Abstract
Since its beginnings in the early 1970s, clinical nuclear cardiology has evolved substantially, gaining both technical sophistication and enhanced imaging capabilities. Importantly, in parallel to these developments, an extensive literature supporting the clinical and cost-effectiveness of this modality has developed. Today, state-of-the-art nuclear cardiology allows for the objective measurement of both myocardial function and relative regional myocardial perfusion at rest and stress, providing accurate risk assessment in a wider variety of patient subsets. This chapter will highlight stress myocardial perfusion single-photon emission CT (SPECT), which currently comprises approximately 95 % of the procedures performed in this field.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Myocardial Perfusion
- Nuclear Cardiology
- Invasive Coronary Angiography
- Myocardial Perfusion SPECT
- Transient Ischemic Dilation
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Since its beginnings in the early 1970s, clinical nuclear cardiology has evolved substantially, gaining both technical sophistication and enhanced imaging capabilities. Importantly, in parallel to these developments, an extensive literature supporting the clinical and cost-effectiveness of this modality has developed. Today, state-of-the-art nuclear cardiology allows for the objective measurement of both myocardial function and relative regional myocardial perfusion at rest and stress, providing accurate risk assessment in a wider variety of patient subsets. This chapter will highlight stress myocardial perfusion single-photon emission CT (SPECT), which currently comprises approximately 95 % of the procedures performed in this field.
The chapter is organized as follows: first, there is a discussion of the general concepts of risk assessment in chronic coronary artery disease (CAD), including evidence for the cost-effective characteristics of stress myocardial perfusion SPECT (MPS) compared with alternative strategies without MPS, as well as data supporting the selection of MPS in specific patient populations. This discussion is followed by the largest section of the chapter, which deals with the current evidence for the use of MPS for risk stratification. This is followed by a brief section dealing with the importance of parameters other than stress myocardial perfusion defects that impact post-MPS patient risk and estimates of risk. The final portion of this chapter deals with the role of MPS in identifying whether patients will have enhanced survival with medical therapy versus revascularization based on the results of the MPS study. In this context, the role of gated SPECT ejection fraction and the potential importance of validated scores to estimate patient risk will be mentioned as well. The conclusion of the chapter addresses the need for the integration of SPECT results with other clinical data in guiding inpatient management decisions.
This chapter will be limited to the consideration of stable patients with known or suspected chronic CAD and will focus primarily on stress myocardial perfusion abnormalities, since myocardial viability (predominantly assessed by resting studies) is addressed in another chapter.
The main use of nuclear cardiology studies for guiding management decisions is determining which patients with suspected or known coronary artery disease require catheterization with consideration of revascularization. In patients who have “limiting” chest pain symptoms, which despite medical therapy affect their well being, nuclear cardiology studies play a limited role; they are chiefly useful for identifying the culprit coronary lesion and determining which vessel or vessels might be most appropriate for revascularization. Since revascularization has been shown to relieve anginal symptoms in patients with CAD, it would not be cost effective to study all patients with limiting symptoms with MPS and direct invasive coronary angiography is generally indicated.
If revascularization is being considered for purposes of improving prognosis, MPS can be helpful in determining whether the patient’s risk is high enough to warrant revascularization. Risk stratification is the most rapidly growing area of application of MPS. The use of MPS for this purpose provides a widely accepted new paradigm in patient management, which is endorsed by clinical guidelines. A risk-based approach to patients with known or suspected CAD is well suited to the current environment, in which cost containment is of great importance and in which dramatic improvements in medical therapy have been developed. In contrast, the approach focusing on simple diagnosis, in which patients with suspected disease undergo invasive coronary angiography and then are frequently revascularized based on coronary anatomic findings, has been shown to be less cost effective. With the risk-based approach, the focus is not on predicting who has anatomic CAD but on identifying and separating patients at higher risk for a major adverse cardiac event from those who are at lower risk.
Pathophysiologic Basis for Risk Assessment in Myocardial Perfusion SPECT
The basis for the power of nuclear testing for risk stratification is found in the fact that the major determinants of prognosis in CAD can be assessed by measurements of stress-induced perfusion or function. These measurements include the amount of infarcted myocardium, the amount of jeopardized myocardium (supplied by vessels with hemodynamically significant stenosis), and the degree of jeopardy (tightness of the individual coronary stenosis). An additional important factor in prognostic assessment is the stability (or instability) of the CAD process. This last consideration may help explain what appears to be a clinical paradox: Nuclear tests, which in general are expected to be positive only in the presence of hemodynamically significant stenosis, are associated with a very low risk of either cardiac death or nonfatal myocardial infarction when normal. In contrast, it has been observed that most myocardial infarctions occur in regions with premyocardial infarction coronary plaques causing less than 50 % of stenosis [1, 2]. It has been postulated that this paradox may be explained by the different response to stress of mild stenosis associated with stable and unstable plaques. For example, it has been shown that mild coronary narrowings associated with unstable plaque manifest a vasoconstrictive response to acetylcholine stimulation due to abnormal endothelial function, whereas stable, mild coronary lesions respond to acetylcholine with vasodilation [1]. It is possible that factors released during exercise or vasodilator stress may be similar to acetylcholine in terms of stimulation of a differential endothelial response in stable and unstable plaques. Thus, beyond the ability to define anatomic stenosis, nuclear tests (by virtue of their assessment of physiology) would be able to discern abnormalities of endothelial function associated with high risk, even in the absence of significant stenosis.
Differentiating Outcome Type by Nuclear Test Results
Recent evidence in large patient cohorts has revealed that factors estimating the extent of left ventricular dysfunction (left ventricular ejection fraction, the extent of infarcted myocardium, transient ischemic dilation of the left ventricle, and increased lung uptake) are excellent predictors of cardiac mortality. In contrast, measurements of inducible ischemia are better predictors of the development of acute ischemic syndromes. These include exertional symptoms and electrocardiographic changes, as well as the extent of perfusion defect reversibility and stress-induced ventricular dyssynergy. Several recent reports have shown that nuclear testing yields an incremental prognostic value over clinical information with respect to cardiac death or the combination of cardiac death and nonfatal myocardial infarction as isolated endpoints. By understanding how clinical information and nuclear test markers can be used to estimate varying outcomes, it is now possible to tailor therapeutic decision making for an individual patient based on the combination of clinical factors and nuclear scan results. For example, a patient with severe perfusion abnormalities on their stress imaging may have a five- to ten-fold higher likelihood of cardiac death compared with a patient with a normal MPS. If the defects are stress induced (reversible), therapies known to improve survival might be chosen in order to result in an optimized outcome for that patient.
Definition of nuclear variables. In order to optimize the prognostic performance of stress myocardial perfusion single-photon emission CT (SPECT), it is crucial to maximize the information extracted from the images at the time of interpretation. Previous studies have shown that the extent and severity of reversible hypoperfusion are independent variables in predicting subsequent cardiac events in patients with suspected coronary artery disease [2]. To this end, it is necessary to consider the full extent and severity of the abnormality, either quantitatively [3–5] or semiquantitatively [6], rather than simply determining that the nuclear study is normal or abnormal. While a 20-segment model was initially widely used [7], a 17-segment model is currently recommended for all forms of tomographic myocardial imaging [8]. This figure diagrammatically represents the segmental division of the SPECT slices and assignment of individual segments to individual coronary arteries using a 17-segment model. The numbers refer to the individual segments. Each segment is scored from 0 (normal) to 4 (absent uptake of radioactivity). In order to circumvent these issues, we have recently proposed normalizing these variables [9] by dividing by the model-dependent maximum potential score and multiplying by 100. The result is the percentage of myocardium abnormal with stress, fixed (nonreversible), and ischemic (reversible) defects, providing intuitively useful information that will apply to any segmental scoring system. LAD left anterior descending coronary artery, LCX left circumflex coronary artery, RCA right coronary artery.
Comparison of the percent myocardium with abnormal perfusion at stress (% myocardium stress) derived from myocardial perfusion single-photon emission CT analyzed with either 20-segment or 17-segment approaches. In a population of 16,020 patients with known or suspected coronary artery disease followed for 2.1 years, equally effective prognostic assessment regarding cardiac death (CD) was shown with the two models. The summed stress score values shown for normal, mildly abnormal, and moderately to severely abnormal were those used in prognostic studies using the 20-segment model. A slight modification would be appropriate for the 17-segment model (Adapted from Berman et al. [6]).
Total perfusion deficit (TPD). Being intrinsically three-dimensional and digital, myocardial perfusion abnormalities with single-photon emission CT (SPECT) or positron emission tomography (PET) lend themselves to automated quantitative analysis. Several software packages for quantitative analysis are commercially available. This figure illustrates the TPD that is a computer-derived analogue of the visual percent myocardium that is abnormal by visual analysis, representing both defect extent and severity of perfusion defect. TPD is calculated as the percentage of the total surface area of the left ventricle below the predefined uniform average deviation threshold [10] using quantitative perfusion SPECT software (see Fig. 7.1) [11]. A circumferential profile for one short-axis slice is shown with corresponding normal limits [9, 10]. The area below the normal limit curve but above the circumferential profile curve for a given slice defines the perfusion deficit in a given slice. These areas are computed for all circumferential profiles in the myocardium and are summed forming TPD. TPD is measured at stress and rest, and ischemic TPD is calculated from the difference (stress TPD minus rest TPD). The reproducibility thresholds for quantitative stress, rest, and ischemic TPD have been reported to all be less than 7 % and smaller than the thresholds for visual percent myocardium abnormal (10–13 %) [12], suggesting that this type of objective, quantitative assessment of ischemia may be more effective in assessing the effects of therapy in individual patients than visual analysis alone. Ischemic TPD was the variable used in the Clinical Outcomes Utilizing Revascularization and Aggressive Drug Evaluation (COURAGE) nuclear substudy to evaluate baseline ischemia and the change in ischemia after therapy (see Fig. 7.44a and b) (Adapted from Berman et al. [9]).
Example of a patient with a small stress perfusion defect resulting in a mildly abnormal summed stress score. The patient is a 69-year-old man with atypical angina. The only risk factor for coronary disease was hypercholesterolemia. The patient exercised for 7 min and 20 s to a heart rate of 139 (92 % of maximal predicted) and had a normal blood pressure response. He developed minimal chest discomfort during stress, which was considered to be equivocal for an ischemic response. The electrocardiogram response to stress was normal. Exercise stress 99mTc-sestamibi (ST MIBI) and rest 201Tl (rest Tl) images are interlaced in the alternate rows, which show short-axis images (top two rows), vertical long-axis images (middle two rows), and horizontal long-axis images (bottom two rows). The images reveal a small to moderately sized defect in the distal anterior left ventricular wall with sparing of the interventricular septum and the apex. This pattern is classic for the territory of the mid to distal portion of the diagonal branch of the left anterior descending coronary artery.
Quantitative perfusion single-photon emission CT analysis of the patient shown in Fig. 7.4, indicating the presence of a small perfusion defect in the diagonal coronary territory. The summed stress score (SSS) that was attributed to the images in this figure is illustrated in the upper right corner. The SSS of 9 indicates a moderate abnormality (see Table 7.1). The quantitative total perfusion deficit is 11 %. The typical diagonal territory location is shown in the two-dimensional (middle panel) and three-dimensional (right panel) images at stress with a normal quantitative pattern at rest.
Example of a patient with a severe and extensive stress-induced perfusion defect. A 69-year-old man with atypical chest pain who had hypertension and diabetes as risk factors as well as left ventricular hypertrophy on resting electrocardiogram (ECG) exercised for 5 min to a heart rate of 139 (87 % of maximal predicted). The patient did develop chest discomfort and had an ischemic ECG response to stress. There was no exercise hypotension. Exercise stress 99mTc-sestamibi (ST MIBI) and rest 201Tl (rest Tl) images are interlaced in the alternate rows, which show short-axis images (top two rows), vertical long-axis images (middle two rows), and horizontal long-axis images (bottom two rows). The myocardial perfusion single-photon emission CT study reveals a severe perfusion defect throughout the distribution of the left anterior descending coronary artery.
Quantitative perfusion single-photon emission CT analysis of the patient in Fig. 7.6. The summed stress score is very high at 24, the summed rest score is low at 2, and the summed difference score is 22. The total perfusion deficit (TPD) measurements revealed that 40 % of the left ventricle is abnormal after stress, corresponding to the entire left anterior descending coronary artery (LAD) territory. The resting TPD was 5 %. Note that 40 % is generally considered the proportion of the myocardium supplied by the LAD. Thus, the findings are predictive of a proximal stenosis of the LAD and the severity of the perfusion defect allows the interpreter to state that the proximal LAD is likely to have a critical stenosis (>90 %) [13, 14]. In this study, the finding of transient ischemic dilation of the left ventricle, measured at 1.43 [11], is an ancillary finding associated with severe and extensive coronary artery disease. At catheterization the patient was found to have a 100 % proximal stenosis of the LAD, a 60 % circumflex lesion, and a 50–60 % midright coronary artery stenosis.
Incremental prognostic value of myocardial perfusion single-photon emission CT (MPS) results over anatomic and clinical data. Borges-Neto et al. [15] examined the incremental value of stress MPS over clinical and catheterization data in 3,275 patients who were followed for 3.1 years for death, cardiovascular death, and a composite of cardiovascular death or nonfatal myocardial infarction. This study constitutes the largest dataset accumulated with both anatomic and MPS data with follow-up. Using these patients, Cox proportional hazards regression models were developed for the prediction of all-cause death, cardiovascular death, and hard events (cardiovascular death or nonfatal myocardial infarction). Based on these models, a one-unit change in the summed stress score was found to be associated with increased risks of 4, 7, and 5 % for death, cardiovascular death, and death or nonfatal myocardial infarction, respectively. With respect to incremental value, the results of Cox proportional hazards modeling of all-cause death and cardiac death are shown, with the strength of various models depicted by their global chi-square. First, the addition of anatomic data from catheterization added incremental prognostic value over clinical data alone in the setting of both endpoints. Further, even after adjusting for clinical and anatomic data, the addition of stress MPS results added further incremental value with respect to prediction of both of these endpoints. Importantly, these results support the concept that the physiologic data contributed by MPS yields additive information that is not available from the assessment of anatomic data alone. Thus, a patient-management strategy of direct referral to catheterization, or an approach of revascularization without consideration of physiologic data, would result in some patients who are undergoing unnecessary and inappropriate procedures, while other patients who, on the basis of MPS data, may benefit from an intervention may not receive one (Adapted from Borges-Neto et al. [15]).
Outcomes and referral rates to catheterization in patients with stable chest pain from the Economics of Noninvasive Diagnosis (END) study group [12]. In this study of 11,372 consecutive stable angina patients who were referred for stress myocardial perfusion tomography or cardiac catheterization, composite 3-year costs of care and patient outcomes were compared as a function of two strategies: invasive (direct referral to cardiac catheterization without stress imaging) versus conservative (initial stress myocardial perfusion tomography and selective catheterization of high-risk patients). After matching patients referred to these two procedures by their pretest clinical risk of coronary disease, comparisons of aggressive and conservative testing strategies revealed that no difference in the rates of cardiac death or nonfatal myocardial infarction (MI) was present between these two groups, suggesting similar quality care. Significantly, the costs of care were higher for invasive care (direct cardiac catheterization) in all clinical risk subsets compared with the costs associated with conservative care (stress myocardial perfusion imaging plus selective catheterization). Importantly, note that the difference in cost between the strategies did not reach significance in the low-risk patient subset. The cost savings identified in the intermediate- and high-risk patient subsets were accrued predominantly by preventing a referral to catheterization in patients without significant myocardial perfusion single-photon emission CT (MPS) abnormalities. This is borne out by significant differences in normal catheterization rates (in the subset of patients referred to catheterization) between the two strategies examined, suggesting that MPS aids in the identification of the appropriate candidate for the catheterization laboratory. Hence, the use of a strategy incorporating MPS as an initial test results in improved cost-effectiveness without compromise of patient outcomes. This finding supports the use of MPS as a reasonable alternative to catheterization in patients presenting with stable angina (Adapted from Shaw et al. [12]).
Cost-effectiveness ratios (costs of testing per hard event [HE] identified) in patients with low pre–exercise tolerance test (ETT) likelihood of coronary artery disease (CAD), patients with low post-ETT likelihood of CAD, and patients with intermediate to high post-ETT likelihood of CAD. While the previous figures support the role of myocardial perfusion single-photon emission CT (MPS) as providing added prognostic value, as well as cost-savings when appropriately utilized before catheterization referral, which patients are optimal candidates for MPS is also an important question to address. In a seminal study, Berman et al. [16] examined the incremental prognostic implications of normal and equivocal exercise MPS results, its incremental prognostic value, and cost implications in 1702 patients without prior revascularization who were followed for 20 ± 5 months. When the complete spectrum of MPS results were considered, MPS yielded incremental prognostic value, as demonstrated by enhanced risk stratification, in all patient subgroups analyzed (low, intermediate, and high likelihood of CAD) (results not shown). However, MPS was cost effective only in patients with interpretable exercise electrocardiogram (ECG) responses and an intermediate to high post-ETT likelihood of CAD and in those with uninterpretable exercise ECG responses and an intermediate to high pre-ETT likelihood of CAD. This study demonstrates the impact of patient selection for MPS on the clinical and cost-effectiveness of testing. The referral of patients identified as low risk by clinical evaluation (low pre-ETT likelihood of CAD) or by ETT (low post-ETT likelihood of CAD) results in excess costs with a minimal impact on the identification of at-risk patients (since so few patients are reclassified with respect to risk in these patient subsets). On the other hand, MPS can be a cost-effective test if patients at adequate risk are referred (Data from Berman et al. [16]).
Successive testing to optimize outcomes and cost. Based on the data from Berman et al. [16] presented above, a potential strategy of successive testing can be hypothesized to optimize outcomes and cost. As shown, a significant number of patients presented to clinical evaluation (n = 1,282). Clinical evaluation alone would have identified 43 % of the patients in this cohort as low risk (0.5 % hard event rate over 20 months) and not in need of further testing. Similarly, the use of exercise tolerance testing (ETT) as the second-line test in the intermediate to high clinical risk patients would have identified an additional 231 patients as not needing further testing (31 % of the intermediate- to high-risk patients, 18 % of the total). This approach would have reduced the number of patients referred to myocardial perfusion single-photon emission CT (MPS) from 1,282 to 503, as shown. The low risk associated with a normal study would have identified an additional 274 patients (54 % of MPS patients) as low risk and not in need of further evaluation. Thus, of 1,282 patients originally referred to MPS, a successive testing strategy may have avoided 39 % of all the MPS performed in these patients (the 779 patients identified as low risk by pre-MPS assessment). As importantly, only 229 patients who were at greater risk (7.9 % hard event rate) would be referred on to catheterization, resulting in a considerable potential cost saving. Thus, a strategy of successive evaluations, with the evaluations of increasing sophistication and cost at each step, results in reduced cost with adequate identification of at-risk patients. This approach ensures both the cost-effectiveness of MPS as a modality within a strategy as well as that of the testing strategy as a whole (Data from Berman et al. [16]).
Cost-effectiveness of myocardial perfusion single-photon emission CT (MPS) in reclassifying patients’ likelihood of high-risk coronary artery disease (CAD). Although risk-based patient-management strategies have gained widespread acceptance, many studies still focus on anatomic endpoints for the assessment of MPS. While it is generally assumed that the two are reasonable alternatives, the test performance characteristics of stress MPS are distinctly different when assessed using an anatomic versus a prognostic endpoint. In 1994, the Mayo Clinic group examined the cost-effectiveness of stress MPS for identifying patients with high-risk anatomic CAD in a cohort of 411 patients with normal resting electrocardiograms (ECGs) and no prior CAD who underwent exercise MPS and were subsequently referred to catheterization [17]. The analytic approach they utilized was to determine each patient’s likelihood of having high-risk anatomic CAD (left main [LM] or three-vessel [3VD] CAD) on the basis of pre-MPS data and assess how many patients’ likelihood were reclassified on the basis of MPS data [17]. These investigators found that although there was a significant reclassification achieved by single-photon emission CT (SPECT) over pre-SPECT data, the number of patients reclassified by SPECT (3 % of all patients) did not justify the cost accrued, as evidenced by an unacceptably high cost-effectiveness ratio. They concluded that although MPS could reclassify patients’ likelihood of high-risk CAD, it failed to do so in a cost-effective manner; hence, it should not be used in patients with normal rest ECG without prior CAD. Interestingly, the Cedars–Sinai group examined this same population (no prior CAD, normal rest ECG) using the same analytic approach (the ability of MPS data to reclassify patients’ likelihood of an outcome) but used outcomes (cardiac death, nonfatal myocardial infarction) rather than an anatomic endpoint [18]. With respect to this prognostic endpoint, the investigators found that SPECT reclassified a far greater proportion of patients with respect to their risk of adverse outcomes (40 %), thus doing so at less than one-third the cost of an anatomic-based approach. Hence, stress SPECT appears to have far greater clinical and cost-effectiveness in the context of an outcome than an anatomic endpoint. Of note, the cost-effectiveness of SPECT with respect to this prognostic endpoint demonstrated this superiority only when patients with intermediate to high risk were examined. The inclusion of low-risk patients, as described previously, compromised the clinical and cost-effectiveness of SPECT.
Identification of the appropriate candidate for stress imaging. This figure shows the initial decision node in the evaluation of patients with known or suspected coronary artery disease (CAD). The first clinical step is the determination of a patient’s pretest likelihood of CAD or their pretest risk of adverse events. In patients with low likelihood or risk, the clinical question is primarily whether the patient is a candidate for primary versus secondary prevention and whether further testing (e.g., atherosclerosis assessment) would be necessary. Patients at intermediate or high likelihood of risk are appropriate candidates for ischemia evaluation. Although this approach appears straightforward, the challenge facing physicians is how to accurately and reliably estimate patients’ likelihood of CAD or the risk of adverse events. This process is complicated by the numerous factors that potentially impact on these estimates. These factors include cardiac risk factors, demographic characteristics, biomarkers, and results of other testing, just to name a few.
Hard event rates after normal myocardial perfusion single-photon emission CT (MPS) (yellow line) and relative risks associated with abnormal versus normal MPS in the 12 prognostic studies cited by the 2003 Radionuclide Guidelines. To date, there is an extensive literature base for examining risk after a normal stress MPS, with most studies reporting rates of hard events (cardiac death or nonfatal myocardial infarction) of less than 1 % per year of follow-up [19, 20]. This level of risk has been described to be independent of gender, age, symptom status, past history of coronary artery disease (CAD), presence of anatomic CAD, imaging technique, or isotope (201Tl or 99mTc-sestamibi) [15]. Two important concepts in understanding how well MPS fulfills the basic requirements of risk stratification are shown in this figure. First, the risk of hard events after a normal MPS is relatively low (right Y axis; < 1 % in 10 of the 12 studies cited). Indeed, these guidelines also pool data from 16 studies, finding that in over 27,000 patients followed for a mean of 26.8 months, the annualized hard event rate was only 0.6 %. The relative risk associated with an abnormal MPS ranges from 3 to 14 in these studies (left Y axis), indicating that MPS successfully aggregates or concentrates risk in patients with abnormal studies relative to normal studies, resulting in the former being of far greater risk than the latter. The identification of low risk with a normal study and the reclassification of higher risk patients with abnormal studies are two of the most basic characteristics of risk stratification with tests (Data from Klocke et al. [19]).
Event risk with abnormal scans. Numerous studies to date have described a direct relationship between increasing the extent and severity of scan abnormality and increasing patient hard event or cardiac mortality risk [18, 20–33]. This relationship, illustrated conceptually here, has been shown to be present irrespective of the type of stress performed, the patient cohort examined (with respect to clinical characteristics or history of coronary artery disease [CAD]), or the particular radiopharmaceutical employed. A decreased slope in the increase in mortality with increasing extent/severity of perfusion defect is probably primarily related to the referral of the most ischemic patients to revascularization, resulting in censoring from the prognostic evaluation of the patients at highest risk. Manuscripts have been written in large patient populations covering each of the specific subsets listed in this figure. While the number of risk-stratification manuscripts is a strength of nuclear cardiology compared with other modalities, the current data supporting this application are based on large observational series. CABG coronary artery bypass graft, DM diabetes mellitus, PTCA percutaneous transluminal coronary angioplasty.
Prediction of myocardial infarction (MI) versus cardiac death (CD) by myocardial perfusion single-photon emission CT (MPS). The extent of abnormality of the MPS provides important additional information regarding risk. The annualized cardiac death rate and MI rate of a large group of patients undergoing stress MPS (two-thirds exercise stress, one-third adenosine stress) is shown. There was a progressive increase in the CD rate as a function of the extent and severity of perfusion defect, as shown. In contrast, while the rate of nonfatal MI was low when the scans were normal, it increased abruptly even when a mild myocardial perfusion defect was noted (Adapted from Hachamovitch et al. [23]).
Incremental prognostic value of stress myocardial perfusion single-photon emission CT (MPS) as a function of prescan likelihood of coronary artery disease (CAD). In a study of 1702 patients undergoing 99mTc-sestamibi imaging, a normal scan was associated with a very low (0.2 %) likelihood of cardiac death (CD) or myocardial infarction (MI) over a 20-month period. This figure illustrates the rate of CD or nonfatal MI throughout the follow-up period as a function of single-photon emission CT results and pre-MPS likelihood of CAD (low likelihood, <0.15; intermediate likelihood, 0.15–0.85; high likelihood, >0.85). These results demonstrate that MPS could be used for prognostic purposes throughout the range of likelihood of CAD and that the greatest impact was in the patients with a high likelihood of CAD. SSS summed stress score (Adapted from Berman et al. [16]).
Risk stratification in patients with a high pretest likelihood of coronary artery disease (CAD). Appropriate patient selection is the first important step in cost-effective risk stratification. Traditionally, anatomic endpoints have served as the basis of patient-management strategies. In this context, the principle guiding the decision to use noninvasive testing in patients with suspected CAD was the patient’s pretest likelihood of angiographically significant CAD [34]. For diagnostic purposes, in accordance with Bayes’ theorem, only patients with an intermediate likelihood of CAD are considered candidates for exercise treadmill testing, because in this range the results would reclassify patients as having either a low likelihood (not in need of further testing) or a high likelihood (in need of angiography to determine the suitability for revascularization). This approach is embodied in multiple American College of Cardiology/American Heart Association guidelines in which stress testing, with and without stress imaging, is considered a class IIb indication (usefulness/efficacy is less well established by evidence/opinion) for diagnostic testing in patients with either a high or low pretest probability of CAD [24, 35, 36]. In an outcomes- or risk-based strategy, intermediate-risk patients would be referred to testing in a pattern similar to the referral of intermediate likelihood of CAD patients in an anatomic-based strategy. In an anatomic strategy, patients with a high likelihood of CAD would be referred for invasive coronary angiography. However, in an outcomes-based strategy, such patients would be referred for stress imaging rather than catheterization, based on the assumption that (1) a normal myocardial perfusion single-photon emission CT (MPS) result would identify them as low risk despite the high likelihood of anatomic CAD and (2) a sufficient majority of patients with high pre-MPS likelihood of CAD would have normal MPS so that the use of single-photon emission CT in this scenario would be cost effective. A validation of an outcomes-based approach to the use of MPS was first evaluated in 1,270 consecutive patients with no previous revascularization or myocardial infarction who had a pre–exercise tolerance test (ETT) likelihood of CAD less than 0.85 and were followed for 2.2 ± 1.2 years [37]. As shown in the figure, a normal MPS was associated with low risk (0.3 % cardiac death [CD] per year, 0.7 % hard event [HE] rate/year), with a significant increase in risk with worsening MPS results. Further, 630 of the 1,028 patients (61 %) included in the survival analysis had normal MPS despite their high likelihood of CAD. A strategy of initial MPS in patients able to exercise was more cost effective than a strategy of initial ETT followed by MPS only in the patients with an intermediate to high post-ETT likelihood of CAD. Also, although the subset of patients with interpretable rest electrocardiograms were risk stratified by ETT without imaging, only a small proportion of these patients were reclassified as sufficiently low risk that no further testing was required. Hence, ETT without imaging was considered to be unlikely to be clinically efficient in practice. Finally, MPS was also a superior strategy to initial catheterization in these patients. Hence, it appears that a risk-based strategy is valid and probably more clinically effective and cost effective than a traditional anatomic-based strategy. NL normal (Adapted from Hachamovitch et al. [37]).
Stress myocardial perfusion single-photon emission CT (MPS) in a patient with a high likelihood of coronary artery disease. The patient, a 71-year-old woman, had chronic, mild typical angina pectoris and a history of hypertension. Being unable to exercise, she had an adenosine stress for the MPS and showed normal clinical and electrocardiographic responses. Stress 99mTc-sestamibi (ST MIBI) and rest 201Tl (rest Tl) images are interlaced in the alternate rows, which show short-axis images (top two rows), vertical long-axis images (middle two rows), and horizontal long-axis images (bottom two rows). The MPS images are entirely normal. With this result, the patient was treated medically. Eleven years following the initial stress imaging study, the patient remained free from cardiac catheterization and free from cardiac events, and a repeat adenosine MPS remained normal.
Hard event rate as a function of summed stress score (SSS) and Duke treadmill (TM) score. In patients with interpretable stress electrocardiograms (ECGs), it has been demonstrated that the Duke TM score can separate patients into low, intermediate, and high risk of cardiac events. Thus, current guidelines suggest beginning with a stress ECG in these patients [38]. However, nuclear testing is recommended as useful in the patients with intermediate- or high-risk Duke TM scores. Stress myocardial perfusion single-photon emission CT (MPS) studies further risk stratify patients within each of these Duke TM score categories [22]. All patients examined had no known coronary artery disease (patients with prior catheterization, myocardial infarction [MI], or revascularization were excluded). The hard event (cardiac death or MI) rate as a function of the Duke TM score category and the nuclear scan results (summed stress score [SSS]) are illustrated. The normal, mild, and severe SSS categories are based on the subgroups of percent myocardium abnormality at stress described in Table 7.1. For purposes of this study, due to small patient numbers, those patients with moderate to severe SSS were categorized as severe. Overall, patients with a low-risk Duke TM score had such a low rate of cardiac events that it would not be cost effective to study them for prognostic purposes. Additionally, since patients with a high-risk Duke TM score usually undergo catheterization, these patients are generally not sent for further nuclear testing. However, 55 % of the population had the intermediate-risk Duke TM score with a cardiac event rate of 2.5 %. Thus, MPS provided excellent stratification of these patients with respect to risk of hard event [22] (Adapted from Hachamovitch et al. [22]).
Long-term outcome of 4,649 patients (pooled from four institutions) with an intermediate-risk exercise electrocardiogram based on the Duke treadmill score and no or minimal stress myocardial perfusion defects. The mortality rate is extremely low for patients with no stress myocardial perfusion defect (Adapted from Gibbons et al. [39]).
Risk stratification with single-photon emission CT (SPECT) imaging. A first step in applying the current evidence on risk stratification with SPECT imaging results to a given population is to understand what the baseline risk is for any given patient cohort [40]. Using this figure, one can visualize that risk stratification is effective for low- to high-risk SPECT results across a spectrum of population event rates. Although it is noted that the general risk for a suspected disease population is fewer than 2 % per year for coronary heart disease death or nonfatal myocardial infarction [40, 41] of this group, there are specific high-risk patient subsets, including diabetic individuals and the elderly, to name a few. Thus, this figure depicts generalities of risk that allow physicians to grasp the idea of risk stratification, even if it may not necessarily be applied to all patient cohorts [40]. Based on the application of risk stratification in this figure, women are unique in that a large proportion falls into the low-risk end of the spectrum. However, diabetic and elderly women and men, and probably those with the metabolic syndrome, form a very high-risk subset whose annual event risk is decidedly high. For African American and Hispanic patients with multiple risk factors, the risk of events is also elevated when compared with white, non-Hispanic patients. With regard to minority patient populations, physicians should take care to also consider nonclinical factors that may elevate a patient’s risk, including delays in healthcare seeking and treatment, the absence of a regular source of care, and other financial hurdles that may render patients at greater risk on presentation to a SPECT imaging laboratory. CAD coronary artery disease (Adapted from Shaw and Iskandrian [40]).
Prognostic value of summed stress scores (SSS) in sestamibi single-photon emission CT (SPECT) in diabetic patients. Risk stratification using myocardial perfusion SPECT (MPS) has been proven effective in a variety of patient subgroups, most importantly among diabetic patients. This figure illustrates the hard cardiac event-free survival rate in patients with diabetes mellitus (DM) and patients without diabetes mellitus (no DM) categorized by the SSS as normal (SSS < 4) (a), mildly abnormal (SSS 4–8) (b), and moderately to severely abnormal (SSS > 8) (c). The study was comprised of 1,271 patients with diabetes and 5,862 patients without diabetes who underwent dual-isotope (rest 201Tl/poststress 99mTc) MPS. After risk adjustment for the pre-scan likelihood of coronary artery disease, inability to exercise (requiring pharmacologic stress), history of coronary artery disease, and SSS, the patients with diabetes had a lower event-free survival in each of the SSS categories compared with the patients without diabetes (all P < 0.001). Given this result, a diabetic patient with only mildly abnormal myocardial perfusion scan results might be considered for cardiac catheterization in the presence of minimal symptoms, whereas in general, patients with only mildly abnormal scans might be considered appropriate for aggressive medical management without catheterization [23, 38, 42]. Similar results were obtained in a smaller diabetic population from a multicenter registry [32]. More recent data from the Detection of Ischemia in Asymptomatic Diabetics (DIAD) study [35] and the Clinical Outcomes Utilizing Revascularization and Aggressive Drug Evaluation (COURAGE) trial [44], however, would suggest that such a referral might not be appropriate unless there is extensive and severe ischemia. Data from the Bypass Angioplasty Revascularization Investigation (BARI 2D) will provide important information regarding the use of MPS in risk stratification in diabetic patients (Adapted from Kang et al. [31]).
Risk of adverse events after a normal myocardial perfusion single-photon emission CT (MPS) study: variation with underlying patient characteristics. More recently, published prognostic studies performed in patients undergoing pharmacologic stress, a population with more comorbidities and at higher risk than patients undergoing exercise stress, have reported hard event rates of 1.3–2.7 % per year with a normal MPS, suggesting that underlying clinical risk and prior coronary artery disease (CAD) may influence event rates even when the perfusion scan is normal [30, 31, 38, 44–46]. Key higher risk subsets have been defined such as those with known CAD or its risk equivalent, which include diabetic patients as well as those with a clustering of risk factors (e.g., metabolic syndrome), noncardiac atherosclerotic disease (e.g., peripheral arterial disease or cerebrovascular disease or high-risk subclinical disease), or those with extensive comorbidity and/or functional disability. Along these lines, a recent study reported a series of 7,376 patients with normal stress MPS, addressing the predictors and temporal characteristics of risk [46]. This study identified a number of variables—the need for pharmacologic stress, the presence of known CAD, diabetes mellitus (DM) (in particular, female diabetic patients), and advanced age were markers of increased risk and shortened time to risk (e.g., risk in the first year of follow-up was less than in the second year). (a and b) Illustrate the increased event rate in diabetic patients and the elderly, particularly in diabetic women. While confirming that, as a whole, patients with normal MPS are at very low risk, several additional insights were revealed by this study. First, baseline patient risk after a normal MPS varied widely as a function of the patient’s clinical characteristics, as described above. In certain patients, for example, elderly patients who were unable to exercise with known CAD or DM, risk of cardiac death or myocardial infarction exceeded 1 % even in the first year of follow-up. This study also showed that, in patients with known CAD who had normal MPS, the temporal component of risk increased rapidly, as shown in (c). Hence, even patients who had low risk in the first year after normal MPS may no longer be at low risk in the second year. Little is known regarding this concept of accelerated risk over time, and further studies are needed to delineate this “warranty period” after a normal MPS in various patient subsets. Thus, to date, there is little information currently available to guide the need for and timing of retesting after a normal scan (Adapted from Hachamovitch et al. [47]).
Annualized cardiac death rates in the US population. Shown are results of an overall study cohort and an overall cohort subgrouped into patients with normal versus abnormal myocardial perfusion single-photon emission CT (MPS). This is an example of the relative nature of what is “low risk” after a normal MPS. Increasingly, studies are reporting event rates after normal MPS to be greater than “expected” based on the definition of less than 1 % risk of cardiac death per year of follow-up (the accepted paradigm of low risk). Since posttest patient risk of adverse events after both normal and abnormal test results will vary as a function of the baseline risk of the population tested, the issue of how to define a threshold for low risk is problematic. A recent study followed 5,200 elderly patients (defined as age greater than or equal to 75 years) for 2.8 ± 1.7 years. In a subgroup of 443 patients aged 85 years old and above who had a normal stress myocardial perfusion imaging, the annual cardiac death rate was 3.3 %, well above the 1 % accepted standard for low risk. However, also shown, the cardiac mortality rate for individuals aged 85 years old and above in the USA in 2005 was 4.8 %, approximately one-third greater than in patients with normal MPS. Hence, elderly patients with normal MPS were at a lower risk than their counterparts in the USA. Thus, although normal MPS may not identify patients at low absolute risk, they do appear to identify patients at low relative risk.
Endpoints in studies of post-imaging outcomes. It is widely agreed that mortality endpoints are superior to “softer” endpoints (e.g., nonfatal myocardial infarction, revascularization, hospitalizations) in studies of post-imaging outcomes. However, whether cardiac death (CD) or all-cause death (ACD) is the more appropriate choice remains controversial. On the one hand, CD has the advantage of being the event we are focused on; our efforts at intervention and therapeutics are focused on reducing the incidence of this event. On the other hand, CD is plagued by issues of misclassification bias; since few autopsies are performed, we cannot be certain as to what was the precise cause of death in any given patient. Death certificates have been found to frequently misclassify the cause of death in many patients. Ideally, studies would use both CD and ACD as primary and secondary endpoints. Practically, cohorts from most studies (patients who are older, patients who have more frequent coronary artery disease and cardiac risk factors) predominantly die from cardiac causes. Thus, this issue is of less concern in many studies. However, a very important exception to this are studies examining event rates after normal studies, especially comparing pharmacologic and exercise stress. While patients who are able to exercise to target heart rates usually do not have major comorbidities and are relatively healthy, patients referred to pharmacologic stress are older and more frequently have multiple comorbidities. Further, many of the patients referred for pharmacologic stress are undergoing testing as part of preoperative cardiovascular clearance and, hence, often have a relatively high risk of noncardiac death. As shown in this figure, a recent study in elderly patients reported that compared to CD rates, ACD rates were several times greater. Further, the risk associated with abnormal myocardial perfusion single-photon emission CT (MPS) relative to normal MPS was attenuated for ACD, suggesting a disproportionate increase in noncardiac deaths in patients with normal studies as compared to CD rates after normal and abnormal MPS. For example, the increase in event rates with CD versus ACD after normal MPS was 4.3 (75–84 years) and 3.2 times (≥85 years), respectively. However, the increase in events after abnormal MPS was 2.5 and 1.5 times, respectively. Thus, there appear to be extra deaths accrued after normal MPS as opposed to abnormal MPS. This increased risk after a normal MPS is probably associated with noncardiac deaths in patients without significant cardiac disease (hence, normal MPS).
Variability in risk-adjusted cardiac mortality as a function of myocardial perfusion single-photon emission CT (MPS)-detected ischemia in medically treated patients. The dependence of post-normal MPS risk on the patients’ underlying clinical, demographic, and historical characteristics also extends to patients with abnormal MPS results. In a large study of 10,627 patients with follow-up, while there is an increase in risk-adjusted cardiac mortality rates with increasing ischemia in the subset of medically treated patients, the precise level of risk associated with mild (5–10 % myocardium ischemic), moderate (10–20 % myocardium ischemic), or large (>20 % myocardium ischemic) amounts of ischemia varies widely. For example, in moderately ischemic patients, the cardiac death risk may be as low as 2 % or as high as 10 % depending on the patient subgroup. Hence, patients who cannot exercise, are older, or are diabetic will have far greater risk than those patients who are younger, able to exercise, or are not diabetic, despite similar extent and severity of ischemia on their stress MPS study. DM diabetes mellitus, M men, W women (Data from Hachamovitch et al. [48]).
Risk-adjusted survival analysis in patients with insulin dependent diabetes mellitus, non-insulin dependent diabetes mellitus, and non-diabetic controls. For example, in a recent large study, for any level of defect extent and severity, risk-adjusted analysis demonstrated that the risk of cardiac death was greater in patients with insulin-dependent diabetes mellitus (IDDM) than in those with non–insulin-dependent diabetes mellitus (NIDDM), who in turn had greater risk than nondiabetics [49]. Along these lines, several studies have now shown that not only does scan data provide incremental prognostic information over prescan information but prescan data also yield incremental prognostic information over myocardial perfusion single-photon emission CT results [9, 27, 48, 50, 51]. Further, the type of event likely to occur on follow-up varies as a function of the type of defect found, with myocardial infarction more likely in the setting of reversible defects and cardiac death more likely in the setting of fixed defects [52] (Adapted from Berman et al. [49]).
Cardiac death rates in patients with and without atrial fibrillation (AF) as a function of myocardial perfusion single-photon emission CT (MPS) results: an example of how prescan information affects risk. In patients with mildly abnormal MPS, those with chronic AF have been shown to have a high risk of cardiac death, whereas those without AF do not. While patients with mildly abnormal MPS results are generally at low risk of cardiac death, this is not the case in patients with significant comorbidities (e.g., advanced age, prior coronary artery disease, diabetes mellitus [31], AF [53], pharmacologic stress). In this light, the decision whether or not to catheterize a patient with a mildly abnormal perfusion scan becomes a function of the underlying patient condition. *P = 0.001; follow-up 2.2 ± 1.2 years (Adapted from Abidov et al. [53]).
Event-free survival in African American and Hispanic patients versus white non-Hispanic patients. An examination of the dramatic differences in event-free survival for African American (a) and Hispanic patients (b) as compared with white non-Hispanic patients (c) reveals several notable phenomena [54]. This was the first study to find that in sufficiently large populations, effective risk stratification is possible using the 20-segment model summed stress score risk groupings in ethnic minority cohorts. Additionally, due to greater comorbidity, African American and Hispanic patients have decidedly higher rates of cardiac death or nonfatal myocardial infarction (MI) when compared with their white non-Hispanic counterparts. Thus, similar to our findings in diabetic patients, one must realize that comorbidity or the underlying hazard (or risk) in the population will drive the expected event rates. Therefore, for higher-risk patient subsets, although one may stratify risk from low to high, the event rates will be higher in minority populations due to more frequent risk factors and a greater comorbidity burden. The effective risk stratification is notable given the evidence of less-prevalent obstructive coronary disease and is supportive of a greater role for physiologic or flow abnormalities in risk assessment for ethnic minority patients, particularly African American and Hispanic patients. A low event rate in 4,629 Asian patients with normal stress myocardial perfusion single-photon emission CT findings was recently reported, with annual cardiac event rates of approximately 0.7 % [55].
Relationship of ischemia and symptoms for predicting long-term outcomes in diabetics. Zellweger et al. [56] recently evaluated 1,430 consecutive diabetic patients, all of whom received rest 201Tl/stress 99mTc-sestamibi myocardial perfusion single-photon emission CT (MPS), in order to assess this relationship. During the follow-up period (median of 2 years) with respect to risk and presenting symptoms, the annual cardiac event (CE) rates (cardiac death or myocardial infarction) among patients with normal MPS findings were similar for patients with angina, asymptomatic patients, and patients with shortness of breath. Among patients with abnormal MPS results, however, patients with shortness of breath had significantly higher CE rates than patients with angina (P = 0.008) and asymptomatic patients (P < 0.001); the outcomes for asymptomatic patients and patients with angina were similar (Adapted from Zellweger et al. [56]).
Prognostic impact of a hemodynamic response to adenosine on patient survival. In many respects, the results of vasodilator stress myocardial perfusion single-photon emission CT (MPS) studies are more difficult to understand compared with those of exercise MPS in that there are a paucity of nonperfusion markers to consider. For example, although the positive predictive value of the electrocardiogram response is quite high, the negative value is not as good. Although symptoms often occur with vasodilator stress, their predictive value is very poor and is most often unrelated to coronary artery disease. Although “walking” vasodilator stress is performed, the exercise capacity is not maximal and, hence, is not prognostically useful. Therefore, it is potentially useful to identify additional putative markers of risk in patients who are undergoing vasodilator stress MPS. To this end, Abidov et al. [57] recently identified both resting heart rate (RHR) and peak heart rate (PHR) as an important and powerful prognostic predictor of cardiac death in these patients. These variables were both independent and incremental risk-adjusted predictors of cardiac death. Increasing values of PHR response to adenosine stress were strongly associated with improved survival, as were low RHRs. In both male and female patients, an increasing ratio of RHR to PHR was associated with increasing cardiac mortality rates (Adapted from Abidov et al. [57]).
Prognostic adenosine score and Kaplan–Meier 2-year survival. The relationship between the complex prognostic adenosine score and 2-year Kaplan–Meier survival free of cardiac death (CD) reveals that over the range of lower risk scores (approximate score <100), the confidence intervals are relatively narrow, permitting relatively more precise estimates of risk in lower risk patients. For values of the prognostic adenosine score greater than 100, the associated risk is sufficiently large that although the confidence intervals are wider, it is not as important.
Relationship between left ventricular ejection fraction (LVEF) measured by gated single-photon emission CT (SPECT) and mortality rate and nonfatal myocardial infarction (MI). In 2,686 consecutive patients undergoing stress 99mTc gated myocardial perfusion SPECT (MPS), there was a curvilinear inverse relationship between LVEF at rest by MPS, performed after stress, and cardiac death [27]. The LVEF was the strongest predictor of mortality in this group. The findings are similar to those reported for rest LVEF acquired with radionuclide angiography in patients after MI (Adapted from Sharir et al. [27]).
Added prognostic value of gated myocardial perfusion single-photon emission CT (MPS) left ventricular perfusion and function. An important early question that faced stress-gated MPS was whether the data provided by the perfusion and function components of the test were additive or redundant. Travin et al. [28] reported on 3,207 patients who underwent stress-gated MPS and were followed up for hard events. Cox proportional hazards regression analysis revealed that the stress perfusion and gated ejection fraction components added incrementally to each other even after considering pre-MPS data. Annualized cardiac death (CD) rates were risk stratified by both perfusion and function data, with increasing risk as a function of both greater perfusion defects and decreasing ejection fraction. *P < 0.05 compared with EF ≥50 %; † P < 0.001 compared with EF ≥50 %; ‡ P < 0.05 compared with 1 vessel disease (VD). LVEF left ventricular ejection fraction (Adapted from Travin et al. [28]).
Cumulative incidence of coronary angiography in 4,649 patients with an intermediate-risk Duke treadmill score and no stress myocardial perfusion defect. Note that the clinicians involved in the decision-making process seldom chose to perform cardiac catheterization in these patients. The findings of this study add strength to the concept that stress myocardial perfusion single-photon emission CT is highly effective in clinical decision-making applied to the management of patients with intermediate-risk Duke treadmill scores (Adapted from Gibbons et al. [39]).
Drivers of referral to catheterization and revascularization after myocardial perfusion single-photon emission CT (MPS). It is currently assumed by many that physicians appropriately weigh the various patient characteristics available to the referring physician after the stress MPS study in formulating the final management decision. In 2003, Hachamovitch et al. [59] demonstrated that the amount of ischemia was strongly related to survival benefit with revascularization and at the same time contributed 83 % of the information in a multivariable model predicting revascularization [52] based on data in 10,627 patients without prior coronary artery disease (CAD) referred to stress MPS (a). Importantly, the shape of this relationship also yields considerable insight into how doctors use MPS results. First, with increasing amounts of ischemia, there are increasing referral rates to revascularization. The ischemia–revascularization relationship, however, is highly nonlinear. With increasing ischemia in the range of no or mild ischemia (<12.5 % myocardium ischemic), there is a steep slope between ischemia and revascularization referral such that a small change in ischemia is associated with a large change in the likelihood of revascularization. At approximately 10–15 % of the myocardium ischemic, this relationship plateaus, such that increasing amounts of ischemia are associated with relatively little increase in the rate of revascularization. Further, referring physicians did not act on the ischemia information alone, but other factors also influenced this referral decision. For example, for any level of ischemia, worsening presenting symptoms (asymptomatic [Asx], atypical symptoms [Atyp], or typical angina [TAP]) resulted in greater rates of referral. Regarding ejection fraction (EF) (b), although revascularization yields the greatest survival benefit in patients with low EF and extensive CAD, whether post-MPS referral to catheterization and revascularization are proportional to patient risk as a function of EF and ischemia was examined only recently [59]. In a cohort of 3,369 patients without prior myocardial infarction or revascularization who underwent exercise or adenosine stress MPS and were followed up for occurrence of early (<60 days) post-SPECT revascularization, 445 patients were referred to catheterization (13.2 %) and 254 to revascularization (7.5 %) early after MPS. Logistic regression analysis was used to determine the association of clinical, historical stress, and MPS factors with referral to catheterization and revascularization in separate models. The likelihood of referral to catheterization increased with both increasing ischemia and decreasing EF. Referral rates to catheterization (b) increased with decreasing values of EF in the setting of no (<5 % myocardium ischemic) or mild to moderate amounts of ischemia (5–15 % myocardium ischemic), but this pattern was reversed in patients with severe ischemia (>15 % myocardium ischemic) wherein predicted referral rates to catheterization decreased with decreasing EF. Referral rates to revascularization increased markedly with increasing amounts of ischemia, plateauing beyond 15 % myocardium ischemic, and demonstrated a mild decrease in referral rates with decreasing EF that was quantitatively not as significant as that found in the referral to catheterization model. Although referral to revascularization seemed to be in proportion to the anticipated risk in these patients, catheterization was the rate-limiting step in the evaluation of these patients and was significantly influenced by an EF-related referral bias in which clinicians may have been hesitant to consider revascularization in patients with low EF at the time of this study. This referral bias helps explain the findings from the Mayo Clinic that found that in a cohort of 77 patients with congestive heart failure, left ventricular EF less than 45 %, and large reversible perfusion defects by single-photon emission CT (SPECT), the 5-year revascularization rate was only 13 % despite a 57.6 % mortality rate over this same period of time (Adapted from Hachamovitch et al. [59]).
Use of noninvasive cardiovascular (CV) imaging. Relative observed (a) and risk-adjusted (b) frequencies of referral to catheterization after normal/nonobstructive, mildly abnormal, and moderately to severely abnormal cardiovascular imaging with stress single-photon emission CT (SPECT) (blue), stress positron emission tomography (PET) (red), and cardiac CT (green): how are referring physicians using the results of noninvasive CV imaging? The SPARC study (Study of Myocardial Perfusion and Coronary Anatomy Imaging Roles in Coronary Artery Disease) prospectively enrolled more than 3,000 patients with an intermediate to high likelihood of coronary artery disease (CAD) or known CAD who were referred to a clinically indicated stress SPECT, stress PET, or cardiac CT at 40 enrolling sites. In an analysis of a subset of 1,703 patients without prior CAD, the authors examined post-imaging referral rates to catheterization. For all three modalities, increasing test abnormality (extent/severity of perfusion defect, extent of anatomic CAD) was associated with increasing referral rates to catheterization. Multivariable modeling revealed that the most important predictor of this referral was the amount of abnormality on the imaging. Importantly, however, in terms of absolute referral rates, in the setting of the most abnormal test results in patients with no prior CAD referred for suspicion of ischemic heart disease, only about half of these patients without prior CAD diagnosis were referred to catheterization. Previous studies examining this phenomenon hypothesized that in these patients physicians were managing patients with aggressive medical therapy rather than immediate referral to an invasive strategy. However, this parameter was also examined in the SPARC study, which found that in patients with the most abnormal test result the degree of medical therapy given was also less than would be expected (c). In these patients, although the proportion of patients on aspirin and β-blocker agents increased after testing, with respect to both these agents as well as lipid-lowering agents, surprising numbers of patients were not prescribed these medications within 90 days after testing. Only about one in five patients was on all three medications at the end of the trial; most were on one or two medications. While the SPARC study was designed to examine posttest resource utilization, it was not designed to identify why referring physicians did or did not alter posttest patient management. These results, while thought provoking, suggest that further studies are needed to fully understand physician decision-making after MPS. Nonetheless, this phenomenon will require further examination in the future. CTA CT angiography.
Myocardial perfusion single-photon emission CT (MPS) results, post-MPS referral patterns to revascularization, and the subsequent posttest referral bias’ obfuscation of post-MPS event rates. It has long been appreciated that the use of MPS data to dictate post-MPS management, as supported by the above, results in a high rate of catheterization in patients with abnormal MPS and a low rate of catheterization in patients with normal MPS, creating a partial verification bias associated with lowered specificity and increased sensitivity in studies assessing MPS test diagnostic accuracy. What is not generally appreciated, however, is that this same referral pattern to catheterization and revascularization that creates a diagnostic bias also results in a prognostic bias (more specifically, a differential treatment selection bias) [60]. Since imaging results affect patient management, especially referral to revascularization, and revascularization affects risk, the association between test results and revascularization referral results in a lowering of observed patients’ risk in proportion to their imaging results. Hence, as seen in Figs. 7.14 and 7.24, risk is underestimated in patients with more abnormal MPS results, resulting in a flattening of the MPS result–risk relationship in proportion to intervention rates. A recent study examined the impact of revascularization on observed hard event (HE) rates in a cohort of patients with high pre-MPS likelihood of coronary artery disease [37]. Examining 240 patients treated medically and 204 patients treated with revascularization, this study found that the HE rate in patients referred to revascularization would have been nearly three times higher (11 vs. 4.4 %) if these patients would have been treated with medical therapy as opposed to revascularization. Thus, this study provides both evidence of this prognostic referral bias and a quantitative handle on its potential impact (Adapted from Hachamovitch et al. [37]).
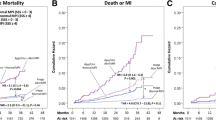
Using myocardial perfusion single-photon emission CT (MPS) for medical decision making: identification of optimal patient management. To date, almost all studies investigating the relationship of MPS results and patient risk have included only those patients who are treated medically (as patients treated with early revascularization are excluded or censored from these analyses since the decision to refer to early revascularization is usually based on the results of the MPS study). Thus, no prognostication can be extrapolated to patients treated with revascularization. In this context, an important study published in 2003 examined the relationship between the extent and severity of ischemia and the survival benefit associated with subsequent revascularization [48]. In this study, 10,627 patients without prior myocardial infarction or revascularization who underwent stress MPS were followed for a mean of 1.9 years (3.98 % lost to follow-up). Over this time period, cardiac death occurred in 146 patients (1.4 % mortality). The authors defined patient treatment on the basis of that received within 60 days post-MPS (revascularization [671 patients, 2.8 % mortality] vs medical therapy [9,956 patients, 1.3 % mortality; P = 0.0004]). The authors used a risk-adjusted approach that included a propensity score to adjust for nonrandomization of the treatment assignment, which was developed using logistic regression. This propensity score was used to adjust survival analyses. Based on the Cox proportional hazards model, which is most predictive of cardiac death (x 2 = 539, P < 0.0001), patients undergoing medical therapy as their initial treatment had superior survival compared to those patients referred to revascularization in the setting of no or mild ischemia. On the other hand, patients undergoing revascularization had an increasing survival benefit over patients who were undergoing medical therapy when moderate to severe ischemia (>10 % of the total myocardium ischemic) was detected by MPS (a). While ischemia was the sole identifier of whether survival was enhanced with revascularization or medical therapy (relative benefit), the absolute benefit (e.g., number of lives saved per 100 treated with different therapies) was impacted by baseline patient risk. Hence, the absolute benefit for revascularization over medical therapy was accentuated in the presence of greater clinical risk (patients undergoing pharmacologic stress, diabetic women, and elderly patients) (b–d) as well as in diabetics (not shown) (Adapted from Hachamovitch et al. [48]).
In the context of the results presented in Fig. 7.39, specifically, the ability of myocardial perfusion single-photon emission CT (MPS)-determined ischemia to identify which patients may benefit from revascularization versus medical therapy, the role of a gated ejection fraction (EF) in identifying patient benefit must also be assessed. In a study of 5,366 consecutive patients without a history of prior revascularization followed up for 2.8 ± 1.2 years (during which 146 cardiac deaths occurred [2.7 %, 1.0 %/year]), the relative roles of ischemia and EF for the assessment of cardiac death (CD) risk and potential benefit with revascularization were examined [50]. A Cox proportional hazards survival model was used to adjust for differences in patients’ baseline characteristics, as well as a propensity score to correct for nonrandomized patient referral to revascularization versus medical therapy. While this model identified EF to be by far the strongest predictor of CD, ischemia, but not EF, was found to have a significant interaction with therapy given. The latter indicates that the survival associated with any level of ischemia was dependent on the treatment given and the survival associated with treatment dependent on the level of ischemia (e.g., superior survival with medical therapy in the presence of little or no ischemia, enhanced survival with revascularization in the setting of increasing ischemia) (a). Further, after adjusting for baseline differences, ischemia and EF added incrementally to each other with respect to the risk of CD, as the risk of CD increased with decreasing values of gated EF and the risk of CD at any level of EF increased with increasing amounts of ischemia (b). Interestingly, 10 % myocardial ischemia appeared to identify patients who would have a survival benefit with revascularization across the spectrum of EF. Thus, while simple measurement of EF alone defines patients at high risk, only ischemia appeared to identify a survival benefit with revascularization. These data illustrate the difference between risk assessment and prediction of benefit from revascularization. The added value of ischemia to EF was only present in medically treated patients, as the relationship between EF and ischemia in patients treated with revascularization is limited to a single line, as increasing levels of ischemia are not associated with increasing risk in the setting of revascularization. The relationship between ischemia and EF is further illustrated in (c)—absolute risk is greatest in the presence of lower EF (as evidenced by the higher CD rates on the right side of the figure). Irrespective of EF, in the absence of ischemia (no ischemia), the risk of CD is greater with early revascularization than medical therapy, while the converse is true in the presence of ischemia. Hence, although benefit is best predicted by ischemia, both risk and relative benefit are best predicted by the combination of EF and ischemia. F/U follow-up, SPECT single-photon emission CT.
Stress myocardial perfusion single-photon emission CT (MPS) techniques to identify the risk of adverse events. The use of stress MPS techniques to identify the risk of adverse events in patients referred for medical therapy after testing separately from the risk of patients referred to revascularization is an important paradigm shift for our field. In the context of patient management, the identification of patient risk may permit more precise risk stratification but will not necessarily aid in the identification of optimal therapeutic selection. Indeed, those factors that identify which patients may accrue a survival benefit from referral to revascularization versus medical therapy are not the most powerful predictors of risk (ischemia), but those factors that best predict post-MPS survival (e.g., scar extent, left ventricular ejection fraction [LVEF]) do not predict potential benefit. In the setting of a healthcare system focusing on improving patient benefit, this approach will become central to our efforts. Since the initial report identifying this finding, several studies have extended our knowledge of key-related details. First, risk-adjusted analyses of observational data in an elderly population with a threshold of greater than or equal to 15 % ischemia identify patients with lower mortality rates with revascularization than medical therapy (47 vs. 58 % over a 6.2 ± 2.9-year follow-up; a). This was not the case in patients with abnormal MPS with ischemia less than 15 % (53 vs. 47 %) nor in patients with abnormal MPS without ischemia (77 vs. 50 %). Further, this same finding was reported in diabetic patients who were referred for MPS. In diabetic patients with approximately greater than or equal to 16 % of the myocardium abnormal, revascularization was associated with superior survival compared to medical therapy (b). The relationship between scar, ischemia, and therapeutic impact is an important one. An important question is whether the presence of an extensive scar, with accompanying remodeling and reductions in LVEF, eliminates the potential survival benefit associated with any significant amount of ischemia. An analysis of data in patients with prior myocardial infarction revealed equipoise between therapeutic strategies across all values of myocardium ischemic; (c, right). However, when the analysis was limited to patients with less than 10 % of the myocardium with fixed defects (b, left), patients with little or no ischemia had worsened survival with the use of revascularization, while patients with more extensive ischemia benefited from this intervention. For example, in the absence of ischemia, patients treated with revascularization had a 49 % greater mortality risk, but patients with 20 % of their myocardium ischemic had a 20 % reduction in risk with revascularization. Thus, based on studies to date, only inducible ischemia appears to identify which patients may benefit from revascularization over medical therapy after MPS. However, whether a benefit is associated with revascularization is sensitive to the extent of scar present. Also, the threshold of ischemia at which equipoise occurs is sensitive to the endpoint used and the population examined. Finally, although the LVEF impacts the absolute benefit (e.g., lives saved per 100 treated) at any level of ischemia, it does not identify which patients will accrue a survival benefit with a specific therapeutic approach.
(a and b) resting 201Tl reversibility added value over summed stress score (SSS) and summed rest score (SRS). In patients with chronic coronary artery disease, the added prognostic value of resting 201Tl reversibility in dual-isotope myocardial perfusion single-photon emission CT is shown. The two curves represent differing amounts of resting reversibility as measured by the summed rest late difference score (SRLDS). When this score is greater than 8 (extensive resting ischemia), the relative risk with respect to subsequent cardiac events is clearly higher than when less resting reversibility is present. The incremental prognostic value of resting reversibility persists when either the SRS or the SSS is considered. These data suggest that a combination of assessing both stress-induced ischemia and resting ischemia (presumably hibernating myocardium) might be more effective than stress-induced ischemia alone in evaluating the risk of patients with chronic coronary artery disease (Adapted from Sharir et al. [36]).
Clinical Outcomes Utilizing Revascularization and Aggressive Drug Evaluation (COURAGE) nuclear substudy. Shaw et al. [61] reported results of a substudy of the COURAGE trial. In this study of 314 patients in whom both pre- and 6- to 18-month postrandomization myocardial perfusion single-photon emission CT (MPS) was performed, patients assigned to percutaneous coronary intervention (PCI) and optimal medical therapy (OMT) demonstrated significantly greater ischemia reduction when compared with patients receiving OMT alone (PCI + OMT: 33 % [n = 159]; OMT alone: 20 % [n = 155]; P = 0.0004) (a). Importantly, the rate of subsequent cardiac events was strongly related to the amount of residual ischemia on MPS studies performed 6–18 months after randomization (b). MI myocardial infarction (Adapted from Shaw et al. [61]).
Complementary roles of myocardial perfusion single-photon emission CT (MPS) and assessment of coronary calcium: who needs single-photon emission CT after the coronary calcium measurements? Recently, the coronary calcium score (CCS) derived from noncontrast CT assessment has become commonly used to assess the coronary atherosclerotic burden in asymptomatic patients. Generally, when the CCS exceeds 100, recommendations for aggressive medical therapy are made. When the atherosclerotic burden becomes extensive, most investigators recommend MPS or other testing for ischemia [51]. Recent data from our institution has confirmed the findings of previous studies with respect to the patients with a CCS greater than or equal to 400 [62]. In 1,195 consecutive patients with no history of coronary artery disease who had electron beam tomography and MPS, among the patients with a CCS less than 100, MPS ischemia was rare, occurring in less than 2 % of such patients [62]. This low frequency of ischemia with a CCS less than 100 was present in patients with and without clinical symptoms, although a trend toward more ischemia in symptomatic patients with scores 10–99 was observed. As the CCS increased in magnitude above 100, the frequency of myocardial ischemia on MPS increased progressively. Among patients with a CCS exceeding 1,000, 20 % manifested an ischemia by MPS (Adapted from Berman et al. [62]).
Complementary roles of myocardial perfusion single-photon emission CT (MPS) and the assessment of coronary calcium: who needs coronary calcium measurement after single-photon emission CT (SPECT)? Of 1,195 patients having both coronary calcium score (CCS) and SPECT studies in our institution, a large proportion had high enough CCS that there would be consensus that aggressive medical management is warranted: 56 % had CCS greater than 100 and 31 % had CCS greater than 400. While this frequency is inflated by a referral bias in which patients with high CCS were more likely to undergo MPS, these findings suggest that if testing begins with MPS in a given patient, further assessment of atherosclerotic burden by coronary calcium testing may be useful in assessing the need for aggressive medical therapy and lifestyle recommendations in an attempt to prevent coronary events. Clinical implications of Figs. 7.44, 7.45, and 7.46 can be summarized as follows: In asymptomatic patients, atherosclerosis imaging is more effective than imaging for ischemia, since it is better suited to defining subclinical disease in need of preventive treatment. Approximately 10 % of asymptomatic patients undergoing atherosclerosis imaging will be defined as having sufficient subclinical disease so that ischemia testing is indicated. Patients who are able to exercise and are found to have extensive atherosclerosis but no ischemia by MPS appear to be at low risk for short- to intermediate-term cardiac events, thus not requiring coronary angiography (Adapted from Berman et al. [62]).
Prognosis of patients with high coronary calcium scores (CCS) and normal exercise myocardial perfusion single-photon emission CT (MPS). Until recently, there was no data upon which to justify the common practice of following medically, without coronary angiography, patients who have normal MPS associated with a very high CCS. A publication by Rozanski et al. [63] has provided data supporting this practice. The findings indicated that the 4-year cardiac event rate in patients without ischemia was equally low in patients with and without extensive coronary atherosclerosis (CCS > 1,000). Given the known adverse prognostic implications of high CCS, these findings imply that in the absence of ischemia and with aggressive medical therapy, the adverse event rate in patients with coronary atherosclerosis is low in patients who are able to exercise. DM diabetes mellitus, MI myocardial infarction, SOB shortness of breath (Adapted from Rozanski et al. [63]).
Relationship between positron emission tomography (PET)-assessed ischemia and coronary calcium score (CCS). A more recent report of 695 symptomatic patients referred for adenosine stress PET who underwent CCS as part of routine image acquisition reported a 48.5 % frequency of abnormal stress PET in patients with CCS greater than or equal to 400, with an only slightly greater frequency (49.4 %) of abnormal PET with a CCS greater than or equal to 1,000 [64]. Interestingly, 16 % of patients with no measurable calcium had PET identified ischemia (negative predictive value 84 %). The discrepancies in the reported frequencies of abnormal myocardial perfusion single-photon emission CT (MPS) in patients with high CCS appear to be largely explained by differences in the underlying patient risk. Recent subset analyses have supported this concept, indicating that the threshold of CCS warranting referral for MPS will vary further as a function of underlying patient risk. In this regard, the frequency of abnormal MPS for any level of CCS has been reported to be higher in patients with type 2 diabetes [65–67], patients with the metabolic syndrome [68], patients with a family history of premature coronary heart disease [66, 67], and patients with a high likelihood of coronary artery disease [67]. Although no validated threshold is currently recognized, in patient cohorts at greater risk for developing early atherosclerosis, it has been suggested that a threshold CCS of greater than or equal to 100 might be appropriate for these patients (Adapted from Schenker et al. [64]).
Prognosis of patients with high coronary calcium scores (CCS) and findings on positron emission tomography (PET) with vasodilator stress. In contrast to the findings of Rozanski et al. [63] showing excellent prognosis in patients with high CCS and normal exercise myocardial perfusion single-photon emission CT (MPS), Schenker et al. [64] have shown that patients who have a nonischemic PET myocardial perfusion scan and have a CCS greater than or equal to 1,000 have a worse prognosis than those with a CCS less than 1,000 (left). These authors also demonstrated that when ischemia was seen on PET, those with a higher CCS also had a worse prognosis than those without extensive CCS (right). Multiple factors likely explain the difference between the prognostic implications of a very high CCS in patients with normal perfusion scans in these studies, with the most prominent being the pretest risk of the patients. In comparing the patients with normal perfusion scans in the two populations, those reported by Schenker et al. [64] had several features implying a “sicker” cohort as described above. The patients were referred for pharmacologic stress, older, more symptomatic, and had a higher pretest likelihood of coronary artery disease. The work of Schenker et al. [64] provides evidence that the measurement of the CCS adds to the prognostic information provided by myocardial perfusion imaging. MI myocardial infarction (Adapted from Schenker et al. [64]).
Conceptual approach to the use of CT coronary calcium measurements and nuclear testing in coronary artery disease (CAD) diagnosis and risk stratification in asymptomatic patients. First, the pretest likelihood of angiographically significant CAD is assessed as low (less than 10 %), low–intermediate (10–50 %), high–intermediate (50–85 %), and high (>85 %) employing age, sex, risk factors, and symptoms. Patients with a low likelihood of CAD (in our experience <15 %) or low 10-year risk (<10 %) require only primary prevention guidelines regarding coronary risk factors (Adult Treatment Panel III) [16]. Patients with a low–intermediate likelihood of CAD (15–50 %), a group which by American College of Cardiology/American Heart Association guidelines might be selected for exercise testing, become excellent candidates for coronary calcium score (CCS) measurement in this approach. Since CCS provides a more sensitive, quantitative measurement of subclinical CAD in this population, we consider it more useful than the exercise electrocardiogram in selecting patients for aggressive medical management. Patients would then have the intensiveness of their medical therapy guided by the degree of CCS abnormality. Scores greater than 100 are regarded by many as the cutoff for recommending aggressive medical therapy with target low-density lipoprotein less than 70 and the target blood pressure would be 120/80 mm Hg [68]. Patients with scores greater than or equal to 10 but less than 100 might be considered as appropriate for aggressive medical therapy when CCS is in the 90th percentile or greater for age and gender [62], although the exact thresholds remain controversial. Regarding further testing, patients with CCS greater than 400 would be candidates for further testing with myocardial perfusion single-photon emission CT (SPECT) for purposes of risk/benefit assessment with respect to the possible need to consider revascularization. The exact cutoff above which patients should be referred for stress imaging is unclear; in the presence of symptoms, referral for nuclear testing might be appropriate with any abnormal score. In asymptomatic patients, the threshold for referral of 400 may be appropriate. In the CCS category of 100–400, it would not be cost effective to refer all patients for myocardial perfusion scanning; however, if tailoring this referral to the individual patient based on age, sex, and risk factors, selective referral for stress imaging might be appropriate. In this regard, a recent manuscript has shown that the category of 100–400 would deserve testing in diabetic patients [69], and preliminary data has suggested that this would be appropriate in patients with the metabolic syndrome [70]. In selected patients with normal or nearly normal nuclear scans, CCS might be appropriate in order to evaluate the extent of atherosclerosis and help guide medical management decisions [71] and to avoid missing extensive atherosclerosis simply because there is no regional stress-induced ischemia (i.e., balanced reduction in flow). While CCS testing might not be needed in patients who are already following an aggressive medical management approach using secondary prevention guidelines, the CCS in this setting may help motivate patients to follow medical approaches to control CAD as well as to guide the intensity of medical management in settings in which the need for secondary prevention is not clear (Adapted from Berman et al. [72]).
References
Hasdai D, Gibbons RJ, Holmes Jr DR, et al. Coronary endothelial dysfunction in humans is associated with myocardial perfusion defects. Circulation. 1997;96:3390–5.
Ladenheim ML, Pollock BH, Rozanski A, et al. Extent and severity of myocardial hypoperfusion as predictors of prognosis in patients with suspected coronary artery disease. J Am Coll Cardiol. 1986;7:464–71.
Garcia EV. Quantitative myocardial perfusion single-photon emission computed tomographic imaging: quo vadis? (Where do we go from here?). J Nucl Cardiol. 1994;1:83–93.
Sharir T, Germano G, Waechter PB, et al. A new algorithm for the quantitation of myocardial perfusion SPECT. II: validation and diagnostic yield. J Nucl Med. 2000;41:720–7.
Germano G, Kavanagh P, Waechter P, et al. A new algorithm for the quantitation of myocardial perfusion SPECT. I: technical principles and reproducibility. J Nucl Med. 2000;41:712–9.
Berman DS, Abidov A, Kang X, et al. Prognostic validation of a 17-segment score derived from a 20-segment score for myocardial perfusion SPECT interpretation. J Nucl Cardiol. 2004;11:414–23.
Berman DS, Kiat H, Friedman JD, et al. Separate acquisition rest thallium-201/stress technetium-99m sestamibi dual-isotope myocardial perfusion single-photon emission computed tomography: a clinical validation study. J Am Coll Cardiol. 1993;22:1455–64.
Cerqueira MD, Weissman NJ, Dilsizian V, et al. Standardized myocardialsegmentation and nomenclature for tomographic imaging of the heart: a statement for healthcare professionals from the Cardiac Imaging Committee of the Council on Clinical Cardiology of the American Heart Association. Circulation. 2002;105:539–42.
Berman DS, Kang X, Gransar H, et al. Quantitative assessment of myocardialperfusion abnormality on SPECT myocardial perfusion imaging is more reproducible than expert visual analysis. J Nucl Cardiol. 2009;16(1):45–53.
Slomka PJ, Nishina H, Berman DS, et al. Automated quantification of myocardial perfusion SPECT using simplified normal limits. J Nucl Cardiol. 2005;12:66–77.
Mazzanti M, Germano G, Kiat H, et al. Identification of severe and extensive coronary artery disease by automatic measurement of transient ischemic dilation of the left ventricle in dual-isotope myocardial perfusion SPECT. J Am Coll Cardiol. 1996;27:1612–20.
Shaw LJ, Hachamovitch R, Berman DS, et al. The economic consequences of available diagnostic and prognostic strategies for the evaluation of stable angina patients: an observational assessment of the value of precatheterization ischemia. J Am Coll Cardiol. 1999;33:661–9.
Matzer L, Kiat H, Van Train K, et al. Quantitative severity of stress thallium-201 myocardial perfusion single-photon emission computed tomography defects in one-vessel coronary artery disease. Am J Cardiol. 1993;72:273–9.
Sharir T, Bacher-Stier C, Dhar S, et al. Identification of severe and extensivecoronary artery disease by postexercise regional wall motion abnormalities inTc-99m sestamibi gated single-photon emission computed tomography. Am J Cardiol. 2000;86:1171–5.
Borges-Neto S, Shaw LK, Tuttle RH. Incremental prognostic power of SPECT myocardial perfusion imaging in patients with known or suspected coronary artery disease. Am J Cardiol. 2005;95:182–8.
Berman DS, Hachamovitch R, Kiat H, et al. Incremental value of prognostic testing in patients with known or suspected ischemic heart disease: a basis for optimal utilization of exercise technetium-99m sestamibi myocardial perfusion single-photon emission computed tomography. J Am Coll Cardiol. 1995;26:639–47 (published erratum appears in J Am Coll Cardiol. 1996;27:756).
Christian TF, Miller TD, Bailey KR, Gibbons RJ. Exercise tomographic thallium-201 imaging in patients with severe coronary artery disease and normal electrocardiograms. Ann Intern Med. 1994;121:825–32.
Hachamovitch R, Berman DS, Kiat H, et al. Value of stress myocardial perfusion single photon emission computed tomography in patients with normal resting electrocardiograms: an evaluation of incremental prognostic value and costeffectiveness. Circulation. 2002;105:823–9.
Klocke FJ, Baird MG, Lorell BH, et al. ACC/AHA/ASNC guidelines for the clinical use of cardiac radionuclide imaging-executive summary. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (ACC/AHA/ASNC committee to revise the 1995 guidelines for the clinical use of cardiac radionuclide imaging). Circulation. 2003;108:1404–18.
Berman DS, Hachamovitch R, Shaw LJ, et al. Nuclear cardiology. In: Fuster V, O’Rourke RA, Roberts R, et al., editors. Hurst’s the heart. 11th ed. New York: McGraw-Hill Companies; 2004. p. 563–97.
Ladenheim ML, Kotler TS, Pollock BH, et al. Incremental prognostic power of clinical history, exercise electrocardiography and myocardial perfusion scintigraphy in suspected coronary artery disease. Am J Cardiol. 1987;59:270–7.
Hachamovitch R, Berman DS, Kiat H, et al. Exercise myocardial perfusion SPECT in patients without known coronary artery disease: incremental prognostic value and use in risk stratification. Circulation. 1996;93:905–14.
Hachamovitch R, Berman DS, Shaw LJ, et al. Incremental prognostic value of myocardial perfusion single photon emission computed tomography for the prediction of cardiac death: differential stratification for risk of cardiac death and myocardial infarction. Circulation. 1998;97:535–43.
Marwick TH, Shaw LJ, Lauer MS, et al. The noninvasive prediction of cardiac mortality in men and women with known or suspected coronary artery disease. Economics of Noninvasive Diagnosis (END) Study Group. Am J Med. 1999;106:172–8.
Sharir T, Germano G, Kang X, et al. Prognostic value of post-stress left ventricular volume and ejection fraction by gated myocardial perfusion single photon emission computed tomography in women: gender related differences in normal limits and outcome [abstract]. Circulation. 2002;106:II–523.
Zellweger MJ, Lewin HC, Lai S, et al. When to stress patients after coronary artery bypass surgery? Risk stratification in patients early and late post-CABG using stress myocardial perfusion SPECT: implications of appropriate clinical strategies. J Am Coll Cardiol. 2001;37:144–52.
Sharir T, Germano G, Kang X, et al. Prediction of myocardial infarction versus cardiac death by gated myocardial perfusion SPECT: risk stratification by the amount of stress-induced ischemia and the poststress ejection fraction. J Nucl Med. 2001;42:831–7.
Travin MI, Heller GV, Johnson LL, et al. The prognostic value of ECG-gated SPECT imaging in patients undergoing stress Tc-99m sestamibi myocardialperfusion imaging. J Nucl Cardiol. 2004;11:253–62.
Thomas GS, Miyamoto MI, Morello AP, et al. Technetium99m based myocardial perfusion imaging predicts clinical outcome in the community outpatient setting: the nuclear utility in the community (“nuc”) study. J Am Coll Cardiol. 2004;43:213–23.
Heller GV, Herman SD, Travin MI, et al. Independent prognostic value of intravenous dipyridamole with technetium-99m sestamibi tomographic imaging in predicting cardiac events and cardiac-related hospital admissions. J Am Coll Cardiol. 1995;26:1202–8.
Kang X, Berman DS, Lewin HC, et al. Incremental prognostic value of myocardial perfusion single photon emission computed tomography in patients with diabetes mellitus. Am Heart J. 1999;138(6 Pt 1):1025–32.
Giri S, Shaw LJ, Murthy DR, et al. Impact of diabetes on the risk stratification using stress single-photon emission computed tomography myocardial perfusion imaging in patients with symptoms suggestive of coronary artery disease. Circulation. 2002;105:32–40.
Vanzetto G, Ormezzano O, Fagret D, et al. Long-term additive prognostic value of thallium-201 myocardial perfusion imaging over clinical and exercise stress test in low to intermediate risk patients: study in 1137 patients with 6-year follow-up. Circulation. 1999;100:1521–7.
Diamond GA, Staniloff HM, Forrester JS, et al. Computer-assisted diagnosis in the noninvasive evaluation of patients with suspected coronary artery disease. J Am Coll Cardiol. 1983;1(2 Pt 1):444–55.
Wackers FJ, Young LH, Inzucchi SE, et al. Detection of silent myocardial ischemia in asymptomatic diabetic subjects: the DIAD study. Diabetes Care. 2004;27:1954–61.
Sharir T, Berman DS, Lewin HC, et al. Incremental prognostic value of rest-redistribution Tl-201 single-photon emission computed tomography. Circulation. 1999;100:1964–70.
Hachamovitch R, Hayes SW, Friedman JD, et al. Stress myocardial perfusion SPECT is clinically effective and cost-effective in risk-stratification of patients with a high likelihood of CAD but no known CAD. J Am Coll Cardiol. 2004;43:200–8.
Gibbons RJ, Chatterjee K, Daley J, et al. ACC/AHA/ACP-ASIM guidelines forthe management of patients with chronic stable angina: a report of the American College of Cardiology/American Heart Association Task Force on PracticeGuidelines (Committee on Management of Patients with Chronic Stable Angina). J Am Coll Cardiol. 1999;33:2092–197.
Gibbons RJ, Hodge DO, Berman DS, et al. Long-term outcome of patients with intermediate-risk exercise electrocardiograms who do not have myocardialperfusion defects on radionuclide imaging. Circulation. 1999;100:2140–5.
Shaw LJ, Iskandrian AE. Prognostic value of gated myocardial perfusion SPECT. J Nucl Cardiol. 2004;11:171–85.
Expert Panel on Detection. Evaluation, and treatment of high blood cholesterol in adults: executive summary of the third report of the National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (adult treatment panel III). JAMA. 2001;285:2486–97.
Beller GA. The epidemics of obesity and type 2 diabetes: Implications for noninvasive cardiovascular imaging. Journal of Nuclear Cardiology 2004; 11(2):105–6
Stratmann HG, Tamesis BR, Younis LT, et al. Prognostic value of dipyridamole technetium-99m sestamibi myocardial tomography in patients with stable chest pain who are unable to exercise. Am J Cardiol. 1994;73:647–52.
Shaw L, Chaitman BR, Hilton TC, et al. Prognostic value of dipyridamole thallium-201 imaging in elderly patients [comment]. J Am Coll Cardiol. 1992;19:1390–8.
Calnon DA, McGrath PD, Doss AL, et al. Prognostic value of dobutamine stress technetium-99m-sestamibi single-photon emission computed tomographymyocardial perfusion imaging: stratification of a high-risk population [comment]. J Am Coll Cardiol. 2001;38:1511–7.
Amanullah AM, Kiat H, Friedman JD, Berman DS. Adenosine technetium-99m sestamibi myocardial perfusion SPECT in women: diagnostic efficacy in detection of coronary artery disease. J Am Coll Cardiol. 1996;27:803–9.
Hachamovitch R, Hayes S, Friedman JD, et al. Determinants of risk and its temporal variation in patients with normal stress myocardial perfusion scans: what is the warranty period of a normal scan? J Am Coll Cardiol. 2003;41:1329–40.
Hachamovitch R, Hayes SW, Friedman JD, et al. Comparison of the short-term survival benefit associated with revascularization compared with medical therapy in patients with no prior coronary artery disease undergoing stress myocardial perfusion single photon emission computed tomography. Circulation. 2003;107:2900–7.
Berman DS, Kang X, Hayes SW, et al. Adenosine myocardial perfusion single-photon emission computed tomography in women compared with men. Impact of diabetes mellitus on incremental prognostic value and effect on patient management. J Am Coll Cardiol. 2003;41:1125–33.
Hachamovitch R, Rozanski A, Hayes SW, et al. Predicting therapeutic benefit from myocardial revascularization procedures: are measurements of both resting left ventricular ejection fraction and stress-induced myocardial ischemia necessary? J Nucl Cardiol. 2006;13:768–78.
He ZX, Hedrick TD, Pratt CM, et al. Severity of coronary artery calcification by electron beam computed tomography predicts silent myocardial ischemia. Circulation. 2000;101:244–51.
Iskander S, Iskandrian AE. Risk assessment using single-photon emission computed tomographic technetium-99m sestamibi imaging. J Am Coll Cardiol. 1998;32:57–62.
Abidov A, Hachamovitch R, Rozanski A, et al. Prognostic implications of atrial fibrillation in patients undergoing myocardial perfusion single-photon emission computed tomography. J Am Coll Cardiol. 2004;44:1062–70.
Shaw LJ, Hendel RC, Cerqueira M, et al. Ethnic differences in the prognostic value of stress technetium-99m tetrofosmin gated single-photon emission computed tomography myocardial perfusion imaging. J Am Coll Cardiol. 2005;45:1494–504.
Matsuo S, Nakajima K, Horie M, J-ACCESS Investigators, et al. Prognostic value of normal stress myocardial perfusion imaging in Japanese population. Circ J. 2008;72:611–7.
Zellweger MJ, Hachamovitch R, Kang X, et al. Prognostic relevance of symptoms versus objective evidence of coronary artery disease in diabetic patients. Euro Heart J. 2004;25:543–50.
Abidov A, Hachamovitch R, Hayes SW, et al. Prognostic impact of hemodynamic response to adenosine in patients older than age 55 years undergoing vasodilator stress myocardial perfusion study. Circulation. 2003;107:2894–9.
Hachamovitch R, Hayes SW, Friedman JD, et al. A prognostic score for prediction of cardiac mortality risk after adenosine stress myocardial perfusion scintigraphy. J Am Coll Cardiol. 2005;45:722–9.
Hachamovitch R, Friedman JD, Cohen I, et al. Is there a referral bias against revascularization of patients with reduced LV ejection fraction? Influence of ejection fraction and inducible ischemia on post-SPECT management of patients without history of CAD. J Am Coll Cardiol. 2003;42:1286–94.
Hachamovitch R, Di Carli MF. Methods and limitations of assessing newnoninvasive tests: part I: anatomy-based validation of noninvasive testing. Circulation. 2008;117:2684–90.
Shaw LJ, Berman DS, Maron DJ, et al. Optimal medical therapy with or without percutaneous coronary intervention to reduce ischemic burden: results from the clinical outcomes utilizing revascularization and aggressive drug evaluation (COURAGE) trial nuclear substudy. Circulation. 2008;117:1283–91.
Berman DS, Wong ND, Gransar H, et al. Relationship between stress-induced myocardial ischemia and atherosclerosis measured by coronary calcium tomography. J Am Coll Cardiol. 2004;44:923–30.
Rozanski A, Gransar H, Wong ND, et al. Clinical outcomes after both coronary calcium scanning and exercise myocardial perfusion scintigraphy. J Am Coll Cardiol. 2007;49:1352–61.
Schenker MP, Dorbala S, Hong EC, et al. Interrelation of coronary calcification, myocardial ischemia, and outcomes in patients with intermediate likelihood of coronary artery disease: a combined positron emission tomography/computed tomography study. Circulation. 2008;117:1693–700.
Anand DV, Lim E, Hopkins D, et al. Risk stratification in uncomplicated type 2 diabetes: prospective evaluation of the combined use of coronary artery calcium imaging and selective myocardial perfusion scintigraphy. Eur Heart J. 2006;27:713–21.
Blumenthal RS, Becker DM, Yanek LR, et al. Comparison of coronary calcium and stress myocardial perfusion imaging in apparently healthy siblings of individuals with premature coronary artery disease. Am J Cardiol. 2006;97:328–33.
Rozanski A, Gransar H, Wong ND, et al. Use of coronary calcium scanning for predicting inducible myocardial ischemia: Influence of patients’ clinical presentation. J Nucl Cardiol. 2007;14:669–79.
Grundy SM, Cleeman JI, Merz CN, et al. Implications of recent clinical trials for the National Cholesterol Education Program Adult Treatment Panel III guidelines. Circulation. 2004;110:227–39.
Anand DV, Lim E, Raval U, et al. Prevalence of silent myocardial ischemia in asymptomatic individuals with subclinical atherosclerosis detected by electron beam tomography. J Nucl Cardiol. 2004;11:450–7.
Wong ND, Rozanski A, Gransar H, et al. Metabolic syndrome and diabetes are associated with an increased likelihood of inducible myocardial ischemia among patients with subclinical atherosclerosis. Diabetes Care. 2005;28:1445–50.
Berman DS, Hayes S, Friedman J, et al. Normal myocardial perfusion SPECT does not imply the absence of significant atherosclerosis [abstract]. Circulation. 2003;108:IV–562.
Berman DS, Hachamovitch R, Shaw LJ, et al. Roles of nuclear cardiology, cardiac computed tomography, and cardiac magnetic resonance: noninvasive risk stratification and a conceptual framework for the selection of noninvasive imaging tests in patients with known or suspected coronary artery disease. J Nucl Med. 2006;47:1107–18.
Acknowledgment
The authors gratefully acknowledge the valuable assistance of Xingping Kang, MD in the preparation of this chapter.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2013 Springer Science+Business Media, LLC
About this chapter
Cite this chapter
Hachamovitch, R., Berman, D., Shaw, L.J., Germano, G., Mieres, J.H. (2013). Risk Stratification and Patient Management. In: Dilsizian, V., Narula, J. (eds) Atlas of Nuclear Cardiology. Springer, New York, NY. https://doi.org/10.1007/978-1-4614-5551-6_7
Download citation
DOI: https://doi.org/10.1007/978-1-4614-5551-6_7
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4614-5549-3
Online ISBN: 978-1-4614-5551-6
eBook Packages: MedicineMedicine (R0)