Abstract
Abnormal eating behaviors are overrepresented in the autism spectrum disorders, including food refusal, pica, rumination, and selective eating. Those disturbances can have detrimental complications and are often resistant to treatment. In autism spectrum disorders the background factors to eating disturbances are more complex than in the general child population, and sensory abnormalities, ritualistic behaviors, and social communication problems all seem to contribute. The eating problems in autism spectrum disorders may increase the risk for developing clinically significant eating disorders such as anorexia nervosa. Autistic traits must be considered in the treatment of the eating disorders and seem to be predictors for a poor psychosocial outcome after recovery from the eating disorder per se.
Access provided by Autonomous University of Puebla. Download reference work entry PDF
Similar content being viewed by others
Keywords
- Autism Spectrum Disorder
- Autism Spectrum Disorder
- Anorexia Nervosa
- Eating Disorder
- Intellectual Disability
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Introduction
Eating disturbances were included among the early descriptions of autism (Asperger 1944; Ritvo and Freeman 1978). Even though they are not included in the diagnostic DSM criteria for autism spectrum disorder (ASD), eating problems, such as feeding difficulties, pica, rumination, or overeating, are clinically important associated features in many cases of ASD (Rastam 2008).
In typically developing children, eating problems are common, affecting 20–40 %. In children with autism, eating problems are even more common affecting most children at some time (Kodak and Piazza 2008). In ASD they can also be more severe and tend to continue into adolescence and adulthood (Nicholls et al. 2001). Childhood “picky eating” and gastrointestinal problems have been linked to the development of teenage anorexia nervosa (AN) (Marchi and Cohen 1990; Rastam 1992). Marchi and Cohen also found problem meals and pica to be significant risk factors for bulimic symptoms. That research group later in a prospective epidemiological study of 800 children and their mothers looked at early childhood eating problems, including pica, and problems with meals. Some of the mealtime problems were related to future problems with anorectic or bulimic symptoms but pica was not (Kotler et al. 2001).
Problematic eating seems to be overrepresented in institutionalized patients with intellectual disability and to a less degree in individuals with intellectual disability living at home (Gravestock 2000; Hove 2004). Few studies of disordered eating in patients with intellectual disabilities include adults diagnosed with autism. Specific medical disorders and developmental disabilities, e.g., Prader-Willi syndrome, associated with specific eating behaviors are best described in the context of the respective syndrome and will not be dealt with in this chapter.
Disordered Eating in ASD
Rumination
Rumination involves repetitive regurgitation of ingested food, rechewing the food, and re-swallowing. Rumination is commonly believed to be an unconscious learned behavioral disorder involving voluntary relaxation of the diaphragm. A detailed story seems to be the best diagnostic tool according to a recent update on the rumination syndrome (Talley 2011). The author states that “pharmacologic therapy is of no value in these patients, as far as I am aware; antireflux therapy does not have an effect.” Further that “diaphragmatic rebreathing training teaches patients to relax their diaphragm during and after meals; because rumination cannot occur in this setting, it is eventually extinguished (unlearned).”
The rumination syndrome is believed to be rare but to be probably more common in autism especially in those with severe intellectual disabilities (Grewal and Fitzgerald 2002). However, rumination should be considered in the ASDs at all ages and at all levels of cognitive functioning (Parry-Jones 1994). A search for eating disorders (EDs) in eight volunteers with rumination found that in three women childhood rumination predated the development of bulimia nervosa (BN) (Eckern et al. 1999). Rumination may lead to weight loss, malnutrition, caries and erosion of the teeth enamel, and electrolyte abnormalities (Chial et al. 2003). Dental problems resulting in painful eating can lead to food refusal. Treatment studies have been done almost exclusively on those with intellectual disabilities. In a comprehensive review Lang and co-workers (Lang et al. 2011) report on 21 studies involving a total of 32 individuals. Only in eight of these 21 studies, individuals with diagnosed autism participated. The studied treatments of rumination include change of diet, most often by giving additional food, sensory-based intervention, e.g., teaching the patient to chew on a ring or gum, and socially based intervention, e.g., giving attention or verbal praise.
Pica
In pica nonedible substances are repeatedly consumed. The phenomenon has been linked to developmental disorders, particularly autism with intellectual disability, but has been described in ASD with normal intellectual abilities. Pica may be looked upon as an impulsive repetitive behavior in ASD that can be stress related or enhanced by boredom. The inedible object may give sensations from the mouth perceived as stimulating, or the mouthed object may in itself be a stimulant such as nicotine.
In 70 mostly adult patients, including 25 outpatients, with classic autism and intellectual disabilities, pica was described in 42 (60 %). They were compared to 70 individuals institutionalized because of Down’s syndrome. Only three in that group had pica, two cases with Down’s syndrome and autism and one with Down’s syndrome and probable schizophrenia (Kinnell 1985). In a study of 48 mentally handicapped adults living in community settings, deviant eating behavior was overrepresented in 15 adults with autism compared to 33 adults with no autism diagnosis (O’Brien and Whitehouse 1990). Only two cases with autism (and none in the other group) had pica. Thus, pica may be rare in autism outside of institutions, but when present it is potentially dangerous and not easy to treat. Pica can result in decreased appetite, gastrointestinal problems, melena, or poisoning with heavy metals (Geier and Geier 2006; Shannon and Graef 1996). In a study of children with classic autism, pica was found in one third (Raiten and Massaro 1986). Among reported complications were malnutrition, ulcers and bleeding from the mouth, esophagus, ventricle, and intestines, even intestinal perforation, and lead and nicotine poisoning.
In individuals within the autism spectrum, unwanted symptoms and behaviors are reduced in an autism-friendly milieu. Depression should be considered and treated. Studied interventions in pica have included to present interesting things to do, to eliminate stress, and to reward other activities (Piazza et al. 1998), and also positive reinforcement, e.g., snacks, increased activation, and praise and attention when the person is engaged in desirable behaviors (Smith 1987). Detecting the plausible cause for pica in a young man who ate cigarettes with nicotine, which has a proven stimulating effect on attention, nicotine cigarettes were replaced with cigarettes instead containing herbs, and the behavior stopped (Piazza et al. 1996).
Prescribed chelators have been used to try to remove tissue-bound heavy metals. A recent study of 17 individuals with autism, 12 of those with pica behavior (Soden et al. 2007), failed to show excess chelatable body burden of arsenic, mercury, lead, or cadmium (cadmium excretion rose marginally). In the case of ingestion of larger (or sharp) objects, surgical removal can be necessary (Rashid et al. 2010).
Overweight
Abnormal sensations of hunger and satiety as well as disordered eating seem to be common in ASD and entail the risk of over- or underweight. In a prospective study in the UK of very young children, despite abnormal feeding habits and a narrow food repertoire in the ASD group, BMI did not differ between 79 children with ASD and 12,901 controls at ages 18 months and at 7 years (Emond et al. 2010). In older children obesity seem to be more common. Using reported height and weight and the corresponding BMI from 46,707 subjects aged 10–17 years collected by the National Survey of Children’s Health (NSCH-2003), a study found the prevalence of obesity among children 10–17 years of age without a chronic condition to be 12.2 % compared to 23.4 % in children with autism. Obesity was defined as ≥95th percentile of the sex-specific BMI for age growth charts, adjusted for underlying demographic and socioeconomic factors (Chen et al. 2010). In adolescents with ASD in a tertiary care clinic in Boston, USA, overweight was significantly more common compared to a group with attention problems and to an age-matched reference population (Curtin et al. 2005). Only a small number of those with ASDs were on medication. In Canada 48 young adults (of 76 eligible) who had been diagnosed with autism as preschoolers participated with their families in a telephone interview at mean age 24 years. Twenty individuals (42 %) were overweight or obese (some of those were on medication), while two individuals were underweight (Eaves and Ho 2008). In adult psychiatry where medication is often used for stress-related behaviors with mood swings and aggressive outbursts, overweight is one of the most common adverse effects.
Eating Disturbances and Underweight in Asperger’s Disorder
Selective eating and extreme diets are common in Asperger’s disorder. An adolescent girl with changed eating habits and resulting weight loss would readily be recognized as AN. In teenage boys with Asperger’s disorder, eating abnormalities resulting in underweight tend to be overlooked. Distorted ideas about food can become obsessive/compulsive, resulting in weight loss, and, while not being typical for AN, may have the same consequences. An overrepresentation of low body weight has been shown in male adolescents with Asperger’s disorder associated with abnormal eating behaviors (Hebebrand et al. 1997; Sobanski et al. 1999) or in one study ascribed to hyperactivity (Bolte et al. 2002). A Danish study found BMI percentile of boys (but not girls) with ASD to be significantly reduced compared with matched BMI growth charts from the general population (Mouridsen et al. 2008). In adults with ASD and normal intelligence, health reasons are often the given explanation for vegetarianism and other special diets. Refusal of prescribed medicine except for vitamins and preference of complimentary herbal medications seem to be common in clinical practice.
Polydipsia
Polydipsia, to the point of dangerous water intoxication, presents a special problem in autism with intellectual disability (Terai et al. 1999). Polydipsia can be life threatening as serum sodium is diluted with a risk for seizures and cardiac arrest. Baseline weights must be established and correlated to serum sodium levels. Water intake may have to be monitored with a weight-water protocol.
Food Neophobia
One aspect of selective eating (see below) is food neophobia. The avoidance or refusal of new foods is overrepresented in ASD and generally in individuals wary of all new sensations and according to studies of twins in the general population in the UK seems to be a heritable trait (Cooke et al. 2007).
Selective Eating
Selective eating is one of the most common eating problems in ASD and can have detrimental effects on nutrition and general wellbeing. Selective eating if occurring in a child with ASD will often continue into adolescence and adult years but has only been studied in a structured way in children. In current taxonomies, selective eating is best placed as a “Feeding disorder of infancy and childhood” in the DSM system. Selective eating in children is extensively described in another chapter in this book.
Gastrointestinal Problems
In children with ASD a high rate of reported gastrointestinal symptoms compared to peers, in most cases with no known medical causes, were reported (Levy et al. 2007), including abnormal stool consistency (e.g., diarrhea in 20 % and constipation in 16 %). About 8 % of all children and 4 % of adults in the general population are allergic to some foods, presumably as many with ASD. Food allergies have been suspected to increase autistic behaviors in autism, leading to the recommendations of diverse diets (Cormier and Elder 2007). It has even been proposed that autism might be a disorder with abdominal features, but according to a recent review, studies are far from conclusive (Erickson et al. 2005). In a large prospective longitudinal study of over 800 children, parent-reported gastrointestinal problems attended by the health services during early childhood were not associated with self-reported autistic traits in young adulthood (Whitehouse et al. 2011).
In individuals with food, appetite, or weight problems, medical explanation must be considered (Buie et al. 2010). Diets free from gluten and casein have been advocated in autism but that has not been substantiated in research according to a recent Cochrane review (Millward et al. 2008). Neither has there been evidence in epidemiological studies for dietary supplementation (vitamins, minerals, or omega-3 fatty acids) in autism. There is some evidence for treatment with omega-3 fatty acids in ADHD, and dietary omega-3 fatty acids can be of use in those with ASD and ADHD combined.
Sensory Abnormalities
Problems with food and mealtime behaviors in individuals with ASDs have a multifactorial background, and sensory abnormalities with hyper- or hyposensitivity to auditory, visual, and tactile stimuli and to smell/taste play a large part. A prospective follow-up study of patients with autism found problems with sensory stimuli to be the most consistently impairing symptoms present from childhood up to age 30 years of age (Billstedt et al. 2007). Sensory sensitivity to food in ASD is extensively described elsewhere in this book.
One common problem in ASDs is to estimate quantity and size. Adults with ASDs prefer exact recipes and “standardized” food portions. An individual with Asperger’s disorder do not understand how many cookies to take when offered. He or she does not wipe his/her mouth when eating because of deficits in tactile sensitivity. The poor time estimation makes it difficult to eat in pace with others.
Interests and Routines
Restricted and intense ideas and interests can play a large part in eating difficulties in ASDs. Behaviors tend to be repetitive and the food repertoire narrow. There is often a lack of knowledge of nutrition and metabolism even in highly intelligent individuals. Some basic cooking training may help them to understand that feeding is not an exact science. Orthorexia nervosa is a fixation on healthy food to a degree when the individual gives up his/her normal life style (Bagci Bosi et al. 2007) and focuses on the quality of food. Some foods are thought to be dangerous or artificial as opposed to healthy or natural. The monomaniac pursuit of an interest in combination with a deficit in common sense could make this fixation particularly dangerous in individuals with ASD according to clinical reports.
Food rituals and routines can be damaging to social life in young people with otherwise some capacities for mixing with others. On the other hand routines can be beneficial, e.g., to have a fixed schedule for most meals.
Social Interaction at Mealtime
Eating with other people is an ordeal for many in the autism spectrum. To manage small talk, and at the same time chew and handle cutlery, requires the ability to perform at least two things simultaneously. Persons with ASD do not seem to pick up mealtime etiquette by observation the way children normally do. Social stories have been used in individual cases (Bledsoe et al. 2003) with some success after repeated practicing. Still, there is the problem in ASD to generalize from one situation to another. Young people with Asperger’s disorder sometimes prefer to study the complex etiquette involved in table manners in books. While it may be helpful for them to learn to use rules and routines around eating situations to their advantage, these same routines may feel like a strait jacket for family and friends.
Motor Problems
Motor problems are common in ASD, and clumsiness is overrepresented in adults with Asperger’s disorder (Tani et al. 2006). Taking the knife and fork in the “wrong” hand seems to be common, maybe because of left-right confusion or because of imitation problems. Oral motor dysfunction should be considered in selective eating with avoidance of food items that are difficult to chew or swallow or cause drooling. Oral motor therapy has shown effect alone or combined with applied behavior analysis in cases with autism comorbid with other medical conditions (Lang et al. 2011).
Eating Disorders in ASD
Social Communication Problems in Eating Disorders
Eating disorders according to the DSM-IV (APA 1994) encompass anorexia nervosa (AN), bulimia nervosa (BN), and eating disorder not otherwise specified (ED NOS). The prevalence of AN, BN, and ED NOS are 0.3–0.7 %, 1 %, and 3 %, respectively, in adolescent girls and young women (Hoek and van Hoeken 2003; Rastam et al. 1989). Prepubertal AN is rare and carries a worse prognosis. In contrast to ASD there is a huge overrepresentation of eating disorders (EDs) in females, with a gender ratio of 10:1–2 (Hoek and van Hoeken 2003). AN is characterized by a refusal to maintain weight at or above a minimally normal weight for age and height; an intense fear of gaining weight, even though underweight; body image distortion; and in postmenarcheal women amenorrhea (APA 1994). To assign a diagnosis of BN, the individual has to exhibit recurrent episodes of binge eating with a sense of lack of control over eating during the episode, recurrent inappropriate compensatory behavior (e.g., self-induced vomiting and misuse of laxatives) in order to prevent weight gain, and a self-evaluation, which is unduly influenced by body shape and weight. The binge eating and the inappropriate compensatory behavior must occur at least twice a week during a 3-month period (APA 1994). ED NOS is a generic for ED diagnoses and comprises subthreshold AN and BN. In addition ED NOS includes binge eating disorder (BED) that resembles BN regarding the binge eating symptomatology, but in BED no inappropriate compensatory behavior is present (APA 1994). Therefore there is a risk for individuals with BED to develop overweight and obesity (Fairburn et al. 2000).
Biological factors play an important role in the development of AN. Neurobiological studies of humans and animals suggest gender differences in body composition, activity levels, and responses to starvation and stress. Family and twin studies show genetic factors to be of great importance regarding the emergence of AN. First-degree relatives of individuals with AN have a tenfold increased risk to develop the ED themselves (Strober et al. 2000). According to a recent Swedish twin study the heritability for AN was 0.56 (Bulik et al. 2006). Individuals who later developed AN were more likely to have complications in the perinatal period (Cnattingius et al. 1999). The etiology of BN is believed to be less biologically loaded than AN and is preferably explained by psychosocial factors. For instance, the concordance of BN among mono- and dizygotic twins is similar, around 30 % in both groups. However, in many cases of BN there is a history of AN.
The psychiatric symptoms seen during AN illness are not pathognomonic for EDs. In the late 1940s an experiment was conducted on healthy males in the United States in order to study the psychological and physical consequences of semi-starvation for half a year, the “Minnesota Starvation Experiment.” Social withdrawal, depressed mood, preoccupation with food, decreased sexual interest, and attention deficits were observed among the males during semi-starvation in the experiment (Keys et al. 1950). These symptoms are also present during the acute phase of AN. Could the poor social functioning in AN be the consequence of the starvation or are there primary problems, before AN onset, with social communication? Several researchers have found problems with social withdrawal before AN onset, which have been described as separation anxiety disorders (Shoebridge and Gowers 2000), social phobia (Godart et al. 2000), ASDs (see the Gothenburg study below), and shyness (Fairburn et al. 1999). The social communication problems may be an important trigger mechanism for developing AN. In fact, one study found that the most common precipitating stressor of AN was severe difficulties interacting with close others (Schmidt et al. 1997). The social communication problems do not solely occur premorbidly and during the acute AN phase but remain after recovery (Anckarsater et al. 2011; Wentz et al. 2009).
The Coexistence of Autism Spectrum Disorders in Eating Disorders
A possible linkage between autism and AN was first suggested by Christopher Gillberg (1983) who described an overrepresentation of AN in close relatives of families with a child with autism.
The Autism Spectrum Quotient, AQ (Baron-Cohen et al. 2001), is a widely used instrument measuring autistic traits in individuals with normal intelligence. AQ has been administered in AN patients, who scored significantly higher than healthy controls both on total scores and on the subscales assessing social skills, attention switching, and imagination (Hambrook et al. 2008). In UK a study of 132 schoolchildren, 61 boys, found a significant relationship between self-reported eating disorder psychopathology and higher levels on AQ (Coombs et al. 2011).
In an 18-year follow-up study of teenage-onset AN (the Gothenburg study; see below), individuals who had at least once been assigned an ASD diagnosis scored significantly higher on all but one AQ subscale compared with a matched comparison group. Interestingly, individuals in the AN group who never had been assigned an ASD diagnosis also differed from the comparison group on the total AQ score and two subscales (attention switching and attention to detail) (Anckarsater et al. 2011).
Alexithymia in Eating Disorders
Alexithymia, which is an impaired ability to identify and describe emotional states, is found in individuals with ASD (Hill et al. 2004) and their close relatives (Szatmari et al. 2008). Higher levels of alexithymia have been identified in both individuals with AN and BN. In BN there are conflicting findings regarding the impact of coexisting depressive symptoms contributing to higher alexithymia scores (Parling et al. 2010; Speranza et al. 2007). Recovered AN individuals who exhibit elevated levels of alexithymia are preferably cases classified with an empathy disorder, in some cases fulfilling an ASD diagnosis (Rastam et al. 1997).
Males with Eating Disorders
Males with EDs are far less studied than females. They comprise a small minority, and the samples are often too small to render enough power in order to perform statistical analyses. The literature often mentions two categories of males with ED; one category that develop an ED in order to accomplish athletic achievements, and another category where the clinical representation resembles that in females. In recent years some studies have looked at sexual orientation and found an overrepresentation of asexual and homosexual males with AN and BN (Carlat et al. 1997; Muise et al. 2003). One study reported on premorbid traits in males with AN. Half the group had few or no friends, and a substantial minority was described as obsessive. Some were characterized as “meticulous,” “thorough,” “ruled by the clock,” or “always taking hobbies to extremes” (Sharp et al. 1994). These premorbid traits are similar to those seen in ASD. A Swedish register study compared 61 males adults born in 1968–1977 hospitalized because of AN at mean age 14.9 years to their age-matched peers in the general population (Lindblad et al. 2006). In adult years they significantly less often had a life involving a partner and children, which is in agreement with another controlled study of male AN (Woodside et al. 2001).
Neuropsychology in AN and BN: Similarities with ASD
Neuropsychological studies on EDs in the past two decades have increased the understanding of the underlying psychopathology of the EDs. Especially in terms of AN, the cognitive profile shows many similarities with ASD. Social communication is one area that can be impaired in EDs, AN in particular. Assessments of facial emotion recognition have shown that individuals with AN perform worse on these tasks compared with healthy controls (Harrison et al. 2010; Pollatos et al. 2008). Interestingly, one study showed that it was most problematic for individuals with AN to interpret neutral faces, which was confirmed by increased neuronal activity using visual evoked potentials (Pollatos et al. 2008). Preliminary findings indicate that impaired facial emotion recognition seems to persist after recovery from AN (Harrison et al. 2010). Legenbauer and co-workers found no difference between individuals with BN and healthy controls regarding recognition of facial emotion expression in general. The emotion “surprise” was the only expression that differed between the groups, showing an impairment in the individuals with BN (Legenbauer et al. 2008). Furthermore, the BN group had problems with emotional self-awareness, which was interpreted as “a cognitive-affective disturbance in emotion recognition.”
Not only visual emotion recognition is impaired in AN, but also reading emotions in voices has been found to be deviant in currently ill AN cases. However, this deficit seems to normalize after the individuals have recovered from their ED (Kucharska-Pietura et al. 2004). Social communication can also be impaired due to lack of facial expression, and one study has found individuals with AN to be less facially expressive than a healthy comparison group concerning positive affect but not negative affect, but that could be attributed to concurrent. depressive symptoms (Davies et al. 2011).
Kate Tchanturia, Janet Treasure, and co-workers have done pioneering work to increase the understanding of the cognitive style in EDs and similarities with ASD regarding flexibility, central coherence, and mentalizing. Flexibility is an executive function that can be assessed with set-shifting tests. Problems with flexibility are well known in ASD and have been repeatedly found in adults with current AN and after weight gain (Roberts et al. 2007; Tchanturia et al. 2004), as well as in other EDs, e.g., BN (Roberts et al. 2007). Interestingly, poor flexibility has also been noticed in healthy sisters of women with AN (Tenconi et al. 2010). Adolescents with AN did not differ from healthy controls regarding set shifting in one study (Shott et al. 2012). The different cognitive pattern in adolescents compared to adults with AN could be due to the more longstanding illness in adults with AN leading to a greater impact on the developing brain (Shott et al. 2012).
Central coherence is characterized by the ability to see the bigger picture as opposed to focusing on details. Weak central coherence is reported in AN both during current illness and after recovery, and also in BN. Sisters of individuals with AN have shown a similar cognitive pattern (Lopez et al. 2009; Tenconi et al. 2010).
Both poor flexibility and weak central coherence have been suggested as possible endophenotypes for EDs, AN in particular (Lopez et al. 2009; Tenconi et al. 2010). Problems with flexibility and central coherence can to some extent explain why AN individuals manage to adhere to a strict diet and are not able to realize the severity of the illness and its devastating consequences.
Theory of mind (ToM) or mentalizing has been explored in AN. Currently ill AN individuals perform significantly worse than healthy comparison cases regarding ToM tasks, e.g., Happé’s cartoon task (Tchanturia et al. 2004). However, divergent findings are reported concerning recovered AN individuals; one study showed normal performance (Oldershaw et al. 2010) and another study reported that long-term recovered AN individuals performed significantly worse than healthy matched controls regarding accuracy on Happé’s cartoon task (Gillberg et al. 2010).
Neuroimaging Correlates in AN
Neuroimaging studies in AN individuals have shown deviant patterns similar to findings in individuals with ASD. Råstam and colleagues (Rastam et al. 2001) used single-photon emission computed tomography (SPECT) to examine a group of females where the great majority had recovered from teenage-onset AN. Hypoperfusion was observed in the temporoparietal and orbitofrontal lobes. Another study found unilateral temporal hypoperfusion in currently ill children and adolescents with AN (Gordon et al. 1997). The hypoperfusion persisted in three individuals who were reassessed after weight gain. The areas affected in the two studies have also shown impaired perfusion in studies of autism (Ito et al. 2005). Controlled studies using functional magnetic resonance imaging (fMRI) in individuals with chronic AN and recovered individuals show reduced activity in rest and increased activity after food stimuli in prefrontal cortex and anterior cingulate cortex (Uher et al. 2003). Both these areas are also known for being engaged in processing theory of mind (Brune and Brune-Cohrs 2006).
The Gothenburg Study
The Gothenburg study is a prospective longitudinal community-based study of teenage-onset AN (Gillberg et al. 1995; Rastam et al. 1989; Wentz et al. 2001; Wentz et al. 2009), which has been reporting on the course of AN over a period of 18 years. The study was the first project in the ED area to investigate systematically the occurrence of autistic traits and ASD. The findings regarding the coexistence of ASD in AN will be described in detail here.
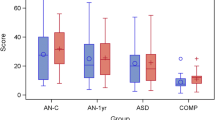
In an epidemiological study a total cohort born in 1970 and living in the city of Gothenburg in 1985 was screened for AN (Rastam 1992; Rastam et al. 1989). In all, there were 25 individuals (two boys) with AN born in 1970. One girl only participated in the screening phase leaving 24 individuals to constitute the population-based group. At the time of the epidemiological study, another 27 individuals (one boy) with AN born in the adjacent years and living in Gothenburg were referred to the study, in most cases by the school nurses. The population-based group and the referred group were compared and found to be similar in almost all aspects other than treatment received. The two groups were pooled together in order to constitute the total AN group consisting of 51 individuals with AN (48 girls and three boys) according to criteria in the DSM-III-R (APA 1987) and the DSM-IV (APA 1994). The school nurses in Gothenburg were asked to select comparison cases without any suspicion of eating problems matched for age, gender, and school (COMP group). The COMP group also consisted of 51 individuals, 48 girls and three boys. The AN and the COMP group have been examined at four occasions starting at mean age 16 years, and with follow-up studies at ages 21, 24, and 32 years.
At all four examinations a rater blinded to group status has assigned autism spectrum diagnoses. At the time of the first examination at mean age 16 years (AN Study 1), all mothers took part in an in-depth interview regarding, among other things, early development, premorbid symptomatology concerning temperament, personality, and mental symptoms. On the basis of de-identified case notes concerning premorbid history, a blinded rater assigned diagnoses of ASD (Rastam 1992). In each follow-up study, when only three individuals had persisting underweight, a new blinded rater assigned ASD diagnoses after personal interview. In Table 1 the instruments used in order to assign ASD diagnoses are shown. In AN Study 3 an instrument for early detection of autistic symptoms in infants was used in those individuals who had become parents. The instrument, CHecklist for Autism in Toddlers, CHAT (Baron-Cohen et al. 1992), has been widely used for autism screening purposes and should preferably be used when the child is 18 months old.
The interviews with the mothers revealed a significant overrepresentation of an early history of extreme feeding problems, severe stomach ache, or other severe gastrointestinal problems causing inpatient treatment in the AN group, affecting half the group (Rastam 1992). Early feeding problems have been put forward (Gillberg 2010) to be one of the first symptoms of ESSENCE (Early Symptomatic Syndromes Eliciting Neurodevelopmental Clinical Examinations) which in turn can develop into a neurodevelopmental disorder such as ASD, ADHD, and speech and language disorder. Based on the retrospective semi-structured interviews with the mothers, the researchers found that obsessionality, poor social skills, and even autistic traits had been present in half the AN group from childhood. Before the study none had been suspected with an ASD diagnosis. The mothers gave descriptions of how their children had distinguished themselves from their peers; they had “poor social interaction with peers,” they tended to be dependent on only one friend that they used as a role model, they were dependent upon “rules, routines, and rituals,” and they were described as “perfectionistic and overambitious,” “stubborn,” having “unusual interests,” had been “unaware of other people’s perspectives,” and had problems with separation anxiety. The family history interview with the mothers in AN Study 1 and with the probands in AN Study 2 showed an overrepresentation of poor social skills in first-degree relatives of individuals in the AN group (Nilsson et al. 1998).
Alexithymia was examined by using Toronto Alexithymia Scale (TAS-20) in AN Study 2 (Rastam et al. 1997). The individuals classified with ASD in AN Study 2 were all among the high scorers of the TAS.
Neuropsychological assessments were administered for the first time in AN Study 2 (Gillberg et al. 1996) when the majority had recovered from AN. The Wechsler scales were used in order to assess intelligence. The AN group did not differ from the COMP group in respect of full scale IQ, but they performed significantly worse on the object assembly subtest. This subtest measures the ability of global processing as opposed to attention to details. The finding was highlighted by the researchers who pointed out the resemblance between this neuropsychological pattern and the one seen in ASD. In AN Study 3, when 10 years had elapsed from AN onset (Gillberg et al. 2007), the AN group showed persisting difficulties with central coherence, and a subgroup classified with ASD had test profiles similar to those found in individuals with high-functioning ASD. In AN Study 4 (Gillberg et al. 2010), 18 years after AN onset, the AN group performed the Tower of London, a test measuring executive functions with a significantly lower speed compared with the COMP group. In order to assess theory of mind, Happé’s mental cartoons were used. The AN group had significantly lower scores regarding accuracy on this test. The scores correlated with psychosocial functioning according to the Global Assessment of Functioning (GAF) of the DSM-IV (APA 1994).
Altogether 16 individuals (32 %) in the AN group had been assigned an ASD diagnosis in at least one of the four studies by a blinded rater (Anckarsater et al. 2011). No individual in the COMP group had been assigned an ASD diagnosis. Two women were omitted, one in the AN and one in the COMP group as their social interaction problems had clear adult-age exogenous causes. One in four in the total AN group had no paid employment due to their ED and/or other psychiatric problems compared with 2 % in the COMP group. Six individuals (12 %) in the AN group had at all four examinations been classified as having ASD, including retrospective history of childhood ASD. Autistic traits premorbidly or in AN Study 2 predicted poor psychosocial outcome at 18-year follow-up (Wentz et al. 2009).
The St. George’s Study, London
In 2002 a study was conducted on chronic ED patients at St. George’s Hospital Medical School in London (Wentz et al. 2005). The aim of the study was to investigate the occurrence of ASD, ADHD, Tourette’s disorder, and other tic disorders in this population. Altogether 30 patients, 21 inpatients and nine outpatients, all tertial referrals, were investigated at mean age 27 years. The majority had AN, 21 women, and nine women had BN. The mean age at current ED onset was 18 years and the average duration of the current ED was 9.5 years. Asperger Syndrome Diagnostic Interview (Gillberg et al. 2001), Checklist for autistic disorder (APA 1994) and Asperger’s syndrome were used to assign diagnoses of ASD. ADHD-RS was used to assess ADHD symptomatology. A checklist for tics and Tourette’s disorder and the Structured Clinical Interview for DSM-IV for Axis II Personality Disorders (SCID-II), a semi-structured interview pertaining to personality disorders, were included.
Among the women with chronic AN one in three had ASD, and one in four had had ADHD during childhood (in three cases they also fulfilled a diagnosis of ADHD in adulthood) (see Table 2). Tourette’s disorder and other chronic tic disorders occurred in both the AN and the BN group (see Table 2). Two individuals had Tourette’s disorder and both of them belonged to the BN group.
Gender and Age: Assessment Problems
Most ED studies have not presented gender-specific results, mostly because of small study samples or exclusion of males. Psychometric tools and outcome criteria used in the EDs have mainly been validated for females only. The finding that the EDs, especially AN, and the ASDs may share personality traits and cognitive style suggests that we miss individuals with EDs who do not conform to the female prototype of AN. Autistic traits in girls with AN is overlooked in the same way as EDs are not recognized in obsessive young males with abnormal eating.
There is a lack of criteria and instruments for assessing deviant eating behavior and mealtime problems in adolescents and adults with ASD and normal intelligence. For this purpose our group has developed a web-based self-report questionnaire, The Swedish Eating Assessment for Autism spectrum disorders, SWEAA. The instrument has been validated from age 15 years and older (Karlsson et al. 2013).
Key Terms
-
Alexithymia. An impaired ability to identify and describe emotional states.
-
Anorexia nervosa. Weight loss by self-starvation and exercise that does not diminish even when the person is sickly underweight.
-
Bulimia nervosa. Repeated binge eating followed by compensatory behaviors to avoid weight gain.
-
Orthorexia nervosa. Correct appetite, meaning an obsession with so-called healthy eating which can lead to an unbalanced diet and malnutrition.
-
Pica. Eating nonedible substances.
-
Rumination. Repetitive regurgitation of ingested food, rechewing the food, and re-swallowing.
-
Set-shifting. An executive function assessing flexibility.
Key Facts of Autism Spectrum Disorders and Eating Problems/Disorders
-
Aberrant eating habits are overrepresented in autism spectrum disorders.
-
In autism spectrum disorders, studies and clinical experience indicate a continuance of eating problems into adolescence and adult age but research is scant.
-
Overweight and obesity are common in autism spectrum disorders, seemingly not in small children, but increasingly prevalent from school age.
-
Individuals with eating disorders, anorexia nervosa in particular, exhibit limited capacity to interpret nonverbal communication.
-
Problems with social communication occur premorbidly both during illness and after recovery in anorexia nervosa.
-
In eating disorders, especially anorexia nervosa, deficits in executive function and mentalizing, similar to those in autism spectrum disorders, are overrepresented even after recovery from the eating disorder per se.
-
Autism spectrum disorders are overrepresented in individuals who develop anorexia nervosa.
-
Autism spectrum disorders are common in chronic cases of anorexia nervosa.
Summary Points
-
Disordered eating occurs in the majority of cases with autism spectrum disorders and lead to severe complications for mental and somatic health but is often not diagnosed or indeed assessed.
-
Aberrant eating habits seem to be only one of many ritualistic behaviors in children with Asperger’s disorder and some of these will persist in their eating patterns in adolescence and adulthood.
-
Assessment of predisposing factors of eating disturbances is necessary to find appropriate interventions.
-
Anorexia nervosa is associated with a range of neuropsychological problems similar to those in the autism spectrum disorders, which are present long after the eating disorder per se is no longer an issue.
-
Some autistic features in anorexia nervosa may be a cognitive style, not deficit. The cognitive style is characterized by limited flexibility, weak central coherence, and mentalizing problems.
-
Some individuals who develop anorexia nervosa meet criteria for autism spectrum disorders. They may represent the extreme of neurocognitive and personality problems to be found more generally in anorexia nervosa.
-
Clinicians must be aware of the neurocognitive problems in anorexia nervosa in order to provide adequate treatment.
References
Anckarsater H, Hofvander B, Billstedt E, et al. The sociocommunicative deficit subgroup in anorexia nervosa: autism spectrum disorders and neurocognition in a community-based, longitudinal study. Psychol Med. 2011;42:1–11.
APA. Diagnostic and statistical manual of mental disorders, 3rd edition revised (DSM-III-R). Washington, DC: American Psychiatric Press; 1987.
APA. Diagnostic and statistical manual of mental disorders, 4th edition (DSM-IV). Washington, DC: American Psychiatric Press; 1994.
Asperger H. Die ‘autistischen psychopathen’ im kindesalter. Arch Psychiatr Nervenkr. 1944;117:76–136.
Bagci Bosi A, Camur D, Güler C. Prevalence of orthorexia nervosa in resident medical doctors in the faculty of medicine (Ankara, Turkey). Appetite. 2007;49:661–6.
Baron-Cohen S, Allen J, Gillberg C. Can autism be detected at 18 months? The needle, the haystack, and the CHAT. Br J Psychiatry. 1992;161:839–43.
Baron-Cohen S, Wheelwright S, Skinner R, et al. The autism-spectrum quotient (AQ): evidence from Asperger syndrome/high-functioning autism, males and females, scientists and mathematicians. J Autism Dev Disord. 2001;31:5–17.
Billstedt E, Gillberg IC, Gillberg C. Autism in adults: symptom patterns and early childhood predictors. Use of the DISCO in a community sample followed from childhood. J Child Psychol Psychiatry. 2007;48:1102–10.
Bledsoe R, Myles BS, Simpson RL. Use of a social story intervention to improve mealtime skills of an adolescent with Asperger syndrome. Autism. 2003;7:289–95.
Bolte S, Ozkara N, Poustka F. Autism spectrum disorders and low body weight: is there really a systematic association? Int J Eat Disord. 2002;31:349–51.
Brune M, Brune-Cohrs U. Theory of mind – evolution, ontogeny, brain mechanisms and psychopathology. Neurosci Biobehav Rev. 2006;30:437–55.
Buie T, Campbell DB, Fuchs 3rd GJ, et al. Evaluation, diagnosis, and treatment of gastrointestinal disorders in individuals with ASDs: a consensus report. Pediatrics. 2010;125 Suppl 1:S1–18.
Bulik CM, Sullivan PF, Tozzi F, et al. Prevalence, heritability, and prospective risk factors for anorexia nervosa. Arch Gen Psychiatry. 2006;63:305–12.
Carlat DJ, Camargo Jr CA, Herzog DB. Eating disorders in males: a report on 135 patients. Am J Psychiatry. 1997;154:1127–32.
Chen AY, Kim SE, Houtrow AJ, et al. Prevalence of obesity among children with chronic conditions. Obesity (Silver Spring). 2010;18:210–3.
Chial HJ, Camilleri M, Williams DE, et al. Rumination syndrome in children and adolescents: diagnosis, treatment, and prognosis. Pediatrics. 2003;111:158–62.
Cnattingius S, Hultman CM, Dahl M, Sparen P. Very preterm birth, birth trauma, and the risk of anorexia nervosa among girls. Arch Gen Psychiatry. 1999;56(7):634–8.
Cooke LJ, Haworth CM, Wardle J. Genetic and environmental influences on children’s food neophobia. Am J Clin Nutr. 2007;86:428–33.
Coombs E, Brosnan M, Bryant-Waugh R, et al. An investigation into the relationship between eating disorder psychopathology and autistic symptomatology in a non-clinical sample. Br J Clin Psychol. 2011;50:326–38.
Cormier E, Elder JH. Diet and child behavior problems: fact or fiction? Pediatr Nurs. 2007;33:138–43.
Curtin C, Bandini LG, Perrin EC, et al. Prevalence of overweight in children and adolescents with attention deficit hyperactivity disorder and autism spectrum disorders: a chart review. BMC Pediatr. 2005;5:48.
Davies H, Schmidt U, Stahl D, et al. Evoked facial emotional expression and emotional experience in people with anorexia nervosa. Int J Eat Disord. 2011;44:531–9.
Dewey M. Living with Asperger’s syndrome. In: Frith U, editor. Autism and Asperger syndrome. Cambridge, England: Cambridge University Press; 1991. p. 184–206.
Eaves LC, Ho HH. Young adult outcome of autism spectrum disorders. J Autism Dev Disord. 2008;38:739–47.
Eckern M, Stevens W, Mitchell J. The relationship between rumination and eating disorders. Int J Eat Disord. 1999;26:414–9.
Emond A, Emmett P, Steer C, et al. Feeding symptoms, dietary patterns, and growth in young children with autism spectrum disorders. Pediatrics. 2010;126:e337–42.
Erickson CA, Stigler KA, Corkins MR, et al. Gastrointestinal factors in autistic disorder: a critical review. J Autism Dev Disord. 2005;35:713–27.
Fairburn CG, Cooper Z, Doll HA, et al. The natural course of bulimia nervosa and binge eating disorder in young women. Arch Gen Psychiatry. 2000;57:659–65.
Fairburn CG, Cooper Z, Doll HA, et al. Risk factors for anorexia nervosa: three integrated case-control comparisons. Arch Gen Psychiatry. 1999;56:468–76.
Geier DA, Geier MR. A prospective assessment of porphyrins in autistic disorders: a potential marker for heavy metal exposure. Neurotox Res. 2006;10:57–64.
Gillberg C. Are autism and anorexia nervosa related? Br J Psychiatry. 1983;142:428.
Gillberg C. The essence in child psychiatry: early symptomatic syndromes eliciting neurodevelopmental clinical examinations. Res Dev Disabil. 2010;31:1543–51.
Gillberg C, Rastam M, Wentz E. The Asperger Syndrome (and high-functioning autism) Diagnostic Interview (ASDI): a preliminary study of a new structured clinical interview. Autism. 2001;5:57–66.
Gillberg IC, Billstedt E, Wentz E, et al. Attention, executive functions, and mentalizing in anorexia nervosa eighteen years after onset of eating disorder. J Clin Exp Neuropsychol. 2010;32:358–65.
Gillberg IC, Gillberg C. Asperger syndrome – some epidemiological considerations: a research note. J Child Psychol Psychiatry. 1989;30:631–8.
Gillberg IC, Gillberg C, Rastam M, et al. The cognitive profile of anorexia nervosa: a comparative study including a community-based sample. Compr Psychiatry. 1996;37:23–30.
Gillberg IC, Rastam M, Gillberg C. Anorexia nervosa 6 years after onset: part I. Personality disorders. Compr Psychiatry. 1995;36:61–9.
Gillberg IC, Rastam M, Wentz E, et al. Cognitive and executive functions in anorexia nervosa ten years after onset of eating disorder. J Clin Exp Neuropsychol. 2007;29:170–8.
Godart NT, Flament MF, Lecrubier Y, et al. Anxiety disorders in anorexia nervosa and bulimia nervosa: co-morbidity and chronology of appearance. Eur Psychiatry. 2000;15:38–45.
Gordon I, Lask B, Bryant-Waugh R, et al. Childhood-onset anorexia nervosa: towards identifying a biological substrate. Int J Eat Disord. 1997;22:159–65.
Gravestock S. Eating disorders in adults with intellectual disability. J Intellect Disabil Res. 2000;44(Pt 6):625–37.
Grewal P, Fitzgerald B. Pica with learning disability. J R Soc Med. 2002;95:39–40.
Hambrook D, Tchanturia K, Schmidt U, et al. Empathy, systemizing, and autistic traits in anorexia nervosa: a pilot study. Br J Clin Psychol. 2008;47:335–9.
Harrison A, Tchanturia K, Treasure J. Attentional bias, emotion recognition, and emotion regulation in anorexia: state or trait? Biol Psychiatry. 2010;68:755–61.
Hebebrand J, Henninghausen K, Nau S, et al. Low body weight in male children and adolescents with schizoid personality disorder or Asperger’s disorder. Acta Psychiatr Scand. 1997;96:64–7.
Hill E, Berthoz S, Frith U. Brief report: cognitive processing of own emotions in individuals with autistic spectrum disorder and in their relatives. J Autism Dev Disord. 2004;34:229–35.
Hoek HW, van Hoeken D. Review of the prevalence and incidence of eating disorders. Int J Eat Disord. 2003;34:383–96.
Hove O. Prevalence of eating disorders in adults with mental retardation living in the community. Am J Ment Retard. 2004;109:501–6.
Ito H, Mori K, Hashimoto T, et al. Findings of brain 99mTc-ECD SPECT in high-functioning autism – 3-dimensional stereotactic ROI template analysis of brain SPECT. J Med Invest. 2005;52:49–56.
Karlsson L, Rastam M, Wentz E. The SWedish Eating Assessment for Autism spectrum disorders (SWEAA)-Validation of a self-report questionnaire targeting eating disturbances within the autism spectrum. Res Dev Disabil. 2013;34(7):2224–33.
Keys A, Brozek J, Henschel A, et al. The biology of human starvation. Minneapolis: University of Minnesota Press; 1950.
Kinnell HG. Pica as a feature of autism. Br J Psychiatry. 1985;147:80–2.
Kodak T, Piazza CC. Assessment and behavioral treatment of feeding and sleeping disorders in children with autism spectrum disorders. Child Adolesc Psychiatr Clin N Am. 2008;17:887–905. x-xi.
Kotler LA, Cohen P, Davies M, et al. Longitudinal relationships between childhood, adolescent, and adult eating disorders. J Am Acad Child Adolesc Psychiatry. 2001;40:1434–40.
Kucharska-Pietura K, Nikolaou V, Masiak M, et al. The recognition of emotion in the faces and voice of anorexia nervosa. Int J Eat Disord. 2004;35:42–7.
Lang R, Mulloy A, Giesbers S, et al. Behavioral interventions for rumination and operant vomiting in individuals with intellectual disabilities: a systematic review. Res Dev Disabil. 2011;32:2193–205.
Legenbauer T, Vocks S, Ruddel H. Emotion recognition, emotional awareness and cognitive bias in individuals with bulimia nervosa. J Clin Psychol. 2008;64:687–702.
Levy SE, Souders MC, Ittenbach RF, et al. Relationship of dietary intake to gastrointestinal symptoms in children with autistic spectrum disorders. Biol Psychiatry. 2007;61:492–7.
Lindblad F, Lindberg L, Hjern A. Anorexia nervosa in young men: a cohort study. Int J Eat Disord. 2006;39:662–6.
Lopez C, Tchanturia K, Stahl D, et al. Weak central coherence in eating disorders: a step towards looking for an endophenotype of eating disorders. J Clin Exp Neuropsychol. 2009;31:117–25.
Marchi M, Cohen P. Early childhood eating behaviors and adolescent eating disorders. J Am Acad Child Adolesc Psychiatry. 1990;29:112–7.
Millward C, Ferriter M, Calver S, et al. Gluten- and casein-free diets for autistic spectrum disorder. Cochrane Database Syst Rev. 2008;16:CD003498.
Mouridsen SE, Rich B, Isager T. Body mass index in male and female children with pervasive developmental disorders. Pediatr Int. 2008;50:569–71.
Muise AM, Stein DG, Arbess G. Eating disorders in adolescent boys: a review of the adolescent and young adult literature. J Adolesc Health. 2003;33:427–35.
Nicholls D, Christie D, Randall L, et al. Selective eating: symptom, disorder or normal variant. Clin Child Psychol Psychiatry. 2001;6:257–70.
Nilsson EW, Gillberg C, Rastam M. Familial factors in anorexia nervosa: a community-based study. Compr Psychiatry. 1998;39:392–9.
O’Brien G, Whitehouse AM. A psychiatric study of deviant eating behaviour among mentally handicapped adults. Br J Psychiatry. 1990;157:281–4.
Oldershaw A, Hambrook D, Tchanturia K, et al. Emotional theory of mind and emotional awareness in recovered anorexia nervosa patients. Psychosom Med. 2010;72:73–9.
Parling T, Mortazavi M, Ghaderi A. Alexithymia and emotional awareness in anorexia nervosa: time for a shift in the measurement of the concept? Eat Behav. 2010;11:205–10.
Parry-Jones B. Merycism or rumination disorder. A historical investigation and current assessment. Br J Psychiatry. 1994;165:303–14.
Piazza CC, Fisher WW, Hanley GP, et al. Treatment of pica through multiple analyses of its reinforcing functions. J Appl Behav Anal. 1998;31:165–89.
Piazza CC, Hanley GP, Fisher WW. Functional analysis and treatment of cigarette pica. J Appl Behav Anal. 1996;29:437–49. quiz 449–450.
Pollatos O, Herbert BM, Schandry R, et al. Impaired central processing of emotional faces in anorexia nervosa. Psychosom Med. 2008;70:701–8.
Raiten DJ, Massaro T. Perspectives on the nutritional ecology of autistic children. J Autism Dev Disord. 1986;16:133–43.
Rashid F, Davies L, Iftikhar SY. Magnetised intragastric foreign body collection and autism: an advice for carers and literature review. Autism. 2010;14:139–45.
Rastam M. Anorexia nervosa in 51 Swedish adolescents: premorbid problems and comorbidity. J Am Acad Child Adolesc Psychiatry. 1992;31:819–29.
Rastam M. Eating disturbances in autism spectrum disorders with focus on adolescent and adult years. Clin Neuropsychiatry. 2008;5:31–42.
Rastam M, Bjure J, Vestergren E, et al. Regional cerebral blood flow in weight-restored anorexia nervosa: a preliminary study. Dev Med Child Neurol. 2001;43:239–42.
Rastam M, Gillberg C, Garton M. Anorexia nervosa in a Swedish urban region. A population-based study. Br J Psychiatry. 1989;155:642–6.
Rastam M, Gillberg C, Gillberg IC, et al. Alexithymia in anorexia nervosa: a controlled study using the 20-item Toronto Alexithymia scale. Acta Psychiatr Scand. 1997;95:385–8.
Ritvo ER, Freeman BJ. Current research on the syndrome of autism: introduction. The national society for autistic children’s definition of the syndrome of autism. J Am Acad Child Psychiatry. 1978;17:565–75.
Roberts ME, Tchanturia K, Stahl D, et al. A systematic review and meta-analysis of set-shifting ability in eating disorders. Psychol Med. 2007;37:1075–84.
Schmidt U, Tiller J, Blanchard M, et al. Is there a specific trauma precipitating anorexia nervosa? Psychol Med. 1997;27:523–30.
Shannon M, Graef JW. Lead intoxication in children with pervasive developmental disorders. J Toxicol Clin Toxicol. 1996;34:177–81.
Sharp CW, Clark SA, Dunan JR, et al. Clinical presentation of anorexia nervosa in males: 24 new cases. Int J Eat Disord. 1994;15:125–34.
Shoebridge P, Gowers SG. Parental high concern and adolescent-onset anorexia nervosa. A case-control study to investigate direction of causality. Br J Psychiatry. 2000;176:132–7.
Shott ME, Filoteo JV, Bhatnagar KA, et al. Cognitive set-shifting in anorexia nervosa. Eur Eat Disord Rev. 2012;20(5):343–9.
Smith MD. Treatment of pica in an adult disabled by autism by differential reinforcement of incompatible behavior. J Behav Ther Exp Psychiatry. 1987;18:285–8.
Sobanski E, Marcus A, Hennighausen K, et al. Further evidence for a low body weight in male children and adolescents with Asperger’s disorder. Eur Child Adolesc Psychiatry. 1999;8:312–4.
Soden SE, Lowry JA, Garrison CB, et al. 24-hour provoked urine excretion test for heavy metals in children with autism and typically developing controls, a pilot study. Clin Toxicol (Phila). 2007;45:476–81.
Speranza M, Loas G, Wallier J, et al. Predictive value of alexithymia in patients with eating disorders: a 3-year prospective study. J Psychosom Res. 2007;63:365–71.
Strober M, Freeman R, Lampert C, et al. Controlled family study of anorexia nervosa and bulimia nervosa: evidence of shared liability and transmission of partial syndromes. Am J Psychiatry. 2000;157:393–401.
Szatmari P, Georgiades S, Duku E, et al. Alexithymia in parents of children with autism spectrum disorder. J Autism Dev Disord. 2008;38:1859–65.
Talley NJ. Rumination syndrome. Gastroenterol Hepatol (N Y). 2011;7:117–8.
Tani P, Lindberg N, Appelberg B, et al. Clinical neurological abnormalities in young adults with Asperger syndrome. Psychiatry Clin Neurosci. 2006;60:253–5.
Tchanturia K, Morris RG, Anderluh MB, et al. Set shifting in anorexia nervosa: an examination before and after weight gain, in full recovery and relationship to childhood and adult OCPD traits. J Psychiatr Res. 2004;38:545–52.
Tenconi E, Santonastaso P, Degortes D, et al. Set-shifting abilities, central coherence, and handedness in anorexia nervosa patients, their unaffected siblings and healthy controls: exploring putative endophenotypes. World J Biol Psychiatry. 2010;11:813–23.
Terai K, Munesue T, Hiratani M. Excessive water drinking behavior in autism. Brain Dev. 1999;21:103–6.
Uher R, Brammer MJ, Murphy T, et al. Recovery and chronicity in anorexia nervosa: brain activity associated with differential outcomes. Biol Psychiatry. 2003;54:934–42.
Wentz E, Gillberg C, Gillberg IC, et al. Ten-year follow-up of adolescent-onset anorexia nervosa: psychiatric disorders and overall functioning scales. J Child Psychol Psychiatry. 2001;42:613–22.
Wentz E, Gillberg IC, Anckarsater H, et al. Adolescent-onset anorexia nervosa: 18-year outcome. Br J Psychiatry. 2009;194:168–74.
Wentz E, Lacey JH, Waller G, et al. Childhood onset neuropsychiatric disorders in adult eating disorder patients. A pilot study. Eur Child Adolesc Psychiatry. 2005;14:431–7.
Whitehouse AJ, Maybery M, Wray JA, et al. No association between early gastrointestinal problems and autistic-like traits in the general population. Dev Med Child Neurol. 2011;53:457–62.
Woodside DB, Garfinkel PE, Lin E, et al. Comparisons of men with full or partial eating disorders, men without eating disorders, and women with eating disorders in the community. Am J Psychiatry. 2001;158:570–4.
Author information
Authors and Affiliations
Corresponding authors
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer Science+Business Media New York
About this entry
Cite this entry
Rastam, M., Wentz, E. (2014). ASD, Eating Problems, and Overlap with Anorexia and Bulimia Nervosa. In: Patel, V., Preedy, V., Martin, C. (eds) Comprehensive Guide to Autism. Springer, New York, NY. https://doi.org/10.1007/978-1-4614-4788-7_121
Download citation
DOI: https://doi.org/10.1007/978-1-4614-4788-7_121
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4614-4787-0
Online ISBN: 978-1-4614-4788-7
eBook Packages: Behavioral ScienceReference Module Humanities and Social SciencesReference Module Business, Economics and Social Sciences