Abstract
Although the data are limited, it is reasonable to state that people with diabetes mellitus behave in the same way to lipid modulating dietary components as people without diabetes. Thus saturated fat elevates and polyunsaturated fat reduces LDL-cholesterol levels. Psyllium and oat bran reduce LDL-cholesterol levels. Low-glycemic-index diets have no effect on plasma lipids, but fish oil lowers circulating triglyceride levels, as do exercise, weight loss, and improved glycemic control. HDL-cholesterol levels are most consistently increased by weight loss. Dietary cholesterol appears to be associated with coronary heart disease in people with diabetes, but cholesterol-feeding studies have not been performed in this group. Although theoretically plant sterols and stanols should be less effective at lowering LDL-cholesterol in people with diabetes, because of lower cholesterol absorption, this does not appear to be true. Modest alcohol intake appears to reduce the incidence of diabetes but does not appear to protect people with diabetes from heart disease. There are no data on strokes or peripheral vascular disease (PVD). There appear to be no alcohol intervention studies in people with diabetes. Fructose intake of less than 20 % of energy improves glycemic control without adversely affecting lipid levels.
This chapter will review the effects of various lifestyle factors, including diet, weight loss, smoking, and exercise, and various dietary components on the lipoprotein profile in people with diabetes mellitus.
Lipid Conversion Units:
To convert mmol/L of cholesterol to mg/dL, multiply by 38.8, and to convert mmol/L of triglyceride to mg/dL, multiply by 88.5.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
General Considerations
Lipid changes occur quickly in response to diet, and in two weeks 80 % of the maximal effect is seen, with no further change beyond four weeks. If diet is maintained, then the effect on circulating lipid levels is persistent. Regardless of the background diet, or if the study is parallel or crossover, then contrasting the effect of two diets on lipids at the end of four weeks is more than adequate to see a clear effect. Washout periods are not required. BMI, diabetes control, nor type of diabetes does not appear to interact with responses to fat or fiber, but they do appear to be related to response to cholesterol and plant sterols.
Dietary Fat and Lipoproteins
Saturated, n6 Polyunsaturated, and Monounsaturated Fat
In non-diabetic subjects the effects of dietary saturated, polyunsaturated, and monounsaturated fat are well described in a meta-analysis of 60 clinical trials published in 2003 by Mensink et al. [1]. In this paper 1 % of energy from saturated fat elevated LDL-cholesterol by 0.03 mmol/L when it replaced carbohydrate, while n6 polyunsaturated fat lowered LDL-cholesterol levels by 0.02 mmol/L when it replaced carbohydrate. The concentration of HDL-cholesterol was elevated by about 0.01 mmol/L by saturated and unsaturated fat in comparison with carbohydrate. Thus an absolute 10 % energy reduction in saturated fat (a very large change) and replacement of this fat entirely with n6 polyunsaturated fat would lower LDL-cholesterol levels by 0.5 mmol/L (or about 14–15 %). If the 10 % saturated fat were replaced entirely by carbohydrate, then LDL-cholesterol would fall by 0.3 mmol/L, HDL-cholesterol would fall by 0.1 mmol/L, and triglyceride levels would rise by 0.24 mmol/L. Is there any evidence that people with diabetes behave in a different way to changes in dietary fat composition? Somewhat surprisingly, it is difficult to answer this question as there have been a very limited number of studies in people with diabetes—either type 1 or type 2 diabetes—and much of the focus has been on glycemic rather than lipid control. All studies contained very small numbers of volunteers, except for the Oxford study.
The Oxford study was begun at a time (1973) when the standard dietary advice was a high fat (40 % of energy), low-carbohydrate diet (maximum of 40 % of energy) and little attention was paid to the type of fat in the diet, which was mostly saturated. The study contrasted the standard diet with a modified fat diet of 30 % of energy with a polyunsaturated/saturated (P/S) fat ratio of 0.9 or above. Two hundred and fifty people with newly diagnosed type 2 diabetes were enrolled between 1973 and 1976 [2]. Total cholesterol levels were 0.7 mmol/L lower on the modified fat diet averaged over 1, 3, and 5 years, which is consistent with an estimated reduction in saturated fat of about 15 % and an increase in polyunsaturated fat of 10 % [3]. Dietary records were not collected.
In a controlled study by Storm et al. [4], a palmitic acid-rich diet (16 % of energy) increased total cholesterol compared with a carbohydrate-rich diet or a stearic acid-rich diet (13 % of energy) for 3 weeks each, but surprisingly LDL- and HDL-cholesterol were not different. However, only 15 volunteers with type 2 diabetes were included in this relatively short study, and the difference in LDL-Cholesterol levels (based on total cholesterol changes) may have been about 0.2–0.3 mmol/L, which is about half of that expected. A 6-week study in 16 patients with type 2 diabetes compared 20 % of energy as saturated fat with 20 % as monounsaturated fat and a 20 % trans monounsaturated fat diet [5]. Lipids, lipoprotein, and apoB levels were the same on the three diets, which would not have been expected. A very small study in Pima Indians (n = 7) by Abbott et al. [6] showed a fall in LDL-cholesterol levels by 17 % with a change in saturated fat of 14 % of energy, and the changes were very similar to those seen in the nondiabetic subjects in the same study. Kinetic studies showed that these changes were due to slower conversion of VLDL to LDL. HDL-cholesterol and fasting TG concentrations were not significantly altered. Heine et al. [7] performed a 30-week study of two diets, one with a low polyunsaturated to saturated fat ratio (P:S 0.3) and one with a P:S of 1.0, in 14 patients with type 2 diabetes in a crossover study. Total dietary fat was 37–38 % with linoleic acid increasing from 4.2 to 10.9 %. LDL-cholesterol levels declined by 9.8 % (p < 0.01) during the high P:S diet. The change in LDL-cholesterol levels of 0.4 mmol/L is what would be expected based on the Mensink meta-analysis. A combination of weight loss and reduced dietary saturated fat lowered LDL-cholesterol levels by 10–17 % with a high-carbohydrate or high-monounsaturated fat diet respectively [8].
Overall, despite the small number of studies, the data suggest that people with type 2 diabetes respond to dietary lipid changes in the same way as non-diabetic subjects. However, a Cochrane review in 2007 [9] of dietary advice for adults with type 2 diabetes, which examined 18 trials of more than six months duration with 1,467 participants and a wide variety of dietary interventions, concluded that there was insufficient data to conclude anything other than that exercise lowered HbA1c.
Dietary Fat vs. Carbohydrate
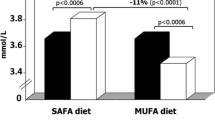
Much of the major disagreements in nutrition over the last 20 years for people with type 2 diabetes have related to replacing saturated fat with carbohydrate as opposed to unsaturated fat. For many years (1970s–1990s), a very high-carbohydrate (and high-fiber) diet was strongly advocated, although some researchers suggested high-carbohydrate diets were theoretically not optimal because of the lowering of HDL-cholesterol and elevation of fasting triglyceride levels (which is also seen to the same degree in non-diabetic subjects). The meta-analysis (n = 133 subjects, nine studies) of Garg in 1998 [10] focused on comparing high-carbohydrate diets (49–60 % of energy) with high-monounsaturated fat diets (24–33 % monounsaturated fat, 37–50 % total fat). A high-monounsaturated fat diet was associated with a reduction in fasting triglyceride levels of 0.36 mmol/L (19 %) and a reduction in VLDL-cholesterol levels of 22.5 %. HDL-cholesterol levels increased by 0.05 mmol/L or 4 %. The remainder of the fat in both diets was 7–21 %, presumably about 5 % polyunsaturated fat with the remainder being saturated fat, but surprisingly in the meta-analysis, neither of these two fats was mentioned. LDL-cholesterol levels were not different between the two diets, but the data are uninterpretable in relation to the effect of saturated fat, and one can only assume that saturated fat was not different between diets. The lack of difference between carbohydrate and monounsaturated fat on LDL-cholesterol levels is consistent with the Mensink data [1] in non-diabetic subjects.
A later meta-analysis by Kodama et al. [11] examined 19 studies with 306 patients and again showed no effect of a high-carbohydrate diet on LDL-cholesterol levels with a rise in triglycerides of 13 % and a lowering of HDL-cholesterol levels of 8 %. These changes are similar to that expected in non-diabetic subjects [12]. Whether these changes with a high-carbohydrate diet promote an increased risk of cardiovascular disease (CVD) is not clear, but there are no data available to refute this suggestion. Secondary intervention studies in non-diabetic subjects suggest that replacing saturated fat with carbohydrate is not beneficial, whereas replacing it with n6 polyunsaturated fat is beneficial [13]. A (pro-atherogenic) smaller LDL particle size in those following a high-carbohydrate diet may contribute to the adverse effect [12].
Replacing carbohydrate with protein and/or polyunsaturated fat would be expected to have similar effects to replacing it with monounsaturated fat. This was demonstrated by Thompson et al. [14] and a small (n = 11 participants) study of a high protein, lower carbohydrate Paleolithic diet that showed a reduction in triglycerides levels of 0.4 mmol/L and an increase in HDL-cholesterol levels of 0.08 mmol/L [15]. Although the Paleolithic diet had a lower glycemic load than the standard American Diabetes Association (ADA) diet, it was also reduced in energy and the 3 kg weight loss may account for some or all of these effects.
Relationship Between Diet and Coronary Events in People with Type 2 Diabetes
Although there is now considerable controversy about the role of dietary saturated fat and cholesterol in promoting CVD, the data in people with type 2 diabetes are relatively clear in the US Nurses’ Health Study [16]. Between 1980 and 1998, 619 new cases of CVD (nonfatal myocardial infarction, fatal coronary heart disease, and stroke) occurred in 5,672 women with type 2 diabetes. The relative risk (RR) of CVD for an increase of 200 mg cholesterol/1,000 kcal was 1.37 (p = 0.003). Each 5 % of energy intake from saturated fat, as compared with equivalent energy from carbohydrates, was associated with a 29 % greater risk of CVD (RR: 1.29 p = 0.04). Keys score (1.26 × (2 x% saturated fat − % polyunsaturated fat) + 1.5 × square root dietary cholesterol in mg/1000 kcal) was the most powerful predictor after multivariate adjustment (p = 0.001). The ratio of polyunsaturated to saturated fat was inversely associated with the risk of fatal CVD (p = 0.007). Replacement of 5 % of energy from saturated fat with equivalent energy from monounsaturated fat was associated with a 37 % lower risk of CVD.
Fish Oil
A Cochrane meta-analysis in 2008 examined 23 randomized controlled trials (1,075 participants with type 2 diabetes), with a mean treatment duration of 8.9 weeks [17]. The mean dose of omega-3 PUFA used in the trials was 3.5 g/day. Among those taking omega-3 PUFA circulating triglyceride levels were significantly lowered by 0.45 mmol/L (p < 0.00001) and levels of VLDL-cholesterol lowered by 0.07 mmol/L (p = 0.04). LDL-cholesterol levels were raised by 0.11 mmol/L (p = 0.05). No significant changes in levels of total or HDL-cholesterol, HbA1c, fasting glucose, fasting insulin, or in body weight were observed. The decrease in VLDL-cholesterol levels was significant only in trials of longer duration and in hypertriglyceridemic patients.
Dietary Cholesterol
A meta-analysis of 17 studies of dietary cholesterol in non-diabetic subjects showed that the addition of 100 mg dietary cholesterol/day increased the ratio of total to HDL-cholesterol by 0.020 U, total cholesterol concentrations by 0.056 mmol, LDL-cholesterol by 0.05 mmol/L, and HDL-cholesterol concentrations by 0.008 mmol/L [18].
Dietary cholesterol had little effect either on total- or LDL-cholesterol-in 31 overweight, insulin-resistant postmenopausal women over four weeks, and the effect was no different to the 34 women who were insulin sensitive [19]. A further 4-week study in insulin-sensitive individuals consuming four eggs/day showed a significant increase in non-HDL-cholesterol levels and in inflammatory markers in insulin-sensitive individuals, which was not observed in lean or obese insulin-resistant individuals, but the difference between the groups was not statistically different [20].
Cholesterol Synthesis and Absorption
Cholesterol synthesis can be assessed by the circulating level of lathosterol, an intermediate in the cholesterol synthetic pathway, while absorption can be assessed by measuring the level of plant sterols sitosterol and campesterol or the level of an endogenous bacterial cholesterol metabolite, cholestanol. All of these are transported in lipoproteins and the higher the lipoprotein level, the higher the sterol level, so adjustment needs to be made for the level of the carrier.
Insulin-sensitive individuals had higher plant sterol levels and lower lathosterol levels, indicative of higher cholesterol absorption and lower cholesterol synthesis. In 761 men of varying degrees of glucose tolerance, including 76 with type 2 diabetes, cholesterol synthesis markers were lowest and absorption markers highest in normoglycemia. Sitosterol was lower in subjects with impaired fasting glucose, impaired glucose tolerance, and type 2 diabetes compared with normoglycemic subjects (111–115 ± 7 vs. 136 ± 3 μmol × 100/mmol of cholesterol, p < 0.05). Campesterol levels were also significantly lower in these groups relative to the normoglycemic control subjects. Peripheral insulin sensitivity evaluated by the Matsuda index was associated with the lathosterol/sitosterol ratio in the entire population (r = −0.457, p < 0.001) and with that of lathosterol/cholestanol independently of obesity [21].
Clinical research on dietary cholesterol and diabetes management is very limited, and there are no clinical intervention trials that have investigated the role of egg consumption in people with type 2 diabetes.
A small study in ten male volunteers with type 1 diabetes showed that 800 mg/day of cholesterol for three weeks increased LDL-cholesterol levels by 12 % with a 7 % increase in control subjects. HDL-cholesterol levels remained the same but tended to increase in control subjects [22]. High-cholesterol absorption markers, e.g., sitosterol or campesterol, and low-cholesterol synthesis markers, e.g., lathosterol, appear to characterize type 1 diabetes [23], and these differ from people with type 2 diabetes [24].
Obesity is inversely related to fractional cholesterol absorption both in diabetic and non-diabetic subjects [25], but absorption is lower in subjects with type 2 diabetes [26]. Cholesterol absorption efficiency was 29 ± 1 % in obese subjects with diabetes vs. 42 ± 2 % in the obese control subjects (p < 0.01). Cholesterol synthesis was higher (17 ± 1 vs. 14 ± 1 mg/kg/day; p < 0.05) and neutral sterol and bile acid excretion and cholesterol turnover tended to be higher in the group with diabetes than in the control group. Blood glucose (measured twice one week apart) was positively related to cholesterol synthesis in the diabetic group (r = 0.663, p < 0.01) and in the control group (r = 0.590, p < 0.05), suggesting that the higher blood glucose level, the higher the cholesterol synthesis. In 16 obese patients with type 2 diabetes, baseline cholesterol absorption and synthesis were related to respective serum sex hormone-binding globulin, glucose, and insulin values. Weight reduction of 6 kg increased cholesterol absorption efficiency and the ratio of serum plant sterols to cholesterol—indicators of cholesterol absorption—increased by 28 % (p < 0.01) and 20–31 % (p < 0.05 for both) and reduced blood glucose by 14 %. Serum cholesterol levels did not change but serum triglyceride levels fell by 13 % [26].
Plant Sterols
Plant sterols are the plant equivalent of cholesterol and are found in cell walls and membranes. They differ from cholesterol by small changes to the side chain. They can be found naturally in oil seeds and cooking oils and are a normal part of the diet—up to 400–800 mg/day. Stanols are the same except for the removal of a double bond in the cholesterol nucleus. Some foods such as milk, margarine, orange juice, cheese, and chocolate are sometimes supplemented with sterols or stanols and deliver 2–2.5 g/day when consumed as directed.
Type 2 diabetes. The data above would suggest that obese subjects with type 2 diabetes would be less sensitive to dietary cholesterol and in turn less sensitive to the effects of dietary plant sterols. However, plant sterols appear to be just as efficacious in people with type 2 diabetes as in nondiabetic subjects. Plant sterols (1.8 g/day) for 21 days significantly reduced (p < 0.05) LDL-cholesterol concentrations from baseline levels in 15 nondiabetic and 14 type 2 diabetic subjects by 15.1 and 26.8 %, respectively, and these were not statistically different from each [27]. A meta-analysis of five clinical trials, involving seven groups (n = 148 subjects with type 2 diabetes, with follow-up range of 3–12 weeks) found the use of sterols/stanols significantly reduced LDL-cholesterol levels by 0.30 mmol/L (9 %, p < 0.01), with no apparent effect on triglycerides and a trend towards raising HDL-cholesterol levels. These results are exactly the same as those seen in a meta-analysis of nondiabetic subjects [28].
Type 1 diabetes. Excellent efficacy of plant sterols is also seen in patients with type 1 diabetes with [29] or without [30] the concomitant use of statins.
Epidemiology of Cholesterol Intake and CVD
Despite the limited effect of dietary cholesterol on fasting lipids, egg consumption of one per day doubles the risk of coronary heart disease in women and all-cause mortality in men with type 2 diabetes compared with an intake of one egg per week [31, 32]. The incidence of type 2 diabetes is also increased with higher egg intake [33, 34].
Fiber
Very high fiber diets were actively promoted and studied in the 1980s both for glycemic and lipid control [35–38], but interest faded as patients found the diets too difficult or they were found in some studies to be ineffective [39–41].
A more recent small intervention study, published in the New England Journal of Medicine [42], in 13 patients with type 2 diabetes compared a high-fiber diet which provided 50 g of total fiber per day (as soluble and insoluble fiber 25 g each), with the standard ADA diet containing 24 g of total fiber per day, with 8 g as soluble fiber and 16 g as insoluble fiber. No fiber supplements were used. As compared with the ADA diet, the high-fiber diet resulted in a lower fasting plasma total cholesterol concentration (by 6.7 %, p = 0.02), a lower plasma triglyceride concentration (by 10.2 %, p = 0.02), and a lower plasma VLDL-cholesterol concentration (by 12.5 %, p = 0.01). The fasting plasma LDL-cholesterol concentration was 6.3 % lower with the high-fiber diet, but this was not statistically significant (p = 0.11), almost certainly due to the small size of the study. There were no significant differences between the two diets in fasting plasma HDL-cholesterol concentrations.
A 6-month Canadian study [43] compared a low-glycemic-index (GI) diet with a high-fiber diet in 210 participants with type 2 diabetes. The high-cereal fiber diet included 35 g of fiber, GI of 86, and glycemic load of 201. The low-GI diet included 42 g of fiber, GI of 62, and glycemic load of 141. There was an increase of HDL-cholesterol levels in the low-GI diet by 1.7 mg/dL compared with a decrease of HDL-cholesterol by −0.2 mg/dL in the high-cereal fiber diet (p = 0.005), but this occurred only after about 16 weeks and was not associated with a change in triglyceride levels, so it is hard to conceive of a mechanism and may just be noise, although HbA1c improved modestly in the low-GI diet. LDL-cholesterol levels did not change.
The effects of specific types of dietary fibre are now summarized. Wheat bran has no effect on lipid levels in type 2 diabetes [44] nor does adherence to a high-fiber, high-vegetable Mediterranean diet [45], admittedly in a small study. Psyllium in a low dose (3.5 g three times/day) in 40 participants for 2 months does not appear to significantly lower LDL-cholesterol or triglyceride levels compared to a control group [46]. However, higher doses of psyllium (15 g/day) can significantly lower triglyceride levels compared with control when enough participants are studied (n = 125) [47]. Psyllium has also been demonstrated to lower LDL-cholesterol levels in some studies [48, 49]. Oat bran can lower LDL-cholesterol—an extra 15 g of fiber from oat bran lowered LDL-cholesterol levels by 0.77 mol/L, but this study [50] was very small (n = 8). Stabilized rice bran (20 g/day for 12 weeks) lowered LDL-cholesterol levels by 13.7 % compared with the control group in a parallel study in 28 subjects with type 2 diabetes [51]. Triglyceride levels were also lowered by 0.5 mmol/L. Guar gum is well established as being able lower LDL-cholesterol levels [52–54], but is not widely used. It would appear from the limited number of studies (except for guar) that soluble fiber can reduce LDL-cholesterol and triglyceride levels to the same degree as in nondiabetic subjects [55].
Low-Glycemic-Index Carbohydrate
As noted above, replacing fat with carbohydrate lowers HDL-cholesterol and increases triglyceride levels. In most of these studies, the GI of the carbohydrate was not assessed. Low-GI carbohydrate may have lesser effects on these lipid levels compared with high-GI carbohydrates. A meta-analysis was performed by Opperman et al. [56] in 2004 who examined lipid changes in 13 studies (eight in people with type 2 diabetes). Seven of the ten studies found an improvement in mean LDL-cholesterol concentrations on a low-GI diet. Overall, low-GI diets tended to decrease LDL-cholesterol concentrations; however, it was not statistically significant (change 0.15 (95 % CI 0.31, 0.00) mmol/L; p = 0.06). The GI of the diets was decreased by 21 (SD 10) units. In type 2 diabetes subjects, it appeared that LDL-cholesterol concentrations were decreased to a greater extent (0.18 mmol/L, p = 0.06) than in healthy subjects. Only six of the 13 studies showed an improvement in triglyceride concentrations with a low-GI diet, and the overall change was not statistically significant (change 0.03 mmol/L, p = 0.73). When divided into subgroups, no significant difference was found within type 2 diabetes, coronary heart disease, or healthy subjects. No effect was observed when only subjects with elevated triglyceride concentrations were included. Lowering the GI of food did not cause an overall significant change in mean HDL-cholesterol levels.
In a 1-year Canadian study [57], subjects with type 2 diabetes managed by diet alone (n = 162) were randomly assigned to receive high-carbohydrate, high-glycemic-index (high-GI), high-carbohydrate, low-glycemic-index (low-GI), or low-carbohydrate, high-monounsaturated fat (low-CHO) diets. With the low-GI diet, overall mean triglyceride levels were 12 % higher and HDL-cholesterol levels were 4 % lower than with the low-CHO diet (p < 0.05), despite a 26 % lower glycemic load. The lack of benefit of a low-GI/low-GL diet on triglyceride and HDL-cholesterol levels confirms the short-term meta-analytic results, but it is not clear why there were adverse changes. LDL-cholesterol responses were not different between the diets.
Epidemiological studies, such as the Zutphen Elderly Study [58] and the EURODIAB Complications Study [59], failed to show a relationship between LDL-cholesterol concentrations and low-GI diets, while other cross-sectional studies, such as the Survey of British Adults (1986–1987) [60] and the Third National Health and Nutrition Examination Survey (1988–1994) [61], found an increase in HDL-cholesterol concentrations with long-term low-GI diets. No relationship was found between low-GI diets and triglyceride concentrations [58, 59].
Fructose
Fructose for many years was promoted as very suitable for people with diabetes because it lowered plasma glucose and insulin levels and improved HbA1c levels when it replaced starch, glucose, or sucrose. Gannon [62] showed a high-fruit and high-vegetable diet with little starch lowered 24 hour blood glucose levels without adverse effects on triglyceride levels compared with a high-starch diet or a usual American diet. 30–60 g/day of pure fructose supplementation (6–12 % of energy) for 3–12 months had no adverse effects on lipids [63–67] or lipid metabolism [68]. A very high intake of fructose (>20 % of energy) has been found to elevate lipids in some studies [69–72], but not in others [73, 74].
Weight Loss
Non-diabetic Subjects
Aucott [75] conducted a systematic review of studies that included lifestyle interventions for adults (18–65 years), with a mean baseline BMI <35 kg/m2, with weight and lipid differences over 2 years. Between 1990 and 2010, 14 studies were identified. From meta-regression they found that a 1 kg maintained weight loss in the long term (2–3 years) could be expected to result in reductions of 1.3 % in total cholesterol, 1.6 % for triglycerides, and 0.34 % for LDL-cholesterol levels with a 4 % increase of HDL-cholesterol levels.
An earlier meta-analysis by Poobalan [76] of 13 long-term studies (both cohort and surgical and non-surgical and drug-based weight loss interventions) with a follow-up of more than two years found that total cholesterol concentrations had a significant positive linear relationship with weight change (r = 0.89), where change in weight explained about 80 % of the cholesterol difference variation. For every 10 kg weight loss, a drop of 0.23 mmol/L in total cholesterol levels may be expected (about 5 %). Triglycerides and LDL-cholesterol concentrations were similarly related to weight loss, with a 10 kg change producing a 0.25 mmol/L and a 0.20 mmol/L change respectively. HDL-cholesterol changes were not related to weight loss. Participants in the two long-term meta-analyses could be on lipid-lowering medication.
In a meta-analysis of 70 short-term dietary weight loss studies in nondiabetic subjects, Dattilo and Kris Etherton [77] found that for every kilogram decrease in body weight, there was a 0.05 mmol/L decrease in total cholesterol levels (about 8–10 %, p < 0.0 1), a 0.02 mmol/L decrease in LDL-cholesterol levels (p < 0.001), a 0.007 mmol/L decrease in HDL-cholesterol for active weight loss (p < 0.05), a 0.009 mmol/L increase in HDL-cholesterol for stabilized weight loss (p < 0.01), and a 0.015 mmol/L decrease in triglyceride levels (p < 0.05). Correlations between weight loss and lipid changes were of the order of 0.3–0.4 and were much lower than in the long-term studies.
In the LIFE study [78] of 212 participants without diabetes, BMI fell in women from 35 to 33.7 kg/m2 over 30 months and from 35 to 33 kg/m2 in men, with a nadir at 12 months in both. In women, multivariate-adjusted HDL-cholesterol concentrations at 6-month follow-up was significantly lower than at baseline, and at subsequent time points HDL-cholesterol concentration was significantly higher than at 6-month follow-up, with no significant differences between the later time points, which however were not significantly different from baseline. In men the small decrease at six months was not statistically significant but later rises in HDL-cholesterol levels were, with a maximum change at 18 months of about 10 %. Triglyceride levels were significantly lower than baseline at six months but rose back to and beyond baseline in women, but remained low in men.
Diabetic Subjects
For participants with diabetes, there are much fewer studies available. The Look Ahead study was a very large randomized study (n = 5,145) of intensive lifestyle interventions (ILI) or standard treatment (DSE) in overweight or obese individuals with type 2 diabetes [79]. After four years, ILI participants had a greater percentage of weight loss than DSE participants (−6.15 vs. −0.88 %; p < 0.001) and superior improvements in HDL-cholesterol levels (3.7 vs. 2.0 mg/dL; p < 0.001) and triglyceride levels (−25.6 vs. −19.75 mg/dL; p < 0.001) averaged across all 4 years. Reductions in LDL-cholesterol levels were greater in DSE than ILI participants (−11.3 vs. 12.8 mg/dL; p = 0 0.009) owing to greater use of medications to lower lipid levels in the DSE group. The effects on triglyceride levels were not statistically significant at four years but the HDL-cholesterol level difference was consistent across all four years. These effects on lipid levels were lower than those in the long-term meta-analyses quoted above, but not different from those of the 2-year studies in nondiabetic subjects from Shai and Sacks [80, 81]. However, HDL-cholesterol changes were very similar to the meta-analysis of short-term studies by Dattilo and Kris Etherton [77].
A weight loss of 4.5 kg in 2,906 patients in the UKPDS reduced triglyceride levels by 0.41 mmol/L in men and 0.23 mmol/L in women with an HDL-cholesterol increase of 0.02 and 0.01 mmol/L, respectively. LDL-cholesterol levels did not change [82].
Glycemic Control
In 2,220 type 2 diabetic patients (aged 35–91 years; male/female ratio, 1.07), HbA1c levels showed direct and significant correlations with total cholesterol, triglyceride, and LDL-cholesterol levels and inverse correlation with levels of HDL-cholesterol [83]. In Italian diabetes outpatient clinics, abnormal lipids were associated with markedly higher HbA1c levels [84] in 12,222 patients. On multiple regression, triglyceride levels were associated with HbA1c after adjustment for age, BMI and diabetes treatment, and a variety of other factors, while HDL-cholesterol levels were related to HbA1c levels in men only.
Interventions to Improve Glycemic Control
A Dutch study [85] which targeted a strict fasting capillary glucose of <6.5 mmol/L vs. a less strict regimen of <8.5 mmol/L in 214 patients over two years looked at individual changes in HbA1c vs. lipid changes. Individuals in whom HbA1c levels decreased had significant favorable concurrent changes in triglycerides r = 0.26 with HbA1c changes (p = 0.001) with an absolute difference of 0.25 mmol/L between those whose HbA1c fell (−0.17 mmol/L) vs. those whose HbA1c rose (0.08 mmol/L). Changes in LDL- and HDL-cholesterol levels were not statistically significant. The difference in HbA1c between the two groups was 1.09 %.
In the Veterans Affairs Cooperative study in 513 male type 2 diabetes patients over two years, triglyceride levels decreased in the intensive-treatment arm from 2.25 ± 0.27 to 1.54 ± 0.14 mmol/L at 1 year (p = 0.004) and to 1.74 ± 0.18 mmol/L at 2 years (p = 0.03); there was no change in the standard-treatment arm. Total cholesterol levels decreased in the intensive-treatment arm at 1 year from 5.4 ± 0.21 to 4.99 ± 0.13 mmol/L (p = 0.02); there was no change in the standard-treatment arm. Levels of LDL- and HDL-cholesterol decreased in the standard-treatment arm only after two years, from 3.44 ± 0.13 to 3.16 ± 0.10 mmol/L (p =0.02) and from 1.10 ± 0.03 to 1.00 ± 0.03 mmol/L (p < 0.001), respectively. Levels of apolipoprotein B decreased in both treatment arms (p < 0.001), and apolipoprotein A1 levels decreased in the standard-treatment arm (p < 0.01). A 2.1 % difference in HbA1c levels was achieved over the 2-year period [86].
The DCCT study [87] and the study by Cusp et al. [88] have shown falls in LDL-cholesterol with intensive diabetes treatment. The latter study was very small (n = 12) and the fall in HbA1c achieved with 80 IU of insulin was 3.7 % over 16 weeks. In the DCCT with 1,441 patients with type 1 diabetes, changes in LDL-cholesterol levels were small, 0.1–0.2 mmol/L, but the risk of developing an LDL-cholesterol level of >4 mmol/L was reduced by 40 % in the intensive diabetes treatment group, although rates were about 1 per 100 patient years or less. Mean HbA1c level in the intensive- and conventional-treatment groups differed by about 2% throughout the follow-up period (7.2 vs. 9.1 %, respectively, p < 0.001).
Alcohol Intake
A moderate alcohol intake is associated with about a 30 % lower incidence of type 2 diabetes but high alcohol intake and binge drinking increases the risk of type 2 diabetes [89, 90]. Alcohol intake in people with type 2 diabetes in the EPIC study [91] did not reduce mortality, although a prospective cohort study in older people showed an 80 % reduction in death due to coronary heart disease with 14 g or more of alcohol/day [92] before and after adjustment for levels of HDL-cholesterol and total cholesterol. In Japanese men with type 2 diabetes, alcohol intake was directly related to HDL-cholesterol levels and hypertension, but the lowest triglyceride level was in the 1–22 g alcohol/day intake group compared with the nondrinker group [93]. There appear to be no alcohol intervention studies in people with diabetes.
Exercise
In a Cochrane meta-analysis [94], 14 randomized controlled trials comparing supervised or well-documented (aerobic, resistance, or mixed) exercise against “no exercise” in type 2 diabetes were identified involving 377 participants. Most studies had three 30–60 min exercise sessions per week. Trials ranged from eight weeks to 12 months duration. No specific exercise program was given to the control group, but there were no reports on their incidental activity. The exercise intervention significantly decreased plasma triglyceride levels (−0.25 mmol/L, 95 % CI −0.48 to −0.02). No significant difference was found between groups in plasma cholesterol levels or LDL-cholesterol or HDL-cholesterol levels.
Smoking
A recent meta-analysis [95] of observational studies in 130,000 people with diabetes showed the relative risk comparing smokers with nonsmokers was 1.48 for total mortality (27 studies), 1.36 for cardiovascular mortality (nine studies), 1.54 for CHD (13 studies), 1.44 for stroke (nine studies), and 1.52 for MI (seven studies). The increased risk of smoking is similar to people without diabetes. Smoking lowers HDL-cholesterol levels. The major lipid-related effect of smoking cessation is an increase (of about 0.1 mmol/L or 3.9 mg/dl) [96].
New Research Areas
Given the association between cholesterol intake and CVD events in people with diabetes, a cholesterol-feeding trial in people with both type 1 and type 2 diabetes needs to be done, focused not just on LDL- and HDL-cholesterol levels, but adhesion molecules and other inflammatory markers.
Long-term dietary intervention studies examining low salt, low saturated fat, high polyunsaturated fat, and high fruit, vegetables, and fiber over a 3-year period need to be done with surrogate cardiovascular measures such as carotid intima-medial thickness as an endpoint.
Conclusions
There is a very limited amount of data related to the lifestyle effects on lipoproteins specifically involving people with diabetes. What data are available suggest they respond in a similar way to people without diabetes to lifestyle measures. The expected responses of LDL-cholesterol levels to dietary changes are summarized in Table 16.1. The effect of dietary cholesterol needs further exploration.
Abbreviations
- ADA:
-
American Diabetes Association
- Apo:
-
Apolipoprotein
- HDL:
-
High-density lipoprotein
- LDL:
-
Low-density lipoprotein
- P:S:
-
Polyunsaturated to saturated fat ratio
- TG:
-
Triglycerides
- VLDL:
-
Very low density lipoprotein
References
Mensink RP, Zock PL, Kester AD, Katan MB. Effects of dietary fatty acids and carbohydrates on the ratio of serum total to HDL cholesterol and on serum lipids and apolipoproteins: a meta-analysis of 60 controlled trials. Am J Clin Nutr. 2003;77(5):1146–55.
Simpson RW, Mann JI, Eaton J, Moore RA, Carter R, Hockaday TDR. Improved glucose control in maturity-onset diabetes treated with high-carbohydrate-modified fat diet. BMJ. 1979;1:1753–6.
Howard-Williams J, Patel P, Jelfs R, et al. Polyunsaturated fatty acids and diabetic retinopathy. Br J Ophthalmol. 1985;69:15–8.
Storm H, Thomsen C, Pedersen E, Rasmussen O, Christiansen C, Hermansen K. Comparison of a carbohydrate-rich diet and diets rich in stearic or palmitic acid in NIDDM patients. Effects on lipids, glycemic control, and diurnal blood pressure. Diabetes Care. 1997;20(12):1807–13.
Christiansen E, Schneider S, Palmvig B, Tauber-Lassen E, Pedersen O. Intake of a diet high in trans monounsaturated fatty acids or saturated fatty acids. Effects on postprandial insulinemia and glycemia in obese patients with NIDDM. Diabetes Care. 1997;20(5):881–7.
Abbott WG, Swinburn B, Ruotolo G, Hara H, Patti L, Harper I, Grundy SM, Howard BV. Effect of a high-carbohydrate, low-saturated-fat diet on apolipoprotein B and triglyceride metabolism in Pima Indians. J Clin Invest. 1990;86(2):642–50.
Heine RJ, Mulder C, Popp-Snijders C, van der Meer J, van der Veen EA. Linoleic-acid-enriched diet: long-term effects on serum lipoprotein and apolipoprotein concentrations and insulin sensitivity in noninsulin-dependent diabetic patients. Am J Clin Nutr. 1989;49(3):448–56.
Heilbronn LK, Noakes M, Clifton PM. Effect of energy restriction, weight loss, and diet composition on plasma lipids and glucose in patients with type 2 diabetes. Diabetes Care. 1999;22(6):889–95.
Nield L, Moore HJ, Hooper L, Cruickshank JK, Vyas A, Whittaker V, Summerbell CD. Dietary advice for treatment of type 2 diabetes mellitus in adults. Cochrane Database Syst Rev. 2007;3, CD004097.
Garg A. High-monounsaturated-fat diets for patients with diabetes mellitus: a meta-analysis. Am J Clin Nutr. 1998;67(3 Suppl):577S–82.
Kodama S, Saito K, Tanaka S, Maki M, Yachi Y, Sato M, Sugawara A, Totsuka K, Shimano H, Ohashi Y, Yamada N, Sone H. Influence of fat and carbohydrate proportions on the metabolic profile in patients with type 2 diabetes: a meta-analysis. Diabetes Care. 2009;32(5):959–65.
Krauss RM, Blanche PJ, Rawlings RS, Fernstrom HS, Williams PT. Separate effects of reduced carbohydrate intake and weight loss on atherogenic dyslipidemia. Am J Clin Nutr. 2006;83(5):1025–31.
Mozaffarian D, Micha R, Wallace S. Effects on coronary heart disease of increasing polyunsaturated fat in place of saturated fat: a systematic review and meta-analysis of randomized controlled trials. PLoS Med. 2010;7(3):e1000252. Review.
Thomsen C, Rasmussen OW, Hansen KW, Vesterlund M, Hermansen K. Comparison of the effects on the diurnal blood pressure, glucose, and lipid levels of a diet rich in monounsaturated fatty acids with a diet rich in polyunsaturated fatty acids in type 2 diabetic subjects. Diabet Med. 1995;12(7):600–6.
Jönsson T, Granfeldt Y, Ahrén B, Branell UC, Pålsson G, Hansson A, Söderström M, Lindeberg S. Beneficial effects of a Paleolithic diet on cardiovascular risk factors in type 2 diabetes: a randomized cross-over pilot study. Cardiovasc Diabetol. 2009;8:35.
Tanasescu M, Cho E, Manson JE, Hu FB. Dietary fat and cholesterol and the risk of cardiovascular disease among women with type 2 diabetes. Am J Clin Nutr. 2004;79:999–1005.
Hartweg J, Perera R, Montori V, Dinneen S, Neil HA, Farmer A. Omega-3 polyunsaturated fatty acids (PUFA) for type 2 diabetes mellitus. Cochrane Database Syst Rev. 2008;1, CD003205.
Weggemans RM, Zock PL, Katan MB. Dietary cholesterol from eggs increases the ratio of total cholesterol to high-density lipoprotein cholesterol in humans: a meta-analysis. Am J Clin Nutr. 2001;73(5):885–91.
Reaven GM. Insulin resistance, dietary cholesterol, and cholesterol concentration in postmenopausal women. Metabolism. 2001;50:594–7.
Tannock LR, O’Brien KD, Knopp RH, et al. Cholesterol feeding increases C-reactive protein and serum amyloid A levels in lean insulin-sensitive subjects. Circulation. 2005;111:3058–62.
Gylling H, Hallikainen M, Pihlajamäki J, Simonen P, Kuusisto J, Laakso M, Miettinen TA. Insulin sensitivity regulates cholesterol metabolism to a greater extent than obesity: lessons from the METSIM Study. J Lipid Res. 2010;51(8):2422–7. Epub 2010 May 1.
Romano G, Tilly-Kiesi MK, Patti L, et al. Effects of dietary cholesterol on plasma lipoproteins and their subclasses in IDDM patients. Diabetologia. 1998;41:193–200.
Gylling H, Tuominen JA, Koivisto VA, Miettinen TA. Cholesterol metabolism in type 1 diabetes. Diabetes. 2004;53(9):2217–22.
Miettinen TA, Gylling H, Tuominen J, Simonen P, Koivisto V. Low synthesis and high absorption of cholesterol characterize type 1 diabetes. Diabetes Care. 2004;27(1):53–8.
Simonen PP, Gylling HK, Miettinen TA. Diabetes contributes to cholesterol metabolism regardless of obesity. Diabetes Care. 2002;25(9):1511–5.
Simonen P, Gylling H, Howard AN, Miettinen TA. Introducing a new component of the metabolic syndrome: low cholesterol absorption. Am J Clin Nutr. 2000;72:82–8.
Lau VW, Journo M, Jones PJ. Plant sterols are efficacious in lowering plasma LDL and non-HDL cholesterol in hypercholesterolemic type 2 diabetic and nondiabetic persons. Am J Clin Nutr. 2005;81(6):1351–8.
Abumweis SS, Barake R, Jones PJ. Plant sterols/stanols as cholesterol lowering agents: a meta-analysis of randomized controlled trials. Food Nutr Res. 2008;52. doi: 10.3402/fnr.v52i0.1811.
Hallikainen M, Kurl S, Laakso M, Miettinen TA, Gylling H. Plant stanol esters lower LDL cholesterol level in statin-treated subjects with type 1 diabetes by interfering the absorption and synthesis of cholesterol. Atherosclerosis. 2011;217(2):473–8. Epub 2011 Apr 5.
Hallikainen M, Lyyra-Laitinen T, Laitinen T, Moilanen L, Miettinen TA, Gylling H. Effects of plant stanol esters on serum cholesterol concentrations, relative markers of cholesterol metabolism and endothelial function in type 1 diabetes. Atherosclerosis. 2008;199(2):432–9. Epub 2007 Dec 11.
Hu FB, Stampfer MJ, Rimm EB, et al. A prospective study of egg consumption and risk of cardiovascular disease in men and women. JAMA. 1999;281:1387–94.
Djousse L, Gaziano JM. Egg consumption in relation to cardiovascular disease and mortality: the physicians’ health study. Am J Clin Nutr. 2008;87:964–9.
Liese AD, Weis KE, Schulz M, Tooze JA. Food intake patterns associated with incident type 2 diabetes: the insulin resistance atherosclerosis study. Diabetes Care. 2009;32:263–8.
Djousse L, Gaziano JM, Buring JE, Lee IM. Egg consumption and risk of type 2 diabetes in men and women. Diabetes Care. 2009;32:295–300.
Rivellese A, Riccardi G, Giacco A, Pacioni D, Genovese S, Mattioli PL, Mancini M. Effect of dietary fibre on glucose control and serum lipoproteins in diabetic patients. Lancet. 1980;2(8192):447–50.
Karlström B, Vessby B, Asp NG, Boberg M, Gustafsson IB, Lithell H, Werner I. Effects of an increased content of cereal fibre in the diet of type 2 (non-insulin-dependent) diabetic patients. Diabetologia. 1984;26(4):272–7.
Riccardi G, Rivellese A, Pacioni D, Genovese S, Mastranzo P, Mancini M. Separate influence of dietary carbohydrate and fibre on the metabolic control in diabetes. Diabetologia. 1984;26(2):116–21.
Lousley SE, Jones DB, Slaughter P, Carter RD, Jelfs R, Mann JI. High carbohydrate-high fibre diets in poorly controlled diabetes. Diabet Med. 1984;1(1):21–5.
Scott AR, Attenborough Y, Peacock I, Fletcher E, Jeffcoate WJ, Tattersall RB. Comparison of high fibre diets, basal insulin supplements, and flexible insulin treatment for non-insulin dependent (type II) diabetics poorly controlled with sulphonylureas. BMJ. 1988;297:707–10.
Hollenbeck CB, Coulston AM, Reaven M. To what extent does increased dietary fiber improve glucose and lipid metabolism in patients with noninsulin-dependent diabetes mellitus (NIDDM). Am J Clin Nutr. 1986;43:16–24.
Beattie VA, Edwards CA, Hosker JP, Cullen DR, Ward JD, Read NW. Does adding fibre to a low energy, high carbohydrate, low fat diet confer any benefit to the management of newly diagnosed overweight type II diabetics? Br Med J (Clin Res Ed). 1988;296(6630):1147–9.
Chandelier M, Garg A, Lutjohann D, von Bergmann K, Grundy SM, Brinkley LJ. Beneficial effects of high dietary fiber intake in patients with type 2 diabetes mellitus. N Engl J Med. 2000;342(19):1392–8.
Jenkins DJ, Kendall CW, McKeown-Eyssen G, Josse RG, Silverberg J, Booth GL, Vidgen E, Josse AR, Nguyen TH, Corrigan S, Banach MS, Ares S, Mitchell S, Emam A, Augustin LS, Parker TL, Leiter LA. Effect of a low-glycemic index or a high-cereal fiber diet on type 2 diabetes: a randomized trial. JAMA. 2008;300(23):2742–53.
Jenkins DJ, Kendall CW, Augustin LS, Martini MC, Axelsen M, Faulkner D, Vidgen E, Parker T, Lau H, Connelly PW, Teitel J, Singer W, Vandenbroucke AC, Leiter LA, Josse RG. Effect of wheat bran on glycemic control and risk factors for cardiovascular disease in type 2 diabetes. Diabetes Care. 2002;25(9):1522–8.
Itsiopoulos C, Brazionis L, Kaimakamis M, Cameron M, Best JD, O'Dea K, Rowley K. Can the Mediterranean diet lower HbA1c in type 2 diabetes? Results from a randomized cross-over study. Nutr Metab Cardiovasc Dis. 2011;21(9):740–7. Epub 2010 Jul 31.
Sartore G, Reitano R, Barison A, Magnanini P, Cosma C, Burlina S, Manzato E, Fedele D, Lapolla A. The effects of psyllium on lipoproteins in type II diabetic patients. Eur J Clin Nutr. 2009;63(10):1269–71. Epub 2009 Jul 22.
Rodriguez-Moran M, Guerrero-Romero F, Lazcano-Burciaga GJ. Lipid- and glucose-lowering efficacy of Plantago Psyllium in type II diabetes. J Diabetes Complications. 1998;12:273–8.
Anderson JW, Allgood LD, Turner J, Oeltgen PR, Daggy BP. Effects of psyllium on glucose and serum lipid responses in men with type 2 diabetes and hypercholesterolemia. Am J Clin Nutr. 1999;70(4):466–73.
Sierra M, García JJ, Fernández N, Diez MJ, Calle AP. Therapeutic effects of psyllium in type 2 diabetic patients. Eur J Clin Nutr. 2002;56(9):830–42.
Pick ME, Hawrysh ZJ, Gee MI, Toth E, Garg ML, Hardin RT. Oat bran concentrate bread products improve long-term control of diabetes: a pilot study. J Am Diet Assoc. 1996;96(12):1254–61.
Cheng HH, Huang HY, Chen YY, Huang CL, Chang CJ, Chen HL, Lai MH. Ameliorative effects of stabilized rice bran on type 2 diabetes patients. Ann Nutr Metab. 2010;56(1):45–51. Epub 2009 Dec 15.
Uusitupa M, Siitonen O, Savolainen K, Silvasti M, Penttilä I, Parviainen M. Metabolic and nutritional effects of long-term use of guar gum in the treatment of noninsulin-dependent diabetes of poor metabolic control. Am J Clin Nutr. 1989;49(2):345–51.
Lalor BC, Bhatnagar D, Winocour PH, Ishola M, Arrol S, Brading M, Durrington PN. Placebo-controlled trial of the effects of guar gum and metformin on fasting blood glucose and serum lipids in obese, type 2 diabetic patients. Diabet Med. 1990;7(3):242–5.
Vuorinen-Markkola H, Sinisalo M, Koivisto VA. Guar gum in insulin-dependent diabetes: effects on glycemic control and serum lipoproteins. Am J Clin Nutr. 1992;56(6):1056–60.
Anderson JW, Allgood LD, Lawrence A, Altringer LA, Jerdack GR, Hengehold DA, et al. Cholesterol-lowering effects of psyllium intake adjunctive to diet therapy in men and women with hypercholesterolemia: meta-analysis of 8 controlled trials. Am J Clin Nutr. 2000;71:472–9.
Opperman AM, Venter CS, Oosthuizen W, Thompson RL, Vorster HH. Meta-analysis of the health effects of using the glycaemic index in meal-planning. Br J Nutr. 2004;92(3):367–81.
Wolever TM, Gibbs AL, Mehling C, Chiasson JL, Connelly PW, Josse RG, Leiter LA, Maheux P, Rabasa-Lhoret R, Rodger NW, Ryan EA. The Canadian Trial of Carbohydrates in Diabetes (CCD), a 1-y controlled trial of low-glycemic-index dietary carbohydrate in type 2 diabetes: no effect on glycated hemoglobin but reduction in C-reactive protein. Am J Clin Nutr. 2008;87(1):114–25.
Van Dam RM, Visscher AWJ, Feskens EJM, Verhoef P, Kromhout D. Dietary glycemic index in relation to metabolic risk factors and incidence of coronary heart disease: the Zutphen Elderly Study. Eur J Clin Nutr. 2000;54:729–31.
Buyken AE, Toeller M, Heitkamp G, Karamaros B, Rottiers R, Muggeo M, Fuller J, The EURODIAB IDDM Complications Study Group. Glycemic index in the diet of European outpatients with type 1 diabetes: relations to glycated hemoglobin and serum lipids. Am J Clin Nutr. 2001;73:574–81.
Frost G, Leeds AA, Doré CJ, Madeiros S, Brading S, Dornhorst A. Glycaemic index as a determinant of serum HDL-cholesterol concentration. Lancet. 1999;353(9158):1045–8.
Ford ES, Liu S. Glycemic index and serum high-density lipoprotein cholesterol concentration among us adults. Arch Intern Med. 2001;161(4):572–6.
Gannon MC, Nuttall FQ, Westphal SA, Fang S, Ercan-Fang N. Acute metabolic response to high-carbohydrate, high-starch meals compared with moderate-carbohydrate, low-starch meals in subjects with type 2 diabetes. Diabetes Care. 1998;21(10):1619–26.
Osei K, Bossetti B. Dietary fructose as a natural sweetener in poorly controlled type 2 diabetes: a 12 month crossover study of effects on glucose, lipoprotein, and apolipoprotein metabolism. Diabet Med. 1989;6:506–11.
Osei K, Falko J, Bossetti BM, Holland GC. Metabolic effects of fructose as a natural sweetener in the physiologic meals of ambulatory obese patients with type II diabetes. Am J Med. 1987;83(2):249–55.
Grigoresco C, Rizkalla SW, Halfon P, Bornet F, Fontvielle AM, Bros M, Dauchy F, Tchobroutsky G, Slama G. Lack of detectable deleterious effects on metabolic control of daily fructose ingestion for 2 mo in NIDDM patients. Diabetes Care. 1988;11:546–50.
Anderson JW, Story LJ, Zettwoch NC, Gustafson NJ, Jefferson BS. Metabolic effects of fructose supplementation in diabetic individuals. Diabetes Care. 1989;12:337–44.
McAteer EJ, O'Reilly G, Hadden DR. The effects of one month high fructose intake on plasma glucose and lipid levels in non-insulin-dependent diabetes. Diabet Med. 1987;4(1):62–4.
Thorburn AW, Crapo PA, Beltz WF, Wallace P, Witztum JL, Henry RR. Lipid metabolism in non-insulin-dependent diabetes: effects of long-term treatment with fructose-supplemented mixed meals. Am J Clin Nutr. 1989;50:1015–22.
Crapo PA, Kolterman OG, Henry RR. Metabolic consequence of two-week fructose feeding in diabetic subjects. Diabetes Care. 1986;9:111–9.
Bantle JP, Swanson JE, Thomas W, Laine DC. Metabolic effects of dietary fructose in diabetic subjects. Diabetes Care. 1992;15:1468–76.
Bantle JP. Dietary fructose and metabolic syndrome and diabetes. J Nutr. 2009;139(6):1263S–8.
Abraha A, Humphreys SM, Clark ML, Matthews DR, Frayn KN. Acute effects of fructose on postprandial lipaemia in diabetic and non-diabetic subjects. Br J Nutr. 1998;80:169–75.
Koivisto VA, Yki-Järvinen H. Fructose and insulin sensitivity in patients with type 2 diabetes. J Intern Med. 1993;233:145–53.
Malerbi DA, Paiva ES, Duarte AL, Wajchenberg BL. Metabolic effects of dietary sucrose and fructose in type II diabetic subjects. Diabetes Care. 1996;19:1249–56.
Aucott L, Gray D, Rothnie H, Thapa M, Waweru C. Effects of lifestyle interventions and long-term weight loss on lipid outcomes – a systematic review. Obes Rev. 2011;12(5):e412–25.
Poobalan A, Aucott L, Smith WCS, Avenel A, Jung R, Broom J, Grant AM. Effects of weight loss in overweight/obese individuals and long-term lipid outcomes – a systematic review. Obes Rev. 2004;5(1):43–50.
Dattilo AM, Kris-Etherton PM. Effects of weight reduction on blood lipids and lipoproteins: a meta-analysis. Am J Clin Nutr. 1992;56:320–8.
Yatsuya H, Jeffery RW, Erickson DJ, Welsh EM, Flood AP, Jaeb MA, Laqua PS, Mitchell NR, Langer SL, Levy RL. Sex-specific HDL cholesterol changes with weight loss and their association with anthropometric variables: the LIFE study. Obesity (Silver Spring). 2011;19(2):429–35.
Look AHEAD Research Group, Wing RR. Long-term effects of a lifestyle intervention on weight and cardiovascular risk factors in individuals with type 2 diabetes mellitus: four-year results of the Look AHEAD trial. Arch Intern Med. 2010;170(17):1566–75.
Shai I, Schwarzfuchs D, Henkin Y, Shahar DR, Witkow S, Greenberg I, Golan R, Fraser D, Bolotin A, Vardi H, Tangi-Rozental O, Zuk-Ramot R, Sarusi B, Brickner D, Schwartz Z, Sheiner E, Marko R, Katorza E, Thiery J, Fiedler GM, Blüher M, Stumvoll M, Stampfer MJ. Dietary intervention randomized controlled trial (DIRECT) group. Weight loss with a low-carbohydrate, Mediterranean, or low-fat diet. N Engl J Med. 2008;359(3):229–41.
Sacks FM, Bray GA, Carey VJ, Smith SR, Ryan DH, Anton SD, McManus K, Champagne CM, Bishop LM, Laranjo N, Leboff MS, Rood JC, de Jonge L, Greenway FL, Loria CM, Obarzanek E, Williamson DA. Comparison of weight-loss diets with different compositions of fat, protein, and carbohydrates. N Engl J Med. 2009;360(9):859–73.
Manley SE, Stratton IM, Cull CA, Frighi V, Eeley EA, Matthews DR, Holman RR, Turner RC, Neil HA, United Kingdom Prospective Diabetes Study Group. Effects of three months’ diet after diagnosis of type 2 diabetes on plasma lipids and lipoproteins (UKPDS 45). Diabet Med. 2000;17(7):518–23.
Ahmad Khan H. Clinical significance of HbA1c as a marker of circulating lipids in male and female type 2 diabetic patients. Acta Diabetol. 2007;44(4):193–200. Epub 2007 Sep 1.
Comaschi M, Coscelli C, Cucinotta D, Malini P, Manzato E, Nicolucci A, SFIDA Study Group-Italian Association of Diabetologists (AMD). Cardiovascular risk factors and metabolic control in type 2 diabetic subjects attending outpatient clinics in Italy: the SFIDA (survey of risk factors in Italian diabetic subjects by AMD) study. Nutr Metab Cardiovasc Dis. 2005;15(3):204–11.
Becker A, van der Does FE, van Hinsbergh VW, Heine RJ, Bouter LM, Stehouwer CD. Improvement of glycaemic control in type 2 diabetes: favourable changes in blood pressure, total cholesterol and triglycerides, but not in HDL cholesterol, fibrinogen, Von Willebrand factor and (pro)insulin. Neth J Med. 2003;61(4):129–36.
Emanuele N, Azad N, Abraira C, et al. Effect of intensive glycemic control on fibrinogen, lipids, and lipoproteins: veterans affairs cooperative study in type II diabetes mellitus. Arch Intern Med. 1998;158:2485–90.
The Diabetes Control and Complications Trial (DCCT) Research Group. Effect of intensive diabetes management on macrovascular events and risk factors in the diabetes control and complications trial. Am J Cardiol. 1995;75:894–903.
Cusi K, Cunningham GR, Comstock JP. Safety and efficacy of normalizing fasting glucose with bedtime NPH insulin alone in NIDDM. Diabetes Care. 1995;18:843–5.
Carlsson S, Hammar N, Grill V, Kaprio J. Alcohol consumption and the incidence of type 2 diabetes: a 20-year follow-up of the Finnish twin cohort study. Diabetes Care. 1998;21(10):1619–26.
Koppes LL, Dekker JM, Hendriks HF, Bouter LM, Heine RJ. Moderate alcohol consumption lowers the risk of type 2 diabetes: a meta-analysis of prospective observational studies. Diabetes Care. 2005;28(3):719–25.
Sluik D, Boeing H, Bergmann MM, Schütze M, Teucher B, Kaaks R, Tjønneland A, Overvad K, Arriola L, Ardanaz E, Bendinelli B, Agnoli C, Tumino R, Ricceri F, Mattiello A, Spijkerman AM, Beulens JW, Grobbee DE, Nilsson PM, Melander O, Franks PW, Rolandsson O, Riboli E, Gallo V, Romaguera D, Nöthlings U. Alcohol consumption and mortality in individuals with diabetes mellitus. Br J Nutr. 2011;15:1–9.
Valmadrid CT, Klein R, Moss SE, Klein BE, Cruickshanks KJ. Alcohol intake and the risk of coronary heart disease mortality in persons with older-onset diabetes mellitus. JAMA. 1999;282(3):239–46.
Wakabayashi I. Association between alcohol drinking and metabolic syndrome in Japanese male workers with diabetes mellitus. J Atheroscler Thromb. 2011;18(8):684–92.
Thomas DE, Elliott EJ, Naughton GA. Exercise for type 2 diabetes mellitus. Cochrane Database Syst Rev. 2006;3, CD002968.
Qin R, Chen T, Lou Q, Yu D. Excess risk of mortality and cardiovascular events associated with smoking among patients with diabetes: meta-analysis of observational prospective studies. Int J Cardiol. 2013;167(2):342–50.
Maeda K, Noguchi Y, Fukui T. The effects of cessation from cigarette smoking on the lipid and lipoprotein profiles: a meta-analysis. Prev Med. 2003;37:283–290.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer Science+Business Media New York
About this chapter
Cite this chapter
Clifton, P. (2014). Effects of Lifestyle (Diet, Plant Sterols, Exercise) and Glycemic Control on Lipoproteins in Diabetes. In: Jenkins, A., Toth, P., Lyons, T. (eds) Lipoproteins in Diabetes Mellitus. Contemporary Diabetes. Humana Press, New York, NY. https://doi.org/10.1007/978-1-4614-7554-5_16
Download citation
DOI: https://doi.org/10.1007/978-1-4614-7554-5_16
Published:
Publisher Name: Humana Press, New York, NY
Print ISBN: 978-1-4614-7553-8
Online ISBN: 978-1-4614-7554-5
eBook Packages: MedicineMedicine (R0)