Abstract
Introduced for use in diagnosis in the mid-1980s, magnetic resonance imaging (MRI) has evolved into the leading modality for use in neurosurgery treatment. The first iMRI system for use in neurosurgery was an open access MRI scanner (SIGNA SP, General Electric Medical System, Milwaukee, WI) codeveloped by GE and investigators of the Brigham and Women’s Hospital at Harvard Medical School that incorporated several concepts and objectives of intraoperative guidance that have since been widely adopted. With the development of higher-field magnets, we are able to achieve excellent image quality and spatial resolution to depict the most exquisite details of the brain’s anatomy so that when MRI is used intraoperatively, it can provide clinicians with much information including an understanding of brain shift and deformations and even data on tissue temperature. Indeed, new MR sequence parameters allow for what modern neurosurgery requires and that is imaging of both brain morphology and function during surgery. Importantly, iMRI, though it entails a longer neurosurgical procedure time, offers a lower percentage of total complications compared to when it is not employed. Through the capabilities of modern MRI technology, IMRI enables and will continue to enable new therapeutic methods like MRI-guided thermal ablations and image-guided robotic tools. With the clinical introduction of these advances, iMRI is rapidly changing the practice of neurosurgery as is seen, in part, by the fact that, today, more than 100 iMRI systems are in use for neurosurgical guidance worldwide.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Diffusion Tensor Imaging
- Nonrigid Registration
- Brain Shift
- Navigational System
- Multiparametric Magnetic Resonance Imaging
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Introduction
Since its introduction for diagnosis in the mid-1980s, magnetic resonance imaging (MRI) has evolved into the leading neuroimaging modality. With the development of higher-field magnets, we are able to achieve excellent image quality and spatial resolution to depict the most exquisite details of the brain’s anatomy. Similarly, the implementation of intraoperative MRI (iMRI) in the early 1990s [1, 2] has had a major impact on the practice of neurosurgery. The first iMRI system was an appropriately configured open access MRI scanner (SIGNA SP, General Electric Medical System, Milwaukee, WI) [3] codeveloped by GE and investigators of the Brigham and Women’s Hospital at Harvard Medical School that incorporated several concepts and objectives of intraoperative guidance that have since been widely adopted. First, it represented the very first attempt to overcome the limitation of traditional neurosurgical navigational systems that use diagnostic preoperative images by enabling the use of intraoperative images that account for brain shifts and deformations. Using iMRI in 3D, structural data can be updated intraoperatively to reflect dynamic anatomical conditions that occur during surgery. Second, in addition to providing access to the patient’s exposed anatomy, iMRI provided the neurosurgeons 3D visualization beyond the exposed surfaces and showed the target lesions deep within the brain. Third, it offered a more sensitive method meaning MRI-based tissue characterization that, compared with direct visualization, allowed for the distinguishing of diseased from normal tissue and, given this, provided the first reliable means of intraoperatively assessing the extent of resection. Finally, MRI allowed one to monitor and detect temperature and tissue changes during thermal ablations such as MRI-guided interstitial laser therapy (ILT) and MRI-guided focused ultrasound surgery (MRgFUS) [4, 5]. The growing preliminary evidence suggests that MRI guidance greatly improves the safety and effectiveness of neurosurgical procedures [6, 7].
Therefore, with the introduction of iMRI, new therapeutic methods like MRI-guided thermal ablations and image-guided robotic tools could be implemented. For example, MRgFUS, among the most promising new therapeutic approaches, is based upon the noninvasive thermal ablation of tumors. Introduced after the successful implementation of MRI-guided ILT of brain tumors, MRgFUS uses MRI guidance to monitor and control the thermal coagulation process and robotic tools to run the hardware that delivers treatment [8–13]. With the clinical introduction of these advances, iMRI is rapidly changing the practice of neurosurgery and, in fact, today, with more than 100 iMRI systems in use for neurosurgical guidance worldwide, it can be concluded that, despite its substantial cost, iMRI is well accepted and embraced by neurosurgery [14].
In modern neurosurgery there is a growing need for imaging of both brain morphology and function during surgery. To achieve this, imaging must be comprehensively integrated with surgery and the various components of the operating environment. The combination of advanced neuronavigation, 3D multimodality image fusion, and iMRI can fulfill the promise of an integrated image-guidance system for neurosurgery. Successful integration entails the introduction of interactive dynamic MR imaging, high-performance computing, and real-time image processing in the operating room. Novel iMRI-based imaging techniques are being aggressively developed and tested for their diagnostic and clinical utility so they can be applied to several revolutionary image-guided therapy methods that are currently being explored and that will eventually be incorporated into routine neurosurgical practice.
Fundamentals of Image-Guided Neurosurgery
The fundamental principle of image-guided neurosurgery is to localize, target, access, and remove intracranial lesions without injuring functional brain tissue or blood vessels. Image guidance not only can assist with localization and trajectory optimization but also allow for the assessing of the extent of resection during surgery.
Early work with brain stereotaxis established the importance and value of image guidance through better determination of tumor margins, localization of lesions, and optimization of targeting. Given that the use of frame-based and frameless stereotaxy based on 2D and 3D preoperative images improved localization of lesions but could not compensate for the intraoperative shifts and deformations that decrease accuracy, today, in current practice, computer-assisted, image-guided surgery has replaced stereotactic neurosurgery [15, 16].
Due to brain shifts and deformations, surgical manipulations result in an often unpredictable change in intracranial anatomy. Cerebrospinal fluid (CSF) leakage, hyperventilation, anesthetics, osmotic agents, and retraction and resection of tissue all contribute to brain shift to make preoperatively acquired images increasingly unreliable over the course of an operation and, therefore, navigation based on the preoperative images also less reliable. Intraoperative imaging, by updating the changes of brain anatomy, can enable correct localization and targeting [17, 18]. For example, iMRI not only updates the continuously changing spatial coordinates but also provides interactive and dynamic imaging, an essential component of an image-guided therapy system. Interactive iMRI guidance with dynamic imaging tools allows accurate localization and targeting and trajectory optimization and the avoidance of functionally critical tissues. IMRI-based navigation updates the preoperative diagnostic studies in a way that can be used to refine the surgical approach. Consequently, iMRI has become an important technical method for intraoperative surgical decision-making and a tremendous help to recognize acute surgical complications.
Since its introduction, iMRI has evolved from research modality to a routinely used, clinically accepted technique that improves the outcome and safety of neurosurgery. The continuously increasing number of neurosurgical iMRI systems throughout the world have been used most commonly to monitor tumor resection [19, 20]. The success of image-guided tumor resection relies largely on the ability of MRI to distinguish between normal and abnormal brain tissue and to detect residual tumor. MRI’s image quality and its sensitivity and specificity allow the surgeon to define the limits of tumor detection. Hence, an increasing number of neurosurgical iMRI systems are at a high field (1.5 or 3 T) and equipped with advanced imaging technology.
Detection of Tumor Boundaries
The preservation of neurological function requires precise definition of functional anatomy and tumor margins. During surgery, it is difficult to distinguish infiltrating malignant tumors from the normal brain tissue. Because of the difficulty in recognizing exact tumor margins, complete resection is often difficult to achieve. Surgical decision-making based on the knowledge of tumor distribution is especially important for glioma surgery. The success of surgery is judged postoperatively based on MRI, and this postoperative MRI is also necessary for planning adjuvant treatment including radiation therapy and chemotherapy as well as emerging approaches such as ablative treatments and noninvasive drug delivery. Improved tumor definition, therefore, has significantly affected outcomes.
Today, the main issue in iMRI is: How confidently can we rely on advanced imaging methods—i.e., tissue characterization by multiparametric MRI to accurately define the full extent of low- and high-grade glial tumors? The current standard imaging approach to brain tumors is mostly based on multiparametric MRI. However, there is limited evidence that correlates radiographic studies with image-registered tissue histopathology. Multiparametric MRI alone is not able to satisfactorily define the full extent of these tumors. It is especially difficult to rely exclusively on MRI if low amounts of tumor cells infiltrate healthy tissue, forming ill-defined tumor margins. For example, low-grade gliomas seldom enhance due to the lack of leaky tumor vessels and intact blood-brain barrier (BBB). The diffusely infiltrative nature of these tumors makes the assessment of tumor boundaries difficult. In the case of higher-grade gliomas, the central portion of the tumor usually contains abnormal tumor vessels with an open BBB that results in enhancement and better definition of the portion of the tumor served by leaky angiogenic vessels. However, tumor cells infiltrate beyond the enhancing margins within the surrounding peritumoral edema that cannot be distinguished from the tumor-infiltrated tissue [21, 22]. Diffusion parameters may also be helpful, however, but they have not been definitively validated against the tumor content of the tissue [23, 24]. The introduction of tumor-detecting molecular imaging agents may provide improvement over the ambiguity of MRI if the agents have high specificity and sensitivity that can be determined only by the validation of images.The use of contrast agents and pharmacokinetic parameters derived from dynamic contrast enhancement (DCE) defines only the part of the tumor that has high-density tumor vessels due to angiogenesis [25]. This tumor component is well defined by perfusion imaging and can be removed surgically or destroyed by high-dose radiation or heat. The main problem is not to define this angiogenetic component but to detect low-density tumor infiltration of normal tissue where there is no angiogenesis and no detectable enhancement. This scenario is encountered in low-grade glioma that can only be imaged with increased T2 relaxation due to the lack of enhancement. Accurate imaging of low-grade gliomas is essential for carrying out surgical resection. Resection of low-grade glioma improves survival by relieving mass effect, decreasing the likelihood of seizure, and reducing the pool of cells capable of undergoing malignant transformation. In more malignant, higher-grade glioma, such as glioblastoma multiforme (GBM), there are also non-enhancing low-tumor-density components that are surrounded by or interspersed with the enhancing tumor part that results in tumor heterogeneity and difficulty in correctly defining the extent of the tumor. This low-density tumor infiltrated with prolonged T2 relaxation coexists with edematous or normal-appearing tissue that is still functioning; if the area of infiltrated brain is involved with important neurologic functions, then it cannot safely be removed surgically or destroyed by radiation or ablation, and it can be treated only with lower-dose radiation or with chemotherapy.
Real-time or iterative iMRI first introduced by us has guided over 3,000 surgical and interventional procedures at the BWH. Those procedures, among others, included more than 1,000 open brain craniotomies [26]. Coupled with new therapy devices and surgical navigation, these systems took on a pivotal role in opening new directions in the surgical management of glioma. We have learned that the identification of tumor margins is essential and that MRI, while necessary, is insufficient to be used as a single modality for this role.
New imaging methods based on MRI and positron emission tomography (PET) can be employed in various stages of disease to detect the presence or biological activity of the tumor cells. The basic assumption for imaging of tumors is that changes in imaging findings represent the biological activity of the tumor. However, conventional imaging strategies can be nonspecific and at best offer a rough approximation of tumor size and grade. For management of individual patients, the combination of advanced imaging techniques such as PET, cerebral blood volume (CBV) assessment with perfusion-weighted MRI, and diffusion MRI might offer more reliable assessment. MRI techniques are able to assess changes in metabolic tissue profile, tissue blood perfusion, microvessel permeability, and water mobility that are biomarkers for pathophysiological and microstructural changes. The amount of hyperperfusion is a marker of the biological behavior and aggressiveness of the tumor, and the estimated relative CBV is a semiquantitative parameter that correlates with the amount of capillaries (angiogenesis). The use of diffusion tissue signatures can delineate the margin of tumors better than conventional imaging and can differentiate regions of gross tumor from regions of tumor infiltration. Such a technique could contribute to targeting specific treatment modalities to the sites of greatest tumor burden and by guiding the optimal combination of treatment options in an individual patient. However, determining the utility of these techniques will depend on a rigorous evaluation of the relation imaging features with tumor histopathology or patient outcomes. Molecular imaging, optical imaging, and other new technologies like mass spectrometry and Raman spectroscopy may complement iMRI in the future and provide better distinction between normal and tumor-infiltrated brain [27–30].
For most patients with malignant brain tumors, neurosurgery is a key component of treatment that should be complemented with other treatment modalities like radiation therapy, radiosurgery, chemotherapy, or targeted drug delivery. Neurosurgical resection decreases mass effect and consequent neurologic deficits, provides tissue samples for pathologic diagnosis, and maximizes the benefit of adjuvant treatments. Nevertheless, successful treatment of patients with primary brain tumors, even when gross total resection is achieved, is limited because surgery is not able to address the infiltrative portion of the tumor. Moreover, targeting of radiation therapy is uncertain since, if the full limits of tumor cannot be defined by conventional imaging, chemotherapy delivery is limited by the intact BBB at the infiltrative portion of the tumor. Thus, even with the therapeutic triad of maximal surgical excision, radiation therapy, and chemotherapy, the prognosis for most patients with primary brain tumors remains poor.Maximal tumor resection, when it can be achieved without increasing neurologic morbidity, improves prognosis for patients with primary brain tumors. Low-grade glioma patients who underwent partial resection have had almost five times higher risk of death than patients who underwent gross total resection. In high-grade gliomas, the extent of resection is also an important prognostic factor. The addition of advanced structural and functional data to conventional imaging and neuronavigation can help surgeons with intraoperative decision-making regarding whether or not to resect tissue. The addition of presurgical diffusion tractography (DTI) to neuronavigation has been found to increase tumor resection and survival and decrease neurologic morbidity [31–34].
The majority of malignant gliomas recur within 2 cm of the enhancing edge of the original tumor making the delineation of the tumor margins particularly critical to inform clinical decision-making. The development of techniques capable of accurately depicting tumor margins in vivo and, if possible, intraoperatively is important for the determination of the optimal resection strategy that maximizes resected tumor while avoiding injury to adjacent brain.
Detection of Intraoperative Complications
Brain surgeries can be carefully planned and then executed under MRI guidance that, in turn, minimizes the surgical exposure and the related damage to the normal brain. The maximal preservation of normal tissue may contribute to decreased surgical morbidity. Specifically, iMRI can decrease surgical complications by identifying normal structures, such as blood vessels, white matter fiber tracts, and cortical regions with functional significance. However, intraoperative complications, such as hemorrhage, ischemia, or edema, are possible and can directly affect the outcome. A major advantage of iMRI is the rapid identification of intraoperative and postoperative complications, such as edema, hemorrhage, and ischemia [20, 35]. Diffusion-weighted imaging (DWI) can be used to exclude ischemia related to distal branch or perforator occlusion [36]. Early intraoperative detection of such changes may warrant their reversibility [37]. In summary, iMRI results in longer neurosurgical procedures but a lower percentage of total complications.
Surgical Planning and Decision-Making
The neurosurgeon should be able to precisely localize the target lesion, choose the optimal trajectory of approach, and, in the case of malignant brain tumors, accurately determine the margins of the tumor. Using advanced computing technologies, these surgical planning “steps” are now undertaken with an extraordinary degree of confidence and accuracy. Surgical planning based on MRI uses multimodality and multiparametric lesion characterization and includes the full depiction of the relevant anatomical structures and their related functions. The use of 3D multimodality image processing and display platforms, like the Slicer, (www.slicer.org) that has been developed in our Surgical Planning Lab [38], represents an enhancement and augmentation of the information provided by the acquired MRI slices alone. While data processing systems cannot change the diagnosis, they can change the approach to the data and maximize the information available from images. Slicer and other image processing and display platforms contribute substantially to surgical planning by providing additional information regarding (a) the selection of optimal craniotomy and corticotomy sites, (b) the definition of surgical excision margins, and (c) the optimization of access trajectories to the targeted tumors or other surgical lesions.
One of the most novel aspects of neurosurgical planning is the intraoperative use of the 3D models for interactive surgical decision-making. Surgical planning also includes various avoidance strategies in the proximity of the lesion to the sensory and motor tracts and deep brain structures (basal ganglia) and to essential vascular structures or cranial nerves. All the available and relevant anatomical and functional information should play a role in the construction of 3D models. Surgical planning is also linked to co-registration (multimodality fusion) and should be initiated before surgery but completed in the operating room with the registration of the 3D surgical planning model to the patient anatomy.
Computer-assisted surgical planning needs optimal image quality data with high spatial and contrast resolution; semiautomated or automated segmentation with identification of the lesion margins and the relevant anatomical structures, accurate 3D model generation from the segmented data, selective visualization and transparency transforms, and co-registration of multiple imaging modalities that involves registration to the patient anatomy using both rigid and nonrigid registration. The final goal of surgical planning and simulation is to incorporate these techniques into intraoperative image guidance [39], an integration that requires the nonrigid registration of the presurgical data (image space) to the patient (physical space) in surgery [40]. With computer-assisted navigational tools, the patient’s anatomy can be visualized in 2D or 3D representations in relationship to the position of tracked, handheld navigational instruments. Algorithms to deform the presurgical data, for example, to compensate for the shift of functional areas, are being tested but are not yet validated or applicable for routine use [41].
Current advances in MRI, specifically functional MRI (fMRI) and diffusion tensor imaging (DTI), significantly improve localization and targeting within the cortex (functional anatomy) and along deep white matter structures (connectivity). In addition, contrast-enhanced dynamic MRI and perfusion imaging, MR angiography (MRA), MR spectroscopy (MRS), and non-MRI methods like PET and the single photon emission computed tomography (SPECT) provide complementary physiologic and/or metabolic data, allowing further differentiation of brain tissue and improved characterization of brain tumors. The recognition of the advantages of multimodality imaging motivated the planning, construction, and current operation of the Brigham and Women’s Advanced Multimodality Image Guided Operating (AMIGO) suite that opened in 2011.
Multimodality and multiparametric model generation requires extensive image processing of the preoperative data from multiple sources as part of preoperative surgical planning. The same tasks can be performed before or during the procedure to support intraoperative surgical decision-making. The multiple data sets are aligned using a multimodal registration method based on the maximization of the inherent mutual information contained by the images originating from the same patient (Fig. 32.1).
Multimodal navigational data for preoperative planning. Tumor segmentation is performed to define the tumor boundaries and/or planned resection (a). Diffusion tensor imaging is added to define the relationship of the tumor to key fiber tracts (b). Functional MRI volumes are added to identify cortical regions that are responsible for motor function (c). All information is combined in a 3D model that can be used to plan a surgical approach (d)
Image acquisition and intraoperative image processing have improved steadily in recent years including a severalfold decrease in processing time that has resulted in increasingly sophisticated multimodality image fusion and nonrigid registration, although most methods are confined to rigid structures. Moreover, clinical experience with image-guided therapy in deep brain structures and with large resections has revealed the current limitations of existing rigid registration and visualization approaches.
Navigation and Interactive Dynamic Imaging
IMRI can aid surgical localization and targeting using interactive multiplanar imaging for intraoperative navigation. One of the initial premises of iMRI was to enable the surgeon to define the imaging plane needed for visualizing the area of interest. There has been significant emergence of interactive and dynamically adaptive imaging techniques in current MRI methods [42] that are primarily used in cardiac and interventional imaging when interactive image plane selection, catheter or probe tracking, and multiresolution imaging are absolutely necessary. These adaptive or dynamic imaging techniques will meet the requirements of real-time image guidance. Cross-referencing of the surgical view and the corresponding volumetric images is available from intraoperative navigational guidance systems. Today’s navigational systems cannot adjust the image-based models to the deformation and shift of brain structures during surgery. If this transformation can be done, it will result in a fundamental change in operating techniques with closer integration of image data into the surgical procedure.
As opposed to current navigational systems, iMRI does not require a frame of reference for transformation and registration. It is possible with iMRI to use direct image coordinates in localizing a lesion in 3D space; this approach also allows this localization to be updated in a dynamic fashion that has major implications on the ability to obtain accurate biopsies or correct resections of margins. Interactive use of MRI also allows for the selection of the optimal trajectories for various neurosurgical approaches [43].
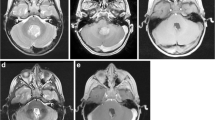
iMRI has a number of applications with specific requirements for dynamic MRI, particularly MRI fluoroscopy and for other real-time imaging methods. Most of these advanced techniques cannot be implemented on an “open” low- or midfield MR scanner and require extraordinary gradient performance or RF coil hardware parameters. With 2D fluoroscopic imaging capability, the surgeon can visually, or with computer assistance, guide and monitor therapy or surgery for greater effectiveness and safety. The most important applications that have specific requirements for dynamic MR are MR fluoroscopy, monitoring thermal therapies, catheter tip tracking, and monitoring the progress of surgical resections (Fig. 32.2).
The use of updated navigational data during surgery from iMRI. Tumor segmentation is performed (a) to plan the resection volume (b). When gross total resection has been carried out, iMRI is used to detect residual tumor. Residual tumor, segmented in red, (c) is used to create an updated navigational data set, including a segmented volume of residual tumor (d) which can be easily identified and removed
Magnet Configuration and Field Strength
Operating with interactive MRI guidance offers neurosurgeons several advantages over traditional stereotactic guidance systems. However, for most cases high spatial resolution is necessary, and only relatively high-field MRIs can produce images with superior resolution. Further, only completely open systems can offer optimal surgical access. Thus, magnet configuration and field strength require a compromise between image quality and accessibility.
Following the introduction of the first iMRI, which was designed explicitly for image-guided neurosurgery, several other groups began to utilize existing commercially available open and closed magnet configurations for neurosurgical guidance. Low- and midfield strength, horizontal, open and closed configuration, and higher-field magnets were placed in operating rooms or in interventional suites that were modified for the needs of neurosurgery [44–46]. The magnets, which were originally designed only for diagnostic imaging, were adapted to image guidance. Most of the efforts concerned the MR table that had to be either revised or redesigned to make it well suited for both brain surgery and MR imaging.
Using these primarily diagnostic MRI systems, the imaging paradigms are more or less constrained by the actual magnet configuration. In all versions, the surgical procedure has to be done outside the magnet. Since the head is not within the imaging volume, the table has to move or swing in and out from the magnet. To avoid major modification of the operating room equipment and to get around the need for table motion and moving the patients, two commercial magnets were introduced. In both solutions the magnet moves towards the head. The high-field (1.5 or 3 T) version (IMRIS, Winnipeg Canada) is ceiling mounted and placed in an adjacent room, allowing the use of non-MRI-compatible instruments. During imaging sessions, the MRI is pulled around to the operating room table [47]. The small, low-field (0.12 T) magnet (PoleStar N20 iMRI system, Medtronic Navigation, Louisville, Colorado) is mounted to the regular operating room table. It is partially open like the “double doughnut” design in that a gap allows the magnet to slide around the head when imaging is needed [46, 48].
As far as field strength is concerned, these two magnet designs represent the two diverging directions in iMRI: It is obvious that the higher the field, the better the image quality, but the lower-field solution is less costly and more adaptable to the operating room environment. The high-field magnet offers more advanced imaging sequences, and the image is acquired much faster. At the lower field, there are fewer problems with safety and compatibility. Midfield magnets offer some compromise, but finding the middle ground may not be acceptable for either side. Today, most neurosurgeons prefer higher magnetic field strength and including advanced neuroimaging capabilities. Besides higher spatial and temporal resolution, the higher field offers the advantages of high image quality and low signal-to-noise. Most neurosurgeons would like to generate and use high-resolution images intraoperatively. Advocates of low-field iMRI believe that the relatively low-quality images are still sufficient to delineate tumor and detect brain shifts and deformations. One solution is nonrigid registration of the preoperative high-field images to the intraoperative low- or midfield intraoperative data that would assure lower-cost intraoperative imaging with high-quality preoperatively obtained information that can be used for procedure guidance. Instead of a preoperative MRI, any other cross-sectional image can be registered to intraoperative images. Multimodality guidance using not only multiple MRI-derived data but also PET, CT, and magnetoencephalogram (MEG) images can be fused and integrated into the surgical navigation system—so-called multimodality navigation [43].
Field strength is not the only criteria when choosing magnet type. The flexibility in patient positioning and the surgeons’ mobility are also critical; this is the main reason neurosurgeons are unyielding about using full-feature operating room tables. Good positioning of the head is critical for brain surgery, and the use of surgical microscopes is also essential. These factors all influence the choice of imaging paradigms and the future design and ergonomics of image-guided operating rooms.
Intraoperative Navigation
In current neurosurgical practice, the localization of a brain lesion and the surrounding anatomy relies exclusively upon anatomic landmarks, preoperative image data, and intraoperative electrophysiological measurements. Although preoperative image data can be used for surgical planning and intraoperative navigational guidance, the use of this information is limited because of the unavoidable deformation of the brain during surgery. iMRI can resolve this problem if appropriate navigational tools are implemented [43]. By using advanced computer technology, neurosurgery can overcome the limitations of frame-based systems. Frameless, computer-assisted navigational systems benefit from image-processing methods such as segmentation, registration, and interactive display in 2D and in 3D. Using various image-processing methods, a computer-based model of the brain can be generated, and within this model, structures can be highlighted.
The ultimate goal of iMRI is to combine preoperative and intraoperative image data into a comprehensive information package that is vital to accurate surgical decision-making. Indeed, this “data package” offers several benefits: with iMRI, images can be obtained at each stage of a surgical procedure, a process made easier if the system is set up without moving the patient, and the target lesion can be accurately localized; changes in the anatomy due to brain shift can be recognized; the relationship between the surgeon’s field of view and the image allow confirmation of the exact location; and serial images allow evaluation of the extent of excision and verify complete removal.
“Tracking” is the process by which interactive localization is achieved within the patient’s coordinate system. Methods of tracking include articulated arms, optical tracking, passive systems, sonic digitizers, and electromagnetic sensors. Active optical trackers use multiple video cameras to triangulate the 3D location of flashing light-emitting diodes (LEDs) that can be mounted on any surgical instrument. Passive tracking systems that do not use a power cable attached to the handheld localizer, work via a video camera (or multiple video cameras) that localizes markers that have been placed on surgical instruments. Active and passive vision localization systems require at least a partial line of sight between the landmarks or emitters and imaging sensor at all times when an object is tracked. Electromagnetic digitizers operate without such restrictions and, further, can track instruments (catheters, flexible endoscopes) when their tips are inside the body and out of view. An ideal iMRI system combines MRI imaging with interactive localization of the surgical instruments, intraoperative displays, and computer workstations. The 3D model of the patient must correlate directly to the actual images. The tracked probe enables the physician to depict the position of the probe relative to the segmented structures and the original scan. The surgeon is thus equipped with an augmented view of the surgical field relative to the entire anatomical model of the patient.
Images can be obtained intraoperatively in a serial fashion to provide image updates about the changing brain anatomy. Serial imaging, however, is extremely time-consuming, and time is a critical factor for surgery. Imaging not only interrupts the flow of surgeries but also adds substantial extra nonsurgical time to the overall duration of the procedure. Surgeons are, therefore, motivated to minimize imaging, yet at the same time they need accurate guidance. These two competing concerns result in a compromise that eventually determines the actual number of imaging sessions. It is undecided how much information is needed to correct intraoperative shifts and deformations and how often data acquisitions should take place. If intraoperative shifts follow a predictable course, computer-based simulation and biomechanical modeling would help to reduce the need for frequent image updates. At present, neither the knowledge of the biomechanical properties of the brain nor the capabilities of computer simulations are sufficient to adequately predict the various deformation patterns during surgery; therefore, the use of this adaptive model is limited.
Only frequent or even continuous volumetric imaging can guarantee accurate and real-time image guidance. Although MRI provides more information about brain morphology, other imaging modalities, such as stereo video systems, laser surface scanning devices, ultrasound, and CT, can also be used during surgery to reveal the changing anatomy. With its high temporal resolution, portability, and lack of ionizing radiation, ultrasound has potential advantages over other existing imaging modalities for intraoperative monitoring, yet ultrasound is rarely used during neurosurgery largely because of the craniotomy requirement to achieve sufficiently useful signals. Prompted by results from recent studies on transcranial MRgFUS, a prototype device that uses the shear mode of transcranial ultrasound transmission for intraoperative monitoring was designed, constructed, and tested with ten human participants. For validation, MRI images were then obtained with the device spatially registered to the MRI reference coordinates [49]. This method could be used to reduce the need for frequent MR image updates, and it can signal a significant degree of shift that indicates new volumetric updates.
In the future, we can use a series of imaging methods and processing algorithms to predict intraoperative changes during neurosurgery. Real-time, automated segmentation methods will provide updated 3D models of the brain [17, 40, 50, 51]. The combination of rigid and nonrigid registration methods, active surface matching techniques, and the application of biomechanically more accurate models of brain deformation will eventually help to decrease the sampling rate needed for the full appreciation of changing brain anatomy during surgery. If a sufficiently accurate biomechanical model exists, the volumetric deformation field can be computed and used for intraoperative modeling.
Clinical Applications
Glioma Surgery
IMRI in glioma surgery can optimize the extent of resection. It has been suggested by several iMRI users that iMRI guidance leads to a higher rate of complete tumor removal, but this is not based on enough scientific evidence. Recently, the first prospective, randomized trial clearly shows that, compared with conventional navigation based on preoperative data, more patients in the iMRI group had complete tumor resection (23 [96 %] of 24 patients) than the patients did in the control group (17 [68 %] of 25,) [7]. Percentages of final tumor volume were significantly reduced in both low-grade (10.3 ± 11.5 % versus 25.8 ± 16.3 %) and high-grade gliomas (5.4 ± 9.9 % versus 19.5 ± 13.0 %). Complete resection was achieved in 36.2 % of all patients (low grade, 57.1 %; high grade, 27.3 %). It is important to note that the introduction of high-field iMRI in conjunction with functional navigation significantly increased the extent of resection without an increase in postoperative neurological deficits [52].
The resection of primary GBM with iMRI guidance also results in a more complete removal of the tumor compared with conventional surgical techniques; also, the overall surgical morbidity is low [53]. Despite extended resections, introduction of high-field iMRI in conjunction with functional navigation did not translate into an increased risk of postoperative deficits.
In the case of low-grade glioma, it is now generally accepted that the more complete the resection, the longer the survival [54]. Patients who underwent subtotal resection were at 1.4 times the risk of recurrence and at 4.9 times the risk of death relative to patients who underwent gross total resection [6]. IMRI-guided surgeries accomplish more extensive tumor removal, but in functionally critical anatomical regions, complete resection is often not possible and tumor cells with later potential malignant transformation may remain. Tumor involvement of the following structures is usually associated with incomplete resection: corpus callosum, corticospinal tract, insular lobe, middle cerebral artery, motor cortex, language cortex and associated white matter fibers, optic radiations, visual cortex, and basal ganglia [55]. In these cases when complete resection is not possible, iMRI still helps to accomplish a well-executed surgical plan that avoids the abovementioned eloquent areas. The combination of anatomical and functional imaging (primarily perfusion, DTI, and fMRI) is an essential part of current surgical planning and helps to define the target that can be safely resected [56, 57]. For surgeons to have optimal intraoperative information concerning white matter anatomy, a platform has been developed that allows the intraoperative real-time querying of DTI data sets during frameless stereotactic neuronavigation [33].
Extra-axial Tumors
One of the great successes of iMRI-guided neurosurgery is transsphenoidal pituitary surgery where MR images are taken at the end of surgery to verify complete removal. iMRI helps to overcome the limitations in direct visualization and enables surgeons to perform such procedures with fewer complications and with more gross total resection [58, 59]. On larger iMRI series there were other benign tumors like meningioma and chordoma [20, 60], but there are not enough conclusive data to assess the use of iMRI in skull base surgery. Skull base tumor surgery is difficult due to the complex and narrow surgical window. Complex skull base surgery appears to be an ideal field for iMRI especially if there is intraoperative shift of relevant structures. iMRI, especially with higher field strength, provides details of the related anatomy and demonstrates changes as the surgery progresses to allow intraoperative modification of the surgical strategy, which is especially useful for larger tumors like chordoma and craniopharyngioma [61, 62]. Combined with a navigation system, iMRI is extremely helpful to maximize the resection of skull base tumors and improve the safety of surgeries.
Other Applications
Applications of the iMRI to spine surgery may include intraoperative guidance for resection of spine and spinal cord tumors and trajectory planning for spinal endoscopy or fixation. iMRI provides accurate and rapid localization in these cases and makes surgeries and decompressions safer especially in the cervical spine [63–66].
Drainage of brain abscesses, cystic or necrotic intracranial lesions with subsequent aspiration, and the management of hydrocephalus can be performed safely and accurately by monitoring the procedure using real-time MR imaging to obtain immediate feedback on related dynamic tissue changes [67–69]. Neuroendoscopy and iMRI complement each other in complicated cases of hydrocephalus. iMRI images provide an updated data set, allowing accurate navigation of the endoscope [70].
iMRI-guided DBS (deep brain stimulation) not only assists targeting and improves accuracy for electrode placement but also may alert the surgeon to potential complications. DBS-related acute changes involving intracranial hemorrhage and air can be seen without extraoperative follow-up imaging, precluding the need for CT examinations [71].
MR-Compatible Robots for Neurosurgery
The concept of 3D image guidance is above all relevant to the control of robotic systems, because the robot requires a well-defined 3D coordinate system to establish its correct motion path. Determination of motion path from near real-time images has not yet been accomplished for most surgical robots, but it is one of the most promising areas of research and development in modern neurosurgery. The Boston iMR-compatible robotic system that was integrated with the Signa SP iMRI was capable of obtaining biopsies and performing simple multitrajectory tasks [72, 73]. The main role for a surgical robot would be to navigate and manipulate needles and other small surgical tools to reach to the target regions with pinpoint accuracy. Therefore, this robot is designed not to block the neurosurgeon’s access to the patient but to maintain the space for the surgeon. In this MRI-integrated robot, the main body of the robot is placed above the surgeon’s head. Two long rigid arms reach to the patient, and a tool holder is attached at the end of the arm. It was demonstrated that the motion of the robot did not cause loss of image quality or pose a safety risk in the MR environment.
The University of Calgary, in collaboration with a space robotics company, has begun construction of an MR-compatible, ambidextrous master–slave robot: the neuroArm [74, 75]. MR compatibility is accomplished with the use of ceramic motors. Its speed of movement and full suite of microsurgical instruments will allow it to perform a broad spectrum of microsurgical procedures outside the closed-bore magnet. No such restrictions will apply to open MR systems. It is anticipated that the tremor filtration and motion scaling of surgical robots will allow neurosurgeons to exceed the limits of their own manual dexterity and conceivably permit procedures that currently are not attempted. The MR-compatible surgical robot was successfully developed and merged with iMRI at both 1.5 or 3.0 T. Image-guidance accuracy and microsurgical capability were established in preclinical trials. Early clinical experience demonstrated feasibility and showed the importance of a master–slave configuration.
Automatic alignment of real-time intraoperative images aids visualization using robots. The image-guided integrated systems can be used for planning and performing simple trajectory procedures—such as biopsies with robotic assistance under MRI guidance. The physician can interact with a planning interface to specify the set of desired trajectories based on anatomical structures and lesions observed in the patient’s MR images. All image-space coordinates are automatically computed and used to position a needle guide or a surgical instrument holder [76].
Cost-Effectiveness
Irrespective of the iMRI system used, operative time and operating room usage increase with the use of iMRI. The true value of iMRI is in the reduction of the need for reoperation both due to complications that could have been detected intraoperatively and suboptimal surgical resection. Complications result in increased hospital stay, time off work, and institutionalization. The ability to acquire frequent updates during resection and the capability of accurate, effective navigation are worth the inconveniences of the limited space, restrictions in positioning, and limited imaging time. Surgical strategies can be reevaluated, if warranted, by serially updated information and surgical procedures can be altered based upon the additional information.
First introduced in 1993, iMRI has since been generally accepted as a valuable image-guidance tool for neurosurgery, but it still applies relatively immature and very diverse technologies; its clinical indications are not well defined and its potential impact on everyday neurosurgical practice is not yet fully realized. The reason for the limited acceptance is that it is not a so-called disruptive technology that necessitates the total transformation of a medical specialty. It has been easy to accept intraoperative guidance by MRI because it uses the same imaging modality for localization during surgery as it does for preoperative diagnosis. It also improves the now universally used intraoperative navigation by real-time interactive and near real-time imaging with frequent volumetric updates but does not change the fundamentals of navigational assistance. The only game changer is that iMRI can compensate for the unavoidable intraoperative deformations and brain shifts, making it advantageous over traditional navigational guidance but not a disruptive step that eliminates a procedure.
The main reason for the relatively slow proliferation of iMRI technology is not necessarily the high cost but the lack of clear definition of the requirements of the various types of iMRI systems. Neither the configuration nor the field strength of the MRIs and their integration with the current conventional operating room environment and with multiple therapy devices have been determined yet. It is also unclear whether iMRI is applicable only for tumor resection control or if it is relevant for other neurosurgical procedures such as cerebrovascular or functional applications.
Conclusion
The surgical community has accepted the role of MR imaging in both diagnosis and therapy. Increasingly, minimally invasive procedures are viewed favorably, and there is a strong demand for their widespread implementation across numerous surgical disciplines that are aided by MRI in many critical ways. Nowhere is this demand more evident than in neurosurgery where advances in iMRI and computing technology have resulted in the beginning of a new and exciting era in the treatment of brain tumors.
Although neurosurgery has combined imaging with various surgical methods, the full utilization of advanced imaging technology has not yet been accomplished. The current trend is focused on the creation of integrated therapy delivery systems in which advanced imaging modalities are closely linked with navigational systems and high-performance computing. Obviously, the operating room of the future will accommodate various instruments, tools, and devices that are attached to the imaging systems and controlled by image-based feedback. We are confident that these innovative technologies especially when applied in an integrated, multimodality imaging environment will produce a range of novel minimally invasive therapies for the brain.
One of the most important consequences of intraoperative image guidance has been the full transformation of traditional brain surgery into image-guided surgery. With more accurate and complete volumetric data, neurosurgeons should be able to operate more effectively and safely. Nevertheless, at this point, iMRI has not simplified the surgical workflow and appears to increase operative time. The improved distinction between normal and pathological tissue and the enhanced appreciation of the related anatomy by iMRI has not led yet into multiple novel approaches or overall reevaluation of current surgical strategies. It is anticipated, however, that the changes in surgical visualization and navigation will eventually change the practice of neurosurgery. As a direct consequence of improved image guidance, new surgical techniques, strategies, and approaches will be introduced into modern neurosurgical practice.
References
Jolesz FA, Blumenfeld SM. Interventional use of magnetic resonance imaging. Magn Reson Q. 1994;10:85–96.
Jolesz FA. Interventional and intraoperative MRI: a general overview of the field. J Magn Reson Imaging. 1998;8:3–7.
Schenck JF, Jolesz FA, Roemer PB, et al. Superconducting open-configuration MR imaging system for image-guided therapy. Radiology. 1995;195:805–14.
Jolesz FA, Talos IF, Schwartz RB, et al. Intraoperative magnetic resonance imaging and magnetic resonance imaging-guided therapy for brain tumors. Neuroimaging Clin N Am. 2002;12:665–83.
McDannold NJ, Jolesz FA. Magnetic resonance image-guided thermal ablations. Top Magn Reson Imaging. 2000;11:191–202.
Claus EB, Horlacher A, Hsu L, et al. Survival rates in patients with low-grade glioma after intraoperative magnetic resonance image guidance. Cancer. 2005;103:1227–33.
Senft C, Bink A, Franz K, Vatter H, Gasser T, Seifert V. Intraoperative MRI guidance and extent of resection in glioma surgery: a randomised, controlled trial. Lancet Oncol. 2011;12: 997–1003.
Jolesz FA. MRI-guided focused ultrasound surgery. Annu Rev Med. 2009;60:417–30.
Kettenbach J, Silverman SG, Hata N, et al. Monitoring and visualization techniques for MR-guided laser ablations in an open MR system. J Magn Reson Imaging. 1998;8:933–43.
Jolesz FA, Bleier AR, Jakab P, Ruenzel PW, Huttl K, Jako GJ. MR imaging of laser-tissue interactions. Radiology. 1988;168:249–53.
Bettag M, Ulrich F, Schober R, et al. Stereotactic laser therapy in cerebral gliomas. Acta Neurochir Suppl. 1991;52:81–3.
Kahn T, Bettag M, Ulrich F, et al. MRI-guided laser-induced interstitial thermotherapy of cerebral neoplasms. J Comput Assist Tomogr. 1994;18:519–32.
Hata NMP, Kettenbach J, Kikinis R, Jolesz FA. Computer-assisted intra-operative MRI monitoring of interstitial laser therapy in the brain: a case report. J Biomed Opt. 1998;3:304–11.
Colen RR, Kekhia H, Jolesz FA. Multimodality intraoperative MRI for brain tumor surgery. Expert Rev Neurother. 2010;10:1545–58.
Jolesz FA, Kikinis R, Talos IF. Neuronavigation in interventional MR imaging. Frameless stereotaxy. Neuroimaging Clin N Am. 2001;11:685–93, ix.
Kettenbach J, Wong T, Kacher D, et al. Computer-based imaging and interventional MRI: applications for neurosurgery. Comput Med Imaging Graph. 1999;23:245–58.
Nabavi A, Black PM, Gering DT, Westin CF, Mehta V, Pergolizzi RS, Ferrant M, Warfield SK, Hata N, Schwartz RB, Wells III WM, Kikinis R, Jolesz F. Serial intraoperative magnetic resonance imaging of brain shift. Neurosurgery. 2001;48:787–98; discussion 97–8.
Nimsky C, Ganslandt O, Cerny S, Hastreiter P, Greiner G, Fahlbusch R. Quantification of, visualization of, and compensation for brain shift using intraoperative magnetic resonance imaging. Neurosurgery. 2000;47:1070–9; discussion 9–80.
Black PM, Alexander 3rd E, Martin C, et al. Craniotomy for tumor treatment in an intraoperative magnetic resonance imaging unit. Neurosurgery. 1999;45:423–31; discussion 31–3.
Schwartz RB, Hsu L, Wong TZ, et al. Intraoperative MR imaging guidance for intracranial neurosurgery: experience with the first 200 cases. Radiology. 1999;211:477–88.
Konukoglu E, Clatz O, Bondiau PY, Delingette H, Ayache N. Extrapolating glioma invasion margin in brain magnetic resonance images: suggesting new irradiation margins. Med Image Anal. 2010;14:111–25.
Di Costanzo A, Scarabino T, Trojsi F, et al. Multiparametric 3T MR approach to the assessment of cerebral gliomas: tumor extent and malignancy. Neuroradiology. 2006;48:622–31.
Sadeghi N, D’Haene N, Decaestecker C, et al. Apparent diffusion coefficient and cerebral blood volume in brain gliomas: relation to tumor cell density and tumor microvessel density based on stereotactic biopsies. AJNR Am J Neuroradiol. 2008;29:476–82.
Price SJ, Jena R, Burnet NG, et al. Improved delineation of glioma margins and regions of infiltration with the use of diffusion tensor imaging: an image-guided biopsy study. AJNR Am J Neuroradiol. 2006;27:1969–74.
Law M, Cha S, Knopp EA, Johnson G, Arnett J, Litt AW. High-grade gliomas and solitary metastases: differentiation by using perfusion and proton spectroscopic MR imaging. Radiology. 2002;222:715–21.
Dimaio SP, Archip N, Hata N, et al. Image-guided neurosurgery at Brigham and Women’s Hospital. IEEE Eng Med Biol Mag. 2006;25:67–73.
Widhalm G, Wolfsberger S, Minchev G, et al. 5-Aminolevulinic acid is a promising marker for detection of anaplastic foci in diffusely infiltrating gliomas with nonsignificant contrast enhancement. Cancer. 2010;116:1545–52.
Agar NY, Golby AJ, Ligon KL, et al. Development of stereotactic mass spectrometry for brain tumor surgery. Neurosurgery. 2011;68:280–9; discussion 90.
Mohs AM, Mancini MC, Singhal S, et al. Hand-held spectroscopic device for in vivo and intraoperative tumor detection: contrast enhancement, detection sensitivity, and tissue penetration. Anal Chem. 2010;82(21):9058–65.
Chen X, Conti PS, Moats RA. In vivo near-infrared fluorescence imaging of integrin alphavbeta3 in brain tumor xenografts. Cancer Res. 2004;64:8009–14.
Nimsky C, Ganslandt O, Hastreiter P, et al. Preoperative and intraoperative diffusion tensor imaging-based fiber tracking in glioma surgery. Neurosurgery. 2007;61:178–85; discussion 86.
Kuhnt D, Bauer MH, Becker A, et al. Intraoperative visualization of fiber tracking based reconstruction of language pathways in glioma surgery. Neurosurgery. 2012;70:911–9; discussion 9–20.
Elhawary H, Liu H, Patel P, et al. Intraoperative real-time querying of white matter tracts during frameless stereotactic neuronavigation. Neurosurgery. 2011;68:506–16; discussion 16.
Golby AJ, Kindlmann G, Norton I, Yarmarkovich A, Pieper S, Kikinis R. Interactive diffusion tensor tractography visualization for neurosurgical planning. Neurosurgery. 2011;68:496–505.
Mamata Y, Mamata H, Nabavi A, et al. Intraoperative diffusion imaging on a 0.5 Tesla interventional scanner. J Magn Reson Imaging. 2001;13:115–9.
Sutherland GR, Kaibara T, Wallace C, Tomanek B, Richter M. Intraoperative assessment of aneurysm clipping using magnetic resonance angiography and diffusion-weighted imaging: technical case report. Neurosurgery. 2002;50:893–7; discussion 7–8.
Maier SE, Bogner P, Bajzik G, et al. Normal brain and brain tumor: multicomponent apparent diffusion coefficient line scan Imaging. Radiology. 2001;219:842–9.
Gering DT, Nabavi A, Kikinis R, et al. An integrated visualization system for surgical planning and guidance using image fusion and an open MR. J Magn Reson Imaging. 2001;13:967–75.
Risholm P, Golby AJ, Wells 3rd W. Multimodal image registration for preoperative planning and image-guided neurosurgical procedures. Neurosurg Clin N Am. 2011;22:197–206, viii.
Warfield S, Talos F, Tei A, Bharatha A, Nabavi A, Ferrant M, Black P, Jolesz F, Kikinis R. Real-time registration of volumetric brain MRI by biomechanical simulation of deformation during image guided neurosurgery. Comput Visual Sci. 2002;5:3–11.
Archip N, Clatz O, Whalen S, et al. Non-rigid alignment of pre-operative MRI, fMRI, and DT-MRI with intra-operative MRI for enhanced visualization and navigation in image-guided neurosurgery. Neuroimage. 2007;35:609–24.
Yutzy SR, Duerk JL. Pulse sequences and system interfaces for interventional and real-time MRI. J Magn Reson Imaging. 2008;27:267–75.
Nimsky C, Ganslandt O, Fahlbusch R. Functional neuronavigation and intraoperative MRI. Adv Tech Stand Neurosurg. 2004;29:229–63.
Fahlbusch R, Ganslandt O, Nimsky C. Intraoperative imaging with open magnetic resonance imaging and neuronavigation. Childs Nerv Syst. 2000;16:829–31.
Liu H, Hall WA, Martin AJ, Maxwell RE, Truwit CL. MR-guided and MR-monitored neurosurgical procedures at 1.5 T. J Comput Assist Tomogr. 2000;24:909–18.
Schulder M, Sernas TJ, Carmel PW. Cranial surgery and navigation with a compact intraoperative MRI system. Acta Neurochir Suppl. 2003;85:79–86.
Sutherland GR, Kaibara T, Louw D, Hoult DI, Tomanek B, Saunders J. A mobile high-field magnetic resonance system for neurosurgery. J Neurosurg. 1999;91:804–13.
Hadani M, Spiegelman R, Feldman Z, Berkenstadt H, Ram Z. Novel, compact, intraoperative magnetic resonance imaging-guided system for conventional neurosurgical operating rooms. Neurosurgery. 2001;48:799–807; discussion −9.
White PJ, Whalen S, Tang SC, Clement GT, Jolesz F, Golby AJ. An intraoperative brain shift monitor using shear mode transcranial ultrasound: preliminary results. J Ultrasound Med. 2009;28:191–203.
Kaus MR, Warfield SK, Nabavi A, Black PM, Jolesz FA, Kikinis R. Automated segmentation of MR images of brain tumors. Radiology. 2001;218:586–91.
Tsai A, Yezzi Jr A, Wells W, et al. A shape-based approach to the segmentation of medical imagery using level sets. IEEE Trans Med Imaging. 2003;22:137–54.
Nimsky C, Fujita A, Ganslandt O, Von Keller B, Fahlbusch R. Volumetric assessment of glioma removal by intraoperative high-field magnetic resonance imaging. Neurosurgery. 2004;55:358–70; discussion 70–1.
Schneider JP, Trantakis C, Rubach M, et al. Intraoperative MRI to guide the resection of primary supratentorial glioblastoma multiforme – a quantitative radiological analysis. Neuroradiology. 2005;47:489–500.
Claus EB, Black PM. Survival rates and patterns of care for patients diagnosed with supratentorial low-grade gliomas: data from the SEER program, 1973–2001. Cancer. 2006;106:1358–63.
Talos IF, Zou KH, Ohno-Machado L, et al. Supratentorial low-grade glioma resectability: statistical predictive analysis based on anatomic MR features and tumor characteristics. Radiology. 2006;239:506–13.
Wu W, Rigolo L, O’Donnell LJ, Norton I, Shriver S, Golby AJ. Visual pathway study using in vivo diffusion tensor imaging tractography to complement classic anatomy. Neurosurgery. 2012;70:145–56; discussion 56.
Shriver S, Knierim KE, O’Shea JP, Glover GH, Golby AJ. Pneumatically driven finger movement: a novel passive functional MR imaging technique for presurgical motor and sensory mapping. AJNR Am J Neuroradiol. 2011;34:E5–7.
Pergolizzi Jr RS, Nabavi A, Schwartz RB, et al. Intra-operative MR guidance during trans-sphenoidal pituitary resection: preliminary results. J Magn Reson Imaging. 2001;13:136–41.
Vitaz TW, Inkabi KE, Carrubba CJ. Intraoperative MRI for transphenoidal procedures: short-term outcome for 100 consecutive cases. Clin Neurol Neurosurg. 2011;113:731–5.
Pamir MN, Peker S, Ozek MM, Dincer A. Intraoperative MR imaging: preliminary results with 3 Tesla MR system. Acta Neurochir Suppl. 2006;98:97–100.
Hofmann BM, Nimsky C, Fahlbusch R. Benefit of 1.5-T intraoperative MR imaging in the surgical treatment of craniopharyngiomas. Acta Neurochir (Wien). 2011;153:1377–90; discussion 90.
Holzmann D, Reisch R, Krayenbuhl N, Hug E, Bernays RL. The transnasal transclival approach for clivus chordoma. Minim Invasive Neurosurg. 2010;53:211–7.
Woodard EJ, Leon SP, Moriarty TM, Quinones A, Zamani AA, Jolesz FA. Initial experience with intraoperative magnetic resonance imaging in spine surgery. Spine. 2001;26:410–7.
Netuka D, Ostry S, Belsan T, Kramar F, Benes V. Intraoperative MR imaging in a case of a cervical spinal cord lesion. J Neurosurg Spine. 2011;14:754–7.
Takahashi S, Morikawa S, Egawa M, Saruhashi Y, Matsusue Y. Magnetic resonance imaging-guided percutaneous fenestration of a cervical intradural cyst. Case report. J Neurosurg. 2003;99:313–5.
Dhaliwal PP, Hurlbert RJ, Sutherland GS. Intraoperative magnetic resonance imaging and neuronavigation for transoral approaches to upper cervical pathology. World Neurosurg. 2011;78:164–9.
Schwartz RB, Hsu L, Black PM, et al. Evaluation of intracranial cysts by intraoperative MR. J Magn Reson Imaging. 1998;8:807–13.
Kollias SS, Bernays RL. Interactive magnetic resonance imaging-guided management of intracranial cystic lesions by using an open magnetic resonance imaging system. J Neurosurg. 2001;95:15–23.
Senft C, Seifert V, Hermann E, Gasser T. Surgical treatment of cerebral abscess with the use of a mobile ultralow-field MRI. Neurosurg Rev. 2009;32:77–84; discussion −5.
Paraskevopoulos D, Biyani N, Constantini S, Beni-Adani L. Combined intraoperative magnetic resonance imaging and navigated neuroendoscopy in children with multicompartmental hydrocephalus and complex cysts: a feasibility study. J Neurosurg Pediatr. 2011;8:279–88.
Huston OO, Watson RE, Bernstein MA, et al. Intraoperative magnetic resonance imaging findings during deep brain stimulation surgery. J Neurosurg. 2011;115:852–7.
Chinzei K, Miller K. Towards MRI guided surgical manipulator. Med Sci Monit. 2001;7:153–63.
Chinzei KHN, Jolesz F, et al. MR compatible surgical assist robot: system integration and preliminary feasibility study. Lect Notes Comput Sci Proc MICCAI. 1935;2000:921–30.
Sutherland GR, Latour I, Greer AD, Fielding T, Feil G, Newhook P. An image-guided magnetic resonance-compatible surgical robot. Neurosurgery. 2008;62:286–92; discussion 92–3.
Pandya S, Motkoski JW, Serrano-Almeida C, Greer AD, Latour I, Sutherland GR. Advancing neurosurgery with image-guided robotics. J Neurosurg. 2009;111:1141–9.
DiMaio SP, Pieper S, Chinzei K, et al. Robot-assisted needle placement in open MRI: system architecture, integration and validation. Comput Aided Surg. 2007;12:15–24.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer Science+Business Media New York
About this chapter
Cite this chapter
Jolesz, F.A., Golby, A.J., Orringer, D.A. (2014). Magnetic Resonance Image-Guided Neurosurgery. In: Jolesz, F. (eds) Intraoperative Imaging and Image-Guided Therapy. Springer, New York, NY. https://doi.org/10.1007/978-1-4614-7657-3_32
Download citation
DOI: https://doi.org/10.1007/978-1-4614-7657-3_32
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4614-7656-6
Online ISBN: 978-1-4614-7657-3
eBook Packages: MedicineMedicine (R0)