Abstract
Maximizing the efficacy of IBD-directed therapies while minimizing their toxicity remains the principal objective in developing management strategies for IBD patients. Pharmacogenetics of Thiopurine S-methyltransferase has helped clinicians achieve these objectives targeted at patients receiving either 6-Mercaptopurine (6-MP) or azathioprine, both members of the thiopurine family. This drug-metabolizing enzyme influences the concentration of thiopurine reaching its target (pharmacokinetics). Currently, most IBD patients are treated as if they are homogenous. However patients would certainly benefit from being stratified into those that will or will not have a benefit from a therapy and further divided into those that will or will not have a toxic response to a therapy. The recognition and understanding of the factors influencing therapeutic response have the potential to allow clinicians and the pharmaceutical industry the ability to individualize dosing and administration regimens to maximize benefit and avoid toxicity.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Introduction
As the arsenal of IBD therapies becomes more powerful, choosing a therapy that is appropriate for an individual patient requires an understanding of the goals of IBD therapy. Maximizing the efficacy of IBD-directed therapies while minimizing their toxicity remains the principal objective in developing management strategies for IBD patients. Unfortunately, for most therapeutic agents and the majority of diseases, it is not currently possible to identify patients most likely to benefit from therapy on the basis of their genetic profile, nor is it possible to identify those individuals at risk of a severe adverse reaction. However, the introduction of pharmacogenetics in the management of IBD patients has helped clinicians achieve these objectives targeted at patients receiving either 6-Mercaptopurine (6-MP) or azathioprine (AZA), both members of the thiopurine family. This research strategy involved studying the Thiopurine S-methyltransferase (TPMT) drug-metabolizing enzyme which influences the concentration of drug reaching its target (pharmacokinetics).
Pharmacogenetics is the study of the role of inheritance in individual variation in drug response—with inadequate therapeutic response at one end of the spectrum and adverse drug reactions at the other. Currently, most IBD patients are treated as if they are homogenous. However patients would certainly benefit from being stratified into those that will or will not have a benefit from a therapy and further divided into those that will or will not have a toxic response to a therapy. Moreover, patients could be directed to an alternate therapy that would be more beneficial or they could avoid toxicities by being aware that the available therapeutics offer little or no benefit. The recognition and understanding of the factors influencing therapeutic response have the potential to allow clinicians and the pharmaceutical industry the ability to individualize dosing and administration regimens to maximize benefit and avoid toxicity.
A Historical Perspective of TPMT Pharmacogenetics
TPMT serves as a model of pharmacogenetic research such that TPMT was highlighted by the United States Food and Drug Administration (FDA) as one of the two “valid biomarkers” for pharmacogenetics and pharmacogenomics in the 2003 FDA “Draft Guidance for Pharmacogenomic Data Submission” [1]. TPMT is a cytosolic drug-metabolizing enzyme that catalyses the S-methylation of 6-MP and AZA [2, 3]. Thiopurines have a relatively narrow therapeutic index, with the potential for life-threatening drug-induced toxicity, primarily myelosuppression [4–6].
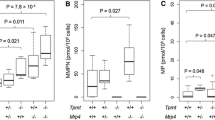
The notion that inherited genetic variability may play an important role in drug responsiveness in patients receiving thiopurines first arose when Weinshilboum noted striking differences in the way patients responded to standard therapeutic doses. He described large inherited variations in human tissue TPMT enzyme activity [7]. Levels of TPMT activity in the RBC reflect relative levels of that enzyme in the kidney, liver, and lymphocyte [8–11]. Population-based studies have demonstrated that TPMT activity is inherited as an autosomal codominant trait. The frequency distribution of the TPMT polymorphisms reveals that 1 in 300 (0.3%) individuals have low to absent enzyme activity (homozygous TPMTL), 11% have intermediate (heterozygous TPMTH/TPMTL) and 89% have normal to high levels of activity (homozygous/wild type TPMTH) [7] (Fig. 25.1). Subsequently the human TPMT gene was cloned [12–14] and to date a total of 21 TPMT genetic polymorphisms have been identified [15]. TPMT*3A, a double mutant, (A719G and G460A) is the most frequent mutant allele and predominates in Caucasians (frequency 5%) (Fig. 25.2). Each mutant, however, TPMT*3B (G460A) and TPMT*3C (A710G), can occur independently. Although mutant allele frequencies may be similar among different ethnicities, the prevalent mutant alleles do differ such that TPMT*3C is most common among African-Americans [16]. TPMT *3C is also the prevalent mutant allele in East Asia (2%) [17]. The degree of reduction in TPMT activity and immunoreactive protein varies based on the mutant allele present in an individual [14]. The presence of TPMT*3A and *3B results in a virtual lack of TPMT enzyme activity and protein in the tissues of subjects who carry these alleles and, as a result, patients homozygous for these alleles can suffer severe, life-threatening myelosuppression when treated with standard doses of thiopurines, i.e., they are “overdosed” on standard doses [4, 5, 18]. TPMT*2, is also associated with a decrease in TPMT enzyme activity yet not to the same extent as TPMT*3A and *3B [14, 15, 19, 20].
Pharmacology of Thiopurines
6-MP and AZA are often used interchangeably in the treatment of IBD. Once absorbed, AZA is rapidly converted via a nonenzymatic process to 6-MP and S-methyl-4-nitro-5-thioimidazole. AZA is 55% of 6-MP by molecular weight and 88% of AZA is converted to 6-MP such that a conversion factor of 2.08 must be taken into account when calculating equivalent doses of 6-MP and AZA. 6-MP (or AZA converted to 6-MP) undergoes a complex biotransformation to its inactive and active metabolites via competing catabolic and anabolic metabolic pathways (Fig. 25.3). 6-MP undergoes extensive “first pass” catabolism by xanthine oxidase (XO), which is present in both the intestinal mucosa and liver limiting the systemic bioavailability of thiopurines. 6-MP also serves as a substrate for the TPMT enzyme, which methylates 6-MP to the inactive methylated-mercaptopurine metabolite (6-MeMP). Like XO, TPMT may be present in the intestinal mucosa and may also contribute to the pre-systemic catabolism of 6-MP. The hypoxanthine phosphoribosyl transferase (HPRT) enzyme is paramount to the initiation of the anabolic transformation of 6-MP to its active metabolites. The intracellular activation of 6-MP yields the first active intermediate metabolite, thioinosine monophosphate (TiMP), which is then rapidly converted to the thioguanine nucleotides (6-TGN). The cytotoxic and immunosuppressive effects of thiopurines, were, until recently, presumed to be primarily mediated via the incorporation of 6-TGN into cellular nucleic acids ultimately resulting in inhibition of lymphocyte proliferation. Recent advances in the understanding of the mechanism of action of thiopurines, however, suggest that the 6-thioguanine triphosphate (6-thio-GTP) nucleotide may play an important role in the process of signaling lymphocyte apoptosis by inhibiting Rac1 activation in T cells [21]. The triphosphate metabolite appears to correlate most with clinical efficacy of thiopurines [22]. Further research is needed to examine the role of 6-thio-GTP in patients with IBD.
Thiopurine metabolism. Oral azathioprine (AZA) is rapidly converted to 6-MP by a nonenzymatic process [19]. Initial 6-MP transformations occur along competing catabolic (XO xanthine oxidase; TPMT thiopurine methyltransferase) and anabolic (HPRT hypoxanthine phosphoribosyltransferase) enzymatic pathways. Once formed, 6-thiosine 5′-monophosphate (6-TImP) may be transformed into 6-thioguanine nucleotides (6-TGN) by the rate limiting inosine monophosphate dehydrogenase (IMPDH) or methylated into 6-methyl-mercaptopurine nucleotides (6-MMP)
The major competing enzymatic process that competes with the intracellular activation pathway is the thiol methylation of TiMP by TPMT. Although these methylated metabolites (Me-TiMP or 6-MMPR) have been shown in vitro to inhibit denovo purine synthesis, in vivo evidence is lacking as to their role in the mechanism of action of thiopurines [6]. TPMT methylation competes with the activation pathway and influences the relative proportion of intracellular active 6-TGN produced by a given individual. This inverse relationship between TPMT and 6-TGN has important implications in both the efficacy and toxicity of thiopurines. Patients with intermediate or absent TPMT activity can produce significantly higher concentrations of 6-TGN. The negative correlation between TPMT and 6-TGN was first reported in the treatment of childhood leukemia [4] and has since been confirmed among pediatric IBD patients [23].
Physicians should also pay particular attention to potential drug interactions such that the inhibition of recombinant human TPMT has been demonstrated in vitro and has been reported in vivo with both 6-MP and olsalazine [24, 25]. Thus caution should be taken when co-administering 5-ASAs and thiopurines as TPMT inhibition may increase the risk of developing myelosuppression. A recent study demonstrated that after 5-ASA withdrawal the mean 6-TGN levels significantly decreased without significant changes in TPMT activity or blood counts suggesting an alternative mechanism to TPMT inhibition [26]. This effect may be additive in patients already genetically determined to produce lower levels of the TPMT enzyme such that diligent blood count monitoring is necessary.
The Clinical Application of TPMT Pharmacogenetics
As explained above, TPMT methylates thiopurine metabolites at the expense of the formation of 6-TGN. However, patients with less than normal TPMT expression and activity can produce significantly higher concentrations of 6-TGN. This inverse relationship between TPMT and 6-TGN has important implications in both the efficacy and toxicity of thiopurines. The association between TPMT and myelosuppression in IBD patients was published by Colombel et al. who reported that 27% of IBD patients experienced leukopenia and/or thrombocytopenia attributable to abnormal TPMT activity [27]. Moreover, TPMT deficiency (homozygote mutant) accounted for 10% of the cases and the median time to onset of bone marrow suppression was 1 month, whilst 17% of the cases were TPMT heterozygotes. In this study only 32% of the cases of myelosupression were secondary to lower TPMT activity. Thus patients should be regularly monitored with complete blood counts and secondary causes such as concomitant medications or concurrent viral illness should be considered. The a priori knowledge of an individual’s TPMT activity can identify those patients prone to early leukopenic events when treated with standard doses of thiopurines as a result of intermediate TPMT levels. Moreover, the 1 in 300 individuals at risk for potentially life-threatening complications can be rapidly identified and alternate immunomodulators can be administered. Intermediate TPMT activity is not a contraindication for thiopurine use and typically these patients can safely receive thiopurines at lower doses (30–50% of standard dose) and dose escalation can be successful while patients are monitored closely with regular blood counts and 6-TGN concentrations [28, 29]. For the majority of thiopurine recipients, clinicians can safely administer what is considered an optimal starting dose of 6-MP (1–1.5 mg/kg/day) and AZA (2.0–2.5 mg/kg/day) as a result of normal to high TPMT activity. Whether it be empiric or TPMT based dosing, patients require regular blood count and liver chemistry monitoring throughout the duration of thiopurine therapy.
It remains unknown as to the safety implications of having high TPMT activity. Elevated levels of 6-MMP have been shown to be associated with an increased frequency of hepatotoxicity as defined by elevations in transaminases >2× normal [23, 30]. Given that TPMT results in the formation of 6-MMP, it could be hypothesized that patients with high TPMT produce potentially hepatotoxic levels of 6-MMP and the first pass catabolism of the drug in the liver by higher than normal TPMT activity may lead to the accumulation of higher levels of 6-MMP. Liver enzyme elevations typically normalize in a timely manner in response to dose reduction as a result of a decrease in 6-MMP levels. Not all patients experience an elevation in transaminases in association with high 6-MMP levels and few merit a significant dose reduction; however, these patients should be closely monitored.
Pharmacokinetics: The Role of Metabolite Monitoring
The importance of metabolite monitoring and TPMT activity was first brought to our attention through the research initiated in childhood acute lymphoblastoid leukemia (ALL) [4]. Initial studies in IBD were conducted in the pediatric age group and reported that 6-TGN was shown to be significantly and independently associated with therapeutic response [23, 31]. This study demonstrated that significantly higher median 6-TGN levels were observed at points of clinical response (312) vs. nonresponse (199). Further analysis revealed that the best probability of treatment response was not significantly increased until 6-TGN levels were greater than 235 and the odds ratio (OR) of a therapeutic response for a 6-TG level higher than a cutoff of 235 was 5.0 as compared to when the levels were below this cut point. A certain percentage of patients did achieve a therapeutic response with levels <235; however, this response rate was almost less than half the proportion of patients (78%) achieving therapeutic response when levels were >235. Subtherapeutic dosing, or based on these studies, perhaps more appropriately subtherapeutic 6-TGN levels, is the most common reason why patients are not responding to thiopurines. Cuffari et al. demonstrated that most patients, initially not responding to low-dose thiopurine therapy that underwent dose escalation responded well once they achieved 6-TGN levels >250 [32]. A meta-analysis reported that patients with 6-TGN levels above the threshold value were more likely to be in remission (62%) than those below the threshold value (36%) (pooled odds ratio, 3.3; 95% confidence interval, 1.7–6.3; P < 0.001) [33].
Metabolite monitoring is most informative in helping clinicians classify therapeutic failures. Non-compliance and under dosing remain the most common reasons for therapeutic failure and can be identified by measuring 6-MP metabolite levels. When both 6-TGN and 6-MMP levels are undetectable, there is a high likelihood that the patient is not adhering to therapy. However, a subgroup of patients continues to fail therapy despite dose escalation and receiving standard or even higher than standard doses of thiopurines. These patients can be divided into two distinct subgroups and are defined biochemically by their metabolite profiles. The most common subgroup is composed of patients resistant to thiopurines and biochemically characterized by the persistence of subtherapeutic 6-TGN (<235) and the preferential shunting towards excessive potentially hepatotoxic 6-MMP levels upon 6-MP/AZA dose escalation [30]. Individuals unmask this metabolic profile when they are challenged with higher doses of the drug. There is a small group of refractory patients who, despite therapeutic (>235) and often potentially toxic 6-TGN (>450) levels, are unable to benefit from the immunosuppressive properties of these therapies. The identification of these two subgroups early on the course of therapy can significantly improve patient outcomes by moving patients quickly to alternative immunomodulator therapy.
Conclusion
Genetic inheritance plays a significant role in determining inter-individual variability of drug response. The goal is for patients to be treated as individuals, with a therapeutic plan that identifies a patient’s specific needs. Pharmacogenetics does look promising as a tool to achieve this goal of truly individualized drug therapy. TPMT remains a key example of the translational potential of pharmacogenetics in the treatment of IBD [34, 35]. It appears that in the future pharmacogenetic studies will broaden its scope to include not only drug metabolism (pharmacokinetics) but also studies on drug targets (pharmacodynamics) [35]. Whole-genome approaches may improve the ability to characterize patient populations and better predict prognosis and drug response.
References
US Department of Health and Human Services Food and Drug Administratio. Center for Drug Evaluation and Research, Center for Biologics Evaluation and Research & Center for Devices and Radiological Health; 2003. www.fda.org.
Remy CN. Metabolism of thiopyrimidines and thiopurines. S-Methylation with S-adenosylmethionine transmethylase and catabolism in mammalian tissues. J Biol Chem. 1963;238:1078–84.
Lennard L. The clinical pharmacology of 6-Mercaptopurine. Eur J Clin Pharmacol. 1992;43:329–339.
Lennard L, Van Loon JA, Weinshilboum RM. Pharmacogenetics of acute azathioprine toxicity: relationship to thiopurine methyltransferase genetic polymorphism. Clin Pharmacol Ther. 1989;46:149–154.
Evans WE, Horner M, Chu YQ, Kalwinsky D, Roberts WM. Altered mercaptopurine metabolism, toxic effects, and dosage requirement in a thiopurine methyltransferase-deficient child with acute lymphocytic leukemia. J Pediatr. 1991;119:985–9.
Lennard L, Van Loon JA, Lilleyman JS, Weinshilboum RM. Thiopurine pharmacogenetics in leukemia: correlation of erythrocyte thiopurine methyltransferase activity and 6-thioguanine nucleotide concentrations. Clin Pharmacol Ther. 1987;41:18–25.
Weinshilboum RM, Sladek SL. Mercaptopurine Pharmacogenetics: Monogenic.inheritance of erythrocyte thiopurine methyltransferase activity. Am J Human Genet. 1980;32:651–62.
Van Loon JA, Weinshilboum RM. Thiopurine methyltransferase biochemical genetics: human lymphocyte activity. Biochem Genet. 1982;20:637–58.
Woodson LC, Dunnette JH, Weinshilboum RM. Pharmacogenetics of human thiopurine methyltransferase: kidney-erythrocyte correlation and immunotitration studies. J Pharmacol Exp Ther. 1982;222:174–81.
Szumlanski CL, Honchel R, Scott MC, Weinshilboum RM. Human liver thiopurine methyltransferase pharmacogenetics: biochemical properties, liver-erythrocyte correlation and presence of isozymes. Pharmacogenetics. 1992;2:148–59.
Coulthard SA, Howell C, Robson J, Hall AG. The relationship between thiopurine methyltransferase activity and genotype in blasts from patients with acute leukemia. Blood. 1998;92:2856–62.
Honchel R, Aksoy I, Szumlanski C, Wood TC, Otterness DM, Wieben ED, et al. Human thiopurine methyltransferase: molecular cloning and expression of T84 colon carcinoma cell cDNA. Mol Pharmacol. 1993;43:878–87.
Szumlanski C, Otterness D, Her C, Lee D, Brandriff B, Kelsell D, et al. Thiopurine methyltransferase pharmacogenetics: human gene cloning and characterization of a common polymorphism. DNA Cell Biol. 1996;15:17–30.
Tai H-L, Krynetski EY, Yates CR, Loennechen T, Fessing MY, Krynetskaia NF, et al. Thiopurine S-methyltransferase deficiency: two nucleotide transitions define the most prevalent mutant allele associated with loss of catalytic activity in Caucasians. Am J Hum Genet. 1996;58:694–702.
Salavaggione OE, Wang L, Wiepert M, Yee VC, Weinshilboum RM. Pharmacogenetics Thiopurine S-methyltransferase pharmacogenetics: variant allele functional and comparative genomics. Genomics. 2005;15:801–15.
Hon YY, Fessing MY, Pui CH, Relling MV, Krynetski EY, Evans WE. Polymorphism of the thiopurine S-methyltransferase gene in African-Americans. Hum Mol Genet. 1999;8:371–6.
Lee FJ, Kalow W. Thiopurine S methyltransferase activity in a Chinese population. Clin Pharmacol Ther. 1993;54:28–33.
Lennard L, Lilleyman JS, Van Loon J, Weinshilboum RM. Genetic variation in response to 6-mercaptopurine for childhood acute lymphoblastic leukaemia. Lancet. 1990;336:225–9.
Tai H-L, Fessing MY, Bonten EJ, Yanishevsky Y, d’Azzo A, Krynetski EY, et al. Enhanced proteasomal degradation of mutant human thiopurine S-methyltransferase TPMT) in mammalian cells: mechanism for TPMT protein deficiency inherited by TPMT*2, TPMT*3A, TPMT*3B or TPMT*3C. Pharmacogenetics. 1999;9:641–50.
Wang L, Sullivan W, Toft D, Weinshilboum R. Thiopurine S-methyltransferase pharmacogenetics: chaperone protein association and allozyme degradation. Pharmacogenetics. 2003;13:555–64.
Tiede I, Fritz G, Strand S, Poppe D, Dvorsky R, Strand D, et al. CD28-dependent Rac1 activation is the molecular target of azathioprine in primary human CD4+ T lymphocytes. J Clin Invest. 2003;111:1133–45.
Neurath MF, Kiesslich R, Teichgraber U, Fischer C, Hofmann U, Eichelbaum M, et al. 6-thioguanosine diphosphate and triphosphate levels in red blood cells and response to azathioprine therapy in Crohn’s disease. Clin Gastroenterol Hepatol. 2005;3:1007–14.
Dubinsky MC, Lamothe S, Yang HY, Targan SR, Sinnett D, Theoret Y, et al. Pharmacogenomics and metabolite measurement for 6-mercaptopurine therapy in inflammatory bowel disease. Gastroenterology. 2000;118:705–7.
Szumlanski CL, Weinshilboum RM. Sulphasalazine inhibition of thiopurine methyltransferase: possible mechanism for interaction with 6-mercaptopurine and azathioprine. Br J Clin Pharmacol. 1995;39:456–9.
Lewis LD, Benin A, Szumlanski CL, Otterness DM, Lennard L, Weinshilboum RM, et al. Olsalazine and 6-mercaptopurine-related bone marrow suppression: a possible drug-drug interaction. Clin Pharmacol Ther. 1997;62:464–75.
Dewitt O, Vanheuverzwyn R, Desager JP, Horsmans Y. Interaction between azathioprine and aminosalicylates: an in vivo study in patients with Crohn’s disease. Aliment Pharmacol Ther. 2002;16:79–85.
Colombel JF, Ferrari N, Debuysere H, Marteau P, Gendre JP, Bonaz B, et al. Genotypic analysis of thiopurine S-methyltransferase in patients with Crohn’s disease and severe myelosuppression during azathioprine therapy. Gastroenterology. 2000;118:1025–30.
Regueiro M, Mardini H. Determination of thiopurine methyltransferase genotype or phenotype optimizes initial dosing of azathioprine for the treatment of Crohn’s disease. J Clin Gastroenterol. 2002;35:240–4.
Campbell S, Kingstone K, Ghosh S. Relevance of thiopurine methyltransferase activity in inflammatory bowel disease patients maintained on low dose azathioprine. Aliment Pharmacol Ther. 2002;16:389–98.
Dubinsky MC, Hassard PV, Seidman EG, Kam LY, Abreu MT, Targan SR, et al. Preliminary evidence suggests that 6-MP metabolite profiles provide a biochemical explanation for 6-MP resistance in patients with inflammatory bowel disease. Gastroenterology. 2002;122:904–15.
Cuffari C, Théorêt Y, Latour S, Seidman EG. 6-mercaptopurine metabolism in Crohn’s disease: correlation with efficacy and toxicity. Gut. 1996;39:401–6.
Cuffari C, Hunt S, Bayless T. Utilization of erythrocyte 6-thioguanine metabolite levels to optimise azathioprine therapy in patients with inflammatory bowel disease. Gut. 2001;48:642–6.
Osterman MT, Kundu R, Lichtenstein GR, Lewis JD. Association of 6-thioguanine nucleotide levels and inflammatory bowel disease activity: a meta-analysis. Gastroenterology. 2006;130:47–53.
Weinshilboum R. Inheritance and drug response. New Engl J Med. 2003;348:529–37.
Weinshilboum R, Wang L. Pharmacogenomics: bench to bedside. Nat Rev Drug Disc. 2004;3:739–48.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2013 Springer Science+Business Media New York
About this chapter
Cite this chapter
Dubinsky, M.C. (2013). Pharmacogenetics in IBD. In: Mamula, P., Markowitz, J., Baldassano, R. (eds) Pediatric Inflammatory Bowel Disease. Springer, New York, NY. https://doi.org/10.1007/978-1-4614-5061-0_25
Download citation
DOI: https://doi.org/10.1007/978-1-4614-5061-0_25
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4614-5060-3
Online ISBN: 978-1-4614-5061-0
eBook Packages: MedicineMedicine (R0)