Abstract
The effects of aging on muscle tissue—in terms of total and regional muscle mass, muscle fiber size and number—and its clinical consequences with respect to muscle power, strength, and endurance have been investigated extensively during the past few decades. The aging process of striated muscle tissue is based on a complex (patho)physiological mechanism that includes numberous interacting factors, such as hormones, sex, nutrition, and physical activity. The histopathological, imaging, and functional (clinical) features of “normal aging muscle” have come under the umbrella of a coined term, “sarcopenia.” Although sarcopenia is a normal aging phenomenon, it has a substantial clinical and financial impact on health systems because the human life-span is increasing, particularly in the developed Western countries. Sarcopenia is strongly related to accidental falls and injuries as well as to a higher incidence of other systemic diseases including osteoporosis, obesity, and insulin resistance. Therefore, sarcopenia is substantially influencing the quality of life of the elderly as well as their life-span.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Introduction
The effects of aging on muscle tissue—in terms of total and regional muscle mass, muscle fiber size and number—and its clinical consequences with respect to muscle power, strength, and endurance have been investigated extensively during the past few decades. The aging process of striated muscle tissue is based on a complex (patho)physiological mechanism that includes numerous interacting factors, such as hormones, sex, nutrition, and physical activity. The histopathological, imaging, and functional (clinical) features of the “normal aging muscle” are referred to as “sarcopenia.” Although sarcopenia is a normal aging phenomenon, it has a substantial clinical and financial impact on health systems because the human life-span is increasing, particularly in the developed Western countries. Sarcopenia is strongly related to accidental falls and injuries as well as to a higher incidence of other systemic diseases including osteoporosis, obesity, and insulin resistance. Therefore, sarcopenia is substantially influencing the quality of life of the elderly as well as their life-span.
2 Sarcopenia
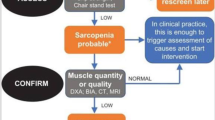
The literal interpretation of the Greek word sarcopenia is “poverty of flesh.” In general, this term describes the age-related changes of striated tissue. Using muscle mass assessment with dual-energy X-ray absorptiometry (DEXA), sarcopenia was defined in research studies as the loss of muscle tissue more than two standard deviations below the mean for young adults. In general, sarcopenia shows a high variability among patients of different ages.
3 Loss of Skeletal Muscle Mass
The total muscle mass is strongly age-dependent. It continuously increases until the age of 24 years. During the span from 24 to 50 years of age, the muscle mass decreases only slightly (∼10 %). In people older than 50 years, the reduction of muscle mass accelerates, and 30 % of muscle is lost between 50 and 80 years of age. Using imaging techniques—computed tomography (CT), magnetic resonance imaging (MRI), ultrasonography (US)—an annual reduction rate in the whole muscle size ranges from 0.5 % to 0.8 % beyond the age of 50 years based on cross-sectional data and 1.4 % based on longitudinal data (Figs. 11.1, 11.2, 11.3; see Chap. 2, Fig. 2.12). Adjusted for age, height, and body weight, men have more muscle tissue than women. However, men experience a higher degree of loss of muscle tissue during aging than do women. This phenomenon is not fully understood. It is probably due to a complex interaction of multiple factors including hormones (growth hormone, insulin-like growth factor, estrogen, testosterone), exercise, and lifestyle.
Axial computed tomography (CT) images obtained from a 33-year-old man (left) and an 88-year-old man in various anatomical regions. Note the generalized loss of muscle tissue, particularly the decreased muscle thickness in the older subject. Note also the increased amount of intermuscular and intramuscular fat tissue
Examples of age-related muscle changes in terms of muscle thickness in men for the biceps brachii, forearm flexor, quadriceps, and anterior tibial muscles. From Pillen S, Arts IMP, Zwarts MJ (2008) Muscle ultrasound in neuromuscular disorders. Muscle Nerve. 37:679–693. Reprinted with permission from John Wiley and Sons
Muscle echo intensity is dependent on age, data on 194 healthy volunteers. The muscle intensity is expressed as a value between 0 (black) and 255 (white). Note that the presented values are specific for the particular ultrasonography system used. During childhood, there are no substantial differences between boys and girls. From early adulthood on, men show lower muscle echo intensity than women. After the age of 40 years, the muscle echo intensity increases continuously. From Pillen S, Arts IMP, Zwarts MJ (2008) Muscle ultrasound in neuromuscular disorders. Muscle Nerve. 37:679–693. Reprinted with permission from John Wiley and Sons
The underlying pathophysiological mechanisms include a decrease in fiber size and number. The aging process in terms of fiber size reduction is more prominent in type II fibers. The reduction of the type II fiber area during aging is 20–50 % compared to 1–25 % of the fiber type I area (Fig. 11.4). Even among the type II fibers there seems to be differences in the degree of fiber size reduction. Several studies have conclusively demonstrated that type IIB fibers were more severely affected than type IIA fibers in elderly women and men.
(a) Age-related changes in (maximum) muscle force in terms of representative isometric twitch contractile responses. (b) Extensor digitorum longus muscle obtained from 16- to 28-month-old rats stained with myosin ATPase. Note the relative increase of the dark-stained type I fibers in the older muscles. From Ryall JG (2008) Cellular and molecular mechanisms underlying age-related skeletal muscle wasting and weakness. Biogerontology 9:213–228. Reprinted with permission from Springer
In contrast to the fiber size area, the reduction in fiber number does equally affect type I and type II muscle fibers. Data from postmortem studies have demonstrated that the number of type I and type II fibers has decreased by 50 % at the ninth decade compared to individuals at the age of 20 years. The rate of decrement in fiber number accelerates during the aging process. Between the third and fifth decade a 5 % reduction can be observed compared to a reduction of 35 % between the fifth and the eighth decades of life.
Although normal aging of the muscle tissue does not affect the overall ratio of fiber types in terms of fiber numbers, there is a certain fiber grouping that can be observed in aging muscle tissue. In young muscle tissue, the various fiber types are scattered, resulting in a normal “checkerboard” mosaic appearance, whereas in older muscle tissue several fibers types are arranged in groups. More recent studies focusing on the myosin heavy-chain composition of different muscle fibers showed that the number of so-called hybrid fibers, expressing more than a single myosin heavy chain isoform, is increased in aging muscle tissue.
4 Pathophysiology of Sarcopenia
Age-related denervation of striated muscle tissue is one of the most important factors leading to loss of muscle fibers/total muscle tissue and associated clinical manifestations in the elderly. It has been conclusively demonstrated that the number of α-motoneurons in the ventral horn of the spinal cord remains almost constant during life until the seventh decade. During the following years of life, the number of α-motoneurons decrease continuously. This leads to progressive denervation of muscle tissue, in turn leading to losses of functional motor units of the proximal and distal muscle in the upper and lower extremities and a subsequent increase in size of the remaining motor units. The chronic denervation process has been linked to possible underlying pathophysiological mechanisms regarding the phenomenon of fiber grouping in aging muscle tissue (described earlier). In addition, the progressive denervation process explains the acceleration of muscle tissue loss in the elderly and the rather constant muscle tissue volume in middle-aged persons. The underlying reason for the loss of motoneurons is still not understood. Molecules influencing function and survival of motoneurons such as the ciliary neurothrophic factor (CNTF) are currently being investigated.
In addition to chronic denervation, there are other multifactorial pathophysiological pathways that contribute to muscle fiber loss and atrophy in sarcopenia. They include hormonal, metabolic, nutritional, and immunological factors.
4.1 Protein Metabolism
Alterations in protein metabolism affect normal aging striated muscle tissue. They can be addressed from various (patho)physiological aspects. First, reduced protein synthesis is observed during the early stages of sarcopenia even in middle-aged persons (50–60 years) before age-related denervation occurs. To a certain extent, this can explain the observation that mild sarcopenia is present before denervation appears. The decline in protein synthesis particularly affects myofibrillar (actin, myosin) and mitochondrial proteins. The assumption that mitochondrial proteins (e.g., aerobic enzymes) are involved is supported by the fact that mitochondria and mitochondrial DNA levels are substantial reduced (approximately 40 %) in normal aging muscle tissue. This decline in oxidative phosphorylation, and therefore adenosine triphosphate (ATP) production, leads to overall impaired protein metabolism with consequences on muscle function.
4.2 Hormone Status
The decreasing blood-borne concentrations of anabolic hormones during aging represent an important factor contributing to sarcopenia. In elderly men, the concentrations of total testosterone and, more importantly, unbound testosterone are reduced by 35 % and 50 %, respectively, between the age of 20 to 80 years. The functioning of the hypothalamic-pituitary-gonadal axis influences the status of testosterone, particularly the circadian variation of testosterone concentrations, in elderly men. The multifactorial aspects of anabolic hormone dysfunction affecting the anabolic hormones include impaired secretion of gonadotropin-releasing hormone (GrH) by the hypothalamus, relative insensitivity of Leydig cells to luteinizing hormone (LH) (which normally stimulates testosterone secretion), and reduced responses of several tissue types (e.g., muscle tissue) to anabolic hormones. It has been conclusively demonstrated that adequate replacement of testosterone in elderly men is an effective treatment strategy regarding muscle mass recovery and has clinical benefits in terms of improved muscle strength.
Another important anabolic hormone that influences muscle metabolism, particularly in women, is the growth hormone (GH). Men and women show a 50 % reduction of GH levels between the age of 20 to 70 years, with a substantial effect on muscle mass reduction. GH also regulates the synthesis of insulin-like growth factor-1 (IGF-1). A reduced IGF-1 level is another contributing factor of sarcopenia. IGF-1 plays an important role in the recruitment of satellite cells in muscle tissue. Satellite cells in the muscle represent the proliferative reserve. Stimulation of satellite cells leads to muscle fiber proliferation. Thus, fewer satellite cells during aging limit the proliferative capacity. IGF-1 not only leads to a proliferation of satellite cells but also stimulates satellite cell mitosis. However, in contrast to testosterone replacement, a therapeutic benefit of GH supplementation has not been conclusively shown. GH replacement can lead to increased muscle mass but not to increased muscle strength. It is therefore not recommended as an effective treatment option in sarcopenia.
4.3 Nutrition
Nutritional status is an important contributing factor to sarcopenia in the elderly. Aging leads to an impaired nutritional state, for which the term “anorexia of aging” has been coined. The underlying pathophysiological mechanism of anorexia and sarcopenia is not fully understood. The impaired intake of proteins under a certain level is crucial for the maintenance of muscle tissue and the impaired intake of certain aliment that play an important role in muscle homeostasis (e.g., creatine) have been suggested as possible factors. The benefit of anorexia treatment in terms of clinical outcome measures (e.g., muscle strength) is still under debate and has not yet been conclusively demonstrated.
4.4 Inflammation
There is increasing evidence that inflammatory reactions in the muscle tissue contribute to sarcopenia. Particularly, increased levels of inflammatory cytokines such as interleukin-6 (IL-6), interleukin-1β (IL-1β), and tumor necrosis factor-α (TNFα) have been observed in aging muscle tissue. These cytokines have some catabolic effects. To what extent these inflammatory changes contribute to sarcopenia is currently under investigation.
4.5 Exercise
Reduced physical activity is a well-known phenomenon in the elderly and contributes significantly to sarcopenia. Resistance exercise can reverse age-related changes in muscle tissue in terms of an increase in muscle mass and benefits regarding functional outcome measures such as muscle strength. Exercise-induced increases in muscle mass (cross-sectional area) of up to 40 % have been reported. It is likely that resistance exercise acts in various ways, directly affecting the muscle tissue. Neuronal mechanisms are also being considered.
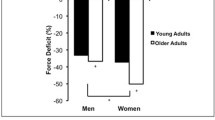
5 Loss of Muscle Function
Age-related loss of muscle strength is the most important clinical manifestation of sarcopenia. In general, the loss involves all domains including concentric, eccentric, and isometric strength, although eccentric strength is relatively preserved. The course of the muscle strength decline corresponds well with the age-related loss of muscle mass (Fig. 11.4). There are no substantial differences in the loss of muscle strength between proximal and distal limb muscles. After reaching 30 years of age, muscle strength shows almost constant values until age 50 years. A rather mild decrease in muscle strength is observed between the ages of 50 and 60 years, followed by a more accelerated loss of muscle strength in people older than 60 years. Men show higher values of muscle mass and strength at baseline, and their absolute loss of muscle strength is greater. However, both men and women show the same rate of age-related muscle strength decline. Several cross-sectional and longitudinal studies have been performed to estimate the rate of muscle strength reduction. The data are difficult to interpret because we are dealing with different baseline ages and different follow-up periods. In general, longitudinal studies show greater declines than do cross-sectional studies. Roughly, a decrease of approximately 15 % per decade is observed in persons beyond the fifth decade of life. Please consider the suggestions for further reading (below) for more detailed information on this topic. Physical activity, particularly resistance training, can influence and recover muscle strength to a certain extent even in very old persons.
In contrast to muscle strength, muscle endurance or, in other words, muscular fatigue is not strongly related to sarcopenia. Studies investigating the effect of aging on muscle endurance are inconclusive, probably due at least partly to methodological differences and difficulties. It has been shown that fatigue in the elderly is not linked to differences of the contractile components in muscle tissue. It has therefore been postulated that fatigue in aged muscle is more likely caused by altered central nervous system factors.
Normal Aging Muscle Tissue
Key Points
-
The term sarcopenia describes age-related changes in muscle tissue in terms of muscle mass and muscle strength.
-
The age-related changes in muscle tissue accelerate in patients beyond the seventh decade of life.
-
The pathophysiology of sarcopenia is complex and multi-factorial, including features of denervation, inflammation, metabolic and hormonal changes, nutritional status, and physical activity.
-
Imaging modalities (US, CT, MRI) are useful for assessing and quantifying the degree of sarcopenia in the elderly.
-
Physical activity (resistance training) is helpful for slowing down the process of sarcopenia and recovering muscle strength.
Suggestions for Further Reading
-
Arts IM, Pillen S, Overeem S, et al. Rise and fall of the skeletal muscle over the entire life span. J Am Geriatr Soc. 2007;55:1150–2.
-
Brown M. Skeletal muscle and bone: effect of steroids and ageing. Adv Physiol Educ. 2008;32:120–6.
-
Doherty TJ. Invited review: ageing and sacropenia. J Appl Physiol. 2003;95:717–27.
-
Kanehisa H, Ikegawa S, Tsunoda N, et al. Cross sectional areas of fat and muscle in limbs during growth and middle age. In J Sports Med. 1994;15:420–5.
-
Roubenhoff R, Hughes VA. Sarcopenia: current concepts. J Gerontol A Biol Sci Med Sci. 2000;55:M716–24.
-
Ryall JG, Schertzer JD, Lynch GS. Cellular and molecular mechnanism underlying age related skeletal muscle wasting and weakness. Biogerontology. 2008;9:213–28.
-
Sakuma K, Yamaguchi A. Novel intriguing strategies attenuating to sarcopenia. J Aging Res. 2012;2012:251217
-
Wang C, Bai L. Sarcopenia in the elderly: basic and clinical issues. Geriatr Gerontol Int. 2012;12:388–96.
-
Welle S. Cellular and molecular basis of age-related sarcopenia. Can J Appl Physiol. 2002;27:19–41.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2013 Springer Science+Business Media New York
About this chapter
Cite this chapter
Wattjes, M.P., Fischer, D. (2013). Normal Aging Muscle Tissue. In: Wattjes, M., Fischer, D. (eds) Neuromuscular Imaging. Springer, New York, NY. https://doi.org/10.1007/978-1-4614-6552-2_11
Download citation
DOI: https://doi.org/10.1007/978-1-4614-6552-2_11
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4614-6551-5
Online ISBN: 978-1-4614-6552-2
eBook Packages: MedicineMedicine (R0)