Abstract
-
Incidence: 12,000/year in the USA
-
Prevalence: ∼265,000 in the USA
-
Age of Injury:
-
Average age 40.7 years
-
Bi-modal distribution between 16 and 30 years and 65+ years
-
-
Gender: 80.7% male
-
Race/Ethnicity:
-
66.5% Caucasian
-
26.8% African–American
-
8.3% Hispanic
-
0.9% Asian
-
-
Etiology:
-
40.4% Motor vehicle accidents
-
27.9% Falls
-
15% Violence
-
8% Sports
-
-
Neurologic Level and Extent of Lesion:
-
39.5% incomplete tetraplegia
-
22.1% complete paraplegia
-
21.7% incomplete paraplegia
-
16.3% complete tetraplegia
-
-
Marital status: 51.9% of persons with spinal cord injury (SCI) are single at the time injury
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Spinal Cord Injury
- Heterotopic Ossification
- Pressure Ulcer
- Lower Motor Neuron
- Spinal Cord Injury Patient
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Epidemiology of SCI [1]
-
Incidence: 12,000/year in the USA
-
Prevalence: ∼265,000 in the USA
-
Age of Injury:
-
Average age 40.7 years
-
Bi-modal distribution between 16 and 30 years and 65+ years
-
-
Gender: 80.7% male
-
Race/Ethnicity:
-
66.5% Caucasian
-
26.8% African–American
-
8.3% Hispanic
-
0.9% Asian
-
-
Etiology:
-
40.4% Motor vehicle accidents
-
27.9% Falls
-
15% Violence
-
8% Sports
-
-
Neurologic Level and Extent of Lesion:
-
39.5% incomplete tetraplegia
-
22.1% complete paraplegia
-
21.7% incomplete paraplegia
-
16.3% complete tetraplegia
-
-
Marital status: 51.9% of persons with spinal cord injury (SCI) are single at the time injury
Spinal Cord Injury Syndromes
Central Cord Syndrome
Cervical spinal cord injury affecting primarily the central tracts
-
Epidemiology: Most common, ∼50% of incomplete injuries, 9% of traumatic SCI [2, 3]
-
Pathophysiology:
-
Risk factors: Cervical stenosis and hyperextension injury
-
Clinical:
-
Upper extremity weakness greater than lower extremity weakness
-
Seen often in elderly patients with cervical spondylosis
-
Usually results from a fall [4]
-
-
Prognosis:
-
Favorable prognosis for functional recovery, especially in patients with initial classification of AIS D [6]
-
Recovery typically occurs first in LEs, then bowel/bladder, then arms, then hands
-
Better prognosis for younger than older patients [7]
-
Independent ambulation (87–97% vs. 31–41%)
-
Bladder function (83% vs. 29%)
-
Dressing (77% vs. 12%)
-
-
Brown-Sequard Syndrome (BSS)
Lateral hemisection of the spinal cord
-
Etiology:
-
Clinical:
-
At level: Loss of all sensory modalities and flaccid paralysis—Lower Motor Neuron (LMN) lesion
-
Below level:
-
Ipsilateral loss of vibration, proprioception; spastic paralysis—Upper Motor Neuron (UMN) lesion
-
Contralateral loss of pain/temperature
-
-
-
-
Best prognosis for functional outcome of the incomplete SCI syndromes
-
75–90% of patients will ambulate independently upon discharge from rehabilitation
-
70% Independent for activities of daily living (ADL’s)
-
Anterior Cord Syndrome
Injury to the anterior 2/3 of the spinal cord with preservation of the posterior columns
-
Epidemiology: 2.7% of all traumatic SCI [9]
-
-
Flexion injury, direct damage from bone fragment or disc compression
-
Vascular insufficiency produced by occlusion of anterior spinal artery
-
-
Clinical:
-
Bilateral loss of motor and pain/temperature
-
Relative preservation of light touch, proprioception
-
-
Prognosis: 10–20% likelihood of motor recovery [14]
Posterior Cord Syndrome
Injury to the dorsal columns of the cord with relative sparing of the anterior 2/3
-
Epidemiology: Least common incomplete injury, incidence <1% [2, 9]
-
Etiology:
-
Hyperextension injuries
-
Posterior spinal artery occlusion
-
Tumors
-
Vitamin B12 deficiency
-
-
Clinical:
-
Loss of proprioception and vibration sense
-
Preservation of motor and pain/temperature
-
-
Prognosis: Poor for ambulation due to proprioceptive deficits
Conus Medullaris and Cauda Equina Syndromes
-
Conus medullaris injuries affect the terminal spinal cord as well as lumbar nerve roots, resulting in UMN and LMN injury.
-
Cauda equina injuries affect only the nerve roots (lumbar and/or sacral) and are therefore LMN injuries.
-
Epidemiology: [2]
-
Cauda equina 5.2% of SCI
-
Conus medullaris 1.7% of SCI
-
-
Etiology:
-
Trauma, fracture, tumor, lumbar spondylosis, abscess, hematoma, spina bifida, ischemia
-
-
Clinical—Cauda equina:
-
Loss of LE, anal, and bulbocavernosis reflexes
-
Flaccid paralysis and atrophy of the LEs
-
Flaccid bowel and bladder, impotence (may be spared if only lumbar roots are affected)
-
Saddle anesthesia
-
-
Clinical—Conus medullaris:
-
Combination of UMN and LMN depending on level
-
Reflexes may be preserved or hyperactive
-
Spasticity may develop in sacral muscles
-
Bladder may be spastic
-
Saddle anesthesia (loss of pain/temp)
-
-
Prognosis:
-
Conus medullaris recovery is similar to other UMN spinal cord injuries
-
Cauda equina injuries may represent a neuropraxia or axonotmesis, which may demonstrate progressive recovery
-
Early diagnosis and surgical decompression predict better outcome [15]
-
SCI Assessment
-
Referring Physician: Name, hospital, and contact information
-
HPI:
-
Clearly describe the mechanism of initial injury
-
Determine if there was secondary trauma (TBI, fractures, blood loss, respiratory failure, etc.)
-
Document if the patient was wearing a helmet or seatbelt, if applicable
-
What did the patient feel immediately following the injury? Was there immediate loss of sensation and/or motor control, or did it develop progressively?
-
Describe initial treatment course (i.e., intubation, use of steroids, emergent surgical interventions)
-
Detail hospital course to date and any complications (skin breakdown, infection, DVT, significant laboratory or imaging findings)
-
Document details including dates and names of surgeons if procedures performed (spinal stabilization, PEG tube, tracheostomy including type of trach and cuff versus uncuffed, IVC filter placement, and if it is removable)
-
-
Current Issues:
-
Neuro—Subjective sensory and motor deficits
-
Instability—Structural injury to spinal column requiring bracing or surgery for immobilization
-
Pain—may be multiple types of pain. For each one, document location, quality, intensity, radiation, aggravating/alleviating factors. Document medications used for pain and their effectiveness.
-
Bladder—voluntary voiding? incontinence? Sensation of genitals? on intermittent catheterization (IC), or Foley?
-
Bowel—Sensation of rectum or bowel movements? voluntary bowel movements, or on a bowel program? incontinence?
-
Spasticity—location, frequency, severity; causing pain, poor sleep, or interfering with function?
-
Respiratory—comfortable? SOB? DOE? on vent or history of vent? secretion management requirement?
-
Skin breakdown? Document location, stage, whether or not the patient was being turned regularly. Document type of mattress patient was on.
-
Psych—symptoms of adjustment d/o or PTSD, flashbacks to event, nightmares, anxiety, disrupted sleep?
-
Cardiovascular: symptoms of orthostasis (lightheadedness, syncopal episodes) or autonomic dysreflexia (headache, sweats, flushing)
-
Diet—previous issues with dysphagia? Give special consideration if the patient underwent anterior cervical fixation which could cause vagal/recurrent laryngeal nerve damage. PEG tube?
-
-
PMH:
-
Include a Full Past Medical History
-
Any previous congenital or acquired spinal disorder (i.e., spina bifida, spinal stenosis)
-
Any condition which may also limit function or which will need to be managed on the rehab unit (i.e., peripheral neuropathy, DJD, asthma/COPD)
-
-
PSH: Include dates of procedures
-
Medications:
-
List home medications including herbal medicines and supplements.
-
Medications used during previous hospital course.
-
Make sure to list significant medicines (e.g., steroids, antibiotics) even if the patient is no longer taking them by the time of discharge to rehab.
-
-
-
Allergies: List drug and environmental allergies.
-
Social history:
-
Type of housing and barriers to home access (single level house or third floor walk-up, narrow hallways, small bathrooms)
-
With whom does the patient live?
-
Support system (close family or friends)
-
Employment history and education level
-
Hobbies
-
Substance abuse history
-
-
Prior Functional History:
-
Ambulation: Independent or with assisted device?
-
Exercise tolerance and reason for limitation (pain or SOB?)
-
ADLs: Independent or require adaptive equipment or assistance?
-
Did the patient have a home health aide?
-
-
Current (Admission) Level of Function:
-
Function as documented on recent PT and OT notes
-
Note any mobility restrictions/precautions or instructions for brace wear
-
-
ROS: Full review of systems
-
Physical examination: In addition to the standard medical physical examination, the SCI exam should emphasize the following elements:
-
Vitals: Hypoxia, tachypnea, tachy- or bradycardia, hyper- or hypotension
-
Range-of-motion: Active and passive
-
Muscle tone: Passively range a joint at varying speeds and grade by modified ashworth scale (MAS) (Table 2.1) [16]
Table 2.1 Modified ashworth scale (MAS) [16] -
Strength: Test key muscles (Table 2.2) and grade from 0 to 5 (Table 2.3)
Table 2.2 Key muscles (myotomes) Table 2.3 Manual muscle testing (MMT) -
Sensation: Test light touch with cotton swab and pinprick in all dermatomes (Table 2.4), and grade from 0 to 2 (Table 2.5). Also check proprioception.
Table 2.4 Key sensory points (dermatomes) Table 2.5 Sensory grading -
Reflexes: Biceps, Triceps, Patellar, Achilles; Babinski and Hoffmann
-
Skin: Examine for breakdown (scapulae, ischia, sacrum, heels), infection; note tube/catheter/trach sites
-
Rectal: Note voluntary and involuntary sphincter tone and whether stool is in the rectal vault.
-
Functional: Bed mobility (rolling, bridging), supine ® sit ® stand, sitting and standing balance, and ambulation as able
-
-
AISA Examination and Classification:
The ASIA Impairment Scale (AIS) allows for classification of the patient’s injury according to the International Standards for Neurological Classification of Spinal Cord Injury, which facilitates research and communication between caregivers and has prognostic value.
-
Motor level: Most caudal level that is graded 3/5 or greater with all segments cephalad graded normal (5/5) strength
-
Motor index score: Calculated by adding the muscle scores of each key muscle group; a total score of 100 is possible.
-
Sensory level: Most caudal dermatome to have normal sensation for both pin prick and light touch on both sides.
-
Sensory index score: Calculated by adding the scores for each dermatome; a total score of 112 is possible for each pin prick and light touch.
-
Neurologic level of injury: Most caudal level at which both motor and sensory modalities are intact.
-
Complete injury: Absence of sensory and motor function in the lowest sacral segments (AIS A)
-
Incomplete injury: Preservation of motor and/or sensory function below the neurologic level that includes the lowest sacral segments (AIS B, C, D, or E).
-
Skeletal level: Level at which, by radiological examination, the greatest vertebral damage is found.
-
Zone of partial preservation (ZPP): Only applicable in complete injuries, refers to the levels caudal to the neurological level that remain partially innervated. Defined by the most caudal segment with some sensory and/or motor function.
-
Table 2.6 American spinal injury association impairment scale [17]
-
-
SCI Admission Orders
-
Admit to: Inpatient rehabilitation
-
Diagnosis: Type and level of spinal cord injury and etiology
-
Condition: Stable/fair
-
Allergies:
-
Vitals: Q Shift unless unstable (which would need more frequent vitals); include pulse oximetry for patients on ventilators, tracheostomies, or with respiratory impairment
-
Diagnosis: SCI—define by level and AIS classification
-
CV: SCI patients are likely to have new lower baseline BP, often relatively hypotensive (SBP 90-110); therefore prone to symptomatic orthostatic hypotension
-
Compression stockings and abdominal binder OOB to prevent orthostasis
-
Ensure appropriate fluid intake
-
-
Pulm on Ventilator: [18]
-
Note ventilator settings from outside hospital; continue same settings on admission
-
If unclear and there is no parenchymal lung injury, start CMV with tidal volume 10–15 cc/kg ideal body weight (about 1 L), rate 12, PEEP 5, titrate FiO2 for SPO2 to >92%
-
Check ABG
-
Daily Vital Capacity (VC) measurement
-
See below and Respiratory section for further details
-
-
Pulm with Trach:
-
Chest Physiotherapy every 6 h; use insufflator–exufflator with therapy
-
CXR (evaluate for PNA or PTX)
-
Check PFTs: (FEV1, Vital capacity, Negative Inspiratory Force)
-
Albuterol and Ipratropium nebs every 6 h standing and q4 prn
-
Suctioning as needed
-
Tracheostomy care orders - clean site with hydrogen peroxide then wash with NS
-
Speech consultation for Passey-muir valve
-
-
Bladder with Foley: Remove Foley, wait 3 h, insert Foley, check U/A and Cx, and refer to Bladder section for further management
-
Bladder without Foley:
-
Check U/A and Cx
-
Check post-void residuals after each void for first 24 h using straight cath or bladder scan.
-
If volumes <200 cc AND patient is able to control voiding, allow patient to void
-
If volumes >200 cc OR patient is unable to control voiding, place a Foley and refer to Bladder section for further management
-
-
-
Bowel (UMN):
-
Colace 100 mg po TID
-
Senna 2 tabs po 8 h prior to bowel routine, this can be increased if needed to a max daily dose of (6 tabs/day)
-
Bowel routine (digital stimulation) with mini enema or suppository 30 min after a meal
-
If distended or having accidents, consider KUB to assess volume of stool in colon
-
-
Bowel (LMN):
-
Requires manual disimpaction each morning after breakfast
-
If possible, have patient seated in commode chair
-
Bowel meds are adjusted for stool consistency to minimize accidents and allow for easy disimpaction
-
If distended or having accidents, consider KUB to assess volume of stool in colon
-
-
Pain:
-
MSK—Tylenol 650 mg q6h prn mild pain
-
Oxycodone 5–10 mg po prn moderate–severe pain
-
Neuropathic—gabapentin 300 mg tid–qid and/or nortriptyline 25 mg qhs
-
-
Chemical prophylaxis may be contraindicated if recent surgery or hemorrhage
-
Check LE duplex for undiagnosed DVT
-
If negative order sequential pneumatic compression devices (SCD)
-
-
AIS D: Enoxaparin 40 mg SQ daily until D/C from Rehabilitation
-
AIS C: Enoxaparin 40 mg SQ daily for 8 weeks
-
AIS A or B: Enoxaparin 40 mg SQ daily for 8 weeks
-
If complicated (LE fracture, h/o thrombosis, cancer, heart failure, obesity, or age >70), needs to be continued for 12 weeks
-
-
-
Skin:
-
Turn patient q2h while in bed to prevent skin breakdown
-
Multipodis boots to prevent heel/calf skin breakdown and contractures
-
If patient already has skin breakdown:
-
Document (photograph, measure, stage)
-
Initiate wound care plan (See Wound Care subsection)
-
-
Pin care if HALO brace or external fixator present (instructions vary by surgeon)
-
-
Spasticity:
-
Note level of current tone compared to discharge exam from prior hospital setting.
-
Acutely increased tone may indicate undiagnosed infection, fracture, or other pathology
-
Consider imaging, CBC, U/A & Cx, ESR, CRP, Alk Phos
-
-
-
Diet:
-
Omeprazole 40 mg daily (for 2+ weeks post-injury to prevent GI stress ulcers)
-
Tube feeding:
-
Convert calories/formula to 16- or 18-h overnight schedule
-
Increase rate by 10 cc every 8 h to optimal target rate
-
Nutrition consultation to optimize protein
-
-
Oral feeding:
-
Speech and Swallow eval if dysphagia is suspected. Good idea for anyone in a C-collar.
-
Continue prior diet unless aspiration is suspected
-
-
Weigh patient on admission and weekly
-
-
Activity:
-
List precautions and restrictions, weight-bearing status of extremities
-
Brace type(s) and instructions for wearing (at all times vs. OOB only)
-
-
Labs:
-
CBC, BMP, LFTs, PT/PTT, U/A & Cx, TSH, Vit D 25, and 1,25
-
Weekly CBC, and BMP unless otherwise indicated
-
-
Imaging:
-
CXR if pulm or vent history
-
KUB if bowel status unclear
-
X-rays of orthopedic or surgical sites
-
Consider LE duplex for DVT; required prior to pneumatic compression device use if no DVT prophylaxis for 72 h [19].
-
-
Consultations:
-
Speech:
-
Assess for aspiration and determine appropriate diet.
-
Teach glossal-pharyngeal (frog) breathing if ventilator dependent
-
Vocalization while on vent or with trach with speaking valve.
-
-
Nutrition: Optimize nutritional status and determine appropriate diet
-
Social work: Evaluate current living environment and social/financial support available for discharge planning
-
Psychology: Eval and continued therapy for adjustment disorder; Family counseling
-
Recreational and vocational therapy: For community reintegration, identifying outpatient services for returning to work, support groups
-
-
Therapy:
-
Dx: Tetraplegia/paraplegia, medical diagnoses
-
Date of onset
-
Precautions: Mobility restrictions (i.e., Spine precautions, Cervical collar on at all times), cardiac (orthostasis), respiratory (RR 12–20), decreased sensation, Autonomic dysreflexia, skin breakdown, anticoagulation, hypoglycemia, etc
-
Weight-bearing status: WBAT all extremities (unless there are any fractures)
-
Short-term goals: Based on impairments, level of injury, and comorbidities, to be accomplished by discharge
-
Long-term goals: Ideally maximized function based on level of injury and comorbidities
-
-
Physical Therapy Rx:
-
Evaluate
-
A/AA/PROM to LEs with stretching as indicated
-
Tone-reducing techniques
-
Strengthening to LEs
-
Mat activities
-
Transfers
-
Sitting/standing balance
-
Proprioceptive exercises
-
Progressive ambulation with assistive device
-
Stair negotiation as tolerated
-
Home exercise program
-
Trial of TENS, FES
-
Ice ×20 min prn
-
Splinting or bracing as indicated
-
-
Occupational Therapy Rx:
-
Evaluation
-
A/AA/PROM to UEs with stretching as indicated
-
ADL training
-
Fine motor coordination
-
Neuromuscular reeducation
-
Tone-reducing techniques
-
Strengthening to UEs
-
Splinting in neutral position or for tenodesis
-
Functional transfers
-
Work Simplification/Energy Conservation
-
Adaptive device evaluation
-
Durable Medical Equipment (DME) Evaluation
-
Home evaluation to determine accessibility and need for equipment
-
Trial of TENS, FES
-
Ice or MHP ×20 min prn
-
-
Wheelchair Prescription:
-
Power recline and/or tilt-in-space wheelchair with head, chin, or breath control
-
Pressure relief cushion
-
Postural support
-
Safety belt
-
-
Adaptive Devices/Home Equipment that May Be Needed:
-
Full electric hospital bed with side rails and Trendelenburg position
-
Transfer board
-
Power or mechanical “Hoyer” lift with U-sling
-
Shampoo tray
-
Handheld shower
-
Padded reclining roll-in shower or commode chair with safety strap
-
Sequelae and Complications of SCI
Neurological Prognosis
-
Life expectancy:
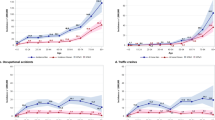
Mortality rates are the highest during the first year after injury [1] (Table 2.7)
Table 2.7 Life expectancy (years) post-injury by severity of injury and age at injury, for those who survive the first 24 h [1] Life expectancy [1]
-
Causes of Death During First Year [21]
-
28% diseases of respiratory system
-
23% Ischemic/hypertensive heart disease
-
9.7% PE
-
7.5% Sepsis
-
-
Functional Outcomes [22, 23](Dep = Dependent, A = Assist, Ind = Independent)
-
C1–C4:
-
-
Respiratory: Complete or partial phrenic nerve paralysis requiring ventilation initially
-
Dep for clearing secretions
-
-
ADLs and Transfers: Dep
-
Pressure reliefs: Ind with tilt-in-space power w/c
-
Mobility: Ind in power w/c with head array or sip and puff
-
-
C5
-
Eating: Mod Ind after setup with adaptive equipment such as wrist splint with utensil holder or universal cuff, bent fork or spoon, nonslip mat, plate guard, and possibly a mobile arm support
-
Grooming: Min A after setup
-
Dressing: A for upper body, Dep for lower body
-
Brushing teeth/grooming: Min A after setup with wrist support and utensil holder
-
Bed mobility and transfers: A
-
Bowel/bladder: Dep
-
Driving: Ind with adaptations
-
-
C6: Highest complete level that can live independently (if motivated)
-
Eating: Ind or Mod Ind
-
Grooming: A to Mod Ind
-
Dressing: Ind for upper body, A for lower body
-
Bathing: A to Mod Ind with wash mitt, handheld shower, U-shaped cuff, lever type faucet, grab bars, and shower chair
-
Bed mobility: A to Ind
-
Transfers: A to Mod Ind with transfer board for transfers on even surfaces. Uneven surfaces may require more assistance
-
Pressure reliefs: Ind with power or manual w/c
-
Bladder:
-
Female: Continuous indwelling Foley most commonly used. May be Mod Ind for self-catheterization with a continent urinary diversion with an abdominal stoma for bladder access.
-
Male: Potentially Mod Ind for intermittent catheterizations
-
-
Bowel:
-
A for transfer and setup on recliner commode
-
Potentially Mod Ind for performance of bowel routine with rectal stimulation using suppository inserter and mirror guidance
-
A for cleanup
-
-
Mobility:
-
Ind driving a van with w/c lift and hand controls from secured wheelchair
-
Ind with power w/c with standard arm controls
-
Potentially Ind with manual w/c indoors with modified hand rims. Power-assist wheels can be useful.
-
-
-
C7: Usual level of injury for functional independence
-
ADLs: A to mod Ind
-
Bed mobility: Min A to Ind
-
Transfers: Mod Ind with transfer board
-
Bladder:
-
Female: Ind with self-catheterization is possible, but technically difficult
-
Male: Mod Ind with intermittent catheterizations.
-
-
Bowel: Mod Ind for performance of bowel routine with rectal stimulation using suppository inserter and mirror guidance
-
Mobility:
-
Ind driving a car or van with hand controls
-
Ind with power w/c
-
Ind with ultra-lightweight manual w/c with modified hand rims, except over curbs and uneven terrain. Power assist wheels can be useful.
-
-
Typing: Min A to Mod Ind (typing splint) for telephone and keyboard use
-
-
T2–T9
-
ADLs: Ind
-
Transfers: Ind for all including floor-to-chair transfers
-
Bowel/bladder: Ind
-
Mobility:
-
Ind with manual w/c including popping a wheelie and curbs
-
Mod Ind Ambulation for exercise with b/l KAFO and forearm crutches or walker
-
-
-
T10–Lumbar:
-
W/C: Ind with manual w/c potentially including ↑/↓ stairs and escalators
-
Ambulation: Mod Ind for ambulation with b/l KAFO and walker or crutches using swing-through gait—high energy expenditure. More for exercise than for functional mobility.
-
Neurologic Complications
-
Syringomyelia (posttraumatic cystic myelopathy)
-
Cyst formation within the gray matter near the level of injury
-
Incidence: 8% starting 2 months after injury [23]
-
Etiology: unclear
-
Hematoma with enzymatic lysis?
-
Scarring with obstruction of CSF flow?
-
-
Clinical:
-
Pain worse with valsalva
-
Ascending loss of reflexes
-
Ascending sensory loss in “cape” distribution
-
Change in spasticity
-
Postural changes
-
-
Workup: MRI with contrast
-
Treatment:
-
Avoid straining for bowel routine/urination
-
Neurosurgical consultation
-
Shunting
-
Cordectomy
-
-
Prognosis: [23]
-
Pain reduction and motor recover > sensory recovery
-
Recurrence rate of ∼50%
-
-
-
Peripheral Nerve Entrapment [3]
-
Carpal tunnel and ulnar neuropathy most common
-
Incidence: CTS 21–65%
-
Treatment:
-
Relative rest
-
Splinting
-
Avoid direct pressure on nerves
-
Modify w/c propulsion and transfer techniques
-
Padded gloves
-
Surgical release/transposition
-
-
See EMG chapter for further details
-
Respiratory [3, 18, 23]
-
Anatomy:
-
Innervation:
-
Phrenic nerve (C3, 4, 5)—diaphragm
-
Vagus nerve—lung parasympathetics
-
-
Inspiratory muscles: diaphragm (65–75% of volume), external intercostals, accessory muscles
-
Expiratory muscles: abdominals, internal intercostals
-
-
Respiratory Changes After SCI:
-
Increased residual volume
-
Decreased vital capacity (VC) and tidal volume (TV)
-
Forced VC may initially be 50% of expected, but may improve to 60% [3]
-
-
Paradoxical chest wall movement
-
Chest wall falls and abdomen protrudes during inspiration
-
-
Diaphragm in biomechanically disadvantaged position
-
Increased secretions from unopposed parasympathetics (Vagus n)
-
-
Impairment by level of injury: [3]
-
C2 or above:
-
No respiratory muscle function (including diaphragm)
-
Requires mechanical ventilation
-
An intact phrenic nerve (EMG) may allow for diaphragmatic pacing
-
-
C3–4:
-
Weak diaphragm, no active expiratory function
-
Initially requires mechanical ventilation, many will wean
-
-
C4–C8:
-
Intact diaphragm, but no active expiratory function
-
Requires assistance for clearing secretion (insufflation–exsufflation, chest PT)
-
Positioning to improve tidal volumes (supine > sitting by 15%)
-
-
T1–T5:
-
No volitional intercostals or abdominal muscle function
-
Requires assistance for clearing secretion (insulflator–exsulflator, chest PT)
-
Positioning to improve tidal volumes (supine > sitting)
-
-
T5–T12:
-
Weak intercostals and abdominals, weak cough
-
Requires assistance for clearing secretion (insulflator–exsulflator, chest PT)
-
-
-
Respiratory Complications: [23]
-
Occur in up to 67% of acute SCI patients
-
Pneumonia
-
Atelectasis
-
Respiratory failure
-
-
Most common in high cervical (C1–C4) injuries
-
Leading cause of death after SCI (21.7%) [24]
-
72.3% due to pneumonia
-
-
Risk increases with age, obesity, h/o asthma, COPD, or smoking
-
Concomitant TBI may affect respiratory drive
-
-
Prevention of Respiratory Complications: [23]
-
Incentive spirometer
-
Monitor VC and pCO2
-
Suctioning
-
Chest PT
-
Cough assist—manual or with insulflator–exsulflator (40 cm H2O)
-
Adequate hydration to thin secretions
-
Teaching glossopharyngeal breathing
-
Abdominal binder (increases VC 16–28% by prepositioning diaphragm)
-
Medication
-
Inhaled bronchodilators (albuterol)
-
Oral mucolytics (guaifenesin, acetylcysteine)
-
Theophylline (decreases spasm, increases surfactant and diaphragmatic contractility)
-
-
-
Initial Workup:
-
ABG
-
Labs, including cardiac enzymes and toxicology
-
CXR
-
EKG
-
Continuous Pulse Ox
-
Pulmonary metrics:
-
Vital capacity (VC)
-
Forced expiratory volume in 1 s (FEV1) or peak cough flow
-
Maximal Negative Inspiratory Force (NIF)
-
-
Calculate Ideal Body Weight (IBW)
-
Males = 50 + 2.3(height in inches –60)
-
Females = 45.5 + 2.3(height in inches –60)
-
-
-
Mechanical Ventilation [18, 23, 24]
-
Indications:
-
Respiratory failure
-
VC <15 cc/kg IBW, or <1L
-
NIF <20 cm H2O
-
pO2 <50
-
pCO2 >50
-
Fatigue
-
-
Intractable atelectasis
-
Recurrent pneumonia related to atelectasis
-
Tracheostomy if expect >5 days on vent
-
-
Mode:
-
Continuous Mandatory Ventilation (CMV, formerly Assist Control) preferred
-
Fixed tidal volume, FiO2, peak flow, and PEEP at set rate
-
Patient may trigger breath, and full tidal volume is delivered
-
Allows patient to speak if cuff partially deflated
-
-
-
Settings:
-
Calculate Tidal Volume (TV) 10–20 cc/kg IBW [3]
-
Increase TV 50–100 cc per day as tolerated to goal volume (>20 cc/kg IBW)
-
High tidal volumes is preferred for treating atelectasis
-
Reduces time to wean in SCI patients [25]
-
Stop increasing TV when
-
Normal SPO2 on room air (21%)
-
No atelectasis
-
-
-
Monitor pressures to avoid barotrauma
-
Peak pressure < 40 cm H2O
-
Plateau pressure < 35 cm H2O
-
-
PEEP = 5 cm H2O
-
May increase to improve pO2 or decrease atelectasis
-
-
Rate = 12
-
FiO2 = 21% (room air) unless underlying lung pathology
-
Peak flow (rate of air delivery) = 60 L/min
-
Sensitivity to trigger breath = −2 cm H2O
-
Do not allow the patient to override the ventilator settings [18]
-
Set alarms
-
High pressure (peak inspiratory pressure + PEEP)
-
Low pressure (usually 10 cm H2O + PEEP)
-
Low exhaled volume (TV—200 cc)
-
-
-
Alternative to traditional ventilator: [26, 27]
-
Noninvasive Intermittent positive pressure ventilation (NIPPV) may be considered for patients with intact bulbar muscles and intact mental status
-
Apparatus similar to CPAP or BiPAP
-
Lower risk of pneumonia than with trach
-
Avoids complications of trach
-
More likely to be discharged home
-
-
-
-
Vent Weaning:
-
Indication: Vital capacity (VC) >10 cc/kg IBW
-
VC of 15–20 cc/kg good predictor of successful weaning [28]
-
Also consider CXR and ability to breathe on room air
-
-
Method: Progressive ventilator-free breathing (PVFB) [3, 24]
-
Start by removing vent for 2–5 min TID
-
Supine position with abdominal binder
-
Increase time off vent as tolerated
-
Provide humidified O2 via trach collar
-
More effective than SIMV in SCI [29]
-
-
Discontinue weaning if:
-
VC drops by 50%
-
Unable to maintain SPO2 >92%
-
RR >30
-
HR >20 above baseline
-
SBP change of 30 points
-
Fatigue or altered mental status
-
-
Noninvasive ventilation may aide weaning [27]
-
Intermittent positive pressure ventilation (IPPV)
-
CPAP, BiPAP
-
Intermittent abdominal pressure ventilator
-
-
Implanted devices: phrenic nerve stimulator, diaphragmatic pacing
-
Require intact phrenic nerve
-
May allow some patients to wean as well as improve speech and mobility
-
Bowel/GI
-
Anatomy/Physiology
-
Parasympathetic—pro-motility
-
Vagus nerve (CN X)—stomach through transverse colon
-
Pelvic splanchnic nerves (S2–4)—transverse colon to internal anal sphincter (IAS)
-
-
Sympathetic—stasis
-
Celiac and Superior Mesenteric Ganglia (T4–12)—stomach through transverse colon
-
Inferior Mesenteric Ganglion (L1–3)—transverse and descending colon
-
-
Somatic—External anal sphincter
-
Pudendal nerve (S2–4) motor and sensory to external anal sphincter (EAS)
-
-
Reflexes
-
Gastrocolic
-
Trigger: Stomach/duodenal distention
-
Opens iliocecal valve
-
Increases colonic peristalsis
-
Timeframe: 15–60 min after meal
-
Mediated by cholecystokinin, serotonin, gastrin
-
-
Rectocolic and Recto-anal inhibition
-
Trigger: Rectal distention/stimulation
-
IAS relaxation and peristalsis
-
Mediated by pelvic nerve
-
Manual stretching/relaxation of EAS to allow stool evacuation
-
-
-
-
Acute SCI
-
Atonic bowel/ileus
-
May last up to 7 days [3]
-
-
Treatment:
-
NG tube to intermittent suction for decompression if vomiting or severe nausea
-
IVF if unable to tolerate fluids
-
TPN if >3 days
-
PPI or H2-blocker (unopposed vagal tone increases acid production)
-
Abdominal massage, TENS
-
May consider trial of metoclopramide 10 mg tid and/or erythromycin
-
-
-
Chronic SCI
-
UMN Bowel (injury above conus medullaris)
-
UMN Bowel (injury above conus medullaris)
-
EAS cannot be voluntarily relaxed, may be spastic
-
Intrinsic reflexes intact and may be hyperactive
-
May have spontaneous BMs (accidents)
-
-
LMN Bowel (injury at or below conus medullaris)
-
-
LMN Bowel (injury at or below conus medullaris)
-
EAS and colon flaccid
-
Intrinsic reflexes absent
-
Colonic dilation and storing of stool
-
-
-
Bowel Program Guidelines:
-
Goal: to have planned, regular bowel evacuations to prevent complications such as constipation, diarrhea, pain, or unplanned bowel movements.
-
Can be done in bed, but preferably, the patient should be sitting upright either in a padded commode chair or recliner commode
-
Should be performed the same time every day
-
Frequency and dosing of laxatives should coincide with established bowel routine
-
During inpatient stay, bowel routine should be performed daily. It may change to an every other day as outpatient if the patient desires.
-
-
UMN Program
-
Take advantage of reflexes
-
Perform 1 h after a meal
-
Use PR medication (suppository or mini-enema) ± digital stimulation with lidocaine 2% jelly
-
Gently insert a gloved, lubricated finger into the rectum and slowly rotate the finger in a circular movement.
-
If tone persists, hold gentle pressure toward sacrum
-
Rotation is continued until relaxation of the bowel wall is felt, flatus passes, stool passes, or the internal sphincter contracts.
-
Digital stimulation is repeated every 5–10 min as necessary until stool evacuation is complete.
-
-
Medications: 3-2-1
-
Docusate 100 mg po tid
-
Senna 2–4 tabs 8 h prior to bowel routine
-
1 enema or suppository to initiate program
-
-
-
LMN Program
-
Manual stool evacuation required—no reflexes to assist removal of stool
-
Perform prior to bathing each morning to prevent accidents during day
-
Insert one or two lubricated fingers into the rectum to break up or hook and remove stool.
-
Performing on commode for gravity and valsalva assistance
-
-
Bulk stool for easy removal and to prevent accidents (psyllium, methylcellulose)
-
Perform 15–30 min after meal to take advantage of gastro-colic reflex
-
-
Bowel Medications
-
Bulking Agents
-
Allow stool to retain more water and produce gel to ease passage
-
Onset of action: 12–72 h
-
Examples:
-
Psyllium (Metamucil)—1 Tablespoon daily—TID
-
Methylcellulose (Citrucel)—1 Tablespoon daily—TID
-
Dietary fiber—At least 15 g/day
-
-
-
Osmotics
-
Poorly absorbed polyvalent ions (Mag, Phos, Sulfate)
-
Increase intestinal H2O and stimulate cholecystokinin
-
Site of action: All, mostly small bowel
-
Onset: ½–6 h
-
Fleet’s (sodium phosphate)—reduces K+, may cause renal failure
-
Mag citrate—300 mL = ∼2 g elemental mag
-
Mag hydroxide (MoM)
-
Mag sulfate (Epsom salt)—most potent
-
Mannitol (>20 g po)
-
-
-
Hyperosmotics
-
Poorly absorbed carbohydrates or polymers
-
Induce osmotic diarrhea—increased volume stimulates peristalsis
-
Site of action: Colon
-
Onset: ½–24 h
-
Glycerin supp—draws H2O into rectum, stretching it to stim reflex
-
Includes sodium stearate which irritates rectum
-
-
Miralax (polyethylene glycol)
-
-
Avoid Lactulose and Sorbitol in SCI patients, as bacterial breakdown of these sugars can cause uncomfortable bloating
-
-
Stimulants (PO)
-
Irritate bowel wall or stimulate plexus
-
May also alter electrolyte secretion
-
Site of action: Colon
-
Onset: 6–10 h
-
Bisacodyl (Dulcolax)
-
Cascara
-
Casanthranol (anthraquinone stimulant, hydrolyzed by colonic bacteria)
-
Senna (Senokot)—stimulates Auerbach’s plexus - peristalsis
-
Complications: Melanosis coli (brownish discoloration of colon), Cathartic colon (atonic, redundant colon; associated w/use >3×/week for >1 year.)
-
-
Aloin—an aloe derivative
-
Aloe and Rhubarb—converted by colonic bacteria into active agent.
-
-
Site of action: Small intestine
-
Onset: 2–6 h
-
Castor Oil—converted to ricinoleic acid
-
-
-
Stimulants (PR)
-
Onset: ¼–1 h
-
Bisacodyl supp (in mineral oil)
-
Microlax 5 cc enema (contains sodium citrate, sodium lauryl sulfoacetate, sorbitol, glycerol, sorbic acid, and H2O)
-
Glycerin supp
-
-
Onset: 5–20 min
-
Bisacodyl enema (1.25 fl oz, 10 mg)
-
Magic Bullet supp (dulcolax in water base)
-
Docusate mini enema (Enemeez)
-
-
-
Enemas
-
Large Volume (500–1,500 cc)
-
Soap Suds = Sodium lauryl sulfate
-
H2O
-
SMOG (Saline, Mineral Oil, Glyercin)
-
-
Standard
-
Fleet’s (sodium phosphate), 133 cc—Avoid in renal failure
-
Mineral oil, 133 cc
-
Glycerin, 8 oz (or mix with H2O for large volume)
-
-
Mini/Micro
-
Docusate +/− Benzocaine (Enemeez)
-
Bisacodyl 10 mg, 1.25 oz (Dulcolax)
-
Microlax 5 cc
-
(Table 2.8) Bowel Medications
Table 2.8 Bowel medications -
Bladder
-
Normal Bladder Anatomy/Physiology:
-
Storage (Sympathetic)
-
Sympathetic (hypogastric nerve T11–L2)
-
Detrusor relaxation (β3-adrenergic)
-
Internal sphincter contraction (α1-adrenergic)
-
-
Somatic (pudendal nerve, S2–4)
-
External sphincter contraction
-
-
Parasympathetic (Pelvic splanchnic nerve, S2–4) motor fibers are inactive, sensory afferent fibers track detrusor stretching
-
Cerebral cortex inhibits the pontine micturition center
-
-
Voiding (Parasympathetic)
-
Full bladder (>150 cc) activates parasympathetic sensory afferents
-
Pontine micturition center coordinates detrusor contraction and sphincter relaxation.
-
Parasympathetic (Pelvic splanchnic nerve, S2–4)
-
Detrusor contraction (cholinergic)
-
-
Sympathetic (hypogastric nerve, T11–L2) motor fibers are inactive
-
Internal sphincter relaxation
-
-
Somatic (pudendal nerve, S2–4)
-
External sphincter relaxation
-
-
-
-
Neurogenic Bladder After SCI
-
Anatomy:
-
Lack of continuity between the sacral nerves and the pontine micturition center results in detrusor-sphincter dyssynergia (DSD), or inability to coordinate contraction/relaxation of the detrusor and sphincter for voiding
-
UMN lesions → spastic bladder, with preservation of sacral reflexes and higher voiding pressures due to DSD.
-
Bladder pressure >40 mmHg may cause hydronephrosis and eventual kidney failure
-
-
LMN lesions (At or below S2) → flaccid bladder, with loss of sacral reflexes
-
-
Clinical: UMN and LMN may present as retention or incontinence
-
Retention may result from:
-
Atonic detrusor (LMN bladder or acute SCI)
-
Sphincter contraction (persistent sympathetic tone, dyssynergia)
-
Other outlet obstruction (urethral stricture, prostate)
-
-
Incontinence may result from:
-
Atonic detrusor with overflow (high volumes)
-
Detrusor Spasticity (low volumes)
-
Preexisting pelvic floor insufficiency
-
-
-
Treatment:
-
The goal in bladder management is to maintaining low bladder pressures and continence while minimizing infections and the risk of upper tract deterioration [30]
-
Initial: Indwelling Foley until spinal shock resolved and orthostasis controlled
-
Trial of void (remove Foley—typically do this early in the AM for convenience)
-
Void with control
-
Check post-void residual (PVR)
-
If <200 cc, acute management complete
-
If >200 cc, may have DSD (UMN) or weak detrusor (LMN)
Intermittent catheterization (IC) prn PVR >200
If UMN, trial of tamsulosin 0.4 mg po qhs to relax sphincter
If LMN, trial of bethanechol 10 mg po tid to facilitate detrusor contraction, may titrate up to 100 mg qid
Consider urodynamic study if no improvement
-
-
-
Spontaneous voiding (reflex voiding without control):
-
Check PVR
-
If <200 cc, may use condom catheter or diaper
-
If >200 cc, will require IC q6h or indwelling catheter
If UMN, trial of tamsulosin 0.4 mg po qhs to relax sphincter
If LMN, trial of bethanechol 10 mg po tid to facilitate detrusor contraction, may titrate up to 100 mg qid
-
-
May decrease spontaneous voiding, but monitor PVRs:
-
Anticholinergics to relax detrusor
Oxybutynin 5 mg po tid, titrate up to 15 mg
Tolterodine 2 mg bid
-
Adrenergics to increase sphincter tone (if on IC)
Pseudoephedrine 30–60mg bid (max 120mg/day)
-
Spasticity management (baclofen, tizanidine)
-
Botulinum toxin injected into the detrusor
-
-
May reduce voiding pressures:
-
Tamsulosin 0.4 mg po qhs to relax sphincter
-
Botulinum toxin injected into urinary sphincter
-
Transurethral sphincterotomy
-
-
Urodynamic study recommended to check voiding pressures [30]
-
-
No voiding after 8 h:
-
Check bladder volume (bladder scan or IC)
-
If <200 cc, hydrate and recheck
-
If >200 cc, start IC q6h
For LMN, trial of bethanecol 10 mg po tid, may titrate up to 100 mg qid
For UMN, trial of tamsulosin 0.4 mg po qhs + anticholinergic (oxybutynin, tolterodine)
-
-
-
-
Catheterization programs
-
Goal: Maintain empty bladder to prevent hydronephrosis, UTI, and incontinence
-
Methods:
-
Intermittent catheterization (IC)
-
Start q6h and adjust frequency to maintain volumes 400–500 cc
-
May help train/strengthen bladder
-
Start patient training ASAP
-
Complications: UTI if poor technique
-
Not recommended for patients with high urine output, AD, strictures, bladder capacity <200 cc, or who are unable to catheterize themselves and do not have a willing caregiver [30].
-
-
Indwelling urethral catheter
-
Appropriate for patients unable to perform self-IC or with high urine output
-
Complications: UTI, urethral erosion, stricture, bladder cancer, bladder/kidney stones
-
-
Suprapubic tube
-
Nongenital placement of indwelling catheter
-
Appropriate for patients with urethral abnormalities, recurrent obstruction, AD, skin breakdown
-
Complications: UTI, bladder cancer, bladder/kidney stones
-
-
Urinary diversion (i.e., Mitrofanoff)
-
Surgical procedure for a continent suprapubic conduit
-
May allow some patients to become independent with an IC program
-
May be performed with bladder augmentation
-
-
-
-
-
Workup: Urodynamic study helps to clarify voiding pattern by looking at:
-
Sphincter and intravesicular (bladder) pressures
-
Bladder emptying
-
Timing, coordination, and strength of detrusor and sphincter contractions
-
-
Chronic SCI bladder management:
-
Renal U/S yearly to check for hydronephrosis
-
BMP checking renal function yearly
-
Cystoscopy every 10 years if indwelling catheter to evaluate for bladder cancer
-
-
-
Urinary Tract Infection (UTI):
-
Antibiotics only indicated for symptomatic bacteriuria or exacerbation of chronic UTI [31, 32]
-
Urinalysis with
-
Bacteria (≥102 cfu/mL for IC, ≥104 cfu/mL for clean catch, or any amount with indwelling foley) [33]
-
0–5 Squamous epithelial cells (marker for contamination)
-
-
Pyuria
-
Symptoms
-
Fever, dysuria, change in voiding, AD, increased spasticity
-
-
Treatment course: [31]
-
Chronic SCI without fever—5 days
-
Acute SCI without fever—7 days
-
SCI with fever—14+ days
-
-
Antibiotic prophylaxis does not prevent UTI [31]
-
-
(Table 2.9) Bladder Medications
Table 2.9 Bladder medications
Spasticity
-
-
Tone: muscle resistance to passive stretch across a joint
-
Spasticity: velocity-dependent increase in tone due to hyperactive stretch reflex (UMN)
-
Rigidity: non-velocity-dependent increase in tone (basal ganglia)
-
-
Treatment Objectives:
-
Not all tone should be treated
-
Lower extremity tone, for example, may facilitate standing transfers or ambulation without the need for bracing
-
-
Indications/Goals of treatment:
-
Improve function: mobility, balance, ADLs, positioning, hygiene
-
Decrease pain
-
Prevent contractures
-
Allow for uninterrupted sleep
-
-
Rule out pathological causes of increased spasticity
-
Infection, pain, constipation, urinary retention, skin breakdown, HO
-
-
Treatment varies by severity, location (generalized vs. focal), age, compliance, and comorbidities.
-
Focal treatments for focal spasticity (i.e., botulinum, TENS, orthoses)
-
Multiple muscles in multiple limbs, consider po medication ± focal treatments
-
-
-
Treatment—Therapy:
-
Correct positioning, splinting, casting, tone-reducing orthoses
-
Stretching, ROM exercises
-
Modalities (TENS, FES)
-
-
Treatment—Oral Medication (See Table 2.10):
-
Baclofen—GABAB agonist, pre- and post-synaptic
-
Start 10 mg po tid and titrate by 10 mg as needed, max 80 mg/day (theoretical)
-
Side effects: sedation, seizure risk with sudden discontinuation
-
-
Tizanidine—α2 agonist, inhibits spinal interneurons
-
Start 2 mg tid–qid and titrate by 2 mg as needed, max 36 mg/day
-
Side effects: sedation, dry mouth, orthostatic hypotension, elevated LFTs
-
-
Clonidine—α2 agonist
-
Use limited due to hypotensive effects, but may be used intrathecally in combination with baclofen for spasticity and pain
-
-
Dantrolene sodium—blocks Ca2+ release from sarcoplasmic reticulum
-
Start 25 mg daily and titrate to 3–4 times a day as needed every 4–7 days, max 400 mg/day
-
Preferred for lack of cognitive and sedative side effects
-
Side effects: Possible liver toxicity—Need to monitor LFTs frequently
-
-
Benzodiazepines—GABAA agonists
-
Start clonazepam 0.5 mg po tid or qhs. May increase to 1 mg tid
-
Alternative is Valium 2–5 mg po qhs, may increase to 10 mg
-
Helpful for painful nocturnal spasms
-
Side effects: tachyphylaxis, drowsiness, confusion
-
-
Treatment—Interventional:
-
Chemical neurolysis with phenol or alcohol
-
Lasts 6–9 months, inexpensive
-
Side effects: dysesthesias, weakness
-
-
Botulinum toxin type A and type B
-
For spasticity in selected muscles
-
Onset 2–3 days, peak 2–3 weeks, duration of effect 3 months
-
May improve ambulation, positioning, and hygiene, and reduce pain [34]
-
Side effects: dysphagia, dyspnea, weakness, fatigue
-
-
Intrathecal Baclofen Pump (ITB)
-
Consider for patients with ADL-limiting spasticity uncontrolled on oral medications (less sedating), including those with hemi-spasticity
-
Less effective for upper extremities
-
Side effects: infection, pump may fail, risk of withdrawal seizures
-
-
Spinal Cord Stimulator (SCS)
-
May improve motor control, but evidence is mixed; no recent studies
-
Side effects: infection, spinal cord injury (Table 2.10)
Table 2.10 Spasticity medications
-
Autonomic Dysreflexia (AD) [35]
Reflex sympathetic response to a noxious stimulus below the level of injury
-
Associated with injuries at or above T6
-
Considered a medical emergency
-
Does not occur until out of spinal shock (first week); subsequently, patients remain at lifelong risk.
Pathophysiology:
-
Noxious stimuli below the level of injury trigger a sympathetic reflex within the spinal cord
-
Catecholamines are released, resulting in vasoconstriction
-
The significance of the T6 level is that the sympathetic supply to the splanchnic vasculature originates from T6–L2.
-
Splanchnic vasoconstriction significantly decreases intravascular volume
-
Due to the SCI, the brain cannot inhibit the sympathetic outflow to the splanchnic circulation
-
-
Combined with the LE vasoconstriction, systemic blood pressure rises
-
The carotid baroreceptors trigger adjustment for hypertension
-
Increased vagal tone → bradycardia, vasodilation above level
-
Descending spinal inhibition of sympathetic outflow (blocked)
Clinical:
-
Systolic Blood Pressure >20 mmHg above baseline (>15 in kids)
-
Anxiety
-
Headache (HA)
-
Blurred vision
-
Nasal congestion
-
Sweating/flushing/piloerection above level
-
Bradycardia
Workup and Treatment:
-
1.
Check blood pressure (BP) and pulse initially and after each adjustment
-
2.
Elevate head/sit patient up to decrease intracranial pressure
-
3.
Loosen restrictive clothing, remove socks, braces, or supports
-
4.
Evaluate for bladder distension/tenderness
-
(a)
For indwelling catheter, ensure it is draining properly
-
If blockage is suspected, irrigate with 10–15 mL of normal saline
-
If the catheter does not start to properly drain after irrigation, then replace with new catheter
-
-
(b)
If no catheter, straight cath with lidocaine jelly
-
If output >200 cc, start IC program (see Sect. 5.5)
-
Collect U/A and culture
-
-
(c)
If no other cause is found, may consider flushing bladder with 5–10 cc lidocaine 1%
-
(a)
-
5.
If SBP >150 or if HA, apply 1″ nitropaste to forehead
-
6.
Check rectum for fecal impaction.(Use lidocaine jelly to prevent additional noxious stimulus)
-
7.
Examine skin for breakdown and note BP response to position changes
-
8.
If cause cannot be immediately identified, treat the pain triggering AD and continue workup with close monitoring of BP
-
(a)
Oxycodone 5 mg PO, or Morphine 4 mg IV
-
(a)
-
9.
If BP continues to rise, treat with 2 in. of Nitropaste (can be wiped off if BP drops too much as AD resolves). This is usually applied to the forehead to ensure it is removed at appropriate time
-
10.
If BP still continues to rise, use Nifedipine 10 mg capsule. Have patient bite capsule to speed effect. Be prepared for possible hypotension when cause of AD is found and is resolved.
-
-
Other Potential Causes of AD to Consider:
-
Fracture, HO, DVT/PE, Infection
-
GU: Bladder distention, kidney/bladder stone, blocked catheter, UTI
-
GI: Appendicitis, impaction, gallstones, ulcers, hemorrhoids
-
Skin: Constrictive clothing, burns, blisters, pressure ulcers, ingrown toenail, cuts
-
Reproductive system: sexual intercourse, infection
-
Males: Ejaculation, epididymitis, scrotal compression
-
Females: Menstruation, pregnancy, vaginitis, ovarian torsion, fibroids
-
-
-
Preeclampsia Versus AD:
-
Preeclampsia never occurs before 24 weeks gestation
-
Triad of HTN, Proteinuria, Edema
-
-
AD may occur during labor. Resolves with epidural anesthesia
-
-
Pediatric population—threshold for pharmacologic intervention: [35]
-
<5 years old: SBP >120
-
5–12 years old: SBP >130
-
>13 years old: SBP >140
-
Heterotopic Ossification (HO)
Formation of mature lamellar bone in soft tissue
-
-
Incidence: 10–78% in SCI
-
Generally diagnosed 1–4 months post-injury, but can occur later
-
Peak incidence at 2 months
-
-
Risk Factors:
-
Complete > Incomplete (RR 2.0 ± 4.2) [37]
-
Prolonged coma (> 2 weeks)
-
Immobility
-
Spasticity (in the involved extremity)
-
Associated long-bone fracture
-
Pressure ulcers
-
Younger age
-
-
Clinical:
-
Complications:
-
Skin breakdown
-
Nerve entrapment
-
Loss of function
-
-
Workup:
-
Laboratory Studies
-
Serum Alkaline Phosphatase (SAP) [38, 39]
-
May be elevated 7 weeks before the first clinical signs become apparent (but often elevated postoperatively without HO as well)
-
Peak levels occur 3 weeks after the appearance of clinical signs
-
Poor specificity (elevated with fractures)
-
-
CPK
-
Erythrocyte sedimentation rate (ESR)
-
Early inflammatory marker, nonspecific
-
-
-
Plain X-rays
-
Only soft tissue edema seen early on
-
Need 2–3 weeks for bone maturation to be visible on X-ray
-
-
Three phase 99m Technetium Bone Scan
-
-
Treatment: [3]
-
Bisphosphonates
-
Inhibits osteoclastic activity but does not reverse or dissolve bone
-
If CPK elevated
-
Etidronate 20 mg/kg/day divided in 2 doses ×6 months
-
-
If CPK normal
-
Etidronate 20 mg/kg/day divided in 2 doses ×3 months, then
-
10 mg/kg/day ×3 months
-
-
-
NSAIDs
-
Consider for inflammation if CRP >8 or CPK elevated
-
Indomethacin 25 mg tid ×2 weeks or until CRP <2 or CPK normal
-
-
Therapy
-
Once acute inflammatory signs have subsided, gentle PROM is indicated to help maintain functional range
-
Avoid aggressive PROM as microtrauma may lead to further HO [40]
-
-
Radiation therapy
-
Surgery—Wedge resection
-
Must have clear goal: hygiene, positioning, ADLs, pain
-
Performed after 12–18 months to allow full bony maturation
-
-
Pressure Ulcers and Wound Care
Lesions resulting from unrelieved pressure which damages underlying tissue [41]
-
-
Prolonged or excessive tissue deformation (compression >70 mmHg, shear or tension) including possible ischemic distortion of the vasculature
-
Muscle tissue is more sensitive than skin to pressure-induced ischemia
-
Pressure ulcers develop in deep structures then progress superficially
-
-
-
24% of Model Systems SCI patients developed at least one pressure ulcer during acute care or rehabilitation
-
15% had a pressure ulcer at their first annual examination, 20% at year 5, 23% at year 10
-
Incidence in cervical complete > thoracic complete > incomplete
-
Most frequent secondary medical complication of SCI in Model Systems [45]
-
Second most common reason for rehospitalization in chronic SCI
-
-
Level and severity of the injury, violent injury, mobility status, gender, ethnicity, marital status, employment status, level of education, tobacco or alcohol use, prior pressure ulcer, nutritional status, anemia, incontinence, muscle atrophy, vascular insufficiency
-
Prevention: [47]
-
Begin pressure relief techniques ASAP
-
Avoid prolonged immobilization
-
Daily visual and tactile skin inspection
-
Turn or reposition patients every 2 h in bed
-
Eliminate stretching and folding of soft tissues and prevent shearing when individuals are repositioned.
-
Avoid side-lying directly on the trochanter.
-
-
Prescribe pressure-relief regimen for w/c use (power or manual)
-
Weight shift every 15 min, reposition every hour [41]
-
-
Apply pressure-reducing support surfaces preventively to protect soft tissues from injury
-
The support surface–skin interface should stay cool and dry
-
Use pillows or cushions to bridge contacting tissues and unload bony prominences (increase weight-bearing surface)
-
Avoid donut-type devices
-
Pressure mapping can help determine the best seating system and ensure pressure reliefs are effective [3]
-
-
Therapy program should include muscle strengthening and cardio to prevent deconditioning
-
Nutritional optimization and smoking cessation [3]
-
Educate patient, family, and aide on ulcer prevention and treatment including skin examination
-
-
Clinical [3]
-
Breakdown occurs over bony prominences
-
Seated: ischial tuberoscity, trochanters, elbows
-
Supine: Sacrum, heels, scapulae, occiput
-
-
Daily physical exam should screen for early signs of potential breakdown
-
Check skin temperature (warmth or coolness)
-
Tissue consistency (firm or boggy feeling)
-
Sensation (pain, itching)
-
-
-
Complications [3]
Infection (cellulitis, osteomyelitis), pain, increased spasticity, AD, adjustment d/o
-
Staging of Pressure Ulcers [48]
-
Suspected Deep Tissue Injury:
-
Purple or maroon discoloration of intact skin or blood-filled blister due to underlying tissue damage
-
-
Stage I
-
Non-blanching erythema of intact skin
-
-
Stage II
-
Partial thickness loss of dermis with pink wound bed, no slough
-
May also be intact or ruptured blister
-
-
Stage III
-
Full thickness loss of dermis with exposed adipose.
-
Slough may be present but should not prevent depth assessment
-
Undermining and sinus tracts may be present
-
-
Stage IV
-
Full thickness loss with exposed bone, muscle, or fascia
-
Slough or eschar may be present but not cover wound bed
-
Undermining and sinus tracts may be present
-
-
Unstageable
-
Full thickness loss with depth assessment obscured by slough or eschar
-
-
-
Wound exam: [47]
-
Location and appearance
-
Size (length, width, and depth)
-
Stage
-
Exudate
-
Odor
-
Necrosis
Undermining/Tunneling/Sinus tracts
Healing (granulation, vascular supply, epithelialization)
-
Margins and surrounding tissue integrity
-
Maceration (white discoloration and bogginess)
-
-
-
Treatment [47]
-
Stage I
-
Monitor nutrition
-
Ensure turns q2h
-
Barrier films or lotions
-
-
Stage II
-
Hydrocolloid gel (bid) or film dressing (leave on until it falls off)
-
-
Stage III and IV
-
Surgical consultation
-
Debridement of eschar, necrotic tissue, and slough (unless on heel)
-
Sharp with scalpel—stop when reach intact capillaries
-
Enzymatic—collagenase bid
-
-
Cleanse at each dressing change with NS or wound cleanser
-
Irrigate with a pressure of 4–15 psi to reduce bacterial load [49]
-
-
Consider negative pressure therapy
-
Electrical stimulation
-
Maintain moist ulcer bed
-
Barrier cream to surrounding intact skin to prevent maceration and dressing to keep it dry
-
Check testosterone levels (men)
-
Men—testosterone 200 mg IM q2 weeks
-
Women—testosterone 50 mg IM q2 weeks
-
Follow serum levels 1 week after administration
-
-
Medical Complications
Orthostatic Hypotension
-
Definition: [57]
-
Decrease in systolic blood pressure (SBP) by at least 20 mmHg, OR
-
Decrease in diastolic blood pressure (DBP) by at least 10 mmHg
-
Within 3 min of standing or being raised greater than 60° on a tilt table.
-
-
Clinical:
-
Lightheadedness, blurry vision, nausea, dizziness, ringing of the ears, fatigue, palpitations, pallor, and syncope
-
Found to limit 43% of therapy sessions in one study, with tetraplegic patients most affected [58]
-
-
Pathophysiology: [59]
-
Carotid baroreceptors sense drop in BP, but due to the SCI, the signal cannot reach the sympathetic system (T1–L2) and trigger vasoconstriction
-
Other factors:
-
Decreased plasma volume associated with prolonged supine position
-
Malnutrition/hypoalbuminemia
-
Cardiovascular deconditioning
-
Motor deficits leading to loss of skeletal muscle pumping activity
-
-
-
Treatment:
-
Compression stockings and abdominal binder prior to sitting up
-
Adequate hydration and nutrition
-
Medication (if non-pharmacological methods insufficient):
-
NaCl tablets 1 g po BID-QID
-
Monitor BMP
-
Contraindicated in CHF
-
-
Midodrine 2.5–10 mg po TID
-
α1 adrenergic agonist → vasoconstriction
-
Side effects: hypertension, urinary retention, headache, paresthesias
-
-
Fludrocortisone 0.1 mg daily
-
Aldosterone analog → Na+ retention, K+ excretion
-
Side effects: Hypertension, CHF exacerbation, dizziness, headache, weakness
-
-
-
Venous Thromboembolic Disease
Including Deep Vein Thrombosis (DVT) and Pulmonary Embolism (PE)
-
Risk Factors: [23]
-
Virchow’s triad: [61]
-
Venous stasis
-
Vessel–wall (endothelial) damage
-
Hypercoagulable state
-
-
Prior DVT
-
Medical comorbidities: vascular disease, DM, cancer, obesity
-
Older age
-
-
DVT Prophylaxis: [19]
-
Sequential compression device (SCD) for first 2 weeks after injury
-
Lower extremity ultrasound if thromboprophylaxis delayed >72 h post-injury
-
-
Consider IVC filter [62–64] if
-
Anticoagulant prophylaxis failed
-
Unable to anticoagulate (high risk of bleeding)
-
Anticoagulant prophylaxis still required once cleared
-
-
-
Anticoagulant should be started within 72 h if not contraindicated
-
AIS D: Enoxaparin 40 mg SQ daily until D/C from Rehabilitation
-
AIS C: Enoxaparin 40 mg SQ daily for up to 8 weeks
-
AIS A or B: Enoxaparin 40 mg SQ daily for at least 8 weeks
-
If complicated (LE fracture, h/o thrombosis, cancer, heart failure, obesity or age >70), needs to be continued for 12 weeks
-
-
-
Start PROM, mobilization ASAP
-
-
Clinical—DVT:
-
Clinical—PE:
-
Clinical signs and symptoms may be absent
-
Dyspnea/desaturation, easy fatigability, tachycardia, EKG changes, flash pulmonary edema, chest pain, or hypoxic seizure
-
Sudden death
-
-
Workup:
-
Imaging
-
Venogram is gold standard [23]
-
Venous doppler
-
CT Angiogram (chest) + venogram (legs)
-
Ventilation/Perfusion (V/Q) scan if unable to have CTA
-
-
ABG—↓PO2
-
-
S1Q3T3—Prominent S in I, Q and inverted T in III
-
Right axis deviation
-
Right bundle branch block
-
ST elevation in VI and aVR
-
Tachycardia or AFib/flutter (Tachycardia may be only sign of PE in otherwise asymptomatic patient. Keep PE high on your list if other causes ruled out).
-
-
-
Treatment:
-
Supplemental O2, titrate SPO2 >92%
-
Medical consultation
-
Hold PROM, mobilization for 48–72 h until anticoagulated [19]
-
Kirschblum et al. recommend 5–10 days of AC prior to mobilization [23]
-
-
Discontinue pneumatic compression device
-
IVC filter when anticoagulation is contraindicated
-
Must start AC as soon as possible, even after filter placement [62]
-
Immediate-acting anticoagulant + warfarin, if not contraindicated
-
Heparin gtt (discuss goal with medicine and neurosurgery)
-
or LMWH, i.e., enoxaparin 1mg/kg q12h
-
-
Warfarin start 5 mg po daily, goal INR of 2–3
-
Treat for 6 months for proximal DVT
-
-
Hypercalcemia
-
Epidemiology: [23]
-
10–23% of patients with SCI
-
More common in tetraplegia than paraplegia
-
Peaks between 1 and 4 months post injury [67]
-
More common in young men
-
-
Pathophysiology: [68]
-
Loss of mechanical loading of the bone → increase in bone resorption
-
In an acute SCI, loss of renal tubular reabsorption → decreased calcium excretion
-
-
Clinical:
-
Constipation
-
Abdominal pain
-
Myalgia, arthralgia
-
Lethargy and fatigue
-
Confusion/psychosis
-
Nausea/vomiting
-
-
Workup: [69]
-
Serum calcium level (normal range 8.5–10.5 mg/dL)
-
Correct for albumin concentration [2]
-
Corrected Calcium = 0.8× (normal albumin—patient’s albumin) + patient’s serum calcium
-
-
-
-
Calcium level <12 mg/dL—immediate treatment not necessary
-
0.9NS IV for adequate hydration (promote urinary excretion)
-
Avoid thiazides, lithium, and vitamin C
-
-
Calcium 12–14 mg/dL
-
If chronic without symptoms, treat like mild hypercalcemia
-
If acute or with, then treat as severe hypercalcemia
-
-
Calcium >14 mg/dL
-
0.9NS IV @ 200–300 cc/h (decrease for CHF, etc.)
-
Place Foley
-
Urine output goal 100–150 cc/h
-
Add loop diuretic for edema
-
Stop when euvolemic
-
-
-
Pamidronate 60 mg IV over 4 h or 90 mg over 24 h
-
Inhibits osteoclast activity
-
Lowers Ca2+ over 3 days, nadir at 7
-
Side effects: Jaw osteonecrosis, fever, nausea, headache, myalgia, anemia
-
-
-
Calcitonin 4 IU/kg IV or SQ q12h
-
May increase up to 6–8 IU/kg q6h
-
Increases renal excretion of Ca2+, decreases bone resorption
-
May lower serum Ca2+ up to 1–2 mg/dL within 4–6 h
-
Peak effect within the first 48 h Nasal application not effective for hypercalcemia
-
-
-
Vitamin D Deficiency
-
Epidemiology
-
Pathophysiology:
-
Workup:
-
Serum 25-hydroxyvitamin D (D2) and Ca2+
-
Normal >30 ng/mL [72]
-
-
-
Treatment:
-
Ergocalciferol (D2) or cholecalciferol (D3) [73]
-
50,000 IU po weekly ×6–8 weeks, then
-
800–1,000 IU po daily
-
-
Testosterone Deficiency (Hypogonadism)
-
Epidemiology:
-
Risk Factors:
-
Pathophysiology:
-
Clinical:
-
Muscle wasting
-
Erectile dysfunction
-
Decreased sex drive
-
Fatigue
-
Depression
-
Increased cholesterol and lipid levels
-
-
Workup:
-
1.
AM serum total testosterone level
-
Normal >325 ng/dL [75]
-
-
2.
Serum FSH, LH and prolactin
-
In primary hypogonadism: ↑FSH, ↑LH, normal prolactin
-
In secondary hypogonadism: ↓FSH, ↓LH, possible ↑prolactin
-
-
1.
-
Treatment:
Sexuality [80]
-
Men
-
Reflexogenic Erections
-
Stimulation of somatic afferent fibers (pudendal nerve, S2–4)
-
Efferent parasympathetic fibers (pelvic nerve, S2–4) trigger NO release
-
-
Psychogenic Erections
-
Cortical modulation of above sacral reflex
-
Mediated by sympathetic fibers from T11–L2
-
-
Ejaculation
-
Sympathetic fibers from T11–L2 contribute to the hypogastric plexus
-
-
(Table 2.11) Prevalence of male sexual dysfunction after SCI: [81, 82]
-
Treatment:
-
Hypogonadism
-
Check AM serum testosterone
-
If low, may replace with 200 mg IM q2 weeks
-
Recheck 1 week after injection to ensure dosing within therapeutic range
-
-
Phosphodiesterase-5 inhibitors
-
Sildenafil 25 mg po daily prn
-
Effective for UMN lesions only
-
Avoid if taking nitrates
-
Caution if prone to AD or hypotension
-
-
Intraurethral or intracorporeal prostaglandin E1 (alprostadil)
-
May be effective for LMN lesions
-
Caution if prone to AD (may be painful)
-
Side effects: priapism, trauma
-
-
Vacuum pump
-
Effective for LMN lesions
-
Side effects: trauma, skin breakdown
-
-
Penile implants
-
Complication rate 8–33% (erosion, infection)
-
-
Vibration
-
Vibrator held along penile shaft
-
Effective for UMN lesions only (96%)
-
May trigger AD
-
-
Electroejaculation
-
Rectal probe electrically stimulates the prostate
-
80–90% Success rates
-
Side effects: AD, pain, rectal burns
-
-
-
-
Women
-
Pregnancy
-
<10% of couples will have successful reproduction without assistance [84]
-
40% of men with SCI who have attempted to father children have done so
-
Infertility
-
Erectile and ejaculatory dysfunction
-
Poor semen quality (esp. motility)
-
Recurrent UTI or chronic inflammation
-
Testicular hyperthermia
-
Stasis of prostatic fluid
-
Sperm contact with urine (retrograde ejaculation)
-
-
-
Assisted Reproduction Success Rates
-
Intrauterine insemination: 10–14%
-
IVF: 30–40%
-
-
Complications of Pregnancy
-
Preterm labor and low birth weight
-
Autonomic dysreflexia
-
May be only manifestation of labor
-
Pre-eclampsia does not occur prior to 24 weeks
-
-
Treatment = epidural anesthesia
-
-
Pressure ulcers
-
Increased spasticity
-
Recurrent UTIs
-
Decreased pulmonary function
-
Constipation
-
Leg edema
-
Thromboembolism
-
May need to adjust wheelchair and transfer techniques
-
-
-
Pain
-
Epidemiology:
-
Classification:
(Table 2.12) The International Associate for the Study of Pain (IASP) Classification of pain after SCI [92, 93]
Table 2.12 The international associate for the study of pain (IASP) classification of pain after SCI [92] -
Upper extremity (UE) Pain:
-
Most commonly reported pain after SCI [94]
-
30–50% patient report shoulder pain interferes with ADLs [95, 96]
-
Acute: usually is related to SCI, more common with tetraplegia
-
Chronic: more common in paraplegia, linked to overuse injury, poor seated posture, spasticity, subluxation, rotator cuff pathology [95, 97, 98]
-
Common examples of shoulder pain: [99]
-
Bicipital tendonitis, subacromial bursitis, adhesive capsulitis, acromioclavicular sprain/strain, subluxation, cervical radiculopathy, spasticity, contractures, HO, or syrinx
-
Overuse injuries: [98]
-
45% wrist or hand
-
CTS, ulnar nerve entrapment, DeQuervain’s tenosynovitis, OA
-
-
32% elbow injuries
-
Ulnar nerve entrapment, lateral epicondylitis, OA
-
-
-
-
-
Visceral Pain:
-
Clinical: Abdominal pain or tenderness, nausea, vomiting, constipation, diarrhea, sweating, AD
-
Common causes: Fecal impaction, bowel obstruction, bowel infarction, bowel perforation, cholecystitis, choledocholithiasis, pancreatitis, appendicitis, splenic rupture, bladder perforation, pyelonephritis, UTI, Renal calculus, dysreflexic headache, pressure sores
-
-
Neuropathic Pain:
-
Etiology: Dysfunction in the peripheral and central nervous systems [100]
-
Neuronal hyperexcitability
-
Reduced inhibition
-
Neuronal reorganization/plasticity
-
-
Clinical: tingling, burning, cramping, electric radiations, allodynia, hyperalgesia
-
-
Complications:
-
Workup:
-
Determine the nature of the lesion, the neurological structures involved, and the changes in the surviving tissue [102]
-
Physical exam
-
Determine the neurological level for neuropathic pain [103]
-
If there seems to be neuropathic pain above the known level of injury, have suspicion for secondary (higher) cord compression or ascending syrinx.
-
-
MSK and medical exam for identifying sources of nociceptive pain
-
-
Additional testing with X-ray, CT, MRI, or electrodiagnostic studies may be indicated [103]
-
For further information, refer to Siddall and Middleton, 2006 [104]
-
-
Treatment:
-
Acute musculoskeletal pain and overuse injuries
-
Relative rest, ice, elevation, NSAIDs, device modifications, behavior modification, supportive orthoses, steroid injection
-
-
Medication (See table 2.13)
-
-
ROM, strengthening, stretching, massage, splinting, modalities
-
Balanced shoulder exercise
-
Maintain proper sitting posture
-
Stretch anterior muscles
-
Strengthen posterior muscles
-
Rowing, backward wheeling
-
-
Proper wheelchair, positive seat angle, vertical and low backrest with adequate support for posture
-
Alternate techniques for transferring, weight shifting, mobility
-
-
Psychological therapy [107]
-
Coping skills, cognitive behavioral therapy, exposure to social, sexual, and communication skill training
-
-
Neuromodulation for At Level pain [100, 108]
-
Transcutaneous electric nerve stimulation (TENs)
-
Spinal cord stimulation
-
Deep brain stimulation
-
-
Surgical interventions [100, 108]
-
Spine stabilization, decompression, synrinx cordotomy, cordectomy, myelotomy, doral root entry zone lesion (DREZ)
-
All surgical treatment options have limited support for effectiveness
-
References
The National SCI Statistical Center. Spinal cord injury facts and figures at a glance. (2011). https://www.nscisc.uab.edu/PublicDocuments/reports/pdf/Facts%202011%20Feb%20Final.pdf. Accessed 3 Jul 2012.
McKinley W, et al. Incidence and outcomes of spinal cord injury clinical syndromes. J Spinal Cord Med. 2007;30(3):215–24.
Kirshblum S, Brooks M. Rehabilitation of spinal cord injury. In: Frontera WR, DeLisa JA, editors. Physical medicine and rehabilitation: principles and practice. Philadelphia: Lippincott Williams & Wilkins Health; 2010. p. 665–716.
Schneider RC, Cherry G, Pantek H. The syndrome of acute central cervical spinal cord injury; with special reference to the mechanisms involved in hyperextension injuries of cervical spine. J Neurosurg. 1954;11(6):546–77.
Levi AD, Tator CH, Bunge RP. Clinical syndromes associated with disproportionate weakness of the upper versus the lower extremities after cervical spinal cord injury. Neurosurgery. 1996;38(1):179–83. discussion 183-5.
Burns SP, et al. Recovery of ambulation in motor-incomplete tetraplegia. Arch Phys Med Rehabil. 1997;78(11):1169–72.
Penrod LE, Hegde SK, Ditunno Jr JF. Age effect on prognosis for functional recovery in acute, traumatic central cord syndrome. Arch Phys Med Rehabil. 1990;71(12):963–8.
Bohlman HH. Acute fractures and dislocations of the cervical spine. An analysis of three hundred hospitalized patients and review of the literature. J Bone Joint Surg Am. 1979;61(8):1119–42.
Bosch A, Stauffer ES, Nickel VL. Incomplete traumatic quadriplegia. A ten-year review. JAMA. 1971;216(3):473–8.
Brown-Séquard E. Course of lectures on the physiology & pathology of the central nervous system: illustrated by numerous engravings, representing the principal experiments and pathological cases. Lancet. 1858;72(1822):109–12.
Roth EJ, et al. Traumatic cervical Brown-Sequard and Brown-Sequard-plus syndromes: the spectrum of presentations and outcomes. Paraplegia. 1991;29(9):582–9.
Tattersall R, Turner B. Brown-Sequard and his syndrome. Lancet. 2000;356(9223):61–3.
Cheshire WP, et al. Spinal cord infarction: etiology and outcome. Neurology. 1996;47(2):321–30.
Maynard Jr FM, et al. International standards for neurological and functional classification of spinal cord injury. American Spinal Injury Association. Spinal Cord. 1997;35(5):266–74.
Kennedy JG, et al. Predictors of outcome in cauda equina syndrome. Eur Spine J. 1999;8(4):317–22.
Bohannon RW, Smith MB. Interrater reliability of a modified Ashworth scale of muscle spasticity. Phys Ther. 1987;67(2):206–7.
Kirshblum SC, et al. International standards for neurological classification of spinal cord injury (revised 2011). J Spinal Cord Med. 2011;34(6):535–46.
Consortium for Spinal Cord Medicine Clinical Practice Guidelines. Respiratory management following spinal cord injury: a clinical practice guideline for health-care professionals. J Spinal Cord Med. 2005;28(3):259–93.
Consortium for Spinal Cord Medicine Clinical Practice Guidelines. Prevention of thromboembolism in spinal cord injury. 2nd ed. Washington, DC: Paralyzed Veterans of America; 1999.
Green D, et al. Prevention of thromboembolism after spinal cord injury using low-molecular-weight heparin. Ann Intern Med. 1990;113(8):571–4.
DeVivo MJ, Krause JS, Lammertse DP. Recent trends in mortality and causes of death among persons with spinal cord injury. Arch Phys Med Rehabil. 1999;80(11):1411–9.
Consortium for Spinal Cord Medicine Clinical Practice Guidelines. Outcomes following traumatic spinal cord injury: clinical practice guidelines for health-care professionals. J Spinal Cord Med. 2000;23(4):289–316.
Kirshblum S, et al. Spinal cord injuries. In: Cuccurullo SJ, editor. Physical medicine and rehabilitation board review. New York: Demos; 2010. p. 535–607.
Bryce TN, Ragnarsson KT, Stein AB. Spinal cord injury. In: Braddom RL, editor. Physical medicine and rehabilitation. Philadelphia: Saunders; 2007. p. 1285–350.
Peterson WP, et al. The effect of tidal volumes on the time to wean persons with high tetraplegia from ventilators. Spinal Cord. 1999;37(4):284–8.
Viroslav J, Rosenblatt R, Tomazevic SM. Respiratory management, survival, and quality of life for high-level traumatic tetraplegics. Respir Care Clin N Am. 1996;2(2):313–22.
Bach JR. Noninvasive respiratory management of high level spinal cord injury. J Spinal Cord Med. 2012;35(2):72–80.
Roth EJ, et al. Pulmonary function testing in spinal cord injury: correlation with vital capacity. Paraplegia. 1995;33(8):454–7.
Peterson W, et al. Two methods of weaning persons with quadriplegia from mechanical ventilators. Paraplegia. 1994;32(2):98–103.
Consortium for Spinal Cord Medicine Clinical Practice Guidelines. Bladder management for adults with spinal cord injury: a clinical practice guideline for health-care providers. J Spinal Cord Med. 2006;29(5):527–73.
Everaert K, et al. Urinary tract infections in spinal cord injury: prevention and treatment guidelines. Acta Clin Belg. 2009;64(4):335–40.
D’Hondt F, Everaert K. Urinary tract infections in patients with spinal cord injuries. Curr Infect Dis Rep. 2011;13(6):544–51.
National Institute on Disability and Rehabilitation Research Consensus Statement. The prevention and management of urinary tract infections among people with spinal cord injuries. J Am Paraplegia Soc. 1992;15(3):194–204.
Marciniak C, Rader L, Gagnon C. The use of botulinum toxin for spasticity after spinal cord injury. Am J Phys Med Rehabil. 2008;87(4):312–7. quiz 318-20, 329.
Consortium for Spinal Cord Medicine Clinical Practice Guidelines. Acute management of autonomic dysreflexia: individuals with spinal cord injury presenting to health-care facilities. J Spinal Cord Med. 2002;25 Suppl 1:S67–88.
Banovac K, et al. Prevention of heterotopic ossification after spinal cord injury with indomethacin. Spinal Cord. 2001;39(7):370–4.
van Kuijk AA, Geurts AC, van Kuppevelt HJ. Neurogenic heterotopic ossification in spinal cord injury. Spinal Cord. 2002;40(7):313–26.
Buschbacher R, et al. Warfarin in prevention of heterotopic ossification. Am J Phys Med Rehabil. 1992;71(2):86–91.
Orzel JA, Rudd TG. Heterotopic bone formation: clinical, laboratory, and imaging correlation. J Nucl Med. 1985;26(2):125–32.
Crawford CM, et al. Heterotopic ossification: are range of motion exercises contraindicated? J Burn Care Rehabil. 1986;7(4):323–7.
Bergstrom N, et al. Pressure ulcers in adults: prediction and prevention. Clinical Practice Guideline Number 3. Rockville: U.S. Department of Health and Human Services, Agency for Health Care Policy and Research; 1992. p. 101.
Daniel RK, Priest DL, Wheatley DC. Etiologic factors in pressure sores: an experimental model. Arch Phys Med Rehabil. 1981;62(10):492–8.
Yarkony GM, Heinemann AW. Pressure ulcers. In: Stover SL, DeLisa JA, Whiteneck GG, editors. Spinal cord injury: clinical outcomes from the model systems. Gaithersburg: Aspen Publications; 1995.
Richardson RR, Meyer Jr PR. Prevalence and incidence of pressure sores in acute spinal cord injuries. Paraplegia. 1981;19(4):235–47.
McKinley WO, et al. Long-term medical complications after traumatic spinal cord injury: a regional model systems analysis. Arch Phys Med Rehabil. 1999;80(11):1402–10.
Ho CH, Bogie K. Rehabilitation of spinal cord injury. In: Frontera WR, DeLisa JA, editors. Physical medicine and rehabilitation: principles and practice. Philadelphia: Lippincott Williams & Wilkins Health; 2010. p. 1393–409.
Consortium for Spinal Cord Medicine Clinical_Practice_Guidelines. Pressure ulcer prevention and treatment following spinal cord injury: a clinical practice guideline for health-care professionals. J Spinal Cord Med. 2001;24 Suppl 1:S40–S101.
National Pressure Ulcer Advisory Panel. (2007). Pressure ulcer stages revised by NPUAP. http://www.npuap.org/pr2.htm. Accessed 5 Aug 2012.
Rodeheaver GT, et al. Wound cleansing by high pressure irrigation. Surg Gynecol Obstet. 1975;141(3):357–62.
Krouskop T, et al. A synthesis of the factors that contribute to pressure sore formation. In: Ghista DN, Frankel HL, editors. Spinal cord injury medical engineering. Springfield: Thomas; 1986. p. 247–67.
Tourtual DM, et al. Predictors of hospital acquired heel pressure ulcers. Ostomy Wound Manage. 1997;43(9):24–8. 30, 32-4 passim.
Blaylock B. A study of risk factors in patients placed on specialty beds. J Wound Ostomy Continence Nurs. 1995;22(6):263–6.
Breslow RA, et al. The importance of dietary protein in healing pressure ulcers. J Am Geriatr Soc. 1993;41(4):357–62.
Brewer Jr RD, Mihaldzic N, Dietz A. The effect of oral zinc sulfate on the healing of decubitus ulcers in spinal cord injured patients. Proc Annu Clin Spinal Cord Inj Conf. 1967;16:70–2.
Eleazer GP, et al. Appropriate protocol for zinc therapy in long term care facilities. J Nutr Elder. 1995;14(4):31–8.
Stechmiller JK, Childress B, Cowan L. Arginine supplementation and wound healing. Nutr Clin Pract. 2005;20(1):52–61.
The Consensus Committee of the American Autonomic Society and the American Academy of Neurology. Consensus statement on the definition of orthostatic hypotension, pure autonomic failure, and multiple system atrophy. Neurology. 1996;46(5):1470.
Illman A, Stiller K, Williams M. The prevalence of orthostatic hypotension during physiotherapy treatment in patients with an acute spinal cord injury. Spinal Cord. 2000;38(12):741–7.
Claydon VE, Steeves JD, Krassioukov A. Orthostatic hypotension following spinal cord injury: understanding clinical pathophysiology. Spinal Cord. 2006;44(6):341–51.
Chen D, et al. Medical complications during acute rehabilitation following spinal cord injury–current experience of the Model Systems. Arch Phys Med Rehabil. 1999;80(11):1397–401.
Virchow R. Thrombosis and emboli (1846-1856). Canton: Science History Publications; 1998. p. 234.
Baglin TP, Brush J, Streiff M. Guidelines on use of vena cava filters. Br J Haematol. 2006;134(6):590–5.
Becker DM, Philbrick JT, Selby JB. Inferior vena cava filters. Indications, safety, effectiveness. Arch Intern Med. 1992;152(10):1985–94.
Giannoudis PV, et al. Safety and efficacy of vena cava filters in trauma patients. Injury. 2007;38(1):7–18.
Dubin D. Pulmonary embolism. In: Dubin D, editor. Rapid interpretation of EKG. Tampa: Cover Pub Co; 2000.
Conover MB. Acute pulmonary embolism. In: Conover MB, editor. Understanding electrocardiography. St. Louis: Mosby; 1996.
Maimoun L, Fattal C, Sultan C. Bone remodeling and calcium homeostasis in patients with spinal cord injury: a review. Metabolism. 2011;60(12):1655–63.
Jiang SD, Jiang LS, Dai LY. Mechanisms of osteoporosis in spinal cord injury. Clin Endocrinol (Oxf). 2006;65(5):555–65.
Shane E, Berenson J. Treatment of hypercalcemia. In: Rosen CJ, editor. UpToDate. Waltham: UpToDate; 2012.
Nemunaitis GA, et al. A descriptive study on vitamin D levels in individuals with spinal cord injury in an acute inpatient rehabilitation setting. PM R. 2010;2(3):202–8. quiz 228.
Oleson CV, Patel PH, Wuermser LA. Influence of season, ethnicity, and chronicity on vitamin D deficiency in traumatic spinal cord injury. J Spinal Cord Med. 2010;33(3):202–13.
Heaney RP, et al. Peak bone mass. Osteoporos Int. 2000;11(12):985–1009.
Dawson-Hughes B, et al. Estimates of optimal vitamin D status. Osteoporos Int. 2005;16(7):713–6.
Schopp LH, et al. Testosterone levels among men with spinal cord injury admitted to inpatient rehabilitation. Am J Phys Med Rehabil. 2006;85(8):678–84. quiz 685-7.
Durga A, et al. Prevalence of testosterone deficiency after spinal cord injury. PM R. 2011;3(10):929–32.
Tsitouras PD, et al. Serum testosterone and growth hormone/insulin-like growth factor-I in adults with spinal cord injury. Horm Metab Res. 1995;27(6):287–92.
Celik B, et al. Sex hormone levels and functional outcomes: a controlled study of patients with spinal cord injury compared with healthy subjects. Am J Phys Med Rehabil. 2007;86(10):784–90.
Clark MJ, et al. Testosterone replacement therapy and motor function in men with spinal cord injury: a retrospective analysis. Am J Phys Med Rehabil. 2008;87(4):281–4.
Snyder PJ. Testosterone treatment of male hypogonadism. In: Matsumoto AM, editor. UpToDate. Waltham: UpToDate; 2012.
Consortium for Spinal Cord Medicine Clinical Practice Guidelines. Sexuality and reproductive health in adults with spinal cord injury: a clinical practice guideline for health-care professionals. J Spinal Cord Med. 2010;33(3):281–336.
Linsenmeyer T. Sexual function and sexuality following spinal cord injury. In: Kirshblum S, Campagnolo DI, DeLisa JA, editors. Spinal cord medicine. Philadelphia: Lippincott Williams & Wilkins; 2002. p. 322–30.
Yarkony GM. Enhancement of sexual function and fertility in spinal cord-injured males. Am J Phys Med Rehabil. 1990;69(2):81–7.
Sipski ML, Alexander CJ, Rosen R. Sexual arousal and orgasm in women: effects of spinal cord injury. Ann Neurol. 2001;49(1):35–44.
Bennett CJ, et al. Sexual dysfunction and electroejaculation in men with spinal cord injury: review. J Urol. 1988;139(3):453–7.
Cardenas DD, et al. Gender and minority differences in the pain experience of people with spinal cord injury. Arch Phys Med Rehabil. 2004;85(11):1774–81.
Donnelly C, Eng JJ. Pain following spinal cord injury: the impact on community reintegration. Spinal Cord. 2005;43(5):278–82.
Ravenscroft A, Ahmed YS, Burnside IG. Chronic pain after SCI. A patient survey. Spinal Cord. 2000;38(10):611–4.
Siddall PJ, et al. A longitudinal study of the prevalence and characteristics of pain in the first 5 years following spinal cord injury. Pain. 2003;103(3):249–57.
Bryce TN, Ragnarsson KT. Epidemiology and classification of pain after spinal cord injury. Top Spinal Cord Inj Rehabil. 2001;7(2):1–17.
Stormer S, et al. Chronic pain/dysaesthesiae in spinal cord injury patients: results of a multicentre study. Spinal Cord. 1997;35(7):446–55.
Siddall PJ, et al. Pain report and the relationship of pain to physical factors in the first 6 months following spinal cord injury. Pain. 1999;81(1–2):187–97.
Siddall PJ, Yezierski RP, Loeser JD. Pain following spinal cord injury: clinical features, prevalence, and taxonomy. IASP Newsletter. 2000;3:3–7.
Siddall PJ, Yezierski RP, Loeser JD. Taxonomy and epidemiology of spinal cord injury pain. In: Yezierski RP, Burchiel KJ, editors. Taxonomy and epidemiology of spinal cord injury pain. Seattle: IASP Press; 2002. p. 9–24.
Dyson-Hudson TA, Kirshblum SC. Shoulder pain in chronic spinal cord injury, Part I: epidemiology, etiology, and pathomechanics. J Spinal Cord Med. 2004;27(1):4–17.
Curtis KA, et al. Shoulder pain in wheelchair users with tetraplegia and paraplegia. Arch Phys Med Rehabil. 1999;80(4):453–7.
Irwin R, Restrepo JA, Sherman A. Musculoskeletal pain in persons with spinal cord injury. Top Spinal Cord Inj Rehabil. 2007;13(2):43–57.
Akbar M, et al. A cross-sectional study of demographic and morphologic features of rotator cuff disease in paraplegic patients. J Shoulder Elbow Surg. 2011;20(7):1108–13.
Goldstein B. Musculoskeletal conditions after spinal cord injury. Phys Med Rehabil Clin N Am. 2000;11(1):91–108. viii-ix.
Hastings J, Goldstein B. Paraplegia and the shoulder. Phys Med Rehabil Clin N Am. 2004;15(3):vii. 699-718.
Finnerup NB, Jensen TS. Spinal cord injury pain–mechanisms and treatment. Eur J Neurol. 2004;11(2):73–82.
Widerstrom-Noga EG, Turk DC. Exacerbation of chronic pain following spinal cord injury. J Neurotrauma. 2004;21(10):1384–95.
Yezierski RP. Pain following spinal cord injury: pathophysiology and central mechanisms. Prog Brain Res. 2000;129:429–49.
Haanpaa M, et al. NeuPSIG guidelines on neuropathic pain assessment. Pain. 2011;152(1):14–27.
Siddall PJ, Middleton JW. A proposed algorithm for the management of pain following spinal cord injury. Spinal Cord. 2006;44(2):67–77.
Dworkin RH, et al. Advances in neuropathic pain: diagnosis, mechanisms, and treatment recommendations. Arch Neurol. 2003;60(11):1524–34.
Dromerick AW. Evidence-based rehabilitation: the case for and against constraint-induced movement therapy. J Rehabil Res Dev. 2003;40(1):vii–ix.
Craig AR, et al. Long-term psychological outcomes in spinal cord injured persons: results of a controlled trial using cognitive behavior therapy. Arch Phys Med Rehabil. 1997;78(1):33–8.
Cioni B, et al. Spinal cord stimulation in the treatment of paraplegic pain. J Neurosurg. 1995;82(1):35–9.
Gu Y, Huang LY. Gabapentin actions on N-methyl-d-aspartate receptor channels are protein kinase C-dependent. Pain. 2001;93(1):85–92.
Hendrich J, et al. Pharmacological disruption of calcium channel trafficking by the alpha2delta ligand gabapentin. Proc Natl Acad Sci USA. 2008;105(9):3628–33.
Finnerup NB, et al. Levetiracetam in spinal cord injury pain: a randomized controlled trial. Spinal Cord. 2009;47(12):861–7.
Teasell RW, et al. A systematic review of pharmacologic treatments of pain after spinal cord injury. Arch Phys Med Rehabil. 2010;91(5):816–31.
Johannessen CU. Mechanisms of action of valproate: a commentary. Neurochem Int. 2000;37(2–3):103–10.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2013 Springer Science+Business Media, LLC
About this chapter
Cite this chapter
Siefferman, J.W., Sahler, C., D’Alessio, D.G., Scott, Y., Shetreat-Klein, A. (2013). Spinal Cord Injury. In: Sackheim, K. (eds) Rehab Clinical Pocket Guide. Springer, New York, NY. https://doi.org/10.1007/978-1-4614-5419-9_2
Download citation
DOI: https://doi.org/10.1007/978-1-4614-5419-9_2
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4614-5418-2
Online ISBN: 978-1-4614-5419-9
eBook Packages: MedicineMedicine (R0)