Abstract
With the recent development of confocal endomicroscopy, bronchoscopy has now entered the era of in vivo microscopic imaging. Confocal fluorescence endomicroscopy is based on the principle of confocal microscopy, where the microscope objective has been replaced by fiber-optic probes. Two endomicroscope systems could theoretically be used for human explorations, differing by the position of the scanning system into the device. Due to the respiratory tract size, the only system currently available, called “probe-based confocal laser endomicroscopy” (or pCLE), uses the principle of proximal scanning. This system produces images through a 1 mm flexible miniprobe that can enter the 2 mm working channel of the bronchoscope. pCLE has a lateral resolution of 3 μm and produces real-time imaging at 9 frames per second. pCLE has the capability to image, at a microscopic scale, the fluorescence of the bronchial epithelial and subepithelial layers, as well as the more distal parts of the lungs, from the terminal bronchioles down to the alveolar ducts and sacs. Confocal endomicroscopy can be coupled with nuclear fluorescent dyes and has the potential to image targeted fluorescent molecular probes. Potential applications of FCFM include “optical biopsy” of early bronchial cancers, bronchial wall remodeling evaluation, diffuse peripheral lung disease exploration, as well as in vivo diagnosis of peripheral lung nodules.
This chapter details the capabilities and possible limitations of confocal microendoscopy for proximal and distal lung exploration with special focus on lung cancer imaging in vivo.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Methylene Blue
- Peripheral Nodule
- Basement Membrane Zone
- Confocal Laser Endomicroscopy
- Pulmonary Alveolar Proteinosis
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Introduction
The principle of confocal microscopy, first described in 1957, relies on both the use of a narrow point illumination light source, which focuses on a single spot in the sample, and of a small aperture or pinhole on the detection path, which focuses the light emitted back by the sample onto the detector. This results in the rejection of out-of-focus information from the material above and below a very thin plane of focus. The illumination and detection systems being conjugated on the same focal plane are termed “confocal.” As only one point in the sample is illuminated at a time, confocal microscopes make use of systems that scan the sample in both lateral dimensions to produce a two-dimensional image—or “slice”—of a few microns depth, parallel to the sample surface. This principle allows confocal microscopes to provide “optical” sectioning of cells and tissue with micrometric lateral and axial resolutions, without tissue destruction. Confocal microscopes have recently been so successfully miniaturized [1, 2] that they can be integrated into endoscopic systems and used for both animal [3–5] and human in vivo explorations [6–8]. This is achieved by using a small optical device held in direct contact with the area to be imaged. Such systems have recently been applied to the in vivo microscopic imaging of both the proximal [7] and distal respiratory systems [8]. With these recent developments, fiber-optic endoscopy of the respiratory tract has now entered the era of in vivo microscopic imaging.
In general, the aim of confocal endomicroscopes is to produce “optical biopsies,” i.e., in vivo microscopic imaging, of a living tissue during endoscopy [9, 10]. Ideally, this direct microscopic imaging could replace tissue sampling or at least allow a very precise targeting of the biopsy area. However, because of optical limitations due to refraction indexes and specular reflexion of the light at the surface of the tissue, reflectance (or “white light”) confocal endomicroscopes are not currently available. Instead, manufacturers have designed fluorescence confocal devices, where the excitation light can easily be filtered out before the light reaches the detector, to only image the fluorescence emitted from the tissue. Obviously, the main limitations of these systems come from the fact that they exclusively record the signal coming from fluorescent structures in response to appropriate excitation wavelengths. Therefore, besides the unusual “en face view,” recorded images may appear for the clinical quite different from its classical histopathology counterparts or require specific cellular fluorophores. On the other hand, in future applications, fluorescence confocal systems may take advantage of molecular-targeted imaging using smart fluorescent probes.
Confocal Endomicroscopes for Human Exploration
The first confocal endomicroscopic systems for human exploration were available in 2005. Two systems have been commercialized that can be distinguished by the technical approach used to conduct the light to the tissue.
The distal scanning principle is used in the Optisan®/Pentax endomicroscopic system. This system is also called a confocal laser endomicroscope—CLE. In distal scanning, the light is conducted by a single fiber back and forth from the distal tip of the system, and the scanning function is accomplished by a very small scanhead (4.5 cm long × 3.5 mm diameter) which is included in the distal end of the endoscope. Tissue fluorescence is induced by a 488 nm laser wavelength. The sensitivity of the system needs the use of IV Fluoresceine as an external fluorophore. The system has an impressive lateral resolution below 1 μm and produces optical slices of 7 μm for a field of view of 475 × 475 μm. The system offers the possibility to adjust the Z-depth range from 0 to 250 μm below the contact surface, so that three-dimensional structures in the specimen and successive layers of the mucosae can be imaged. However, because of the added sizes of the distal scanhead, working channel, conventional light guide, and CCD camera, the diameter of the distal tip of the endoscope is larger than 12 mm, a size barely compatible with the exploration of the human trachea and large main bronchi, which explains why only a confocal GI endoscope had been launched over the past years. Another limitation is due to the miniaturization of the distal scanhead that results in scanning rates of 1 frame/s, which needs a very efficient stabilization system of the distal tip of the endoscope onto the mucosae, in order to produce crisp microscopic images of the epithelium. In spite of these limitations, Optiscan® endomicroscopic images from the gastrointestinal tract appear very close to conventional histology.
This prototype system is able to provide “en face” imaging of the bronchial epithelium with a lateral resolution of less than one micrometer.
Recently, endomicroscopic images of the proximal bronchial tree of both normal and tumoral epithelium have been obtained by Musani et al. from 5 patients, using a miniaturized prototype of the Optiscan system [11]. The confocal device was composed of a 6.2 mm flexible bronchoscope, devoid of working channel and distal optics, in which the distal end has been replaced by a 4.4 cm scanning device. This prototype was introduced within a 12.5 mm rigid bronchoscope in parallel to the rigid optics. Fluoresceine IV infusion was administered before the procedure. Because of the rigidity of the prototype distal tip, the confocal exploration was limited to the primary and secondary carina of the main bronchus and to an endobronchial mass in one patient. En face images of the respiratory produced by the system were impressive, with a lateral resolution of less than 1 μm, that allowed clear imaging of the intercellular margins between the normal epithelial cells, as well as imaging of the basement membrane/subepithelial areas due to folds of the epithelium (Fig. 14.1). Motion artifacts were observed in 60% of the frames, which allowed interpretation of the images in all patients.
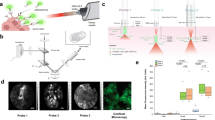
The second commercially available confocal endomicroscopy system (Cellvizio®, Mauna Kea Technologies, Paris, France) uses the principle of proximal scanning in which the illumination light scans the proximal part of a coherent fiber bundle or miniprobe. This bundle conducts the light back and forth from the imaged area at the tip of the miniprobe [12]. The light delivery, scanning, spectral filtering, and imaging systems are located at the proximal part of the device, the distal part being a separate miniprobe, including both the fiber bundle and its connector to the laser scanning unit (Fig. 14.2).
This fiber bundle-based system, also described as “fibered confocal fluorescent microscopy (FCFM)” or more recently “probe-based confocal laser endomicroscopy” or “pCLE,” uses very thin and flexible miniprobes (300 μm to 2 mm in diameter) that can contain up to 30,000 compacted microfibers. Similar to bench confocal microscopes, pCLE uses two rapidly moving mirrors to scan the microfibers across the coherent fiber bundle in a raster fashion. Each microfiber, which is scanned one at a time by the laser light, acts as a light delivery and collection system and is, in essence, its own pinhole. The main advantages of this design is the very small size and the flexibility of the probe that can reach the more distal part of the lungs [8], as well as the fast image collection speed that helps to avoid artifacts due to tissue movement. The system produces endomicroscopic imaging in real time at 9–12 frames/s.
Specific miniprobes for bronchial and alveolar imaging (Alveoflex®) have a diameter of 1 mm or less that can enter the working channel of any adult bronchoscope. These probes are designed for only 20 uses, at an approximate cost of 5,000 euros/miniprobe. Alveoflex® miniprobes are devoid of distal optics and have a depth of focus of 0–50 μm, a lateral resolution of 3 μm for a field of view of 600 × 600 μm. Thinner and more flexible probes are available for other applications as for the bile duct exploration (Cholangioflex®) or even probes that can fit into a 19 gauge needle (AQ-Flex®) for endoscopic ultrasound (EUS) lymph node/cysts explorations. Those probes may prove useful in the future for specific intrathoracic applications.
Two pCLE devices using different excitation wavelengths are currently available. The Cellvizio 488 nm is used for autofluorescence imaging of the respiratory tract as well as for fluorescein-induced imaging of the GI tract [7, 8, 13]. Another device at 660 nm excitation can be used for epithelial cell imaging after topical application of exogenous fluorophores such as methylene blue [14–16]. Whereas these two systems are currently sold as separate devices, a dual-band system is currently available for small animal imaging that avoids to disconnect the miniprobe from the LSU in case a dual imaging (488 nm/660 nm with methylene blue) would be indicated.
pCLE Imaging of the Proximal Bronchi
pCLE can easily be performed during a fiber-optic bronchoscopy under local anesthesia [7, 8]. The technique of in vivo bronchial pCLE imaging is simple: the miniprobe is introduced into the 2 mm working channel of the bronchoscope and the probe tip applied onto the bronchial mucosae under sight control. The depth of focus being 50 μm below the contact surface, the system can image the first layers of the bronchial subepithelial connective tissue, presumably the lamina densa and the lamina reticularis [7].
At 488 nm excitation, pCLE produces very precise microscopic fluorescent images of the bronchial basement membrane zone (Fig. 14.3). pCLE bronchial microimaging reveals a mat of large fibers mainly oriented along the longitudinal axis of the airways with cross-linked smaller fibers, as well as larger openings—100 to 200 μm—corresponding to the bronchial glands origins. In vivo, the technique also makes it possible to record high resolution images of small airways such as terminal bronchioles, which are recognizable by the presence of the helicoidal imprint of the smooth muscle on the inner part of the bronchiole [7].
Bronchial confocal microendoscopy imaging. (a) Normal elastic-fibered network of the basement membrane zone. (b) Disorganized basement membrane zone elastic network at the vicinity of a bronchial CIS. (c) Regular normal bronchial epithelium 660 nm excitation FCFM after topical application of methylene blue (0.1%). (d) CIS imaging, FCFM at 660 nm and topical methylene blue. Modified from Musani et al. J Bronchol Intervent Pulmonol, 2010 [11], with permission of the author
Fluorescence properties of the bronchial mucosae at 488 nm excitation are determined by the concentration of various cellular and extracellular fluorophores, including the intracellular flavins, that could originate from the epithelial cells, and specific cross-links of collagens and elastin present in the subepithelial areas [2, 17, 18]. Microspectrometer experiments coupled with pCLE imaging have clearly demonstrated that the main fluorescence signal emitted after 488 nm excitation from both bronchial and alveolar human system originates from the elastin component of the tissue [7, 8, 19]. Indeed, flavin cellular autofluorescence appears too weak to allow imaging of the epithelial layer using 488 nm pCLE without exogenous fluorophore [20]. Similarly, the collagen fluorescence does not significantly affect the pCLE image produced at 488 nm, the fluorescence yield of collagen at this wavelength being at least one order of magnitude smaller than that of elastin.
As a result, 488 nm excitation pCLE specifically images the elastin respiratory network that is contained in the basement membrane of the proximal airways and participates to the axial backbone of the peripheral interstitial respiratory system. In the future, it is possible that a modified pCLE device using several wavelengths [21] or devices based on a multiphoton approach [22–24] may enable imaging of collagen, elastin, and flavins simultaneously.
Distal Lung pCLE Imaging In Vivo: From the Distal Bronchioles Down to the Lung Acini
In the acinus, elastin is present in the axial backbone of the alveolar ducts and alveolar entrances, as well as in the external sheath of the extra-alveolar microvessels [25, 26]. pCLE acinar imaging is easily obtained by pushing forward the probe a few centimeters after the endoscope is distally blocked into a subsegmental bronchi. When progressing towards the more distal parts of the lungs, the entry into the alveolar space is obtained by penetration through the bronchiolar wall. Alveolar fluorescence imaging in active smokers dramatically differs from imaging in nonsmokers. The alveolar areas of smokers are usually filled with highly fluorescent cells corresponding to alveolar fluorescent macrophages, the presence of which appears very specific of active smoking [8]. In situ alveolar microspectrometric measurements have been performed in active smokers, which evidenced that the main fluorophore contributing to the pCLE alveolar signal corresponds to the tobacco tar by itself, explaining this difference [8, 19].
Potential Clinical Applications for Lung Cancer Detection in the Proximal Tree Using pCLE
Preliminary studies have shown that per endoscopic pCLE could be used to study specific basement membrane remodeling alterations in benign or malignant/premalignant bronchial alterations [7, 27]. In the first human study using pCLE in the respiratory tract in vivo, the structure of the bronchial wall was analyzed in 29 patients at high risk for lung cancer that also underwent an autofluorescence bronchoscopy [7]. In this study, the fibered network of the basement membrane zone underlying premalignant epithelia was found significantly altered. This was observed in one invasive cancer, three CIS, two mild and one moderate dysplastic, and three metaplastic lesions. In these precancerous conditions, the elastic fibered pattern of the lamina reticularis was found absent or disorganized (Fig. 14.4). This supported the hypothesis of an early degradation of the basement membrane components in preinvasive bronchial lesions. However, while this observation shed some light on the origin of the autofluorescence defect in precancerous bronchial lesions, the absence of epithelial cell visualization did not allow the technique to differentiate between the different grades of progression of the precancerous bronchial lesions such as metaplasia/dysplasia/carcinoma in situ.
pCLE imaging of normal distal lung and peripheral lung nodule. (a) pCLE imaging of normal distal lung. (b) Interstitial fiber network disorganization in a peripheral lung adenocarcinoma (488 nm excitation wave length). (c) pCLE cellular imaging of a peripheral lung adenocarcinoma (660 nm excitation and topical methylene blue). (d) pCLE cellular imaging of a peripheral small-cell lung cancer (660 nm excitation and topical methylene blue)
In order to be successfully applied to the exploration of precancerous/cancerous bronchial epithelial layer, the pCLE technique would need to be coupled with the use of an exogenous nontoxic fluorophore. Ex vivo studies have shown that the resolution of the system is not a limitation for nuclear or cellular imaging [7, 8].
A few exogenous fluorophores could be activated at 488 nm.
Acriflavin hydrochloride is an acridine-derived dye containing both proflavine and euflavine, which binds to DNA by intercalating between base pairs. Acriflavin produces a strong nuclear fluorescence with 488 nm pCLE when topically applicated on the top of the bronchial epithelium ex vivo [7]. Acriflavin has been used in a couple of in vivo study using CLE in the GI tract [28], without demonstrated side effect. However, comet assay of cells exposed in vitro to acriflavin solution shows significant DNA damage after 2 nm illumination with 488 nm Cellvizio (personal data). This observation needs further studies before acriflavin use for bronchial explorations, especially in patients at risk for cancer. Acriflavin is not currently approved for bronchial use.
Fluorescein has been used in Musani study with some success [11]. However, fluorescein, which does not enter the cells and therefore does not stain the nuclei [29], does not provide cellular imaging using pCLE. This is probably linked to the lower lateral resolution of pCLE compared to CLE and the impossibility to distinguish intercellular space with pCLE. Recently, Lane et al. have used a confocal microendoscope prototype at 488 nm excitation and topical physiological PH cresyl violet to provide cellular contrast in the bronchial epithelium both in vitro and in vivo [30].
Methylene blue is a nontoxic agent which is commonly used during bronchoscopy for the diagnostic of broncho-pleural fistulae. MB is also used in gastroenterology for chromo-endoscopic detection of precancerous lesions [31–33], as well as for in vivo microscopic examination of the GI tract and bronchus using a novel endocytoscopic system [34, 35]. MB is a potent fluorophore which enters the nuclei and reversibly binds to the DNA, before being reabsorbed by the lymphatics. In order to give a fluorescent signal, MB needs to be excited around 660 nm and is therefore accessible to FCFM intravital imaging using this excitation wavelength. In our hands, no DNA damage could be observed using comet assay from lymphocytes exposed to methylene blue in vitro and 660 nm Cellvizio for 2 min.
Human preliminary study has demonstrated that Cellvizio 660/topical methylene blue makes it possible to reproducibly image the normal and tumoral epithelial layer of the main bronchi [16, 36]. Unpublished data from our center also show that the technique easily differentiates small-cell lung cancer from non-small-cell lung cancer in vivo and normal epithelium from CIS (Fig. 14.3). Future studies using this technique have to show whether the technique allows to differentiate normal, premalignant, and malignant alterations at the microscopic level. If this strategy is successful, FCFM may become a very powerful technique for in vivo diagnostic of early malignant and premalignant conditions of the bronchial tree, allowing the analysis of both the epithelial and subepithelial layers during the same procedure.
pCLE for the Exploration of Peripheral Lung Nodules
Potential applications for in vivo distal lung imaging using pCLE appear wide. Some limitations of the technique could be predicted from its basic principles, such as artifacts linked to fragile parenchymal lung structures compression, as well as difficulties of interpretation of an imaging technique mainly based on elastin network assessment. However, preliminary results are encouraging in specific diffuse or focal lung diseases, such as in pulmonary alveolar proteinosis [37], diffuse emphysema [38], or peripheral lung nodules.
Coupled to electromagnetic navigation or radial EBUS, pCLE has the potential to image microstructural and cellular patterns of peripheral solid lung nodules in vivo at both 448 nm and 660 nm [15, 16] (Fig. 14.4). After navigation bronchoscopy to the peripheral nodule has been achieved and the peripheral nodule located, the Alveoflex® miniprobe can enter the extended working channel of both radial EBUS or superdimension system, except for the posterior and apical segments of the upper lobe due to the relative rigidity of the miniprobe. In such case, a smaller probe such as the Cholangioflex® should be used.
Confocal imaging of the peripheral nodule can be performed at either 488 nm (autofluorescence) or 660 nm after distal deposition of a few microliters of methylene blue for cellular imaging.
Recently, Arenberg et al. made use of pCLE at 488 nm to explore peripheral lung nodule in 39 patients from two centers [39]. Three investigators with different pCLE experiences met to develop descriptive criteria through a consensus review of 5 teaching and 5 training cases. Twenty-nine randomized pCLE sequences of lung nodules were secondly blindly reviewed and scored. The more reliable criteria for lung cancer diagnostic was the “solid” or “compact” pattern (Fig. 14.4). Interobserver agreement for this item was moderate (0.54). Using this single item, the sensitivities of detection of cancer are 70%, 70%, and 80% for the three observers, with specificities of 58%, 58%, and 74%, respectively. Future studies will assess the technique as an aid to localize the peripheral nodule and to differentiate benign from cancerous lesion.
Besides autofluorescence solid pattern at 488 nm, we have shown that topical methylene blue/660 nm pCLE makes it possible to image the cellular organization of peripheral lung nodules [15] and to differentiate small-cell lung cancers from the other histological type (Fig. 14.4). Again, more studies are needed to determine if the technique has a place in the clinical assessment of peripheral nodules.
Conclusion
Confocal fluorescence endomicroscopy is an emerging fascinating technique that allows optical microimaging of both the proximal and distal bronchial tree. Potential applications for lung cancer diagnosis include the exploration of both basement membrane alteration and epithelial layer of the proximal airways, as well as peripheral nodule assessment. Until now, pCLE only used endogenous autofluorescence or simple fluorescent contrast agents. In the future, the use of fluorescent molecular compounds will make it possible to extend applications of the technique. Pilot studies exploring this strategy have recently been published that provided specific confocal imaging of molecular probes in precancerous conditions of the oral cavity ex vivo [40] and of colonic dysplasia in vivo [41], and even invasive fungal diseases [42]. Coupled to FCFM, molecular imaging may help in the future to enable early diagnosis, rapid typing of molecular markers, and assessment of therapeutic outcome in many lung diseases.
References
St. Croix CM, Leelavanichkul K, Watkins SC. Intravital fluorescence microscopy in pulmonary research. Adv Drug Deliv Rev. 2006;58(7):834–40.
MacAulay C, Lane P, Richards-Kortum R. In vivo pathology: microendoscopy as a new endoscopic imaging modality. Gastrointest Endosc Clin N Am. 2004;14(3):595–620.
Boyette LB, Reardon MA, Mirelman AJ, Kirkley TD, Lysiak JJ, Tuttle JB, Steers WD. Fiberoptic imaging of cavernous nerves in vivo. J Urol. 2007;178(6):2694–700.
Le Goualher G, Perchant A, Genet M, Cave C, Viellerobe B, Berier F, Abrat B, Ayache N. Towards optical biopsies with an integrated fibered confocal fluorescence microscope. Lect Notes Comput Sci. 2004;3217(11):761–8.
Vincent P, Maskos U, Charvet I, Bourgeais L, Stoppini L, Leresche N, Changeux JP, Lambert R, Meda P, Paupardin-Tritsch D. Live imaging of neural structure and function by fibred fluorescence microscopy. EMBO Rep. 2006;7(11):1154–61.
Hoffman A, Goetz M, Vieth M, Galle PR, Neurath MF, Kiesslich R. Confocal laser endomicroscopy: technical status and current indications. Endoscopy. 2006;38(12):1275–83.
Thiberville L, Moreno-Swirc S, Vercauteren T, Peltier E, Cave C, Bourg Heckly G. In vivo imaging of the bronchial wall microstructure using fibered confocal fluorescence microscopy. Am J Respir Crit Care Med. 2007;175:22–31.
Thiberville L, Salaun M, Lachkar S, Dominique S, Moreno-Swirc S, Vever-Bizet C, Bourg-Heckly G. Human in-vivo fluorescence microimaging of the alveolar ducts and sacs during bronchoscopy. Eur Respir J. 2009;33(5):974–85.
Kiesslich R, Goetz M, Neurath MF. Virtual histology. Best Pract Res Clin Gastroenterol. 2008;22(5):883–97.
Guillaud M, Richards-Kortum R, Follen M. Paradigm shift: a new breed of pathologist. Gynecol Oncol. 2007;107(1 Suppl 1):S46–9.
Musani A, Sims MW, Sareli C, Russell W, McLaren W, Delaney P, Litzky L, Panettieri RA. A pilot study of the feasibility of confocal endomicroscopy for examination of the human airway. J Bronchol Intervent Pulmonol. 2010;17(2):126–30.
Georges Le Goualher AP, Genet M, Cave C, Viellerobe B, Berier F, Abrat B, Ayache N. Towards optical biopsies with an integrated fibered confocal fluorescence microscope. Lect Notes Comput Sci. 2004;3217(11):761–8.
Meining A, Schwendy S, Becker V, Schmid RM, Prinz C. In vivo histopathology of lymphocytic colitis. Gastrointest Endosc. 2007;66(2):398–9, discussion 400. Discussion 400.
Peng Q, Brown SB, Moan J, Nesland JM, Wainwright M, Griffiths J, Dixon B, Cruse-Sawyer J, Vernon D. Biodistribution of a methylene blue derivative in tumor and normal tissues of rats. J Photochem Photobiol B. 1993;20(1):63–71.
Thiberville L, Salaün M, Lachkar S, Moreno-Swirc S, Bourg-Heckly G. In-vivo confocal endomicroscopy of peripheral lung nodules using 488nm/660 nm induced fluorescence and topical methylene blue (abstract). Proceedings of European Respiratory Society Meeting; 2008; Berlin: European Respiratory Society; 2008. p. 263s.
Thiberville L, Salaün M, Moreno-Swirc S, Bourg Heckly G. In vivo endoscopic microimaging of the bronchial epithelial layer using 660 nm fibered confocal fluorescence microscopy and topical methylene blue. Proceedings of European Respiratory Society Meeting; 2007; Stockolm: European Respiratory Society; 2007. p. 712S.
Gabrecht T, Andrejevic-Blant S, Wagnieres G. Blue-violet excited autofluorescence spectroscopy and imaging of normal and cancerous human bronchial tissue after formalin fixation. Photochem Photobiol. 2007;83(2):450–8.
Richards-Kortum R, Sevick-Murac E. Quantitative optical spectroscopy for tissue diagnosis. Annu Rev Phys Chem. 1996;47:555–606.
Bourg Heckly G, Thiberville L, Vever-Bizet C, Vielerobe B. In vivo endoscopic autofluorescence microspectro-imaging of bronchi and alveoli. Proc SPIE. 2008;2008:6851.
Qu J, MacAulay C, Lam S, Palcic B. Laser-induced fluorescence spectroscopy at endoscopy:tissue optics, Monte Carlo modeling and in vivo measurements. Opt Eng. 1995;34:3334–43.
Jean F, Bourg-Heckly G, Viellerobe B. Fibered confocal spectroscopy and multicolor imaging system for in vivo fluorescence analysis. Opt Exp. 2007;15(7):4008–17.
Skala MC, Squirrell JM, Vrotsos KM, Eickhoff JC, Gendron-Fitzpatrick A, Eliceiri KW, Ramanujam N. Multiphoton microscopy of endogenous fluorescence differentiates normal, precancerous, and cancerous squamous epithelial tissues. Cancer Res. 2005;65(4):1180–6.
Peyrot DA, Lefort C, Steffenhagen M, Mansuryan T, Ducourthial G, Abi-Haidar D, Sandeau N, Vever-Bizet C, Kruglik SG, Thiberville L, Louradour F, Bourg-Heckly G. Development of a nonlinear fiber-optic spectrometer for human lung tissue exploration. Biomed Opt Exp. 2012;3(5):840–53.
Pavlova I, Hume KR, Yazinski SA, Flanders J, Southard TL, Weiss RS, Webb WW. Multiphoton microscopy and microspectroscopy for diagnostics of inflammatory and neoplastic lung. J Biomed Opt. 2012;17(3):036014.
Weibel ER, Sapoval B, Filoche M. Design of peripheral airways for efficient gas exchange. Respir Physiol Neurobiol. 2005;148(1–2):3–21.
Weibel ER, Hsia CC, Ochs M. How much is there really? Why stereology is essential in lung morphometry. J Appl Physiol. 2007;102(1):459–67.
Yick CY, von der Thusen JH, Bel EH, Sterk PJ, Kunst PW. In vivo imaging of the airway wall in asthma: fibered confocal fluorescence microscopy in relation to histology and lung function. Respir Res. 2011;12(1):85.
Kiesslich R, Burg J, Vieth M, Gnaendiger J, Enders M, Delaney P, Polglase A, McLaren W, Janell D, Thomas S, Nafe B, Galle PR, Neurath MF. Confocal laser endoscopy for diagnosing intraepithelial neoplasias and colorectal cancer in vivo. Gastroenterology. 2004;127(3):706–13.
Becker V, von Delius S, Bajbouj M, Karagianni A, Schmid RM, Meining A. Intravenous application of fluorescein for confocal laser scanning microscopy: evaluation of contrast dynamics and image quality with increasing injection-to-imaging time. Gastrointest Endosc. 2008;68(2):319–23.
Lane P, Lam S, McWilliams A, leRiche J, Anderson M, MacAulay C. Confocal fluorescence microendoscopy of bronchial epithelium. J Biomed Opt. 2009;14(2):024008.
Kiesslich R, Fritsch J, Holtmann M, Koehler HH, Stolte M, Kanzler S, Nafe B, Jung M, Galle PR, Neurath MF. Methylene blue-aided chromoendoscopy for the detection of intraepithelial neoplasia and colon cancer in ulcerative colitis. Gastroenterology. 2003;124(4):880–8.
Taghavi SA, Membari ME, Dehghani SM, Eshraghian A, Hamidpour L, Khademalhoseini F. Comparison of chromoendoscopy and conventional endoscopy in the detection of premalignant gastric lesions. Can J Gastroenterol. 2009;23(2):105–8.
Marion JF, Waye JD, Present DH, Israel Y, Bodian C, Harpaz N, Chapman M, Itzkowitz S, Steinlauf AF, Abreu MT, Ullman TA, Aisenberg J, Mayer L. Chromoendoscopy-targeted biopsies are superior to standard colonoscopic surveillance for detecting dysplasia in inflammatory bowel disease patients: a prospective endoscopic trial. Am J Gastroenterol. 2008;103(9):2342–9.
Inoue H, Kazawa T, Sato Y, Satodate H, Sasajima K, Kudo SE, Shiokawa A. In vivo observation of living cancer cells in the esophagus, stomach, and colon using catheter-type contact endoscope, “Endo-Cytoscopy system”. Gastrointest Endosc Clin N Am. 2004;14(3):589–594, x–xi.
Shibuya K, Yasufuku K, Chiyo M, Nakajima T, Fujiwara T, Nagato K, Suzuki H, Iyoda A, et al. Endo-cytoscopy system is a novel endoscopic technology to visualize microscopic imaging of the tracheobronchial tree (abstract). Proceedings of European Respiratory Society Meeting; 2008; Berlin: European Respiratory Society; 2008. p. 263s.
Thiberville L, Salaün M, Lachkar S, Dominique S, Moreno-Swirc S, Vever-Bizet C, Bourg Heckly G. In-vivo confocal fluorescence endomicroscopy of lung cancer. J Thorac Oncol. 2009;4(9):S49–51.
Salaun M, Roussel F, Hauss PA, Lachkar S, Thiberville L. In vivo imaging of pulmonary alveolar proteinosis using confocal endomicroscopy. Eur Respir J. 2010;36(2):451–3.
Thiberville L, Salaün M, Hauss PA, Lachkar S, Dominique S. In vivo microimaging of the alveolar capillary network during alveoscopy (abstract). Proceedings of European Respiratory Society Meeting; 2009; Vienna; 2009.
Arenberg DA, Gildea T, Wilson D. Proposed classification of probe-based confocal laser endomicroscopy (PCLE) findings for evaluation of indeterminate peripheral lung nodules. Am J Respir Crit Care Med. 2011;183:A6097.
Hsu ER, Gillenwater AM, Hasan MQ, Williams MD, El-Naggar AK, Richards-Kortum RR. Real-time detection of epidermal growth factor receptor expression in fresh oral cavity biopsies using a molecular-specific contrast agent. Int J Cancer. 2006;118(12):3062–71.
Hsiung PL, Hardy J, Friedland S, Soetikno R, Du CB, Wu AP, Sahbaie P, Crawford JM, Lowe AW, Contag CH, Wang TD. Detection of colonic dysplasia in vivo using a targeted heptapeptide and confocal microendoscopy. Nat Med. 2008;14(4):454–8.
Morisse H, Heyman L, Salaun M, Favennec L, Picquenot JM, Bohn P, Thiberville L. In vivo and in situ imaging of experimental invasive pulmonary aspergillosis using fibered /confocal fluorescence microscopy. Med Mycol. 2012;50(4):386–95.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2013 Springer Science+Business Media New York
About this chapter
Cite this chapter
Thiberville, L., Salaun, M. (2013). Diagnostic of Lung Cancer: Confocal Bronchoscopy. In: Díaz-Jimenez, J., Rodriguez, A. (eds) Interventions in Pulmonary Medicine. Springer, New York, NY. https://doi.org/10.1007/978-1-4614-6009-1_14
Download citation
DOI: https://doi.org/10.1007/978-1-4614-6009-1_14
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4614-6008-4
Online ISBN: 978-1-4614-6009-1
eBook Packages: MedicineMedicine (R0)