Abstract
This chapter will provide the reader with a framework of how vaccine safety is currently assessed and will review the strengths and limitations of tools utilized preclinically to determine the safety of new vaccines (with a focus on adjuvanted vaccines). The specific safety challenge that has faced vaccines recently and will undoubtedly face the next generation vaccines is that of the infrequent and delayed adverse event of autoimmune disease which shares ingredients of the immune response that are being modulated by next generation vaccines (e.g., T-cells, B-cells, tolerance, TLR, inflammasome). Therefore, the following sections will provide an introduction to the challenges facing preclinical and clinical studies utilizing novel adjuvants. Finally, this chapter will conclude with a “translational” section related to biomarkers and their potential to predict outcome in subjects receiving vaccination. Examples of vaccine-dependent signatures with the potential to predict subject responses, such as immunogenicity, efficacy and safety, as well as subject-specific signatures (e.g., genetic makeup) that may modulate these responses will be provided to emphasize the dual-edge of how increasing the immune response may be favorable for efficacy but potentially detrimental for safety. This is one of the key challenges for the next generation of vaccines and the identification of reliable biomarkers that have the potential to overcome this challenge. The chapter will thus conclude with the huge quantity of information that is likely to result from biomarker research and what will need to be addressed to enable biomarkers to fulfill their promise.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Introduction
This chapter will provide the reader with a framework of how vaccine safety is currently assessed and will review the strengths and limitations of tools utilized preclinically to determine the safety of new vaccines (with a focus on adjuvanted vaccines). The specific safety challenge that has faced vaccines recently and will undoubtedly face the next generation vaccines is that of the infrequent and delayed adverse event of autoimmune disease which shares ingredients of the immune response that are being modulated by next generation vaccines (e.g., T-cells, B-cells, tolerance, TLR, inflammasome). Therefore, the following sections will provide an introduction to the challenges facing preclinical and clinical studies utilizing novel adjuvants. Finally, this chapter will conclude with a “translational” section related to biomarkers and their potential to predict outcome in subjects receiving vaccination. Examples of vaccine-dependent signatures with the potential to predict subject responses, such as immunogenicity, efficacy and safety, as well as subject-specific signatures (e.g., genetic makeup) that may modulate these responses will be provided to emphasize the dual-edge of how increasing the immune response may be favorable for efficacy but potentially detrimental for safety. This is one of the key challenges for the next generation of vaccines and the identification of reliable biomarkers that have the potential to overcome this challenge. The chapter will thus conclude with the large quantity of information that is likely to result from biomarker research and what will need to be addressed to enable biomarkers to fulfill their promise.
2 Current Vaccine Safety Assessments
Because vaccines are usually administered to subjects who are otherwise healthy, they are placed under higher levels of scrutiny regarding related toxicity/adverse events than other pharmaceuticals. Furthermore, vaccines are composed of numerous components (Table 17.1) which, theoretically, have the potential to increase the chances for eliciting an associated toxicity compared to small molecule therapies that consist of single compounds.
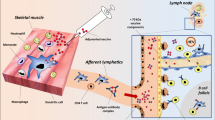
Furthermore, there is a diverse range of adjuvants (e.g., inorganic salts such as alum, oligonucleotides, emulsions such as MF59, and agonists of various Toll-like receptors and other components of the innate immune system) that can be formulated with certain vaccines to enhance the immune response. Each of the ingredients comprising a vaccine, particularly novel adjuvants, requires the same careful evaluation that a new chemical entity undergoes. There are clearly defined guidelines from the US Food and Drug Administration, European Medicines Agency, and the World Health Organization [1] that form the basis of current preclinical toxicology studies for vaccines to assess the risk for human toxicity, including the following: single-dose studies, repeat-dose studies, local tolerance, safety pharmacology, development and reproductive studies, specialized toxicity, and toxicology for new chemically synthesized adjuvants. The signals assessed by these studies focus on changes in physiology, histopathology, injection site irritation, specific organ systems, fertility/fetal development, theoretical concerns, and hypersensitivity/genotoxicity.
These preclinical toxicology studies are designed to assess the intrinsic toxicity of vaccine formulations (including vaccine antigens, adjuvants and excipients), as well as toxicity resulting from the induced immune response. However, such routine studies have their limitations as dramatically illustrated by the unanticipated serious adverse events produced by anti-CD28 therapy in humans that was not observed in animal testing [2]. Furthermore, preclinical safety evaluations may not be adequate for identifying certain rare but potentially serious vaccine-associated adverse events, such as intussusception, hypersensitivity, febrile seizures, or anaphylaxis, and these evaluations are limited in predicting certain types of acute toxicities in the absence of a relevant species for toxicity assessment. For example, with adjuvanted vaccines in particular, species-specific differences in cells, receptors, signaling pathways, and the tissue distribution of common components of the immune system targeted by adjuvants may lead to erroneous conclusions regarding human safety. One can imagine the difficulty in accurately predicting toxicities that are rare and that might occur acutely (such as viscerotropic disease and neurotropic disease after yellow fever vaccination) or arise months or years after vaccination (as seen with autoimmune diseases).
3 Focusing on Adverse Events
Potent stimulation of the immune response with adjuvanted vaccines has led to concerns regarding possible induction of autoreactivity. However, such concerns need to be methodically and thoroughly investigated due to the negative consequences to the welfare of the public when a safe and effective vaccine is incorrectly linked to an adverse event. For example, the false association between the measles/mumps/rubella (MMR) vaccine and the development of autism [3] led to a decrease in vaccination in the United Kingdom with subsequent increases in cases of measles. So why are adjuvants used in vaccines? The main reason is to enhance the effect of antigens or antigenic preparations for vaccines. For example, the use of highly purified subunit and recombinant antigen vaccines has resulted in less immunogenic second generation vaccines due to the absence of ill-defined immunostimulatory contaminants contained in earlier vaccines. Such was the case for whole-cell diphtheria, pertussis, and tetanus (DTwP) vaccine [4], where traces of immunostimulatory components [5] that may have been ligands for TLR and other innate immune receptors [6, 7]. Thus, the addition of adjuvants may compensate for the reduced immunogenicity of purer antigen preparations. Other important reasons to include adjuvants are to overcome hyporesponsiveness in certain populations (e.g., infants, elderly, immunocompromised), reduce the dose of vaccine required, reduce the number of injections, and enhance the quality or breadth of the immune response [8]. However, as more insights have been gained about the pathways by which the innate immune system recognizes pathogens, there have been increasing concerns that potent adjuvants may trigger unwanted inflammation and autoimmunity.
3.1 Historical Concern for Adjuvants Triggering Autoimmunity
There have been only a few documented cases of autoimmune disease induced by vaccines (Table 17.2). The rabies vaccine used in the 1920s contained phenolized sheep brain and induced encephalomyelitis in 0.1% of vaccinees. This vaccine preparation is no longer used in humans. The influenza vaccine used in the 1970s contained the high-yielding influenza recombinant X-53 and had an estimated risk of one case per 100,000 of Guillain–Barre syndrome. Subsequent influenza vaccines based on different strains have a much lower risk of 1 in 1 million [13]. Both the measles vaccine and the MMR vaccine are associated with a risk of immune-mediated thrombocytopenia (1 in 30,000). However, the risk induced by the vaccines is substantially lower than after contraction of the natural diseases of measles or rubella (1 in 3,000 to 1 in 6,000, respectively) [14].
3.2 Utility of Preclinical Studies for Adjuvant-Triggered Human Autoimmune Disease
Strategies that are currently approved for assessing adjuvant toxicity preclinically have been insightful for more general and acute adverse reactions including skin eruptions at the injection site, musculoskeletal symptoms, and those of systemic inflammation (e.g., fever). However, preclinical models for predicting autoimmune diseases remain elusive for the reasons related to the differences in genetics and physiology between animals and humans, and the uncertainties and differences regarding the etiologies of autoimmune diseases in both species. There are numerous animal models of autoimmune disease, but their ability to predict human disease is limited in several respects. First, these models typically mimic the human disease that converge at the levels of end-stage pathology but differ in their pathogenetic mechanisms of action. For example, the MRL-FASlpr mouse strains [15] show similarities in the high titers of autoantibodies and renal disease but lack other clinical manifestations typically identified in the human disease. Second, the use of animal models that develop autoimmune disease at a high frequency (e.g., 90% incidence) may not be able to predict the incidence of rare autoimmune disease events in humans. Third, animal models induced to develop autoimmune disease may have an induction phase with very little relevance to the disease development in humans (e.g., experimental autoimmune encephalomyelitis [16] in rodents for predicting human multiple sclerosis development). Fourth, spontaneous animal models of autoimmunity may have similar pathologies to humans, but the genetic basis and mechanism of pathogenesis may be quite different. The MRL-Fas lpr mouse model, which spontaneously develops lupus nephritis, has a mutation in the Fas gene responsible for defective lymphocytes apoptosis [15]. Polymorphisms in the Fas gene, however, have not been reported to be linked to lupus susceptibility in genome-wide association studies in humans [17, 18]. Finally, it is also important to consider species-specific differences related to an adjuvant’s mode of action. For example, studies in humans have demonstrated that TLR9 is expressed in plasmacytoid dendritic cells and B cells [19–21]; in mice, however, this TLR is additionally expressed in macrophages, myeloid dendritic cells, and activated T-cells [22–25]. Another important component of the innate immune system, TLR8, appears to utilize different agonists in humans versus other species [26]. These species differences in agonist usage, expression, and cellular distribution make inferences from preclinical toxicology studies assessing novel adjuvants difficult and highlight the need for more preclinical models that can better reflect human physiology (e.g., humanized, non-rodent species, or transgenic models, or in vitro cell- and organ-based systems based on human tissues).
3.3 Hypersensitivity: A Rare but Relevant Safety Signal
Induction of hypersensitivity reactions by today’s vaccine preparations is rare but can still happen. In fact, although the exact figures are unknown, it is estimated that at least one per 500,000 individuals develop immediate or late hypersensitivity reactions to vaccines [27, 28]. Of these, most reactions occur to vaccine components used to formulate, produce, or potentiate their action including but not limited to ovalbumin, aluminium, yeast proteins, gelatin, antibiotics or some preservatives and stabilizers such as 2-phenoxyethanol and thiomersal [29–44]. While the cumulative experience in the field of vaccine research and development has allowed us to predict and prevent the occurrence of severe immediate hypersensitivity reactions, most allergic reactions are confined to the local site of injection and are also limited in time. Immediate and local reactions are mostly represented by erythema, swelling, and local pain accompanied infrequently by symptoms derived from the activation of the systemic immunological system (e.g., fever and irritability) [45]. Most common delayed-type hypersensitivity reactions may manifest as eczema which extend beyond the area of inoculation or the typical Arthus-like reaction classically seen in hyperimmune individuals receiving the tetanus vaccination [46, 47]. Although these are all clinically self-limiting, the prediction of adverse events related to occurrence of hypersensitivity reactions have been and continue to be one of the first considerations in the design of clinical trials.
Both local and systemic reactions to adjuvants can be somehow attributed to the activation of immune inflammatory mechanisms triggered by tissue damage and mediated by a range of cytokines such as IL-1, TNFα and IL-6. These are responsible for commonly seem flu-like symptoms, acute vascular responses, worsening of autoimmune or allergic diseases or other manifestations of immunotoxicity [45]. Delayed-type hypersensitivity constitute the basis of the histopathological mechanisms that participate in these reactions and are clinically involved in diseases such as MMF (macrophagic myofasciitis), which has been associated with the local administration of aluminum salts, although evidence of its etiological link remains controversial [48–50].
Perhaps one of the key safety issues to consider in terms of the potential development of hypersensitivity and toxicity reactions is the predictability of safety signals in adjuvanted vaccines administered to pregnant women. The potential advantages of providing ante-natal protection to diseases for which no natural immunity develops within the first 6–8 months of life is of paramount importance. Immunotoxicity studies in this context are limited and preliminary. For example, it has been shown in animal experimental models that injection of high doses of CpG adjuvant can increase the incidence of fetal resorption and craniofacial and limb defects, while a contrary effect can be obtained when lower doses are administered [51–54]. This effect was attributed to the development of Th1-mediated immune responses that correlated with the development of cellular necrosis and a mixed inflammation reaction and calcification in the spongiotrophoblast layer of the placenta [51]. Induction of secretion of cytokines by adjuvants is a well-known and expected mechanism responsible for the recruitment of both innate and adaptive immune cell mediators to the site of injection and for the systemic effects of all adjuvanted vaccine formulations. In this sense, it has been proposed an active role of the placenta in the development and regulation of gene expression related to immunoregulatory component (i.e., cytokines) during organogenesis and hence the potential involvement of the fetal tissue in modulatory effects to vaccines [52, 54]. These and the issues discussed above has prompted the need for biomarker discovery to predict such adverse reactions and design safer, more effective vaccines.
3.4 Clinical Challenges
Given the above-mentioned limitations in translating preclinical findings to responses in humans, it will be necessary to develop alternative preclinical tools to better assess risk in humans. To tackle the issue of autoimmune disease, the clearest answer would be derived from clinical studies that include patients with active autoimmune disease or at high risk of developing disease. However such scientifically and medically driven strategies face obvious ethical issues when considering treatments that could trigger or exacerbate underlying disease. A more feasible approach could investigate whether markers of biological processes that are known to occur in patients with autoimmune disease are seen in normal subjects after vaccination. Such a signature in response to vaccination (that would be safe in normal individuals with normal regulatory processes of the immune system) could highlight a potential risk if the vaccine was given to a “susceptible” subject with a defective regulatory mechanisms. For example, the gene signature regulated by interferon type 1 is consistently associated with systemic lupus erythematosus and other autoimmune diseases [55]. However, similar signatures are also elevated after natural viral infections and immunization by live vaccines regarded to be safe for humans (e.g., yellow fever) [56, 57]. Therefore, other factors such as location and duration of the induced signature are likely to be important with local and transient signatures being of less concern than systemic and continuously elevated signatures.
4 Translational Studies: The Promise of Biomarkers
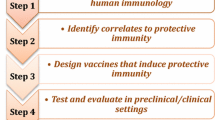
Vaccine biomarker efforts have typically involved measurement of basic immune responses, but it is becoming evident that there is a wide variability in the human immune and other host responses, which will make the interpretation of these vaccine-induced immune responses challenging. These variables include age-related differences in the quality of the immune response, subtleties related to approaches for prophylactic vs. therapeutic vaccines, and how differences in the genetics and general health status of the host can alter the resultant immune response. To begin to address these variables, efforts are underway to benchmark next generation vaccines (e.g., with novel adjuvants) against natural infection or licensed vaccines that have demonstrated acceptable immunogenicity and efficacy and are generally considered to be safe. Such studies will collect detailed information on a wide variety of early and late human host responses and will form the basis for creating a comprehensive database of information from which biomarkers and signatures may be generated. The goal of such biomarkers would be to enable the development of vaccines that safely mimic the host response to natural infection or demonstrate in early clinical studies an immunogenicity or safety profile similar to a licensed vaccines. An extension of the accumulated biomarker data to late stage clinical studies testing efficacy provide the opportunity to develop correlates of protection and safety.
4.1 Vaccine-Dependent Signatures
4.1.1 Predicting Efficacy
While gene expression signatures found their niche in cancer prognosis [58], their successful application to vaccine development will require a better understanding of the human immune response (innate and adaptive immunity) in general, in the setting of immunization, and in response to various types of infection. The feasibility of such an approach was demonstrated in an elegant study [57] where gene signatures were explored in peripheral blood mononuclear cells obtained from subjects immunized with the yellow fever vaccine (YFV-17D). This licensed vaccine serves as a useful benchmark as it is considered to be one of the most effective vaccines (e.g., broad immune response with single injection) that has been administered to more than half a billion people. The authors of this study applied a systems biology approach and extracted distinct gene signatures correlating with the magnitude of the CD8 T-cell response induced by immunization with YFV-17D or those that are associated with increased antibody titers. These signatures were validated in an independent study and were almost 90% accurate in predicting response rate within a few days after vaccination versus those subjects likely to develop protective levels of antibody. Although the dream of many is that a single vaccine modality should protect against a particular infectious disease in all people, the reality is that certain individuals will be predisposed to respond differently to a vaccine, particularly as has been documented by the relatively poor responsiveness to the hepatitis B vaccine in subjects with specific HLA haplotypes [59] or polymorphisms in cytokine-related genes [60]. Recently, it was demonstrated that individuals possess distinct populations of commensal microorganisms (or microbiota) [61]. It is probable that such differences could influence the course of an infection or response to an immunization, particularly those involving mucosal administration. These subject-specific differences may be exploited by future technologies to enable the efficacy of the next generation of vaccines to be tailored to populations as a function of their genetic makeup and microbiota. Both of the above-mentioned examples highlight the potential for gene expression signatures in predicting responses and eventually safety provided that such signatures undergo extensive validation.
4.2 Subject-Specific Signatures
4.2.1 Predicting Safety
As alluded to earlier, continuously evolving technologies may eventually provide the tools to exploit genetic and environmental differences among subjects to improve vaccine efficacy but the same approach can be utilized to improve vaccine safety. For example, serum samples obtained from subjects who have experienced adverse events during a vaccine clinical trial (if timed appropriately) may enable the identification of safety biomarkers. A study illustrative of this personalized medicine approach was the prediction of fever after administration of the smallpox vaccine according to genetic predisposition [62]. This detailed study performed genotyping and sequencing of DNA obtained from the whole blood of more than 300 subjects immunized with the Dryvax smallpox vaccine. Data from this study demonstrated that specific haplotypes in the interleukin-1 (IL-1) gene complex and in interleukin-18 (IL-18) could predict those subjects developing fever after immunization. Similarly, another haplotype in the interleukin-4 gene was associated with protection from the development of high fever. These data illustrate that even simple signatures could potentially be used to identify safety risks in individuals receiving other types of vaccines.
Another study also targeting smallpox vaccination [63] utilized a systems biology approach to identify biomarkers for adverse events. High-dimension genetic studies to examine 1,442 single nucleotide polymorphisms were coupled with more functionally relevant proteomic data to probe associations with adverse events to components of the immune system that were stimulated excessively or prolonged after vaccination. Sixty-one subjects had five clinical visits for adverse event assessments (fever, generalized rash, or lymphadenopathy) in the month following immunization and collection of serum samples for cytokine measurements prior to and in the 5–7 day period post-vaccination evaluation period. The investigators used the Random Forest method to develop a decision-flow algorithm based on three proteomic variables (intracellular adhesion molecule 1 [CD54], interleukin-10, and colony-stimulating factor 3) and a genetic polymorphism in the interleukin-4 cytokine gene. Utilizing these variables, this algorithm was capable of correctly classifying 89% of individuals with respect to their risk for particular adverse events. This systems biology approach visualized complex interactions among multiple factors including genetics (SNPs in and around genes having various immunological functions) and proteomics (cytokines responsible for mediating inflammation), but was limited in scope to a few specific genes. One could anticipate similar genotyping and sequencing efforts on a broader scale on DNA obtained from responders and non-responders to highly efficacious vaccines like yellow fever and hepatitis B to see whether a genotype was associated with the quality of the immune response (good vs. poor). While a comprehensive approach may seem unrealistic today, enabling technologies in the rapidly advancing field of deep genome sequencing will make it feasible in the future.
5 Challenges Facing Biomarkers
The challenges facing biomarkers are related to limitations in current technologies, our understanding of the human immune response, and the limited information that can be translated from vaccines that were licensed in the past and have withstood the test of time with regards to efficacy and safety. These challenges fall into two basic categories: interpretation of information, as previously discussed, and collection of samples from which the information is measured. Ideally, one will need to understand host responses both locally at the injection site and draining lymph nodes and systemically. This will be true for early responses (within minutes) and late responses (days to months). To this end, we will need (1) noninvasive means of frequent sampling (e.g., implantable devices for continuous feedback), (2) miniaturization of assays to maximize the amount of information gathered from small tissue samples, and (3) high throughput means to assess safety and efficacy of vaccine candidates. Together, advances in these areas will allow us to keep pace with our ability to generate better antigens, adjuvants, delivery systems, and combinations thereof.
A recent perspective [64] illustrated that biomarker signatures (e.g., gene array) have failed to translate into clinical relevant tools due to the failure of performing adequate validations in independent clinical trials and the overestimation of a signature’s performance. A key challenge facing biomarkers is that knowledge of how to read the messages in the genome remains elusive. This genetic illiteracy coupled with the absence of tools to reliably interpret how genetic data translates into biological pathways greatly complicates the prediction of cause and effect. The development of the next generation of vaccines would be greatly facilitated if comparable biomarker data from different vaccine developers were available in a standardized format that preserved proprietary interests. Such an effort would require the establishment of repositories requiring public funding and agreement on standardization. Furthermore, as mentioned previously, even the creation of a well-stocked repository of “omics” data about novel adjuvants and next generation vaccines may be of limited value if there is no frame of reference for interpreting the data and generating hypotheses about factors that predict safety. Therefore, “benchmark” studies will need to be undertaken to compare human and animal model responses with next generation vaccines to those elicited with approved vaccines for which the safety profiles and the adverse events are well known. The regulatory considerations for first-in-human clinical trials with vaccines are elegantly presented in a recent publication [65] and should serve as the frame of reference for next generation vaccines. As more data is obtained on the human response to licensed vaccines and adjuvants with established safety records, the need for guidelines on how to apply these data to evaluate novel adjuvants and next generation vaccines is paramount. Along these lines, the U.S. Food and Drug Administration has created a Genomics Evaluation Team for Safety to develop approaches for the application of new technologies to the safety of biologics. Using the existing structure of the Voluntary Exploratory Data Submission (VXDS) process [66], one could envision the submission of biomarker data from vaccines with known benefit–risk profiles that would facilitate future biomarker development, clinical translation, and regulatory qualification.
6 Conclusion
Vaccines are a critical component of preventive medicine, and delays in the implementation of next generation vaccines due to the risks of rare adverse events (real or perceived) will need to be balanced with the larger disease-associated morbidity and mortality caused by infection in the general population not receiving the vaccine. The highest hurdle for future vaccines will be the same challenge that has faced older vaccines—safety! For next generation vaccines (especially those containing adjuvants), there will be a need for carefully designed preclinical studies that decipher the mode of action according to standards set by regulatory agencies working in conjunction with industry. Furthermore, as our knowledge of the mode of action becomes more sophisticated, paradoxically, so will the public perception of safety as links will be drawn to potentially rare or irrelevant diseases based on commonalities in the immune system, the vaccine mode of action, and pathways of human disease. Therefore, there will also be a need for large-scale epidemiological studies in human populations to confirm the safety of the next generation of vaccines (especially for the risk of rare or delayed adverse events, such as autoimmune disease). The reader should appreciate that in addition to the challenges of vaccine-related adverse events, there will always be the delays to safe and effective next generation vaccines caused by coincidental associations (not vaccine-related) that will occur with longer follow-up periods of vaccinated subjects due to factors related to the environment, diet, age-related changes in the immune system, and conditions associated with triggering autoimmune disease in susceptible subjects (e.g., pregnancy or exposure to natural infections).
References
Wolf JJ, Kaplanski CV, Lebron JA (2010) Nonclinical safety assessment of vaccines and adjuvants. Methods Mol Biol 626:29–40
Suntharalingam G, Perry MR, Ward S, Brett SJ, Castello-Cortes A, Brunner MD, Panoskaltsis N (2006) Cytokine storm in a phase 1 trial of the anti-CD28 monoclonal antibody TGN1412. N Engl J Med 355:1018–1028
Dyer C (2010) Wakefield was dishonest and irresponsible over MMR research, says GMC. BMJ 340:c593
Edwards KM, Decker MD (2004) Vaccines. Saunders, Philadelphia
Ellis RW (2008) Vaccines. Saunders, Philadelphia
Fransen F, Stenger RM, Poelen MC, van Dijken HH, Kuipers B, Boog CJ, van Putten JP, van Els CA, van der Ley P (2010) Differential effect of TLR2 and TLR4 on the immune response after immunization with a vaccine against Neisseria meningitidis or Bordetella pertussis. PLoS One 5:e15692
Kimman TG, Banus S, Reijmerink N, Reimerink J, Stelma FF, Koppelman GH, Thijs C, Postma DS, Kerkhof M (2008) Association of interacting genes in the toll-like receptor signaling pathway and the antibody response to pertussis vaccination. PLoS One 3:e3665
Singh M, O’Hagan DT (2002) Recent advances in vaccine adjuvants. Pharm Res 19:715–728
Stuart G, Krikorian KS (1928) The neuro-paralytic accidents of anti-rabies treatment. Ann Trop Med Parasitol 22:327–377
Schonberger LB, Bregman DJ, Sullivan-Bolyai JZ, Keenlyside RA, Ziegler DW, Retailliau HF, Eddins DL, Bryan JA (1979) Guillain-Barre syndrome following vaccination in the National Influenza Immunization Program, United States, 1976–1977. Am J Epidemiol 110:105–123
Beeler J, Varricchio F, Wise R (1996) Thrombocytopenia after immunization with measles vaccines: review of the vaccine adverse events reporting system (1990 to 1994). Pediatr Infect Dis J 15:88–90
Mutsch M, Zhou W, Rhodes P, Bopp M, Chen RT, Linder T, Spyr C, Steffen R (2004) Use of the inactivated intranasal influenza vaccine and the risk of Bell’s palsy in Switzerland. N Engl J Med 350:896–903
Chen RT, Pless R, Destefano F (2001) Epidemiology of autoimmune reactions induced by vaccination. J Autoimmun 16:309–318
Wraith DC, Goldman M, Lambert PH (2003) Vaccination and autoimmune disease: what is the evidence? Lancet 362:1659–1666
Kono DH, Theofilopoulos AN (2006) Genetics of SLE in mice. Springer Semin Immunopathol 28:83–96
Hemmer B, Nessler S, Zhou D, Kieseier B, Hartung HP (2006) Immunopathogenesis and immunotherapy of multiple sclerosis. Nat Clin Pract Neurol 2:201–211
Aumeunier A, Grela F, Ramadan A, Van Pham L, Bardel E, Gomez Alcala A, Jeannin P, Akira S, Bach JF, Thieblemont N (2010) Systemic Toll-like receptor stimulation suppresses experimental allergic asthma and autoimmune diabetes in NOD mice. PLoS One 5:e11484
Crow MK (2008) Collaboration, genetic associations, and lupus erythematosus. N Engl J Med 358:956–961
Bernasconi NL, Onai N, Lanzavecchia A (2003) A role for Toll-like receptors in acquired immunity: up-regulation of TLR9 by BCR triggering in naive B cells and constitutive expression in memory B cells. Blood 101:4500–4504
Hornung V, Rothenfusser S, Britsch S, Krug A, Jahrsdorfer B, Giese T, Endres S, Hartmann G (2002) Quantitative expression of toll-like receptor 1-10 mRNA in cellular subsets of human peripheral blood mononuclear cells and sensitivity to CpG oligodeoxynucleotides. J Immunol 168:4531–4537
Rothenfusser S, Tuma E, Endres S, Hartmann G (2002) Plasmacytoid dendritic cells: the key to CpG. Hum Immunol 63:1111–1119
Gelman AE, Zhang J, Choi Y, Turka LA (2004) Toll-like receptor ligands directly promote activated CD4+ T cell survival. J Immunol 172:6065–6073
Gilliet M, Boonstra A, Paturel C, Antonenko S, Xu XL, Trinchieri G, O’Garra A, Liu YJ (2002) The development of murine plasmacytoid dendritic cell precursors is differentially regulated by FLT3-ligand and granulocyte/macrophage colony-stimulating factor. J Exp Med 195:953–958
Martin-Orozco E, Kobayashi H, Van Uden J, Nguyen MD, Kornbluth RS, Raz E (1999) Enhancement of antigen-presenting cell surface molecules involved in cognate interactions by immunostimulatory DNA sequences. Int Immunol 11:1111–1118
Suzuki K, Suda T, Naito T, Ide K, Chida K, Nakamura H (2005) Impaired toll-like receptor 9 expression in alveolar macrophages with no sensitivity to CpG DNA. Am J Respir Crit Care Med 171:707–713
Govindaraj RG, Manavalan B, Basith S, Choi S (2011) Comparative analysis of species-specific ligand recognition in Toll-like receptor 8 signaling: a hypothesis. PLoS One 6:e25118
Fritsche PJ, Helbling A, Ballmer-Weber BK (2010) Vaccine hypersensitivity—update and overview. Swiss Med Wkly 140:238–246
Lawrence GL, Boyd I, McIntyre PB, Isaacs D (2005) Annual report: surveillance of adverse events following immunisation in Australia, 2004. Commun Dis Intell 29:248–262
Rennels MB, Deloria MA, Pichichero ME, Losonsky GA, Englund JA, Meade BD, Anderson EL, Steinhoff MC, Edwards KM (2000) Extensive swelling after booster doses of acellular pertussis-tetanus-diphtheria vaccines. Pediatrics 105:e12
Tariq SM, Matthews SM, Hakim EA, Arshad SH (2000) Egg allergy in infancy predicts respiratory allergic disease by 4 years of age. Pediatr Allergy Immunol 11:162–167
Zeiger RS (2002) Current issues with influenza vaccination in egg allergy. J Allergy Clin Immunol 110:834–840
Pool V, Braun MM, Kelso JM, Mootrey G, Chen RT, Yunginger JW, Jacobson RM, Gargiullo PM (2002) Prevalence of anti-gelatin IgE antibodies in people with anaphylaxis after measles-mumps rubella vaccine in the United States. Pediatrics 110:e71
Scherer KR, Zentner MR, Stern D (2004) Beyond surprise: the puzzle of infants’ expressive reactions to expectancy violation. Emotion 4:389–402
Zent O, Hennig R (2004) Post-marketing surveillance of immediate allergic reactions: polygeline-based versus polygeline-free pediatric TBE vaccine. Vaccine 23:579–584
DiMiceli L, Pool V, Kelso JM, Shadomy SV, Iskander J (2006) Vaccination of yeast sensitive individuals: review of safety data in the US vaccine adverse event reporting system (VAERS). Vaccine 24:703–707
Chow C, Cardona M, Raju PK, Iyengar S, Sukumar A, Raju R, Colman S, Madhav P, Reddy KS, Celermajer D, Neal B (2007) Cardiovascular disease and risk factors among 345 adults in rural India—the Andhra Pradesh Rural Health Initiative. Int J Cardiol 116:180–185
Jarvie HP, Neal C, Withers PJ (2006) Sewage-effluent phosphorus: a greater risk to river eutrophication than agricultural phosphorus? Sci Total Environ 360:246–253
Kemp PA, Neale J, Robertson M (2006) Homelessness among problem drug users: prevalence, risk factors and trigger events. Health Soc Care Community 14:319–328
Simons JS, Neal DJ, Gaher RM (2006) Risk for marijuana-related problems among college students: an application of zero-inflated negative binomial regression. Am J Drug Alcohol Abuse 32:41–53
Kwittken PL, Rosen S, Sweinberg SK (1993) MMR vaccine and neomycin allergy. Am J Dis Child 147:128–129
Kumar M, Behera AK, Hu J, Lockey RF, Mohapatra SS (2001) IFN-gamma and IL-12 plasmid DNAs as vaccine adjuvant in a murine model of grass allergy. J Allergy Clin Immunol 108:402–408
Zheng W, Dreskin SC (2007) Thimerosal in influenza vaccine: an immediate hypersensitivity reaction. Ann Allergy Asthma Immunol 99:574–575
DeStefano F (2007) Vaccines and autism: evidence does not support a causal association. Clin Pharmacol Ther 82:756–759
Offit PA, Jew RK (2003) Addressing parents’ concerns: do vaccines contain harmful preservatives, adjuvants, additives, or residuals? Pediatrics 112:1394–1397
Batista-Duharte A, Lindblad EB, Oviedo-Orta E (2011) Progress in understanding adjuvant immunotoxicity mechanisms. Toxicol Lett 203:97–105
Mowat AM, Donachie AM, Reid G, Jarrett O (1991) Immune-stimulating complexes containing Quil A and protein antigen prime class I MHC-restricted T lymphocytes in vivo and are immunogenic by the oral route. Immunology 72:317–322
Furrie E, Smith RE, Turner MW, Strobel S, Mowat AM (2002) Induction of local innate immune responses and modulation of antigen uptake as mechanisms underlying the mucosal adjuvant properties of immune stimulating complexes (ISCOMS). Vaccine 20:2254–2262
Authier FJ, Cherin P, Creange A, Bonnotte B, Ferrer X, Abdelmoumni A, Ranoux D, Pelletier J, Figarella-Branger D, Granel B, Maisonobe T, Coquet M, Degos JD, Gherardi RK (2001) Central nervous system disease in patients with macrophagic myofasciitis. Brain 124:974–983
Gherardi RK (2003) Lessons from macrophagic myofasciitis: towards definition of a vaccine adjuvant-related syndrome. Rev Neurol (Paris) 159:162–164
Gherardi RK, Coquet M, Cherin P, Belec L, Moretto P, Dreyfus PA, Pellissier JF, Chariot P, Authier FJ (2001) Macrophagic myofasciitis lesions assess long-term persistence of vaccine-derived aluminium hydroxide in muscle. Brain 124:1821–1831
Prater MR, Johnson VJ, Germolec DR, Luster MI, Holladay SD (2006) Maternal treatment with a high dose of CpG ODN during gestation alters fetal craniofacial and distal limb development in C57BL/6 mice. Vaccine 24:263–271
Szekeres-Bartho J (2002) Immunological relationship between the mother and the fetus. Int Rev Immunol 21:471–495
Raghupathy R (1997) Th1-type immunity is incompatible with successful pregnancy. Immunol Today 18:478–482
Kushima K, Oda K, Sakuma S, Furusawa S, Fujiwara M (2007) Effect of prenatal administration of NSAIDs on the immune response in juvenile and adult rats. Toxicology 232:257–267
Banchereau J, Pascual V (2006) Type I interferon in systemic lupus erythematosus and other autoimmune diseases. Immunity 25:383–392
Gaucher D, Therrien R, Kettaf N, Angermann BR, Boucher G, Filali-Mouhim A, Moser JM, Mehta RS, Drake DR 3rd, Castro E, Akondy R, Rinfret A, Yassine-Diab B, Said EA, Chouikh Y, Cameron MJ, Clum R, Kelvin D, Somogyi R, Greller LD, Balderas RS, Wilkinson P, Pantaleo G, Tartaglia J, Haddad EK, Sekaly RP (2008) Yellow fever vaccine induces integrated multilineage and polyfunctional immune responses. J Exp Med 205:3119–3131
Querec TD, Akondy RS, Lee EK, Cao W, Nakaya HI, Teuwen D, Pirani A, Gernert K, Deng J, Marzolf B, Kennedy K, Wu H, Bennouna S, Oluoch H, Miller J, Vencio RZ, Mulligan M, Aderem A, Ahmed R, Pulendran B (2009) Systems biology approach predicts immunogenicity of the yellow fever vaccine in humans. Nat Immunol 10:116–125
Van’t Veer LJ, Dai H, van de Vijver MJ, He YD, Hart AA, Mao M, Peterse HL, van der Kooy K, Marton MJ, Witteveen AT, Schreiber GJ, Kerkhoven RM, Roberts C, Linsley PS, Bernards R, Friend SH (2002) Gene expression profiling predicts clinical outcome of breast cancer. Nature 415:530–536
Milich DR, Leroux-Roels GG (2003) Immunogenetics of the response to HBsAg vaccination. Autoimmun Rev 2:248–257
Chen J, Liang Z, Lu F, Fang X, Liu S, Zeng Y, Zhu F, Chen X, Shen T, Li J, Zhuang H (2011) Toll-like receptors and cytokines/cytokine receptors polymorphisms associate with non-response to hepatitis B vaccine. Vaccine 29:706–711
Lathrop SK, Bloom SM, Rao SM, Nutsch K, Lio CW, Santacruz N, Peterson DA, Stappenbeck TS, Hsieh CS (2011) Peripheral education of the immune system by colonic commensal microbiota. Nature 478:250–254
Stanley SL Jr, Frey SE, Taillon-Miller P, Guo J, Miller RD, Koboldt DC, Elashoff M, Christensen R, Saccone NL, Belshe RB (2007) The immunogenetics of smallpox vaccination. J Infect Dis 196:212–219
Reif DM, Motsinger-Reif AA, McKinney BA, Rock MT, Crowe JE Jr, Moore JH (2009) Integrated analysis of genetic and proteomic data identifies biomarkers associated with adverse events following smallpox vaccination. Genes Immun 10:112–119
Koscielny S (2010) Why most gene expression signatures of tumors have not been useful in the clinic. Sci Transl Med 2:14ps12
Goetz KB, Pfleiderer M, Schneider CK (2010) First-in-human clinical trials with vaccines—what regulators want. Nat Biotechnol 28:910–916
Goodsaid FM, Amur S, Aubrecht J, Burczynski ME, Carl K, Catalano J, Charlab R, Close S, Cornu-Artis C, Essioux L, Fornace AJ Jr, Hinman L, Hong H, Hunt I, Jacobson-Kram D, Jawaid A, Laurie D, Lesko L, Li HH, Lindpaintner K, Mayne J, Morrow P, Papaluca-Amati M, Robison TW, Roth J, Schuppe-Koistinen I, Shi L, Spleiss O, Tong W, Truter SL, Vonderscher J, Westelinck A, Zhang L, Zineh I (2010) Voluntary exploratory data submissions to the US FDA and the EMA: experience and impact. Nat Rev Drug Discov 9:435–445
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2013 Springer Science+Business Media New York
About this chapter
Cite this chapter
Ahmed, S.S., Oviedo-Orta, E., Ulmer, J. (2013). Safety Challenges Facing Next Generation Vaccines and the Role for Biomarkers. In: Singh, M. (eds) Novel Immune Potentiators and Delivery Technologies for Next Generation Vaccines. Springer, Boston, MA. https://doi.org/10.1007/978-1-4614-5380-2_17
Download citation
DOI: https://doi.org/10.1007/978-1-4614-5380-2_17
Published:
Publisher Name: Springer, Boston, MA
Print ISBN: 978-1-4614-5379-6
Online ISBN: 978-1-4614-5380-2
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)