Abstract
Ultrasound allows both the detection of the primary lesion in skin cancer and the performance of an adequate locoregional staging. The pre-surgical use of ultrasound can support the decrease of recurrences and improve the cosmetic prognosis of the patient. An introduction to the use of diagnostic ultrasound in skin cancer is performed in this chapter. Sonographic key signs of the most common types of malignant tumors are also provided.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
FormalPara Key Points-
The primary lesions in skin cancer can be recognized on ultrasound.
-
Ultrasound provides relevant anatomical data on extension in all axes, exact location, vascularity and deeper involvement.
-
Locoregional staging of skin cancer can also be performed using ultrasound.
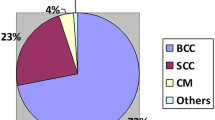
Skin cancers comprise the most frequent malignant condition among human beings. Even though NMSC (nonmelanoma skin cancer: basal cell and squamous cell carcinoma) is rarely a mortal disease and it rarely metastasizes, it can generate considerable disfigurement and usually affects highly exposed areas of the body such as the face. NMSC represents approximately 88 % of all malignant skin neoplasms [1]. Some authors report that up to 45.5 % of recurrent basal cell carcinomas are due to incomplete resections and up to 54.8 % have demonstrated at least partial aggressive-growth features [2].
Cutaneous malignant melanoma constitutes 4–11 % of all skin cancers but is responsible for more than 75 % of skin cancer-related deaths, producing more than 8,000 deaths per year in the United States [3, 4]. Thus, the assessment of depth in melanoma is a critical issue that may influence important clinical decisions such as the performance of a sentinel node procedure or the size of the excision [3].
In recent years, new ultrasound technology has been developed which has allowed a better defini tion of the sonographic images of the skin layers and deeper structures. These more sophisticated ultrasound machines have more channels and work with higher and variable frequency probes. Usually, their highest frequencies range between 15 and 22 MHz.
The main advantage of ultrasound is the provision of real-time images with a reasonable balance between resolution and penetration that allows the observation of tumors whose depth is between 0.1 and 60 mm, without changing the probe. The latter issue can be relevant since other imaging technologies used in dermatology, such as confocal microscopy (CFM) or optical coherence tomography (OCT), do not penetrate more than 0.5 mm (CFM) or 2 mm (OCT) which may leave critical information (deeper tumors) out of the medical treatment plan. This may be a potential source of recurrences. Another advantage of ultrasound is the assessment of the vascularization of the tumor by qualifying and quantifying in vivo the vessels within the tumor through the use of color Doppler and spectral curve analysis (showing the type of vessel and velocity of flow). Ultrasound also provides the anatomical location and extension of the tumors in all axes which may support one-time surgical planning [5].
The limitations of ultrasound are for lesions that measure less than 0.1 mm, the epidermal-only tumors, and the detection of pigments such as melanin [5]. However, the solid component of the primary tumor and its secondary lesions (nodal and extra-nodal) can be defined.
Thus, a very good correlation has been reported between the sonographic and histologic assessment of depth in basal cell carcinoma and melanoma [6, 7]. Furthermore, sonographic detection of subclinical basal cell carcinoma lesions has already been reported [6].
Also, ultrasonography may differentiate between melanomas that measure more or less than 1 mm depth and can assess the early anatomical changes in skin cancer, both in depth and vascularity, using a nonsurgical treatment [8].
Furthermore, the use of this noninvasive imaging technology can support the management of pleomorphic or asymmetric tumors that can show confusing histologic results due to partial samples of tissue. Also, this technique can provide a non-invasive follow-up in cases that are managed with nonsurgical treatments [9].
The objectives of ultrasonography are to provide additional and relevant information to that one already deduced by the naked eye of a well-trained physician [10]. Therefore, the assessment of anatomical sonographic patterns in the different types of skin cancer can support an early diagnosis and management and also may help to decrease the recurrence rates and improve the cosmetic prognosis of these patients [11].
Sonographic Signs in Primary Skin Cancer
Basal cell carcinoma usually appears on ultrasound as a well-defined, oval shape and hypoechoic lesion that commonly presents hyperechoic spots. Slow flow arterial and venous vessels are commonly detected at the bottom of the lesion. Occasionally, basal cell carcinoma shows pleomorphic presentations with asymmetric, bulging, lobulated or irregular appearances [12] (Figs. 14.1, 14.2 and 14.3).
Squamous cell carcinoma tends to appear as a well or ill-defined hypoechoic lesion that commonly infiltrates deeper layers (for example cartilage or muscle). Importantly, intra-lesional hyperechoic spots have not been reported in squamous cell carcinoma. Vascularity is usually more prominent compared to basal cell carcinoma. On color Doppler squamous cell carcinoma usually presents slow flow arterial and venous vessels [11] (Fig. 14.4).
(a, b) Squamous cell carcinoma. (a) Grey scale ultrasound (longitudinal view, left cheek) demonstrates a 3.38 cm (long) × 1.25 cm (depth) well defined hypoechoic lesion (asterisk) affecting dermis and hypodermis. (b) Color Doppler ultrasound (transverse view, frontal region) shows ill-defined hypoechoic lesion ( asterisk and outlined) that involves dermis and hypodermis. Notice the prominent blood flow within the mass (colors)
Melanoma, tend to show as a well- defined fusiform hypoechoic lesion that commonly present strong vascularity with slow flow vessels (arterial and venous). Hyperechoic spots have not been reported in melanoma. Ultrasound is also used to detect satellite (< 2 cm from the primary tumor), in–transit (≥ 2 cm from the primary tumor) or nodal metastases (Fig. 14.5). Locoregional sonographic staging of melanomas has allowed identification of the secondary involvement. The most common sonographic signs of malignant nodal infiltration are: balloon shape, nodular thickening of the cortex and loss of hyperechogenicity of the medullae. The anechoic areas frequently detected within the secondary lesions (extranodal or nodal) seem to be caused by the hypercellularity of the tumor rather than necrosis. Vascular density has been correlated with the metastatic potential in melanoma, and neovascularization has been described as a prognostic factor for metastasis equivalent to the Breslow index [3].
Conclusion
Ultrasound has proven to support the diagnosis of the skin cancer primary lesions and their locoregional staging. This non- invasive imaging technique can provide detailed anatomical data on extension in all axes, exact location, vascularity and deeper involvement.
References
Andrade P, Brites MM, Vieira R, Mariano A, Reis JP, Tellechea O, et al. Epidemiology of basal cell carcinomas and squamous cell carcinomas in a Department of Dermatology: a 5 year review. An Bras Dermatol. 2012;87:212–9.
Bartoš V, Pokorný D, Zacharová O, Haluska P, Doboszová J, Kullová M, et al. Recurrent basal cell carcinoma: a clinicopathological study and evaluation of histomorphological findings in primary and recurrent lesions. Acta Dermatovenerol Alp Panonica Adriat. 2011;20:67–75.
Wortsman X. Sonography of the primary cutaneous melanoma: a review. Radiol Res Pract. 2012;2012:814396.
Ekwueme DU, Guy G, Li C, Rim SH, Parelkar P, Chen SC. The health burden and economic costs of cutaneous melanoma mortality by race/ethnicity-United States, 2000 to 2006. J Am Acad Dermatol. 2011;65:S133–43.
Wortsman X, Wortsman J. Clinical usefulness of variable frequency ultrasound in localized lesions of the skin. J Am Acad Dermatol. 2010;62:247–56.
Bobadilla F, Wortsman X, Muñoz C, Segovia L, Espinoza M, Jemec GBE. Pre-surgical high resolution ultrasound of facial basal cell carcinoma: correlation with histology. Cancer Imaging. 2008;22:163–72.
Lassau N, Koscielny S, Avril MF, Margulis A, Duvillard P, De Baere T, et al. Prognostic value of angiogenesis evaluated with high-frequency and color Doppler sonography for preoperative assessment of melanomas. AJR Am J Roentgenol. 2002;178:1547–51.
Music MM, Hertl K, Kadivec M, Pavlović MD, Hocevar M. Pre-operative ultrasound with a 12–15 MHz linear probe reliably differentiates between melanoma thicker and thinner than 1 mm. J Eur Acad Dermatol Venereol. 2010;24:1105–8.
Murchison AP, Walrath JD, Washington CV. Non-surgical treatments of primary, non-melanoma eyelid malignancies: a review. Clin Experiment Ophthalmol. 2011;39:65–83.
Wortsman X, Jemec G. Common inflammatory diseases of the skin: from the skin to the screen. Adv Psor Inflamm Skin Dis. 2010;2:9–15.
Wortsman X. Common applications of dermatologic sonography. J Ultrasound Med. 2012;31(1):97–111.
Wortsman X. Sonography of facial cutaneous basal cell carcinoma: a first-line imaging technique. J Ultrasound Med. 2013;32:567–72.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Glossary
- Color Doppler Ultrasound
-
is a imaging technique which allows to visualize bloodflow. Using a Doppler effect, the US transducer detects pith changes found in vessels. A color value is assigned whether blood is moving forward or away from the transducer. In addition, color intensity will depend on the velocity of flow
- HFUS
-
High Frequency Ultrasound
- Hyperechoic
-
refers to an area that appears white. In skin malignant tumors, hyperechoic spots have been described inside basal cell carcinomas
- Hypoechoic
-
refers to an area that appears darker than the adjacent tissue. Skin malignant tumors (Basal and squamous cell carcinomas; melanomas) appear hipoechoic
- Spectral curve analysis of blood flow
-
is a tool that utilizes time, frequency, velocity and doppler signal power to give information on the blood flow. Vascular scattering can be represented as spectral wave velocity depending on time (velocity/time curve), or as dual-scale color mapping depending on the changes in average blood velocity. The flow-in is depicted in red and the flow-out in blue
Rights and permissions
Copyright information
© 2014 Springer Science+Business Media New York
About this chapter
Cite this chapter
Wortsman, X. (2014). Introduction to Ultrasonography in Skin Cancer. In: Baldi, A., Pasquali, P., Spugnini, E. (eds) Skin Cancer. Current Clinical Pathology. Humana Press, New York, NY. https://doi.org/10.1007/978-1-4614-7357-2_14
Download citation
DOI: https://doi.org/10.1007/978-1-4614-7357-2_14
Published:
Publisher Name: Humana Press, New York, NY
Print ISBN: 978-1-4614-7356-5
Online ISBN: 978-1-4614-7357-2
eBook Packages: MedicineMedicine (R0)