minimally invasive modification that prevents confounding effects of surgical procedures, reduces leakage of blood from the subarachnoid space, and minimizes risk of infection [55]. The rat was placed prone with the head downward to 90° in a stereotactic frame, so that the cisterna magna was aligned with the intermeatal line. An angiocatheter is advanced in a vertical trajectory level with the external auditory canals. The needle is slowly advanced to puncture the atlanto-occipital membrane and observed for CSF. A syringe withdraws a small amount of CSF and the blood is injected into the subarachnoid space. After 24 h, the procedure was repeated. This model was feasible and produced neurological deficits as previous double-injection models. It consequently appears to be an excellent platform for future laboratories to study neuroprotective treatments for delayed vasospasm and neurological dysfunction following SAH.
A modified SAH model was presented in mice [56, 57]. Briefly, under general anesthesia, animals were flipped into the prone position. A mechanical support was placed under the clavicles to position the head flexed at a 30° angle. Using a surgical microscope, the posterior cervical muscles were initially dissected through a suboccipital midline skin incision. The transparent atlanto-occipital membrane and an underlying intracisternal vein were exposed. Blood was allowed to transect from the vein to the subarachnoid space through a pair of microjewelers. This procedure has the advantage of requiring surgery at only one site. The model not only inherited the advantages of currently used mouse models of vasospasm but also streamlined the procedure without losing reliable vasospasm development.
To circumvent the disadvantages of directly injecting blood into the cisterna magna, especially those related to the blind nature of the second injection, this study, based on the method from Solomon et al. [58], employed the injection of autologous blood into the cisterna magna via a thin catheter, which was carefully implanted through a small burr hole in the parieto-occipital. The catheter was left in position with a tight-fitting, flexible inner wire, allowing for SAH induction that is several times safer. Autologous blood was aspirated from a tube in the left femoral artery. Consequently, one strength of this model is its low mortality rate, only 1.5 %. Furthermore, the authors observed a lower blood volume resulted in a lower mortality rate. This low-mortality, double hemorrhage model seemed to be suitable for studying both acute and chronic injury after SAH [46].
5 Future Direction of the SAH Model
A suitable animal model to optimize the pathophysiology of SAH in humans remains a challenge. The limitations of recent models must be carefully considered. We propose some aspects to improve the SAH model for successful translation of pathophysiological concepts and therapeutics from bench to bedside.
Previously, neurovascular unit was restricted to endothelial cells, neurons and glia within millimeters of the cerebral capillary microcirculation. We now highlighted the roles of vascular smooth muscle, endothelial cells, and perivascular innervation of cerebral arteries in the neurovascular unit to prevent and progress the stroke. We also proposed that the vascular neural network should be considered the key target for therapeutic intervention after cerebrovascular damage in future [59].
All recent models aimed to mimic EBI and delayed vasospasm. However, little literature focused on long-term studies. Since one-third of SAH patients will survive and suffer with long-term disabilities, we should pay more attention to long-term SAH studies. Thus, a suitable model for long-term SAH study should be developed.
SAH is well known for inducing hydrocephalus, seizures, and other complications. Most studies report an overall 20–30 % incidence of hydrocephalus after SAH [60]. Those complications are often associated with unfavorable outcomes [61]. However, animal models focusing on complications after SAH are very rare. Future studies should differentiate suitable models in detail that target those complications.
SAH is also associated with weakness, fatigue, sleep disturbances, anxiety, depression, posttraumatic stress disorder, as well as cognitive and physical impairment [62]. Symptoms of depression and/or posttraumatic stress disorder have been shown to be present up to 41 % of post-SAH patients. Those symptoms are usually associated with white matter injury. The mechanism of post-SAH white brain injury remains unclear, possibly due to the lack of experimental studies. Thus, there is great need for development of animal models for post-SAH white matter injury.
Genome-wide association studies have identified novel genetic factors that contribute to intracranial aneurysm susceptibility. Hence, it is possible to produce an aneurysm on cerebral vessels experimentally using genetic technology [63]. We can study aneurysmal SAH using transgenic mice, which is close to the whole natural history in SAH patients.
6 Conclusion
In conclusion, although there are no ideal models or animal species that can mimic the natural history in SAH patients, each model can be used to study certain aspects of the pathophysiological process behind SAH. At present, there are no good alternatives for in vitro SAH modeling that equal in vivo models. Furthermore, future models focusing on complications after SAH are needed to improve SAH research and develop better outcomes for SAH patients.
References
Ingall T, Asplund K, Mahonen M, Bonita R (2000) A multinational comparison of subarachnoid hemorrhage epidemiology in the WHO MONICA stroke study. Stroke 31:1054–1061
Venti M (2012) Subarachnoid and intraventricular hemorrhage. Front Neurol Neurosci 30:149–153
Connolly ES Jr, Rabinstein AA, Carhuapoma JR, Derdeyn CP, Dion J, Higashida RT, Hoh BL, Kirkness CJ, Naidech AM, Ogilvy CS, Patel AB, Thompson BG, Vespa P (2012) Guidelines for the management of aneurysmal subarachnoid hemorrhage: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 43:1711–1737
Broderick JP, Brott TG, Duldner JE, Tomsick T, Leach A (1994) Initial and recurrent bleeding are the major causes of death following subarachnoid hemorrhage. Stroke 25:1342–1347
Macdonald RL, Higashida RT, Keller E, Mayer SA, Molyneux A, Raabe A, Vajkoczy P, Wanke I, Bach D, Frey A, Marr A, Roux S, Kassell N (2011) Clazosentan, an endothelin receptor antagonist, in patients with aneurysmal subarachnoid haemorrhage undergoing surgical clipping: a randomised, double-blind, placebo-controlled phase 3 trial (CONSCIOUS-2). Lancet Neurol 10:618–625
Macdonald RL, Higashida RT, Keller E, Mayer SA, Molyneux A, Raabe A, Vajkoczy P, Wanke I, Bach D, Frey A, Nowbakht P, Roux S, Kassell N (2012) Randomized trial of clazosentan in patients with aneurysmal subarachnoid hemorrhage undergoing endovascular coiling. Stroke 43:1463–1469
Kusaka G, Ishikawa M, Nanda A, Granger DN, Zhang JH (2004) Signaling pathways for early brain injury after subarachnoid hemorrhage. J Cereb Blood Flow Metab 24:916–925
Cahill J, Calvert JW, Zhang JH (2006) Mechanisms of early brain injury after subarachnoid hemorrhage. J Cereb Blood Flow Metab 26:1341–1353
Crompton MR (1964) The pathogenesis of cerebral infarction following the rupture of cerebral berry aneurysms. Brain 87:491–510
Megyesi JF, Vollrath B, Cook DA, Findlay JM (2000) In vivo animal models of cerebral vasospasm: a review. Neurosurgery 46:448–460, discussion 460–441
Sehba FA, Bederson JB (2006) Mechanisms of acute brain injury after subarachnoid hemorrhage. Neurol Res 28:381–398
Marbacher S, Fandino J, Kitchen ND (2010) Standard intracranial in vivo animal models of delayed cerebral vasospasm. Br J Neurosurg 24:415–434
Brawley BW, Strandness DE Jr, Kelly WA (1968) The biphasic response of cerebral vasospasm in experimental subarachnoid hemorrhage. J Neurosurg 28:1–8
Nagai H, Suzuki Y, Sugiura M, Noda S, Mabe H (1974) Experimental cerebral vasospasm. 1: Factors contributing to early spasm. J Neurosurg 41:285–292
Asano T, Sano K (1977) Pathogenetic role of no-reflow phenomenon in experimental subarachnoid hemorrhage in dogs. J Neurosurg 46:454–466
Barry KJ, Gogjian MA, Stein BM (1979) Small animal model for investigation of subarachnoid hemorrhage and cerebral vasospasm. Stroke 10:538–541
Kader A, Krauss WE, Onesti ST, Elliott JP, Solomon RA (1990) Chronic cerebral blood flow changes following experimental subarachnoid hemorrhage in rats. Stroke 21:577–581
Bederson JB, Germano IM, Guarino L (1995) Cortical blood flow and cerebral perfusion pressure in a new noncraniotomy model of subarachnoid hemorrhage in the rat. Stroke 26:1086–1091, discussion 1091–1082
Veelken JA, Laing RJ, Jakubowski J (1995) The Sheffield model of subarachnoid hemorrhage in rats. Stroke 26:1279–1283, discussion 1284
Bederson JB, Levy AL, Ding WH, Kahn R, DiPerna CA, Jenkins AL III, Vallabhajosyula P (1998) Acute vasoconstriction after subarachnoid hemorrhage. Neurosurgery 42:352–360, discussion 360–352
Sugawara T, Ayer R, Jadhav V, Chen W, Tsubokawa T, Zhang JH (2008) Simvastatin attenuation of cerebral vasospasm after subarachnoid hemorrhage in rats via increased phosphorylation of Akt and endothelial nitric oxide synthase. J Neurosci Res 86:3635–3643
Prunell GF, Mathiesen T, Svendgaard NA (2004) Experimental subarachnoid hemorrhage: cerebral blood flow and brain metabolism during the acute phase in three different models in the rat. Neurosurgery 54:426–436, discussion 436–427
Alkan T, Tureyen K, Ulutas M, Kahveci N, Goren B, Korfali E, Ozluk K (2001) Acute and delayed vasoconstriction after subarachnoid hemorrhage: local cerebral blood flow, histopathology, and morphology in the rat basilar artery. Arch Physiol Biochem 109:145–153
Park IS, Meno JR, Witt CE, Suttle TK, Chowdhary A, Nguyen TS, Ngai AC, Britz GW (2008) Subarachnoid hemorrhage model in the rat: modification of the endovascular filament model. J Neurosci Methods 172:195–200
Schwartz AY, Masago A, Sehba FA, Bederson JB (2000) Experimental models of subarachnoid hemorrhage in the rat: a refinement of the endovascular filament model. J Neurosci Methods 96:161–167
Kamii H, Kato I, Kinouchi H, Chan PH, Epstein CJ, Akabane A, Okamoto H, Yoshimoto T (1999) Amelioration of vasospasm after subarachnoid hemorrhage in transgenic mice overexpressing CuZn-superoxide dismutase. Stroke 30:867–871, discussion 872
Altay O, Hasegawa Y, Sherchan P, Suzuki H, Khatibi NH, Tang J, Zhang JH (2012) Isoflurane delays the development of early brain injury after subarachnoid hemorrhage through sphingosine-related pathway activation in mice. Crit Care Med 40:1908–1913
Altay O, Suzuki H, Hasegawa Y, Caner B, Krafft PR, Fujii M, Tang J, Zhang JH (2012) Isoflurane attenuates blood–brain barrier disruption in ipsilateral hemisphere after subarachnoid hemorrhage in mice. Stroke 43:2513–2516
Simeone FA, Ryan KG, Cotter JR (1968) Prolonged experimental cerebral vasospasm. J Neurosurg 29:357–366
Simeone FA, Trepper PJ, Brown DJ (1972) Cerebral blood flow evaluation of prolonged experimental vasospasm. J Neurosurg 37:302–311
Schwartz AY, Sehba FA, Bederson JB (2000) Decreased nitric oxide availability contributes to acute cerebral ischemia after subarachnoid hemorrhage. Neurosurgery 47:208–214, discussion 214–205
Lougheed WM, Tom M (1961) A method of introducing blood into the subarachnoid space in the region of the circle of Willis in dogs. Can J Surg 4:329–337
McQueen JD, Jeanes LD (1964) Dehydration and rehydration of the brain with hypertonic urea and mannitol. J Neurosurg 21:118–128
McQueen JD, Jelsma LF (1967) Intracranial hypertension. Cerebrospinal fluid pressure rises following intracisternal infusions of blood components in dogs. Arch Neurol 16:501–508
Martins AN, Doyle TF, Newby N, Kobrine AI, Ramirez A (1975) The effect of a simulated subarachnoid hemorrhage on cerebral blood flow in the monkey. Stroke 6:664–672
Prunell GF, Mathiesen T, Svendgaard NA (2002) A new experimental model in rats for study of the pathophysiology of subarachnoid hemorrhage. Neuroreport 13:2553–2556
Kassell NF, Torner JC, Haley EC Jr, Jane JA, Adams HP, Kongable GL (1990) The international cooperative study on the timing of aneurysm surgery. Part 1: Overall management results. J Neurosurg 73:18–36
Peters ND, Di Chiro G (1976) A model for spasm of the anterior cerebral artery. Stroke 7:243–247
Chow RW, Newton TH, Smith MC, Adams JE (1968) Cerebral vasospasm induced by subarachnoid blood and serotonin. An angiographic study. Invest Radiol 3:402–407
Echlin FA (1965) Spasm of basilar and vertebral arteries caused by experimental subarachnoid hemorrhage. J Neurosurg 23:1–11
Matz PG, Fujimura M, Lewen A, Morita-Fujimura Y, Chan PH (2001) Increased cytochrome c-mediated DNA fragmentation and cell death in manganese-superoxide dismutase-deficient mice after exposure to subarachnoid hemolysate. Stroke 32:506–515
Peerless SJ, Fox AJ, Komatsu K, Hunter IG (1982) Angiographic study of vasospasm following subarachnoid hemorrhage in monkeys. Stroke 13:473–479
Delgado-Zygmunt TJ, Arbab MA, Shiokawa Y, Svendgaard NA (1992) A primate model for acute and late cerebral vasospasm: angiographic findings. Acta Neurochir 118:130–136
Varsos VG, Liszczak TM, Han DH, Kistler JP, Vielma J, Black PM, Heros RC, Zervas NT (1983) Delayed cerebral vasospasm is not reversible by aminophylline, nifedipine, or papaverine in a “two-hemorrhage” canine model. J Neurosurg 58:11–17
Prunell GF, Mathiesen T, Diemer NH, Svendgaard NA (2003) Experimental subarachnoid hemorrhage: subarachnoid blood volume, mortality rate, neuronal death, cerebral blood flow, and perfusion pressure in three different rat models. Neurosurgery 52:165–175, discussion 175–166
Lee JY, Huang DL, Keep R, Sagher O (2008) Characterization of an improved double hemorrhage rat model for the study of delayed cerebral vasospasm. J Neurosci Methods 168:358–366
Krafft PR, Bailey EL, Lekic T, Rolland WB, Altay O, Tang J, Wardlaw JM, Zhang JH, Sudlow CL (2012) Etiology of stroke and choice of models. Int J Stroke 7:398–406
Clark JF, Sharp FR (2006) Bilirubin oxidation products (boxes) and their role in cerebral vasospasm after subarachnoid hemorrhage. J Cereb Blood Flow Metab 26:1223–1233
Pyne GJ, Cadoux-Hudson TA, Clark JF (2001) Cerebrospinal fluid from subarachnoid haemorrhage patients causes excessive oxidative metabolism compared to vascular smooth muscle force generation. Acta Neurochir 143:59–62, discussion 62–53
Zhao W, Ujiie H, Tamano Y, Akimoto K, Hori T, Takakura K (1999) Sudden death in a rat subarachnoid hemorrhage model. Neurol Med Chir (Tokyo) 39:735–741, discussion 741–733
Marbacher S, Andereggen L, Neuschmelting V, Widmer HR, von Gunten M, Takala J, Jakob SM, Fandino J (2012) A new rabbit model for the study of early brain injury after subarachnoid hemorrhage. J Neurosci Methods 208:138–145
Marbacher S, Sherif C, Neuschmelting V, Schlappi JA, Takala J, Jakob SM, Fandino J (2010) Extra-intracranial blood shunt mimicking aneurysm rupture: Intracranial-pressure-controlled rabbit subarachnoid hemorrhage model. J Neurosci Methods 191:227–233
Munoz-Sanchez MA, Egea-Guerrero JJ, Revuelto-Rey J, Moreno-Valladares M, Murillo-Cabezas F (2012) A new percutaneous model of subarachnoid haemorrhage in rats. J Neurosci Methods 211:88–93
Simard JM, Tosun C, Ivanova S, Kurland DB, Hong C, Radecki L, Gisriel C, Mehta R, Schreibman D, Gerzanich V (2012) Heparin reduces neuroinflammation and transsynaptic neuronal apoptosis in a model of subarachnoid hemorrhage. Transl Stroke Res 3:155–165
Dusick JR, Evans BC, Laiwalla A, Krahl S, Gonzalez NR (2011) A minimally-invasive rat model of subarachnoid hemorrhage and delayed ischemic injury. Surg Neurol Int 2:99
Lin CL, Calisaneller T, Ukita N, Dumont AS, Kassell NF, Lee KS (2003) A murine model of subarachnoid hemorrhage-induced cerebral vasospasm. J Neurosci Methods 123:89–97
Altay T, Smithason S, Volokh N, Rasmussen PA, Ransohoff RM, Provencio JJ (2009) A novel method for subarachnoid hemorrhage to induce vasospasm in mice. J Neurosci Methods 183:136–140
Solomon RA, Antunes JL, Chen RY, Bland L, Chien S (1985) Decrease in cerebral blood flow in rats after experimental subarachnoid hemorrhage: a new animal model. Stroke 16:58–64
Zhang JH, Badaut J, Tang J, Obenaus A, Hartman R, Pearce WJ (2012) The vascular neural network-a new paradigm in stroke pathophysiology. Nat Rev Neurol 8:711–716
Germanwala AV, Huang J, Tamargo RJ (2010) Hydrocephalus after aneurysmal subarachnoid hemorrhage. Neurosurg Clin N Am 21:263–270
Wang YM, Lin YJ, Chuang MJ, Lee TH, Tsai NW, Cheng BC, Lin WC, Su BY, Yang TM, Chang WN, Huang CC, Kung CT, Lee LH, Wang HC, Lu CH (2012) Predictors and outcomes of shunt-dependent hydrocephalus in patients with aneurysmal sub-arachnoid hemorrhage. BMC Surg 12:12
Kagerbauer SM, Rothoerl RD, Brawanski A (2007) Pituitary dysfunction after aneurysmal subarachnoid hemorrhage. Neurol Res 29:283–288
Suda N, Moriyama K, Ganburged G (2013) Effect of angiotensin II receptor blocker on experimental periodontitis in a mouse model of Marfan syndrome. Infect Immun 81(1):182–188
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer Science+Business Media New York
About this chapter
Cite this chapter
Chen, S., Klebe, D., Vakhmyanin, A., Fujii, M., Zhang, J.H. (2014). SAH Models: Review, New Modification, and Prospective. In: Lo, E., Lok, J., Ning, M., Whalen, M. (eds) Vascular Mechanisms in CNS Trauma. Springer Series in Translational Stroke Research, vol 5. Springer, New York, NY. https://doi.org/10.1007/978-1-4614-8690-9_14
Download citation
DOI: https://doi.org/10.1007/978-1-4614-8690-9_14
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4614-8689-3
Online ISBN: 978-1-4614-8690-9
eBook Packages: MedicineMedicine (R0)