Abstract
The ulnar nerve in children is not commonly injured. The most common causes of trauma to the ulnar nerve in children involve fractures around the elbow and their treatment, namely, supracondylar humerus and medial epicondylar fractures. Knowledge of the ulnar nerve anatomy and issues that can arise during treatment of these fractures can lessen the chance of iatrogenic ulnar nerve injury.
The ulnar nerve can also be subject to compression syndromes in children, primarily at the elbow and less commonly at the wrist. Most often, the cause of nerve compression is not known, but it can be due to fracture malunion or a space-occupying lesion.
Direct trauma to the ulnar nerve can be watched if the nerve is in continuity, or repaired or grafted if the nerve has been severed or ruptured. Innovative surgeries including nerve transfers have been developed, but results have only been reported in adults. Fortunately, ulnar nerve recovery in children tends to have good results, likely due to the greater potential for nerve regeneration in the pediatric population.
Access provided by Autonomous University of Puebla. Download reference work entry PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Introduction
Pediatric peripheral nerve injuries are relatively uncommon. They differ from adult nerve injuries in their potential for greater neural plasticity and quicker axonal regeneration, with rates of axonal regrowth thought to be as quick as 5 mm/day in children. The ulnar nerve in particular is a mixed motor and sensory nerve, with a long distance to travel to its end motor targets in the hand (intrinsic muscles). Hence, ulnar nerve injury in adults has demonstrated less favorable outcomes than those of median or radial nerve injuries. However, due the greater potential for nerve regrowth in children, an otherwise devastating nerve injury may ultimately end up with a good result. Ulnar nerve conditions in children can be largely grouped into compression (direct or due to mass effect) and trauma (fracture or directly to the nerve). Primary nerve tumors are uncommon.
Ulnar Nerve Brief Anatomy
The ulnar nerve arises mainly from the C8 and T1 nerve roots, with a sometimes contribution from C7 nerve root. These roots contribute to the lower trunk and subsequently the medial cord of the brachial plexus. As it courses distally in the upper arm, the ulnar nerve does not usually give off any branches proximal to the antebrachial area, although occasionally a motor branch to the triceps can be seen. The nerve runs accompanied by the superior ulnar collateral branch of the brachial artery and later by the ulnar collateral branch of the radial artery. At the elbow, the ulnar nerve courses posterior to the medial epicondyle. In children, the medial epicondylar ossification center appears at 5–7 years of age and completes its fusion to the distal humerus at 15–20 years of age. The ulnar nerve passes through the cubital tunnel behind the medial epicondyle in the ulnar groove and can give a few branches to the capsule at this level. The ulnar nerve then proceeds to provide its first motor branch to the flexor carpi ulnaris.
In the proximal forearm, the ulnar nerve innervates the flexor digitorum profundus to the ring and small fingers. As it continues distally, approximately 6–8 cm proximal to the ulnar styloid, the dorsal sensory branches from the ulnar nerve proper, which provides sensation to the dorsal ulnar portion of the hand (usually the small finger and the ulnar portion of the ring finger to the proximal interphalangeal joint). The ulnar nerve then passes through Guyon’s canal, where it proceeds to give off a branch to the hypothenar muscle; it then splits into sensory and motor components. The sensory component provides volar sensation to the ulnar side of the ring finger and both sides of the small finger. The motor branch dives deep and courses across the palm in a radial direction to innervate the intrinsic muscles and half of the flexor pollicis brevis (the other half is innervated by the median nerve).
The topography of the ulnar nerve has been studied with respect to ulnar nerve grafting and nerve transfers. Proximally, the sensory and motor fibers intermingle with a considerable amount of fine interplexal connections. As the nerve courses more distally, the sensory and motor portions become more distinct. At the level of the elbow, the motor portion of the ulnar nerve courses more along the volar side, between two sensory portions. This arrangement changes as the nerve runs through Guyon’s canal at the wrist, with the motor portion then becoming more dorsal and radial in location (Brown et al. 2009).
Nerve cross-sectional area has been evaluated and has been found to correlate with increasing age. Cartwright et al. (2013) found on ultrasound of normal subjects that nerve cross-sectional size increased also with body mass index but correlated most closely with age.
Physical Examination
Diagnosis of nerve injuries and specific muscle testing is challenging in children. The child may be agitated or uncomfortable. He or she may be unable to follow commands for sensory and motor testing. Children often do not understand the meaning of tingling and numbness (Hosalkar et al. 2006). These confounding factors can delay accurate diagnosis. It is imperative to assess all major nerves (radial, ulnar, and median) to diagnose motor and sensory deficits. In the older child, two-point discrimination should be tested with the child’s eyes closed. Vibrometry and Semmes-Weinstein monofilament exam can be used to test vibration and pressure thresholds, respectively (Hosalkar et al. 2006). Ulnar nerve sensory loss includes the small finger and ulnar half of the ring finger.
The ulnar deficits will vary according to the level of injury (Fig. 1). High ulnar nerve injures (above the elbow) will negate flexor carpi ulnaris, flexor digitorum superficialis (ring and small), and flexor digitorum profundus function along with all of the ulnar intrinsic muscles within the hand. Low ulnar nerve injuries (at the wrist) will not affect those forearm muscles. Low lesions result in clawing of the ring and small digits as the flexor digitorum profundus provides the deforming force. The classic findings of ulnar nerve injury include the inability to cross fingers and marked loss of dexterity. The classic signs are Froment’s sign (loss of the adductor pollicis and substitution by the flexor pollicis longus) and Wartenberg’s sign (loss of the palmar interosseous and pull of the extensor digit minimi).
Seventeen year-old male that sustained a medial arm laceration involving the ulnar nerve (Courtesy of Shriners Hospital for Children, Philadelphia). (a) Medial arm laceration. (b) Loss of flexor digitorum profundus function. (c) Inability to cross fingers. (d) Positive Froment’s sign. (e) Positive Wartenberg’s sign
Nerve Conduction Studies
Nerve conduction studies are generally of limited use in the young pediatric population, largely due to difficulties with patient compliance and tolerance. In addition, the clinically observed functional improvement may not always correspond to electrical improvement and vice versa. In addition, in order to obtain a good study, sedation is often required, which confounds the interpretation. Thus, the routine use of electrophysiologic studies in children is not universally embraced. Nevertheless, ulnar mononeuropathy is one of the more frequently seen pediatric nerve diagnoses, with the electrophysiologic prognosis being more favorable in nontraumatic causes as compared to traumatic ones (Felice and Royden Jones 1996).
In addition, two particular scenarios in children may cause altered responses with respect to the results of electrophysiologic studies. Firstly, it has been found that prenatal alcohol exposure (>2 oz. absolute alcohol/day) in young children can cause abnormalities in nerve conduction studies, with slower nerve velocities and smaller proximal and distal amplitudes as compared to controls (Avaria Mde et al. 2004). Secondly, it has also been found that nerve conduction results are altered in children with Type I diabetes mellitus. Cenesiz et al. (2003) examined electrophysiologic studies in forty children with Type I diabetes and compared the results to a control group of thirty patients. All nerve conduction values in children with diabetes mellitus were found to be significantly lower as compared to those of the control group, and overall. Sixty percent of diabetic children were found to have some type of peripheral neuropathy.
Ulnar Nerve Subluxation
Ulnar nerve subluxation at the elbow can be a cause of medial elbow pain, mostly in adults. This subluxation finding can be seen in children, although it is usually asymptomatic. Erez et al. (2012) demonstrated in an ultrasound study that 37 % of normal children had subluxating or dislocating ulnar nerves at the elbow. Patients with unstable ulnar nerves tended to be younger (aged 6–10 years) and were more likely to have generalized ligamentous laxity. Waters and colleagues also examined normal pediatric subjects and found a statistical association between young age, ligamentous laxity, and ulnar nerve instability, as well as a strong presence of bilateral ulnar nerve subluxation (Zaltz et al. 1996).
Subluxating ulnar nerves that are symptomatic may need to have treatment similar to that of cubital tunnel syndrome (Fig. 2). Most cases are asymptomatic and are simply associated with young age and ligamentous laxity. This finding can be important when considering pinning of supracondylar humerus fractures. If 10 % of all children have unstable ulnar nerves in flexion, a subluxating or dislocating ulnar nerve could be particularly at risk with a medial pin.
Ulnar Nerve Compression
Cubital Tunnel Syndrome
The ulnar nerve can be subject to compression at several sites along its course. At the elbow, the possible common sites of nerve compression are (from proximal to distal) the arcade of Struthers (an overlying fascial layer), the medial head of the triceps, the medial intermuscular septum, the medial epicondyle itself (especially if there are bony abnormalities), Osborne’s ligament (also sometimes referred to as Osborne’s band or Osborne’s fascia) that overlies the cubital tunnel, and lastly between the heads of the flexor carpi ulnaris muscle. Collectively, compression of the ulnar nerve in any of these potential areas can lead to cubital tunnel syndrome. In addition, flexion of the elbow causes flattening of the cubital tunnel, decreasing its volume and compressing the ulnar nerve.
Cubital tunnel syndrome is rare in the pediatric and adolescent population, though it has been reported in the young, throwing athlete (Godshall and Hansen 1971). In the average pediatric patient presenting with symptoms of cubital tunnel syndrome, Stutz et al. (2012) found in 39 extremities that nonoperative treatment (including nighttime splinting, anti-inflammatory medication, and activity modification) was not uniformly successful, but they still recommended conservative treatment as an initial approach. They did find that patients who underwent surgical release (30 extremities) obtained good relief of symptoms. Most of the time, the etiology of cubital tunnel in the pediatric and adolescent population is idiopathic. In some cases, the cause may be related to a subluxating ulnar nerve. Less common etiologies of compression of the ulnar nerve in the cubital tunnel area include compression by the anconeus epitrochlearis muscle (Fig. 3) (Boero et al. 2009). A single case of cubital tunnel has been reported in a child with Larsen’s syndrome and a dysplastic medial epicondyle (Tubbs et al. 2008).
The surgical options for the treatment of cubital tunnel are similar to adults with no technique demonstrating superior efficacy. Symptomatic subluxation requires anterior transposition (Fig. 4).
Guyon’s Canal Compression
At the wrist, the ulnar nerve can become compressed within Guyon’s canal, which is a fibro-osseous tunnel distal to the wrist flexor retinaculum where the ulnar nerve and artery enter the hand. The roof of Guyon’s canal is composed of the volar carpal ligament and the pisohamate ligament. The cause of ulnar nerve compression within Guyon’s canal can be idiopathic (most common) or due to a space-occupying lesion such as a ganglion or vascular mass (ulnar artery aneurysm). Entrapment of the ulnar nerve at Guyon’s canal in general is also rare in children. It has been reported in a case associated with exuberant scar tissue formation after a laceration over the volar ulnar wrist (Kalaci et al. 2008).
Compression by Mass Lesions
The ulnar nerve can become compressed by a mass anywhere along its course in the upper extremity. Such lesions can arise from the bone, the soft tissue, the vascular system, or the joint. Some of the more commonly seen benign masses in children include ganglion cysts and osteochondromas.
Ganglion Cysts
Ganglion cysts are thought to be outpouchings of the joint lining and are filled with synovial fluid. Most cases associated with ulnar nerve compression have been reported in the adult literature, both at the cubital tunnel/elbow region and in Guyon’s canal. Only one case has been reported in a child, in the Japanese literature, which occurred distally at the wrist (Miwa et al. 1970). Treatment of symptomatic lesions consists of excision of the mass, along with nerve exploration and decompression.
Osteochondromas
Osteochondromas in children can occur either as a singular lesion or multiple lesions (also known as multiple hereditary exostosis). They tend to occur at the physeal region of bones and actively grow until skeletal maturity, after which point the lesions become more quiescent. Lesions that occur about the elbow could have the potential to cause ulnar nerve stretch or compression, but this has not been commonly reported, with only one report in an adult in the Turkish literature (Karakurt et al. 2004). Excision of the lesion is recommended if persistent ulnar nerve symptoms arise, along with exploration and decompression of the nerve.
Other Compressions
The ulnar nerve can be at risk in the upper extremity for compression from such entities as fluid accumulation and swelling. Some of the more unusual cases of ulnar palsy reported in children due to compression include intraneural hemorrhage in a hemophiliac (Cordingly and Crawford 1984) and after intravenous fluid extravasation (Dunn and Wilensky 1984).
In addition, children born with congenital constriction band syndrome have been reported to have ulnar nerve involvement (Uchida and Sugioka 1991; Weeks 1982). An early suspicion for ulnar nerve involvement is recommended, with prompt nerve decompression to maximize the chance for nerve recovery.
Injury
Fractures
Most neuropathies associated with a fracture at the time of injury are likely neuropraxic and can be monitored for recovery; however, the ulnar nerve, due to its relatively superficial location and close association with the ulnohumeral joint, has a particular risk of injury with elbow fractures. Entrapment of the ulnar nerve has been reported in an olecranon fracture (Ertem 2009) and an elbow dislocation (Reed and Reed 2012), and entrapment with laceration of the ulnar nerve has been reported in forearm fractures (Stahl et al. 1997). The following section discusses some of the more common elbow fractures that may result in ulnar nerve injury. Careful observation of the initial fracture pattern and displacement along with a meticulous physical exam, combined with a close assessment of clinical recovery, can aid in decision making regarding potential nerve exploration.
Supracondylar Humerus Fractures
Supracondylar humerus fractures are the most commonly seen elbow fractures in children. Fractures needing surgical intervention are often treated by crossed pinning, but one of the most worrisome possible complications is that of ulnar nerve injury associated with the injury itself, or from fixation of the fracture. Fracture pinning is usually performed with the elbow in the flexed position for fracture reduction, but this maneuver can cause anterior subluxation of the ulnar nerve, especially in young, lax children, which puts the ulnar nerve at direct risk during medial pinning.
One meta-analysis examining neuropraxias associated with supracondylar humerus fractures showed that the overall incidence of ulnar nerve injury with surgical treatment of supracondylar humerus fractures was 6 %. The ulnar nerve was the most frequently damaged nerve, occurring mostly in flexion-type fractures, whereas the anterior interosseous nerve was at higher risk in extension type fractures (Babal et al. 2010). Eberl et al. (2011) found a higher rate of iatrogenic ulnar nerve injury (15 %) in children treated with crossed pins as compared to .4 % in children treated by antegrade nailing. However, pinning is the most common method to surgically treat supracondylar humerus fractures, and much literature has been devoted to determining the safest and most stable pin configuration.
A few meta-analyses of pinning methods have demonstrated greater fracture stability but up to fourfold increased risk of iatrogenic ulnar nerve injury with crossed pins as compared to lateral pins (Woratanarat et al. 2012; Zhao et al. 2013), and another meta-analysis suggested there is an iatrogenic ulnar nerve injury for every 28 patients treated with crossed pinning as compared with lateral pinning (Slobogean et al. 2010). Eberl et al. (2011) also found that medial pinning conferred the highest overall risk of nerve injury, including the ulnar nerve. In patients demonstrating neuropathy associated with supracondylar humerus fractures however, most studies have shown good results in terms of nerve recovery (including median, radial, and ulnar nerves) with observation. Therefore, routine nerve exploration is not recommended particularly if a mini-open approach was used (Ramachandran et al. 2006; Khademolhosseini et al. 2013). In summary, one should be aware of the increased concern for ulnar nerve injury with a flexion-type supracondylar humerus fracture, especially with treatment by medial or crossed pinning, and use of a mini-open incision should be considered to visualize the ulnar nerve.
Medial Epicondylar Fractures
Medial epicondyle fractures are relatively uncommon, accounting for only about 20 % of total pediatric elbow fractures. The mechanism of injury can be by direct trauma, by avulsion, or associated with an elbow dislocation (roughly 60 % of medial epicondylar fractures are associated with an elbow dislocation ). Surgical indications include open fractures, an intra-articular fracture fragment, gross instability, and ulnar nerve entrapment (Fig. 5).
Fifteen year-old right hand-dominant male dislocated right elbow (Courtesy of Shriners Hospital for Children, Philadelphia). (a) X-rays demonstrate posterolateral dislocation with displaced medial epicondyle fracture. (b) Following closed reduction, medial epicondylar fragment appears to be within the ulnohumeral joint. (c) Sagittal CT scan cut infers medial epicondyle within the ulnohumeral joint. (d) Coronal CT scan confirms medial epicondyle within the ulnohumeral joint. In addition, physical examination revealed absent sensation in the ring and small fingers and inability to cross his fingers or contract his first dorsal interosseous muscle. (e) Medial incision with extrication of ulnar nerve traveling into ulnohumeral joint (Courtesy of Shriners Hospital for Children, Philadelphia). (f) AP X-ray after fixation with a cannulated screw
The incidence of ulnar nerve injury, despite a close anatomic association with the area of injury, is relatively low. It has been recommended that the ulnar nerve be protected during fixation, but routine dissection is unnecessary (Gottschalk et al. 2012). However, if the medial epicondylar fragment is small and the injury associated with an elbow dislocation, late ulnar nerve palsy has been reported due to a trapped nerve (Haflah et al. 2010; Lima et al. 2013). Therefore, a high index of suspicion for ulnar nerve entrapment in these cases is warranted. Clinical results in treatment of medial epicondylar fractures overall are good; specifically with respect to the ulnar nerve, Kamath et al. (2009) found in their systematic review no difference in postoperative ulnar nerve symptoms between fractures treated operatively versus nonoperatively, regardless of their preoperative ulnar nerve symptoms.
Tardy Ulnar Palsy
Tardy ulnar palsy can develop after a child incurs an elbow injury associated with bony nonunion, malunion, or simply bony overgrowth with time. Around the elbow, supracondylar humerus fractures as well as medial or lateral condylar fractures can heal and proceed to develop an angular deformity, resulting in cubitus varus or valgus, both of which can be associated with ulnar nerve symptoms (Fig. 6).
Ten year-old boy with left lateral condylar nonunion, progressive valgus, and tardy ulnar nerve palsy (Courtesy of Shriners Hospital for Children, Philadelphia). (a) Photograph demonstrating left elbow cubitus valgus deformity. (b) Anteroposterior X-ray of lateral condylar nonunion. (c) Child positioned prone on operating table and anatomic landmarks drawn on posterior elbow. (d) Fixation of nonunion site with cannulated screws. (e) Dome osteotomy about lateral condylar nonunion site. A second dome was completed to allow lateral translation of the distal fragment. The intervening piece of bone is removed. (f) Medial plate and screw fixation. Note lax ulnar nerve after dome osteotomy. (g) Postoperative X-ray following screw fixation of lateral condylar nonunion and dome osteotomy
Cubitus Valgus
Tardy ulnar palsy associated with posttraumatic cubitus valgus is thought mainly to be due to stretch on the ulnar nerve due to changes in the configuration of the distal humerus in the medial epicondylar region. The normal carrying angle of the elbow is around 11° of valgus, and increasing amounts of valgus can increase stretch on the ulnar nerve as the nerve is relatively tethered in the area of the cubital tunnel. Good results have been reported after surgery by nerve decompression, both with and without associated corrective osteotomy of the distal humerus (Mortazavi et al. 2008; Kang et al. 2013).
Cubitus Varus
The etiology of ulnar neuropathy in cubitus varus is not as straightforward as in cubital valgus. Cubitus varus is thought to cause tardy ulnar palsy not primarily by nerve traction, but secondarily through changes in the elbow anatomy. Kwanishi et al. (2013) studied three-dimensional bone models of patients with cubitus varus and found that the posterior trochlea, distal lateral capitellum, radial head, and ulnar articular surface were all enlarged compared to the normal side. In addition, the ulna was shifted more medially and distally. Some authors have reported muscle impingement on the nerve with a forward shifting of the medial head of the triceps (Ogino et al. 1986; Spinner et al. 1999), whereas others have noted subluxation or instability of the ulnar nerve with compression by fibrous bands of the FCU (Abe et al. 1995; Fujioka et al. 1995; Jeon et al. 2006). In all cases, good results were obtained by treatment with nerve decompression, again with or without corrective osteotomy of the distal humerus.
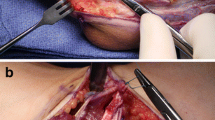
Direct Trauma
Unfortunately, the relatively superficial position of the ulnar nerve at the elbow and wrist puts it at risk during penetrating trauma. Fortunately, as previously mentioned, children have a greater potential for nerve regrowth and more favorable plasticity of the neural circuits than adults that can yield in good (Video 1) results after severe injury. Complete disruption of the ulnar nerve is treated with direct repair if possible or cable grafting for a larger defect (Fig. 7). More recently nerve transfer of the anterior interosseous nerve to the motor branch of the ulnar nerve has been utilized, although the results of nerve transfers have mainly been reported in adults (Video 1). The ulnar nerve can be transposed at the elbow to lessen tension on the repair or grafting site, and the arm can also be immobilized in a position of elbow and wrist flexion to decrease tension on a nerve repair or graft.

Video 1
Baysefer et al. (2004) reported on a series of 21 pediatric ulnar nerve explorations and repair s due to trauma (fracture or laceration) in children and found better results in lesions requiring only neurolysis or decompression as opposed to discontinuous lesions (Fig. 8). This finding is similar to outcomes seen in the adult literature, where neurolysis of intact nerve lesions can usually have good results over 90 % of the time. Chemnitz et al. (2013) reported on long-term outcomes after 45 pediatric ulnar and median nerve repairs in the forearm with an average follow-up of 31 years. In patients less than 12 years of age at the time of repair, 87 % had complete recovery ; in contrast, if the repair was performed between 12 and 20 years of age, only 67 % achieved full recovery. There were no differences in the outcomes between median and ulnar nerves. Overall motor function was close to normal, and cold intolerance was not an issue.
A small series of secondary (delayed) median and ulnar nerve grafting in children with a mean follow-up of 7 years showed results were superior to a comparison group of adults but inferior to those obtained by primary repair (Ceynowa et al. 2012).
Overall, although the ulnar nerve has relatively poorer recovery with repair or reconstruction as compared to the median and radial nerves, largely due to the distal location of its motor targets, children can demonstrate good results especially with younger age at time of injury and an injury in a more distal location.
Ulnar Pediatric Nerve Tumors
Primary nerve tumors in general are not common in the pediatric population. They have on occasion been reported in the ulnar nerve: an ossifying fibrolipomatous hamartoma has been documented in a 5-year-old (Drut 1988), and Cavanagh and Pincott (1977) described a small case series of pediatric ulnar nerve tumors including a neurilemmoma (also known as schwannoma, a tumor which usually arises from a single nerve fascicle) (Fig. 9) and a neurofibroma (a usually more involved nerve and fibrous lesion, which can be solitary or associated with general neurofibromatosis). Both authors described meticulous dissection of the nerve and knowledge of the nerve anatomy, allowing for sparing of intact branches whenever possible.
Summary
The pediatric ulnar nerve may be injured due to trauma, compression, or mass effect. Symptoms may be acute or seen later in life as a sequel of a childhood event. The greater neural plasticity in children affords good results with prompt treatment, even in the setting of nerve disruption. Intimate knowledge of the ulnar nerve anatomy can aid in dissection and repair or reconstruction, thus maximizing the chances for nerve recovery.
References
Abe M, Ishizu T, Shirai H, Okamoto M, Onomura T. Tardy ulnar nerve palsy caused by cubitus varus deformity. J Hand Surg. 1995;20:5–9.
Avaria Mde L, Mills JL, Kleinsteuber K, Aros S, Conley MR, Cox C, et al. Peripheral nerve conduction abnormalities in children exposed to alcohol in utero. J Pediatr. 2004;144:338–43.
Babal JC, Mehlman CT, Klein G. Nerve injuries associated with pediatric supracondylar humeral fractures: a meta-analysis. J Pediatr Orthop. 2010;30:253–63.
Baysefer A, Izci Y, Melih Akay K, Kayali H, Timurkaynak E. Surgical outcomes of ulnar nerve lesions in children. Pediatr Neurosurg. 2004;40:107–11.
Boero S, Senes FM, Catena N. Pediatric cubital tunnel syndrome by anconeus epitrochlearis: a case report. J Shoulder Elbow Surg. 2009;18:e21–3.
Brown JM, Yee A, Mackinnon SE. Distal median to ulnar nerve transfers to restore ulnar motor and sensory function within the hand: technical nuances. Neurosurgery. 2009;65(5):966–77.
Cartwright MS, Mayans DR, Gillson NA, Griffin LP, Walker FO. Nerve cross-sectional area in extremes of age. Muscle Nerve. 2013;6:890–3.
Cavanagh NPC, Pincott JR. Ulnar nerve tumors of the hand in childhood. J Neurol Neurosurg Psychiatry. 1977;40:795–800.
Cenesiz F, Tur BS, Tezic T, Gurer Y. Nerve conduction in children suffering insulin dependent diabetes mellitus. Indian J Pediatr. 2003;70:945–51.
Ceynowa M, Mazurek T, Sikora T. Median and ulnar nerve grafting in children. J Pediatr Orthop B. 2012;21(6):525–8.
Chemnitz A, Bjorkman A, Dahlin LB, Rosen B. Functional outcome thirty years after median and ulnar nerve repair in childhood and adolescence. J Bone Joint Surg. 2013;20:329–37.
Cordingly FT, Crawford GPM. Ulnar nerve palsy in a haemophiliac due to intraneural haemorrhage. Br Med J. 1984;289:18–9.
Drut R. Ossifying fibrolipomatous hamartoma of the ulnar nerve. Pediatr Pathol. 1988;8:179–84.
Dunn D, Wilensky M. Median and ulnar palsies after infiltration of intravenous fluid. South Med J. 1984;77(10):1345.
Eberl R, Eder C, Smolle E, Weinberg AM, Hoellwarth ME, Singer G. Iatrogenic ulnar nerve injury after pin fixation and after antegrade nailing of supracondylar humeral fractures in children. Acta Orthop. 2011;82:606–9.
Erez O, Khalil JG, Legakis JE, Tweedie J, Kaminski E, Reynolds RAK. Ultrasound evaluation of ulnar nerve anatomy in the pediatric population. J Pediatr Orthop. 2012;32:641–6.
Ertem K. An unusual complication of ulnar nerve entrapment in a pediatric olecranon fracture: a case report. J Pediatr Orthop B. 2009;18:135–7.
Felice KJ, Royden Jones Jr H. Pediatric ulnar mononeuropathy: report of 21 electromyography-documented cases and review of the literature. J Child Neurol. 1996;11:116–20.
Fujioka H, Nakabayashi Y, Hirata S, Go G, Nishi S, Mizunoi K. Analysis of tardy ulnar nerve palsy associated with cubitus varus deformity after a supracondylar fracture of the humerus: a report of four cases. J Orthop Trauma. 1995;9:435–40.
Godshall RW, Hansen CA. Traumatic ulnar neuropathy in adolescent baseball pitchers. J Bone Joint Surg. 1971;53A:359–61.
Gottschalk HP, Eisner E, Hosalkar HS. Medial epicondyle fractures in the pediatric population. J Am Acad Orthop Surg. 2012;20:223–32.
Haflah NH, Ibrahim S, Sapuan J, Abdullah S. An elbow dislocation in a child with missed medial epicondyle fracture and late ulnar nerve palsy. J Pediatr Orthop B. 2010;19(5):459–61.
Hosalkar HS, Matzon JL, Chang B. Nerve palsies related to pediatric upper extremity fractures. Hand Clin. 2006;22(1):87–98.
Jeon IH, Oh CW, Kyung HS, Park IH, Kim PT. Tardy ulnar nerve palsy in cubitus varus deformity associated with ulnar nerve dislocation in adults. J Shoulder Elbow Surg. 2006;15:474–8.
Kalaci A, Dogramaci Y, Sevinc TT, Yanat AN. Guyon tunnel syndrome secondary to excessive healing tissue in a child: a case report. J Brachial Plex Peripher Nerve Inj. 2008;28:16.
Kamath AF, Bladwin K, Horneff J, Hosalkar HS. Operative versus non-operative management of pediatric medial epicondyle fractures: a systematic review. J Child Orthop. 2009;3:331–6.
Kang HJ, Koh IH, Jeong YC, Yoon TH, Choi YR. Efficacy of combined osteotomy and ulnar nerve transposition for cubitus valgus with ulnar nerve palsy in adults. Clin Orthop Relat Res. 2013;471:3244–3250 (Epub ahead of print).
Karakurt L, Yilmaz E, Varol T, Ozdemir H, Serin E. Solitary osteochondroma of the elbow causing ulnar nerve compression: a case report. Acta Orthop Traumatol Turc. 2004;38(4):291–4 [Article in Turkish].
Khademolhosseini M, Abd Rashid AH, Ibrahim S. Nerve injuries in supracondylar fractures of the humerus in children: is nerve exploration indicated? J Pediatr Orthop B. 2013;22(2):123–6.
Kwanishi Y, Miyake J, Kataoka T, Omori S, Sugamoto K, Yoshikawa H, Murase T. Does cubitus varus case morphologic and alignment changes in the elbow joint? J Shoulder Elbow Surg. 2013;22:915–23.
Lima S, Correia J, Ribeiro R, Martins R, Alegrete N, Coutinho J, Costa G. A rare cast of elbow dislocation associated with unrecognized fracture of medial epicondyle and delayed ulnar neuropathy in pediatric age. J Shoulder Elbow Surg. 2013;22:e9–11.
Miwa M, Imai H, Saito T. Case of distal ulnar nerve paralysis due to ganglion in a youth. Seikei Geka. 1970;21:957–8 [Article in Japanese].
Mortazavi SM, Heidari P, Asadollahi S, Farzan M. Severe tardy ulnar nerve palsy caused by traumatic cubitus valgus deformity: functional outcome of subcutaneous anterior transposition. J Hand Surg Eur Vol. 2008;33:575–80.
Ogino T, Minami A, Fukuda K. Tardy ulnar nerve palsy caused cubitus varus deformity. J Hand Surg. 1986;11(3):352–6.
Ramachandran M, Birch R, Eastwood DM. Clinical outcome of nerve injuries associated with supracondylar fractures of the humerus in children: the experience of a specialist referral centre. J Bone Joint Surg Br. 2006;88(1):90–4.
Reed MW, Reed DN. Acute ulnar nerve entrapment after closed reduction of a posterior fracture dislocation of the elbow: a case report. Pediatr Emerg Care. 2012;28:570–2.
Slobogean BL, Jacklman H, Tennant S, Slobogean GP, Mulpuri K. Iatrogenic ulnar nerve injury after the surgical treatment of displaced supracondylar fractures of the humerus: number needed to harm, a systematic review. J Pediatr Orthop. 2010;30:430–6.
Spinner RJ, O’Driscoll SW, Davids JR, Goldner RD. Cubitus varus associated with dislocation of both the medial portion of the triceps and the ulnar nerve. J Hand Surg. 1999;24:718–26.
Stahl S, Rozen N, Michaelson M. Ulnar nerve injury following midshaft forearm fractures in children. J Hand Surg (B). 1997;22:788–9.
Stutz CM, Calfee RP, Steffen JA, Goldfarb CA. Surgical and nonsurgical treatment of cubital tunnel syndrome in pediatric and adolescent patients. J Hand Surg. 2012;37:657–62.
Tubbs RS, Oakes WJ, Wellons JC, Grabb PA. Ulnar nerve palsy in a child with Larsen syndrome. J Neurosurg Pediatr. 2008;1:107.
Uchida Y, Sugioka Y. Peripheral nerve palsy associated with congenital constriction band syndrome. J Hand Surg Br. 1991;16:109–12.
Weeks PM. Radial, median and ulnar nerve dysfunction associated with a congenital constricting band of the arm. Plast Reconstr Surg. 1982;69:333–6.
Woratanarat P, Angsanuntsukh C, Rattanasiri S, Sttia J, Woratanarat T, Thankkinstian A. Meta-analysis of pinning in supracondylar fracture of the humerus in children. J Orthop Trauma. 2012;26:48–53.
Zaltz I, Waters PM, Kasser JR. Ulnar nerve instability in children. J Pediatr Orthop. 1996;16:567–9.
Zhao JG, Wang J, Zhang P. Is lateral pin fixation for displaced supracondylar fractures of the humerus better than crossed pins in children? Clin Orthop Relat Res. 2013;471:2942–53.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Electronic supplementary material
Video 1
MOV file: 75591 kB
Rights and permissions
Copyright information
© 2015 Springer Science+Business Media New York
About this entry
Cite this entry
Wang, A. (2015). Ulnar Nerve Injury. In: Abzug, J., Kozin, S., Zlotolow, D. (eds) The Pediatric Upper Extremity. Springer, New York, NY. https://doi.org/10.1007/978-1-4614-8515-5_24
Download citation
DOI: https://doi.org/10.1007/978-1-4614-8515-5_24
Received:
Accepted:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4614-8513-1
Online ISBN: 978-1-4614-8515-5
eBook Packages: MedicineReference Module Medicine