Abstract
Image-guided percutaneous needle biopsy of the spine is a safe and effective technique for obtaining tissue samples from spine lesions. Percutaneous biopsies of the spine are generally performed under fluoroscopic or computed tomography (CT) guidance. Although fluoroscopy provides real-time imaging capability, this technique is limited by its poor visualization of soft tissue. Many interventional radiologists prefer CT’s superior spatial and contrast resolution and ability to delineate adjacent soft-tissue structures, especially for biopsies of cervical spine lesions. A variety of bone biopsy needle systems are commercially available, any of which can be used to obtain specimens from spinal lesions. Different approaches for cervical spinal biopsy include the anterolateral, posterolateral, posterior, transoral, and paramaxillary approaches. Thoracic lesions are usually accessed for biopsy by transpedicular, transcostovertebral, and posterolateral approaches. Common approaches for biopsying lumbar vertebral lesions include transpedicular and posterolateral methods. The diagnostic accuracy of percutaneous biopsy of spinal lesions ranges from 67–100 % according to the needle used, the radiographic appearance of the biopsied lesions, the underlying pathology, and the operator’s experience.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Background
Image-guided percutaneous biopsy of the spine is a safe, accurate, and widely used technique for obtaining tissue samples from spinal or paraspinal lesions. Before the advent of modern imaging modalities, spinal biopsies were performed as open surgical procedures. Since the initial reports in the 1930s demonstrating the feasibility and efficacy of obtaining biopsy specimens from bone lesions using small-caliber needles [1–3], the technique for percutaneous needle biopsy of the spine has evolved considerably. The use of image guidance for needle biopsy of the spine was first reported in 1949 [4]. Initially, percutaneous spinal biopsy was performed with radiographic or fluoroscopic guidance using relatively large-bore needle systems; as a result, these procedures were generally limited to the lower thoracic and lumbar segments of the spine [4]. The use of computed tomography (CT) guidance for spinal biopsy was first reported in the 1980s [5, 6]. Rapid advances in imaging technology, including the clinical introduction of multidetector wide-bore CT along with advances in the design of needle biopsy systems, have enabled image-guided percutaneous biopsy to be used safely today at virtually all levels of the spine. This chapter will review the indications and contraindications for image-guided percutaneous biopsy of the spine; the techniques, devices, and relevant considerations; and outcomes and results documented from the literature.
Indications and Patient Selection
Common indications for percutaneous spinal biopsy include (1) a focal vertebral lesion in a symptomatic or asymptomatic patient, (2) a destructive vertebral lesion in a patient with or without a known primary tumor, (3) clinically or radiologically suspected osteomyelitis/discitis, (4) isolation of an organism in a patient with a diagnosis of osteomyelitis/discitis, (5) a new vertebral bony compression fracture of unknown etiology, and (6) a previously treated vertebral lesion needing evaluation for tumor viability [7].
Contraindications
The only absolute contraindication for spinal biopsy is an uncorrectable coagulation disorder in the patient. Relative contraindications include hypervascular lesions at risk of bleeding into confined spaces (such as epidural or precervical spaces), infected soft tissues in the needle path, uncooperative patient, pregnancy, and severe allergy to any medication required to perform the procedure.
Although certain locations (e.g., the anterior arch of C1 and the dens) previously were considered inaccessible, with the newer imaging modalities there are few, if any, lesions that cannot be successfully and safely biopsied by trained and experienced interventional radiologists.
Technique
Image Guidance
Percutaneous biopsies of the spine are commonly done with fluoroscopic or CT guidance. The choice of imaging modality is based on the preference of the physician, the size and location of the target lesion, the potential access routes, the ability to visualize the lesion, and the availability and cost of the equipment. Some of the advantages associated with fluoroscopic guidance are real-time visualization of needle position in both the anteroposterior and cephalocaudal direction, inexpensive cost, and short procedure times [7–9]. Fluoroscopy, however, requires the use of ionizing radiation and provides poor visualization of soft tissue, which increases the risk of needle damage to major vessels, nerves, and spinal structures, especially in the cervical region. CT imaging precisely delineates the vertebral lesions, any associated soft-tissue components, and the lesion’s relationship to adjacent structures, thus enabling the selection of a safe approach for biopsy [7, 10–12]. CT also helps distinguish necrotic from solid lesions and unequivocally document position of the needle tip. However, CT-guided percutaneous biopsy is limited by the long duration of the procedure and the inability to monitor the needle continuously during insertion and sampling. CT fluoroscopy (CTF) combines the advantages of conventional fluoroscopy with nearly real-time visualization. One of the major concerns about CTF, however, is that it exposes both the patient and the operator to a high level of radiation.
Magnetic resonance imaging (MRI) guidance can also been used for biopsies of spinal lesions. The potential advantages of MRI as a guidance modality for percutaneous biopsy procedures include its high-contrast resolution, multiplanar imaging capacity, ability to visualize vessels without the need to administer a contrast agent, lack of ionizing radiation, and 2- and 3-dimensional imaging capabilities. The superior contrast resolution of MRI may allow visualization of lesions not readily apparent on other imaging modalities.
Sonographic guidance is not routinely used for biopsies of spinal and other skeletal regions because of the inability of the ultrasound beam to penetrate an intact cortex. However, destructive or lytic bony lesions with a break in the overlying cortex and lesions with extraosseous soft-tissue extensions can be visualized with sonography, enabling the biopsy needle to be passed into the lesion under real-time guidance [13–15]. However, patients with sclerotic vertebral or small lytic bone lesions without a cortical break or extraosseous soft-tissue extension are not candidates for a sonographically guided procedure; in these cases, CT or fluoroscopic guidance is necessary.
In a study by Gupta et al., sonographic guidance was found to be particularly useful for cervical spinal biopsies [13, 14]. Real-time sonography allows continuous monitoring of the needle tip and surrounding structures and thus reduces the risk of injury to the many vital structures located in the neck. In addition, cervical lesions involving any part of the vertebra, including the body, transverse process, articular processes, or posterior elements, are accessible to sonographic visualization and hence to sonographically guided fine-needle aspiration biopsy (FNAB). However, in thoracic, lumbar, and sacral regions, the role of sonographically guided FNAB is limited mostly to lesions involving the posterior elements. In rare instances, however, in thin patients, lumbar spinal lesions within the vertebral body and those with paravertebral soft-tissue components can be safely approached from the anterior aspect; with real-time sonographic monitoring, the anteriorly located vessels and other vital structures can be avoided easily [13, 14].
Bone Biopsy Needles
A variety of needle systems for biopsy of bone are commercially available, and any of these is adequate for obtaining biopsy specimens from spinal lesions[7]. Detailed descriptions of all available biopsy systems are beyond the scope of this chapter, but we will describe a few bone-specific biopsy systems to illustrate the general technique for obtaining tissue specimens.
Bone-specific biopsy systems generally use needles with trephine tips, which have a serrated edge for cutting tissue specimens for histologic analysis [6, 16, 17]. Most of the available trephine bone biopsy systems consist of a large-caliber (8- to 16-gauge) outer cannula fitted with an inner stylet or obturator, which is advanced to the proximal edge of the lesion. After removing the stylet, the hollow trephine needle is placed through the cannula and advanced with a clockwise (drilling) motion through the lesion to obtain a core specimen. Most systems come with a metal obturator to push the core sample from inside the trephine needle. Once the outer cannula has been advanced through the cortex, it can also serve as a coaxial guide needle for obtaining FNAB and cutting-needle biopsies using any of the commercially available needles of various calibers. The Craig (10-gauge; Becton Dickinson, Rutherford, NJ) and the Ackerman (12-gauge; Cook Inc., Bloomington, IN) bone biopsy needles have the configuration described above and allow large-core bone biopsies. The Elson bone biopsy set (Cook Inc) is a modification of the Ackerman set that allows initial placement of a thin, 22-gauge, 25-cm needle with removable hub close to the periosteal margin of the vertebra at the selected location. After removing the hub and inner stylet from the 22-gauge needle, a 2-piece biopsy system consisting of an outer 12-gauge cannula with a tapered inner cannula is advanced over the 22-gauge needle to the proximal margin of the lesion. The main advantage of initially introducing the thin needle is that it provides a safe pathway for the larger-caliber needles, and this is especially useful in high-risk areas such as the upper thoracic and cervical spine. This method also facilitates infiltration of local anesthetic into the periosteum at the intended puncture site. The Geremia biopsy system (16-gauge; Cook Inc) is similar to the Elson system and comes with a 40-cm stiffener wire that can be advanced through the 22-gauge, 25-cm introducer needle; this allows sufficient exchange length so that the wire is exposed at all times during coaxial advancement of the biopsy needle [18].
In some biopsy systems, the outer cannula has a sharp beveled edge for cutting through the bone. In these systems, after using the outer cannula for obtaining multiple coaxial biopsies, the outer cannula itself (without the inner stylet) can be advanced into the lesion to obtain a large-core sample. Many of these biopsy systems have T-shaped interlocking handles attached to the inner and outer needles that fit easily into the operator’s hand, allowing increased control during insertion of the needle. The needle is advanced using a manual clockwise rotary (drilling) motion with forward pressure or by tapping on the needle handle with a sterile surgical hammer. The Temno bone biopsy needle system (Bauer Medical Inc, Clearwater, FL) consists of an 8- to 13-gauge outer cannula with a T-shaped handle and a diamond-tip inner stylet. The outer cannula has a sharp beveled tip for cutting through the bone. In the Jamshidi needle system (Manan Medical Products, Northbrook, IL), the 8- to 13-gauge outer cannula has a T-shaped handle and a triple-crown trephine cutting edge, and the inner stylet has a trocar tip. Osteo-Site Bone Access Needle Sets (Cook Inc) are available in 11- and 13-gauge calibers. The outer cannula has a beveled cutting edge and T-shaped handle and is fitted with a diamond-tip inner stylet. The Ostycut bone biopsy needle (CR Bard, Covington, GA) has a threaded outer cannula with a sharp beveled cutting tip and a trocar-point stylet; the needle has the dual advantages of having strength to allow it to be advanced through normal bone or overlying intact cortex to provide access and also having the capability of obtaining a core specimen. The Osteo-Rx needle (Cook Inc) is a modification of the Osteo-Site and consists of a 10-gauge outer cannula and a steerable 13-gauge nitinol needle with a 90° curved tip that allows sampling of multiple locations within the vertebra from a single access site. The Bonopty coaxial bone biopsy system (CR Bard) consists of a 14-gauge cannula and a 15-gauge drill. The eccentrically cutting drill tip is ideally suited for penetrating intact cortical bone.
The choice of a biopsy needle system depends on the availability and cost of the system, the location of the target lesion, the suspected pathology, the integrity of the overlying bone cortex, the internal consistency of the target lesion, the availability of on-site pathology support, and, most important, the experience and familiarity of the operator with the given needle system [7].
Once the outer cannula has been placed in or at the edge of the target lesion, the internal consistency of the lesion determines the choice of needles used to obtain the tissue samples. For lesions that are sclerotic, calcified, ossified, or composed of intact trabeculae infiltrated with tumor cells, large-caliber (15-gauge or larger) stiff bone-cutting needles (such as the trephine needles) are necessary for obtaining core specimens. Once the trephine needle has created a space in the hard lesion, 22-gauge needles can be used to obtain fine-needle aspiration samples. On the other hand, for “soft” bone lesions or soft-tissue mass lesions, use of bone-cutting needles is unlikely to yield tissue. Any of the commercially available FNAB needles and spring-driven slotted cutting needles can be used in such cases to obtain biopsy specimens.
Approaches to Spinal Biopsy and Anatomic Considerations
Cervical Spine
Different approaches for cervical spinal biopsy include the anterolateral, posterolateral, posterior, transoral, and paramaxillary approaches (Fig. 22.1a–c) [19, 20].
Anterolateral Approach
The anterolateral approach allows access to lesions of the mid and lower cervical vertebrae (C4–C7) and discs and to lesions in the prevertebral space [10, 21]. This approach allows easier access to the anterior aspect of the vertebral body and also allows access to the intervertebral disc because it is not hidden by the uncovertebral joint, which is located more posterolaterally. This approach can also be used to access lesions involving the transverse process of the vertebrae as long as the vertebral artery is not in the needle path [22].
For the anterolateral approach, the patient is placed in the supine position with the head turned toward the opposite side, with the neck in extension, and with a pillow or bolster under the shoulders. The needle is inserted anterior to the sternocleidomastoid muscle and is advanced posteromedially between the visceral space and the carotid space (Fig. 22.2) [10, 13, 14, 21]. Care should be taken to avoid the hypopharynx and especially the piriform fossa and esophagus. In some cases, it may be helpful to manually retract the great vessels laterally, especially if the procedure is performed with fluoroscopic guidance [19, 20].
(a, b) Cervical spine. Anterolateral approach. (a) Contrast-enhanced axial magnetic resonance image shows an abnormal area of enhancement (asterisk) in a C4 vertebral body. (b) Computed tomography image during the biopsy procedure shows the biopsy needle (arrow) inserted through the sternocleidomastoid muscle (M) and advanced medial to the carotid artery (A) and jugular vein (V) into the C4 vertebral body
As the needle is pushed posteriorly toward the vertebral body, care should be taken to avoid the vertebral artery. From the subclavian artery, the vessel goes upward toward the foramen in the base of the transverse process of the sixth cervical vertebra and then passes upward through the canal in the transverse processes. Between the foramina, the vertebral artery is located lateral to the mid or posterior part of the vertebral body or disc; care should be taken to avoid the lateral aspect of the vertebral body. Because the needle is directed posteriorly and medially in this approach, theoretically, the spinal canal could be penetrated through the neural foramina, which are directed anterolaterally. However, the use of intermittent CT scans to check the position and trajectory of the needle tip can protect against the penetration of the spinal canal and prevent possible damage to vascular and neural structures. Furthermore, the presence of the carotid sheath tends to keep the needle pointed medially and away from the neural foramen and the vertebral artery [22].
Other important structures that could be in the needle path when this approach is used include the superior and middle thyroid vessels, the superior and inferior laryngeal nerves, the loop of the hypoglossal nerve, and the cervical ganglia of the sympathetic system. However, the small-caliber needles used for the biopsy are unlikely to cause serious damage to the blood vessels or nerves.
Posterolateral Approach
The posterolateral approach is used for sampling lower cervical (C4–C7) vertebral lesions that involve the transverse process, pedicle, articular pillar, or lamina and for sampling lesions in the prevertebral and lateral paraspinal portions of the perivertebral space [7, 19]. This approach can also be used for sampling lateral masses involving C1 and C2.
With the patient in the supine, prone, or lateral decubitus position, the needle is inserted through the sternocleidomastoid muscle and the posterior cervical space and advanced posterior to the carotid sheath (Fig. 22.3). Depending on the vertebral level (mid vs. lower cervical), the patient’s position, and the size and location of the carotid sheath, the needle may be advanced anteromedially or posteromedially. The soft tissues overlying the clavicles and shoulder may interfere with needle placement in the lower neck, particularly in patients with prominent clavicles and short necks. An out-of-plane angled approach with a caudal needle angulation can be used in this situation; the needle is inserted in a plane cranial to the level of the target lesion and advanced caudally and medially (Fig. 22.4).
(a, b) Cervical spine. Posterolateral approach. (a) Computed tomography (CT) scan shows a lytic process (asterisk) involving the C3 vertebral body. (b) CT image during the biopsy procedure shows the biopsy needle (arrow) inserted through the sternocleidomastoid muscle (M) and advanced posterior to the carotid sheath vessels (V) into the C3 lesion (asterisk)
(a, b) Cervical spine. Angled posterolateral approach. (a) Magnetic resonance image shows a hyperintense lesion (arrowheads) involving the right transverse process of the C6 vertebra extending into the prevertebral space. The vertebral artery (arrow) is immediately posterior to the mass. (b) CT scan shows the needle tip (arrow) in the prevertebral portion of the mass (M). The needle was inserted at a more cranial level, directed caudally, and advanced posterior to the internal jugular vein (V) and the common carotid artery (arrow)
With this approach, the vertebral artery is the structure most vulnerable to injury during the biopsy, especially at levels between the transverse foramina, where the vessel is located lateral to the vertebral body and disc. Also, a needle inserted behind the carotid sheath and advanced posteromedially toward a lesion involving the seventh cervical vertebra could potentially injure the vertebral artery. Using contrast medium to identify the vertebral artery can reduce the risk of injury. Because the intervertebral foramina run from the spinal canal in an oblique medial-to-lateral and posterior-to-anterior direction, penetrating the spinal canal with this approach is not possible. Furthermore, a small-caliber needle puncture of the brachial or cervical plexus as it runs between the scalene muscles is not dangerous, although it may cause transient pain. When this approach is used for biopsy of C1 and C2 lesions, care should be taken to identify and avoid the vertebral artery (Fig. 22.5).
Cervical spine. Posterolateral approach. Use of contrast agent to identify and avoid the vertebral artery. (a) Contrast-enhanced computed tomography scan with the patient in a supine position shows a lytic lesion with soft-tissue extension (asterisks) involving the lateral mass of the C1 vertebra. The carotid artery (A) and jugular vein (V) are displaced anteriorly by the mass. Note the posterior location of the vertebral artery (arrowheads). (b) Computed tomography scan shows the coaxial biopsy system with an outer guide needle (arrow) and an inner core biopsy needle (open arrow) advanced posterior to the carotid artery (A) and jugular vein (V) into the mass (asterisk)
Posterior Approach
The posterior approach is used for biopsy of lesions involving the spinous process, lamina, and articular pillars and processes of the cervical vertebrae as well as lesions in the posterior and lateral paraspinal portions of the perivertebral space [22]. This approach also can be used occasionally for sampling lateral masses involving C1 and C2, provided care is taken to identify and avoid the vertebral artery[22].
With the patient in the prone or lateral decubitus position, the needle is advanced through the posterior paraspinal muscles in an anterior direction toward the target lesion (Fig. 22.6). Risk of injury to major vessels or nerves with this approach is extremely low. During biopsy of lesions involving the laminae, care should be taken to ensure that the needle does not penetrate the spinal canal or thecal sac. For sampling lesions involving a lateral mass of C1 using a posterior approach, the needle should be advanced under the lamina, not above it [22]. The vertebral artery, after exiting the C1 foramen, courses posteriorly along the upper surface of the C1 lamina. If necessary, intravenous administration of contrast medium can be used to help identify and avoid the vertebral artery (Fig. 22.7).
Cervical spine. Posterior approach. Use of contrast administration to identify and avoid the vertebral artery. (a) Contrast-enhanced computed tomography scan with the patient in a prone position shows a lytic lesion (arrowheads) involving the body and lateral mass of C2 vertebra. Note the vertebral artery (arrow) encased and narrowed by the lesion. (b) Computed tomography scan shows the biopsy needle (arrow) passing through the anterior portion of the lamina into the lesion posterior to the expected location of the vertebral artery (open arrow)
Transoral Approach
The transoral approach can be used for percutaneous access to lesions involving the anterior portions of the C1 and C2 vertebrae, including the odontoid [19, 22, 23]. The use of this approach requires general anesthesia. An otolaryngologic retractor is placed in order to provide adequate visibility of the oropharyngeal space. The uvula is pushed away with a retractor or a nasal tube. Some operators recommend placement of an inflatable bronchial blocker into the esophagus to prevent antiseptic fluids or blood from entering the stomach. The oral pharynx and cavity is prepared with antiseptic solution. The posterior pharyngeal wall is sprayed and infiltrated with local anesthetic. The needle is inserted through the posterior pharyngeal mucosa and is advanced posteriorly through the retropharyngeal space and prevertebral muscles toward the target lesion (Fig. 22.8). This is a relatively safe approach because no important structure lies between the posterior pharyngeal wall and the bone. Use of antibiotics in this setting is recommended because of the difficulty in maintaining a sterile field with the transoral approach.
Paramaxillary Approach
Although the presence of facial skeleton precludes the use of the standard anterolateral approach for C1 and C2 lesions, a transfacial paramaxillary approach offers safe anterior access to anterior C1 and C2 lesions [22]. The needle is inserted inferior to the zygomatic process of the maxilla and advanced posteriorly through the buccal space between the maxilla and mandible. The needle is advanced through the lateral and medial pterygoid muscles and the parapharyngeal and retropharyngeal spaces for accessing C1 and C2 lesions (Fig. 22.9).
Cervical spine. Paramaxillary approach. (a) Contrast-enhanced computed tomography scan with the patient in a supine position shows a lytic lesion (asterisks) involving the body of C2 vertebra. Note the position of the carotid artery (A), jugular vein (V), and the vertebral artery (VA). (b) Computed tomography scan shows the biopsy needle (arrow) advanced through the masticator, parapharyngeal spaces, and prevertebral muscles into a lytic lesion (asterisks) involving the C2 vertebral body
It is important to avoid the carotid artery; administration of contrast may occasionally be required to visualize this artery. Other structures present in the needle path that could potentially be injured with this approach include the facial artery, internal maxillary artery and its branches, the pterygoid venus plexus, branches of the mandibular and maxillary nerves, and the external carotid artery as it courses laterally deep to the lateral pterygoid muscle. Using a Hawkins-Akins needle (Meditech, Westwood, MA) with a blunt-tip stylet as the outer guiding needle decreases the risk of injury to the vessels and nerves in these spaces [22].
Thoracic Spine
Various approaches can be used for thoracic vertebral biopsies (Fig. 22.10). The vertebral level, the location of the lesion in or adjacent to the vertebral body, and the lesion size are the major determinants to use in selecting an approach. Selection of an approach is also affected by the body habitus and the presence and severity of kyphosis and scoliosis.
Transpedicular Approach
The pedicle provides a short and safe path to the vertebral body [24]. A transpedicular approach is generally used for lesions located within or just anterior to the pedicle (Fig. 22.11). This approach is also the preferred approach for lesions that involve the entire vertebral body.
Thoracic spine. Transpedicular approach. Computed tomography scan with the patient in the prone position shows the guide needle (arrow) and the coaxially inserted core biopsy needle (open arrow) advanced through the right pedicle (P) of the T11 vertebra for biopsy of a lytic lesion (asterisks) located immediately anterior to the pedicle
The transpedicular approach avoids risk of injury to major vessels, the thecal sac and the cord, and the nerve roots [25, 26]. Another advantage of the transpedicular approach is that the needle is perpendicular to the bone cortex at the point of entry. In addition, the cortical bone of the posterior pedicle is typically thin, thus facilitating needle insertion. Since the pedicle is attached to the cranial half of the vertebral body, this approach is generally suitable for lesions involving the upper part of the vertebral body. However, the use of craniocaudal needle angulation with this approach, wherein the needle entering the cranial part of the pedicle is angled caudally, allows access to lesions involving the mid to lower part of the vertebral body (Fig. 22.12).
Thoracic spine. Angled transpedicular approach. (a) Computed tomography scan with the patient in the supine position shows a lytic process (asterisks) involving the T5 vertebral body. Note the lesion is located caudal to the level of the pedicle, precluding a direct transpedicular approach. (b–d) The needle (arrow) was inserted at a level cranial to the lesion and directed caudally through the pedicle (P) into the lesion (asterisk)
The transverse diameter of the thoracic pedicle is smaller than that of the lumbar pedicle, leaving less room for error when placing a large-caliber needle through the pedicle [27, 28]. The transverse diameter of the pedicle is smallest (4.6 mm on average) at the T5 level. Thus, a biopsy needle with an outside diameter of 3 mm might injure the medial walls of the pedicle [25]. The small size of the pedicle also restricts the entry angle of the biopsy needle. Although thoracic pedicles generally will accommodate an 11-gauge needle, smaller gauge needles may be preferable, especially at upper and middle thoracic vertebral levels.
Thoracic transpedicular biopsy can be performed with fluoroscopic or CT guidance. Because of the occasional difficulty in visualizing the small thoracic pedicle with X-ray fluoroscopy, CT guidance is the preferred method.
Costovertebral/Transcostovertebral/Costotransverse Joint Approach
For the transcostovertebral approach, the needle is inserted laterally and advanced anteromedially, passing in between the tubercle of the rib and the corresponding transverse process (Fig. 22.10b) [29]. The needle enters the posterolateral aspect of the vertebral body across the costotransverse ligament (Fig. 22.13). CT guidance is necessary to directly visualize accurate needle positioning between the transverse process and the rib.
Thoracic spine. Costotransverse approach. Computed tomography scan with the patient in the prone position shows the biopsy needle (arrow) advanced in between the left ninth rib (R) and the transverse process (TP) for biopsy of a sclerotic lesion (asterisk) involving the left posterior part of the T9 vertebral body
The needle trajectory is dependent on the orientation and the thickness of the rib and transverse process. With this approach, the bony structures do not leave much room for needle angulation. The head of the rib articulates with the superior costal facet of the corresponding thoracic vertebra, which is located in posterolateral aspect of the upper half of the vertebra immediately caudal to the superior end plate. Thus, this approach allows access to lesions involving the upper part of the vertebral body. This approach allows access to lesions involving posterior or posterolateral parts of the vertebral body on the ipsilateral side (Fig. 22.13) and also to lesions involving the anterior part of the ipsilateral pedicle (Fig. 22.10b). However, lesions involving the ipsilateral anterior or anterolateral portion of the vertebral body cannot be reached with this approach. However, this approach allows access to a much larger area of the vertebral body, including the anterior half, on the side contralateral to the needle insertion (Fig. 22.14). This approach can also be used to access the intervertebral disc one level above the level of the corresponding thoracic vertebra.
Thoracic spine. Costotransverse approach. Computed tomography scan with the patient in the prone position shows the biopsy needle (arrow) advanced in between the left tenth rib (R) and the transverse process (TP) for biopsy of a lytic lesion (asterisk) involving the right anterior part of the T10 vertebral body
With this approach, the bony structures (namely, the transverse process and the rib) keep the biopsy needle away from the lung, pleura, and the exiting nerve roots. The presence of rib anterior to the needle path prevents inadvertent pleural transgression and prevents the needle from sliding forward along the lateral cortex of the vertebral body. The transverse process prevents passage of the needle into the spinal canal. Damage to the costotransverse articulation remains a theoretical possibility with this approach.
Costovertebral Groove Approach
Costovertebral groove approach is a modification of the costotransverse approach. With this approach, the needle is advanced in the groove between the vertebral pedicle (upper portion) and the head of the rib, entering the posterolateral edge of the vertebral body (Fig. 22.10c). This groove/space is located at a level immediately above the level of the transverse process. Because of the absence of transverse process at this level, there is more room for needle angulation than in the costotransverse approach, allowing easy access to larger areas of the vertebral body, including the anterior half of the vertebral body on the ipsilateral side (Fig. 22.15). However, similar to the costotransverse approach, this approach allows access only to lesions involving the upper portion of the vertebral body and the adjoining disc space (Fig. 22.16). When this approach is used with CT guidance, and the needle is advanced in the same axial plane, this allows access only to lesions involving the upper portion of the vertebral body and the adjoining disc space. However, if a craniocaudal angulation is used, this approach can also allow access to lesions in the middle or lower part of the vertebral body. Gantry tilt may be used to align the needle path in one axial plane.
Thoracic spine. Costovertebral groove approach. Computed tomography scan with the patient in the prone position shows the biopsy needle (arrow) advanced in between the head of right eleventh rib (R) and the pedicle (P) for biopsy of a sclerotic lesion (asterisk) involving the ipsilateral anterior part of the T11 vertebral body
Posterolateral Intercostal Approach
The intercostal approach involves needle placement in the posteromedial intercostal space, anterior to the head of the rib and costovertebral joint (Fig. 22.10d). This approach is generally used for biopsy of paravertebral soft-tissue masses or lateral vertebral body masses (Fig. 22.17) [30]. This approach is also used for lesions located in the lower part of the vertebral body, as these lesions cannot be accessed easily by the standard transpedicular or transcostovertebral approaches. Posterolateral approach can also be used for biopsy of lesions located predominantly in the intervertebral disc. Lesions located in the posterior part of the vertebral body, especially posterocentral lesions, are difficult to access with this approach and there is a risk of inadvertent lung puncture as well. However, injection of saline solution into the paravertebral soft tissues can be used to push the pleura and lung forward, allowing safe needle placement. In addition, the needle may cause injury to the intercostal vessels or paraspinal veins, increasing the risk of paraspinal hematoma.
Transforaminodiscal approach
A transforaminodiscal approach that involves accessing the vertebral body through the intervertebral disc above has also been described [31]. The needle is directed from a superior to inferior direction and from a lateral to medial direction to pass through the intervertebral foramen between the targeted vertebra and the superior vertebra. Since the biopsy needle passes through the inferior half of the foramen, there is almost no risk of injuring the nerve root, because the roots course very close to the inferior edge of the upper pedicle and exit in the upper half portion of the foramen. It is important to ensure that the needle trajectory does not cross the medial pedicular line before entering the intervertebral space; this avoids the possibility of penetrating the dural sac. The entire vertebral body, except for the extreme superomedial aspect, can be sampled with this approach. However, this is a complex pathway requiring more images and prebiopsy calculations, lengthening the average total procedure time.
Posterior Approach
A direct posterior approach is used for lesions involving the posterior elements of the thoracic vertebra.
Lumbar Spine
Approaches to lumbar vertebral lesions include transpedicular, posterolateral, lateral, and posterior methods (Fig. 22.18). Selection of a particular approach depends on the location of the lesion within the vertebra.
Transpedicular Approach
The transpedicular approach provides safe passageway to the vertebral body and is used if a lesion is within the pedicle or central vertebral bodies [24–26, 32]. The pedicle selected for the vertebral biopsy depends on the location of the lesion within the vertebra. Transpedicular approach is also the preferred approach for lesions involving the entire vertebral body. Lesions of the intervertebral discs cannot be reached using this route.
Some of the advantages of a transpedicular biopsy include the following: (a) the needle tract is shorter, (b) the acute angle between the transverse process and the mamillary process helps guide the needle tip toward the pedicle, (c) the biopsy needle is perpendicular to the cortex of the bone at the point of entry, and (d) the cortical bone along the posterior aspect of the pedicle is thin and easy to penetrate with the biopsy needle.
For a CT-guided transpedicular approach, the patient is placed in a prone position. The needle entry site is determined by extrapolating the long axis of the pedicle to the skin surface. It is important to anesthetize the subcutaneous soft tissues up to the level of the periosteum. The course of biopsy needle should be along the long axis of the pedicle. Care should be taken to keep the needle away from the cortical bone of the pedicle, especially along the medial and inferior aspect of the pedicle. This is important to prevent the spread of hematoma, infection, or tumor inside the spinal canal.
Biplane fluoroscopy is useful for the transpedicular approach, because it permits simultaneous visualization of the position of the needle in both the frontal and lateral views. The patient is placed in a prone position on the fluoroscopy table and the C-arm is angled along the inclination of the pedicle selected for the biopsy to obtain an end-on view of the center of the pedicle. The needle track is anesthetized using 1 % lidocaine hydrochloride, and the periosteum surrounding the pedicle and the area at the junction of transverse process and superior facet are anesthetized. The biopsy needle is placed on the skin and angulated to obtain an end-on view in the center of the pedicle (the bull’s-eye) on the fluoroscopic image. With the use of a mallet, the guide needle is tapped gently through the pedicle and into the lesion intended for biopsy as determined by fluoroscopy on frontal and lateral views. This is important to ensure that the biopsy needle is in a central position in the pedicle and not near the cortical bone. Puncture of the medial or inferior walls of the pedicle can potentially result in spinal canal damage or nerve root injury.
Modified Transpedicular Approach for Accessing Disc Lesions
A modified transpedicular approach has been described that allows sampling of the intervertebral disc space as well as both vertebral end plates adjacent to the involved disc [33]. This is an exaggerated oblique transpedicular approach similar to that described for vertebroplasty procedures. The traditional transpedicular approach generally places the needle in a horizontal plane, making access to the disc space and adjacent vertebral bodies impossible. In the modified approach, the needle is placed in the caudal part of the pedicle with a caudal-to-cranial angulation; this allows improved access to the intervertebral disc space.
Posterolateral Paravertebral Approach
With the patient in the prone position, the needle is introduced 5–8 cm lateral to the midline and advanced anteromedially (Fig. 22.19) [4]. The needle passes anterior to the transverse process toward the lateral aspect of the vertebral body [11, 34]. Careful attention should be given to avoid the nerve roots, kidney, renal vessels, and large vessels.
This approach is also useful for accessing disc space lesions. This approach is also useful when a lesion is located in the lower part of the vertebral body, as these lesions are difficult to access with the transpedicular approach. However, lesions located in the pedicle or in the posterior part of the vertebral body are difficult to access with this approach.
Lateral Approach
A lateral approach with the patient in lateral decubitus has also been described, allowing access to the vertebral body, disc, and paraspinal soft tissues [35]. Lateral decubitus positioning results in anterior displacement of abdominal viscera, thereby providing a clear view of the lateral aspect of the lumbar spine. The main advantage of this approach is that the needle is generally a safe distance away from the nerve roots, kidneys, renal pedicle, and large vessels.
Posterior Approach
A direct posterior approach is used for lesions involving the posterior elements of the lumbar vertebra.
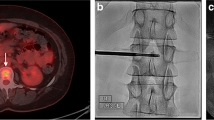
Sacrum
Sacral lesions are generally accessed from a posterior approach (Fig. 22.20). A direct anterior approach may occasionally be used for presacral lesions and lesions involving the anterior body of the sacrum. However, presence of bowel loops, bladder, and other viscera makes this a difficult approach.
Sacrum. Posterior approach. (a) Positron-emission tomography-computed tomography image shows fluorodeoxyglucose (FDG)-avid lesion in the right sacrum (asterisks). (b) Computed tomography scan shows no corresponding abnormality in the sacrum. (c) Magnetic resonance imaging during the biopsy procedure shows the needle (arrow) used to sample the abnormal signal intensity area in the right sacrum (asterisk)
Complications
The incidence of complications after image-guided percutaneous spine biopsy is less than 1–3 % [7, 36]. The risk of potential complications is greater with cervical spine biopsies than for biopsies of the lumbar and thoracic regions because of the proximity to many vital structures surrounding the cervical spine [20, 21].
Pneumothorax is a potential complication that can be seen with biopsy of the lower cervical or thoracic vertebral lesions [37]. Neural injury, particularly of the spinal cord and nerve roots, is a serious complication that can result in foot drop, transient paresis, transient paraplegia, and paraplegia [5, 38]. However, with careful attention in selecting the needle path and the use of image guidance for needle placement, any serious neural injury is rare. Nerve injury can be caused by direct nerve root injury with the biopsy needle or by anesthesia. Paresis or paralysis resulting from anesthetizing major motor nerves generally dissipates within 3–4 h [39].
Bleeding can occur from needle injury to vertebral arteries, paraspinal veins, azygos veins, or, rarely, the aorta, resulting in paraspinal hematomas [40]. Most of the hematomas are small, clinically insignificant, and do not require any treatment [32, 39]. Paravertebral pseudoaneurysm formation has been reported but is extremely rare; this injury can be treated with arterial embolization or percutaneous injection of thrombin [41, 42]. Injury of paravertebral vessels is more common with a paravertebral approach and can be avoided by using a transpedicular approach whenever possible. Biopsy of hypervascular tumors that involve the posterior vertebral body cortex and extend into the central canal can result in bleeding into the canal, causing cord compression.
Other complications that have been reported rarely after percutaneous vertebral biopsy include fracture, vasovagal reaction, puncture of the thecal sac, disc space infection, osteomyelitis, meningitis, epidural hematoma, tumor seeding along the needle tract, and death [7, 25, 26, 36, 43–52].
Use of CT guidance for needle placement for vertebral biopsies has greatly enhanced the safety of the procedure. CT imaging, with its high-contrast and spatial resolution, shows the relationship of the vertebral lesion to adjacent vital structures, allowing the selection of a safe route.
Outcome and Results
The reported accuracy of imaging-guided percutaneous biopsy of vertebral lesions ranges from 67–100 % [7, 25, 26, 36, 43–52]. The diagnostic accuracy of percutaneous vertebral biopsy varies according to the site biopsied, needle used, radiographic appearance of the biopsied lesions, underlying pathology, and operator’s experience.
Sampling errors during percutaneous needle biopsy can lead to false-negative results; therefore, negative results should be viewed with caution. Crushing artifacts and insufficient tissue samples are two major limitations of needle biopsies that can lead to false-negative diagnoses [53]. It is also difficult to obtain sufficient samples in necrotic or cystic lesions [39].
In many patients, the vertebral lesion may be seen only through MRI or positron-emission tomography (PET) imaging, with no radiographically visible changes apparent on CT scans [47]. In these situations, a discrepancy in counting vertebral levels may lead to sampling the wrong vertebra [40]. A false-negative biopsy result in such patients may also result from sampling the wrong part of the involved vertebra because of lack of a visible target.
Another reason for nondiagnostic sampling is biopsy of infectious spondylodiscitis, as tissue specimens generally show nonspecific histologic features. Also, the ability to culture from an infection is generally poor, even more so in patients with fungal discitis [54, 55]. This is especially true if the infection is chronic or if the patient has been treated with broad-spectrum antimicrobials [52]. Improper handling of specimens and failure to perform appropriate microbiologic testing may also result in nondiagnostic sampling [56]. Paravertebral abscesses or fluid obtained from the intervertebral space or vertebral bodies in spondylitis are often sterile. Brugieres et al. [49] described a series of 89 spinal biopsies in which a pathogenic organism was found in 53 % of cases. Michel et al. [55] showed that CT-guided spinal biopsy produced positive bacteriologic examinations in 61 % of patients with spondylitis.
FNAB of vertebral lesions has been shown to have a lower success rate than core biopsy [57]. Core needle biopsy and FNAB are generally considered to be complementary techniques, and combined use of the two techniques can potentially increase the diagnostic yield of vertebral biopsy procedures. In one reported study, the positive predictive value of combined needle aspiration and core biopsy was 82 % and the negative predictive value 100 % [58].
A relationship between the spinal level and the accuracy of biopsy results has been reported in some studies [34, 36, 46]. Nondiagnostic biopsies are more frequently seen with biopsies of cervical and thoracic vertebral lesions than with those at lumbar and sacral levels; this is probably related to the small vertebral body size and technical difficulties associated with achieving percutaneous access to these lesions [34, 36, 46]. The increased accuracy rate with the lower lumbar and sacrum biopsies is likely due to easier access and the absence of vital structures (e.g., spinal cord or major vessels), which allows the use of larger needles and more aggressive sampling of lesions. However, other studies have found no difference in diagnostic accuracy rates based on spinal level [50, 52, 59].
Sclerotic or densely osteoblastic lesions generally have lower diagnostic yields [47]. Brugieres et al. [49] reported higher accuracy rates with osteolytic (94 %) than with osteosclerotic lesions (75 %), whereas Ghelman et al. observed an accuracy rate of 95 % for lytic lesions and 42 % for mixed lesions [34]. Stoker and Kissin also reported lower accuracy rates for sclerotic lesions [50]. The lower diagnostic yield in patients with sclerotic lesions is probably related to the fact that the actual tumor volume that leads to reactive bony sclerosis is very small, and it is impossible to tell which part of the sclerosis represents the tumor. Using large-bore trephine needles, sampling the least-dense portions of the sclerotic lesions, obtaining multiple samples, and sampling different portions of the sclerotic area are some of the methods that can potentially increase the diagnostic yield in such patients.
The histologic type of the target lesion also influences the diagnostic accuracy of image-guided percutaneous biopsy [60]. Diagnostic accuracy rates of metastatic lesions are generally higher than those of primary bone tumors and fractures [59]. Benign bone tumors are associated with a high incidence of false-negative biopsy results [43, 60]. False-negative results are also frequent with biopsies of bone involvement in hematopoietic malignant disorders such as lymphoma. Since these tumors tend to cause diffuse infiltration of bone rather than focal lesions, needle biopsy may not yield sufficient amounts of representative samples. False-negative biopsies in such cases have also been attributed to prolonged decalcification during the histologic preparation of the obtained material, resulting in negative results from immunohistochemical analysis [36].
Summary
Percutaneous needle biopsy of the spine using CT or fluoroscopic guidance is a safe, accurate, and widely used method for establishing the correct pathologic diagnosis in patients presenting with undiagnosed vertebral and paravertebral lesions. Various approaches can be used for spinal biopsies; the choice of approach is generally determined by the vertebral level, the location of the lesion in or adjacent to the vertebral body, and the lesion size.
References
Martin HE, Ellis EB. Biopsy by needle puncture and aspiration. Ann Surg. 1930;92:169–81.
Coley BLSG, Ellis EB. Diagnosis of bone tumors by aspiration. Am J Surg. 1931;13:215–24.
Robertson RCBR. Destructive spine lesions: diagnosis by needle biopsy. J Bone Joint Surg. 1935;17:749.
Siffert RS, Arkin AM. Trephine biopsy of bone with special reference to the lumbar vertebral bodies. J Bone Joint Surg Am. 1949;31A:146–9.
Adapon BD, Legada Jr BD, Lim EV, Silao Jr JV, Dalmacio-Cruz A. CT-guided closed biopsy of the spine. J Comput Assist Tomogr. 1981;5:73–8.
Mick CA, Zinreich J. Percutaneous trephine bone biopsy of the thoracic spine. Spine (Phila Pa 1976). 1985;10:737–40.
Geremia G, Joglekar S. Percutaneous needle biopsy of the spine. Neuroimaging Clin N Am. 2000;10:503–33.
Pierot L, Boulin A. Percutaneous biopsy of the thoracic and lumbar spine: transpedicular approach under fluoroscopic guidance. AJNR Am J Neuroradiol. 1999;20:23–5.
Murphy WA, Destouet JM, Gilula LA. Percutaneous skeletal biopsy 1981: a procedure for radiologists–results, review, and recommendations. Radiology. 1981;139:545–9.
Kattapuram SV, Rosenthal DI. Percutaneous biopsy of the cervical spine using CT guidance. AJR Am J Roentgenol. 1987;149:539–41.
Babu NV, Titus VT, Chittaranjan S, Abraham G, Prem H, Korula RJ. Computed tomographically guided biopsy of the spine. Spine (Phila Pa 1976). 1994;19:2436–42.
Kang M, Gupta S, Khandelwal N, Shankar S, Gulati M, Suri S. CT-guided fine-needle aspiration biopsy of spinal lesions. Acta Radiol. 1999;40:474–8.
Gupta RK, Gupta S, Tandon P, Chhabra DK. Ultrasound-guided needle biopsy of lytic lesions of the cervical spine. J Clin Ultrasound. 1993;21:194–7.
Gupta S, Takhtani D, Gulati M, et al. Sonographically guided fine-needle aspiration biopsy of lytic lesions of the spine: technique and indications. J Clin Ultrasound. 1999;27:123–9.
Civardi G, Livraghi T, Colombo P, Fornari F, Cavanna L, Buscarini L. Lytic bone lesions suspected for metastasis: ultrasonically guided fine-needle aspiration biopsy. J Clin Ultrasound. 1994;22:307–11.
Debnam JW, Staple TW. Trephine bone biopsy by radiologists: results of 73 procedures. Radiology. 1975;116:607–9.
Laredo JD, Bard M. Thoracic spine: percutaneous trephine biopsy. Radiology. 1986;160:485–9.
Geremia GK, Charletta DA, Granato DB, Raju S. Biopsy of vertebral and paravertebral structures with a new coaxial needle system. AJNR Am J Neuroradiol. 1992;13:169–71.
Ottolenghi CE, Schajowicz F, Deschant FA. Aspiration biopsy of the cervical spine. Technique and results in thirty-four cases. J Bone Joint Surg Am. 1964;46:715–33.
Tampieri D, Weill A, Melanson D, Ethier R. Percutaneous aspiration biopsy in cervical spine lytic lesions. Indications and Technique. Neuroradiology. 1991;33:43–7.
Brugieres P, Gaston A, Voisin MC, Ricolfi F, Chakir N. CT-guided percutaneous biopsy of the cervical spine: a series of 12 cases. Neuroradiology. 1992;34:358–60.
Gupta S, Henningsen JA, Wallace MJ, et al. Percutaneous biopsy of head and neck lesions with CT guidance: various approaches and relevant anatomic and technical considerations. Radiographics. 2007;27:371–90.
Patil AA. Transoral stereotactic biopsy of the second cervical vertebral body: case report with technical note. Neurosurgery. 1989;25:999–1001; discussion 1001–1002.
Renfrew DL, Whitten CG, Wiese JA, el-Khoury GY, Harris KG. CT-guided percutaneous transpedicular biopsy of the spine. Radiology. 1991;180:574–6.
Ashizawa R, Ohtsuka K, Kamimura M, Ebara S, Takaoka K. Percutaneous transpedicular biopsy of thoracic and lumbar vertebrae–method and diagnostic validity. Surg Neurol. 1999;52:545–51.
Stringham DR, Hadjipavlou A, Dzioba RB, Lander P. Percutaneous transpedicular biopsy of the spine. Spine (Phila Pa 1976). 1994;19:1985–91.
Zindrick MR, Wiltse LL, Doornik A, et al. Analysis of the morphometric characteristics of the thoracic and lumbar pedicles. Spine (Phila Pa 1976). 1987;12:160–6.
Misenhimer GR, Peek RD, Wiltse LL, Rothman SL, Widell Jr EH. Anatomic analysis of pedicle cortical and cancellous diameter as related to screw size. Spine (Phila Pa 1976). 1989;14:367–72.
Brugieres P, Gaston A, Heran F, Voisin MC, Marsault C. Percutaneous biopsies of the thoracic spine under CT guidance: transcostovertebral approach. J Comput Assist Tomogr. 1990;14:446–8.
Bender CE, Berquist TH, Wold LE. Imaging-assisted percutaneous biopsy of the thoracic spine. Mayo Clin Proc. 1986;61:942–50.
Sucu HK, Bezircioglu H, Cicek C, Ersahin Y. Computerized tomography-guided percutaneous transforaminodiscal biopsy sampling of vertebral body lesions. J Neurosurg. 2003;99:51–5.
Jelinek JS, Kransdorf MJ, Gray R, Aboulafia AJ, Malawer MM. Percutaneous transpedicular biopsy of vertebral body lesions. Spine (Phila Pa 1976). 1996;21:2035–40.
Layton KF, Thielen KR, Wald JT. A modified vertebroplasty approach for spine biopsies. AJNR Am J Neuroradiol. 2006;27:596–7.
Ghelman B, Lospinuso MF, Levine DB, O’Leary PF, Burke SW. Percutaneous computed-tomography-guided biopsy of the thoracic and lumbar spine. Spine (Phila Pa 1976). 1991;16:736–9.
Garces J, Hidalgo G. Lateral access for CT-guided percutaneous biopsy of the lumbar spine. AJR Am J Roentgenol. 2000;174:425–6.
Rimondi E, Staals EL, Errani C, et al. Percutaneous CT-guided biopsy of the spine: results of 430 biopsies. Eur Spine J. 2008;17:975–81.
Metzger CS, Johnson DW, Donaldson 3rd WF. Percutaneous biopsy in the anterior thoracic spine. Spine (Phila Pa 1976). 1993;18:374–8.
McLaughlin RE, Miller WR, Miller CW. Quadriparesis after needle aspiration of the cervical spine. Report of a case. J Bone Joint Surg Am. 1976;58:1167–8.
Kattapuram SV, Rosenthal DI. Percutaneous biopsy of skeletal lesions. AJR Am J Roentgenol. 1991;157:935–42.
Olscamp A, Rollins J, Tao SS, Ebraheim NA. Complications of CT-guided biopsy of the spine and sacrum. Orthopedics. 1997;20:1149–52.
Kulkarni K, Matravers P, Mehta A, Mitchell A. Pseudoaneurysm following vertebral biopsy and treatment with percutaneous thrombin injection. Skeletal Radiol. 2007;36:1195–8.
Stevens KJ, Gregson RH, Kerslake RW. False aneurysm of a lumbar artery following vertebral biopsy. Eur Spine J. 1997;6:205–7.
Dupuy DE, Rosenberg AE, Punyaratabandhu T, Tan MH, Mankin HJ. Accuracy of CT-guided needle biopsy of musculoskeletal neoplasms. AJR Am J Roentgenol. 1998;171:759–62.
Schweitzer ME, Deely DM. Percutaneous biopsy of osteolytic lesions: use of a biopsy gun. Radiology. 1993;189:615–16.
Nourbakhsh A, Grady JJ, Garges KJ. Percutaneous spine biopsy: a meta-analysis. J Bone Joint Surg Am. 2008;90:1722–5.
Kornblum MB, Wesolowski DP, Fischgrund JS, Herkowitz HN. Computed tomography-guided biopsy of the spine. A review of 103 patients. Spine (Phila Pa 1976). 1998;23:81–5.
Lis E, Bilsky MH, Pisinski L, et al. Percutaneous CT-guided biopsy of osseous lesion of the spine in patients with known or suspected malignancy. AJNR Am J Neuroradiol. 2004;25:1583–8.
Donaldson 3rd WF, Johnson DW. Percutaneous biopsy of the thoracic spine. Neurosurg Clin N Am. 1996;7:135–44.
Brugieres P, Revel MP, Dumas JL, Heran F, Voisin MC, Gaston A. CT-guided vertebral biopsy. A report of 89 cases. J Neuroradiol. 1991;18:351–9.
Stoker DJ, Kissin CM. Percutaneous vertebral biopsy: a review of 135 cases. Clin Radiol. 1985;36:569–77.
Akhtar I, Flowers R, Siddiqi A, Heard K, Baliga M. Fine needle aspiration biopsy of vertebral and paravertebral lesions: retrospective study of 124 cases. Acta Cytol. 2006;50:364–71.
Heyer CM, Al-Hadari A, Mueller KM, Stachon A, Nicolas V. Effectiveness of CT-guided percutaneous biopsies of the spine: an analysis of 202 examinations. Acad Radiol. 2008;15:901–11.
Zornoza J. Needle biopsy of metastases. Radiol Clin North Am. 1982;20:569–90.
Laredo JD, Bellaiche L, Hamze B, Naouri JF, Bondeville JM, Tubiana JM. Current status of musculoskeletal interventional radiology. Radiol Clin North Am. 1994;32:377–98.
Michel SC, Pfirrmann CW, Boos N, Hodler J. CT-guided core biopsy of subchondral bone and intervertebral space in suspected spondylodiskitis. AJR Am J Roentgenol. 2006;186:977–80.
Tehranzadeh J, Tao C, Browning CA. Percutaneous needle biopsy of the spine. Acta Radiol. 2007;48:860–8.
Fyfe IS, Henry AP, Mulholland RC. Closed vertebral biopsy. J Bone Joint Surg Br. 1983;65:140–3.
Leffler SG, Chew FS. CT-guided percutaneous biopsy of sclerotic bone lesions: diagnostic yield and accuracy. AJR Am J Roentgenol. 1999;172:1389–92.
Kattapuram SV, Khurana JS, Rosenthal DI. Percutaneous needle biopsy of the spine. Spine (Phila Pa 1976). 1992;17:561–4.
Logan PM, Connell DG, O’Connell JX, Munk PL, Janzen DL. Image-guided percutaneous biopsy of musculoskeletal tumors: an algorithm for selection of specific biopsy techniques. AJR Am J Roentgenol. 1996;166:137–41.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer Science+Business Media New York
About this chapter
Cite this chapter
Gupta, S. (2014). Biopsy of the Spine. In: Ahrar, K., Gupta, S. (eds) Percutaneous Image-Guided Biopsy. Springer, New York, NY. https://doi.org/10.1007/978-1-4614-8217-8_22
Download citation
DOI: https://doi.org/10.1007/978-1-4614-8217-8_22
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4614-8216-1
Online ISBN: 978-1-4614-8217-8
eBook Packages: MedicineMedicine (R0)