Abstract
Globally, malaria remains a substantial public health burden with an estimated 349–552 million clinical cases of P. falciparum malaria each year—leading to 780,000 deaths directly attributable to the disease. Whilst the outcome from severe malaria in Africa children remains poor, recent developments in the management of malaria have come from two key sources—the introduction of new, safe and rapidly-effective anti-malarials and high quality evidence from two of the largest clinical trials ever conducted in African children with severe malaria. As a result, the time-honoured anti-malarial treatment for severe malaria, quinine, will now be replaced by artesunate, a water-soluble artemisinin derivative. Supportive care, specifically the management of shock, has been informed by a large late phase clinical trial which concluded that bolus resuscitation is harmful and therefore should be avoided in children with severe malaria, including the high risk group with severe metabolic acidosis and advanced shock.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
20.1 Background
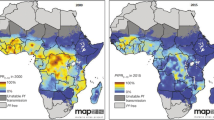
Of the five species of malaria that infect humans, Plasmodium falciparum causes most severe and fatal disease in the tropics. In recent years, Plasmodium vivax has been also been described as causing severe and complicated malaria in Asia [1]. Globally, the most reliable recent estimate indicates that there were 349–552 million clinical cases of P. falciparum malaria in 2007 [2], with up to 7,80,000 deaths directly attributable to the disease [3]. The burden and spectrum of malaria varies from one geographical region to another, with intensity of transmission and between adults and children. There have been some encouraging reports of declining malaria incidence, but these relate to selected areas and may not reflect the general situation [4]. Better malaria control, early diagnosis and improved drug treatment may each contribute to changing malaria epidemiology but overall trends are not yet comprehensively understood. In areas with high malaria transmission, incidence has not changed and in some areas increases in disease burden have been reported [5, 6].
Prompt diagnosis and treatment is crucial to prevent mortality especially in high-risk groups including young children and some visitors, who have little or no immunity. Travellers, of any age, from non-endemic areas are particularly at risk, including those formerly from endemic areas and returning for short or long visits to their home or other endemic areas, because naturally-acquired immunity wanes rapidly. In the past decade there have been substantial therapeutic advances in the management of both mild and severe disease, with newer drugs, in particular artemisinin based combinations replacing time-honoured chloroquine and quinine. These developments are welcome as parasite resistance to malaria treatments continues to threaten malaria control and effective case management globally. This chapter focuses on the management of severe malaria with specific reference to the latest developments in treatment.
In 2010 and 2011, two of the largest clinical trials ever conducted in African children with severe malaria were published, both with groundbreaking results [7, 8]. Most of the latter part of this chapter is dedicated to discussing these trials. Both manuscripts are openly accessible on-line and we recommend that readers refer to these manuscripts as necessary. By way of introduction and to put into to context the relevance of the trials to the clinical management of paediatric malaria in Africa and, by extrapolation, to the management of children in the UK, we first describe the clinical spectrum of severe malaria.
20.2 What Defines Severe Malaria?
For decades severe malaria in African children had been rationalised into two non-over-lapping major syndromic presentations, those of cerebral malaria and severe malarial anaemia [9, 10]. Research over the years has established that severe acidosis, clinically manifesting as respiratory distress (Kausmaul’s breathing), is a common complication and the leading independent factor predicting fatal outcome [11, 12]. Severe falciparum malaria has more recently been described as a complex syndrome, affecting many organ systems, which has many features in common with sepsis syndrome [13]. Indeed, clinical distinction between severe malaria and other common causes of life-threatening febrile illnesses including bacterial sepsis, pneumonia and CNS infection is often impossible at the time of presentation [14] (see Table 20.1 for summary of clinical characteristics) . The most comprehensive description of the clinical spectrum of severe malaria in African children is the AQUAMAT trial [7]. The trial involved 11 centres in 9 countries including a mixture of urban and rural hospitals and populations with differing malaria endemicities. All 5,425 participants in the trial had clinical evidence of severe malaria and the diagnosis was reinforced by quality controlled laboratory evidence of Plasmodium falciparum infection. Overall, at baseline, 37 % had coma, 32 % had convulsions, 9 % had compensated shock (capillary refilling time greater or equal to 3 s) and 3 % decompensated shock (systolic blood pressure < 70 mmHg and cool peripheries). Only 2 % had clinical jaundice. Among admission laboratory parameters, 30 % had severe anaemia (haemoglobin < 5 g/dl), 10 % were hypoglycaemic (blood sugar level < 3 mmol/l) and 43 % had severe acidosis (base deficit > 8). Co-morbidities included 13 % with (clinician diagnosed) sepsis (including 10 % with culture proven sepsis); 13 % with radiological evidence of pneumonia and 2 % with HIV, malnutrition or meningitis. Whilst dark urine (or haemoglobinuria also known as ‘blackwater fever’) and clinical jaundice were infrequent in these centres, there are other areas in Africa where these complications are more common (Olupot-Olupot, unpublished data). Key independent predictors of fatal outcome included acidosis, cerebral involvement, renal impairment and comorbidity [15].
We have recently published a review of the features of severe malaria and proposed UK management guidelines [16], which are based on information obtained from personal archives of references, the current World Health Organization (WHO) guidelines [17] and the Advanced Paediatric Life Support (APLS) guidelines [18]. Our recommendations for diagnosis are largely unchanged with the exception of shock —which we suggest should be defined by low systolic blood pressure, the rationale for which is discussed below as are the implications of recent results for therapeutic and supportive management recommendations.
20.2.1 Bacterial Infection
Comorbidity in children presenting to hospital is common in malaria-endemic Africa. Invasive bacterial disease is reported in 5–12 % of children with recent or current malaria, commonly Gram-negative (GN) infections [19, 20]. However, the sensitivity of blood cultures to detect septicaemia is low, so it is likely that the figures are underestimates [21]. Non-typhoidal salmonellae (NTS) are the most common isolate, particularly in younger children suffering from moderate or severe anaemia [22, 23]. The mechanisms underlying this apparent susceptibility remain uncertain. Since children in malaria-endemic areas often present to hospital with malaria parasitaemia—there is a possibility that the association with bacteraemia is largely observer bias. However, the most persuasive data that there is a significant biological association come from the study of Nadjm and colleagues in Tanzania [20], describing the spectrum of bacteraemia in unselected children admitted to hospital. Three subgroups were described, children who were malaria-negative, cases with recent malaria (malaria antigen positive but slide negative) and children with positive malaria slides. Among malaria-negative children with bacteraemia, 51 % had Gram-positive organisms isolated and 49 % Gram-negative (GN). Among children with recent or intercurrent malaria 76 % of bacteraemias were with non-Haemophilus influenzae GN organisms (of which 90 % were NTS). There was also a trend towards increasing proportion of non-Haemophilus influenzae (and non-NTS) Gram-negative enteric (‘other’ GN) organisms with increasing density of malaria parasitaemia. However, invasive bacterial disease is much less commonly reported in imported malaria in non-endemic settings [20].
20.3 Recent Changes in the Management of Severe Malaria
20.3.1 The AQUAMAT Trial
20.3.1.1 Background
Quinine has been used to treat malaria for over three centuries and until recently was the mainstay of treatment in African children with severe disease. In South East Asia the problem of quinine resistance, the substantial case fatality of severe malaria in adults and the availability of artemisinin derivatives prompted the performance of a large multicentre randomised trial (SEAQUAMAT) comparing parenteral artesunate with quinine in four countries [24] . The trial included 1,461 patients, most of whom were adults, and was stopped early by the data monitoring and safety committee following a planned interim analysis, which showed a substantial benefit in favour of artesunate. Mortality in patients receiving artesunate was 17 % (107/730) compared to 22 % (164/731) in patients receiving quinine. This equates to a relative reduction in mortality following artesunate compared to quinine of 34.7 % (95 % CI 18.5–47.6 %; p = 0·0002) . Since this trial, artesunate has been the drug recommended for treatment of severe malaria in adults by the WHO.
A separate trial in African children was justified on several grounds. First, there were important differences between the clinical manifestations, the tempo of the disease and the response to treatment in African children with severe malaria compared with adults in South East Asia. In severe malaria in children most deaths occur within the first 24 h—far sooner than in most adults in the SEAQUAMAT trial. This provides a much narrower time-window for any advantage of artesunate in killing young ring stage parasites more rapidly to translate into clinical benefit . Second, malaria parasites in Africa are more quinine sensitive, with no reported quinine resistance at the time of the trial. Third, drug cost and availability were also potential issues. Finally, previous trials in children in Africa comparing artemether with quinine found little evidence of superiority. However, artemether is an oil-based formulation of artemesinin, which needs to be given by intramuscular injection. Pharmacokinetic studies showed that the drug is only slowly and erratically released from the intramuscular injection site [25, 26] suggesting a possible reason for the previous failure to show a significant difference between quinine and artemisinin derivatives in African children. The advantages of intravenous (IV) artesunate include its potency compared to artemether [27] and instant bioavailability by both IV and intramuscular routes leading to rapid peak concentrations within 1 h [26, 28] . All these considerations supported the need for a conclusive trial to establish best practice.
20.3.1.2 Study Design
The AQUAMAT was conducted in nine African countries, and ran between October 2005 and July 2010 when the recruitment target was reached. Participating hospitals included university hospitals, research institutes and rural hospitals without prior research experience. None of the facilities had intensive care units—so the large majority of children were managed pragmatically on general paediatric wards . Children were eligible if they were under 15 years old with clinical evidence of severe malaria and a positive rapid malaria test (Optimal ä ) for Plasmodium falciparum malaria (indicating current malaria infection). Treatment, at recommended dosages, with parenteral quinine or an artemisinin derivative for more than 24 h before admission were the only exclusion criteria. The trial was an open label trial of both antimalarials given parenterally (either by intramuscular or intravenous administration) . Randomisation was masked as study numbers were kept inside opaque sealed paper envelopes and opened in numerical order. The card inside directed the clinician to a separate, sealed trial pack which contained the assigned intervention was on the first page. Blinding was not possible owing to the different methods of drug dilution and administration—artesunate requiring a two-step procedure for preparation and intravenous quinine needs to be given as an infusion, whereas artesunate is given as an injection . The interventions were given until the child was able to take an oral combination treatment, Coartem® (Artemether-Lumafantrine)—which was used to complete the treatment course. The primary outcome was in-hospital mortality and secondary outcomes included the incidence of severe complications and neurological sequelae.
20.3.1.3 Results
By intention to treat 572 (9.7 %) of the 5,425 children enrolled in the trial died. Whilst baseline characteristics of the children in the two arms were similar, mortality was substantially lower in the artesunate group 230/2,712 (8.5 %) compared to 297/2,713 (10.9 %) in the quinine arm. Comparing quinine to artesunate-treated children, the relative risk of death was 22.5 % (95 % CI 8.1–36.9) greater in the quinine arm (p = 0.002). There was no difference in outcome whether the drugs were administered intravenously or intramuscularly, nor were there any differences in outcome across any of the major clinical spectra defining severe malaria.
The development of coma and/or convulsion was more common during hospital admission in the quinine arm (p = 0.02); however there were no other differences between the arms in number of complications, additional treatments prescribed, time to recovery or numbers with neurological sequelae—which included 61 persistent mild, moderate or severe such sequelae among survivors.
20.3.1.4 Outcome: Change of Policy
Based upon the results of the SEAQUAMAT trial and now the AQUAMAT trial, parenteral artesunate is now recommended by the WHO and being adopted by individual countries as policy as the first line treatment for severe malaria in both adults and children. Artesunate should be given at admission then at 12 and 24 h, and once a day thereafter until the children can take and retain oral medication . Treatment must then be completed with a full course of artemisinin based combination therapy (ACT). If parenteral artesunate is not available, artemether or quinine are acceptable alternatives.
20.3.2 FEAST Trial
20.3.2.1 Background
The FEAST trial (Fluid Expansion As Supportive Treatment) was the first large controlled trial of fluid resuscitation comparing the use of early bolus resuscitation with local standard of care (no bolus) . At the time this trial was conducted, the recommendations for fluid resuscitation in Africa were substantially different from those in other parts of the world [29] and use of fluid resuscitation was highly controversial in children with severe malaria [30–32] . Although there was evidence to suggest that hypovolaemia contributes to the pathophysiology of severe malaria [33, 34], there were conflicting recommendations as to how it should be treated. Published WHO guidelines suggested that children might respond favourably to extra fluid in the presence of concomitant dehydration. However, specific recommendations regarding the type, rate or volume of fluid administration were not provided [35]. Use of invasive central venous pressure monitoring was recommended to monitor fluid replacement [35]. However, for the vast majority of children in sub-Saharan African hospitals this was neither available nor feasible. Therefore most such children with severe malaria were receiving no specific fluid management apart from blood transfusion in some cases, as this is recommended for the management of severe anaemia [36].
FEAST was designed to address this controversy [8]. However, severe malaria and bacteraemic sepsis syndrome are similar and simple bedside and laboratory assessment cannot distinguish between them [14, 37–40]. The FEAST trial was designed as a pragmatic trial incorporating both populations in order to provide practical information for hospitals with few diagnostic facilities.
20.3.2.2 Choice of Study Fluids
The trial was an open label randomised controlled trial of fluid resuscitation. Comparisons were at three levels; firstly, 0.9 % saline (a crystalloid) was compared with 5 % human albumin solution (colloid). Secondly, each of the fluids was compared to no bolus (control arm) and thirdly, both fluids were compared against no bolus (control). The inclusion of albumin (HAS) was based upon the results of three Phase II trials in Kenya comparing different fluids in children with severe malaria and signs of hypovolaemia [41–43]. The first trial had shown that up to 40 ml/kg of 0.9 % saline or HAS was safe and corrected haemodynamic indices of hypovolaemia [41]. The second trial was an open label, randomised comparison of saline and HAS in 117 children with severe malaria and acidosis. Mortality in children treated with HAS was 3.6 % (2/56), compared to 18 % (11/61) in those treated with saline (p = 0.01) [42]. In the subgroup of children with coma, only 1/21 (5 %) of children receiving HAS died, compared with 11/24 (46 %) who received saline (p = 0.002). Possibly owing to the greater survival rate in the HAS arm there was a non-significantly higher rate of neurological deficit (11 %; 6/54) compared to the saline arm (4 %, 2/50) [42]. In a further trial, mortality among children treated with HAS was lower (2.3 %; 1/44) than among those treated with the synthetic colloid Gelofusine (16 %; 7/44) [43]. In the sub group with coma, 1/ 25 (4 %) of HAS recipients died compared to 6/23 (26 %) in the Gelofusine arm (p = 0.04). Neurological sequelae complicated 3/43 (7 %) survivors receiving HAS and 1/37 (3 %) survivors receiving Gelofusine [43]. A meta-analysis of the combined data from the four trials (Fig. 20.1) demonstrated a reduced mortality with HAS compared to saline or other colloids (Peto odds ratio 0.30; 95 % confidence interval 0.15, 0.63; p = 0.001 and test for heterogeneity- c 2 = 3.58, p = 0.31) but also noted the potential with such small sample sizes to overestimate effect. On the basis of the evidence from these previous trials, it was decided to include randomisation to HAS in the FEAST trial .
20.3.2.3 FEAST Trial Design
Children aged > 60 days presenting with severe febrile illness and signs of impaired perfusion in six centres in three East African countries (Uganda, Kenya and Tanzania) were eligible for inclusion. Cases of gastroenteritis , severe malnutrition and non-medical causes (burns and trauma) were excluded from the trial, since the design and interventions were not relevant to these easily identifiable clinical presentations. Children were enrolled in two strata according to systolic blood pressure at presentation: 3,141 children without severe hypotension were enrolled in stratum A and received either an immediate bolus of 20 ml/kg given over 1 h (later increased to 40 ml/kg after protocol amendment) of 5 % HAS (1,050 children) or 0.9 % saline solution (1,047 children) or no bolus as controls (1,044 children); stratum B enrolled 29 children with severe hypotension (systolic blood pressure < 50 mmHg if < 12 m; < 60 mmHg if 1–5years; < 70 mmHg if > 5 years) were randomized to receive either 40 ml/kg (later increased to 60 ml/kg after protocol amendment) HAS or saline boluses—there were no control arm in stratum B. After 1 h saline-bolus and albumin-bolus arms, but not the control arm, received an additional 20 ml/kg bolus if signs of impaired perfusion persisted. Beyond this time point further fluid boluses in all three arms were only prescribed for severe hypotension (see above definition)—where an additional 40 ml/kg boluses of study fluid (saline for the control arm) was given over 1 h. No crossover between the saline and albumin was permitted [8].
20.3.2.4 Supportive Care
All children were managed on general paediatric wards . Ventilation facilities other than short-term ‘bag and mask’ support were unavailable. Training in triage and emergency paediatric life support was given throughout the trial to optimize case recognition, supportive management and ensure protocol adherence. Basic infrastructural support for emergency care, oxygen saturation and automatic blood pressure monitoring was provided. All children received maintenance fluids, anti-malarials and/or antibiotics as required. Throughout the hospital admission time, episodes of hypotensive shock within 48 h and Adverse Events (AE) potentially related to fluid resuscitation Pulmonary Edema (PE), Raised Intracranial Pressure (RICP) and severe allergic reaction were actively solicited. AEs were sent to the Clinical Trials Facility, Kilifi, Kenya within 2 days where they were reviewed by an independent clinician. All AEs were subsequently monitored on site against source documents by visiting monitors. Twenty-eight-days reviews for neurological deficit were performed by an independent clinician, blind to treatment allocation. Children with neurological impairment at day 28 were re-assessed at 6 months.
The primary endpoint was mortality at 48-h after randomisation . Secondary endpoints included mortality at 28-days, neurological sequelae at 28-days and 24 weeks, episodes of hypotensive shock within 48 h of randomisation and adverse events related to fluid resuscitation (pulmonary oedema, intracranial hypertension or severe allergic reaction among those receiving HAS).
20.3.2.5 Results
Among the 3,141 children in stratum A, there were no major differences in baseline characteristics across the three arms. Median age was 24 months (IQR 13–38); 62 % had prostration, 15 % were comatose and 83 % had increased work of breathing. Moderate-severe acidosis was present in 1,070 (52 %) and severe lactic acidosis in 1,159 (39 %). Severely anaemic children were 987 (32 %) and 187 (6 %) had hypoglycaemia. Malaria was confirmed in 1,793 (57 %); 126/1,070 (12 %) had bacteraemia and 4.4 % were HIV seropositive.
In stratum A, 48-h mortality was 111/1,050 (10.6 %), 110/1,047 (10.5 %) and 76/1,044 (7.3 %) in HAS-bolus, saline-bolus and control arms, respectively. Risk ratios (95 % confidence intervals): saline-bolus versus control was 1.44 (1.09–1.90, p = 0.01); HAS-bolus versus saline-bolus was 1.01 (0.78–1.29, p = 0.96); bolus (HAS or saline) versus control was 1.45 (1.13–1.86, p = 0.003). Most fatalities occurred before 24 h (259; 87 %). The small number of fatalities occurring after 48 h provided no evidence that children in the control arm had excess delayed mortality [8].
In stratum B (children with severe hypotension and impaired perfusion) a total of 29 children, were enrolled with a median systolic blood pressure of 57 mmHg (interquartile range, 51–59). Thirteen were randomised to HAS of whom 9 (69 %) died and 16 randomised to saline and 9 died (56 %) died (relative risk of 48 h mortality with HAS bolus, 1.23; 95 % CI, 0.70–2.16; p = 0.45) .
Excess mortality associated with bolus arms compared to control was consistent across all pre-specified subgroups. Moreover, there was no difference in outcome between the two bolus arms (for all saline versus albumin comparisons), including the children in coma among whom we had hypothesised that albumin infusion might be neuroprotective [13]. At 28 days, HAS-saline-control mortality and neurological abnormality rates were 12 %, 12 % and 8.7 % (p = 0.004 for bolus versus control) and 2.1 %, 1.3 %, 1.8 % (p = 0.85 for bolus versus control); pulmonary oedema or raised intracranial pressure were reported in 30, 24 and 17 children, respectively.
20.3.2.6 Interpretation
Since the paper was published, there has been considerable debate through commentary papers, letters, at journal clubs and web-based discussion groups about the interpretation of the FEAST trial results [44–49] . The FEAST trial was even the subject of a pro/con debate at the IIC Meeting, Oxford July 2011. Many commentators on the FEAST trial have speculated on the reason for this surprising result, some raising concerns about the broad entry criteria. One of the major causes for concern was the definition of shock . In a subsequent letter to the NEJM, responding to nine of the numerous letters selected for publication, the investigating group presented new data on the relevance of the FEAST trial cohort to other definitions of shock [50]. These data are summarised in Table 20.1.
20.3.3 Implications for Policy
The results of the FEAST trial challenge the primacy of bolus resuscitation as a life-saving intervention in paediatric emergencies . The trial results showed that 89.4 % of those given boluses survived the first 48 h in hospital. But those given only maintenance fluids did better: 92.7 % of them survived. Put another way, this means that compared to maintenance fluids, boluses cause more than three children (3.3 %) to die out of every hundred treated.
These results are applicable to Africa, under the conditions that prevailed in the FEAST trial . There may be reasons why fluid boluses are harmful in such African children including specific range of pathogens and nutritional status. However, there should be further research to re-examine the physiological changes in shock and host response. For severe malaria, which was present in 57 % of the study population, the results are clear and should inform future policy. Hypovolaemic shock in severe malaria should not be resuscitated with boluses of isotonic crystalloid or colloids as outcome is worse than in children receiving maintenance fluids only. Children with signs of dehydration can safely be managed with dextrose/isotonic saline (0.9 %) maintenance fluids (4 ml/kg/h) since outcome is better than more aggressive rehydration or resuscitation with isotonic fluid boluses.
References
Anstey NM, Russell B, Yeo TW, Price RN (2009) The pathophysiology of vivax malaria. Trends Parasitol 25(5):220–227
Hay SI, Guerra CA, Gething PW, Patil AP, Tatem AJ, Noor AM et al (2009) A world malaria map: Plasmodium falciparum endemicity in 2007. PLoS Med 6(3):e1000048
Hay SI, Okiro EA, Gething PW, Patil AP, Tatem AJ, Guerra CA et al (2010) Estimating the global clinical burden of Plasmodium falciparum malaria in 2007. PLoS Med 7(6):e1000290
Okiro EA, Alegana VA, Noor AM, Mutheu JJ, Juma E, Snow RW (2009) Malaria paediatric hospitalization between 1999 and 2008 across Kenya. BMC Med 7(1):75
Okiro EA, Alegana VA, Noor AM, Snow RW (2010) Changing malaria intervention coverage, transmission and hospitalization in Kenya. Malar J 9:285
Okiro EA, Bitira D, Mbabazi G, Mpimbaza A, Alegana VA, Talisuna AO et al (2011) Increasing malaria hospital admissions in Uganda between 1999 and 2009. BMC Med 9:37
Dondorp AM, Fanello CI, Hendriksen IC, Gomes E, Seni A, Chhaganlal KD et al (2010) Artesunate versus quinine in the treatment of severe falciparum malaria in African children (AQUAMAT): an open-label, randomised trial. Lancet 376(9753):1647–1657
Maitland K, Kiguli S, Opoka RO, Engoru C, Olupot-Olupot P, Akech SO et al (2011) Mortality after fluid bolus in African children with severe infection. N Engl J Med 364(26):2483–2495
Greenwood BM, Bradley AK, Greenwood AM, Byass P, Jammeh K, Marsh K et al (1987) Mortality and morbidity from malaria among children in a rural area of The Gambia, West Africa. Trans R Soc Trop Med Hyg 81(3):478–486
Newton CR, Krishna S (1998) Severe falciparum malaria in children: current understanding of pathophysiology and supportive treatment. Pharmacol Ther 79(1):1–53
English M, Waruiru C, Amukoye E, Murphy S, Crawley J, Mwangi I et al (1996) Deep breathing in children with severe malaria: indicator of metabolic acidosis and poor outcome. Am J Trop Med Hyg 55(5):521–524
Marsh K, Forster D, Waruiru C, Mwangi I, Winstanley M, Marsh V et al (1995) Indicators of life-threatening malaria in African children. N Engl J Med 332(21):1399–1404
Maitland K (2006) Severe malaria: lessons learned from the management of critical illness in children. Trends Parasitol 22(10):457–462
English M, Punt J, Mwangi I, McHugh K, Marsh K (1996) Clinical overlap between malaria and severe pneumonia in Africa children in hospital. Trans R Soc Trop Med Hyg 90(6):658–662
von Seidlein L, Olaosebikan R, Hendriksen IC, Lee SJ, Adedoyin OT, Agbenyega T et al (2012) Predicting the clinical outcome of severe falciparum malaria in african children: findings from a large randomized trial. Clin Infect Dis 54(8):1080–1090
Maitland K, Nadel S, Pollard AJ, Williams TN, Newton CR, Levin M (2005) Management of severe malaria in children: proposed guidelines for the United Kingdom. BMJ 331(7512):337–343
World Health Organization, Communicable Diseases Cluster (2000) Severe falciparum malaria. Trans R Soc Trop Med Hyg 94(Suppl 1):S1–90
Paediatric basic and advanced life support guidelines: An update. Paediatrics & child health. 2007; 12(6):495–500
Berkley J, Mwarumba S, Bramham K, Lowe B, Marsh K (1999) Bacteraemia complicating severe malaria in children. Trans R Soc Trop Med Hyg 93(3):283–286
Nadjm B, Amos B, Mtove G, Ostermann J, Chonya S, Wangai H et al (2010) WHO guidelines for antimicrobial treatment in children admitted to hospital in an area of intense Plasmodium falciparum transmission: prospective study. BMJ 340:c1350
Mancini N, Carletti S, Ghidoli N, Cichero P, Burioni R, Clementi M (2010) The era of molecular and other non-culture-based methods in diagnosis of sepsis. Clin Microbiol Rev 23(1):235–251
Graham SM, Walsh AL, Molyneux EM, Phiri AJ, Molyneux ME (2000) Clinical presentation of non-typhoidal Salmonella bacteraemia in Malawian children. Trans R Soc Trop Med Hyg 94(3):310–314
Mtove G, Amos B, von Seidlein L, Hendriksen I, Mwambuli A, Kimera J et al (2010) Invasive salmonellosis among children admitted to a rural Tanzanian hospital and a comparison with previous studies. PLoS One 5(2):e9244
Dondorp A, Nosten F, Stepniewska K, Day N, White N (2005) Artesunate versus quinine for treatment of severe falciparum malaria: a randomised trial. Lancet 366(9487):717–725
Murphy SA, Mberu E, Muhia D, English M, Crawley J, Waruiru C et al (1997) The disposition of intramuscular artemether in children with cerebral malaria; a preliminary study. Trans R Soc Trop Med Hyg 91(3):331–334
Hien T, Davis T, Chuong L, Ilett K, Sinh D, Phu N et al (2004) Comparative pharmacokinetics of intramuscular artesunate and artemether in patients with severe falciparum malaria. Antimicrob agents chemother 48:4234–4239
Brockman A, Price R, van Vugt M, Heppner D, Walsh D, Sooklo P et al (2000) Plasmodium falciparum antimalarial drug susceptibility on the northwestern border of Thailand during five years of extensive artesunate-mefloquine use. Trans R Soc Trop Med Hyg 94:537–544
Nealon C, Dzeing A, Muller-Romer U, Planche T, Sinou V, Kombila M et al (2002) Intramuscular bioavailability and clinical efficacy of artesunate in gabonese children with severe malaria. Antimicrob Agents Chemother 46(12):3933–3939
World Health Organization (2005) Hospital care for children: guidelines for the management of common illnesses with limited resources. Geneva, Switzerland. Report No.: ISBN 92 4 154670 0
Planche T, Onanga M, Schwenk A, Dzeing A, Borrmann S, Faucher JF et al (2004) Assessment of volume depletion in children with malaria. Plos Med 1(1):e18
Planche T (2006) Malaria and fluids—balancing acts. Trends Parasitol 21:562–567
Crawley J, Chu C, Mtove G, Nosten F (2010) Malaria in children. Lancet 375(9724):1468–1481
Maitland K, Levin M, English M, Mithwani S, Peshu N, Marsh K, Severe P et al (2003) Falciparum malaria in Kenyan children: evidence for hypovolaemia. QJM 96(6):427–434
Maitland K, Pamba A, Newton CR, Levin M (2003) Response to volume resuscitation in children with severe malaria. Pediatr Crit Care Med 4(4):426–431
Beare NA, Riva CE, Taylor TE, Molyneux ME, Kayira K, White VA et al (2006) Changes in optic nerve head blood flow in children with cerebral malaria and acute papilloedema. J Neurol Neurosurg Psychiatry 77(11):1288–1290
English M (2000) Life-threatening severe malarial anaemia. Trans R Soc Trop Med Hyg 94(6):585–588
Reyburn H, Mbatia R, Drakeley C, Carneiro I, Mwakasungula E, Mwerinde O et al (2004) Overdiagnosis of malaria in patients with severe febrile illness in Tanzania: a prospective study. BMJ 329(7476):1212
Evans JA, Adusei A, Timmann C, May J, Mack D, Agbenyega T et al (2004) High mortality of infant bacteraemia clinically indistinguishable from severe malaria. QJM 97(9):591–597
Taylor TE, Fu WJ, Carr RA, Whitten RO, Mueller JG, Fosiko NG et al (2004) Differentiating the pathologies of cerebral malaria by postmortem parasite counts. Nat Med 10(2):143–145
Bronzan RN, Taylor TE, Mwenechanya J, Tembo M, Kayira K, Bwanaisa L et al (2007) Bacteremia in Malawian children with severe malaria: prevalence, etiology, HIV coinfection, and outcome. J Infect Dis 195(6):895–904
Maitland K, Pamba A, Newton CR, Levin M (2003) Response to volume resuscitation in children with severe malaria. Pediatr Crit Care Med 4(4):426–431
Maitland K, Pamba A, English M, Peshu N, Marsh K, Newton CRJC et al (2005) Randomized trial of volume expansion with albumin or saline in children with severe malaria: preliminary evidence of albumin benefit. Clin Infect Dis 40:538–545
Akech S, Gwer S, Idro R, Fegan G, Eziefula AC, Newton CR et al (2006) Volume expansion with albumin compared to gelofusine in children with severe malaria: results of a controlled trial. PLoS Clin Trials 1(5):e21
Southall DP, Samuels MP (2011) Treating the wrong children with fluids will cause harm: response to ’mortality after fluid bolus in African children with severe infection’. Arch Dis Child 96(10):905–906
Myburgh JA (2011) Fluid resuscitation in acute illness–time to reappraise the basics. N Engl J Med 364(26):2543–2544
Hilton AK, Bellomo R (2011) Totem and taboo: fluids in sepsis. Critical Care 15(3):164
Duke T (2011) What the African fluid-bolus trial means. Lancet 378(9804):1685–1687
Bates I (2011) Detrimental effect of fluid resuscitation in the initial management of severely ill children in Africa. Transfus Med 21(5):289–290
Maitland K, Babiker A, Kiguli S, Molyneux E (2012) The FEAST trial of fluid bolus in African children with severe infection. Lancet 379(9816):613; (author reply − 4)
Maitland K, Akech S, Russell E (2011) Mortality after fluid bolus in African children with sepsis reply. N Engl J Med 365(14):1351–1353
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2013 Springer Science+Business Media New York
About this chapter
Cite this chapter
Olupot-Olupot, P., Maitland, K. (2013). Management of Severe Malaria: Results from Recent Trials. In: Curtis, N., Finn, A., Pollard, A. (eds) Hot Topics in Infection and Immunity in Children IX. Advances in Experimental Medicine and Biology, vol 764. Springer, New York, NY. https://doi.org/10.1007/978-1-4614-4726-9_20
Download citation
DOI: https://doi.org/10.1007/978-1-4614-4726-9_20
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4614-4725-2
Online ISBN: 978-1-4614-4726-9
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)