Abstract
Hypopituitarism refers to a complex medical condition characterized by the deficiency of one or more of the hormones of the pituitary gland. Its prevalence is around 45 cases per 100,000 individuals. There are numerous causes of hypopituitarism, with sellar (e.g., pituitary adenoma) and perisellar tumors being the commonest etiologic factors, along with the sequelae generated by the different therapeutical modalities employed towards its resolution, such as surgery and radiotherapy. Clinical presentation may have a broad spectrum depending on cause and age of onset, and may vary from chronic/subacute nonspecific general ill feeling and mass effect related symptoms, as it commonly occurs with space-occupying sellar masses, to an acute and life-threatening presentation, such as that seen in pituitary apoplexy. Diagnostic approaches towards identifying the etiologic factors and each hormonal axis deficiency (i.e., GH, LH/FSH, TSH, ACTH, and ADH), as well as the description of the different available schemes of hormone replacement therapy, are thoroughly reviewed in this chapter.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Growth Hormone
- Growth Hormone Therapy
- Pituitary Apoplexy
- Growth Hormone Replacement
- Central Hypothyroidism
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Hypopituitarism is a complex medical condition with variable clinical manifestations associated with significant morbidity and mortality. The term describes the deficiency of one or more of the hormones of the anterior or posterior pituitary gland. The majority of patients with hypopituitarism have 3–5 hormones deficits.
Hypopituitarism affects approximately 4 out of every 100,000 individuals each year [1] with a prevalence of approximately 45 cases per 100,000 individuals. The causes, clinical features, diagnosis, management of hypopituitarism (including endocrine replacement therapy), interaction of hormone replacement, and long-term management are considered in this chapter.
Causes
There are numerous causes of hypopituitarism (Tables 8.1 and 8.2). The etiologic factors are determinants in the clinical presentation of this condition. For instance, pituitary apoplexy constitutes a medical emergency with the possibility of acute adrenal crisis and sudden loss of vision. On the other hand, functioning pituitary adenomas lead to a clinical picture that predominates the stigmata of the corresponding hormonal hypersecretion. Signs and symptoms related to local mass effect, including associated secondary hypothyroidism and hypocortisolism, may occur as a nonspecific presentation and remain unrecognizable for a long period of time.
Diagnosis
Clinical Presentation
The clinical presentation of hypopituitarism is often vague and nonspecific, leading to a further delay in diagnosis. Nonspecific symptoms include a feeling of general poor health, increased lethargy, feeling cool, chronic tiredness, reduced appetite, weight loss, and abdominal pain [2, 3]. Hypopituitarism can sometimes develops acutely, leading to a rapid onset of symptoms (excruciating headache, meningism, and cardiovascular collapse) necessitating admission and intensive care management, as is often seen in patients with tumor apoplexy.
The signs and symptoms of underlying diseases can sometimes follow hypopituitarism [3]. Symptoms attributed to the local effects of tumoral masses in the sellar region with suprasellar extension, such as headaches, rhinorrhea, and visual disturbances (typically bilateral hemianopsia, but can also occur as unilateral) frequently remain unrecognized by patients, mostly men, for a long period of time.
Deficits of anterior pituitary hormones may be secondary to hormone excess caused by functioning pituitary tumors, which produces a complex picture combining hormone excess and deficiencies, such as suppression of gonadotropins in hyperprolactinemia, growth hormone deficiency (GHD) caused by cortisol excess in Cushing’s syndrome [4] or growth hormone (GH) secreting macroadenoma that causes acromegaly and hypogonadism [5]. The presence of central Diabetes Insipidus (DI) usually indicates a non-pituitary lesion affecting the hypothalamus or pituitary stalk. Preoperatively, pituitary adenomas rarely cause DI.
Somatotropin Deficiency
Children
GHD in childhood promotes short stature and delayed bone age with slow growth velocity. Idiopathic GHD is the most common etiology. GH does not appear to have a relevant role in fetal growth. Therefore, in general, children are born with normal length, weight, and general appearance. However, microphallus and cryptorchidism may be present, especially with gonadotropin associated deficiency. Prolonged jaundice, hypoglycemia-associated seizures (when GHD occurs in conjunction with Adrenocorticotropic Hormone (ACTH) deficiency), and midline abnormalities suggest a congenital etiology.
Recognition of GHD is more common from the first 12–18 months after birth, with slow growth as an early sign and a consequent downward shift in the normal growth curve. Children tend to present with adiposity around the trunk. They have immature body and facial traits, a high-pitched voice, prominent forehead, depressed mid-face development, delayed dentition, and small hands and feet.
Adults
The severity of the clinical manifestations of GHD in adults depends on the timing of onset. In general, patients present nonspecific symptoms, such as fatigue, decreased energy, low mood, and altered body composition with increased fat and decreased lean body mass and muscle strength, as well as reduced bone mineral density, compromised metabolism of glucose and lipids, and poor quality of life [6]. Childhood-onset GHD patients have a lower lean body mass, bone mineral content, and better quality of life compared to adult-onset GHD patients.
Gonadotropin Deficiency
The clinical presentation of male hypogonadism depends on the time of onset of androgen deficiency. In men with recent onset hypogonadism, the physical examination is usually normal, while diminished facial and body hair, gynecomastia, and small soft testes are features of longstanding hypogonadism [2]. The principal signs and symptoms of androgen deficiency in men are loss of libido, decreased sexual potency, loss of body hair (axillary and pubic), infertility, and low bone mineral density. The threshold testosterone level below which symptoms of androgen deficiency and adverse health outcomes occur and testosterone administration improves outcomes in the general population is currently not known [7].
Female adolescents have primary amenorrhea and lack of breast development, whereas in adult women, gonadotropin deficiency leads to reduced secretion of estradiol, resulting in infertility and oligo/amenorrhea. Low estrogen is also responsible for genital atrophy and decreased breast volume in chronic hypogonadism. There is a reduction of pubic and axillary hair, especially when concomitant dysfunction of the corticotroph axis is present.
At the prepubertal age, no obvious clinical signs or symptoms are present until the normal age of puberty onset (9–14 years in boys and 8–13 years in girls), when a lack of signs of normal pubertal development are then observed. It should be emphasized that micropenis with or without associated cryptorchidism is an important clinical clue that suggests congenital hypogonadotropic hypogonadism (where there is lack of the normal fetal secretion and postnatal surge of gonadotropins) rather than acquired hypogonadotropic hypogonadism [8].
Thyrotropin Deficiency
The clinical picture of central hypothyroidism is very similar to primary hypothyroidism, but is often milder. Symptoms include cold intolerance, dry skin, decreased appetite with mild weight gain, and fatigue [9]. The presence of goiter usually indicates primary thyroid disease. In children, decreased growth velocity with impairment of neurological development is an important sign.
Corticotropin Deficiency
ACTH deficiency leads to decreased glucocorticoid levels. Mineralocorticoid secretion is preserved, since it is primarily modulated by the renin–angiotensin system. Hyperpigmentation is typical of primary adrenal disease and is absent in central disease. Symptoms of ACTH deficiency are largely nonspecific, including weakness, fatigue, anorexia, weight loss, arthralgia, postural hypotension, and tachycardia [10]. Hyponatremia, hypoglycemia, and eosinophilia may also occur. Ultimately, if left untreated, ACTH deficiency may lead to death due to vascular collapse, since cortisol is needed to maintain vascular tone. Mild ACTH deficiency may remain clinically unnoticed when cortisol production is sufficient for preventing symptoms in the absence of clinical stressors (e.g., infections). Hence, laboratorial evaluation is recommended in all patients at risk of ACTH deficiency.
Antidiuretic Hormone (ADH) Deficiency
ADH deficiency results in polyuria (urine volume >3 L/day in adults) and polydipsia. If the thirst mechanism is not present, as is the case in some patients with hypothalamic lesions, then lack of polydipsia leads to a high risk of life-threatening dehydration and hypernatremia [11].
Diagnostic Testing
The diagnosis of hypopituitarism can often be made through simultaneous measurements of basal anterior pituitary and target gland hormone levels. Each axis should be assessed in patients suspected of having partial or complete loss of pituitary function, because the impairment in these patients is often partial rather than complete.
Low or inappropriately normal serum levels of pituitary hormones in conjunction with low peripheral hormones indicate hypopituitarism. FSH, LH, estradiol (women), testosterone (men), prolactin, TSH, free thyroxine (FT4), 9 am cortisol, and insulin-like growth factor-I (IGF-I) tests form the baseline parameters to assess. In addition, dynamic studies are necessary in most cases for documenting hypopituitarism, particularly for assessing GH secretory reserve and the ACTH-adrenal axis (Table 8.3) [5].
Somatotropin Deficiency
Children
GHD in children is based on auxological data, which is considered the gold standard in such diagnosis [12]. An appropriate differential diagnosis must be performed ruling out other causes of growth failure, such as hypothyroidism, Turner syndrome, and systemic diseases.
Evaluation should be considered when patients present with one of the following conditions: (1) short stature of more than 2.5 standard deviations (SD) below the mean; (2) growth failure, which is defined as height velocity less than 2 SD below the mean for age; (3) a combination of less severe short stature (2–2.5 SD below the mean for age) and growth failure (growth velocity less than 1 SD); (4) clinical picture suggesting hypothalamic-pituitary dysfunction, such as hypoglycemia, microphallus, intracranial tumor, or history of cranial irradiation with decelerating growth; and (5) evidence of deficiency in other hypothalamic–pituitary hormones [13].
The pulsatile nature and short half-life of GH preclude the random measurement of serum GH levels as a useful tool for diagnosing GHD. Thus, IGF-I and IGF-binding Protein 3 (IGFBP-3) are appropriate initial tests for GHD in children providing that conditions such as poor nutrition, hypothyroidism, and chronic systemic diseases are excluded. These hormones reflect an integrated assessment of GH secretion because of negligible diurnal variation [14].
IGF-I and IGFBP-3 measurements should be interpreted in relation to reference ranges that are standardized for sex and age. An important drawback to using serum IGF-I for GHD diagnosis is that its values are low in very young children and overlap in GHD patients and normal children. In this context, IGFBP-3 levels, which are less related to age, are more discriminatory than IGF-I levels at the lower end of the normal range [15].
These tests present less than adequate sensitivity, although specificity is high. Thus, in patients with severe GHD, IGF-I and IGFBP-3 levels are invariably reduced; On the other hand, patients with milder abnormalities of GH secretion demonstrate normal levels of IGF-I and its binding protein in a significant percentage of cases [16].
Despite these limitations, measurement of IGF-I and IGFBP-3 levels associated with provocative testing in an appropriate clinical context is now commonly performed when investigating GHD in childhood.
GH Stimulation Testing in Children
Provocative GH testing has several caveats. They are not physiological, since the secretagogues used do not reflect normal GH secretion; the cutoff level of normal is arbitrary and the tests are age dependent. Furthermore, the tests rely upon GH assays of variable accuracy and are all uncomfortable, cumbersome, and risky for the patient [12, 17]. Therefore, there is currently no gold standard provocative GH test for GHD in children. As a result, subnormal responses to two secretagogues are necessary for diagnosis, with the exception of patients presenting with a central nervous system disorder, multiple pituitary hormone defects, or a known genetic defect. In these cases, one test is sufficient to establish the diagnosis [18].
These stimulation tests are performed after an overnight fasting. After the pharmacologic stimulus, serum samples are collected at intervals designed to capture the peak GH level. A “normal” response is defined by a serum GH concentration of greater than 7–10 mcg/L, although the ideal threshold may vary with the assay used. Of note, all patients should be euthyroid and should not be under supraphysiological doses of glucocorticoids before any testing is performed (Tables 8.3 and 8.4).
Clonidine, an α-2 adrenergic receptor agonist, promotes GH release, mainly through GHRH secretion. It is a stronger stimulant for growth hormone release, and therefore false negative results can follow. On the other hand, children presenting with a GH subnormal response to such stimulus rarely secrete normal GH in response to any other stimuli [19]. The test commonly causes hypotension and drowsiness that may last for hours and promote late hypoglycemia.
Insulin-induced hypoglycemia is a potent stimulant of GH release and, therefore, the Insulin Tolerance Test (ITT) is among the most specific tests for GHD. However, safety concerns have prevented the widespread use of this test. The proposed mechanism by which hypoglycemia promotes GH secretion is through the suppression of somatostatin tone and stimulation of α-adrenergic receptors [20]. This test requires constant supervision by a clinician and is contraindicated in children less than 2 years of age.
Administration of glucagon promotes GH secretion through a poorly understood mechanism, with the activation of central noradrenergic pathways as a plausible hypothesis [21]. Glucagon presents mild and transient side effects, such as nausea, vomiting, and sweating, and therefore is a very good choice for infants and young children who are more susceptible to the risks of insulin-induced hypoglycemia.
Adults
In adults, the clinical picture of GHD is subtle and nonspecific, and therefore the diagnosis relies on biochemical testing. Patients with structural hypothalamic and/or pituitary disease, surgery, or irradiation in these areas as well as TBI, SAH, or evidence of other pituitary hormone deficiencies should be evaluated for acquired GHD. Otherwise, the presence of three or more pituitary hormone deficiencies associated with a low IGF-I is highly predictive of GHD, in which case provocative testing is not necessary [22]. In addition, patients should receive adequate replacement of other deficient hormones before GH stimulation testing is performed.
GH Stimulation Testing in Adults
ITT is considered the most validated test currently available and is the diagnostic test of choice for GHD in adults. However, it is contraindicated in patients with seizure disorders or ischemic heart disease and requires monitoring, even in healthy adults. Adequate hypoglycemia (<2.2 mmol/L) is not always achieved, and therefore, larger doses of insulin up to 0.3 U/kg may be necessary in obese patients and those with fasting blood glucose above 5.5 mmol/L [23]. An assay cutoff of 5.1 μg/L is recommended for diagnosis [22].
A GHRH and arginine test (GHRH-Arg test) is a very potent and reproducible test. Arginine potentiates the response to GHRH presumably through the inhibition of hypothalamic somatostatin secretion [24]. This combined test is not affected by gender or age and shows few side effects with no hypoglycemia. On the other hand, the assay cutoff for GHD diagnosis depends on the body mass index (BMI) [25]. In addition, GHRH directly stimulates the pituitary, and patients with GHD of hypothalamic origin, mainly after radiotherapy, could present a falsely normal GH response [26].
Administration of glucagon allows for the assessment of GH and ACTH-cortisol reserves, and has few side effects with minimal contraindications. It is a good choice when other tests are unavailable or contraindicated. In adults, an assay cutoff between 2.5 and 3.0 μg/L is recommended for GHD diagnosis [22].
Transitional Period
In the transition period (i.e., after the cessation of linear growth and completion of puberty), the majority of GHD patients must be retested. Those patients with conditions causing multiple pituitary hormone deficiencies (MPHD) (i.e., three or more pituitary hormone deficits), can continue on GH therapy, but require determination of an adequate dose. Other patients without MPHD but who present with known mutations or irreversible structural hypothalamic-pituitary lesions/damage should be screened for serum IGF-I levels after terminating therapy for at least 1 month. IGF-I levels below −2 SD are sufficient for GH therapy reinstitution. If the IGF-I level is within the normal range, then one provocative testing is mandatory for GH therapy in case of a subnormal response.
In the remaining patients, mostly with idiopathic causes, a serum IGF-I test and one provocative test must be performed, and in case of discordant results, a second provocative test is necessary for the diagnosis of persistent GHD [22, 27].
It is unclear whether different assay cutoffs should be adopted during this transitional period, as opposed to GHD assay cutoffs in adults. Some studies suggest that the assay cutoffs in these cases should be higher than for older adults, with levels of 6.1 μg/L and 19.0 μg/L for the ITT and GHRH-arg, respectively [28, 29].
Gonadotropin Deficiency
In men, low or inappropriately normal levels of gonadotropins combined with low levels of serum testosterone are indicative of secondary hypogonadism. Semen analysis is indicated when considering fertility and may demonstrate a reduced sperm count or possibly azoospermia.
In younger women, oligo/amenorrhoea with low serum estradiol levels and low or inappropriately normal FSH and LH concentrations is consistent with secondary hypogonadism. In postmenopausal women, the absence of the normal rise of FSH and LH levels is sufficient for establishing a diagnosis.
In secondary hypogonadism, serum prolactin should always be measured to exclude hyperprolactinemia, which might occur for several reasons, such as prolactinomas, sellar and parasellar masses causing pituitary stalk compression, and use of drugs with antidopaminergic activity.
In adults, there is no usefulness in performing the gonadotropin-releasing hormone (GnRH) provocative test because it does not provide any additional information [5].
Thyrotropin Deficiency
Evaluation of the thyrotrophic axis is based on the measurement of basal serum TSH and thyroid hormone levels. Central hypothyroidism is diagnosed when serum TSH levels are low or inappropriately normal coupled with low levels of serum free T4. Occasionally, TSH levels may be slightly elevated but usually remain lower than 10 mIU/mL. In these patients, the elevation of serum TSH is associated with decreased bioactivity due to increased sialylation [30]. In patients with concomitant GH and TSH deficiencies, serum-free T4 may be normal (usually at the lower tertile), decreasing only after GH replacement [31, 32]. More recently, it has been proposed that echocardiography can be useful in the evaluation of patients with hypothalamic-pituitary disease and free T4 levels within reference range, as some of these patients present signs of tissue hypothyroidism, a condition that could be named “subclinical central hypothyroidism” [33].
The TRH stimulation test has been performed in the past to diagnose central hypothyroidism [34]. However, this test is not currently recommended due to a lack of accuracy [35].
Corticotropin Deficiency
Cortisol secretion follows a circadian cycle, being highest in the early morning and lowest at midnight. Hence, a basal serum cortisol measurement may not reflect disturbances of the hypothalamus-pituitary-adrenal (HPA) axis. In addition, alterations in the levels of cortisol-binding globulin (CBG), which is frequently seen in clinical practice (e.g., higher levels of CBG, and consequently serum total cortisol, during oral estrogen treatment as a contraceptive) may also mask the diagnosis of central hypoadrenalism. Therefore, early morning serum cortisol (between 07:00 and 09:00) may be measured as a first step in the evaluation [10]. Stimulation tests are frequently required for corticotropic assessment. The most commonly used stimuli in clinical practice are insulin-induced hypoglycemia, Metyrapone, synthetic ACTH (ACTH1-24), and CRH (Tables 8.3 and 8.4).
Hypoglycemia is a potent activator of the HPA axis, and the ITT is usually regarded as the “gold standard” for diagnosis (see more details in “GH stimulation testing”).
ACTH1-24 administration is currently the most commonly used test in clinical practice for assessing HPA axis. Adrenal atrophy is required for the test to be positive in cases of ACTH deficiency. Hence, this test should not be performed within 2 weeks of an insult to the hypothalamus or pituitary (e.g., pituitary surgery) [36]. A low-dose (1 μg) ACTH1-24 test has been reported to induce improved sensitivity by some studies [37] but not others [38].
Metyrapone decreases serum cortisol by inhibiting the enzyme 11-beta-hydroxylase and this test is usually not performed due to limited availability of the drug.
CRH has been used to differentiate hypothalamic from pituitary disease in secondary adrenal insufficiency. However, CRH stimulation is not particularly useful in diagnosing secondary adrenal insufficiency because individual responses to exogenous CRH are extremely variable.
ADH Deficiency
DI may be diagnosed with a proper clinical presentation, for example, in a patient with known pituitary/hypothalamic disease if other causes of polyuria (e.g., diabetes mellitus, use of diuretics) are excluded. Serum sodium is usually above the middle of the reference range, but hypernatremia is not seen in patients with an intact thirst mechanism. In situations where diagnosis is not clear-cut, a water deprivation test is warranted. Maximum urine osmolality is less than 300 mOsm/Kg H2O in patients with complete DI. In patients with subnormally elevated osmolality after water deprivation (300 mOsm/Kg < osmolarity < 800 mOsm/Kg H2O), further steps are needed, including magnetic resonance imaging (MRI) of the hypothalamic-pituitary region and/or a therapeutic trial with Desmopressin [11].
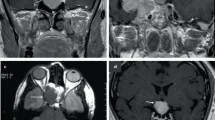
Imaging
MRI is currently the single best imaging procedure in the investigation for most sellar masses. After hypopituitarism has been confirmed, MRI should be performed to exclude tumors and other lesions of the sellar and parasellar region. When this is not possible, computerized tomography (CT) provides a suitable alternative. Micro- and macroadenomas of the pituitary as well as other sellar masses, such as craniopharyngiomas and meningiomas, usually take up contrast to a lesser degree than the normal pituitary. Craniopharyngiomas and even pituitary adenomas may have a partially cystic content and, therefore, have low-intensity signals. Hemorrhage has a high-intensity signal on both T1- and T2-weighted images. On the other hand, asymptomatic pituitary adenomas are found upon autopsy in approximately 11 % of individuals. Such adenomas may also be commonly seen as incidental findings (incidentalomas) on head CT or MRI scans performed for other reasons [39].
Recent MRI studies of the pituitary in patients who had suffered a TBI demonstrated pathological changes consistent with vascular injury. In the acute phase, the pituitary glands of these patients are significantly enlarged and may also present other abnormalities, such as hemorrhage, infarction, and partial stalk transection [40]. In the chronic phase, patients often demonstrate pituitary volume loss or empty sella, perfusion deficits, or lack of a posterior pituitary signal. Such abnormalities were reported to occur in 80 % of patients with hypopituitarism compared to 29 % of those without hypopituitarism [41].
Neuro-Ophthalmic Exam
Patients with a known pituitary tumor must be carefully followed for evidence of growth with early chiasmal-optic nerve compression. The frequency of visual evaluation must be individualized based on the size of the tumor and its relation to critical structures. Goldmann perimetry is useful in plotting the visual field defects and also assists in follow-up.
Management
Understanding the underlying pathophysiology in each patient and recognizing the probability for recovery of function are among the most important issues to be emphasized in the management of patients with hypopituitarism. Treatment is based on the underlying disease that leads to pituitary insufficiency.
Pituitary tumors may be treated with medical therapy, surgery, radiotherapy, or a combination of these modalities depending on the tumor subtype and clinical presentation [5]. Whereas prolactinomas are almost exclusively treated with dopamine agonists, neurosurgical removal is indicated for most other pituitary sellar and parasellar masses. Infections (e.g., meningoencephalitis, tuberculosis, or syphilis) are treated with antibiotics or antivirals and granulomatous infiltrations (e.g., sarcoidosis) are treated with immunosuppressants.
The goal of hormone replacement therapy is to achieve normal levels of the circulating hormones in order to restore normal physiology as close as possible and to avoid the symptoms of deficiency with minimal side effects. Target peripheral hormones, rather than deficient pituitary hormones, should be replaced, except for GH deficiency, ADH deficiency, and gonadotropins, when fertility is desired [5]. Hormone replacement therapy should be started as soon as the diagnosis of hypopituitarism is made (Box 8.1). It is very important to carefully evaluate whether hypopituitarism is likely to be reversible or whether it is permanent, thereby requiring life-long hormone replacement therapy.
Hormone Replacement Therapy
Hyposomatotropism
Children
Childhood GHD should be treated as soon as possible in order to improve linear growth. The individual response to GH therapy is widely variable and unpredictable. Dosing is mainly based on weight and can range from 0.021 to 0.050 mg/kg/day (0.033 mg/kg/day is the most suitable initial dose) up to 0.1 mg/kg/day in adolescents. It should be given once a day by subcutaneous injection, and should be adjusted based on growth response and IGF-I levels [42, 43].
Therapy should be started as early as possible in order to achieve the best results in growth where patients can achieve height within the midparental target height [44].
GH therapy in children is safe and adverse events are uncommon. Idiopathic intracranial hypertension (pseudotumor cerebri) is a rare occurrence that tends to occur early in therapy, and if it occurs then drug discontinuation and subsequent cautious reintroduction is necessary. Some patients may present increased insulin resistance, which appears not to translate into marked glucose abnormalities [45].
The goals of therapy are to achieve therapeutic levels of IGF-I that are slightly above the mid-normal range (approximately 1 SD above the mean) adjusted for age, pubertal stage, and growth velocity above the 75th percentile curve [46, 47]. An evaluation is performed 4 weeks after beginning treatment, and in case of an adequate IGF-I response, the length/height should be rechecked every 3–6 months and IGF-I levels should be rechecked every 6–12 months.
Caution is necessary with unmasking hypothyroidism after GH therapy as previously discussed. Thus, free T4 should be assessed every 3 and 6 months after initiation of this therapy and yearly thereafter.
Adults
In adults, GH dosing regimens are not weight-based as in children, but rather are initialized with a lower dose and then titrated according to clinical parameters and IGF-I levels. The recommended GH starting dose is 0.2–0.3 mg/day for most patients and 0.1–0.2 mg/day for the elderly patients that are more susceptible to adverse events linked to therapy [22]. A target for IGF-I levels is the upper half of normal range.
The most common side effects, which occur in 5–18 % of patients, are joint stiffness, peripheral edema, arthralgias, and myalgias. Carpal tunnel syndrome and increased blood pressure are infrequent, but when present, are related to supraphysiological doses in most cases. When this occurs, a reduction in the dose is appropriate [48].
Although there are no conclusive data of a GH role in the development or recurrence of malignant diseases, GH is contraindicated in adult patients with an active malignancy. A slight increase in the risk for DM has been observed with GH therapy, and therefore diabetic patients may require changes in the doses of current medications [22].
Adjustments should be performed every 1–2 months during dose titration. A clinical response, IGF-I levels, and side effects should guide the choice of dose. After titration, evaluation should be performed at 6 months intervals.
Transitional Period
In the transition phase, the recommended dose is 0.4–0.5 mg/day with the goal of achieving IGF-1 levels between 0 and +2 SD with adjustments made at 1–2 month intervals. Reassessment should be made every 6 months thereafter until the patient is in their mid-twenties [22, 27].
Hypogonadism (in the Adult Female)
Estrogen deficiency requires replacement for the relief of symptoms, such as loss of libido and dyspareunia as well as for the prevention of osteoporosis and premature cardiovascular disease. Epidemiological studies in women with anterior pituitary deficiency have demonstrated excessive cardiovascular mortality in untreated versus treated hypogonadism [49]. Thus, it is strongly recommended to replace sex steroids in younger women until the average age of menopause is reached (approximately 52 years of age in healthy subjects). On the other hand, findings of large studies of sex hormone replacement therapy in non-pituitary postmenopausal patients have shown an increased risk of cardiovascular and neoplastic diseases. Therefore, termination of sex hormone substitution in hypogonadal women after the average menopause age is recommended [50, 51].
The biological potency of 20 μg ethinyl estradiol, 1.25 mg conjugated estrogen, and 100 μg transdermal 17β-estradiol is comparable [52]. In premenopausal women, an oral contraceptive containing 20–35 μg ethinyl estradiol is an effective form of replacement therapy. Alternatively, oral estrogen preparations (conjugated estrogen 0.625–1.25 mg daily or estradiol valerate 1–2 mg) given cyclically or continuously with a progestagen can be administered. Transdermal application of estradiol (50–100 μg/day) is preferred over oral preparations because it avoids hepatic first-pass metabolism. In addition, the transdermal preparation minimizes the synthesis of procoagulatory factors and acute phase proteins, which are potential vascular risk factors [53], and eliminates the growth-hormone resistant effects of estrogen on IGF-I production in the liver [54]. All women who have an intact uterus should receive concomitant progesterone therapy. Breast cancer is clearly an absolute contraindication for sex steroid replacement therapy.
Pubertal Development
The goal for therapy in this case is to approximate normal development, and the appropriate age for intervention is around the chronological age of 11 years. Conjugated estrogens (initial dose 0.15 mg daily or 0.3 mg on alternate days), ethinyl estradiol (2.5–5 μg daily), or 17β-estradiol (initial dose 5 μg/kg daily) may be administered, and the dose should be gradually increased every 6–12 months over the following 2–3 years until the adult replacement dose is reached. After 6 months of therapy or in case of spotting or menstrual bleeding, cyclic progestagens (usually medroxyprogesterone 5–10 mg daily or norethisterone 0.7–1.0 mg daily) should be added for 12–14 days every month [55].
Estrogen-release patches offer an alternative treatment option. The smallest commercially available patch releases 25 μg 17β-estradiol daily. The patch can be divided into six to eight fragments, and each fragment allows a release of 0.08–0.12 μg/kg daily. Application of the patch may be limited to nighttime in order to mimic the pattern of estrogen secretion that is predominantly nocturnal during the initiation of puberty [56]. The dosage should be increased every 6–12 months until the adult replacement dosage is achieved.
Fertility Treatment
Pulsatile GnRH is mostly used for ovulation induction in patients with hypothalamic hypogonadotropic hypogonadism and normal gonadotropin levels. However, such therapy should only be performed at centers with extensive experience in ovarian stimulation techniques.
Gonadotropin therapy is indicated in patients with gonadotropin deficiency or GnRH resistance, but can also be used in patients with GnRH defects [57]. Ovulation induction is initiated with 75 IU daily of a preparation containing only FSH or a mixture of FSH and LH (human menopausal gonadotropins). Careful ultrasound monitoring is recommended to ensure that only one or two follicles develop in order to prevent ovarian superstimulation and prevent multiple pregnancies. Once a follicle has become mature, a single dose of 5,000 IU of human chorionic gonadotropin (hCG) is administered to stimulate ovulation, which occurs within 36–48 h of administration. Conception occurs in 5–15 % of cycles and cumulative conception rates average between 30 and 60 % [57].
Hypogonadism (in the Adult Male)
The aim of androgen substitution is to restore the serum testosterone concentration to the normal range (in the mid-normal range) in order to maintain secondary sexual characteristics, prevent loss and optimize bone mass, and improve sexual function [7].
The route of delivery depends on availability, patient preference, consideration of pharmacokinetics, treatment burden, and cost. Testosterone therapy is contraindicated in patients with prostate cancer, untreated severe obstructive sleep apnea, and uncontrolled or poorly controlled heart failure [7].
Oral Testosterone
Oral testosterone undecanoate is commercially available in many countries under various brand names in 40 mg capsules, but is not available in the United States. It is absorbed through the lymphatic system and bypasses the portal vein due to esterification at the 17β position. The daily dose is 80–240 mg given throughout the day with meals. However, this drug has low bioavailability and substantial interindividual and intraindividual variability in absorption [58]. Therefore, it is more suitable for patients who cannot tolerate transdermal or intramuscular administration.
Intramuscular Depot
Testosterone enanthate and testosterone cypionate are 17β esters of testosterone that have been the standard preparations for testosterone treatment for decades and have been proven to be safe with few unwanted side effects. Both esters are more lipophilic than native testosterone and have a long half-life and duration of action.
After intramuscular administration of testosterone enanthate, serum testosterone peaks to maximal supraphysiological levels in approximately 10 h, followed by a gradual decline to low normal or even subnormal levels [59]. Intramuscular doses of testosterone enanthate or cypionate from 100 mg/week or 150–200 mg every 2 weeks are biologically effective. Serum testosterone should be monitored between midway injections aiming at a serum level between 350 ng/dL (12–3 nmol/L) and 750 ng/dL (24–5 nmol/L). Some clinicians prefer to monitor serum testosterone levels immediately prior to the next injection with a goal of achieving a level in the low normal range. Dose adjustment is performed by varying injection intervals or injection dosage.
Testosterone undecanoate (Nebido®) is another ester of testosterone that has a markedly longer half-life (34 days) and duration of effect than testosterone enanthate and cypionate. Intramuscular injection of testosterone undecanoate 1,000 mg every 3 months leads to constant physiological serum testosterone levels without the undesired initial peak in drug concentration observed with the other depot formulations. A reduction in the injection interval between the first and second administration is recommended [60] and with this loading dose, sufficient steady state testosterone levels may be achieved more rapidly. Serum testosterone should be monitored at the end of the injection interval with the goal of achieving a serum level of testosterone in the mid-normal range. Dose adjustment is performed by varying the injection intervals.
Transdermal Systems
Transdermal systems are a popular treatment modality for hypogonadal men. Transdermal gel and patches provide a useful delivery system for normalizing serum testosterone in these patients [61]. The transdermal gel has the best pharmacokinetic properties of all the available formulations and can achieve stable serum testosterone concentrations within the normal range using a noninvasive topical application that is applied once a day on non-pressure areas of the body. Potential limitations of transdermal systems include a high rate of skin irritation observed with patches and the possibility that the testosterone gel may be transferred to other individuals through skin contact [62]. Four testosterone gels are currently available in United States, including AndroGel®, Testim®, Axiron®, and Fortesta®. A multicenter study conducted by Swerdloff et al. [63] (Testosterone Gel Study Group) showed that a daily transdermal application of a hydroalcoholic gel containing 1 % testosterone (AndroGel®) at 5.0 and 10.0 g of gel (equivalent to 50 and 100 mg) increased serum testosterone levels in hypogonadal men to within the normal range. Treatment should be started with 5.0 g and adjusted as necessary up to a maximum of 10.0 g. Testim® is another brand of hydroalcoholic gel with the same concentration.
The 2 % formulation of testosterone topical solution (Axiron®) is a non-occlusive topical formulation administered to the axilla, instead of the hands. A multicenter study conducted by Wang et al. [64] in hypogonadal men treated with 30–90 mg of this preparation showed that application of the gel restored physiological testosterone levels in 84.8 % of treated patients. This finding is similar to results previously reported with testosterone gel and mucoadhesive buccal therapies. The suggested dose of Axiron® is 60 mg (30 mg applied to each axilla once a day), with adjustment of the dose ranging from 30 to 120 mg, as determined by the serum testosterone concentration.
A novel 2 % testosterone gel for the treatment of hypogonadal male (Fortesta®) is also supplied in a metered dose pump, which is applied to the front and inner thighs. A multicenter study [65] in hypogonadal men followed for 90 days demonstrated that a single daily dose of this preparation restored normal levels of testosterone in more than 75 % of hypogonadal patients, with a low risk of supraphysiological testosterone levels. The recommended starting dose is 40 mg once a day (2 g/2 mL of gel) with adjustment of the dose ranging from 10 to 70 mg, as determined by the serum testosterone concentration.
The transdermal system patch (Androderm®) delivers approximately 5 mg of testosterone every 24 h and results in normal serum testosterone concentrations in most hypogonadal men [66]. The application of one or two testosterone patches is recommended to be applied nightly over the skin of the back, thigh, or upper arm, away from pressure areas. Testosterone serum levels can be assessed 3–12 h after the application of the patch. The dose should be adjusted to achieve testosterone levels in the mid-normal range. The scrotal patch is no longer available in the United States.
Testosterone in an adhesive matrix patch is now available in many countries. The recommended regimen consists of 2 × 60 cm2 patches that delivers approximately 4.8 mg of testosterone per day and lasts for approximately 2 days. However, some patients experience skin irritation with this preparation [7].
Buccal Tablet
A controlled release testosterone buccal system (Striant SR®) contains 30 mg of testosterone and mucoadhesive excipients, which rapidly adhere to the buccal mucosa and slowly form a gel. Transbuccal delivery of testosterone substantially circumvents hepatic first-pass metabolism. A study by Wang et al. [67] demonstrated that the administration of this preparation maintained serum testosterone concentrations within the normal range in most hypogonadal men. The recommended dose is 30 mg applied to the buccal region twice a day. Testosterone serum levels can be assessed immediately before or after application of the fresh system. Gum-related adverse events occurred in 16 % of treated subjects.
Pellets
Subcutaneous pellets (Testospel®) provide stable physiological testosterone levels, but a minor surgical procedure is required for administration [68]. The pellets are implanted into the subdermal fat of the lower abdominal wall, buttock, or thigh. The dose and regimen vary with formulation. The manufacturer recommends implantation of three to six 75 mg pellets every 3–6 months [7]. Extrusion of the pellets and infection are the main risks of this treatment.
Monitoring During Androgen Therapy
Men younger than 40 years of age may not need prostate monitoring as they are at low risk for the development of prostate cancer. In men 40 years of age or older with a baseline prostatic specific antigen (PSA) level greater than 0.6 ng/mL, rectal digital examination should be performed before initiating treatment, and PSA levels should be checked 3–6 months after the start of treatment and annually thereafter. A urological consultation is necessary if there is an increase in serum PSA concentration to a level greater than 1.4 ng/mL within any 12 month period of testosterone treatment. Hematocrit should be checked at baseline, at 3–6 months after the start of therapy, and annually thereafter. If the hematocrit is greater than 54 %, then the treatment should be stopped until it decreases to a safe level [7].
Infants/Pubertal Development
Infants and children with micropenis (penile length less than 2.5 cm at birth and in infancy) related to congenital hypopituitarism may be treated with three courses of testosterone enanthate 25 mg given IM each month with the goal of increasing penis size. If the desirable increase in penile length (>0.9 cm) has not occurred, then another three course trial can be repeated [8].
There is no general consensus regarding the best time to induce pubertal development. An acceptable proposal may be to induce pubertal development at 13 years and obtain a slow and progressive increase. A monthly dose of testosterone enanthate or cypionate 25–50 mg IM may be used. The dose should be kept as low as possible in order to preserve maximal growth potential. The dose should be increased every 6–12 months until reaching the adult replacement therapy within 3–5 years [57].
Fertility Treatment
In secondary hypogonadism, spermatogenesis and fertility can be induced. Men with prepubertal onset hypogonadism are more likely to require replacement of FSH as well as LH, whereas men with postpubertal onset are more likely to require replacement of LH only.
The classical gonadotropin regimen combines hCG and human menopausal gonadotropin (hMG) given as IM or subcutaneous (SC) injections, depending on the available preparation [69]. After stopping testosterone treatment, hCG can be used initially at a dose of 2,000 IU twice a week to stimulate spermatogenesis. The dose is titrated against testicular volume and serum testosterone, which should be measured every 1–2 months, with the goal of achieving levels between 400 and 900 ng/dL within 3–4 months after initiating treatment. Some patients require as little as 500 IU per dose, while other patients need as much as 10,000 IU per dose. Sperm count is measured every 2–4 weeks, but the value is not used to adjust the hCG dose. Most patients who eventually reach a normal sperm count (over 20 million/mL) do so within 6 months, but some require 12–24 months. The addition of hMG should be considered if the sperm count does not reach one-half of the normal level within 12–24 months. The pharmaceutical preparation of hMG contains FSH and is used to replace FSH for stimulating spermatogenesis in men who are infertile due to secondary hypogonadism. Recombinant human FSH is also available, but has not been as well studied in men and is more expensive. FSH appears to be necessary for the initiation of spermatogenesis, but not for its maintenance or reinitiation. Therefore, for patients with prepubertal onset of secondary hypogonadism, the treatment should be started with both hCG 2,000 IU and hMG three times a week while titrating hCG doses based on serum testosterone levels.
Thyrotropin Deficiency
Levothyroxine is the replacement of choice for central hypothyroidism [70]. Most patients use 75–125 mcg/day of L-T4 (for pediatric dosages, see Box 8.1). Laboratory monitoring of serum-free T4 levels should be performed. The FT4 levels should remain in the upper half of the reference range for patients with concomitant untreated GH deficiency in order to ensure adequate replacement [31]. In eusomatotropic patients, the FT4 levels should be in the mid-normal reference range [31, 71] (see “Hormone Replacement Therapy Interactions” below).
ACTH Deficiency
Glucocorticoid replacement is a priority because its deficiency is potentially life-threatening. Replacement therapy should be initiated before the beginning of thyroxine and/or GH replacement, since these latter treatments may precipitate adrenal crisis. There is no consensus on the best glucocorticoid replacement regimen [10]. Many centers use hydrocortisone (15–20 mg/day) in divided doses in an attempt to mimic circadian variation (e.g., 10–15 mg in the morning and 5 mg in the early afternoon; see Box 8.1). Equivalent doses of prednisone, dexamethasone, or cortisone acetate have also been used. Approximate equivalent doses to 20 mg of hydrocortisone include cortisone acetate, 25 mg, prednisone, 5 mg, and dexamethasone, 0.75 mg. Mineralocorticoid is not required in ACTH deficient patients, since its secretion is under the control of the renin–angiotensin system. For children, hydrocortisone is usually the glucocorticoid of choice (10–24 mg/m2/day in divided doses). Prednisolone (3–5 mg/m2/day) is also used, albeit less frequently. Due to its higher potency and possible negative effects on growth, dexamethasone is avoided during childhood.
As a general rule, during acute illness, the usual glucocorticoid replacement dose is increased two to three times over a course of at least 3 days or more, if needed. If patients cannot take oral glucocorticoids or experience severe illness, then in IV/IM hydrocortisone is given as 200–300 mg/day in 3–4 doses (e.g., 50 mg every 6 h) [10, 72].
Adult women with hypopituitarism show decreased levels of androgens, including dehydroepiandrosterone (DHEA), dehydroepiandrosterone sulfate (DHEA-S), androstenedione, and testosterone. Some studies on DHEA replacement therapy to these patients have shown beneficial results on quality of life as well as improved mood and sexual function [73–76], whereas other studies have not shown such benefits [77, 78]. A meta-analysis that included randomized studies on the effect of DHEA replacement therapy on the quality of life of primary or secondary adrenal insufficient patients showed a small improvement in quality of life and depression, but no effect on anxiety and sexual well-being [79]. In the same meta-analysis, the most commonly reported side effects were greasy skin, hirsutism, acne, scalp itching, and increased apocrine sweat secretion and odor [79]. However, to date there is insufficient evidence to recommend routine DHEA replacement to these patients [72]. Moreover, in many countries, DHEA is only available as a dietary supplement, and therefore there are often variable and unreliable amounts of the drug in each pill. When DHEA is replaced, the usual dosage ranges from 25 to 50 mg in a single morning dose [80]. Clinical effects are observed only after several weeks of treatment. Monitoring should include measurement of DHEA-S (24 h after the previous dose) as well as free testosterone or total testosterone with sex hormone-binding globulin (SHBG) and estimation of free testosterone. If side effects are observed, then the dosage may be decreased by 50 %.
ADH Deficiency
Since polyuria and nocturia impair the quality of life, Desmopressin, a vasopressin analogue, should be given to most patients with DI [81]. Desmopressin is usually started as a single dose at night before the patient goes to sleep (e.g., 1 puff), which is increased until nocturia is controlled. A second dose (in the morning) and less commonly a third dose (in the afternoon) may be added as needed. Desmopressin is usually available as nasal spray, with one puff delivering 10 mcg. It is also available as a pill at a concentration of 0.1 mg per dose. In the inpatient setting, Desmopressin may also be given intravenously or subcutaneously at a dosage of 2–4 mcg/day in two divided doses.
Hormone Replacement Therapy Interactions
A critical aspect in the management of patients with hypopituitarism is the interplay between different replacement therapies. Remarkably, GH status impacts thyroid and adrenal replacement, and estrogen influences growth hormone dosages.
GH increases the conversion of T4 to T3 [31]. Hence, patients with combined and untreated GH and TSH deficiencies may show normal serum T4 levels, usually at the lower tertile, which masks the diagnosis of central hypothyroidism. Serum T4 levels fall below the normal range only after GH replacement in these cases [32]. On the other hand, a decrease in serum T4 levels after GH replacement should be evaluated carefully, since T3 levels usually concomitantly rise. If serum T4 levels fall to the mid-normal range, an increase in the dosage of levothyroxine is usually not necessary. Additionally, during concomitant GH and levothyroxine replacement therapy, serum T3 measurements may help to detect thyroxine over replacement [71].
In contrast to the action of GH on thyroid axis, GH enhances the conversion of cortisol to the biologically inactive cortisone through 11β-hydroxysteroid dehydrogenase type 1 [82]. Therefore, GH replacement may induce glucocorticoid insufficiency. This effect has been observed in patients with multiple pituitary deficiencies [83], but not in patients with isolated GH deficiency [84].
Oral estrogen replacement decreases the effect of GH on hepatic tissue, which consequently decreases IGF-I levels. Thus, patients on oral estrogen should have their dosage of GH increased [52, 85]. Since this effect is not observed in patients on transdermal estrogen due to lower concentrations of estrogen in the liver, this mode of administration is usually preferred in GH-deficient patients.
Long-Term Management
While radiotherapy is associated with progressive hypopituitarism, in the case of a pituitary tumor, even if hypofunction is present before surgical treatment, pituitary function should be reassessed postoperatively, as nearly as 50 % of pituitary deficiencies will resolve. Lifelong substitution therapy may thus not be necessary.
There is no evidence that GH replacement therapy is associated with the development of cancer, although the association of IGF-I levels and cancer in epidemiological studies has been explored. In addition, the evidence linking GH replacement therapy in GHD patients with the reversal of the highest rates of mortality observed in hypopituitarism is inconclusive.
More studies are needed in order to determine whether testosterone replacement in hypogonadal men increases the risk of developing or converting histological prostate cancer to the clinical form.
Potential Future Therapy
The presence of stem cells in the pituitary gland, which can give rise to all pituitary hormone cells, implies that these cells can be replaced after being lost or damaged. These stem cells could be of great usefulness in the treatment of hypopituitarism and may also have utility in the long-term management of pituitary deficiencies [86].
References
Regal M, et al. Prevalence and incidence of hypopituitarism in an adult Caucasian population in northwestern Spain. Clin Endocrinol (Oxf). 2001;55(6):735–40.
van Aken MO, Lamberts SW. Diagnosis and treatment of hypopituitarism: an update. Pituitary. 2005;8(3–4):183–91.
Toogood AA, Stewart PM. Hypopituitarism: clinical features, diagnosis, and management. Endocrinol Metab Clin North Am. 2008;37(1):235–61. x.
Hughes NR, Lissett CA, Shalet SM. Growth hormone status following treatment for Cushing’s syndrome. Clin Endocrinol (Oxf). 1999;51(1):61–6.
Prabhakar VK, Shalet SM. Aetiology, diagnosis, and management of hypopituitarism in adult life. Postgrad Med J. 2006;82(966):259–66.
Carroll PV, et al. Growth hormone deficiency in adulthood and the effects of growth hormone replacement: a review. Growth Hormone Research Society Scientific Committee. J Clin Endocrinol Metab. 1998;83(2):382–95.
Bhasin S, et al. Testosterone therapy in men with androgen deficiency syndromes: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2010;95(6):2536–59.
Bin-Abbas B, et al. Congenital hypogonadotropic hypogonadism and micropenis: effect of testosterone treatment on adult penile size why sex reversal is not indicated. J Pediatr. 1999;134(5):579–83.
Alexopoulou O, et al. Clinical and hormonal characteristics of central hypothyroidism at diagnosis and during follow-up in adult patients. Eur J Endocrinol. 2004;150(1):1–8.
Arlt W, Allolio B. Adrenal insufficiency. Lancet. 2003;361(9372):1881–93.
Fenske W, Allolio B. Current state and future perspectives in the diagnosis of diabetes insipidus: a clinical review. J Clin Endocrinol Metab. 2012;97:3426–37.
Rosenfeld RG, et al. Diagnostic controversy: the diagnosis of childhood growth hormone deficiency revisited. J Clin Endocrinol Metab. 1995;80(5):1532–40.
Richmond EJ, Rogol AD. Growth hormone deficiency in children. Pituitary. 2008;11(2):115–20.
Martha Jr PM, et al. Alterations in the pulsatile properties of circulating growth hormone concentrations during puberty in boys. J Clin Endocrinol Metab. 1989;69(3):563–70.
Bhala A, et al. Insulin-like growth factor axis parameters in sick hospitalized neonates. J Pediatr Endocrinol Metab. 1998;11(3):451–9.
Strasburger CJ, Bidlingmaier M. How robust are laboratory measures of growth hormone status? Horm Res. 2005;64 Suppl 2:1–5.
Gandrud LM, Wilson DM. Is growth hormone stimulation testing in children still appropriate? Growth Horm IGF Res. 2004;14(3):185–94.
Growth Hormone Research Society. Consensus guidelines for the diagnosis and treatment of growth hormone (GH) deficiency in childhood and adolescence: summary statement of the GH Research Society. GH Research Society. J Clin Endocrinol Metab. 2000;85(11):3990–3.
Lanes R, Hurtado E. Oral clonidine-an effective growth hormone-releasing agent in prepubertal subjects. J Pediatr. 1982;100(5):710–4.
Sandra P, Popovic V. Diagnosis of growth hormone deficiency in adults. In: Ho K, editor. Growth hormone related diseases and therapy: a molecular and physiological perspective for the clinician. New York, NY: Springer Science + business Media; 2011.
Leong KS, et al. An audit of 500 subcutaneous glucagon stimulation tests to assess growth hormone and ACTH secretion in patients with hypothalamic-pituitary disease. Clin Endocrinol (Oxf). 2001;54(4):463–8.
Molitch ME, et al. Evaluation and treatment of adult growth hormone deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2011;96(6):1587–609.
Lee P, Greenfield JR, Ho KK. Factors determining inadequate hypoglycaemia during insulin tolerance testing (ITT) after pituitary surgery. Clin Endocrinol (Oxf). 2009;71(1):82–5.
Ghigo E, et al. Arginine abolishes the inhibitory effect of glucose on the growth hormone response to growth hormone-releasing hormone in man. Metabolism. 1992;41(9):1000–3.
Corneli G, et al. The cut-off limits of the GH response to GH-releasing hormone-arginine test related to body mass index. Eur J Endocrinol. 2005;153(2):257–64.
Darzy KH, et al. The usefulness of the combined growth hormone (GH)-releasing hormone and arginine stimulation test in the diagnosis of radiation-induced GH deficiency is dependent on the post-irradiation time interval. J Clin Endocrinol Metab. 2003;88(1):95–102.
Clayton PE, et al. Consensus statement on the management of the GH-treated adolescent in the transition to adult care. Eur J Endocrinol. 2005;152(2):165–70.
Corneli G, et al. Cut-off limits of the GH response to GHRH plus arginine test and IGF-I levels for the diagnosis of GH deficiency in late adolescents and young adults. Eur J Endocrinol. 2007;157(6):701–8.
Maghnie M, et al. Diagnosis of GH deficiency in the transition period: accuracy of insulin tolerance test and insulin-like growth factor-I measurement. Eur J Endocrinol. 2005;152(4):589–96.
Oliveira JH, et al. Investigating the paradox of hypothyroidism and increased serum thyrotropin (TSH) levels in Sheehan’s syndrome: characterization of TSH carbohydrate content and bioactivity. J Clin Endocrinol Metab. 2001;86(4):1694–9.
Behan LA, Monson JP, Agha A. The interaction between growth hormone and the thyroid axis in hypopituitary patients. Clin Endocrinol (Oxf). 2011;74(3):281–8.
Portes ES, et al. Changes in serum thyroid hormones levels and their mechanisms during long-term growth hormone (GH) replacement therapy in GH deficient children. Clin Endocrinol (Oxf). 2000;53(2):183–9.
Doin FC, et al. Diagnosis of subclinical central hypothyroidism in patients with hypothalamic-pituitary disease by Doppler echocardiography. Eur J Endocrinol. 2012;166(4):631–40.
Faglia G. The clinical impact of the thyrotropin-releasing hormone test. Thyroid. 1998;8(10):903–8.
Mehta A, et al. Is the thyrotropin-releasing hormone test necessary in the diagnosis of central hypothyroidism in children. J Clin Endocrinol Metab. 2003;88(12):5696–703.
Wallace I, Cunningham S, Lindsay J. The diagnosis and investigation of adrenal insufficiency in adults. Ann Clin Biochem. 2009;46(Pt 5):351–67.
Thaler LM, Blevins Jr LS. The low dose (1-microg) adrenocorticotropin stimulation test in the evaluation of patients with suspected central adrenal insufficiency. J Clin Endocrinol Metab. 1998;83(8):2726–9.
Dorin RI, Qualls CR, Crapo LM. Diagnosis of adrenal insufficiency. Ann Intern Med. 2003;139(3):194–204.
Molitch ME. Pituitary tumours: pituitary incidentalomas. Best Pract Res Clin Endocrinol Metab. 2009;23(5):667–75.
Maiya B, et al. Magnetic resonance imaging changes in the pituitary gland following acute traumatic brain injury. Intensive Care Med. 2008;34(3):468–75.
Schneider HJ, et al. Pituitary imaging abnormalities in patients with and without hypopituitarism after traumatic brain injury. J Endocrinol Invest. 2007;30(4):RC9–12.
Wit JM. Growth hormone therapy. Best Pract Res Clin Endocrinol Metab. 2002;16(3):483–503.
Mauras N, et al. High dose recombinant human growth hormone (GH) treatment of GH-deficient patients in puberty increases near-final height: a randomized, multicenter trial. Genentech, Inc., Cooperative Study Group. J Clin Endocrinol Metab. 2000;85(10):3653–60.
Reiter EO, et al. Effect of growth hormone (GH) treatment on the near-final height of 1258 patients with idiopathic GH deficiency: analysis of a large international database. J Clin Endocrinol Metab. 2006;91(6):2047–54.
Cutfield WS, et al. Incidence of diabetes mellitus and impaired glucose tolerance in children and adolescents receiving growth-hormone treatment. Lancet. 2000;355(9204):610–3.
Cohen P, et al. Variable degree of growth hormone (GH) and insulin-like growth factor (IGF) sensitivity in children with idiopathic short stature compared with GH-deficient patients: evidence from an IGF-based dosing study of short children. J Clin Endocrinol Metab. 2010;95(5):2089–98.
Ranke MB, Lindberg A. Observed and predicted growth responses in prepubertal children with growth disorders: guidance of growth hormone treatment by empirical variables. J Clin Endocrinol Metab. 2010;95(3):1229–37.
Thuesen L, et al. Short and long-term cardiovascular effects of growth hormone therapy in growth hormone deficient adults. Clin Endocrinol (Oxf). 1994;41(5):615–20.
Tomlinson JW, et al. Association between premature mortality and hypopituitarism. West Midlands Prospective Hypopituitary Study Group. Lancet. 2001;357(9254):425–31.
Rossouw JE, et al. Risks and benefits of estrogen plus progestin in healthy postmenopausal women: principal results From the Women’s Health Initiative randomized controlled trial. JAMA. 2002;288(3):321–33.
Beral V. Breast cancer and hormone-replacement therapy in the Million Women Study. Lancet. 2003;362(9382):419–27.
Mah PM, et al. Estrogen replacement in women of fertile years with hypopituitarism. J Clin Endocrinol Metab. 2005;90(11):5964–9.
Menon DV, Vongpatanasin W. Effects of transdermal estrogen replacement therapy on cardiovascular risk factors. Treat Endocrinol. 2006;5(1):37–51.
Leung KC, et al. Estrogen regulation of growth hormone action. Endocr Rev. 2004;25(5):693–721.
Kiess W, et al. Induction of puberty in the hypogonadal girl–practices and attitudes of pediatric endocrinologists in Europe. Horm Res. 2002;57(1–2):66–71.
Ankarberg-Lindgren C, et al. Nocturnal application of transdermal estradiol patches produces levels of estradiol that mimic those seen at the onset of spontaneous puberty in girls. J Clin Endocrinol Metab. 2001;86(7):3039–44.
Ascoli P, Cavagnini F. Hypopituitarism. Pituitary. 2006;9(4):335–42.
Schurmeyer T, et al. Saliva and serum testosterone following oral testosterone undecanoate administration in normal and hypogonadal men. Acta Endocrinol (Copenh). 1983;102(3):456–62.
Schulte-Beerbuhl M, Nieschlag E. Comparison of testosterone, dihydrotestosterone, luteinizing hormone, and follicle-stimulating hormone in serum after injection of testosterone enanthate of testosterone cypionate. Fertil Steril. 1980;33(2):201–3.
Schubert M, et al. Intramuscular testosterone undecanoate: pharmacokinetic aspects of a novel testosterone formulation during long-term treatment of men with hypogonadism. J Clin Endocrinol Metab. 2004;89(11):5429–34.
Zitzmann M, Nieschlag E. Hormone substitution in male hypogonadism. Mol Cell Endocrinol. 2000;161(1–2):73–88.
Jordan Jr WP. Allergy and topical irritation associated with transdermal testosterone administration: a comparison of scrotal and nonscrotal transdermal systems. Am J Contact Dermat. 1997;8(2):108–13.
Swerdloff RS, et al. Long-term pharmacokinetics of transdermal testosterone gel in hypogonadal men. J Clin Endocrinol Metab. 2000;85(12):4500–10.
Wang C, et al. Efficacy and safety of the 2% formulation of testosterone topical solution applied to the axillae in androgen-deficient men. Clin Endocrinol (Oxf). 2011;75(6):836–43.
Dobs AS, et al. A novel testosterone 2% gel for the treatment of hypogonadal males. J Androl. 2012;33(4):601–7.
Meikle AW, et al. Pharmacokinetics and metabolism of a permeation-enhanced testosterone transdermal system in hypogonadal men: influence of application site- -a clinical research center study. J Clin Endocrinol Metab. 1996;81(5):1832–40.
Wang C, et al. New testosterone buccal system (Striant) delivers physiological testosterone levels: pharmacokinetics study in hypogonadal men. J Clin Endocrinol Metab. 2004;89(8):3821–9.
Jockenhovel F, et al. Pharmacokinetics and pharmacodynamics of subcutaneous testosterone implants in hypogonadal men. Clin Endocrinol (Oxf). 1996;45(1):61–71.
Vicari E, et al. Therapy with human chorionic gonadotrophin alone induces spermatogenesis in men with isolated hypogonadotrophic hypogonadism–long-term follow-up. Int J Androl. 1992;15(4):320–9.
Yamada M, Mori M. Mechanisms related to the pathophysiology and management of central hypothyroidism. Nat Clin Pract Endocrinol Metab. 2008;4(12):683–94.
Martins MR, et al. Growth hormone replacement improves thyroxine biological effects: implications for management of central hypothyroidism. J Clin Endocrinol Metab. 2007;92(11):4144–53.
Neary N, Nieman L. Adrenal insufficiency: etiology, diagnosis and treatment. Curr Opin Endocrinol Diabetes Obes. 2010;17(3):217–23.
Arlt W, et al. Oral dehydroepiandrosterone for adrenal androgen replacement: pharmacokinetics and peripheral conversion to androgens and estrogens in young healthy females after dexamethasone suppression. J Clin Endocrinol Metab. 1998;83(6):1928–34.
Bilger M, et al. Androgen replacement in adolescents and young women with hypopituitarism. J Pediatr Endocrinol Metab. 2005;18(4):355–62.
Johannsson G, et al. Low dose dehydroepiandrosterone affects behavior in hypopituitary androgen-deficient women: a placebo-controlled trial. J Clin Endocrinol Metab. 2002;87(5):2046–52.
van Thiel SW, et al. Effects of dehydroepiandrostenedione, superimposed on growth hormone substitution, on quality of life and insulin-like growth factor I in patients with secondary adrenal insufficiency: a randomized, placebo-controlled, cross-over trial. J Clin Endocrinol Metab. 2005;90(6):3295–303.
Libe R, et al. Effects of dehydroepiandrosterone (DHEA) supplementation on hormonal, metabolic and behavioral status in patients with hypoadrenalism. J Endocrinol Invest. 2004;27(8):736–41.
Lovas K, et al. Replacement of dehydroepiandrosterone in adrenal failure: no benefit for subjective health status and sexuality in a 9-month, randomized, parallel group clinical trial. J Clin Endocrinol Metab. 2003;88(3):1112–8.
Alkatib AA, et al. A systematic review and meta-analysis of randomized placebo-controlled trials of DHEA treatment effects on quality of life in women with adrenal insufficiency. J Clin Endocrinol Metab. 2009;94(10):3676–81.
Hahner S, Allolio B. Therapeutic management of adrenal insufficiency. Best Pract Res Clin Endocrinol Metab. 2009;23(2):167–79.
Schneider HJ, et al. Hypopituitarism. Lancet. 2007;369(9571):1461–70.
Filipsson H, Johannsson G. GH replacement in adults: interactions with other pituitary hormone deficiencies and replacement therapies. Eur J Endocrinol. 2009;161 Suppl 1:S85–95.
Giavoli C, et al. Effect of recombinant human growth hormone (GH) replacement on the hypothalamic-pituitary-adrenal axis in adult GH-deficient patients. J Clin Endocrinol Metab. 2004;89(11):5397–401.
Giavoli C, et al. Effect of growth hormone deficiency and recombinant hGH (rhGH) replacement on the hypothalamic-pituitary-adrenal axis in children with idiopathic isolated GH deficiency. Clin Endocrinol (Oxf). 2008;68(2):247–51.
Cook DM, Ludlam WH, Cook MB. Route of estrogen administration helps to determine growth hormone (GH) replacement dose in GH-deficient adults. J Clin Endocrinol Metab. 1999;84(11):3956–60.
Castinetti F, et al. Pituitary stem cell update and potential implications for treating hypopituitarism. Endocr Rev. 2011;32(4):453–71.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer Science+Business Media New York
About this chapter
Cite this chapter
Faria, M., Nascimento, G.C., Faria, A.M., Martins, M.R.A. (2014). Hypopituitarism. In: Bandeira, F., Gharib, H., Golbert, A., Griz, L., Faria, M. (eds) Endocrinology and Diabetes. Springer, New York, NY. https://doi.org/10.1007/978-1-4614-8684-8_8
Download citation
DOI: https://doi.org/10.1007/978-1-4614-8684-8_8
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4614-8683-1
Online ISBN: 978-1-4614-8684-8
eBook Packages: MedicineMedicine (R0)