Abstract
Nerve injuries in the pediatric upper extremity offer unique diagnostic challenges. Young patients may not understand the interview questions or be able to adequately express themselves. The physical exam is often limited due to fear, anxiety, or the inability to follow commands. As a result of these obstacles, nerve injuries amenable to repair might be observed for unreasonable amounts of time while the patient is put through repeat and unnecessary diagnostic evaluations. This chapter provides a comprehensive description of gross and microscopic nerve anatomy, an overview of the pathophysiology of nerve injury, how to conduct a physical exam, and how to best utilize electrodiagnostic testing and other imaging modalities such as ultrasound and MRI.
Access provided by Autonomous University of Puebla. Download reference work entry PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Introduction
The location and composition of peripheral nerves are set in utero, and therefore, their anatomic relationships, motor innervation targets, and sensory distribution patterns are similar to those seen in adults. Despite these similarities, nerve injuries in the pediatric upper extremity exhibit unique challenges in ascertaining their diagnosis. A proper history may be difficult to obtain due to communication obstacles as the patient may not understand your questions or be able to adequately express themselves. The physical exam is often limited due to fear, anxiety, or the inability to follow commands. Therefore, to adequately treat the pediatric patient, one must have a thorough understanding of the anatomy, a strong comprehension of the mechanism of injury, an appropriate algorithm of tests, and a high index of suspicion.
Nerve Anatomy
Nerves of the upper extremity originate from ventral nerve roots typically from C5 through T1, which then intermingle to form the brachial plexus in the posterior cervical triangle (Johnson et al. 2010). The brachial plexus can be further broken down into nerve roots, trunks, divisions, and cords from which numerous important nerves originate (Fig. 1). The proximal aspect of the brachial plexus runs between the anterior and middle scalene muscles and courses towards the axilla and under the clavicle. The infraclavicular portion of the plexus, known as the cords, forms the terminal branches making up the major peripheral nerves of the upper extremity.
Peripheral nerves of the upper extremity. A summary view of the brachial plexus organization and the paths of the ulnar, radial, and median nerves. The site of each plane transition, identified as where the nerves pierce through or traverse above or below a given anatomic structure, along the respective nerve’s course is represented (Reprinted from Neurology board review: an illustrated study guide. M Mowzoon, 2007, Rochester, MN: Mayo Clinic Scientific Press. Copyright by Taylor and Francis Group LLC Books. Reprinted with permission. License Id: 3254140720553)
The long thoracic nerve (C5, 6, 7), dorsal scapular nerve (C5), and innervation for the scalene muscles (C5, 6) originate from the nerve roots in the posterior cervical triangle. The long thoracic nerve innervates the serratus anterior, which is responsible for stabilizing the scapula to allow anteversion of the arm. The dorsal scapular nerve pierces the middle scalene and innervates the rhomboid muscles, which stabilize and adduct the scapula. The superior trunk gives rise the subclavius nerve (C5, 6) and the suprascapular nerve (C5, 6). The suprascapular nerve travels with the suprascapular artery and vein before innervating the supraspinatus and infraspinatus muscles which assist with arm abduction and external rotation. The subclavius nerve often travels to the subclavius muscle with the phrenic nerve (Tubbs et al. 2010).
Emerging from the posterior cord are the upper subscapular (C5, 6), thoracodorsal (C5, 6, 7), lower subscapular (C5, 6), axillary (C5, 6), and radial nerves (C5, 6, 7, 8, T1). The thoracodorsal nerve follows the subscapular artery before innervating the latissimus dorsi muscle which produces arm adduction. The axillary nerve passes through the quadrangular space before dividing into an anterior and posterior branch with the anterior branch intimately winding around the surgical neck of the humerus (Fig. 2). The axillary nerve is mostly a motor nerve providing innervation to the deltoid, teres minor, and long head of triceps brachii muscles and therefore influences arm abduction, flexion, extension, and rotation (Tubbs et al. 2010). From the medial cord originate the medial pectoral nerve (C8, T1), medial brachial cutaneous nerve (C8, T1), medial antebrachial cutaneous nerve (C8, T1), a portion of the median nerve (C8, T1) and ulnar nerve (C8, T1). The medial pectoral nerve assists with arm adduction by always innervating the pectoralis minor and frequently the pectoralis major muscles. The medial brachial cutaneous nerve courses along the medial side of the proximal brachial artery and innervates the medial distal third of the arm. The medial antebrachial cutaneous nerve (MAC) also initially runs medial to the brachial artery but transitions to a superficial position in the middle arm as it runs with the basilic vein. In the antecubital fossa the MAC bifurcates to continue its venous relationship with the volar branch anterior to the median basilic vein and the ulnar branch posterior to the median vein. The MAC innervates the volar distal third of the arm and the ulnar half of both volar and dorsal surfaces of the forearm (Tubbs et al. 2010).
Posterior view of the arm. The axillary nerve passes through the quadrangular space and then wraps around the surgical neck of the humerus with the posterior humeral circumflex artery. Note the early strong relationship between the radial nerve and the brachial artery as they enter the arm and travel along the spiral groove of the humerus. The medial and lateral heads of the triceps are resected but can be seen receiving radial innervation (Reprinted with permission from “Anatomy and landmarks for branches of the brachial plexus: a vade mecum,” by S.R. Tubbs et al. 2010, Surgical and Radiologic Anatomy, 32(3), p. 265. Copyright 2010 by Springer-Verlag France. Artist David License Id: 3244201311409)
The lateral pectoral nerve (C5, 6, 7) and musculocutaneous nerve (C5, 6, 7), and the remaining contribution to the median nerve (C5, 6, 7) arise from the lateral cord (Jacobson et al. 2010; Tubbs et al. 2010). The lateral pectoral nerve innervates the pectoralis major muscle also contributing to arm adduction. The musculocutaneous nerve penetrates and innervates the coracobrachialis muscle and then traverses the remainder of the arm radially between the biceps brachii and brachialis muscles, both of which receive innervation. After the motor innervation is exhausted, the nerve becomes the lateral antebrachial cutaneous nerve which runs under the bicipital aponeurosis before bifurcating and innervates the radial half of the volar forearm. The anterior branch of the lateral antebrachial cutaneous nerve terminates at the base of the thumb after traversing anteriorly over the radial artery at the wrist (Tubbs et al. 2010).
The ulnar nerve proceeds down the arm parallel and posterior to the brachial artery close to the humerus until the distal third of the arm where it then turns dorsally away from the artery. The nerve penetrates the medial intermuscular septum and lies against the medial head of the triceps muscle (Jacobson et al. 2010). The ulnar nerve will then pass under the arcade of Struthers, a fibrous band originating from the medial head of the triceps and inserting onto the medial intermuscular septum. The arcade of Struthers is present in approximately 70 % of the population but more likely to be altogether absent in younger pediatric patients (Feinberg et al. 1997). At the elbow the ulnar nerve lies posterior to the medial epicondyle of the humerus and continues under the cubital tunnel retinaculum, a short, thin fibrous band traversing between the medial epicondyle and the olecranon (Fig. 1). The cubital tunnel is immediately distal to the retinaculum with the floor formed by the ulna and the roof by Osborne’s ligament which bridges the two heads of the flexor carpi ulnaris (FCU) (Jacobson et al. 2010). The anconeus epitrochlearis, an established variant present in up to one third of the population, is an accessory muscle proximal to the cubital tunnel that inserts between the medial epicondyle and the olecranon and overlies the ulnar nerve parallel to Osborne’s fascia (Jacobson et al. 2010). In addition to the cubital tunnel itself, the anconeus epitrochlearis may be a source of ulnar nerve compression (Stutz et al. 2012). After exiting the cubital tunnel, the ulnar nerve lies between the FCU and flexor digitorum profundus (FDP) muscle bellies (Figs. 1 and 3). It is here that the nerve innervates the FCU and the ulnar muscle bellies of the FDP controlling the ring and little fingers (Jacobson et al. 2010). At or just proximal to the level of the wrist, two sensory nerves originate: the ulnar palmar cutaneous nerve providing sensation for the hypothenar eminence and the dorsal cutaneous nerve which provides sensation to the ulnar dorsal surface of the hand, the dorsal little finger, and a variable portion of the dorsal ring finger (Engber and Gmeiner 1980; Tagliafico et al. 2012).
Anterior view of the forearm. In the distal arm, the median nerve is ulnar to the brachial artery, and after traversing the elbow, the anterior interosseous nerve is closely associated with the respective artery. In the mid-forearm the ulnar nerve becomes closely associated with the ulnar artery as it travels ulnarly between the flexor digitorum profundus and the flexor carpi ulnaris (cut) (Reprinted with permission from “Anatomy and landmarks for branches of the brachial plexus: a vade mecum,” by S.R. Tubbs et al. 2010, Surgical and Radiologic Anatomy, 32(3), p. 265. Copyright 2010 by Springer-Verlag France. Artist David Fisher. License Id: 3244201311409)
Distally the ulnar nerve joins the ulnar artery and enters Guyon’s canal, a tunnel formed by the pisiform bone, flexor retinaculum, and the palmar carpal ligament. Variably within the canal or shortly after exiting, the nerve either bifurcates or trifurcates into primarily sensory or motor nerves. The deeper motor branch passes under the flexor digiti minimi brevis and abductor digiti minimi to supply the hypothenar muscles, the deep head of flexor pollicis brevis, the adductor pollicis, the dorsal and palmar interossel, and the third and fourth lumbrical muscles (Jacobson et al. 2010; Tagliafico et al. 2012; Tubbs et al. 2010). The superficial sensory portion innervates the palmar surface of the distal ulnar palm and form the proper digital nerves to the little finger and ulnar half of the ring finger (Fig. 1) (Tagliafico et al. 2012).
In the arm the radial nerve travels diagonally in an ulnar to radial direction along the posterior aspect of the humerus in the spiral groove (Jacobson et al. 2010). Proximally the nerve innervates the medial and lateral heads of the triceps brachii muscle and the anconeus muscle, in addition to emitting several sensory nerves to provide sensation to the posterior arm and forearm: the posterior cutaneous nerve, the lower lateral cutaneous nerve, and the posterior cutaneous nerve of the forearm (Figs. 1 and 2). In the distal arm, the radial nerve penetrates the lateral intermuscular septum and courses under the brachioradialis muscle (Jacobson et al. 2010; Tubbs et al. 2010). Here the brachioradialis and extensor carpi radialis brevis and longus muscles receive their innervation (Tagliafico et al. 2012). After passing the elbow joint level at the lateral epicondyle, the radial nerve enters the anterior compartment of the forearm between the brachialis, brachioradialis, and extensor carpi radialis longus muscles before bifurcating into the superficial radial nerve and the deeper posterior interosseous nerve (PIN).
The PIN travels posteriorly through the arcade of Frohse between the two heads of the supinator and then courses in an intramuscular path close to the radius (Jacobson et al. 2010) (Fig. 1). The PIN is responsible for providing the innervation to the entire extensor compartment including the brachioradialis, supinator, extensor digitorum communis, extensor carpi ulnaris, extensor digiti minimi, abductor pollicis longus, abductor pollicis brevis, extensor pollicis longus (EPL), and extensor indicis muscles. While the PIN does not provide any cutaneous innervation, it does provide sensory feedback from the dorsal wrist capsule, through the terminal sensory branch, which travels posterior to the posterior interosseous membrane and anterior to the EPL (Smith et al. 2011; Tubbs et al. 2010).
The superficial branch of the radial nerve briefly follows the radial artery before coursing laterally in proximity to the cephalic vein and then through the anatomic snuffbox. The superficial branch is entirely sensory and innervates the radial aspect of the dorsum of the hand, the dorsum of thumb, index, long, and radial half of the ring fingers proximal to the distal interphalangeal joint (Jacobson et al. 2010; Tagliafico et al. 2012).
The median nerve descends down the arm adjacent to the brachial artery, generally lateral to the artery proximally, and then becomes medial to the artery distally (Fig. 3) (Jacobson et al. 2010). The median nerve traverses the elbow joint level adjacent to the origin of the pronator teres humeral head and then typically goes under this muscle belly, although a less common course is intramuscular through the pronator teres or brachialis muscles (Jacobson et al. 2010). Along the forearm the median nerve courses between the FDP and flexor digitorum superficialis (FDS) (Klauser et al. 2010). The anterior interosseous nerve (AIN) branches off radially after the median nerve crosses the two heads of the pronator teres and enters the FDP muscle belly before continuing on the volar surface of the interosseous membrane in proximity to the interosseous artery (Chin and Meals 2004). The AIN innervates the flexor pollicis longus, FDP of the index and middle fingers, and quadratus muscles. The AIN terminates as sensory innervation for the radiocarpal, midcarpal, and carpometacarpal joints (Chin and Meals 2004). The median nerve proper will innervate the pronator teres, flexor carpi radialis, FDS, and palmaris longus. Alternatively, the FDS may be innervated by the AIN, a reported variant, manifesting in weakness of all proximal interphalangeal joints following an isolated AIN injury (Chin and Meals 2004). Proximal to the carpal tunnel, the median nerve gives off the median palmar cutaneous branch which innervates the thenar eminence and the palmar triangle. At the wrist, the median nerve enters the carpal tunnel, which is formed by the carpus on the floor and the transverse carpal ligament as the roof (Figs. 1 and 3). Within the tunnel the median nerve lies superficial and radial, surrounded by the FPL radially and both FDP and FDS tendons of the index finger dorsally and ulnarly (Klauser et al. 2010). After exiting the carpal tunnel, the median nerve bifurcates into a smaller radial branch and a larger ulnar branch. The radial branch first gives off the recurrent motor branch for the thenar muscles and then trifurcates into three proper palmar digital nerves, two to the thumb and one to the radial side of the index finger. The recurrent motor nerve innervates the opponens pollicis, abductor pollicis brevis, and the superficial head of the flexor pollicis brevis muscles. The proper palmar digital nerves provide innervation to the entire palmar surface of the thumb and radial aspect of the index finger – with the index finger nerve also innervating the first lumbrical. The larger ulnar branch of the median nerve further bifurcates into two common palmar digital nerves, with the first common nerve innervating the second lumbrical and forming the proper digital nerves for the ulnar index finger and radial middle finger. The other common palmar digital nerve innervates the ulnar middle and radial ring fingers after dividing into the respective proper digital nerves. A dorsal branch from each proper digital nerve communicates with the digital nerves of the superficial radial branches to innervate the dorsal distal phalanx of the index, middle, and radial half of the ring fingers (Tagliafico et al. 2012).
It is important to remember that the aforementioned sensory and motor assignments are typical but not the rule as variations are commonplace. One of the more common variants is Martin-Gruber anastomoses, which involve upper forearm communications between the ulnar and median nerves; present in upwards of 17–31 % of the population. These communications are frequently unilateral and typically only carry motor fibers. Their presence can clearly confound the expected presentation of a given nerve injury (Loukas et al. 2011). The specific sensory and motor anatomic variants described in the arm, forearm, and hand are beyond the scope of this chapter, but the surgeon should always suspect their presence when the clinical picture does not conform to the standard expectations.
Brief Review of Microanatomy
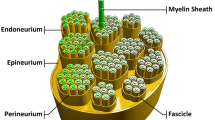
Peripheral nerve structure and its response to injury are important to comprehend as this knowledge will affect the interpretation of diagnostic tests and influence treatment. Each individual axon is covered by a connective tissue matrix called the endoneurium . The axons are then grouped into a fascicle which is enclosed by perineurium. The interfascicular tissue is the internal epineural layer with the peripheral nerve’s outermost sheath being the external epineurium . The perineurium is the source of a nerve’s tensile strength, while the inner epineurial layer provides for some compressive protection. Therefore, nerves with less inner epineurium are most susceptible to compression injury. Blood vessels run longitudinally along both layers of the epineurium and the perineurium (Feinberg et al. 1997; Sunderland 1990).
Peripheral nerves can be either monofascicular or polyfascicular. As a general principle, distally nerves become more polyfascicular with each fascicle corresponding to either a sensory or motor function, particularly near branch points (Kaufman et al. 2009; Sunderland 1990). The specific motor or sensory designations at certain anatomic locations can also be estimated to assist with diagnosis or repair. Within the median nerve prior to AIN branch formation, the motor fibers corresponding to the AIN are posterior (Chin and Meals 2004). After the AIN branch point, the motor fascicles of the median nerve are localized radially. For the ulnar nerve in the mid-forearm, the motor group is centrally located between the outer dorsal and volar sensory fascicles (Kaufman et al. 2009).
Pathophysiology of Nerve Injury
The two most commonly used classifications of nerve injury were developed by Seddon and Sunderland. Neuropraxia , or Sunderland’s first-degree injury, describes an injury of a transient localized conduction block in the absence of structural damage (Burnett and Zager 2004; Sunderland 1990). Axonotmesis , Sunderland’s second-degree injury, occurs with isolated axonal and myelin injury but the endoneurium is left intact. Sunderland’s third- and fourth-degree injuries are progressively more severe forms of axonotmesis, as the injury is now associated with endoneurial damage causing fibrosis and loss of the guiding endoneurial tubes. The complete disruption of the axons, endoneurium, and perineurium across the entire fascicle marks fourth-degree injuries. Neurotmesis , Sunderland’s fifth-degree injury, occurs with complete transection of the entire peripheral nerve including the epineurium. Sunderland’s (modified) sixth-degree injury describes a crush or traction injury resulting in diffuse mixed degrees of nerve injury (which may result in partial regeneration) (Hosalkar et al. 2006; Kaufman et al. 2009; Sunderland 1990).
With all second-degree injuries and greater, Wallerian degeneration occurs in the axon distal to the site of injury. During this process, which begins within several hours of injury, the axons and myelin break down. Schwann cells proliferate and assist the influx of macrophages in phagocytosis of the debris. After 2 weeks, the endoneurial tubes begin to shrink. By 5–8 weeks the endoneurial tubes will be completely empty. In third-degree injuries, there is an even greater inflammatory response due to hemorrhage from the injured blood vessels leading to an influx of fibroblasts and subsequent scar formation. The diameter of the distal endoneurial tubes progressively decreases to a nadir at 3–4 months post-injury, but without a regenerating axon becomes obliterated from progressive fibrosis by increased collagen deposition within the endoneurial sheath over a course of many months (Burnett and Zager 2004; Sunderland and Bradley 1950). In fourth- and fifth-degree injuries, perineurium and epineurium are disrupted which no longer limits the inflammatory response in either the proximal or distal stumps, often preventing the passage of a regenerating axon (Burnett and Zager 2004; Sunderland 1990).
A specialized growth cone arises at the distal tip of the proximally injured axon. Multiple filopodia arise from the growth cone and facilitate the progression of the regenerating nerve through the Schwann cell tunnels (Burnett and Zager 2004). In third-degree injuries and greater, there is an increased likelihood that the growing axon will enter an endoneurial tube different than its original. In mixed nerves, if a sensory axon enters an endoneurial tube of a motor axon, that nerve will fail to mature. While the traditionally stated rate of nerve regeneration is 1 mm per day, the rate is in fact variable as the growth rate decreases with increasing distance from the cell body. The maturation of regenerating nerves comprised of remyelination and progressive increase in axonal diameter occurs at a slower rate than axonal growth. With motor nerves, the muscle itself gradually loses the ability to support functional reinnervation – a process that takes around 18 months (Burnett and Zager 2004; Lee et al. 2004). Upon reinnervation, collateral sprouting occurs resulting in groups of reinnervated muscle fibers typically larger and less organized than pre-injury motor units (Lee et al. 2004; Wilbourn 2002).
While first- and second-degree injuries can likely recover with conservative management, some third-degree and all of the fourth- through sixth-degree injuries require surgical intervention to achieve the best chance of functional recovery (Kaufman et al. 2009). It is the discretion of the surgeon to determine if surgery is indicated after obtaining all pertinent data from the physical exam and diagnostic tests.
Diagnostic Evaluation
Physical Examination
The history and physical exam are often limited in the pediatric patient population. The patient may be nonverbal, uncooperative, or unable to fully comprehend questioning. The inciting injury may have been unwitnessed or the functional deficit may have been insidiously present for a significant amount of time. Pain from other injuries may confound the exam by producing voluntary or involuntary weakness (Feinberg et al. 1997).
Static and moving two-point discrimination are valuable sensory tests in older children though younger children will struggle in interpreting what they are being asked. They may not admit this and will often “guess” the “right answer” (Hosalkar et al. 2006). Intact digital nerves should successfully distinguish moving points 2–5 mm apart at the fingertip and 7–12 mm apart at the palmar base (Kaufman et al. 2009). Vibrometers, which assess large myelinated fibers, and Semmes-Weinstein monofilament instruments, which assess pressure thresholds, are also useful adjuncts, though again successful evaluation of these tools is dependent upon the patient’s age (Hosalkar et al. 2006; Kaufman et al. 2009; Werner and Andary 2002). Indirect measurement of anhidrosis can identify underlying nerve damage. The absence of wrinkled skin after prolonged submersion in water is suggestive of nerve injury but may be less sensitive in the acute setting (Kaufman et al. 2009; Panthaki 2009). Keeping the test as simple as possible may also be a useful tactic, such as limiting the assessment to sharp and dull discrimination and then comparing sensation of the affected digit with a normal digit.
When evaluating sensation, there are three areas that are most consistently innervated by a single nerve: the dorsal first web space for the radial nerve, the palmar distal phalanx of the little finger for the ulnar nerve, and the palmar distal phalanx of the index finger for the median nerve.
Motor exam should initially assess the resting posture and finger cascade followed by assessing passive and active movement from the shoulder to the distal interphalangeal joints. Strength testing is best carried out in an organized systematic approach covering the length of the extremity.
Useful tricks to assess finger abduction or adduction are to have the patient cross their fingers or hold a piece of paper between their fingers. Adjuncts to an exam for young or uncooperative patients can include observation of a patient interacting with a toy or building blocks. Sometimes trying to get the child to reach for keys or a cookie (while restraining the normal limb) can be the only way to illicit activity. Obviously pain and anxiety (including the parents’) can make this a trying exercise for everyone in the room. Repeat exams (on different visits) can be especially helpful in this subset of patients.
In the acute traumatic situation, deep lacerations with any suggestion of nerve injury should be explored, while closed trauma requires a more in-depth assessment as described above.
Electrodiagnostic Testing
Electrodiagnostic evaluation with nerve conduction (NC) studies and electromyography (EMG) can be particularly helpful tests when the history and exam are difficult to interpret. However, an accurate test requires a relaxed patient. A cooperative patient may quickly become uncooperative once the discomfort of this test is realized. A reasonable and often-used approach is to perform the EMG under anesthesia if it cannot be completed without this intervention – though some portions of the test such as active recruitment will be lost. EMG and NC studies can be helpful in localizing a lesion and differentiating between neuropraxic injuries and axonotmetic injuries but cannot otherwise predict which injuries will spontaneously recover and which ones require surgical intervention.
Variables assessed during a motor nerve conduction study include latency, conduction, nerve conduction velocity, and compound muscle action potential (Lee et al. 2004). Latency is the time required to generate a compound muscle action potential in the target muscle after stimulating the nerve. The distal latency is the time needed to stimulate the same muscle from a more distal location on the motor nerve. The conduction time is the difference between the latency and the distal latency and therefore is a direct measurement of conduction along the nerve and independent of factors affecting the motor end plate and subsequent muscle depolarization. Nerve conduction velocity is determined by dividing the conduction by the distance between the proximal and distal stimulation sites. The conduction velocity increases in the presence of myelin and is also directly proportional to the axonal diameter due to the decreasing resistance with increasing axon thickness. The measured nerve conduction velocity will not diminish until a significant number of nerve fibers are affected, as this is a measurement of the fastest intact nerve fibers. The waveform of the compound muscle action potential (also known as an M wave) can yield substantial information. A prolonged duration of the potential indicates slowing of some nerve fibers as slower conduction will induce muscle contraction at a later time. A decreased amplitude indicates incomplete motor nerve conduction, either due to conduction block or axonal loss (Kane and Oware 2012; Lee et al. 2004; Wilbourn 2002). F-waves, variable low-amplitude waves from recurrent discharge of a few motor neurons after a supramaximal stimulus, are either absent or mildly prolonged in severe radiculopathy (Kane and Oware 2012; Lee et al. 2004). Delayed F-waves may be present in demyelination (Kane and Oware 2012).
The EMG is the more invasive portion of electrodiagnostic studies and involves inserting a needle into the muscle belly to measure the intrinsic electrical activity. EMG assesses the electrical activity at rest, the motor unit potential on minimal voluntary contraction, and the recruitment pattern on maximal contraction (if the patient is awake and cooperative). Insertion of the needle will normally cause a small temporary discharge of electrical activity. After the initial insertional activity, there should be minimal or no electrical activity in a normal innervated muscle. Increased spontaneous activity due to hyperexcitable motor end plates is pathologic and typically a consequence of denervation. Fibrillations, positive sharp waves, and fasciculations are commonly present in denervation but are not unique to this condition. Fibrillations are irregular spontaneous contractions of individual muscle fibers, whereas fasciculations are spontaneous contractions of the entire motor unit and are therefore visible and palpable on exam. After approximately 2–3 weeks post-injury, the motor end plates will have undergone enough changes such that fibrillations and positive sharp waves can be detected. Like in NC studies, the shape of the motor unit potential offers further insight into the status of the motor unit. The amplitude represents the number of muscle fibers activated by stimulation of a motor unit, whereas the duration represents recruitment and synchrony of muscle fiber firing (Lee et al. 2004). While acute denervation will result in a short amplitude and short duration, early reinnervation will produce a high-amplitude and long-duration potential due to the surviving nerve fibers branching out to many denervated muscle fibers and increasing their motor unit territory (each axon now innervates more muscle fibers than they did pre-injury) (Burnett and Zager 2004; Lee et al. 2004; Wilbourn 2002).
The timing of performing electrodiagnostic tests in relation to the initial injury is crucial to obtaining an accurate diagnosis due to the temporal changes of nerve and muscle. Neurotmesis and axonotmesis are indistinguishable initially since time is needed to allow for Wallerian degeneration to occur. For instance, it may take up to 10 days for the compound nerve action potential to disappear in the distal nerve segment after a fifth-degree injury, though all degrees of injury will exhibit a “conduction block” immediately. Hyperexcitable changes in the muscle such as fibrillation potentials may not be present for 10 days or more depending on the distance of the injury from the target muscle (Kane and Oware 2012; Lee et al. 2004). Therefore, the initial electrodiagnostic testing should not be performed acutely and should be performed roughly 2 weeks post-injury (Hosalkar et al. 2006).
While providing important and often useful information, the knowledge obtained with serial EMG and NC studies obtained should be weighed against the associated discomfort and risk (if sedation required). The question should be asked, “how will this information potentially change my treatment?” Obviously differentiating neuropraxic injuries bodes an excellent prognosis and diminishes anxiety. However, repeat exams with this diagnosis do not add much to the plan of expectant observation. Likewise, once the diagnosis of axonotmetic injury has been established, the remaining clinical dilemma is whether or not the injury will regenerate on its own or whether surgical intervention will be necessary. Repeat testing should be timed with potential reinnervation. Randomly repeating conduction studies is rarely helpful. If a nerve injury is noted to be 4 in. proximal to a denervated muscle, a new EMG should be delayed until such testing would confirm or challenge the onset of reinnervation of that muscle. Since axon regeneration occurs at approximately 1 in. per month, in this hypothetical scenario, repeat testing would be helpful at 4 months – but not at 3 months.
Nerve Visualizing Modalities: Ultrasound
As the quality and ease of ultrasound imaging improves, this painless and versatile modality becomes a particularly attractive diagnostic tool in evaluating pediatric nerve injuries. When the nerve of interest can be identified, high-frequency transducers provide a greater spatial resolution than magnetic resonance imaging (MRI) and allow for visualization of submillimeter objects such as digital nerves and even, potentially, the nerve macrostructure (Kessler et al. 2012; Kinni et al. 2009; Smith et al. 2011). Outer and inner epineurial layers are hyperechoic, whereas the endoneurium and nerve fascicles are hypoechoic (Fig. 4) (Koenig et al. 2009). This alternating pattern is responsible for the striped appearance in a longitudinal view and honeycombed appearance in a transverse view (Jacobson et al. 2010; Kessler et al. 2012). The echotexture of nerves is often comparable to tendons and can be differentiated from tendons by their immobility during passive movement of joints (Koenig et al. 2009). To readily differentiate peripheral nerves from arteries or veins, which are pulsatile or compressible, respectively, the Doppler mode can be used. Arteries or veins also serve as landmarks to orient the user due to their close association with nerves throughout the majority of the upper extremity.
The depth of sound wave penetration is inversely dependent upon the frequency, with less penetration as the frequency increases. Alternatively, the resolution is directly dependent upon the frequency, with a greater appreciation for detail with increasing frequency. This is why high-frequency transducers in the range of 15–18 MHz should ideally be used to visualize superficially located nerves such as the ulnar nerve at the elbow or the median nerve through the carpal tunnel, but lower-frequency transducers in the range of 9–12 MHz should be used to visualize deep tissue nerves such as the brachial plexus (Koenig et al. 2009).
During the evaluation of a nerve injury, ultrasonography is often able to identify the location of injury and offer important information on nerve integrity. Sonographic characteristics of an entrapped nerve include decreased echogenicity and fusiform thickening of the nerve immediately proximal to the site of compression with distal nerve flattening (Jacobson et al. 2010; Kessler et al. 2012; Kinni et al. 2009; Koenig et al. 2009). To facilitate treatment, ultrasound can frequently establish the source of compression such as ganglia, tumors, accessory muscle bellies, boney callous, fixation screws or plates, and small structural tissue such as the ligament of Struthers as well (Jacobson et al. 2010; Kinni et al. 2009; Koenig et al. 2009). In trauma, nerve laceration versus transection can often be differentiated. In the nonacute setting, the terminal neuroma or the presence of scar encasement of the injured nerve may be identified (Martinoli et al. 2011). Like the use of ultrasound to assess other pathologies, the quality of the information obtained is related to operator experience, depth and size of the structure being investigated, overlying tissue damage and edema, and the patient’s body habitus. Thin, small limbs, as seen in pediatric patients, make pediatrics a particularly appealing patient population for this modality, and it has become a valuable assessment tool, though should not be considered a “crystal ball.”
Nerve Visualizing Modalities: Magnetic Resonance Imaging
MRI is another useful modality to evaluate for nerve injury, particularly in this patient population though, has the disadvantage (compared with ultrasound) that the child must remain perfectly still in an often loud and intimidating environment. MRI can potentially visualize the major nerves of the upper extremity and localize the injury. On both T1- and T2-weighted images, nerves have a similar signal intensity to muscle, but will not enhance with gadolinium-based contrast (Andreisek et al. 2006). Nerves are best visualized by the surrounding circumferential layer of extraneural fat which distinguishes them from the neighboring musculature (Andreisek et al. 2006; Kijowski et al. 2005). Inflammation from chronic nerve compression can cause thickening of the nerve and increased signal intensity (Kijowski et al. 2005). While MRI is typically unable to detect smaller nerves such as the anterior interosseous nerve, it is still sensitive at detecting nerve injuries through changes in the muscle (Kim et al. 2007). In the acute phase, neurogenic muscle edema may be noted (Andreisek et al. 2006). Chronic denervation will demonstrate atrophied muscle with fatty infiltrate (Kijowski et al. 2005). The major obstacle to this modality (also when compared to ultrasound) is the multiplane nature of the nerve paths. The nerve cannot typically be seen in its entirety, although the axial plane is typically the most practical perspective to assess the peripheral nerve (Andreisek et al. 2006). Though loss of continuity can sometimes be visualized, often the tests are indeterminant – especially in areas of complex anatomy such as the brachial plexus.
Summary
Nerve injuries in general have a better prognosis in children than adults, but many surgeons are reluctant to perform “unnecessary” surgery on children. Nerve injuries amendable to repair are often observed for unreasonable amounts of time with the hope of avoiding surgery at all. Repeat and often pointless testing and diagnostic evaluations are offered instead. Indeed, this patient population offers unique challenges to the nerve surgeon trying to adequately assess the risk-benefit ratio of surgical intervention. Injured children are often unable or unwilling to communicate their subjective complaints, demonstrate their objective deficits, or tolerate appropriate testing. The surgeon must compensate for these obstacles with a high index of suspicion, repeat physical examinations, and the judicious use of sometimes painful studies. Increased risks of sedation to obtain further information must be weighed against the risk of early surgical exploration. Ultrasound imaging, and to a lesser extent MRI, may have a greater role in this particular patient population because of this and similar dilemmas especially as the quality of these modalities improves.
References
Andreisek G, Crook DW, Burg D, Marincek B, Weishaupt D. Peripheral neuropathies of the median, radial, and ulnar nerves: MR imaging features. Radiographics. 2006;26(5):1267–87.
Burnett MG, Zager EL. Pathophysiology of peripheral nerve injury: a brief review. Neurosurg Focus. 2004;16(5):E1.
Chin D, Meals R. Anterior interosseous nerve syndrome. Am Soc Surg Hand. 2004;1(4):249–57.
Engber WD, Gmeiner JG. Palmar cutaneous branch of the ulnar nerve. J Hand Surg Am. 1980;5(1):26–9.
Feinberg JH, Nadler SF, Krivickas LS. Peripheral nerve injuries in the athlete. Sports Med. 1997;24(6):385–408.
Hosalkar HS, Matzon JL, Chang B. Nerve palsies related to pediatric upper extremity fractures. Hand Clin. 2006;22(1):87–98.
Jacobson JA, Fessell DP, Lobo Lda G, Yang LJ. Entrapment neuropathies I: upper limb (carpal tunnel excluded). Semin Musculoskelet Radiol. 2010;14(5):473–86.
Johnson EO, Vekris M, Demesticha T, Soucacos PN. Neuroanatomy of the brachial plexus: normal and variant anatomy of its formation. Surg Radiol Anat. 2010;32(3):291–7.
Kane NM, Oware A. Nerve conduction and electromyography studies. J Neurol. 2012;259(7):1502–8.
Kaufman Y, Cole P, Hollier L. Peripheral nerve injuries of the pediatric hand: issues in diagnosis and management. J Craniofac Surg. 2009;20(4):1011–5.
Kessler JM, de la Lama M, Umans HR, Negron J. High-frequency sonography of the volar digital nerves of the hand. Muscle Nerve. 2012;45(2):222–6.
Kijowski R, Tuite M, Sanford M. Magnetic resonance imaging of the elbow. Part II: abnormalities of the ligaments, tendons, and nerves. Skelet Radiol. 2005;34(1):1–18.
Kim S, Choi JY, Huh YM, Song HT, Lee SA, Kim SM, et al. Role of magnetic resonance imaging in entrapment and compressive neuropathy – what, where, and how to see the peripheral nerves on the musculoskeletal magnetic resonance image: part 2. Upper extremity. Eur Radiol. 2007;17(2):509–22.
Kinni V, Craig J, van Holsbeeck M, Ditmars D. Entrapment of the posterior interosseous nerve at the arcade of Frohse with sonographic, magnetic resonance imaging, and intraoperative confirmation. J Ultrasound Med. 2009;28(6):807–12.
Klauser AS, Faschingbauer R, Bauer T, Wick MC, Gabl M, Arora R, et al. Entrapment neuropathies II: carpal tunnel syndrome. Semin Musculoskelet Radiol. 2010;14(5):487–500.
Koenig RW, Pedro MT, Heinen CP, Schmidt T, Richter HP, Antoniadis G, et al. High-resolution ultrasonography in evaluating peripheral nerve entrapment and trauma. Neurosurg Focus. 2009;26(2):E13.
Lee DH, Claussen GC, Oh S. Clinical nerve conduction and needle electromyography studies. J Am Acad Orthop Surg. 2004;12(4):276–87.
Loukas M, Abel N, Tubbs RS, Matusz P, Zurada A, Cohen-Gadol AA. Neural interconnections between the nerves of the upper limb and surgical implications. J Neurosurg. 2011;114(1):225–35.
Martinoli C, Valle M, Malattia C, Beatrice Damasio M, Tagliafico A. Paediatric musculoskeletal US beyond the hip joint. Pediatr Radiol. 2011;41 Suppl 1:S113–24.
Panthaki ZJ. Innovations in innervation; further thoughts on peripheral nerve injuries of the pediatric hand: issues in diagnosis and management. J Craniofac Surg. 2009;20(4):1016–7.
Smith J, Rizzo M, Finnoff JT, Sayeed YA, Michaud J, Martinoli C. Sonographic appearance of the posterior interosseous nerve at the wrist. J Ultrasound Med. 2011;30(9):1233–9.
Stutz CM, Calfee RP, Steffen JA, Goldfarb CA. Surgical and nonsurgical treatment of cubital tunnel syndrome in pediatric and adolescent patients. J Hand Surg [Am]. 2012;37(4):657–62.
Sunderland S. The anatomy and physiology of nerve injury. Muscle Nerve. 1990;13(9):771–84.
Sunderland S, Bradley KC. Endoneurial tube shrinkage in the distal segment of a severed nerve. J Comp Neurol. 1950;93(3):411–20.
Tagliafico A, Cadoni A, Fisci E, Gennaro S, Molfetta L, Perez MM, et al. Nerves of the hand beyond the carpal tunnel. Semin Musculoskelet Radiol. 2012;16(2):129–36.
Tubbs RS, Jones VL, Loukas M, Comert A, Shoja MM, Wellons 3rd JC. Anatomy and landmarks for branches of the brachial plexus: a vade mecum. Surg Radiol Anat. 2010;32(3):261–70.
Werner RA, Andary M. Carpal tunnel syndrome: pathophysiology and clinical neurophysiology. Clin Neurophysiol. 2002;113(9):1373–81.
Wilbourn AJ. Nerve conduction studies. Types, components, abnormalities, and value in localization. Neurol Clin. 2002;20(2):305–38, v.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer Science+Business Media New York
About this entry
Cite this entry
Stromberg, J.A., Isaacs, J. (2015). Nerve Anatomy and Diagnostic Evaluation. In: Abzug, J., Kozin, S., Zlotolow, D. (eds) The Pediatric Upper Extremity. Springer, New York, NY. https://doi.org/10.1007/978-1-4614-8515-5_23
Download citation
DOI: https://doi.org/10.1007/978-1-4614-8515-5_23
Received:
Accepted:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4614-8513-1
Online ISBN: 978-1-4614-8515-5
eBook Packages: MedicineReference Module Medicine