Abstract
T-bet is a transcription factor that regulates CD4 Th1 cell differentiation and mice deficient in T-bet fail to develop experimental autoimmune encephalomyelitis, demonstrating its critical role in the generation of immune-mediated demyelinating disease. More importantly, silencing T-bet in a model for multiple sclerosis (MS) demonstrates that it is a viable therapeutic target. T-bet has been found to correlate with disease activity and therapeutic efficacy, suggesting that it may also be a biomarker for MS. Defining the role of T-bet in generating encephalitogenic T cells and their effector functions may provide insight into the mechanisms that underlie the pathology of MS lesions.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Multiple Sclerosis
- Experimental Autoimmune Encephalomyelitis
- Multiple Sclerosis Patient
- Multiple Sclerosis Lesion
- Experimental Autoimmune Encephalomyelitis Induction
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
3.1 Introduction
T-bet was originally cloned and characterized in 2000 by Laurie Glimcher’s laboratory in an effort to dissect the regulatory pathway that ultimately led to the development of Th1 cells (Szabo et al. 2000). Under the hypothesis that the IL2, IFNg, and TNFb genes would all be regulated by a common transcription factor, which would result in Th1 cells, since the expression of these cytokines defines Th1 cells, at least one hybrid system utilizing an IL-2 promoter–reporter construct was used to identify mRNA that was differentially expressed in Th1 cells relative to Th2 cells . Sequence homology to the T box family of transcription factors was the basis for the name T-bet, T box expressed in T cells . T-bet is a 530 amino acid protein encoded by the Tbx21 gene on chromosome 17 in humans and chromosome 11 in mice, and it contains a 189 amino acid T box DNA-binding domain. T-bet was found to directly regulate the expression of IFNγ and repress the expression of Th2 cytokines (Szabo et al. 2000; Finotto et al. 2002; Lovett-Racke et al. 2004; Hwang et al. 2005; Jenner et al. 2009). Since myelin-specific Th1 cells were capable of inducing experimental autoimmune encephalomyelitis (EAE) , a model of multiple sclerosis (MS) , and Th1 cells were found in the central nervous system (CNS) of MS patients, a tremendous amount of research has focused on the role of Th1 cells and associated signaling pathways as a means to understand the pathophysiology of MS (McDonald and Swanborg 1988; Ando et al. 1989; Waldburger et al. 1996; Yura et al. 2001; Lovett-Racke et al. 2004; Gocke et al. 2007; Yang et al. 2009). T-bet, a Th1-associated transcription factor, has been found to be a critical factor in the development of encephalitogenic CD4 T cells in EAE, as well as an effective therapeutic target (Lovett-Racke et al. 2004; Bettelli et al. 2004; Gocke et al. 2007; Yang et al. 2009). Furthermore, T-bet has been identified as a potential biomarker for disease activity and therapeutic efficacy in MS patients (Nath et al. 2004; Frisullo et al. 2006; Peng et al. 2006; Frisullo et al. 2007; Drulovic et al. 2009; Iorio et al. 2009; Kleiter et al. 2010; Frisullo et al. 2011). Thus, T-bet provides insight into the mechanisms by which CD4 T cells mediate CNS lesion development, as well as a potential therapeutic target for the treatment of MS.
3.2 Characterization of the Immune Response in Multiple Sclerosis
MS is an old disease whose pathology was not formally articulated until the nineteenth century when Jean-Marie Charcot described CNS lesions associated with episodic neurological deficits.
On histological sections, multiple sclerosis lesions contain perivascular inflammation and demyelination . Plaques occur anywhere within the white matter of the central nervous system. The most frequently affected sites are optic nerves, brainstem, cerebellum and spinal cord. Lesions in these areas often correlate with clinical systems. In the cerebral hemispheres, periventricular distribution of plaques is often seen. When plaques are adjacent to the cortex, subcortical myelinated nerves are often spared. Plaques located near the gray matter may spread into the gray matter, including deep nuclei and the cortex. Axons are spared within the initial lesions, but are later destroyed (Charcot 1968; translated from French).
Although tremendous research has been done to understand the pathophysiology of MS, Charcot’s initial description is still as accurate a description of the MS lesions as any published since that time. In addition, the components of the lesions as delineated by Charcot, inflammation, demyelination, and axonal destruction, have been the basis of most research on MS. Since inflammation appears to be the predecessor of the demyelination and axonal damage, characterization of the inflammatory response has been a priority in MS research. As our understanding of immunology has evolved over the past decades, our understanding of the inflammatory response in the CNS of MS patients has also evolved, yet the cause of the disease remains unknown and our ability to modify the disease course limited.
3.3 CD4 T Cell Lineages
The hallmark observation that CD4 T cells can express distinct cytokine profiles and play different roles in protective immunity has shed light on the differential role of CD4 T cell lineages in health and disease. The original observation that effector CD4 T cells primarily expressed the signature cytokines IFNγ or IL-4, known as T-helper 1 (Th1) or T-helper 2 (Th2) cells, respectively, prompted interest in how these two lineages develop (Mosmann et al. 1986). T cell receptor (TCR) binding to MHC/peptide complexes (signal 1) and CD28 interaction with CD80 /CD86 (signal 2) are the initial activation signals required for the activation of T cells via antigen-presenting cells (APCs ; Fig. 3.1; June et al. 1990). However, cytokines produced in the microenvironment provide critical signals that determine the lineage commitment of CD4 T cells. If the environment is rich in IFNγ and IL-12 , CD4 T cells differentiate into Th1 cells (Figs. 3.1 and 3.2). All CD4 T cells express the interferon receptor, which when engaged, results in the phosphorylation of the transcription factor STAT1 and translocation to the nucleus (Fig. 3.2a; Afkarian et al. 2002). STAT1 contributes to the expression of T-bet , the master regulator of Th1 cells (Fig. 3.2b–c; Lovett-Racke et al. 2004). There is a positive feedback loop between STAT1 and T-bet that promotes the Th1 phenotype and induces the expression of the IL-12 receptor β2 chain (IL12Rβ2). When the IL12Rβ2 chain pairs with the constitutively expressed IL12Rβ1 chain, this allows IL-12 signaling to occur. IL-12 receptor signaling causes phosphorylation of STAT4 , translocation to the nucleus, and binding to the Ifng gene promoter (Fig. 3.2d; Jacobson et al. 1995). In conjunction with STAT1 and T-bet, STAT4 induces expression of IFNγ and lineage commitment to a Th1 phenotype (Fig. 3.2e). Since Th1 cells express IFNγ and IFNγ initiates the differentiation of Th1 cells, the microenvironment will continue to favor the differentiation of naive CD4 T cells into Th1 cells, and thus an immune response to a particular antigen is typically dominated by a specific CD4 T cell lineage. Similarly, CD4 Th2 cells are generated by IL-4 receptor signaling that causes phosphorylation of STAT6, translocation to the nucleus, and binding to the gata3 gene promoter (Hsieh et al. 1992; Hou et al. 1994; Zheng and Flavell 1997). GATA3 is the master transcriptional regulator of Th2 cells that promotes the expression of IL-4 as well as other Th2-associated cytokines such as IL-5 and IL-13.
Differentiation of CD4 T cells into effector T cells that mediate central nervous system (CNS) demyelination. Naive CD4 T cells engage antigen-presenting cells (APC) to become activated. Both MHC/peptide engagement with the T cell receptor (TCR) and costimulation mediated by CD80/86 (B7.1/B7.2) with CD28 is required to initiate T cells activation. These activated T cells have the capacity to differentiate into different T cell lineages depending on the cytokines in the local environment. IFNγ and IL-12 promote the differentiation of Th1 cells, which are primarily regulated by the transcription factor T-bet, express IFNγ, and can mediate experimental autoimmune encephalomyelitis (EAE). Th2 cells depend on IL-4 activation via the transcription GATA3 and typically are associated with EAE resistance. Th17 cells can be generated in the presence of IL-6 in the presence or absence of TGFβ; however, only Th17 generated in the absence of TGFβ are capable of causing EAE due to the negative regulation of T-bet by TGFβ. CD4 T cells can also develop into a regulatory population that limits the activation and effector functions of other CD4 T cells
Th1 and Th17 cells have the capacity to cause immune-mediated demyelinating disease via signaling pathways dependent on T-bet. Both Th1 and Th17 cells can cause experimental autoimmune encephalomyelitis (EAE) and both populations are present in multiple sclerosis (MS) lesions. (a) Th1 cells differentiate due to the initial signaling via the IFNγ receptor resulting in STAT1 phosphorylation and translocation to the nucleus whereby T-bet and STAT1 regulate each other’s expression in a positive feedback loop and induce expression of the IL-12 receptor β2 chain (b). T-bet regulates STAT1 and IL-23 receptor expression (c). IL-12 receptor signaling can proceed (d), resulting in STAT4 phosphorylation and translocation to the nucleus, which ultimately leads to the activation of the IFNγ gene (e). The IL-23 receptor is upregulated during T cell differentiation (f), at least partially due to T-bet, and this is necessary for critical signals required for acquisition of an encephalitogenic phenotype. (g) IL-6 signaling during T cell activation favors Th17 development via phosphorylation of STAT3, a transcription factor that coordinates with RORγt to regulate IL-17 gene transcription (h). Phosphorylation STAT3 also contributes to the expression of the IL-23 receptor gene, making transcription factors commonly associated with both Th1 and Th17 cells necessary for induction of the IL-23 receptor (i). However, it is unknown what critical function is induced by IL-23 receptor signaling
More recently, a unique population of CD4 T cells known as Th17 cells has been identified as another lineage defined by the expression of IL-17 (Yao et al. 1995). IL-6 appears to be the critical cytokine for the differentiation of naive CD4 T cells into Th17 cells (Veldhoen et al. 2006; Bettelli et al. 2006; Mangan et al. 2006; Acosta-Rodriguiz et al. 2007; Wilson et al. 2007; Yang et al. 2008a, 2008b; Yang et al. 2009; Ghoreschi et al. 2010). IL-6 receptor signaling causes the phosphorylation of STAT3, which in coordination with the transcription factor RORγt induce IL-17 expression (Fig. 3.2g–h). However, other cytokines have been implicated to enhance Th17 commitment in conjunction with IL-6, namely TGFβ in murine T cells (Figs. 3.1 and 3.2g) and TGFβ, IL-1β, and IL-21 in human T cells . Myelin-specific Th1 and Th17 cells are present in mice with EAE and MS patients, and both populations appear to mediate CNS pathology (Traugott and Lebon 1988; McDonald and Swanborg 1988; Ando et al. 1989; Waldburger et al. 1996; Yura et al. 2001; Lock et al. 2002; Lovett-Racke et al. 2004; Gocke et al. 2007; Kroenke and Segal 2007; Tzartos et al. 2008; Yang et al. 2009).
CD4-positive T cells may also develop into a regulatory population that plays a vital role in controlling and dampening of effector T cells to maintain the balance between protection and potential immune-mediated pathology (Kumar et al. 1996; Hori et al. 2003). CD4-regulatory T cells (Tregs) can develop in the thymus or in the periphery. TGFβ signaling is believed to be the critical cytokine signaling required for Treg development, which induces the expression of Foxp3, the transcription factor required for Treg development and function (Fig. 3.1; Marie et al. 2005). These four dominant populations of CD4 T cells provide molecular signals to other cells of the immune system, which coordinate an immune response to protect us from pathogens and cancer. The effectiveness of our immune system is evident in that the vast majority of us live long and healthy lives. However, approximately 5 % of the population suffers from some form of autoimmunity and since autoimmunity is mediated by adaptive immune responses, a tremendous amount of research has focused on the role of CD4 T cells in the onset and progression of autoimmune diseases . Although the pathology of autoimmune diseases may be caused by auto-antibodies or cytotoxic CD8 T cells, CD4 T cells play vital roles in the development of antibodies and CD8 T cells, making CD4 T cells a potential common link among all autoimmune diseases .
3.4 Role of CD4 T Cells in Experimental Autoimmune Encephalomyelitis
EAE has been used as a model for MS research since the 1960s. The model originated from the observation that a small number of individuals who received the rabies virus vaccine, a live-attenuated vaccine grown in the CNS of rabbits, developed encephalomyelitis. Investigation into the cause of the postvaccine encephalomyelitis led to the discovery that the CNS material that contaminated the vaccine could induce a hypersensitivity reaction that resulted in an immune-mediated encephalomyelitis and the onset of symptoms reminiscent of MS (Rivers et al. 1933). EAE is typically induced in rodents by subcutaneous immunization of myelin proteins or peptides emulsified in Complete Freund’s Adjuvant (CFA) . However, adoptive transfer of myelin-specific CD4 Th1 cells into naive recipient mice will also result in EAE development (McDonald and Swanborg 1988; Ando et al. 1989; Waldburger et al. 1996; Yura et al. 2001; Lovett-Racke et al. 2004; Gocke et al. 2007; Yang et al. 2009), supporting the hypothesis that CD4 T cells are the primary mediator of this model autoimmune disease .
Since myelin-specific Th1 cells were sufficient to induce EAE in mice, research on the role of T cells in MS focused on Th1 cells. Several studies that reduced IFNγ in myelin-specific T cells prior to transfer to recipient mice found that changing the signaling pathways, which are necessary for Th1 cell differentiation, diminishes the encephalitogenic capacity of these myelin-specific CD4 T cells (Racke et al. 1994; Racke et al. 1995; Lovett-Racke et al. 2004). Furthermore, mice deficient in STAT4 and T-bet , two transcription factors that play vital roles in the Th1 differentiation pathway, were resistant to EAE induction, supporting the hypothesis that EAE is mediated by Th1 cells (Chitnis et al. 2001; Bettelli et al. 2004; Nath et al. 2006). To determine whether IFNγ was a potential therapeutic target, EAE experiments in mice deficient in IFNγ signaling were performed. Contrary to expectations, mice deficient in IFNγ were susceptible to EAE (Ferber et al. 1996). In addition, systemic treatment of mice with IFNγ-neutralizing antibodies did not suppress EAE (Lublin et al. 1993; Heremans et al. 1996; Willenborg et al. 1996). Together, these studies indicate that IFNγ is not essential for the development of encephalitogenic T cells in mice; however, molecules in the Th1 differentiation pathway are necessary.
The observation that CD4 Th1 cells were sufficient to cause EAE, yet IFNγ was dispensable, prompted the investigation of other cytokines in the development and function of encephalitogenic T cells . Since IL-12 was a key cytokine necessary for Th1 cell differentiation, the components of IL-12 and the IL-12 receptor were analyzed using mice genetically deficient in each subunit of the IL-12 cytokine and receptor. IL-12 is a heterodimer composed of a p40 and p35 subunit. Mice deficient in the IL-12p40 were resistant to EAE, yet mice deficient in IL-12p35 remained susceptible to EAE (Becher et al. 2002; Gran et al. 2002). Since IL-12p40 was also a component of IL-23 (Oppmann et al. 2000), EAE was evaluated in mice deficient in the IL-23-specific subunit, p19. IL-23p19-deficient mice were protected from EAE induction, similar to the IL-12p40-deficient mice, indicating that IL-23 signaling was necessary for EAE development (Cua et al. 2003). Culturing of myelin-specific T cells isolated from immunized mice with IL-23 promoted the expansion of myelin-specific IL-17-producing T cells (Langrish et al. 2005). In addition, transfer of these IL-23-expanded T cells into naive mice resulted in EAE, leading to speculation that Th17 cells were actually the primary encephalitogenic CD4 T cell population in EAE and perhaps MS. However, mice deficient in IL-17 remained susceptible to EAE, although the disease may be less severe, suggesting that IL-17 is also not necessary for the development of encephalitogenic T cells (Komiyama et al. 2006; Haak et al. 2009). These data indicate that IL-23, an APC-produced cytokine, is necessary for the development of encephalitogenic T cells . Yet, IFNγ and IL-17, the cytokines that define Th1 and Th17 cells, are not essential.
So what molecules expressed by myelin-specific CD4 effector T cells are required for encephalitogenicity? Use of genetic knock-out mice has shown that GM-CSF (Ponomarev et al. 2007; Codarri et al. 2011; El-Behi et al. 2011), STAT4 (Chitnis et al. 2001), and T-bet (Bettelli et al. 2004; Nath et al. 2006) are required for T cell encephalitogenicity. GM-CSF , a cytokine expressed by numerous cell types including macrophages , endothelial cells, and fibroblasts, is expressed by both Th1 and Th17 cells. However, STAT4 and T-bet are transcription factors that are typically associated with Th1 cells, making it unclear why deletion of these genes would result in EAE resistance if Th17 cells are sufficient to induce EAE. Suppression of T-bet with an siRNA in mice found that not only was EAE inhibited, but both Th1 and Th17 cells failed to differentiate indicating that T-bet was affecting both encephalitogenic T cell populations (Gocke et al. 2007; Yang et al. 2009). Thus, the contribution of T-bet in regulating genes in encephalitogenic T cells must extend beyond IFNγ and Th1-associated genes.
3.5 Role of T-bet in Regulating Gene Expression in CD4 T Cells
T-bet was originally described as the “master” regulator of Th1 cell differentiation because it directly regulates the expression of the IFNγ in CD4 T cells (Szabo et al. 2000). In naive CD4 T cells, the Ifng gene is epigenetically repressed by histone 3 lysine 4 trimethylation (H3K27me3; Fig. 3.3). Upon T cell activation and differentiation into a Th1 phenotype, T-bet physically associates with the Ifng promoter. This causes recruitment of H3K27 demethylase complexes to the Ifng loci to reverse the epigenetically repressed state (Lewis et al. 2007; Miller et al. 2008). T-bet subsequently recruits a permissive H3K4 methyl transferase to establish a permissive epigenetic state via H3K4me2, resulting in chromatin remodeling which allows T-bet and STAT4 to bind to the Ifng promoter. Typically within 3 days of activation, a naive CD4 T cell will express IFNγ and commit to a Th1 lineage. However, T-bet also plays a repressive role in Th1 cells by recruiting Bcl-6 to the Ifng loci late in Th1 cell differentiation (Oestreich et al. 2011). This results in reducing IFNγ production and return to a resting state of Th1 cells, probably to limit the effector function of Th1 cells, minimize tissue damage, and reduce the potential for autoimmunity.
T-bet is the critical transcription factor for the regulation of the IFNγ gene. a IFNγ gene is epigenetically repressed via H3K27me3 in naive CD4 T cells. b IFNγ and IL-12 receptor signaling induces T-bet, which recruits H3K27 demethylase complexes to the Ifng loci to reverse the epigenetically repressed state. c T-bet recruits a permissive H3K4 methyl transferase to establish a permissive epigenetic state via H3K4me2. d Chromatin remodeling allows Th1-associated transcription factors to bind and promote IFNγ production and the Th1 phenotype. e T-bet recruits the transcriptional repressor Bcl-6 to the Ifng loci late in Th1 cell differentiation to limit IFNγ production and return Th1 cells to a resting state
T-bet-deficient mice are resistant to EAE development (Bettelli et al. 2004; Lovett-Racke et al. 2004; Nath et al. 2006), while IFNγ-deficient mice remain susceptible to EAE (Ferber et al. 1996). This suggests that T-bet must regulate genes other than Ifng that are necessary for EAE development. Since it had been shown that suppressing T-bet not only reduced Th1 cells but also Th17 cells in mice with EAE, T-bet may be regulating gene(s) common to both Th1 and Th17 cells (Gocke et al. 2007; Yang et al. 2009). Using chromatin immunoprecipitation assays, as well as overexpression of T-bet in cell lines, T-bet was found to positively regulate the expression of the Il23r gene (Gocke et al. 2007). It had previously been observed that IL-23 and IL-23 receptor-deficient mice were resistant to EAE suggesting that IL-23 receptor signaling is a vital component of EAE regardless of whether it is mediated by Th1 or Th17 cells (Zhang et al. 2003; Cua et al. 2003). Prior to the discovery of Th17 cells, it had been shown that IL-23 receptor was expressed on activated T cells that were largely of a Th1 phenotype (Oppmann et al. 2000; Parham et al. 2002), so it is feasible that IL-23 may affect both Th1 and Th17 cells. In addition, IL-23 had been shown to promote the expansion of encephalitogenic Th17 cells (Langrish et al. 2005), while neutralizing IL-23 can ameliorate EAE (Chen et al. 2006). It was also shown that IL-23 produced by microglia and CNS-infiltrating macrophages was necessary for the onset of EAE, indicating that myelin-specific T cells required IL-23 receptor expression to mediate demyelination in the CNS (Becher et al. 2003). Using primary microglia cultures, it was found that IFNγ enhanced IL-23 expression, supporting the hypothesis that CNS-infiltrating Th1 cells may contribute to expansion of Th17 cells in the CNS via their production of IFNγ . Similarly, Th17 cells are found in the CNS of mice with EAE induced by adoptive transfer of myelin-specific Th1 cells (Gocke et al. 2007; Lees et al. 2008). Thus, T-bet appears to be critical for EAE due to its role in upregulating the expression of the IL-23 receptor during T cell activation and differentiation.
It had been shown that CD4 T cell lineage commitment is determined by the interaction of T-bet and GATA-3 . T-bet represses Th2 cell differentiation by a tyrosine kinase-mediated interaction with GATA-3 (Hwang et al. 2005). Since encephalitogenic CD4 T cells could be both Th1 and Th17 , this led to the intriguing question as to what was the role of T-bet in encephalitogenic Th17 cells, beyond IL-23 receptor expression. As previously mentioned, silencing T-bet in wild-type mice with EAE results in fewer Th17 cells. However, induction of EAE in T-bet-deficient mice results in a significant population of myelin-specific Th17 cells, yet these T-bet- deficient mice fail to develop EAE (Yang et al. 2009). This suggests that T-bet is critical in the development of encephalitogenic Th17 cells, but not in the development of CD4 T cells that are capable of expressing IL-17. Several studies showed that naive murine T cells could be differentiated into Th17 cells with IL-6 and TGFβ (Fig. 3.1; Veldhoen et al. 2006; Bettelli et al. 2006; Mangan et al. 2006). However, these differentiation conditions failed to generate Th17 cells that could induce EAE when transferred into wild-type mice, suggesting that the in vivo conditions that generate encephalitogenic T cells must be different (Yang et al. 2009; Ghoreschi et al. 2010). It was subsequently shown that differentiation of naive T cells with IL-6, in the absence of TGFβ and cytokines that promote Th1 or Th2 cells , generates Th17 cells capable of transferring EAE (Fig. 3.1; Yang et al. 2009; Ghoreschi et al. 2010). This observation was consistent with a previous study that found that TGFβ is a negative regulator of T-bet (Gorelik et al. 2002; Park et al. 2005). Therefore, Th17-inducing conditions that included TGFβ-generated T cells failed to express T-bet. Although these T cells expressed significant amounts of IL-17, they were T-bet-negative and lacked a critical element of an encephalitogenic T cell. However, encephalitogenic T cells from wild-type mice had T-bet-positive Th17 cells, and Th17 cells differentiated in vivo with IL-6 in the absence of TGFβ also expressed T-bet , indicating that T-bet was a critical factor in encephalitogenic T cells regardless of whether they expressed a Th1 or Th17 phenotype (Yang et al. 2009).
T-bet has been implicated in the regulation of other molecules associated with the Th1 phenotype and encephalitogenicity. For example, T-bet has been shown to be required for optimal migration of Th1 cells into tissues. T-bet appears to regulate the binding of Th1 cells to P-selectin, an adhesion molecule expressed on inflamed endothelium (Lord et al. 2005). T-bet has also been found to regulate the chemokine receptor CXCR3, which is highly expressed on encephalitogenic Th1 cells (Qin et al. 1998; Sallusto et al. 1998; Beima et al. 2006). This led to speculation that CXCR3 may be vital to T cell trafficking to the CNS and thus, T-bet may be critical due to its role in upregulating CXCR3 expression on CD4 T cells . Although CXCR3 inhibitors have been shown to slightly diminish EAE severity (Kohler et al. 2008; Ni et al. 2009; Sporici and Issekutz 2010), CXCR3-deficient mice remain susceptible to EAE (Liu et al. 2006; Muller et al. 2007) indicating that CXCR3 is not critical to EAE development and, therefore, it is not an essential element regulated by T-bet . This indicates that the diminished trafficking capacity of T-bet-deficient CD4 T cells is probably mediated by a mechanism independent of CXCR3.
CD80 /86 on APCs interaction with C28 on T cells is necessary to activate naive T cells in conjunction with TCR engagement (Fig. 3.1). However, memory and effector T cell populations do not require this costimulation signal via CD28 , making it possible for memory and effector T cells to function in a rapid and precise manner (Dubey et al. 1996; Yi-qun et al. 1996; Lovett-Racke et al. 1998). More recently, it was discovered that there were other costimulatory molecules , such as inducible costimulator (ICOS) expressed on memory and effector T cells that contribute to their effector function. Inhibition of ICOS after the induction of EAE attenuated the disease (Rottman et al. 2001; Sporici et al. 2001). Ex vivo analysis of the CNS of these mice showed that the myelin-specific CD4 T cells became activated, produced IL-2, and trafficked to the CNS. However, IFNγ production was diminished and enhanced the apoptosis of memory T cells . T-bet was found to bind the ICOS promoter to regulate ICOS expression in conjunction with the transcription factor, NFATc2 (Tan et al. 2008). Since T-bet is not expressed in naive T cells and only expressed following T cell differentiation, the induction of ICOS in memory and effector T cells is temporally consistent with T-bet expression. In human T cells, ICOS was found to dramatically enhance the expansion of IFNγ + IL-17 + T cells, which have been found to have enhanced proinflammatory effector function in EAE and other diseases (Paulos et al. 2010). Interestingly, these cells also express high levels of T-bet , suggesting that T-bet may be enhancing the pathogenic potential of IFNγ + IL-17 + T cells via ICOS costimulation.
In 2001, a large-scale sequencing of cDNA libraries acquired from CNS lesions from MS patients found enhanced expression of osteopontin, a cytokine previously associated with bone formation (Chabas et al. 2001). Rats with EAE were also found to have enhanced osteopontin expression in their CNS. Although mice deficient in osteopontin develop EAE, the disease is less severe, had fewer relapses, and diminished proinflammatory cytokine expression (Chabas et al. 2001; Jansson et al. 2002). T-bet was found to at least partially regulate osteopontin expression, and T-bet-dependent osteopontin expression is necessary for optimal differentiation of Th1 cells (Shinohara et al. 2005). Osteopontin was subsequently found to initiate recurrent relapses and enhance neurological deficits in mice with EAE via enhanced survival of myelin-specific T cells (Hur et al. 2007). T-bet had originally been considered a transcription factor, critical in the initial differentiation of CD4 T cells, but this study indicates that T-bet function in effector and memory T cells via ICOS and osteopontin may be just as important in demyelinating autoimmunity. This was validated in treatment studies of EAE with an siRNA specific for T-bet in which disease was virtually halted in mice when T-bet was suppressed (Gocke et al. 2007). Furthermore, osteopontin levels are elevated in the CSF and serum of MS patients, and elevated osteopontin in the CSF appears to be correlated with relapses (Bornsen et al. 2011; Wen et al. 2012), reminiscent of elevated T-bet levels in MS patients (Frisullo et al. 2009; Kleiter et al. 2010).
T cell Ig- and mucin-domain-containing molecule 3 (Tim-3) was found to be expressed by Th1 cells and blockade of Tim-3 in EAE results in enhanced disease severity, suggesting that Tim-3 plays a role in limiting the effector function of Th1 cells (Monney et al. 2002; Khademi et al. 2004). Tim-3 was also found to be expressed on resident CNS cells in rats with EAE, suggesting that it may contribute CNS autoimmunity in the target organ as well as the infiltrating T cells (Gielen et al. 2005). T cell clones from the CSF of MS patients found that Tim-3 and T-bet were reduced compared to clones derived from control subjects, and that the MS patient T cells had enhanced production of IFNγ suggesting that Tim-3 inversely correlates with IFNγ expression (Koguchi et al. 2006). Using an siRNA specific for Tim-3 , T cell proliferation and IFNγ production were reduced, demonstrating the Tim-3 expression plays a significant role in Th1 cell function. CSF T cell clones with low Tim-3 levels also demonstrated resistance to inhibitor signals via CTLA-4 , suggesting that their enhanced effector functions may be partially due to diminished regulation (Koguchi et al. 2006). Blockade of Tim-3 ex vivo in MS patients’ CD4 T cells did not alter IFNγ production as it did in control subjects, demonstrating a defect in Tim-3 immunoregulation (Yang et al. 2008a, 2008b). Interestingly, glatiramer acetate or IFNβ treatment reversed the functional defect. Thus, dysregulated expression of Tim-3 in MS patients may contribute to disease pathology, and current immunomodulatory drugs may be beneficial at normalizing immune dysregulation mediated by Tim-3. T-bet was found to contribute to the expression of Tim-3 in Th1 cells (Anderson et al. 2010). Since Tim-3 plays a role in dampening Th1 responses, it appears that T-bet-regulated expression of Tim-3 plays a role in not only inducing Th1 responses, but also regulating them in a manner that limits Th1 effector functions. Since MS patients appear to have diminished Tim-3 expression in effector/memory T cells, the balance of protective adaptive immune responses may be tipped such that proinflammatory T cells go unregulated for extended periods of time resulting in autoimmune tissue damage.
Together, these studies demonstrate that T-bet regulates the expression of several genes that play different roles in T cells’ differentiation and effector functions. T-bet may be an effective therapeutic target in EAE due to its ability to modulate different mechanisms in T cells that are required for development, trafficking, and pathogenesis in immune-mediated demyelinating disease.
3.6 Relevance of T-bet in Multiple Sclerosis
It is clear that T-bet is an essential factor in encephalitogenic T cells in mice. Yet, its role in MS is much more difficult to assess. However, changes in T-bet levels have become a common measure of therapeutic potential of drugs evaluated in EAE and MS patients. T-bet levels in peripheral T cells are enhanced in MS patients during relapses relative to remission and are elevated in MS patients compared to healthy controls (Frisullo et al. 2006; Kleiter et al. 2010). In addition, pSTAT1, the transcription factor that is initially activated during Th1 cell differentiation (Fig. 3.1a) is also upregulated. Since pSTAT1 contributes to the expression of T-bet (Afkarian et al. 2002; Lovett-Racke et al. 2004), it is not surprising that T-bet and pSTAT1 levels have a positive correlation. In addition, T-bet and pSTAT1 levels correlated with active lesions in the CNS as determined by MRI, suggesting that T-bet may be a marker of disease activity in MS. Glucocorticoids, which have anti-inflammatory properties, have been used successfully to treat MS exacerbations for decades. Ex vivo analysis of T cells from MS patients treated with glucocorticoids found that T-bet and pSTAT1 were reduced, as well as IFNγ production by peripheral lymphocytes (Frisullo et al. 2007), indicating that T-bet may be a potential biomarker of therapeutic efficacy.
During pregnancy, MS patients have a reduced exacerbation rate compared to pre- and postpregnancy (Korn-Lubetzki et al. 1984). The mechanisms that underlie this protection probably lie in the immune-tolerant state that is induced to protect the fetus. Interestingly, relapse rates in women postdelivery are often enhanced but typically return to prepregnancy levels within 1 year. In pregnant MS patients, T-bet levels are reduced, consistent with an anti-inflammatory or tolerant state (Iorio et al. 2009). However, in MS patients who have a relapse after delivery or have new active lesions, T-bet and pSTAT1 levels are enhanced, as well as IFNγ and IL-17 levels. In addition, there is an increase in CD4+ CD25+ Foxp3+- regulatory T cell population during pregnancy that may be suppressing the T-bet + T cells. Again, this study indicates that T-bet may be a marker of disease activity in MS.
For the past two decades, IFNβ has been used as a therapy for relapsing–remitting MS . In a study to determine whether Th1 or Th17 cells were altered due to IFNβ therapy , IFNγ and T-bet mRNA levels were reduced at 1-year postinitiation of IFNβ therapy, while IL-17 and RORγt (the Th17-associated transcription factor) were unchanged (Drulovic et al. 2009). Analysis of IFNβ responders versus nonresponders found that reduced T-bet levels correlated with a favorable clinical response to IFNβ treatment, further supporting the role of T-bet as a critical molecule in MS pathogenesis and as a potential indicator of therapeutic efficacy.
More recently, T-bet expression has been evaluated in clinical trials of new potential therapies for MS. Statins, 3-hydroxy-3-mehtylglutaryl coenzyme-A reductase inhibitors that have traditionally been used to reduce cholesterol, have been found to have immunomodulatory effects. Due to their widespread use and good safety record, they have been evaluated in MS as potential therapies. In clinical trials, ex vivo analysis revealed that MS patients on statins had reduced T cell proliferation, reduced proinflammatory cytokine expression and reduced T-bet expression, as well as significant clinical benefit to the patients (Peng et al. 2006).
Although there is evidence that T-bet levels correlate with disease activity and treatment efficacy in MS patients, it is still unclear whether T-bet is aberrantly expressed in MS patients, perhaps making them more susceptible to proinflammatory responses and the development of autoimmunity. MS patients have an increased incidence of other Th1-mediated autoimmune diseases such as diabetes, thyroiditis, and psoriasis, suggesting that they may possess a bias toward robust Th1 responses that may make them susceptible to Th1-mediated autoimmune diseases (Roquer et al. 1987; Karni and Abramsky 1999; Sloka 2002; Annunziata et al. 2003; Nielsen et al. 2006). A comprehensive analysis of miRNA expression in naive CD4 T cells of MS patients suggested that MS patients may have an inherent propensity to differentiate into Th1 cells due to loss of miRNA-mediated regulation of genes in the Th2 pathway (Guerau-de-Arellano et al. 2011). Since miRNAs negatively regulate gene expression, enhanced miRNA expression will result in decreased target gene expression. It was found that MS patients have enhanced expression of miR-27, miR-128, and miR-340 in CD4 T cells, resulting in decreased expression of Bmi1, GATA3, and IL-4. Since GATA3 and T-bet compete for lineage commitment during activation of naive T cells, reduced GATA3 leads to a dominant Th1 response. This study suggests that T-bet may be aberrantly expressed in CD4 T cells of MS patients due to miRNA-mediated suppression of Th2-associated molecules.
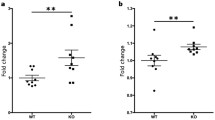
Several studies found that T-bet and IFNγ expression were also regulated by miRNA (Ma et al. 2011; Steiner et al. 2011; Smith et al. 2012). IFNγ induces the expression of miR-29, as well as T-bet, in CD4 T cells (Smith et al. 2012). T-bet directly regulates the expression of IFNγ, committing the CD4 T cell to the Th1 lineage. However, miR-29 subsequently binds to the mRNA of T-bet and IFNγ, demonstrating that a negative feedback loop exists as an additional mechanism to maintain a proper balance of IFNγ and to dampen effector Th1 responses appropriately following an inflammatory response. In resting memory, CD4 T cells of MS patients, T-bet, and miR-29 levels are increased, compared to control subjects (Smith et al. 2012). However, activation of MS patient memory CD4 T cells results in a significant decrease in miR-29 levels indicating that the feedback loop between miR-29 and T-bet/IFNγ is dysregulated in MS patients. The diminished capacity of miR-29 to regulate T-bet levels may be another mechanism that may promote chronic inflammation in MS patients.
3.7 Is T-bet a Valid Therapeutic Target for Multiple Sclerosis?
The T-bet-regulated gene that has been studied the most extensively is IFNγ. The contradictory data on the role of IFNγ in EAE and MS suggest that care must be taken on how therapies may systemically alter IFNγ levels. So is T-bet a valid therapeutic target in light of the data of EAE when IFNγ is suppressed? The observation that IFNγ-deficient mice remained susceptible to EAE (Ferber et al. 1996), and often had a more severe disease course than wild-type controls, led to caution about using drugs that may dramatically effect IFNγ levels. The EAE data in IFNγ-deficient mice and mice treated with antibodies to neutralize IFNγ suggested the IFNγ may play a positive regulatory role in the disease course (Lublin et al. 1993; Ferber et al. 1996; Heremans et al. 1996; Willenborg et al. 1996). However, there were two small clinical trials in MS patients that may suggest that inhibiting IFNγ in humans may be beneficial. In the 1980s, it was recognized that cytokines regulate immune responses and it was hypothesized that IFNγ may be beneficial in normalizing the aberrant immune responses observed in MS patients. IFNγ was administered to MS patients, resulting in an increased number of clinical exacerbations in the patients (Panitch et al. 1987). Subsequently, it was observed that IFNγ induces apoptosis of human oligodendrocytes , the cells that make myelin, and IFNγ expression in MS lesions colocalizes with apoptotic oligodendrocytes (Vartanian et al. 1995; Baerwald and Popko 1998), suggesting that IFNγ may play a role in the demyelination observed in the CNS of MS patients. These observations led to a clinical trial in which an IFNγ-neutralizing antibody was administered to MS patients, resulting in a clinical benefit (Skurkovich et al. 2001). Due to the contradictory data between mice and humans, systemic blockade of IFNγ has not continued in humans. However, the beneficial observations in humans suggest that the Th1 pathway is a viable therapeutic target.
When T-bet is genetically deleted or when T-bet is suppressed systemically with siRNA, mice are resistant to EAE induction, supporting T-bet as an effective therapeutic target (Bettelli et al. 2004; Lovett-Racke et al. 2004). Moreover, administration of a T-bet siRNA after the onset of EAE suggests that T-bet is a potential therapeutic target for established autoimmune demyelinating disease (Gocke et al. 2007). This is a critical point since we cannot predict who will develop MS and, therefore, must develop therapeutics that can prevent the development of autoreactive T cells, as well as suppress the effector/memory T cells that are already mediating lesion formation in MS patients. Furthermore, in MS patients treated with nonspecific immunomodulatory drugs, T-bet is reduced in patients who have clinical benefit (Drulovic et al. 2009).
Although T-bet is expressed in most immune cells, its role in EAE appears to be primarily mediated by CD4 T cells . In addition, T-bet regulates IFNγ in CD4 T cells, but does not appear to regulate IFNγ expression extensively in other immune cells (Szabo et al. 2000; Szabo et al. 2002). Therefore, suppression of T-bet does not result in systemic loss of IFNγ production and any positive effects of IFNγ that may be mediated by other immune cells would not be dramatically affected by suppression of T-bet. Thus, targeting T-bet may have far fewer potential side effects compared to global suppression of IFNγ .
T-bet and GATA3, the Th2 -associated transcription factor, physically associate and compete to dominate lineage-specific genes in order to generate Th1 or Th2 cells (Hwang et al. 2005; Jenner et al. 2009). There is concern that suppression of T-bet may make individuals susceptible to Th2-mediated diseases, since GATA3 will not be as tightly regulated in the absence of T-bet. T-bet-deficient mice develop lung pathology consistent with allergic asthma (Finotto et al. 2002), a classic Th2-mediated disease. However, in mice treated with a T-bet siRNA, no lung pathology was observed, suggesting that diminishing T-bet expression, as opposed to complete abrogation of T-bet , may not have the same outcome (Lovett-Racke et al. 2004). The observation that MS patients have a decreased incidence of allergy and asthma is evidence that their immune responses may be biased away from Th2 responses (Bergamaschi et al. 2009; Pedotti et al. 2009). Thus, reducing T-bet expression in MS patients may simply normalize immune responses such that proinflammatory T cell effector functions are reduced, but not such that Th2 -mediated diseases are a real threat.
3.8 Conclusion
MS is a complex disease that involves both inflammation and neurodegeneration. Since the inflammation appears to precede pathology and neurological deficits, a tremendous amount of research has been devoted to understanding the inflammatory process that is occurring at the site of lesion formation. In this quest, effector CD4 T cells have been found to be at the center of the immune response that results in demyelination and axonal damage. Why and how CD4 T cells become programmed to enter the apparently healthy CNS and mediate damage is unclear. However, T-bet is one molecule that appears to be associated with the capacity of CD4 T cells to cause CNS injury. Due to its relatively limited expression in humans, it may be a viable therapeutic target for MS. In addition, defining the role of T-bet in generating encephalitogenic T cells and their effector functions provides insight into the mechanisms that underlie the pathology of MS lesions.
References
Acosta-Rodriguez EV, Napolitani G, Lanzavecchia A, Salluston F (2007) Interleukins 1beta and 6 but not transforming growth factor-beta are essential for the differentiation of interleukin 17-producing human T helper cells. Nat Immunol 8:942–949
Afkarian M, Sedy JR, Yang J, Jacobson NG, Cereg N, Yang SY, Murphy TL, Murphy KM (2002) T-bet is a STAT1-induced regulator of IL-12R expression in naïve CD4+ T cells. Nat Immunol 3:549–557
Anderson AC, Lord GM, Dardalhon V, Lee DH, Sabatos-Peyton CA, Glimcher LH, Kuchroo VK (2010) T-bet, a Th1 transcription factor regulates the expression of Tim-3. Eur J Immunol 40:859–866
Ando DG, Clayton J, Dono D, Urban JL, Sercarz EE (1989) Encephalitogenic T cells in the B10.PL model of experimental allergic encephalomyelitis (EAE) are of the Th-1 lymphokine subtype. Cell Immunol 124:132–43
Annunziata P, Morana P, Giorgio A, Galeazzi M, Campanella V, Lore F et al (2003) High frequency of psoriasis in relatives is associated with early onset in an Italian multiple sclerosis cohort. Acta Neurol Scand 108:327–331
Baerwald KD, Popko B (1998) Developing and mature oliodendrocytes respond differently to the immune cytokine interferon-gamma. J Neurosci Res 52:230–239
Becher B, Durell BG, Noelle R (2002) Experimental autoimmune encephalitis and inflammation in the absence of interleukin-12. J Clin Invest 110:493–497
Becher B, Durell BG, Noelle RJ (2003) IL-23 produced by CNS-resident cells controls T cell encephalitogenicity during the effector phase of experimental autoimmune encephalomyelitis. J Clin Invest 112:1186–1191
Beima KM, Miazgowicz MM, Lewis MD, Yan PS, Huang TH, Weinmann AS (2006) T-bet binding to newly identified target gene promoters is cell type-independent but results in variable context-dependent functional effects. J Biol Chem 281:11992–12000
Bergamaschi R, Villani S, Crabbio M, Ponzio M, Romani A, Verri A et al (2009) Inverse relationship between multiple sclerosis and allergic respiratory diseases. Neurol Sci 30:115–118
Bettelli E, Sullivan B, Szabo SJ, Sobel RA, Glimcher LH, Kuchroo VK (2004) Loss of T-bet but not STAT1, prevents the development of experimental autoimmune encephalomyelitis. J Exp Med 200:79–87
Bettelli E, Carrier Y, Gao W, Kom T, Strom TB, Oukka M, Weiner HL, Kuchroo VK (2006) Reciprocal developmental pathways for the generation of pathogenic effector TH17 and regulatory T cells. Nature 441:235–238
Bornsen L, Khademi M, Olsson T, Sorensen PS, Sellebjerg F (2011) Osteopontin concentrations are increased in cerebrospinal fluid during attacks of multiple sclerosis. Mult Scler 17:32–42
Chabas D, Baranzini SE, Mitchell D, Bernard CC, Rittling SR, Denhardt DT, Sobel RA, Lock C, Karpuj M, Pedotti R, Heller R, Oksenberg JR, Steinman L (2001) The influence of the proinflammatory cytokine, osteopontin, on autoimmune demyelinating disease. Science 294:1731–1735
Charcot JM (1968) Histologie de la sclerose en plaques Gazette des hopitaux. Paris 41:554–555
Chen Y, Langrish CL, McKenzie B, Joyce-Shaikh B, Stumhofer JS, McClanahan T, Blumenschein W, Churakovsa T, Low J, Presta L, Hunter CA, Kastelein RA, Cua DJ (2006) Anti-IL-23 therapy inhibits multiple inflammatory pathways and ameliorates autoimmune encephalomyelitis. J Clin Invest 116:1317–26
Chitnis T, Najafian N, Benou C, Salama AD, Grusby MJ, Sayegh MH, Khoury SJ (2001) Effect of targeted disruption of STAT4 and STAT6 on the induction of experimental autoimmune encephalomyelitis. J Clin Invest 108:739–747
Codarri L, Gyulveszi G, Tosevski V, Hesske L, Fontana A, Magnenat L, Suter T, Becher B (2011) RORγt drives production of the cytokine GM-CSF in helper T cells, which is essential for the effector phase of autoimmune neuroinflammation. Nat Immunol 12:560–567
Cua DJ, Sherlock J, Chen Y, Murphy CA, Joyce B, Seymour B, Lucian L, To W, Kwan S, Churakova T, Zurawski S, Wiekowski M, Lira SA, Gorman D, Kastelein RA, Sedgwick JD (2003) Interleukin-23 rather than interleukin-12 is the critical cytokine for autoimmune inflammation of the brain. Nature 421:744–748
Drulovic J, Savic E, Pekmezovic T, Mesaros S, Stojavljevic N, Dujmovic-Basiroski I, Kostic J, Vasic V, Stojkovic MM, Popadic D (2009) Expression of Th1 and Th17 cytokines and transcription factors in multiple sclerosis patients: Does baseline T-bet mRNA predict the response to interferon-beta treatment? J Neuroimmunol 215:90–95
Dubey C, Croft M, Swain SL (1996) Naïve and effector CD4 T cells differ in their requirements for T cell receptor versus costimulatory signals. J Immunol 157:3280–3289
El-Behi M, Ciric B, Dai H, Yan Y, Cullimore M, Safavi F, Zhang GX, Dittel BN, Rostami A (2011) The encephalitogenicity of T(H)17 cells is dependent on IL-1- and IL-23-induced production of the cytokine GM-CSF. Nat Immunol 12:568–575
Ferber IA, Brock S, Taylor-Edwards C, Ridgway W, Dinisco C, Steinman L, Dalton D, Fathman CG (1996) Mice with a disrupted IFN-gamma gene are susceptible to the induction of experimental autoimmune encephalomyelitis (EAE). J Immunol 156:5–7
Finotto S, Neurath MF, Glickman JN, Qin S, Lehr HA, Green FH, Ackerman K, Haley K, Galle PR, Szabo SJ, Drazen JM, De Sanctis GT, Glimcher LH (2002) Development of spontaneous airway changes consistent with human asthma in mice lacking T-bet. Science 295:336–338
Frisullo G, Angelucci F, Caggiula M, Nociti V, Iorio R, Patanella AK, Sancricca C, Mirabella M, Tonali PA, Batocchi AP (2006) pSTAT1, pSTAT3, and T-bet expression in peripheral blood mononuclear cells from relapsing-remitting multiple sclerosis patients correlates with disease activity. J Neurosci Res 84:1027–1036
Frisullo G, Nociti V, Iorio R, Patanella KA, Bianco A, Caggiula M, Sancricca C, Tonali PA, Mirabella M, Batocchi AP (2007) Glucocorticoid treatment reduces T-bet and pSTAT1 expression in mononuclear cells from relapsing remitting multiple sclerosis patients. Clin Immunol 124:284–293
Frisullo G, Nociti V, Iorio R, Patanella AK, Caggiula M, Marti A, Sancricca C, Angelucci F, Mirabella M, Tonali PA, Batocchi AP (2009) Regulatory T cells fail to suppress CD4+ T-bet + T cells in relapsing multiple sclerosis patients. Immunology 127:418–428
Frisullo G, Iorio R, Plantone D, Marti A, Nociti V, Patanella AD, Batocchi AP (2011) CD4+ T-bet+, CD4+ pSTAT3+ and CD8+ T-bet+ T cells accumulate in peripheral blood during NZB treatment. Mult Scler 17:556–566
Ghoreschi K, Laurence A, Yang XP, Tato CM, McGeachy MJ, Konkel JE, Ramos HL, Wei L, Davidson TS, Bouladoux N, Grainger JR, Chen Q, Kanno Y, Watford WT, Sun HW, Eberl G, Shevach EM, Belkaid Y, Cua DJ, Chen W, O’Shea JJ (2010) Generation of pathogenic T(H)17 cells in the absence of TGF-β signalling. Nature 467(7318):967–971. doi: 10.1038/nature09447
Gielen AW, Lobell A, Lidman O, Khademi M, Olsson T, Piehl F (2005) Expression of T cell immunoglobulin- and mucin-domain-containing molecules-1 and -3 (TIM-1 and -3) in the rat nervous and immune systems. J Neuroimmunol 164:93–104
Gocke AR, Cravens PD, Ben LH, Hussain RZ, Northrop SC, Racke MK, Lovett-Racke AE (2007) T-bet regulates the fate of Th1 and Th17 lymphocytes in autoimmunity. J Immunol 178:1341–1348
Gorelik L, Constant S, Flavell RA (2002) Mechanism of transforming growth factor beta-induced inhibition of T helper type 1 differentiation. J Exp Med 195:1499–1505
Gran B, Zhang GX, Yu S, Li J, Chen XH, Ventura ES, Kamoun M, Rostami A (2002) IL-12p35-deficient mice are susceptible to experimental autoimmune encephalomyelitis: evidence for redundancy in the IL-12 system in the induction of central nervous system autoimmune demyelination. J Immunol 169:7104–7410
Guerau-de-Arellano M, Smith KM, Godlewski J, Liu Y, winger R, Lawler SE, Whitacre CC, Racke MK, Lovett-Racke AE (2011) Micro-RNA dysregulation in multiple sclerosis favours pro-inflammatory T-cell-mediated autoimmunity. Brain 134:3578–89
Haak S, Croxford AL, Dreymborg K, Heppner FL, Pouly S, Becher B, Waisman A (2009) IL-17 A and IL-17 F do not contribute vitally to autoimmune neuro-inflammation in mice. J Clin Invest 119:61–69
Heremans H, Dillen C, Groenen M, Martens E, Billiau A (1996) Chronic relapsing experimental autoimmune encephalomyelitis (CREAE) in mice: enhancement by monoclonal antibodies against interferon-gamma. Eur J Immunol 26:2393–2398
Hori S, Takahashi T, Sakaguchi S (2003) Control autoimmunity by naturally arising regulatory CD4+ T cells. Adv Immunol 81:331–371
Hou J, Schindler U, Henzel WJ, Ho TC, Brasseur M, McKnight SL (1994) An interleukin-4-induced transcription factor: IL-4 Stat. Science 265:1701–1706
Hsieh CS, Heimberger AB, Gold JS, O’Garra A, Murphy KM (1992) Differential regulation of T helper phenotype development by interleukin 4 and 10 in an alpha beta T-cell-receptor transgenic system. Proc Natl Acad Sci U S A 89:6065–6069
Hur EM, Youssef S, Haws ME, Zhang SY, Sobel RA, Steinman L (2007) Osteopontin-induced relapse and progression of autoimmune brain disease through enhanced survival of activated T cells. Nat Immunol 8:74–83
Hwang ES, Szabo SJ, Schwartzberg PL, Glimcher LH (2005) T helper cell fate specified by kinase-mediated interaction of T-bet with GATA-3. Science 307:430–343
Iorio R, Frisullo G, Nociti V, Patanella KA, Bianco A, Marti A, Mirabella M, Tonali PA, Batocchi AP (2009) T-bet pSTAT1 and pSTAT3 expression in peripheral blood mononuclear cells during pregnancy correlates with post-partum activation of multiple sclerosis. Clin Immunol 131:70–83
Jacobson NF, Szabo SJ, Weber-Nordt RM, Zhong Z, Schreiber RD, Darnell JE, Murphy KM (1995) Interleukin 12 signaling in T helper type 1 (Th1) cells involves tyrosine phosphorylation of signal transducer and activator of transcription (Stat) 3 and Stat4. J Exp Med 181:1755–1762
Jansson M, Panoutsakopoulou V, Baker J, Klein L, Cantor H (2002) Cutting edge: Attenuated experimental autoimmune encephalomyelitis in eta-1/osteopontin-deficient mice. J Immunol 168:2096–2099
Jenner RG, Townsend MJ, Jackson I, Sun K, Bouwman RD, Young RA, Glimcher LH, Lord GM (2009) The transcription factors T-bet and GATA-3 control alternative pathways of T-cell differentiation through a shared set of target genes. Proc Natl Acad Sci U S A 106:17876–17881
June CH, Ledbetter JA, Linsley PS, Thompson CB (1990) Role of the CD28 receptor in T-cell activation. Immunol Today 11:211–216
Karni A, Abramsky O (1999) Association of MS with thyroid disorders. Neurology 53:883–885
Khademi M, Illes Z, Gielen AW, Marta M, Takazawa N, Baecher-Allan C, Brundin L, Hannerz J, Martin C, Harris RA, Hafler DA, Kuchroo VK, Olsson T, Piehl F, Wallstrom E (2004) T cell Ig- and mucin-domain-containing molecule-3 (TIM-3) and TIM-1 molecules are differentially expressed on human Th1 and Th2 cells and in cerebrospinal fluid-derived mononuclear cells in multiple sclerosis. J Immunol 172:7169–7176
Kleiter I, Song J, Lukas D, hasan M, Neumann B, Croxford AL, Pedre X, Hovelmeyer N, Yogev N, Mildner A, Prinz M, Wiese e, Reifenberg K, Bittner S, Siendl H, Steinman L, Becker C, Bogdahn U, Neurath MF, Steinbrecher A, Waisman A (2010) Smad7 in T cells drives T helper 1 responses in multiple sclerosis and experimental autoimmune encephalomyelitis. Brain 133:1067–1081
Koguchi K, Anderson DE, Yang L, O’Connor KC, Kuchroo VK, Hafler DA (2006) Dysregulated T cell expression of TIM3 in multiple sclerosis. J Exp Med 203:1413–1418
Kohler RE, Comerford I, Townley S, Haylock-Jacobs S, Clark-Lewis I, McColl SR (2008) Antagonism of the chemokine receptors CXCR3 and CXCR4 reduces the pathology of experimental autoimmune encephalomyelitis. Brain Pathol 18:504–516
Komiyama Y, Nakae S, Matsuki T, Nambu A, Ishigame H, Kakuta S, Suko K, Iwakura Y (2006) IL-17 plays an important role in the development of experimental autoimmune encephalomyelitis. J Immunol 177:566–573
Korn-Lubetzki I, Kahana E, Cooper G, Abramsky O (1984) Activity of multiple sclerosis during pregnancy and puerperium. Ann Neurol 16:229–231
Kroenke MA, Segal BM (2007) Th17 and Th1 responses directed against the immunizing epitope, as opposed to secondary epitopes, dominate the autoimmune repertoire during relapses of experimental autoimmune encephalomyelitis. J Neurosci Res 85:1685–1693
Kumar V, Stellrecht K, Sercarz E (1996) Inactivation of T cell receptor peptide-specific CD4 regulatory T cells induces chronic experimental autoimmune encephalomyelitis (EAE). J Exp Med 184:1609–1617
Langrish CL, Chen Y, Blumenschein WM, Mattson J, Basham B, Sedgwick JD, McClanahan T, Kastelein RA, Cua DJ (2005) IL-23 drives a pathogenic T cell population that induces autoimmune inflammation. J Exp Med 201:233–40
Lees JR, Iwakura Y, Russell JH (2008) Host T cells are the main producers of IL-17 within the central nervous system during initiation of experimental autoimmune encephalomyelitis induced by adoptive transfer of Th1 cell lines. J Immunol 180:8066–72
Lewis MD, Miller SA, Miazgowicz MM, Beima KM, Weinmann AS (2007) T-bet’s ability to regulate individual target genes requires the conserved T-box domain to recruit histone methyltransferase activity and a separate family member-specific transactivation domain. Mol Cell Biol 27:8510–8521
Liu L, Huang D, Matsui M, He TT, Hu T, Demartino J, Lu B, Gerard C, Ransohoff RM (2006) Severe disease, unaltered leukocyte migration, and reduced IFN-gamma production in CXCR3-/- mice with experimental autoimmune encephalomyelitis. J Immunol 176:4399–4409
Lock C, Hermans G, Pedotti R, Brendolan A, Schadt E, Garren H, Langer-Gould A, Strober S, Cannella B, Allard J, Klonowski P, Austin A, Lad N, Kaminski N, Galli SJ, Oksenberg JK, Raine CS, Heller R, Steinman L (2002) Gene-microarray analysis of multiple sclerosis lesions yields new targets validated in autoimmune encephalomyelitis. Nat Med 8:500–508
Lord GM, Rao RM, Choe H, Sullivan BM, Lichtman AH, Luscinskas FW, Glimcher LH (2005) T-bet is required for optimal proinflammatory CD4+ T-cell trafficking. Blood 106:3432–3439
Lovett-Racke AE, Trotter JL, Lauber J, Perrin PJ, June CH, Racke MK (1998) Decreased dependence of myelin basic protein-reactive T cells on CD28-mediated costimulation in multiple sclerosis patients. A marker of activated/memory T cells. J Clin Invest 101:725–730
Lovett-Racke AE, Rocchini AE, Choy J, Northrop SC, Hussain RZ, Ratts RB, Sikder D, Racke MK (2004) Silencing T-bet defines a critical role in the differentiation of autoreactive T lymphocytes. Immunity 21:719–731
Lublin FD, Knobler RL, Kalman B, Goldhaber M, Marini J, Perrault M, D’Imperio C, Joseph J, Alkan SS, Korngold R (1993) Monoclonal anti-gamma interferon antibodies enhance experimental allergic encephalomyelitis. Autoimmunity 16:267–274
Ma F, Xu S, Liu X, Zhang Q, Xu X, Liu M, Hua M, Li N, Yao H, Cao X (2011) The microRNA miR-29 controls innate and adaptive immune responses to intracellular bacterial infection by targeting interferon-γ. Nat Immunol 12:861–869
Mangan PR, Harrington LE, O’Quinn DB, Helms WS, Bullard DC, Elson CO, Hatton RD, Wahl SM, Schoeb TR, Weaver CT (2006) Transforming growth factor-β induces development of the Th17 lineage. Nature 441:231–234
Marie JC, Letterio JJ, Gavin M, Rudensky AY (2005) TGF-beta1 maintains suppressor function and Foxp3 expression in CD4+ CD25 + regulatory T cells. J Exp Med 201:1061–1067
McDonald AH, Swanborg RH (1988) Antigen-specific inhibition of immune interferon production by suppressor cells of autoimmune encephalomyelitis. J Immunol 140:1132–1138
Miller SA, Huang AC, Miazgowicz MM, Brassil MM, Weinmann AS (2008) Coordinated but physically separable interaction with H3K27-demethylase and H3K4-methyltransferase activities are required for T-box protein-mediated activation of developmental gene expression. Genes Dev 22:2980–2993
Monney L, Sabatos CA, Gaglia JL, Ryu A, Waldner H, Chernova T, Manning S, Greenfield EA, Coyle AJ, Sobel RA, Freeman GJ, Kuchroo VK (2002) Th1-specific cell surface protein Tim-3 regulates macrophage activation and severity of an autoimmune disease. Nature 415:536–541
Mosmann TR, Cherwinski H, Bond MS, Giedlin MA, Coffman RL (1986) Two types of murine helper T cell clones. I Definition according to profiles of lymphokine activities and secreted proteins. J Immunol 136:2348–2357
Muller M, Carter SL, Hofer MJ, Manders P, Getts DR, Getts MT, Dreykluft A, Lu B, Gerard C, King NJ, Campbell IL (2007) CXCR3 signaling reduces severity of experimental autoimmune encephalomyelitis by controlling the parenchymal distribution of effector and regulatory T cells in the central nervous system. J Immunol 179:2774–2786
Nath N, Giri S, Prasad R, Singh AK, Singh I (2004) Potential targets of 3-hydroxy-3-methylglutaryl coenzyme A reductase inhibitor for multiple sclerosis therapy. J Immunol 172:1273–1286
Nath N, Prasad R, Giri S, Singh AK, Singh I (2006) T-bet is essential for the progression of experimental autoimmune encephalomyelitis. Immunology 118:384–391
Ni J, Zhu YN, Zhong XG, Ding Y, Hou LF, Tong XK, Tang W, Ono S, Yang YF, Zuo JP (2009) The chemokine receptor antagonist, TAK-779, decreased experimental autoimmune encephalomyelitis by reducing inflammatory cell migration into the central nervous system, without affecting T cell function. Br J Pharmacol 158:2046–2056
Nielsen NM, Westergaard T, Frisch M, Rostgaard K, Wohlfahrt J, Koch-Henriksen N et al (2006) Type 1 diabetes and multiple sclerosis: A Danish population-based cohort study. Arch Neurol 63:1001–1004
Oestreich KJ, Huang AC, Weinmann AS (2011) The lineage-defining factors T-bet and Bcl-6 collaborate to regulate Th1 gene expression patterns. J Exp Med 208:1001–1013
Oppmann B, Lesley R, Blom B, Timans JC, Xu Y, Hunte B, Vega F, Yu N, Wang J, Singh K, Zonin F, Vaisberg E, Churakova T, Liu M, Gorman D, Wagner J, Zurawski S, Liu Y, Abrams JS, Moore KW, Rennick D, Waal-Malefyt R de, Hannum C, Bazan JF, Kastelein RA (2000) Novel p19 protein engages IL-12p40 to form a cytokine, IL-23, with biological activities similar as well as distinct from IL-12. Immunity 13:715–725
Panitch HS, Hirsch RL, Haley AS, Johnson KP (1987) Exacerbation of multiple sclerosis in patients treated with gamma interferon. Lancet 1:893–895
Parham C, Chirica M, Timans J, Vaisberg E, Travis M, Cheung J, Pflanz S, Zhang R, Singh KP, Vega F, To W, Wagner J, O’Farrell AM, McClanahan T, Zurawski S, Hannum C, Gorman D, Rennick DM, Kastelein RA, de Waal Malefyt R, Moore KW (2002) A receptor for the heterodimeric cytokine IL-23 is composed of IL- 12Rbeta1 and a novel cytokine receptor subunit IL-23R. J Immunol 168:5699–5708
Park IK, Shultz LD, Letterio JJ, Gorham JD (2005) TGF-beta1 inhibits T-bet induction by IFN-gamma in murine CD4+ T cells through the protein tyrosine phosphatase Src homology region 2 domain-containing phosphatase-1. J Immunol 175:5666–5674
Paulos CM, Carpenito C, Plesa G, Suhoski MM, Varela-Rohena A, Golovina TN, Carroll RG, Riley JL, June CH (2010) The inducible costimulator (ICOS) is critical for the development of human T(H)17 cells. Sci Transl Med 2:55ra78
Pedotti R, Farinotti M, Falcone C, Borgonovo L, Confalonieri P, Campanella A et al (2009) Allergy and multiple sclerosis: a population-based case-control study. Mult Scler 15:899–906
Peng X, Jin J, Montes M, Sujkowski D, Tang Y, Smrtka J, Vollmer T, Singh I, Markovic-Plese S (2006) Immunomodulatory effects of 3-hydroxy-3-methylglutaryl coenzyme-A reductase inhibitors, potential therapy for relapsing remitting multiple sclerosis. J Neuroimmunol 178:130–139
Ponomarev ED, Shriver LP, Maresz K, Pedras-Vasconcelos J, Verthelyi D, Dittel BN (2007) GM-CSF production by autoreactive T cells is required for the activation of microglial cells and the onset of experimental autoimmune encephalomyelitis. J Immunol 178:39–48
Qin S, Rottman JB, Myers P, Kasam N, Weinblatt M, Loetscher M, Koch AE, Moser B, Mackay CR (1998) The chemokine receptors CXCR3 and CCR5 mark subsets of T cells associated with certain inflammatory reactions. J Clin Invest 101:746–754
Racke MK, Bonomo A, Scott DE, Cannella B, Levine A, Raine CS, Shevach EM, Rocken M (1994) Cytokine-induced immune deviation as a therapy for inflammatory autoimmune disease. J Exp Med 180:1961–1966
Racke MK, Burnett D, Pak SH, Albert PS, Cannella B, Raine CS, McFarlin DE, Scott DE (1995) Retinoid treatment of experimental allergic encephalomyelitis. IL-4 production correlates with improved disease course. J Immunol 154:450–458
Rivers RM, Spunt DH, Berry GP (1933) Observations on attempts to produce acute disseminated encephalomyelitis in monkeys. J Exp Med 58:39–53
Roquer J, Escudero D, Herraiz J, Maso E, Cano F (1987) Multiple sclerosis and Hashimoto’s thyroiditis. J Neurol 234:23–24
Rottman JB, Smith T, Tonra JR, Ganley K, Bloom T, Silva R, Pierce B, Gutierrez-Ramos JC, Ozkaynak E, Coyle AJ (2001) The costimulatory molecule ICOS plays an important role in the immunopathogenesis of EAE. Nat Immunol 2:605–611
Sallusto F, Lenig D, Mackay CR, Lanzavecchia A (1998) Flexible programs of chemokine receptor expression on human polarized T helper 1 and 2 lymphocytes. J Exp Med 187:875–883
Shinohara ML, Jansson M, Hwang ES, Werneck MK, Glimcher LH, Cantor H (2005) T-bet-dependent expression of osteopontin contributes to T cell polarization. Proc Natl Acad Sci U S A 102:17101–17106
Skurkovich S, Boilo A, Beliaeva I, Buglak A, Alekseeva T, Smirnova N, Kulakova O, Tchechonin V, Gurova O, Deomina T, Favorova OO, Skurkovic B, Gusev E (2001) Randomized study of antibodies to IFN-gamma and TNF-alpha in secondary progressive multiple sclerosis. Mult Scler 7:277–284
Sloka S (2002) Observations on recent studies showing increased co-occurrence of autoimmune diseases. J Autoimmun 18:251–257
Smith KM, Guerau-de-Arellano M, Costinean S, Williams JL, Bottoni A, Mavrikis Cox G, Satoskar AR, Croce CM, Racke MK, Lovett-Racke AE, Whitacre CC (2012) miR-29ab1 deficiency identifies a negative feedback loop controlling Th1 bias that is dysregulated inmultiple sclerosis. J Immunol 189(4):1567–1576. doi: 10.4049/jimmunol.1103171. (Epub 2012 Jul 6)
Sporici RA, Beswick RL, von Allmen C, Rumbley CA, Hayden-Ledbetter M, Ledbetter JA, Perrin PJ (2001) ICOS ligand costimulation is required for T-cell encephalitogenicity. Clin Immunol 100:277–288
Sporici R, Issekutz TB (2010) CXCR3 blockade inhibits T-cell migration into the CNS during EAE and prevents development of adoptively transferred, but not actively induced disease. Eur J Immunol 40:2751–2761
Steiner DF, Thomas MF, Hu JK, Yang Z, Babiarz JE, Allen CD, Matloubian M, Blelloch R, Ansel KM (2011) MicroRNA-29 regulates T-box transcription factors and interferon-γ production in helper T cells. Immunity 36:169–181
Szabo SJ, Kim ST, Costa GL, Zhang X, Fathman CG, Glimcher LH (2000) A novel transcription factor, T-bet directs th1 lineage commitment. Cell 100:655–669
Szabo SJ, Sullivan BM, Stemmann C, Satoskar AR, Sleckman BP, Glimcher LH (2002) Distinct effects of T-bet in Th1 lineage commitment and IFN-γ production in CD4 and CD8 T cells. Science 295:338–342
Tan AH, Goh SY, Wong SC, Lam KP (2008) T helper cell-specific regulation of inducible costimulator expression via distinct mechanisms mediated by T-bet and GATA-3. J Biol Chem 283:128–136
Traugott U, Lebon P (1988) Multiple sclerosis: involvement of interferons in lesion pathogenesis. Ann Neurol 24:243–251
Tzartos JS, Friese MA, Craner MJ, Palace J, Newcombe J, Esiri MM, Fugger L (2008) Interleukin-17 production in central nervous system-infiltrating T cells and glial cells is associated with active disease in multiple sclerosis. Am J Pathol 172:146–155
Vartanian T, Li Y, Zhao M, Stefansson K (1995) Interferon-gamma-induced oligodendrocyte cell death: implications for the pathogenesis of multiple sclerosis. Mol Med 1:732–743
Veldhoen M, Hocking RJ, Atkins CJ, Locksley RM, Stockinger B (2006) TGFbeta in the context of an inflammatory cytokine nilieu supports de novo differentiation of IL-17-producing T cells. Immunity 24:179–189
Waldburger KE, Hastings RC, Schaub RG, Goldman SL, Leonard JP (1996) Adoptive transfer of experimental allergic encephalomyelitis after in vitro treatment with recombinant murine interleukin-12. Preferential expansion of interferon-gamma-producing cells and increased expression of macrophage-associated inducible nitric oxide synthase as immunomodulatory mechanisms. Am J Pathol 148:375–382
Wen ST, Liu GJ, Feng RN, Gong FC, Zhong H, Duan SR, Bi S (2012) Increased levels of IL-23 and osteopontin in serum and cerebrospinal fluid of multiple sclerosis patients. J Neuroimmunol 244:94–96
Willenborg DO, Fordham S, Bernard CC, Cowden WB, Ramshaw IA (1996) IFN-gamma plays a critical down-regulatory role in the induction and effector phase of myelin oligodendrocyte glycoprotein-induced autoimmune encephalomyelitis. J Immunol 157:3223–3227
Wilson NJ, Boniface K, Chan JR, McKenzie BS, Blumenschein WM, Mattson JD, Basham B, Smith K, Chen T, Morel F, Lecron JC, Kastelein RA, Cua DJ, McClanahan TK, Bowman EP, de Waal Malefyt R (2007) Development, cytokine profile and function of human interleukin 17-producing helper T cells. Nat Immunol 8:950–957
Yang L, Anderson D, Baecher-Allan C, Hastings WD, Bettelli E, Oukka M, Kuchroo VK and H (2008a) Il-21 and TGF-beta are required for differentiation of human T(H)17 cells. Nature 454:350–352
Yang L, Anderson DE, Kuchroo VK, Hafler DA (2008b) Lack of TIM-3 immunoregulation in multiple sclerosis. J Immunol 180:4409–4414
Yang Y, Weiner J, Liu Y, Smith AJ, Huss DJ, Winger R, Peng H, Cravens PD, Racke MK, Lovett-Racke AE (2009) T-bet is essential for encephalitogenicity of both Th1 and Th17 cells. J Exp Med 206:1549–1564
Yao Z, Painter SL, Fanslow WC, Ulrich D, Macduff BM, Springs MK, Armitage RJ (1995) Human IL-17: a novel cytokine derived from T cells. J Immunol 155:5483–5486
Yi-qun Z, Joost van Neerven RJ, Kasran A, Boer M de, Ceuppens JL (1996) Differential requirements for co-stimulatory signals from B7 family members by resting versus recently activated memory T cells towards soluble recall antigens. Int Immunol 8:37–44
Yura M, Takahashi I, Serada M, Koshio T, Nakagami K, Yuki Y, Kiyono H (2001) Role of MOG-stimulated Th1 type “light up” (GFP+) CD4+ T cells for the development of experimental autoimmune encephalomyelitis (EAE). J Autoimmun 17:17–25
Zhang GX, Yu S, Gran B, Li J, Siglienti I, Chen X, Calida D, Ventura E, Kamoun M, Rostami A (2003) Role of IL-12 receptor beta 1 in regulation of T cell response by APC in experimental autoimmune encephalomyelitis. J Immunol 171:4485–4492
Zheng W, Flavell RA (1997) The transcription factor GATA-3 is necessary and sufficient for Th2 cytokine gene expression in CD4 T cells. Cell 89:587–596
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2013 Springer Science+Business Media New York
About this chapter
Cite this chapter
Lovett-Racke, A., Racke, M. (2013). T-bet: A Critical Regulator of Encephalitogenic T Cells. In: Yamamura, T., Gran, B. (eds) Multiple Sclerosis Immunology. Springer, New York, NY. https://doi.org/10.1007/978-1-4614-7953-6_3
Download citation
DOI: https://doi.org/10.1007/978-1-4614-7953-6_3
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4614-7952-9
Online ISBN: 978-1-4614-7953-6
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)