Abstract
The goals of medical treatment of celiac disease (CD) are to: (1) encourage dietary compliance, (2) manage and monitor symptoms, and (3) prevent and detect associated diseases and/or complications. The underlying aim in the care of patients with CD is to ensure that patients have initial and sustained symptomatic improvement and to prevent long-term sequelae that can result from chronic gluten exposure. Currently, available guidelines on the follow-up of patients with CD are often incomplete or variable, partially due to a dearth of research on this topic. This chapter synthesizes available guidelines and expert opinion to recommend the essential components of medical follow-up of CD patients for practicing physicians.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Introduction
The only available treatment for celiac disease (CD) is a strict, lifelong gluten-free diet, which requires avoidance of gluten-containing grains such as wheat, barley, and rye. Although oats are generally safe in those with CD, cross-contamination can lead to inadvertent gluten ingestion, so oats are often avoided for the first year after the diagnosis of CD is made, with introduction thereafter if symptoms are controlled. Patients need to be advised that many other products may contain gluten, such as medications (including vitamin and mineral supplements), cosmetics, dental products, adhesive glues (envelopes), communion wafers, and more. Research has found in some patients as little as one-thirtieth of a loaf of bread can have enough gluten to cause intestinal damage if consumed regularly [1, 2].
Given the lack of currently available pharmacologic treatments, some may perceive the management of CD to be “out of the hands of the physician.” However, this is far from the truth, as physicians play a pivotal role in the counseling of patients with CD. Without such support, patients may have poor compliance with treatment, which can lead to delayed intestinal healing, ongoing symptoms, and an increased risk for associated diseases, including malignancy [3, 4]. The mortality risk for undiagnosed or noncompliant CD patients appears to be increased compared to the general population; however, when a gluten-free diet is followed, this risk may decrease, which can be an additional motivating factor for patients beyond control of symptoms [5–7]. In the following chapter, we will discuss the management of CD via a concerted multidisciplinary approach with attention given to the medical, dietary, and psychosocial aspects of this complex disease in order to avoid celiac-related complications.
Rationale for Follow-Up
CD is a chronic disease that is felt to be lifelong and as such requires long-term follow-up. Although there are rare reports of patients who develop latency of their CD and have resumed a gluten-containing diet, this is certainly the exception and may put these individuals at risk of developing recurrent small bowel inflammation and associated complications [8].
CD has protean manifestations. While the classic features of CD include malabsorption, diarrhea, weight loss, malnutrition, and delayed growth, there is a broad spectrum of disease manifestations including iron-deficiency anemia, metabolic bone disease, infertility, fatigue, dermatitis herpetiformis, and many more. Symptomatically, the vast majority of patients with celiac disease who start a gluten-free diet can see improvement in diarrhea within days after initiation, and most will have complete resolution of diarrhea by 6 months into treatment, with a mean improvement time of 4 weeks [7, 9]. Additionally, other gastrointestinal features of CD (bloating, abdominal pain, fecal incontinence, weight loss) tend to improve at a similar rate for most patients [9].
The gluten-free diet, albeit a challenge to ascribe to, is safe and effective in treating CD [10]. The situations where compliance with a gluten-free diet can be most challenging include a change in social situation (going to college, moving in with others, etc.), eating out at restaurants, grocery shopping, traveling, or when patients are asymptomatic or detected through family screening. The availability of regular follow-up with a multidisciplinary team that has specialized knowledge of a gluten-free diet and is familiar with overcoming barriers to adherence is absolutely necessary.
Despite an increasing awareness of CD in the community, it is concerning that patients have such a variable rate of adherence to a gluten-free diet. In a 2009 systematic review, compliance with a gluten-free diet was found to be anywhere from 42 % to 91 % among CD patients, but typically lower rates of compliance were seen when a gluten-free diet was defined more rigorously [1, 4]. Even more concerning is recent literature that highlights that physicians are failing to assess CD patients regarding compliance to a gluten-free diet, further impacting patients’ perception of its importance. A 2012 retrospective assessment of medical care in a CD population living in Olmsted County revealed that nearly one-third of patients followed longitudinally had “celiac disease assessments” that did not document nor discuss compliance to a gluten-free diet [11].
A lack of appropriate dietary counseling can lead to adverse consequences, given a large portion of CD has been shown to have inadequate mucosal healing long after the disease has been diagnosed and despite ascribing to what they believe is an appropriate diet, highlighting that inadequate education can lead to inadvertent ingestion [7, 12]. Although mucosal healing may take several years to occur (especially in adults), it is a possible and desirable outcome. Noting the likelihood for ongoing disease activity in a majority of the CD population, it is not entirely surprising that patients with CD appear to have a modestly increased risk of mortality conferred by poor compliance to a gluten-free diet and ongoing intestinal inflammation [5–7].
There are diseases and conditions associated with CD such as autoimmune thyroid disease, type 1 diabetes, microscopic colitis, IgA deficiency, infertility, autoimmune liver disease, neurologic conditions, and genetic syndromes (Down, Turner, and Williams) [13–17]. It important for the clinician and patient to be aware of these associations and to also realize that untreated CD with ongoing gluten exposure and intestinal mucosal inflammation is likely to increase the severity of many extraintestinal manifestations (such as iron deficiency anemia, metabolic bone disease, and many others). Adherence to a gluten-free diet is correlated with not only improved health but also improved scores on standardized quality of life assessments [14, 18, 19].
The need for regular follow-up to promote compliance and avoid complications in CD has been well established, and it is becoming increasingly clear that many medical providers and patients may not be aware of current recommendations [11, 20].
Current Expert Opinion and Medical Society Recommendations
Despite multiple expert opinion papers and practice guidelines published on the optimal long-term monitoring of patients with CD, it remains a controversial topic due to disparate guidelines, scarce good-quality research (evidence-based recommendations), and highly variable practices among clinicians [10, 11, 14, 21–28]. A systematic review synthesizing the multiple practice guidelines also exists, which highlights the highly variable cost of care among guidelines [28]. Many guidelines focus largely on the diagnosis of CD, where more objective data have been presented. Table 12.1 reviews the currently published recommendations for longitudinal follow-up of patients with CD.
Essential Aspects of Follow-Up
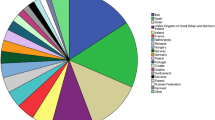
The following recommendations reflect a synthesis of available guidelines and expert opinions, and in instances where there was a paucity of evidence, the authors’ expert opinion and institutional practice were included. For a graphic representation of these recommendations, please see Fig. 12.1.
Proposed CD management plan. 1TTG tissue transglutaminase, 3DEXA dual-energy X-ray absorptiometry, 2DGP deaminated gliadin peptide, EMA endomysial antibody, CBC complete blood count, TSH thyroid-stimulating hormone. Adapted from [61]
Overall Objectives
-
1.
Encourage dietary compliance through increased education and accountability
-
2.
Monitor for ongoing or recurrent symptoms
-
3.
Prevention and early detection of celiac-associated diseases and conditions
Frequency of Follow-Up
Follow-up is important in encouraging dietary compliance; however, there is no solid evidence to guide the optimal schedule for follow-up of patients with CD. A reasonable approach to follow-up is a visit in 3–6 months, then annually from date of diagnosis. In one study, annual follow-up with serology (tissue transglutaminase antibody) improved adherence to a gluten-free diet and led to seroconversion in 95 % of patients over a period of 5 years [20]. Ideally, the patient’s primary care provider should be knowledgeable about CD in order to evaluate their status at routine annual visits, which are often used for other immunizations, growth assessments, screening, and medication refills. The follow-up interval can be lengthened to every 2 years, but only if patients are doing well on a gluten-free diet, have no ongoing symptoms, negative celiac serologies, and no nutritional deficiencies.
Provider Type
The concept of a multidisciplinary approach to follow-up has been of interest in a time when specialization and non-physician provider use has increased. Additionally, it has become clear that many physicians, regardless of specialty, have limited knowledge of CD and do not adequately assess compliance to the gluten-free diet or screen for disease-specific complications [11, 29]. Patient preference for follow-up is also important in aiding in compliance, given a British survey of patients with CD found that patients preferred that their annual follow-up was with a dietitian, with a doctor available if necessary [30]. It is important to note that most of these patients also felt that the annual review, associated with reassurance and blood testing, was “very useful,” highlighting that the annual visit would require a physician to order and review serologic assessments in most medical systems.
In another study, 698 Finnish patients who were newly diagnosed with CD were surveyed to assess their experiences regarding the management of their disease. Patients were more pleased when they obtained dietary counseling from dieticians, and felt that the dietary counseling provided from physicians was not adequate or felt rushed [31]. Thus, the most important factor in choosing a long-term provider is selecting one with a knowledge and interest in caring for those with CD and finding a dietician well versed in the disease. In our practice, follow-up is guided by a physician. Assessment of the diet by an expert dietician is highly encouraged.
Serology
Serology can be useful in confirming response and compliance to the gluten-free diet. Adherence to a gluten-free diet is associated with a decrease in the absolute value of baseline celiac serology levels [32, 33]. The most accepted serologic studies for following CD activity include IgA tissue trans-glutaminase (TTG), IgA or IgG deaminated gliadin peptide (DGP), or IgA endomysial antibody (EMA). In patients who are known to be IgA deficient, an IgG-based serologic study (TTG or DGP) would be needed for diagnosis and monitoring. In this role, the sensitivity of TTG and EMA appear to be similar, with DGP being shown more recently to have some superiority [34]. It is important to note that the sensitivity of these markers decreases for small to moderate dietary transgressions, and so a normal value does not ensure full compliance [34, 35]. Increasingly, data have indicated that patients with normalized serology may continue to have ongoing intestinal inflammation and gluten contamination in their diets [36]. While it is expected that a patient who follows a gluten-free diet will have serologic normalization as early as 3 months after diagnosis, the converse is not always true, in that a patient who continues to consume gluten may have falsely normal serology, and therefore serology should not be the solitary means to monitor for treatment compliance [32]. There is no evidence to guide optimal frequency of serologic monitoring in CD patients; however, most guidelines suggest a reasonable approach would be annual serology, with consideration given to extending the interval only after a patient has proven to be very stable and successful on the gluten-free diet.
Assessing Mucosal Recovery: Repeat Duodenal Biopsy
Mucosal recovery generally requires several years of strict gluten avoidance in adults and is often patchy or incomplete [7, 12, 37, 38]. Duodenal biopsy is the gold standard for assessing mucosal healing. While it has been proposed that repeating duodenal biopsy to confirm healing should be a regular measure in all CD patients after 12 months on a gluten-free diet, the cost and invasive nature of endoscopic biopsy must be considered, as well as the lack of solid evidence supporting this practice. It is notable that adult celiac specialists often favor repeat intestinal biopsy over pediatric celiac specialists, which may be due to a variety of factors; adults often have delayed healing and are at increased risk for refractory CD and lymphoproliferative disease if inflammation is persistent [39].
In patients with persistent or recurrent symptoms, detailed dietary review is indicated, and if necessary, small bowel biopsy or other investigations should be employed. If a patient has persistent symptoms, despite strictly following a gluten-free diet, it is essential to repeat biopsy to look for evidence of refractory CD [40].
Capsule endoscopy is a new technique that can detect mucosal lesions that suggest villous atrophy (fissures, loss of folds, cobblestone pattern, scalloping), but this method has not been widely used or systematically evaluated as a method of clinical follow-up and may be reserved for those presenting with refractory symptoms, assuming there are no obstructing processes within the small bowel such as intussusception or malignancy [41]. Additionally, capsule endoscopy may be useful for patients unwilling or unable to undergo upper endoscopy.
Use of Routine Laboratory Studies
The use of routine laboratory studies in following CD has also not been systematically studied, but should be used to confirm resolution of nutritional deficiencies or abnormalities that were present at diagnosis. At diagnosis, it is recommended that patients be assessed for anemia, malnutrition, vitamin or mineral deficiencies, liver test abnormalities, and thyroid dysfunction [14, 42]. This can be done by checking a complete blood count (with serum ferritin if anemia is present), vitamin B12, folate, albumin, calcium, 25-hydroxyvitamin D3, alkaline phosphatase, alanine aminotransferase, and thyroid stimulating hormone levels. If indicated based on clinical symptoms or features of fat malabsorption, vitamin A and E levels could be checked, and similarly, trace minerals as indicated by the clinical presentation (may include zinc or copper). These should be followed until corrected and then periodically thereafter if there are ongoing concerns. If there is delayed or no recovery from baseline laboratory abnormalities, this may suggest gluten contamination in the diet, refractory CD, or another underlying disorder.
Hyposplenism and Immunization
CD is commonly correlated with functional hyposplenia (33–76 % prevalence) and increased risk of sepsis [43, 44]. Thus, immunization for encapsulated organisms in celiac patients including Streptococcus pneumonia, Haemophilus influenza type B, and Neisseria meningitides is recommended if not already immunized at time of diagnosis.
Screening for Associated Diseases
Decreased Bone Density
Patients with CD have an increased risk of low bone mineral density and an increased risk of fracture [45]. There is evidence that bone demineralization will improve and possibly reverse upon institution of a gluten-free diet after adequate time for recovery [46, 47]. Thus, the most important preventive measure is gluten avoidance. The 2012 British Society for Gastroenterology recommends that only those patients with CD who have additional risk factors (age, smoking, low BMI, persistent malabsorptive symptoms, etc.) undergo dual X-ray absorptiometry (DEXA) scan at diagnosis. Others have recommended DEXA in all adult patients diagnosed with CD, with repeat testing in subsequent years only if the baseline study was abnormal or if other risk factors for metabolic bone disease are present (i.e., menopause) [2]. All patients with CD should have periodic assessment of risk and repeat DEXA scanning if appropriate. Patients should have adequate dietary calcium and vitamin D supplementation for their age, or based on laboratory or DEXA testing. Baseline assessment of calcium, alkaline phosphatase, and 25-hydroxyvitamin D3 levels should be considered [45]. Antiresorptive agents should be considered in patients with persistent or progressive bone loss in addition to continuing a gluten-free diet, calcium, and vitamin D supplementation [48, 49].
Screening for Malignancy
The increased risk of malignancy in CD is attributable to non-Hodgkin lymphoma, particularly enteropathy associated T-cell lymphoma (EATL). For patients who follow a strict gluten-free diet and achieve mucosal healing, the risk of EATL is felt to be on par with that of the general population [50]. Thus, regular follow-up to encourage compliance of a gluten-free diet is the best method for reducing risk of malignancy. Aside from this, there is no evidence to support routine screening for malignancy in celiac patients beyond what would be recommended for the general population. However, if a patient has refractory symptoms, they must undergo further evaluation to assess for lymphoproliferative changes of the small bowel [39]. Patients with CD have a higher risk of small bowel adenocarcinoma, nasopharyngeal carcinoma, and carcinoma of the esophagus, but these reports have not always been fully validated in multiple geographic locations [51]. The presence of symptoms or signs suggestive of these malignancies should prompt immediate clinical evaluation [2, 39].
Other Autoimmune Diseases
Many autoimmune diseases do appear to have increased prevalence among patients with CD, which include type 1 diabetes melitus (DM), autoimmune thyroid disease, autoimmune liver disease, alopecia areata, and microscopic colitis [14]. While no routine screening is required for these conditions, patients should have thyroid testing and baseline liver biochemistries at time of diagnosis, and only repeated later if a baseline study was abnormal or there are new clinical symptoms or concerns.
Alarm Features
The following symptoms and signs should prompt further work-up to investigate the potential complications and associated diseases involved in CD including enteropathy associated T-cell lymphoma, ulcerative jejunitis, or refractory CD (types I and II.)
-
“B symptoms” (night sweats, fevers, weight loss)
-
Increasing titers or persistently positive celiac serology
-
New or persistent nutritional abnormalities
-
New or persistent symptoms
Special Considerations for Children
Like in adults, the majority of children with CD are asymptomatic [52]. Clinical features of CD in children differ by age. Intestinal symptoms are common in children diagnosed within the first 2 years of life; failure to thrive, chronic diarrhea, vomiting, and abdominal distention are present in most cases. Extraintestinal manifestations, without any accompanying digestive symptoms, are more common in older children and adolescents. Short stature and iron deficiency anemia are the most recognized non-digestive manifestation of CD in children [53, 54].
Rapid resolution of the clinical symptoms is usually noted within a few weeks after starting the gluten-free diet. Most children are compliant with a gluten-free diet, especially when diagnosed early in life. Asymptomatic older children and adolescents may experience difficulties in modifying their lifestyles and being compliant with a gluten-free diet [55].
When a child is diagnosed with CD, all immediate family members should be screened with serologic testing. There are no clear guidelines on when to screen younger siblings (infants). The current practice is to screen them between 2 and 3 years of age, sooner if symptomatic, and consider repeating at 3- to 5-year intervals if asymptomatic until adulthood.
Children with positive serology and normal intestinal mucosa are referred to as “potential celiac” patients, and unlike adults patients with latent CD, they have never experienced intestinal villous atrophy [56]. There is no agreement on the management of these patients, but they will be given the option of normal diet with close observation and follow-up.
Psycho-Social Support
Patients often struggle with attending social gatherings, which are frequently oriented around food, much of which they will be unable to consume. This can leave patients feeling frustrated, isolated, and depressed, not to mention perhaps under more financial stress given the increased cost associated with a gluten-free diet prescription. Patients with CD benefit from involvement in local celiac support groups and societies; when involved, they are more likely to be compliant on a gluten-free diet and cope better with the burden of disease [57].
Improvements on the Forefront for Celiac Disease Management
Improving Compliance and Risk Stratification
More CD research has allowed for a better understanding of patient preferences and unique risks. Certain patients with CD appear to be less likely to follow the gluten-free diet, such as those diagnosed as adolescents, those without classic symptoms and those asymptomatic individuals diagnosed through family screening programs [58]. These groups should be targeted for future research and intervention. More exploration is needed to identify genetically high-risk subgroups of CD populations and tailor our management approach as well. This could allow for closer surveillance in groups with higher risk of developing refractory CD or other complications. Drug development is an area of active research that may become a reality in the near future.
Quality Improvement
A unique approach to assess compliance with validated questionnaires has been explored and could have increased utilization and applicability within new electronic medical record systems [59, 60]. Use of medical care process models could guide physicians to a standardized approach to the diagnosis and follow-up of patients with CD and would provide a quick reference during an office visit to improve the quality and cost-effectiveness of care.
Conclusion
An active livelong follow-up strategy is necessary in patients with CD to improve clinical outcomes and patient satisfaction. Further research and refinement of guidelines are likely to occur in the next few years and will help to further guide practitioners.
References
Catassi C, Fabiani E, Iacono G, D’Agate C, Francavilla R, Biagi F, et al. A prospective, double-blind, placebo-controlled trial to establish a safe gluten threshold for patients with celiac disease [Multicenter Study Randomized Controlled Trial Research Support, Non-U.S. Gov’t]. Am J Clin Nutr. 2007;85(1):160–6.
Leffler D. Celiac disease diagnosis and management: a 46-year-old woman with anemia [Case Reports Clinical Conference]. JAMA. 2011;306(14):1582–92.
Godfrey JD, Brantner TL, Brinjikji W, Christensen KN, Brogan DL, Van Dyke CT, et al. Morbidity and mortality among older individuals with undiagnosed celiac disease [Research Support, N.I.H., Extramural]. Gastroenterology. 2010;139(3):763–9.
Hall NJ, Rubin G, Charnock A. Systematic review: adherence to a gluten-free diet in adult patients with coeliac disease [Research Support, Non-U.S. Gov’t Review]. Aliment Pharmacol Ther. 2009;30(4):315–30.
Rubio-Tapia A, Kyle RA, Kaplan EL, Johnson DR, Page W, Erdtmann F, et al. Increased prevalence and mortality in undiagnosed celiac disease [Research Support, N.I.H., Extramural]. Gastroenterology. 2009;137(1):88–93.
Ludvigsson JF, Montgomery SM, Ekbom A, Brandt L, Granath F. Small-intestinal histopathology and mortality risk in celiac disease [Research Support, Non-U.S. Gov’t]. JAMA. 2009;302(11):1171–8.
Rubio-Tapia A, Rahim MW, See JA, Lahr BD, Wu TT, Murray JA. Mucosal recovery and mortality in adults with celiac disease after treatment with a gluten-free diet [Research Support, N.I.H., Extramural]. Am J Gastroenterol. 2010;105(6):1412–20.
Matysiak-Budnik T, Malamut G, de Serre NPM, Grosdidier E, Seguier S, Brousse N, et al. Long-term follow-up of 61 coeliac patients diagnosed in childhood: evolution toward latency is possible on a normal diet. Gut. 2007;56(10):1379–86.
Murray JA, Watson T, Clearman B, Mitros F. Effect of a gluten-free diet on gastrointestinal symptoms in celiac disease [Research Support, U.S. Gov’t, P.H.S.]. Am J Clin Nutr. 2004;79(4):669–73.
Pietzak MM. Follow-up of patients with celiac disease: achieving compliance with treatment. Gastroenterology. 2005;128(4 Suppl 1):S135–41.
Herman ML, Rubio-Tapia A, Lahr BD, Larson JJ, Van Dyke CT, Murray JA. Patients with celiac disease are not followed up adequately [Research Support, N.I.H., Extramural Research Support, Non-U.S. Gov’t]. Clin Gastroenterol Hepatol. 2012;10(8):893–9.e1.
Lanzini A, Lanzarotto F, Villanacci V, Mora A, Bertolazzi S, Turini D, et al. Complete recovery of intestinal mucosa occurs very rarely in adult coeliac patients despite adherence to gluten-free diet. Aliment Pharmacol Ther. 2009;29(12):1299–308.
Hernandez L, Green PH. Extraintestinal manifestations of celiac disease [Review]. Curr Gastroenterol Rep. 2006;8(5):383–9.
Haines ML, Anderson RP, Gibson PR. Systematic review: the evidence base for long-term management of coeliac disease [Review]. Aliment Pharmacol Ther. 2008;28(9):1042–66.
Dias JA, Walker-Smith J. Down’s syndrome and coeliac disease [Case Reports]. J Pediatr Gastroenterol Nutr. 1990;10(1):41–3.
Bonamico M, Pasquino AM, Mariani P, Danesi HM, Culasso F, Mazzanti L, et al. Prevalence and clinical picture of celiac disease in Turner syndrome [Multicenter Study Research Support, Non-U.S. Gov’t]. J Clin Endocrinol Metab. 2002;87(12):5495–8.
Giannotti A, Tiberio G, Castro M, Virgilii F, Colistro F, Ferretti F, et al. Coeliac disease in Williams syndrome. J Med Genet. 2001;38(11):767–8.
Nachman F, del Campo MP, Gonzalez A, Corzo L, Vazquez H, Sfoggia C, et al. Long-term deterioration of quality of life in adult patients with celiac disease is associated with treatment noncompliance [Comparative Study Research Support, Non-U.S. Gov’t]. Dig Liver Dis. 2010;42(10):685–91.
Nachman F, Maurino E, Vazquez H, Sfoggia C, Gonzalez A, Gonzalez V, et al. Quality of life in celiac disease patients: prospective analysis on the importance of clinical severity at diagnosis and the impact of treatment [Comparative Study Research Support, Non-U.S. Gov’t]. Dig Liver Dis. 2009;41(1):15–25.
Zanini B, Lanzarotto F, Mora A, Bertolazzi S, Turini D, Cesana B, et al. Five year time course of celiac disease serology during gluten-free diet: results of a community based “CD-Watch” program. Dig Liver Dis. 2010;42(12):865–70.
AGA Institute Medical Position Statement on the Diagnosis and management of celiac disease [Practice Guideline]. Gastroenterology. 2006;131(6):1977–80.
National Institutes of Health Consensus Development Conference Statement on Celiac Disease, June 28–30, 2004 [Consensus Development Conference Consensus Development Conference, NIH Review]. Gastroenterology. 2005;128(4 Suppl 1):S1–9.
Hill ID, Dirks MH, Liptak GS, Colletti RB, Fasano A, Guandalini S, et al. Guideline for the diagnosis and treatment of celiac disease in children: recommendations of the North American Society for Pediatric Gastroenterology, Hepatology and Nutrition [Practice Guideline]. J Pediatr Gastroenterol Nutr. 2005;40(1):1–19.
Bai JF, Corazza GR, Schuppan DL, Farthing M, Catassi C, Greco L, Cohen H, Ciacci C, Fasano A, González A, Krabshuis JH, LeMair A. World Gastroenterology Organisation Global Guidelines–Celiac disease. Milwaukee, WI: World Gastroenterology Organisation; 2012.
Guidelines for the management of patients with coeliac disease. Glasgow: British Society for Gastroenterology; 2010.
The management of adults with coeliac disease in primary care. London: Primary Care Society for Gastroenterology; 2006.
Fasano A, Catassi C. Celiac disease. N Engl J Med. 2012;367(25):2419–26.
Silvester JA, Rashid M. Long-term follow-up of individuals with celiac disease: an evaluation of current practice guidelines [Review]. Can J Gastroenterol. 2007;21(9):557–64.
Leffler DA, Edwards George JB, Dennis M, Cook EF, Schuppan D, Kelly CP. A prospective comparative study of five measures of gluten-free diet adherence in adults with coeliac disease [Comparative Study Research Support, N.I.H., Extramural Research Support, Non-U.S. Gov’t]. Aliment Pharmacol Ther. 2007;26(9):1227–35.
Bebb JR, Lawson A, Knight T, Long RG. Long-term follow-up of coeliac disease–what do coeliac patients want? Aliment Pharmacol Ther. 2006;23(6):827–31.
Ukkola A, Maki M, Kurppa K, Collin P, Huhtala H, Kekkonen L, et al. Patients’ experiences and perceptions of living with coeliac disease – implications for optimizing care [Clinical Trial Research Support, Non-U.S. Gov’t]. J Gastrointest Liver Dis. 2012;21(1):17–22.
Nachman F, Sugai E, Vazquez H, Gonzalez A, Andrenacci P, Niveloni S, et al. Serological tests for celiac disease as indicators of long-term compliance with the gluten-free diet [Research Support, Non-U.S. Gov’t]. Eur J Gastroenterol Hepatol. 2011;23(6):473–80.
Sugai E, Nachman F, Vaquez H, Gonzalez A, Andrenacci P, Czech A, et al. Dynamics of celiac disease-specific serology after initiation of a gluten-free diet and use in the assessment of compliance with treatment [Research Support, Non-U.S. Gov’t]. Dig Liver Dis. 2010;42(5):352–8.
Monzani A, Rapa A, Fonio P, Tognato E, Panigati L, Oderda G. Use of deamidated gliadin peptide antibodies to monitor diet compliance in childhood celiac disease [Comparative Study Research Support, Non-U.S. Gov’t]. J Pediatr Gastroenterol Nutr. 2011;53(1):55–60.
Vahedi K, Mascart F, Mary JY, Laberenne JE, Bouhnik Y, Morin MC, et al. Reliability of antitransglutaminase antibodies as predictors of gluten-free diet compliance in adult celiac disease [Comparative Study]. Am J Gastroenterol. 2003;98(5):1079–87.
Tursi A, Brandimarte G, Giorgetti GM. Lack of usefulness of anti-transglutaminase antibodies in assessing histologic recovery after gluten-free diet in celiac disease. J Clin Gastroenterol. 2003;37(5):387–91.
Wahab PJ, Meijer JW, Mulder CJ. Histologic follow-up of people with celiac disease on a gluten-free diet: slow and incomplete recovery. Am J Clin Pathol. 2002;118(3):459–63.
Macdonald WC, Brandborg LL, Flick AL, Trier JS, Rubin CE. Studies of celiac sprue. IV. The response of the whole length of the small bowel to a gluten-free diet. Gastroenterology. 1964;47:573–89.
Rubio-Tapia A, Murray JA. Classification and management of refractory coeliac disease [Research Support, N.I.H., Extramural Review]. Gut. 2010;59(4):547–57.
Daum S, Ipczynski R, Schumann M, Wahnschaffe U, Zeitz M, Ullrich R. High rates of complications and substantial mortality in both types of refractory sprue. Eur J Gastroenterol Hepatol. 2009;21(1):66–70.
Atlas DS, Rubio-Tapia A, Van Dyke CT, Lahr BD, Murray JA. Capsule endoscopy in nonresponsive celiac disease [Comparative Study Research Support, N.I.H., Extramural Research Support, Non-U.S. Gov’t]. Gastrointest Endosc. 2011;74(6):1315–22.
Sategna-Guidetti C, Volta U, Ciacci C, Usai P, Carlino A, De Franceschi L, et al. Prevalence of thyroid disorders in untreated adult celiac disease patients and effect of gluten withdrawal: an Italian multicenter study [Multicenter Study]. Am J Gastroenterol. 2001;96(3):751–7.
Di Sabatino A, Carsetti R, Corazza GR. Post-splenectomy and hyposplenic states [Review]. Lancet. 2011;378(9785):86–97.
Ludvigsson JF, Olen O, Bell M, Ekbom A, Montgomery SM. Coeliac disease and risk of sepsis [Multicenter Study Research Support, Non-U.S. Gov’t]. Gut. 2008;57(8):1074–80.
Fouda MA, Khan AA, Sultan MS, Rios LP, McAssey K, Armstrong D. Evaluation and management of skeletal health in celiac disease: position statement. Can J Gastroenterol. 2012;26(11):819–29.
Mora S, Barera G, Beccio S, Menni L, Proverbio MC, Bianchi C, et al. A prospective, longitudinal study of the long-term effect of treatment on bone density in children with celiac disease [Clinical Trial]. J Pediatr. 2001;139(4):516–21.
Sategna-Guidetti C, Grosso SB, Grosso S, Mengozzi G, Aimo G, Zaccaria T, et al. The effects of 1-year gluten withdrawal on bone mass, bone metabolism and nutritional status in newly-diagnosed adult coeliac disease patients [Clinical Trial Research Support, Non-U.S. Gov’t]. Aliment Pharmacol Ther. 2000;14(1):35–43.
Osteoporosis prevention, diagnosis, and therapy [Consensus Development Conference Consensus Development Conference, NIH Review]. JAMA. 2001;285(6):785–95.
Pinkerton JV, Dalkin AC, Crowe SE, Wilson BB, Stelow EB. Treatment of postmenopausal osteoporosis in a patient with celiac disease [Case Reports]. Nat Rev Endocrinol. 2010;6(3):167–71.
Elfstrom P, Granath F, Ekstrom Smedby K, Montgomery SM, Askling J, Ekbom A, et al. Risk of lymphoproliferative malignancy in relation to small intestinal histopathology among patients with celiac disease [Multicenter StudyResearch Support, Non-U.S. Gov’t]. J Natl Cancer Inst. 2011;103(5):436–44.
Ludvigsson JF. Mortality and malignancy in celiac disease [Research Support, Non-U.S. Gov’t]. Gastrointest Endosc Clin N Am. 2012;22(4):705–22.
Catassi C, Fabiani E, Ratsch IM, Coppa GV, Giorgi PL, Pierdomenico R, et al. The coeliac iceberg in Italy. A multicentre antigliadin antibodies screening for coeliac disease in school-age subjects [Clinical Trial Multicenter Study]. Acta Paediatr Suppl. 1996;412:29–35.
Cacciari E, Salardi S, Volta U, Biasco G, Lazzari R, Corazza GR, et al. Can antigliadin antibody detect symptomless coeliac disease in children with short stature? [Comparative Study Research Support, Non-U.S. Gov’t]. Lancet. 1985;1(8444):1469–71.
Bottaro G, Cataldo F, Rotolo N, Spina M, Corazza GR. The clinical pattern of subclinical/silent celiac disease: an analysis on 1026 consecutive cases [Multicenter Study]. Am J Gastroenterol. 1999;94(3):691–6.
Rashid M, Cranney A, Zarkadas M, Graham ID, Switzer C, Case S, et al. Celiac disease: evaluation of the diagnosis and dietary compliance in Canadian children [Research Support, Non-U.S. Gov’t]. Pediatrics. 2005;116(6):e754–9.
Paparo F, Petrone E, Tosco A, Maglio M, Borrelli M, Salvati VM, et al. Clinical, HLA, and small bowel immunohistochemical features of children with positive serum antiendomysium antibodies and architecturally normal small intestinal mucosa [Research Support, Non-U.S. Gov’t]. Am J Gastroenterol. 2005;100(10):2294–8.
Leffler DA, Edwards-George J, Dennis M, Schuppan D, Cook F, Franko DL, et al. Factors that influence adherence to a gluten-free diet in adults with celiac disease [Research Support, N.I.H., Extramural Research Support, Non-U.S. Gov’t]. Dig Dis Sci. 2008;53(6):1573–81.
Fabiani E, Catassi C, Villari A, Gismondi P, Pierdomenico R, Ratsch IM, et al. Dietary compliance in screening-detected coeliac disease adolescents. Acta Paediatr Suppl. 1996;412:65–7.
Biagi F, Bianchi PI, Marchese A, Trotta L, Vattiato C, Balduzzi D, Brusco G, Andrealli A, Cisarò F, Astegiano M, Pellegrino S, Magazzù G, Klersy C, Corazza GR. A score that verifies adherence to a gluten-free diet: a cross-sectional, multicentre validation in real clinical life. Br J Nutr. 2012;108(10):1884–8.
Leffler DA, Dennis M, Edwards George JB, Jamma S, Magge S, Cook EF, et al. A simple validated gluten-free diet adherence survey for adults with celiac disease [Evaluation Studies Research Support, N.I.H., Extramural]. Clin Gastroenterol Hepatol. 2009;7(5):530–6, 6 e1–2.
Rubio-Tapia A. Seguimiento Médico del Paciente Celiaco. In: Rodrigo L, Pena A, editors. Enfermedad Celiaca. Barcelona: OmniaScience; 2012.
Acknowledgments
Supported by American College of Gastroenterology Junior Faculty Development Award (to A.R.T).
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer Science+Business Media New York
About this chapter
Cite this chapter
Herman, M.L., Absah, I., Oxentenko, A.S., Rubio-Tapia, A. (2014). Monitoring and Follow-Up of Patients with Celiac Disease. In: Rampertab, S., Mullin, G. (eds) Celiac Disease. Clinical Gastroenterology. Humana Press, New York, NY. https://doi.org/10.1007/978-1-4614-8560-5_12
Download citation
DOI: https://doi.org/10.1007/978-1-4614-8560-5_12
Published:
Publisher Name: Humana Press, New York, NY
Print ISBN: 978-1-4614-8559-9
Online ISBN: 978-1-4614-8560-5
eBook Packages: MedicineMedicine (R0)