Abstract
Learning from errors is fundamental to adaptive human behavior. It requires detecting errors, evaluating what went wrong, and adjusting behavior accordingly. These dynamic adjustments are at the heart of behavioral flexibility and accumulating evidence suggests that deficient error processing contributes to maladaptively rigid and repetitive behavior in a range of neuropsychiatric disorders. Neuroimaging and electrophysiological studies reveal highly reliable neural markers of error processing. In this review, we evaluate the evidence that abnormalities in these neural markers can serve as sensitive endophenotypes of neuropsychiatric disorders. We describe the behavioral and neural hallmarks of error processing, their mediation by common genetic polymorphisms, and impairments in schizophrenia, obsessive–compulsive disorder, and autism spectrum disorders. We conclude that neural markers of errors meet several important criteria as endophenotypes including heritability, established neuroanatomical and neurochemical substrates, association with neuropsychiatric disorders, presence in syndromally unaffected family members, and evidence of genetic mediation. Understanding the mechanisms of error processing deficits in neuropsychiatric disorders may provide novel neural and behavioral targets for treatment and sensitive surrogate markers of treatment response. Treating error processing deficits may improve functional outcome since error signals provide crucial information for flexible adaptation to changing environments. Given the dearth of effective interventions for cognitive deficits in neuropsychiatric disorders, this represents a potentially promising approach.
Support: National Institute for Mental Health: R01 MH67720 (DSM); F32 MH088081 (YA).
Note from Volume Editors:
This chapter was published in the open source journal ‘Frontiers in Human Neuroscience,’ July 2013, Vol. 7, Article 350. In view of the topical and thematic overlap between the invited chapter and the journal article that the chapter authors had submitted at the time of the invitation, the authors kindly granted permission to reproduce the article in this volume.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Autism Spectrum Disorder
- Autism Spectrum Disorder
- Anterior Cingulate Cortex
- Repetitive Behavior
- Neuropsychiatric Disorder
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Introduction
Learning from errors is fundamental to adaptive human behavior. It requires detecting errors, evaluating what went wrong, and adjusting behavior accordingly. These dynamic adjustments are at the heart of behavioral flexibility and accumulating evidence suggests that deficient error processing contributes to maladaptively rigid and repetitive behavior in a range of neuropsychiatric disorders. Neuroimaging and electrophysiological studies reveal highly reliable neural markers of error processing. In this review, we evaluate the evidence that abnormalities in these neural markers can serve as sensitive endophenotypes of neuropsychiatric disorders. We describe the behavioral and neural hallmarks of error processing, their mediation by common genetic polymorphisms, and impairments in schizophrenia, obsessive–compulsive disorder, and autism spectrum disorders. We conclude that neural markers of errors meet several important criteria as endophenotypes including heritability, established neuroanatomical and neurochemical substrates, association with neuropsychiatric disorders, presence in syndromally unaffected family members, and evidence of genetic mediation. Understanding the mechanisms of error processing deficits in neuropsychiatric disorders may provide novel neural and behavioral targets for treatment and sensitive surrogate markers of treatment response. Treating error processing deficits may improve functional outcome since error signals provide crucial information for flexible adaptation to changing environments. Given the dearth of effective interventions for cognitive deficits in neuropsychiatric disorders, this represents a promising approach.
To adapt to the environment, human beings must learn from the consequences of their behavior. Understanding the nature of the brain mechanisms that flexibly modify behavior based on its consequences is a fundamental goal of neuroscience. These mechanisms are also of considerable clinical importance since a number of neuropsychiatric disorders are strongly associated with maladaptively rigid and repetitive behaviors that are not optimally responsive to outcomes. One approach to understanding the neural basis of learning from consequences is to study error processing. Errors provide critical information for adjusting behavior to optimize outcomes. Error processing, which is also referred to as ‘response monitoring’ or ‘performance monitoring,’ involves detecting errors during task performance, evaluating what went wrong, and adjusting behavior accordingly. These dynamic adjustments of responses are at the heart of behavioral flexibility. They enable individuals to optimize function in complex, uncertain, and constantly changing environments. Since learning from errors is impaired in several neuropsychiatric disorders, understanding the neural and genetic mechanisms of error processing has important clinical implications. Identifying specific deficits can illuminate the pathophysiology of these disorders and provide novel targets for treatment. Below, we selectively review the behavioral and neural hallmarks of error processing; impairments in schizophrenia, obsessive–compulsive disorder, and autism spectrum disorders; and genetic contributions. The goal is to evaluate the potential of the neural markers of errors to serve as endophenotypes. Endophenotypes are biologically based heritable dysfunctions that are thought to be a closer reflection of the effects of the genes that predispose to illness than either the diagnosis itself, or the symptoms that define it (Gottesman and Gould 2003). The identification of clinically relevant endophenotypes can facilitate the discovery of susceptibility genes, mechanisms of illness, and targets for intervention (Hariri et al. 2006).
2 Behavioral Indices of Error Processing
Both the behavioral and neural markers of error processing are considered to be ‘generic’ in that they are elicited by a wide range of tasks regardless of response modality (Holroyd and Coles 2002). Many experimental tasks used to study error processing in humans require response inhibition, or the suppression of prepotent but contextually inappropriate responses. These include variations of go/no-go, antisaccade (Hallett 1978), countermanding, or stop signal (Logan and Cowan 1984), Stroop (1935), Simon (1969), and perhaps most commonly, Eriksen flanker (Eriksen and Eriksen 1974) tasks.
Errors give rise to both immediate and longer-term remedial adjustments of behavior. Short-term or trial-by-trial adjustments include the immediate self-correction of errors and the slowing of reaction time (RT) in trials that follow an error (i.e., post-error slowing) (Rabbitt 1966). These trial-by-trail adjustments of RT based on the error history are well described by the Speed-Accuracy Trade-Off (SATO) function. The SATO function depicts the nonlinear relation between speed and accuracy such that faster responding does not affect accuracy, but only up to a point. Beyond that point, speed and accuracy are inversely related, with slower responses having a greater probability of being correct (Fig. 9.1). This transition point can be regarded as an optimum, where the best accuracy is achieved at the fastest possible speed. Over trials, responses speed up until an error is committed (Ridderinkhof et al. 2003), and following an error, RT slows, and the probability of an error decreases (Fig. 9.1). This pattern can be interpreted as a progression to riskier positions on the SATO function culminating in an error. The error is followed by a shift back to a safer position on the function that has a greater likelihood of a correct response.
Trial-by-trial adjustments of reaction time (RT). a A schematic depiction of the speed-accuracy trade-off (SATO) function. The circle denotes the optimum: the point at which the highest accuracy is achieved at the fastest possible speed. Beyond this point, speedier responses entail a cost (trade-off) in reduced accuracy. b Mean saccadic RT during an antisaccade task as a function of trial position relative to an error trial. Post-error slowing (PES) is defined as the difference in RT between the trial following the error (1Post) and the trial preceding the error (1Pre). Error bars represent the standard error of the mean
Reinforcement learning theory (Thorndike 1911) can be invoked to account for longer-term behavioral changes in response to errors. Its main principle is that rewarded actions are more likely to be repeated, while actions with negative consequences are less likely to recur. In behavioral terms, reinforcement learning involves the strengthening or weakening of stimulus–response mappings based on behavioral outcomes. While reinforcement learning has traditionally been studied using explicit rewards and punishments, recent theory extends it to errors (Holroyd and Coles 2002). Errors on cognitive tasks are both salient (in that they are often unexpected) and aversive (representing the non-achievement of a goal). As failures of performance they often have negative consequences. For these reasons, errors prompt reinforcement learning.
3 Neural Markers of Errors, Their Functional Significance, and Relations to One Another
Electrophysiological and neuroimaging studies have identified two highly reliable neural markers of error commission—the error-related negativity (ERN) and functional MRI (fMRI) activation of the dorsal anterior cingulate cortex (dACC; (Taylor et al. 2007)—that are the focus of the present review. Although these error markers have been extensively studied, their functional significance and relations to one another are incompletely understood.
3.1 The Error-Related Negativity (ERN)
The ERN or error negativity (Ne) is an event-related potential that peaks ~100 ms following an error (Fig. 9.2, Dehaene et al. 1994; Falkenstein et al. 1991; Gehring et al. 1993; van Veen and Carter 2002) and is usually measured on the scalp with electroencephalography (EEG), magnetoencephalography (MEG; Keil et al. 2010), or a combination of both techniques (Agam et al. 2011). The ERN is usually defined as the peak of the difference between the averaged waveforms of error and correct trials time-locked to the onset of the response. The ERN is the earliest error marker and is ‘generic’ in that it is seen across a variety of behavioral paradigms and response modalities. Comparisons of ERNs time-locked to button presses, saccadic eye movements, or foot presses, reveal a similar morphology, amplitude, and scalp topography (Holroyd et al. 1998; Van’t Ent and Apkarian 1999). ERN latency, however, varies based on the measurement technique. Button presses elicit shorter latencies than ERNs locked to the electromyography (EMG) or saccadic responses as measured by electrooculography (EOG). This reflects that EMG and EOG measure the onset of movement, which occurs earlier than its outcome (e.g., a button press). The ERN is usually maximal at electrode Cz on the scalp (e.g., Agam et al. 2011; van Schie et al. 2004; van Veen and Carter 2002), but the peak location can be more anterior (e.g., Endrass et al. 2005; Gehring and Fencsik 2001; Nieuwenhuis et al. 2003) or posterior (e.g., Hajcak et al. 2004; Ladouceur et al. 2007; van Boxtel et al. 2005) and factors such as response modality and task fail to provide a convincing account of this variability.
The error-related negativity (ERN). a Grand average waveforms for correct (black) and error (red) antisaccade trials, time-locked to the onset of the saccade. b Difference waveform, obtained by subtracting the correct waveform from the error waveform. c Scalp distribution of the ERN, displayed on a template head model. Adapted from Agam et al. (2011)
The ERN has been proposed to reflect error detection and reinforcement learning (Holroyd and Coles 2002; Holroyd et al. 2004b; Paus et al. 1993). Its amplitude is greater when accuracy is emphasized over speed (Gehring et al. 1993), when errors are corrected (Scheffers and Coles 2000), when errors incur greater loss (Holroyd et al. 2004a), and when errors are less frequent and therefore also less expected (Gehring et al. 1993; Hajcak et al. 2003). Larger ERNs are associated with greater post-error slowing of responses (Debener et al. 2005), and ERN latency predicts the speed of self-corrections (Fiehler et al. 2005). These findings suggest that the ERN detects errors, is sensitive to both the predictability and value of outcomes, and contributes to dynamic, trial-by-trial adjustments of performance.
3.2 Error Positivity (Pe)
A second EEG error marker warrants consideration given its relevance to neuropsychiatric disorders. The error positivity or Pe (van Veen and Carter 2002) is an event-related potential that occurs approximately 300–500 ms following an error (for review see, Overbeek et al. 2005). The Pe has been localized to the rostral anterior cingulate cortex (van Boxtel et al. 2005; van Veen and Carter 2002), though one study reported a dACC source (Herrmann et al. 2004). The Pe is not as well characterized and is less consistently observed than the ERN, which may reflect that it is a later and more variable component of error processing. While the ERN is present regardless of whether an error was perceived, the Pe is present only for perceived errors and is thought to index error awareness (Endrass et al. 2007; Nieuwenhuis et al. 2001). The Pe has also been associated with the subjective or emotional appraisal of errors (van Veen and Carter 2002) and with short-term performance adjustments such as error correction and post-error slowing (Nieuwenhuis et al. 2001).
3.3 Error-Related FMRI Activation of the Anterior Cingulate Cortex (ACC)
Error commission is also reliably associated with increased fMRI activation of the ACC on error compared with correct trials (i.e., error-related activation, Fig. 9.3; (for review, see Taylor et al. 2007). The ACC can be divided into a dorsal region (dACC) that extends caudally from the genu of the corpus callosum to the vertical plane of the anterior commissure, and interacts with the striatum and other cortical regions to mediate motor and cognitive processing, and a rostral region (rACC) that lies anterior and ventral to the genu of the corpus callosum and interacts with other paralimbic and limbic regions, including the amygdala and insula, to mediate emotional processing (Bush et al. 1998, 2000; Devinsky et al. 1995; Phillips et al. 2003; Whalen et al. 1998). Like the Pe, error-related rACC activation is thought to reflect appraisal of the affective or motivational significance of errors (Luu et al. 2003; Taylor et al. 2006; van Veen and Carter 2002). Such appraisal may also involve the insula and amygdala, both of which are densely interconnected with the rACC (van Hoesen et al. 1993) and show increased activity with errors (Brazdil et al. 2002; Garavan et al. 2002; Menon et al. 2001; Polli et al. 2009). While both dACC and rACC show error-related activation (Luu et al. 2003; Taylor et al. 2006; van Veen and Carter 2002), dACC activation is more consistently observed. Like the ERN, greater error-related dACC activation is associated with lower error rates (Fitzgerald et al. 2010; Polli et al. 2008) and increased post-error slowing (Garavan et al. 2002; Kerns et al. 2004; Klein et al. 2007a).
Error-related activation in the anterior cingulate cortex (ACC). Statistical maps, displayed on medial cortical surface templates, show activation on correct trials versus a fixation baseline (top), error versus fixation (middle), and error versus correct (bottom). Gray masks cover subcortical regions in which activation is displaced in a surface rendering. The dACC and rACC are outlined in blue and red, respectively. Adapted from Polli et al. (2005)
3.4 Modulation of Default Network Activation in Relation to Errors
The brain’s default network is thought to mediate self-referential and affective processing and is usually deactivated during effortful cognitive tasks (Buckner et al. 2008; Raichle et al. 2001). During error trials (Polli et al. 2005) and trials immediately preceding errors (Eichele et al. 2008; Li et al. 2007), however, the default network shows relatively increased activation, which may reflect increased focus on the internal milieu at the expense of attention to the task (Drevets and Raichle 1998). In trials that follow errors, task-induced deactivation is re-established (Eichele et al. 2008). This cyclical pattern of default network activation in trials including and surrounding errors correlates with speed-accuracy trade-off-based changes in RT (i.e., pre-error speeding, faster errors, and post-error slowing, Agam et al., in press) and suggests that interference from internally directed thought culminates in an error, which, in turn prompts renewed attention to the task in the subsequent trial. These changes in activation are not strictly error markers (i.e., they are not specific to errors nor do they necessarily indicate that an error has occurred), but they may contribute to error commission and to behavioral adjustments following errors such as post-error slowing. Several reviews have addressed the role of default network function in neuropsychiatric disorders (e.g., Broyd et al. 2009; Buckner et al. 2008; Sandrone 2012; Whitfield-Gabrieli and Ford 2012). Whether changes of default network activity in relation to errors are affected in neuropsychiatric disorders, however, is largely unexplored.
3.5 Error-Based Reinforcement Learning
Error-related dACC activation is often assumed to be the hemodynamic correlate of the ERN. This assumption is consistent with both EEG and MEG studies that have reported a dACC source for the ERN and with models that attribute both error markers to a specific neural mechanism that implements error-based reinforcement learning (Holroyd and Coles 2002; Ridderinkhof et al. 2004; Taylor et al. 2007). Consistent with animal neurophysiology and human neuroimaging findings, these models view the neural sequelae of error commission as indices of error-based reinforcement learning (Holroyd and Coles 2002; Schultz 2002). When an error occurs, the striatum detects a mismatch between the intended (correct) outcome and actual (error) outcome. This mismatch or ‘prediction error’ results in a phasic decrease in mesencephalic dopamine (DA) release that results in the disinhibition of neurons in the dACC. These neurons generate the ERN. According to this theory, both increased dACC activation and the ERN reflect the use of DA-dependent error signals to modify the associative strength of stimulus–response mappings in the service of optimizing behavioral outcomes (Holroyd et al. 2003, 2004b). Thus, both error-related dACC activation and ERN can be conceptualized as DA-dependent training signals that are used to learn from errors (Brown and Braver 2005; Holroyd and Coles 2002). Similar neural mechanisms of error processing have been observed across species for a variety of learning tasks. For example, the songbird uses input from a basal ganglia—thalamocortical circuit to recognize and correct vocal errors while learning its distinctive song (Andalman and Fee 2009). Such findings suggest that this neural circuitry represents an evolutionarily conserved mechanism for learning from errors.
3.6 Relation of the ERN to DACC Activation
Despite the many studies that report a dACC source for the ERN, the location of the neural generator of the ERN is still a topic of debate. When compared across studies, the dACC source loci of the ERN show considerable variation (for review, see Agam et al. 2011) and all are posterior to the mean location of error-related fMRI activation (based on a meta-analysis of 13 fMRI studies, Ridderinkhof et al. 2004). Some ERN loci also fall in the posterior cingulate cortex (PCC) according to standard anatomical definitions that place the ACC/PCC border between y = −2 and y = −12 mm in Talairach space (Bush et al. 2000). The PCC is also a plausible generator of the ERN. It shows error-related fMRI activation (Fassbender et al. 2004; Menon et al. 2001; Wittfoth et al. 2008), though not nearly as consistently as the dACC, and like the ERN, its activity is modulated by the value of behavioral outcomes (Fujiwara et al. 2009; McCoy et al. 2003; Smith et al. 2009). An MEG study reported a PCC source for the feedback-related negativity, which is thought to be generated by the same generic mechanism as the ERN (Donamayor et al. 2011). Further, a study from Agam and colleagues that combined data from EEG and MEG localized the source of the ERN to the PCC (Agam et al. 2011). This PCC region was clearly distinct from error-related dACC activation measured in the same participants performing the same task during fMRI.
These findings challenge the view that dACC activation and the ERN are different measurements of the same underlying neural mechanism. Instead, they indicate that the ERN and fMRI activation of the dACC reflect distinct neural responses to errors. In the combined MEG/EEG, fMRI, and diffusion tensor imaging (DTI) study of Agam and colleagues, ERN amplitude correlated with fMRI activation in both the PCC and dACC, and these two regions showed coordinated activity based on functional connectivity MRI. This suggests that the dACC and PCC are components of a functional network that mediates error processing. The PCC and ACC have direct anatomical connections through the cingulum bundle (Schmahmann et al. 2007) and increased microstructural integrity of the posterior cingulum bundle (as indexed by DTI measurements of fractional anisotropy) predicted faster error self-correction. To the degree that fractional anisotropy reflects myelination, increased myelination along the cingulum bundle may speed the conduction of the message that an error has occurred, thereby resulting in faster corrective responses. Taken together, these findings are consistent with the theory that the PCC detects errors, gives rise to the ERN, and then relays error information to the dACC via the cingulum bundle to implement corrective behavior. Refinements of this working model will likely follow given that the mechanisms of error processing remain a highly active area of research.
4 Error Processing Impairments in Neuropsychiatric Disorders
Although the present review focuses on schizophrenia, obsessive–compulsive disorder (OCD) and autism spectrum disorder (ASD), accumulating evidence suggests that error processing deficits contribute to rigid, repetitive behavior in a range of disorders. For example, a previous review described ERN abnormalities in anxiety disorders, depression, and substance abuse and their relations to symptoms (Olvet and Hajcak 2008). Emerging evidence also indicates that error processing deficits differ by diagnosis suggesting distinct neural mechanisms and genetic contributions. This has important implications for understanding pathophysiology and for the treatment of associated cognitive and behavioral dysfunction. Below, we evaluate evidence that neuroimaging-based markers of deficient error processing can serve as sensitive endophenotypes of neuropsychiatric disorders.
4.1 Schizophrenia
Perseveration, or the contextually inappropriate and unintentional repetition of responses, is a classic behavioral abnormality in schizophrenia. At least some forms of perseveration may reflect a failure to use error feedback to guide behavior. A classic example is continuing to make a previously reinforced response to the Wisconsin Card Sort Test even though feedback indicates that it is no longer correct (e.g., Goldberg et al. 1987). These perseverative errors reflect both motivational and cognitive factors (Summerfelt et al. 1991) and exemplify the behavioral rigidity despite changing contingencies that is often observed in schizophrenia.
Both neuroimaging and electrophysiological studies consistently report blunted neural responses to errors in schizophrenia. fMRI studies show reduced error-related dACC and rACC activations (Carter et al. 2001; Kerns et al. 2005; Laurens et al. 2003). Reduced error-related activation extends to ‘reinforcement learning circuitry,’ comprising the dACC, substantia nigra, caudate, and putamen, and to ‘affective appraisal circuitry’ comprising the rACC, insula, and amygdala, in which reduced activation may reflect diminished concern regarding behavioral outcomes (Polli et al. 2008). These reductions remain after statistically controlling for the effects of antipsychotic medication dose and error rate, the latter indicating that the blunted neural response to errors in schizophrenia is not simply a reflection of more frequent, and therefore more predictable errors.
Patients with schizophrenia also consistently show a blunted ERN (Alain et al. 2002; Bates et al. 2002; Foti et al. 2012; Kopp and Rist 1999; Mathalon et al. 2002; Morris et al. 2006; Perez et al. 2012). Even in the context of an abnormal ERN, however, the Pe is intact in patients in many (Alain et al. 2002; Mathalon et al. 2002; Morris et al. 2006; Simmonite et al. 2012) but not all studies (Foti et al. 2012; Perez et al. 2012). Immediate error-related performance adjustments such as post-error slowing and error self-correction are also often intact (Kopp and Rist 1994, 1999; Laurens et al. 2003; Levy et al. 1998; Mathalon et al. 2002; Polli et al. 2006, 2008), although impaired performance adjustments have also been reported (Carter et al. 2001; Malenka et al. 1982, 1986; Turken et al. 2003). Dissociations between intact performance adjustments and reduced ACC activity and ERN amplitude are often seen within single studies (Kopp and Rist 1999; Laurens et al. 2003; Mathalon et al. 2002; Polli et al. 2008) and suggest that error processing deficits in schizophrenia are selective.
Findings of blunted ERN and dACC activation in schizophrenia are remarkably consistent and may reflect a more general problem with reinforcement learning, which is impaired in schizophrenia (Waltz et al. 2007, 2010; Waltz and Gold 2007). They may also reflect functional and structural abnormalities of the cingulate cortex. There is overwhelming evidence of abnormal ACC function and structure in schizophrenia including gray matter abnormalities (e.g., Goldstein et al. 1999; Ha et al. 2004; Kuperberg et al. 2003; Mitelman et al. 2005; Ohnuma et al. 1997; Sigmundsson et al. 2001; Suzuki et al. 2002; Yamasue et al. 2004), volume reductions in the white matter underlying the ACC (McDonald et al. 2005; Mitelman et al. 2005) and reduced fractional anisotropy of white matter underlying the cingulate cortex in many (Ardekani et al. 2003; Hao et al. 2006; Kubicki et al. 2003; Manoach et al. 2007; Sun et al. 2003; Wang et al. 2004) but not all studies (Agartz et al. 2001; Buchsbaum et al. 1998; Burns et al. 2003; Foong et al. 2002). Histopathological studies give evidence of disturbances in ACC micro- and macrocircuitry that might alter communication with connected regions (e.g., Benes 1993, 2000), consistent with reports of reduced functional and structural connectivity of the ACC in schizophrenia (e.g., Kyriakopoulos et al. 2012; Manoach et al. 2007; Tu et al. 2010; Yan et al. 2012).
Treatment with antipsychotic drugs is an important confound in this literature given their effects on dopamine neurotransmission and indices of error processing (e.g., Zirnheld et al. 2004). Several lines of evidence suggest that deficient error processing is not merely a side effect of treatment. Functional and structural ACC abnormalities, which predict the onset of psychosis (Fornito et al. 2008), are also seen in never-medicated high-risk youth (Whalley et al. 2006), and in never-medicated children experiencing psychotic symptoms (Jacobson et al. 2009). In addition, a blunted ERN, similar to that observed in schizophrenia, is seen in syndromally unaffected siblings (Simmonite et al. 2012), in never-medicated children with putative antecedents to schizophrenia (Laurens et al. 2009) and in antipsychotic naïve patients at high clinical risk for psychosis (Perez et al. 2012). These studies suggest that antipsychotic drugs do not fully account for blunted error processing or other functional and structural ACC abnormalities in schizophrenia. Instead, this literature suggests that ACC abnormalities and error processing deficits are trait markers of genetic vulnerability to schizophrenia that predate the onset of illness. Impairments in evaluating and learning from errors in schizophrenia may substantially contribute to the rigid, perseverative, and maladaptive patterns of thought and behavior that characterize schizophrenia and compromise social and occupational function (Kim et al. 2006). In support of this possibility, a recent study reported that a blunted ERN was associated with more severe negative symptoms and poorer real-world function as indicated by unemployment and rehospitalization (Foti et al. 2012).
4.2 Obsessive–Compulsive Disorder (OCD)
OCD is characterized by uncontrollable, unwanted thoughts (i.e., obsessions) and repetitive, ritualized behaviors that individuals feel compelled to perform (compulsions). In contrast to the blunted neural responses to errors in schizophrenia, OCD is often associated with exaggerated error responses including increased error-related ACC activation (Fitzgerald et al. 2005, 2010; Maltby et al. 2005; Ursu et al. 2003) and increased ERN amplitude not only on error trials (Endrass et al. 2008, 2010; Gehring et al. 2000; Johannes et al. 2001; Ruchsow et al. 2005; Santesso et al. 2006; Xiao et al. 2011) but also on correct trials in some (Maltby et al. 2005; Ursu et al. 2003), but not all studies (Fitzgerald et al. 2005; Gehring et al. 2000). One study reported a normal ERN to errors in OCD (e.g., Nieuwenhuis et al. 2005) and recent findings (Kaczkurkin 2013) including those of a meta-analysis (Mathews et al. 2012) suggest that while the ERN is generally increased, this varies based on the type of task, the level of difficulty and the symptoms present. A recent study of children with OCD found an increased ERN in both patients and their unaffected siblings relative to controls suggesting that the ERN is a marker of genetic risk for OCD (Carrasco et al. 2013). Both increased ERN amplitude (Gehring et al. 2000) and error-related ACC activation (Fitzgerald et al. 2005; Ursu et al. 2003) have been associated with the severity of obsessions and compulsions in OCD suggesting that hyperactive error processing contributes to the defining features of behavioral and cognitive repetition and rigidity. This hypothesis is consistent with a long-standing theory of OCD that inappropriate and exaggerated error signals in response to behavioral outcomes lead to a pervasive sense of incompleteness and self-doubt (Pitman 1987) that triggers the compulsion to repeat behaviors, even if they were already successfully completed (Maltby et al. 2005). In this scenario, an individual suffering from OCD may remember correctly that they locked the door, but inappropriate and persistent error signals may indicate that something is ‘not quite right’ and compel them to check repeatedly that the door is indeed locked. Findings that the ACC and connected regions show increased activation during symptom provocation in OCD (Breiter et al. 1996) and that cingulotomy relieves obsessions and compulsions (Dougherty et al. 2002) also support the link between hyperactivity in ACC circuitry and rigid, repetitive behaviors.
Measurements of obsessive-compulsive behavior have also been related to indices of error processing in non-clinical samples. Obsessive characteristics are related to the amplitudes of the ERN and Pe in children (Santesso et al. 2006) and to the amplitude of the ERN in college undergraduates (Hajcak and Simons 2002). These findings suggest that obsessive–compulsive traits in the general population are also mediated by error processing mechanisms.
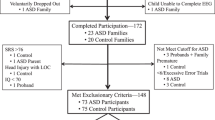
4.3 Autism Spectrum Disorders (ASDs)
ASDs are neurodevelopmental disorders that are characterized by three core features: impaired social interaction; impaired communication; and restricted, repetitive, and stereotyped patterns of behavior, interests, and activities. Although repetitive and restricted behaviors are often the most disabling feature of ASD (Bishop et al. 2007), they have received the least research attention. They are present as early as 18 months, predict outcome independently of social and communication deficits, and may interfere with the development of social and communication skills that are deficient in ASD (Morgan et al. 2008; Watt et al. 2008). The hypothesis that error processing deficits characterize ASD and contribute to behavioral repetition and rigidity receives only mixed support from the literature.
Several studies have reported a blunted ERN in ASD (Santesso et al. 2011; Sokhadze et al. 2010, 2012b; South et al. 2010; Vlamings et al. 2008), one has reported normal ERN (Groen et al. 2008), and yet another found an increased latency (and amplitude in a high-functioning subset of participants) of the ERN (Henderson et al. 2006). The finding that repetitive low-frequency transcranial magnetic stimulation (rTMS) to bilateral dorsolateral prefrontal cortex in high-functioning children with ASD was associated with an increased ERN (but also a decreased error rate) suggests the possibility of intervention to modulate error processing (Sokhadze et al. 2012a).
Behaviorally, reduced error self-correction (Russell and Jarrold 1998), normal rates of error self-correction (Thakkar et al. 2008), and reduced post-error slowing (Bogte et al. 2007) have all been observed. Two fMRI studies reported exaggerated error-related ACC activation in ASD (Goldberg et al. 2011; Thakkar et al. 2008) and in one of these, increased ACC activation on correct trials that correlated with higher clinical ratings of restricted, repetitive behavior in ASD, thus linking abnormal error processing to a core symptom (Thakkar et al. 2008). This relation may reflect that reduced discrimination between correct and error outcomes interferes with adjusting behavior to obtain the most favorable outcome. Another compatible possibility is that like OCD, in ASD uncomfortable error signals following correct responses compel repetitive behavior. In ASD, these abnormal signals on correct trials were maximal in the rACC, which is thought to contribute to an appraisal of the affective or motivational salience of errors (Luu et al. 2003; Taylor et al. 2006; van Veen and Carter 2002). Finally, three studies, including the one reporting increased ACC activation on both error and correct trials, have reported reduced fractional anisotropy (FA) in ACC white matter as measured by DTI (Barnea-Goraly et al. 2004; Noriuchi et al. 2010; Thakkar et al. 2008), but not a fourth, which reported increased FA in ACC white matter (Cheng et al. 2010).
In summary, the literature provides only preliminary support for the hypothesis that cingulate cortex abnormalities impair error processing in ASD and contribute to restricted, repetitive behavior. At present, repetitive behaviors in ASD are incompletely understood and neurobiologically valid dimensions have not been delineated. Efforts to understand the contribution of error processing to specific dimensions of repetitive behavior and to identify the underlying mechanisms can guide the development of targeted treatments.
5 Rationale for the Use of Neuroimaging-Based Cognitive Endophenotypes
Although Diagnostic and Statistical Manual (DSM) Axis I psychiatric disorders are highly heritable, their genetic origins remain elusive. A major obstacle to identifying genetic risk factors is the difficulty defining neurobiologically valid phenotypes for inclusion in studies. Current DSM criteria for disorders such as schizophrenia and autism define phenotypes that are so broad that it is possible for two study samples with the same diagnosis to bear little resemblance to one another. This phenotypic heterogeneity suggests etiological and genetic heterogeneity, and reliance on such overly broad diagnostic categories can lead to inconsistent findings across genetic studies. Within studies, relatively large effects may be obscured because they only characterize a subset of the sample. While phenotypic heterogeneity is expected in complex genetic disorders such as schizophrenia and autism, subdivision based on the phenotype has not led to neurobiologically valid subtyping schemes. In schizophrenia, for example, most subtyping schemes have been based on the symptoms (e.g., positive vs. negative, deficit vs. non-deficit, and paranoid vs. non-paranoid), but symptom definitions are broad and imprecise and their assessment is heavily dependent on the self-report of individuals whose disorder often robs them of insight. In addition, symptoms often lack temporal stability and predictive validity (i.e., they do not provide an adequate account of variability in other important measures such as brain structure or function, disease course, or functional outcome). Moreover, neither diagnosis nor symptoms can identify syndromally unaffected relatives who carry susceptibility genes. Finally, the substantially shared genetic liability for neuropsychiatric disorders such as schizophrenia, major depressive disorder, autism spectrum disorder, attention-deficit/hyperactivity disorder and bipolar disorder (e.g., Craddock et al. 2006a; Crespi et al. 2009; Cross-Disorder Group of the Psychiatric Genomics et al. 2013; Purcell et al. 2009) reinforces the fact that our present diagnostic categories and symptom definitions do not map onto distinct underlying genetic etiologies. To the extent that genes cause psychiatric disorders and their signs and symptoms, they do so via their effects on brain function (Tan et al. 2008). Given the heterogeneity of present diagnostic categories, alternate phenotyping strategies are needed to understand the genetic origins of psychiatric disorders and to facilitate the development of more valid psychiatric nosology and more effective interventions. This imperative spurred the National Institute of Mental Health (NIMH) to implement a Research Domain Criteria Project, or ‘RDoC’ (see http://www.nimh.nih.gov/research-funding/rdoc/index.shtml) strategy. The RDoC strategy involves developing, ‘…for research purposes, new ways of classifying mental disorders based on the dimensions of observable behavior and neurobiological measures.’ RDoC encourages researchers to base their selection of subjects on neurobiologically valid dimensions that can be characterized along the causal chain from genes to molecules to circuits to behavior, rather than relying on DSM categories (Fig. 9.4 illustrates a theoretical causal chain for error processing). ‘Cognitive Systems’ is one of the broad domains identified by RDoC for study, and below, we argue that neuroimaging-based measures of cognition are more sensitive indices of genetic mechanisms than behavior.
Model of a causal pathway for error processing. Specific genetic polymorphisms affect dopamine neurotransmission, which may interact with a neuropsychiatric disorder to affect neuroimaging-based endophenotypes. These endophenotypes, in turn, contribute to the expression of phenotypes, which may influence whether a psychiatric diagnosis is given
While it is well accepted that genetic variation influences brain function and contributes to cognitive deficits in neuropsychiatric disorders, genetically mediated alterations in brain function are not always manifest at the level of behavior. Preserved behavior may reflect the use of an alternate strategy and/or the recruitment of compensatory neural circuitry. Conversely, disordered behavior may reflect not only the brain function of interest, but deficits of other systems, including of the motor output systems that are required to produce the behavior. Thus, behavior is an indirect and possibly unreliable index of genetic effects on brain function. Because brain function is a more direct index of genetic mechanisms than behavior, neuroimaging-based endophenotypes can result in increased effect sizes in studies of genetic variation. Gene effects on functional and structural neuroimaging phenotypes are often highly penetrant (e.g., Canli et al. 2005) and can be surprisingly large (e.g., Roffman et al. 2008a). This allows the investigation of substantially smaller sample sizes and makes it possible to detect significant genotype effects in the absence of overt behavioral differences (e.g., Roffman et al. 2008a). For these reasons, the study of genetic mediation using neuroimaging-based endophenotypes holds promise for uncovering susceptibility genes, mechanisms of illness, and targets for intervention (Hariri et al. 2006).
Neural markers of errors, such as the ERN, meet several important criteria as endophenotypes (Gottesman and Gould 2003) including high heritability based on both sibling (Albrecht et al. 2008) and twin (Anokhin et al. 2008) studies, established neuroanatomical and neurochemical substrates, and association with psychiatric disorders, though they are also seen in the general population (Fig. 9.5). There is also growing evidence of genetic mediation of neural error markers both in health and psychopathology.
A schematic illustration of the endophenotype concept. Shaded areas indicate the presence of the endophenotype in affected patients, individuals with spectrum disorders, syndromally unaffected family members and the general population. Criteria taken from Gould and Gottesman (2006)
6 Genetic Variation Influences Error Processing in Health and Neuropsychiatric Disorders (See Table 9.1 for a Summary)
6.1 The Role of Dopamine in Error Processing
Empirical work and theory document a critical role for the dopaminergic system, particularly D2-like DA receptors, in reinforcement learning (Schultz et al. 1997). Reinforcement learning theory has been extended to encompass error-based reinforcement learning and, as described above, both the ERN and error-related dACC activation are seen to arise from this DA-dependent mechanism (Holroyd and Coles 2002). Converging lines of evidence support a role for DA in error processing. Individuals with Parkinson’s disease, which is caused by a loss of midbrain DA neurons, have a blunted ERN (Falkenstein et al. 2001; Ito and Kitagawa 2006; Willemssen et al. 2009). Pharmacological manipulation of DA affects neural responses to errors. Haloperidol, a DA D2 receptor antagonist, blunted ERN amplitude in two studies (de Bruijn et al. 2006; Zirnheld et al. 2004), while d-amphetamine, an indirect DA agonist, increased it (de Bruijn et al. 2004). Additional support for a DA-dependent mechanism of error processing comes from findings that genetic polymorphisms affecting DA neurotransmission influence error markers in both health and neuropsychiatric disorders.
DRD2 TAQ - IA: The DA D2 receptor gene is a risk gene for schizophrenia (Shi et al. 2008) and the polymorphism, TAQ-1A (rs1800497), which is associated with schizophrenia (Parsons et al. 2007), predicts response to treatment with risperidone (Ikeda et al. 2008) and aripiprazole (Kwon et al. 2008). An fMRI study of healthy individuals (Klein et al. 2007b) found that A1-allele carriers, with putatively reduced striatal DA receptor density (Jonsson et al. 1999; Pohjalainen et al. 1998; Ritchie and Noble 2003), showed decreased dACC activation in response to errors and decreased avoidance learning, suggesting that they were less efficient in learning from errors. A1-allele carriers also showed decreased functional connectivity of the dACC and striatum. With regard to the ERN, there are conflicting reports of no association with DRD2 TAQ-IA (Althaus et al. 2009) and an increased ERN amplitude in A1-allele carriers (Meyer et al. 2012).
DRD4 C - 521T: The DA D4 receptor gene (DRD4) is also a candidate gene for schizophrenia (Shi et al. 2008) and the -521 single nucleotide polymorphism (SNP) refers to a C-to-T substitution in the DRD4 promoter region (rs1800955) with the T allele resulting in 40% less transcriptional efficiency (Okuyama et al. 1999). The DRD4-521C allele has been associated with schizophrenia (Allen et al. 2008; Okuyama et al. 1999; Xing et al. 2003) and healthy individuals homozygous for the C allele showed a decreased ERN and decreased post-error slowing compared to T homozygotes (Kramer et al. 2007).
DRD4 exon 3 VNTR: Another DRD4 polymorphism linked to error processing consists of a variable number of tandem repeats of a 48-base-pair sequence in the third exon (Van Tol et al. 1992). The most frequently occurring numbers of repeats are 4 (4R; 70%), 7 (7R; 20%), and 2 (2R; 5%) (Asghari et al. 1995). The 7R allele has been associated with higher risk of OCD (Taj et al. 2013), with tics in OCD (Cruz et al. 1997), and with reduced ERN amplitude, but comparable Pe (Biehl et al. 2011).
The DA transporter (DAT1) 3′-UTR VNTR: DAT1 plays a key role in regulating DA neurotransmission by facilitating reuptake of DA in the synaptic cleft (Jaber et al. 1997). A polymorphism in the 3′-untranslated region (3′-UTR) of this gene consists of a variable number of tandem repeats of a 40-base-pair sequence, ranging from 3 to 11 copies of the repeated sequence, with the most common variants being 9 (9R; 24%) and 10 (10R; 70%) repeats (Vandenbergh et al. 1992). Carriers of the 9R allele have increased levels of DAT1 in the striatum (van de Giessen et al. 2009; van Dyck et al. 2005) and a trend for increased risk of OCD based on the meta-analysis (Liu et al. 2012). The 9R allele has also been associated with a larger ERN (referred to as ΔERN in Meyer et al. 2012), and a larger Pe in one study (Althaus et al. 2010), but a smaller Pe in a second study (Biehl et al. 2011).
COMT Val 158 Met: A G-to-A SNP in the catechol-O-methyltransferase (COMT) gene leads to a valine-to-methionine substitution (COMT Val 158 Met, rs4680). COMT metabolizes released DA and the Met allele significantly reduces COMT activity, leading to higher DA. The COMT Val 158 Met polymorphism has been studied extensively in relation to schizophrenia, and several meta-analyses have argued against association (Fan et al. 2005; Munafo et al. 2005; Okochi et al. 2009). While COMT Val 158 Met primarily affects DA availability in the prefrontal cortex (Craddock et al. 2006b; Egan et al. 2001), it may also have downstream effects on midbrain DA (Meyer-Lindenberg et al. 2005). Studies of error processing have yielded inconsistent findings, showing an increased amplitude of the ERN in Val-allele carriers (Osinsky et al. 2012), only a trend-level enhancement of the ERN in Val compared to Met homozygotes (Kramer et al. 2007), and no effect of COMT Val 158 Met on the ERN but an increased Pe in Met homozygotes compared to Val carriers (Frank et al. 2007).
MTHFR 677C > T: The hypofunctional 677T variant in the methylenetetrahydrofolate reductase gene (MTHFR 677C>T, rs1801133) has been associated with increased risk for schizophrenia (Allen et al. 2008; Gilbody et al. 2007), executive dysfunction (Roffman et al. 2008b), and negative symptoms (Roffman et al. 2008c). Several steps in the DA life cycle rely on methylation reactions regulated by MTHFR (Friso et al. 2002) and each copy of the T allele reduces MTHFR activity by 35% (Frosst et al. 1995). The T allele has been shown to reduce dorsolateral prefrontal cortex fMRI activation during working memory performance in schizophrenia, both on its own, and via epistatic interactions with the low-DA COMT 158Val allele, supporting a role of MTHFR in prefrontal DA signaling (Roffman et al. 2008a). There is also indirect evidence linking MTHFR to striatal DA. MTHFR is a key enzyme in the metabolism of homocysteine, which has toxic effects on DA neurons in the striatum of rats (Imamura et al. 2007). In alcohol-dependent individuals, MTHFR 677T has been associated with higher plasma levels of homocysteine and increased risk of withdrawal seizures, which were interpreted to reflect the neurotoxic effects of homocysteine on the mesencephalic DA system (Lutz 2008; Lutz et al. 2006, 2007).
In a prior study of executive function in schizophrenia (Roffman et al. 2008b), MTHFR 677T was specifically related to a behavioral index of error processing, namely increased perseverative errors on the Wisconsin Card Sort Test, which reflect a failure to use feedback to adjust behavior. Recent work has demonstrated significant 677T-allele-related reductions in error-related fMRI activation of the dACC in healthy individuals and in two independent samples of patients with schizophrenia (Roffman et al. 2011a, b). The reductions in dACC activation were linearly related to allele dose regardless of diagnosis (Roffman et al. 2011a). This suggests that MTHFR 677T mediates error processing in both health and schizophrenia.
6.2 Other Genetic Variation Related to Error Processing
The serotonin transporter gene (5-HTTLPR): Evidence linking serotonin to ACC function and structure comes from studies of a functional length variation in the transcriptional control region of the serotonin transporter gene in healthy individuals. This polymorphism was associated with differences in the anatomy and function of the amygdala-rACC circuit in healthy individuals (Pezawas et al. 2005), which has been implicated in generating and learning from negative affect (for review, see Baxter and Murray 2002; Drevets 2000; Zald 2003). This learning may extend to errors since both rACC and amygdala respond to errors, and together, activation in these structures predicts error rate (Polli et al. 2008, 2009).
More direct evidence of a role for this polymorphism in error processing are findings of a significantly increased ERN amplitude and a trend to increased Pe amplitude in short allele homozygotes, who presumably produce less serotonin transporter transcript, compared to long allele homozygotes (Fallgatter et al. 2004). A larger study, however, failed to replicate the association of 5-HTTLPR genotype with ERN amplitude (Olvet et al. 2010).
5-HT1A receptor gene C-1019G: A SNP present in about a third of the population consisting of an extra base pair in the promoter region of the 5-HT1A receptor gene (C-1019G, rs6295) has been associated with reduced ERN and post-error slowing (Beste et al. 2010). The presence of a guanine nucleotide prevents binding of repressor proteins, which leads to enhanced gene expression and reduced serotonergic transmission (Lemonde et al. 2003). The G allele has been linked to increased risk of schizophrenia (Huang et al. 2004) and to worse treatment outcomes (Mossner et al. 2009; Reynolds et al. 2006), but a meta-analysis reported no association with schizophrenia (Kishi et al. 2011).
BDNF Val 66 Met: The brain-derived neurotrophic factor (BDNF) is a nerve growth factor thought to facilitate synaptic connections in the brain (Cohen-Cory et al. 1996). A SNP in the eponymous gene, which encodes for BDNF, results in valine-to-methionine substitution in the prodomain of the protein (BDNF Val 66 Met, rs6265) that leads to reduced activity-dependent secretion of BDNF (Egan et al. 2003). One meta-analysis found an elevated risk for schizophrenia in homozygous Met carriers (Gratacos et al. 2007), but another did not (Kanazawa et al. 2007). The Met allele has been associated with earlier onset of schizophrenia (Chao et al. 2008) and reductions of ERN amplitude and post-error slowing (Beste et al. 2012).
NPSR Asn 107 Ile: Neuropeptide S (NPS) is a 20 amino acid peptide that modulates stress and arousal (Okamura and Reinscheid 2007). An A-to-T substitution at position 107 of the gene encoding for the NPS receptor (NPSR) leads to an amino acid exchange from Asn to Ile (Asn107Ile, rs324981) and increases the efficacy of NPS about tenfold (Reinscheid et al. 2005). The T allele is thought to be related to anxiety disorders, particularly panic disorder (Domschke et al. 2011), and is associated with an increased ERN and more pronounced post-error slowing (Beste et al. 2013).
7 Challenges to the Study of Neural Indices Error Processing as Endophenotypes
7.1 Failures of Replication in Imaging-Genetics Studies
Failures of replication are extremely common in imaging-genetics studies and represent a major challenge. Imaging-genetics findings are often based on relatively small samples, and negative results are much less likely to be published. Smaller samples are often justified based on the evidence that neuroimaging-based endophenotypes result in increased effect sizes in studies of genetic variation than behavior or diagnosis. The pragmatic justification is that neuroimaging studies are costly and require considerable infrastructure to accomplish. Relatively small and comprehensive studies can identify the most promising cognitive constructs and endophenotypes, which can then be exported for use in larger multisite studies of patients, relatives, and racially and ethnically homogeneous groups as has been done for studies of other putative cognitive endophenotypes (e.g., Radant et al. 2010; Turetsky et al. 2008). Studies in developing countries such as China can complement and extend these efforts by identifying overlapping and distinct genetic contributions in non-Western populations (e.g., Chan et al. 2010). To protect against false-positive associations in smaller studies, it is often advisable to investigate the effects of only a limited set of polymorphisms that are selected based on stringent criteria and to seek convergence in the data. This strategy can maximize scientific yield while minimizing the risk of spurious findings by focusing on a hypothesis-driven set of loci that affect specific neural mechanisms and are most likely to affect a particular endophenotype or set of related endophenotypes given the current state of knowledge. A limitation to this approach is that it will not represent the full complement of genes that influence the phenotypes of interest.
7.2 Methodological Differences Across Studies May Lead to Conflicting Findings
A major challenge in the error processing literature is that the definition and measurement of neural indices of error processing vary across studies. The ERN, for example, can be defined based on the peak of negativity in either the error waveform alone or in the difference (error vs. correct) waveform. It is arguable which method is more valid. Such measurement differences can affect study outcomes as can be illustrated in OCD, which is characterized by exaggerated neural responses on both correct and error trials. Several studies reporting an increased ERN in OCD, or in non-clinical populations with OCD symptoms defined it using only the error trial (Endrass et al. 2008, 2010; Gehring et al. 2000; Hajcak and Simons 2002; Johannes et al. 2001). In at least two of these studies, the waveform for correct trials was also more negative in OCD participants than controls (referred to as the correct-related negativity or CRN). Consequently, had the ERN been defined as the difference waveform, it might not have been greater in OCD patients than controls.
Methodological differences may also contribute to discrepancies in fMRI results. For example, most standard fMRI analysis techniques assume a shape to the hemodynamic response. While this is a statistically powerful technique when the models are correct, a single assumed model is unlikely to be valid across all brain regions and stimulus types (Duann et al. 2002) and, importantly, model inaccuracies may lead to the misattribution of activity to adjacent events (Manoach et al. 2003). Thus, it is possible that in some studies, increased ACC activation on error trials may reflect greater activation while planning or preparing the response rather than an exaggerated response to the error. Finite impulse response (FIR, Burock and Dale 2000; Jansma et al. 2013) or other models that make no a priori assumptions about the shape of the hemodynamic response may more accurately distinguish preparatory activation from error-related activation and can also be used to evaluate the temporal characteristics of the hemodynamic response, which may differ between the study groups (e.g., Dyckman et al. 2011).
Conflicting findings of error processing deficits in particular disorders may also arise from the use of different tasks and levels of difficulty. The characteristics of the samples studied such as whether certain symptoms are present, treatment with medications, and task performance also matter (e.g., Mathews et al. 2012). By affecting neurotransmitter systems that mediate error responses, medications such as antipsychotics, selective serotonin reuptake inhibitors, and antidepressants may affect outcome measures and obscure group differences and effects of genetic variation. Task performance is also important to consider in evaluating error indices. More frequent errors are also more predictable, and ERN amplitude is thought to code the degree to which errors are unexpected (Brown and Braver 2005; Holroyd and Coles 2002), consistent with findings of inverse correlations between error rate and ERN amplitude (Agam et al. 2011; Gehring et al. 1993; Hajcak et al. 2003). The same may be true for dACC activation, which also correlates with error rate in some studies (e.g., Polli et al. 2008). Thus, different error rates in patient and control samples or in pre- and post-treatment conditions (e.g., Sokhadze et al. 2012a) represent a potential confound that could be statistically controlled (e.g., Polli et al. 2008). For example, in several ERN studies, ASD participants had a higher error rate than controls (e.g., Sokhadze et al. 2010, 2012b; South et al. 2010), making it unclear whether the blunted ERN reflected more frequent errors or deficient error recognition and signaling.
7.3 Limitations to the Clinical Utility of Error Processing Endophenotypes
Unlike neurodegenerative disorders such as Alzheimer’s disease, which are associated with specific neuropathologies, neuropsychiatric disorders likely have multiple overlapping etiologies and neuropathologies. Consequently, neuropsychiatric disorders lack sensitive and specific pathophysiological markers such as amyloid beta-protein, which is specific to Alzheimer’s disease, is thought to cause the associated dementia, and can be measured in vivo to assess the risk of developing symptoms and response to therapy (Klunk 2011). Error processing endophenotypes, in contrast to amyloid beta-protein, do not index a known, specific neuropathology, rather they may indicate cognitive dysfunction and genetic vulnerability to illness and their diagnostic specificity remains to be established. Also, unlike amyloid beta-protein, whose presence is usually associated with pathology, neural error markers are normally present and abnormality is defined as statistical deviation of their parameters from the norm, which varies from study to study. Measurement variability, the lack of consensus definitions of error markers, and the absence of large-scale studies make it difficult to define clear cutoffs for ‘normality.’ In addition, error processing endophenotypes, such as a blunted or exaggerated ERN or error-related dACC activation, are only probabilistically associated with illness, they do not determine illness. The cognitive dysfunction that they index may make illness more probable, but is likely just one of a number of cumulative hits of relatively small effect. Given that we lack a comprehensive understanding of the genetic contributions to these markers, it is difficult to distinguish ‘false positives’ (i.e., abnormal error markers in the absence of genetic risk in an otherwise healthy individual) from valid genetic vulnerability for a disorder that has not manifested itself for environmental reasons or due to other, protective, epigenetic, or genetic factors. Similarly, because endophenotypes are only probabilistically related to illness and current diagnostic categories are heterogeneous, they may only be present in a subset of individuals within a given diagnostic group.
Establishing the clinical relevance of error processing deficits: While there is clear evidence that deficient error processing is associated with symptoms and functional outcome in neuropsychiatric disorders, further research is required to fully elaborate the bases of these relations both within and across the disorders. If, as we and others have proposed, deficient error processing mediates the pathway between genetic predisposition and illness by interfering with adaptive responses to outcomes (e.g., Olvet and Hajcak 2008), early intervention and prevention may be possible, for example, in individuals at high risk for schizophrenia who show a blunted ERN (e.g., Laurens et al. 2009; Perez et al. 2012; Simmonite et al. 2012). It may also be possible to intervene to prevent relapse. Two recent studies demonstrate that error-related dACC activation predicts relapse and time to relapse in cocaine-dependent individuals (Luo et al. 2013) and recidivism in criminal offenders (Aharoni et al. 2013). These findings provide a rationale for the development of interventions to ameliorate error processing deficits in neuropsychiatric disorders as well as other populations characterized by repetitive, maladaptive behaviors.
8 Conclusion
The existing literature on error processing allows the generation of biologically plausible hypotheses concerning the effects of genetic variation on well-validated and heritable indices of error processing that are abnormal in neuropsychiatric disorders, show evidence of diagnostic specificity, contribute to disability, and are thought to be mediated by specific neural mechanisms. Understanding the genetic mediation and mechanisms of error processing deficits in neuropsychiatric disorders may eventually lead to the development of specifically targeted interventions and enable the use genetic information to identify individuals most likely to benefit from these treatments. This can substantially reduce outcome variability, thereby increasing power, and reducing the required sample size and cost of treatment trials. The findings of imaging-genetics investigations may also provide novel neural and behavioral targets for treatment and sensitive surrogate markers of treatment response. Treating error processing deficits may significantly affect functional outcome in neuropsychiatric disorders or possibly even prevent onset or relapse since error signals provide crucial information for flexible adaptation to changing environments, and deficits in learning from errors, as indexed by abnormal neural responses and reduced behavioral adaptation, likely substantially contribute to rigid, perseverative, and maladaptive patterns of behavior. Given the dearth of effective interventions for cognitive deficits in neuropsychiatric disorders, this represents a promising approach.
References
Agam Y, Hamalainen MS, Lee AK et al (2011) Multimodal neuroimaging dissociates hemodynamic and electrophysiological correlates of error processing. Proc Natl Acad Sci U S A 108(42):17556–17561
Agam Y, Carey C, Barton JJS et al (in press) Network dynamics underlying speed-accuracy trade-offs in response to errors. PLoS One 12;8(9):e73692
Agartz I, Andersson JL, Skare S (2001) Abnormal brain white matter in schizophrenia: a diffusion tensor imaging study. NeuroReport 12(10):2251–2254
Aharoni E, Vincent GM, Harenski CL et al (2013) Neuroprediction of future rearrest. Proc Natl Acad Sci U S A 9;110(15):6223–6228
Alain C, McNeely HE, He Y et al (2002) Neurophysiological evidence of error-monitoring deficits in patients with schizophrenia. Cereb Cortex 12(8):840–846
Albrecht B, Brandeis D, Uebel H et al (2008) Action monitoring in boys with attention-deficit/hyperactivity disorder, their nonaffected siblings, and normal control subjects: evidence for an endophenotype. Biol Psychiatry 64(7):615–625
Allen NC, Bagade S, McQueen MB et al (2008) Systematic meta-analyses and field synopsis of genetic association studies in schizophrenia: the SzGene database. Nat Genet 40(7):827–834
Althaus M, Groen Y, Wijers AA et al (2009) Differential effects of 5-HTTLPR and DRD2/ANKK1 polymorphisms on electrocortical measures of error and feedback processing in children. Clin Neurophysiol 120(1):93–107
Althaus M, Groen Y, Wijers AA et al (2010) Variants of the SLC6A3 (DAT1) polymorphism affect performance monitoring-related cortical evoked potentials that are associated with ADHD. Biol Psychol 85(1):19–32
Andalman AS, Fee MS (2009) A basal ganglia-forebrain circuit in the songbird biases motor output to avoid vocal errors. Proc Natl Acad Sci U S A 106(30):12518–12523
Anokhin AP, Golosheykin S, Heath AC (2008) Heritability of frontal brain function related to action monitoring. Psychophysiology 45(4):524–534
Ardekani BA, Nierenberg J, Hoptman MJ et al (2003) MRI study of white matter diffusion anisotropy in schizophrenia. NeuroReport 14(16):2025–2029
Asghari V, Sanyal S, Buchwaldt S et al (1995) Modulation of intracellular cyclic AMP levels by different human dopamine D4 receptor variants. J Neurochem 65(3):1157–1165
Barnea-Goraly N, Kwon H, Menon V et al (2004) White matter structure in autism: preliminary evidence from diffusion tensor imaging. Biol Psychiatry 55(3):323–326
Bates AT, Kiehl KA, Laurens KR et al (2002) Error-related negativity and correct response negativity in schizophrenia. Clin Neurophysiol 113(9):1454–1463
Baxter MG, Murray EA (2002) The amygdala and reward. Nat Rev Neurosci 3(7):563–573
Benes FM (1993) Neurobiological investigations in cingulate cortex of schizophrenic brain. Schizophr Bull 19(3):537–549
Benes FM (2000) Emerging principles of altered neural circuitry in schizophrenia. Brain Res Brain Res Rev 31(2–3):251–269
Beste C, Domschke K, Kolev V et al (2010) Functional 5-HT1a receptor polymorphism selectively modulates error-specific subprocesses of performance monitoring. Hum Brain Mapp 31(4):621–630
Beste C, Kolev V, Yordanova J et al (2012) The role of the BDNF Val66Met polymorphism for the synchronization of error-specific neural networks. J Neurosci 30(32):10727–10733
Beste C, Konrad C, Uhlmann C et al (2013) Neuropeptide S receptor (NPSR1) gene variation modulates response inhibition and error monitoring. Neuroimage 71:1–9
Biehl SC, Dresler T, Reif A et al (2011) Dopamine transporter (DAT1) and dopamine receptor D4 (DRD4) genotypes differentially impact on electrophysiological correlates of error processing. PLoS ONE 6(12):e28396
Bishop SL, Richler J, Cain AC et al (2007) Predictors of perceived negative impact in mothers of children with autism spectrum disorder. Am J Ment Retard 112(6):450–461
Bogte H, Flamma B, van der Meere J et al (2007) Post-error adaptation in adults with high functioning autism. Neuropsychologia 45(8):1707–1714
Brazdil M, Roman R, Falkenstein M et al (2002) Error processing–evidence from intracerebral ERP recordings. Exp Brain Res 146(4):460–466
Breiter HC, Rauch SL, Kwong KK et al (1996) Functional magnetic resonance imaging of symptom provocation in obsessive-compulsive disorder. Arch Gen Psychiatry 53(7):595–606
Brown JW, Braver TS (2005) Learned predictions of error likelihood in the anterior cingulate cortex. Science 307(5712):1118–1121
Broyd SJ, Demanuele C, Debener S et al (2009) Default-mode brain dysfunction in mental disorders: a systematic review. Neurosci Biobehav Rev 33(3):279–296
Buchsbaum MS, Tang CY, Peled S et al (1998) MRI white matter diffusion anisotropy and PET metabolic rate in schizophrenia. NeuroReport 9(3):425–430
Buckner RL, Andrews-Hanna JR, Schacter DL (2008) The brain’s default network: anatomy, function, and relevance to disease. Ann N Y Acad Sci 1124:1–38
Burns J, Job D, Bastin ME et al (2003) Structural disconnectivity in schizophrenia: a diffusion tensor magnetic resonance imaging study. Br J Psychiatry 182:439–443
Burock MA, Dale AM (2000) Estimation and detection of event-related fMRI signals with temporally correlated noise: a statistically efficient and unbiased approach. Hum Brain Mapp 11(4):249–260
Bush G, Whalen PJ, Rosen BR et al (1998) The counting stroop: an interference task specialized for functional neuroimaging—validation study with functional MRI. Hum Brain Mapp 6(4):270–282
Bush G, Luu P, Posner MI (2000) Cognitive and emotional influences in anterior cingulate cortex. Trends Cogn Sci 4(6):215–222
Canli T, Omura K, Haas BW et al (2005) Beyond affect: a role for genetic variation of the serotonin transporter in neural activation during a cognitive attention task. Proc Natl Acad Sci U S A 102(34):12224–12229
Carrasco M, Harbin SM, Nienhuis JK et al (2013) Increased error-related brain activity in youth with obsessive-compulsive disorder and unaffected siblings. Depress Anxiety 30(1):39–46
Carter CS, MacDonald AW 3rd, Ross LL et al (2001) Anterior cingulate cortex activity and impaired self-monitoring of performance in patients with schizophrenia: an event-related fMRI study. Am J Psychiatry 158(9):1423–1428
Chan RC, Gottesman II, Ge X et al (2010) Strategies for the study of neuropsychiatric disorders using endophenotypes in developing countries: a potential databank from China. Front Hum Neurosci 4:207
Chao HM, Kao HT, Porton B (2008) BDNF Val66Met variant and age of onset in schizophrenia. Am J Med Genet B Neuropsychiatr Genet 147B(4):505–506
Cheng Y, Chou KH, Chen IY et al (2010) Atypical development of white matter microstructure in adolescents with autism spectrum disorders. Neuroimage 50(3):873–882
Cohen-Cory S, Escandon E, Fraser SE (1996) The cellular patterns of BDNF and trkB expression suggest multiple roles for BDNF during Xenopus visual system development. Dev Biol 179(1):102–115
Craddock N, O’Donovan MC, Owen MJ (2006a) Genes for schizophrenia and bipolar disorder? Implications for psychiatric nosology. Schizophr Bull 32(1):9–16
Craddock N, Owen MJ, O’Donovan MC (2006b) The catechol-O-methyl transferase (COMT) gene as a candidate for psychiatric phenotypes: evidence and lessons. Mol Psychiatry 11(5):446–458
Crespi B, Stead P, Elliot M (2009) Evolution in health and medicine Sackler colloquium: comparative genomics of autism and schizophrenia. Proc Natl Acad Sci U S A 26(107 Suppl 1):1736–1741
Cross-Disorder Group of the Psychiatric Genomics Consortium, Smoller JW, Craddock N et al (2013) Identification of risk loci with shared effects on five major psychiatric disorders: a genome-wide analysis. Lancet 381(9875):1371–1379
Cruz C, Camarena B, King N et al (1997) Increased prevalence of the seven-repeat variant of the dopamine D4 receptor gene in patients with obsessive-compulsive disorder with tics. Neurosci Lett 231(1):1–4
de Bruijn ER, Hulstijn W, Verkes RJ et al (2004) Drug-induced stimulation and suppression of action monitoring in healthy volunteers. Psychopharmacology 177(1–2):151–160
de Bruijn ER, Sabbe BG, Hulstijn W et al (2006) Effects of antipsychotic and antidepressant drugs on action monitoring in healthy volunteers. Brain Res 1105(1):122–129
Debener S, Ullsperger M, Siegel M et al (2005) Trial-by-trial coupling of concurrent electroencephalogram and functional magnetic resonance imaging identifies the dynamics of performance monitoring. J Neurosci 25(50):11730–11737
Dehaene S, Posner MI, Tucker DM (1994) Localization of a neural system for error detection and compensation. Psychol Sci 5(5):303–305
Devinsky O, Morrell MJ, Vogt BA (1995) Contributions of anterior cingulate cortex to behaviour. Brain 118(Pt 1):279–306
Domschke K, Reif A, Weber H et al (2011) Neuropeptide S receptor gene—converging evidence for a role in panic disorder. Mol psychiatry 16(9):938–948
Donamayor N, Marco-Pallares J, Heldmann M et al (2011) Temporal dynamics of reward processing revealed by magnetoencephalography. Hum Brain Mapp 32(12):2228–2240
Dougherty DD, Baer L, Cosgrove GR et al (2002) Prospective long-term follow-up of 44 patients who received cingulotomy for treatment-refractory obsessive-compulsive disorder. Am J Psychiatry 159(2):269–275
Drevets WC (2000) Neuroimaging studies of mood disorders. Biol Psychiatry 48(8):813–829
Drevets WC, Raichle ME (1998) Reciprocal suppression of regional cerebral blood flow during emotional versus higher cognitive processes: implications for interactions between emotion and cognition. Cognit Emot 12(3):353–385
Duann JR, Jung TP, Kuo WJ et al (2002) Single-trial variability in event-related BOLD signals. Neuroimage 15(4):823–835
Dyckman KA, Lee AKC, Agam Y et al (2011) Abnormally persistent fMRI activation during antisaccades in schizophrenia: a neural correlate of perseveration? Schizophr Res 132(1):62–68
Egan MF, Goldberg TE, Kolachana BS et al (2001) Effect of COMT Val108/158 Met genotype on frontal lobe function and risk for schizophrenia. Proc Natl Acad Sci U S A 98(12):6917–6922
Egan MF, Kojima M, Callicott JH et al (2003) The BDNF val66met polymorphism affects activity-dependent secretion of BDNF and human memory and hippocampal function. Cell 112(2):257–269
Eichele T, Debener S, Calhoun VD et al (2008) Prediction of human errors by maladaptive changes in event-related brain networks. Proc Natl Acad Sci U S A 105(16):6173–6178
Endrass T, Franke C, Kathmann N (2005) Error awareness in a saccade countermanding task. J Psychophysiol 19(4):275–280
Endrass T, Reuter B, Kathmann N (2007) ERP correlates of conscious error recognition: aware and unaware errors in an antisaccade task. Eur J Neurosci 26(6):1714–1720
Endrass T, Klawohn J, Schuster F et al (2008) Overactive performance monitoring in obsessive-compulsive disorder: ERP evidence from correct and erroneous reactions. Neuropsychologia 46(7):1877–1887
Endrass T, Schuermann B, Kaufmann C et al (2010) Performance monitoring and error significance in patients with obsessive-compulsive disorder. Biol Psychol 84(2):257–263
Eriksen BA, Eriksen CW (1974) Effects of noise letters upon the identification of a target letter in a nonsearch task. Percept Psychophys 16:143–149
Falkenstein M, Hohnsbein J, Hoormann J et al (1991) Effects of crossmodal divided attention on late ERP components. II. Error processing in choice reaction tasks. Electroencephalogr Clin Neurophysiol 78(6):447–455
Falkenstein M, Hielscher H, Dziobek I et al (2001) Action monitoring, error detection, and the basal ganglia: an ERP study. NeuroReport 12(1):157–161
Fallgatter AJ, Herrmann MJ, Roemmler J et al (2004) Allelic variation of serotonin transporter function modulates the brain electrical response for error processing. Neuropsychopharmacology 29(8):1506–1511
Fan JB, Zhang CS, Gu NF et al (2005) Catechol-O-methyltransferase gene Val/Met functional polymorphism and risk of schizophrenia: a large-scale association study plus meta-analysis. Biol Psychiatry 57(2):139–144
Fassbender C, Murphy K, Foxe JJ et al (2004) A topography of executive functions and their interactions revealed by functional magnetic resonance imaging. Brain Res Cogn Brain Res 20(2):132–143
Fiehler K, Ullsperger M, von Cramon DY (2005) Electrophysiological correlates of error correction. Psychophysiology 42(1):72–82
Fitzgerald KD, Welsh RC, Gehring WJ et al (2005) Error-related hyperactivity of the anterior cingulate cortex in obsessive-compulsive disorder. Biol Psychiatry 57(3):287–294
Fitzgerald KD, Perkins SC, Angstadt M et al (2010) The development of performance-monitoring function in the posterior medial frontal cortex. Neuroimage 49(4):3463–3473
Foong J, Symms MR, Barker GJ et al (2002) Investigating regional white matter in schizophrenia using diffusion tensor imaging. NeuroReport 13(3):333–336
Fornito A, Yung AR, Wood SJ et al (2008) Anatomic abnormalities of the anterior cingulate cortex before psychosis onset: an MRI study of ultra-high-risk individuals. Biol Psychiatry 64(9):758–765
Foti D, Kotov R, Bromet E et al (2012) Beyond the broken error-related negativity: functional and diagnostic correlates of error processing in psychosis. Biol Psychiatry 71(10):864–872
Frank MJ, D’Lauro C, Curran T (2007) Cross-task individual differences in error processing: neural, electrophysiological, and genetic components. Cogn Affect Behav Neurosci 7(4):297–308
Friso S, Choi SW, Girelli D et al (2002) A common mutation in the 5,10-methylenetetrahydrofolate reductase gene affects genomic DNA methylation through an interaction with folate status. Proc Natl Acad Sci U S A 99(8):5606–5611
Frosst P, Blom HJ, Milos R et al (1995) A candidate genetic risk factor for vascular disease: a common mutation in methylenetetrahydrofolate reductase. Nat Genet 10(1):111–113
Fujiwara J, Tobler PN, Taira M et al (2009) Segregated and integrated coding of reward and punishment in the cingulate cortex. J Neurophysiol 101(6):3284–3293
Garavan H, Ross TJ, Murphy K et al (2002) Dissociable executive functions in the dynamic control of behavior: inhibition, error detection, and correction. NeuroImage 17(4):1820–1829
Gehring WJ, Fencsik DE (2001) Functions of the medial frontal cortex in the processing of conflict and errors. J Neurosci 21(23):9430–9437
Gehring WJ, Goss B, Coles MG et al (1993) A neural system for error detection and compensation. Psychol Sci 4(6):385–390
Gehring WJ, Himle J, Nisenson LG (2000) Action-monitoring dysfunction in obsessive-compulsive disorder. Psychol Sci 11(1):1–6
Gilbody S, Lewis S, Lightfoot T (2007) Methylenetetrahydrofolate reductase (MTHFR) genetic polymorphisms and psychiatric disorders: a HuGE review. Am J Epidemiol 165(1):1–13
Goldberg TE, Weinberger DR, Berman KF et al (1987) Further evidence for dementia of the prefrontal type in schizophrenia? A controlled study of teaching the Wisconsin Card Sorting Test [see comments]. Arch Gen Psychiatry 44(11):1008–1014
Goldberg MC, Spinelli S, Joel S et al (2011) Children with high functioning autism show increased prefrontal and temporal cortex activity during error monitoring. Dev Cogn Neurosci 1(1):47–56
Goldstein JM, Goodman JM, Seidman LJ et al (1999) Cortical abnormalities in schizophrenia identified by structural magnetic resonance imaging. Arch Gen Psychiatry 56(6):537–547
Gottesman II, Gould TD (2003) The endophenotype concept in psychiatry: etymology and strategic intentions. Am J Psychiatry 160(4):636–645
Gould TD, Gottesman II (2006) Psychiatric endophenotypes and the development of valid animal models. Genes Brain Behav 5(2):113–119
Gratacos M, Gonzalez JR, Mercader JM et al (2007) Brain-derived neurotrophic factor Val66Met and psychiatric disorders: meta-analysis of case-control studies confirm association to substance-related disorders, eating disorders, and schizophrenia. Biol Psychiatry 61(7):911–922
Groen Y, Wijers AA, Mulder LJ et al (2008) Error and feedback processing in children with ADHD and children with Autistic Spectrum Disorder: an EEG event-related potential study. Clin Neurophysiol 119(11):2476–2493
Ha TH, Youn T, Ha KS et al (2004) Gray matter abnormalities in paranoid schizophrenia and their clinical correlations. Psychiatry Res 132(3):251–260
Hajcak G, Simons RF (2002) Error-related brain activity in obsessive-compulsive undergraduates. Psychiatry Res 110(1):63–72
Hajcak G, McDonald N, Simons RF (2003) To err is autonomic: error-related brain potentials, ANS activity, and post-error compensatory behavior. Psychophysiology 40(6):895–903
Hajcak G, McDonald N, Simons RF (2004) Error-related psychophysiology and negative affect. Brain Cogn 56(2):189–197
Hallett PE (1978) Primary and secondary saccades to goals defined by instructions. Vision Res 18(10):1279–1296
Hao Y, Liu Z, Jiang T et al (2006) White matter integrity of the whole brain is disrupted in first-episode schizophrenia. NeuroReport 17(1):23–26
Hariri AR, Drabant EM, Weinberger DR (2006) Imaging genetics: perspectives from studies of genetically driven variation in serotonin function and corticolimbic affective processing. Biol Psychiatry 59(10):888–897
Henderson H, Schwartz C, Mundy P et al (2006) Response monitoring, the error-related negativity, and differences in social behavior in autism. Brain Cogn 61(1):96–109
Herrmann MJ, Rommler J, Ehlis AC et al (2004) Source localization (LORETA) of the error-related-negativity (ERN/Ne) and positivity (Pe). Brain Res Cogn Brain Res 20(2):294–299
Holroyd CB, Coles MG (2002) The neural basis of human error processing: reinforcement learning, dopamine, and the error-related negativity. Psychol Rev 109(4):679–709
Holroyd CB, Dien J, Coles MG (1998) Error-related scalp potentials elicited by hand and foot movements: evidence for an output-independent error-processing system in humans. Neurosci Lett 242(2):65–68
Holroyd CB, Nieuwenhuis S, Yeung N et al (2003) Errors in reward prediction are reflected in the event-related brain potential. NeuroReport 14(18):2481–2484
Holroyd CB, Larsen JT, Cohen JD (2004a) Context dependence of the event-related brain potential associated with reward and punishment. Psychophysiology 41(2):245–253
Holroyd CB, Nieuwenhuis S, Yeung N et al (2004b) Dorsal anterior cingulate cortex shows fMRI response to internal and external error signals. Nat Neurosci 7(5):497–498
Huang YY, Battistuzzi C, Oquendo MA et al (2004) Human 5-HT1A receptor C(-1019)G polymorphism and psychopathology. Int J Neuropsychoph 4:441–451
Ikeda M, Yamanouchi Y, Kinoshita Y et al (2008) Variants of dopamine and serotonin candidate genes as predictors of response to risperidone treatment in first-episode schizophrenia. Pharmacogenomics 9(10):1437–1443
Imamura K, Takeshima T, Nakaso K et al (2007) Homocysteine is toxic for dopaminergic neurons in primary mesencephalic culture. NeuroReport 18(13):1319–1322
Ito J, Kitagawa J (2006) Performance monitoring and error processing during a lexical decision task in patients with Parkinson’s disease. J Geriatr Psychiatry Neurol 19(1):46–54
Jaber M, Jones S, Giros B et al (1997) The dopamine transporter: a crucial component regulating dopamine transmission. Mov Disord 12(5):629–633
Jacobson S, Kelleher I, Harley M et al (2009) Structural and functional brain correlates of subclinical psychotic symptoms in 11–13 year old schoolchildren. Neuroimage
Jansma JM, de Zwart JA, van Gelderen P et al (2013) In vivo evaluation of the effect of stimulus distribution on FIR statistical efficiency in event-related fMRI. J Neurosci Methods 215(2):190–195
Johannes S, Wieringa BM, Nager W et al (2001) Discrepant target detection and action monitoring in obsessive-compulsive disorder. Psychiatry Res 108(2):101–110
Jonsson EG, Nothen MM, Grunhage F et al (1999) Polymorphisms in the dopamine D2 receptor gene and their relationships to striatal dopamine receptor density of healthy volunteers. Mol Psychiatry 4(3):290–296
Kaczkurkin AN (2013) The effect of manipulating task difficulty on error-related negativity in individuals with obsessive-compulsive symptoms. Biol Psychol 93(1):122–131
Kanazawa T, Glatt SJ, Kia-Keating B et al (2007) Meta-analysis reveals no association of the Val66Met polymorphism of brain-derived neurotrophic factor with either schizophrenia or bipolar disorder. Psychiatric Genet 17(3):165–170
Keil J, Weisz N, Paul-Jordanov I et al (2010) Localization of the magnetic equivalent of the ERN and induced oscillatory brain activity. Neuroimage 51(1):404–411
Kerns JG, Cohen JD, MacDonald AW 3rd et al (2004) Anterior cingulate conflict monitoring and adjustments in control. Science 303:1023–1026
Kerns JG, Cohen JD, MacDonald AW 3rd et al (2005) Decreased conflict- and error-related activity in the anterior cingulate cortex in subjects with schizophrenia. Am J Psychiatry 162(10):1833–1839
Kim MS, Kang SS, Shin KS et al (2006) Neuropsychological correlates of error negativity and positivity in schizophrenia patients. Psychiatry Clin Neurosci 60(3):303–311
Kishi T, Okochi T, Tsunoka T et al (2011) Serotonin 1A receptor gene, schizophrenia and bipolar disorder: an association study and meta-analysis. Psychiatry Res 185(1–2):20–26
Klein TA, Endrass T, Kathmann N et al (2007a) Neural correlates of error awareness. Neuroimage 34(4):1774–1781
Klein TA, Neumann J, Reuter M et al (2007b) Genetically determined differences in learning from errors. Science 318(5856):1642–1645
Klunk WE (2011) Amyloid imaging as a biomarker for cerebral beta-amyloidosis and risk prediction for Alzheimer dementia. Neurobiol Aging 32(Suppl 1):S20–S36
Kopp B, Rist F (1994) Error-correcting behavior in schizophrenic patients. Schizophr Res 13(1):11–22
Kopp B, Rist F (1999) An event-related brain potential substrate of disturbed response monitoring in paranoid schizophrenic patients. J Abnorm Psychol 108(2):337–346
Kramer UM, Cunillera T, Camara E et al (2007) The impact of catechol-O-methyltransferase and dopamine D4 receptor genotypes on neurophysiological markers of performance monitoring. J Neurosci 27(51):14190–14198
Kubicki M, Westin CF, Nestor PG et al (2003) Cingulate fasciculus integrity disruption in schizophrenia: a magnetic resonance diffusion tensor imaging study. Biol Psychiatry 54(11):1171–1180
Kuperberg GR, Broome MR, McGuire PK et al (2003) Regionally localized thinning of the cerebral cortex in schizophrenia. Arch Gen Psychiatry 60(9):878–888
Kwon JS, Kim E, Kang DH et al (2008) Taq1A polymorphism in the dopamine D2 receptor gene as a predictor of clinical response to aripiprazole. Eur Neuropsychopharmacol 18(12):897–907
Kyriakopoulos M, Dima D, Roiser JP et al (2012) Abnormal functional activation and connectivity in the working memory network in early-onset schizophrenia. J Am Acad Child Adolesc Psychiatry 51(9):911–920 e912
Ladouceur CD, Dahl RE, Carter CS (2007) Development of action monitoring through adolescence into adulthood: ERP and source localization. Dev Sci 10(6):874–891
Laurens KR, Ngan ET, Bates AT et al (2003) Rostral anterior cingulate cortex dysfunction during error processing in schizophrenia. Brain 126(Pt 3):610–622
Laurens KR, Hodgins S, Mould GL et al (2009) Error-related processing dysfunction in children aged 9 to 12 years presenting putative antecedents of schizophrenia. Biol Psychiatry 1;67(3):238–245
Lemonde S, Turecki G, Bakish D et al (2003) Impaired repression at a 5-hydroxytryptamine 1A receptor gene polymorphism associated with major depression and suicide. J Neurosci 23(25):8788–8799
Levy DL, Mendell NR, LaVancher CA et al (1998) Disinhibition in antisaccade performance in schizophrenia. In: Lenzenweger MF, Dworkin RH (eds) Origins and development of schizophrenia. American Psychological Association, Washington DC, pp 185–210
Li CS, Yan P, Bergquist KL et al (2007) Greater activation of the “default” brain regions predicts stop signal errors. Neuroimage 38(3):640–648
Liu Y, Gehring WJ, Weissman DH et al (2012) Trial-by-trial adjustments of cognitive control following errors and response conflict are altered in pediatric obsessive compulsive disorder. Front Psychiatry 3:41
Logan GD, Cowan WB (1984) On the ability to inhibit thought and action: a theory of an act of control. Psychol Rev 91:295–327
Luo X, Zhang S, Hu S et al (2013) Error processing and gender-shared and -specific neural predictors of relapse in cocaine dependence. Brain 136(Pt 4):1231–1244
Lutz UC (2008) Alterations in homocysteine metabolism among alcohol dependent patients—clinical, pathobiochemical and genetic aspects. Curr Drug Abuse Rev 1(1):47–55
Lutz UC, Batra A, Kolb W et al (2006) Methylenetetrahydrofolate reductase C677T-polymorphism and its association with alcohol withdrawal seizure. Alcohol Clin Exp Res 30(12):1966–1971
Lutz UC, Batra A, Wiatr G et al (2007) Significant impact of MTHFR C677T polymorphism on plasma homovanillic acid (HVA) levels among alcohol-dependent patients. Addict Biol 12(1):100–105
Luu P, Tucker DM, Derryberry D et al (2003) Electrophysiological responses to errors and feedback in the process of action regulation. Psychol Sci 14(1):47–53
Malenka RC, Angel RW, Hampton B et al (1982) Impaired central error-correcting behavior in schizophrenia. Arch Gen Psychiatry 39(1):101–107
Malenka RC, Angel RW, Thiemann S et al (1986) Central error-correcting behavior in schizophrenia and depression. Biol Psychiatry 21(3):263–273
Maltby N, Tolin DF, Worhunsky P et al (2005) Dysfunctional action monitoring hyperactivates frontal-striatal circuits in obsessive-compulsive disorder: an event-related fMRI study. Neuroimage 24(2):495–503
Manoach DS, Greve DN, Lindgren KA et al (2003) Identifying regional activity associated with temporally separated components of working memory using event-related functional MRI. Neuroimage 20(3):1670–1684
Manoach DS, Ketwaroo GA, Polli FE et al (2007) Reduced microstructural integrity of the white matter underlying anterior cingulate cortex is associated with increased saccadic latency in schizophrenia. Neuroimage 37(2):599–610
Mathalon DH, Fedor M, Faustman WO et al (2002) Response-monitoring dysfunction in schizophrenia: an event-related brain potential study. J Abnorm Psychol 111(1):22–41
Mathews CA, Perez VB, Delucchi KL et al (2012) Error-related negativity in individuals with obsessive-compulsive symptoms: toward an understanding of hoarding behaviors. Biol Psychol 89(2):487–494
McCoy AN, Crowley JC, Haghighian G et al (2003) Saccade reward signals in posterior cingulate cortex. Neuron 40(5):1031–1040
McDonald C, Bullmore E, Sham P et al (2005) Regional volume deviations of brain structure in schizophrenia and psychotic bipolar disorder: computational morphometry study. Br J Psychiatry 186:369–377
Menon V, Adleman NE, White CD et al (2001) Error-related brain activation during a Go/NoGo response inhibition task. Hum Brain Mapp 12(3):131–143
Meyer A, Klein DN, Torpey DC et al (2012) Additive effects of the dopamine D2 receptor and dopamine transporter genes on the error-related negativity in young children. Genes Brain Behav 11(6):695–703
Meyer-Lindenberg A, Kohn PD, Kolachana B et al (2005) Midbrain dopamine and prefrontal function in humans: interaction and modulation by COMT genotype. Nat Neurosci 8(5):594–596
Mitelman SA, Shihabuddin L, Brickman AM et al (2005) Volume of the cingulate and outcome in schizophrenia. Schizophr Res 72(2–3):91–108
Morgan L, Wetherby AM, Barber A (2008) Repetitive and stereotyped movements in children with autism spectrum disorders late in the second year of life. J Child Psychol Psychiatry 49(8):826–837
Morris SE, Yee CM, Nuechterlein KH (2006) Electrophysiological analysis of error monitoring in schizophrenia. J Abnorm Psychol 115(2):239–250
Mossner R, Schuhmacher A, Kuhn KU et al (2009) Functional serotonin 1A receptor variant influences treatment response to atypical antipsychotics in schizophrenia. Pharmacogenet Genomics 19(1):91–94
Munafo MR, Bowes L, Clark TG et al (2005) Lack of association of the COMT (Val158/108 Met) gene and schizophrenia: a meta-analysis of case-control studies. Mol Psychiatry 10(8):765–770
Nieuwenhuis S, Ridderinkhof KR, Blom J et al (2001) Error-related brain potentials are differentially related to awareness of response errors: evidence from an antisaccade task. Psychophysiology 38(5):752–760
Nieuwenhuis S, Yeung N, van den Wildenberg W et al (2003) Electrophysiological correlates of anterior cingulate function in a go/no-go task: effects of response conflict and trial type frequency. Cogn Affect Behav Neurosci 3(1):17–26
Nieuwenhuis S, Nielen MM, Mol N et al (2005) Performance monitoring in obsessive-compulsive disorder. Psychiatry Res 134(2):111–122
Noriuchi M, Kikuchi Y, Yoshiura T et al (2010) Altered white matter fractional anisotropy and social impairment in children with autism spectrum disorder. Brain Res 1362:141–149
Ohnuma T, Kimura M, Takahashi T et al (1997) A magnetic resonance imaging study in first-episode disorganized-type patients with schizophrenia. Psychiatry Clin Neurosci 51(1):9–15
Okamura N, Reinscheid RK (2007) Neuropeptide S: a novel modulator of stress and arousal. Stress 10(3):221–226
Okochi T, Ikeda M, Kishi T et al (2009) Meta-analysis of association between genetic variants in COMT and schizophrenia: an update. Schizophr Res 110(1–3):140–148
Okuyama Y, Ishiguro H, Toru M et al (1999) A genetic polymorphism in the promoter region of DRD4 associated with expression and schizophrenia. Biochem Biophys Res Commun 258(2):292–295
Olvet DM, Hajcak G (2008) The error-related negativity (ERN) and psychopathology: toward an endophenotype. Clin Psychol Rev 28(8):1343–1354
Olvet DM, Hatchwell E, Hajcak G (2010) Lack of association between the 5-HTTLPR and the error-related negativity (ERN). Biol Psychol 85(3):504–508
Osinsky R, Hewig J, Alexander N et al (2012) COMT Val158Met genotype and the common basis of error and conflict monitoring. Brain Res 1452:108–118
Overbeek TJM, Nieuwenhuis S, Ridderinkhof KR (2005) Dissociable components of error processing. J Psychophysiology 19(4):319–329
Parsons MJ, Mata I, Beperet M et al (2007) A dopamine D2 receptor gene-related polymorphism is associated with schizophrenia in a Spanish population isolate. Psychiatr Genet 17(3):159–163
Paus T, Petrides M, Evans AC et al (1993) Role of the human anterior cingulate cortex in the control of oculomotor, manual, and speech responses: a positron emission tomography study. J Neurophysiol 70(2):453–469
Perez VB, Ford JM, Roach BJ et al (2012) Error monitoring dysfunction across the illness course of schizophrenia. J Abnorm Psychol 121(2):372–387
Pezawas L, Meyer-Lindenberg A, Drabant EM et al (2005) 5-HTTLPR polymorphism impacts human cingulate-amygdala interactions: a genetic susceptibility mechanism for depression. Nat Neurosci 8(6):828–834
Phillips ML, Drevets WC, Rauch SL et al (2003) Neurobiology of emotion perception I: the neural basis of normal emotion perception. Biol Psychiatry 54(5):504–514
Pitman RK (1987) A cybernetic model of obsessive-compulsive psychopathology. Compr Psychiatry 28(4):334–343
Pohjalainen T, Rinne JO, Nagren K et al (1998) The A1 allele of the human D2 dopamine receptor gene predicts low D2 receptor availability in healthy volunteers. Mol Psychiatry 3(3):256–260
Polli FE, Barton JJ, Cain MS et al (2005) Rostral and dorsal anterior cingulate cortex make dissociable contributions during antisaccade error commission. Proc Natl Acad Sci U S A 102(43):15700–15705
Polli FE, Barton JJ, Vangel M et al (2006) Schizophrenia patients show intact immediate error-related performance adjustments on an antisaccade task. Schizophr Res 82(2–3):191–201
Polli FE, Barton JJ, Thakkar KN et al (2008) Reduced error-related activation in two anterior cingulate circuits is related to impaired performance in schizophrenia. Brain 131(4):971–986
Polli FE, Wright CI, Milad MR et al (2009) Hemispheric differences in amygdala contributions to response monitoring. NeuroReport 20(4):398–402
Purcell SM, Wray NR, Stone JL et al (2009) Common polygenic variation contributes to risk of schizophrenia and bipolar disorder. Nature 460(7256):748–752
Rabbitt PM (1966) Errors and error correction in choice-response tasks. J Exp Psychol 71(2):264–272
Radant AD, Dobie DJ, Calkins ME et al (2010) Antisaccade performance in schizophrenia patients, their first-degree biological relatives, and community comparison subjects: data from the COGS study. Psychophysiology 47(5):846–856
Raichle ME, MacLeod AM, Snyder AZ et al (2001) A default mode of brain function. Proc Natl Acad Sci U S A 98(2):676–682
Reinscheid RK, Xu YL, Okamura N et al (2005) Pharmacological characterization of human and murine neuropeptide s receptor variants. J Pharmacol Exp Ther 3:1338–1345
Reynolds GP, Arranz B, Templeman LA et al (2006) Effect of 5-HT1A receptor gene polymorphism on negative and depressive symptom response to antipsychotic treatment of drug-naive psychotic patients. Am J Psychiatry 163(10):1826–1829
Ridderinkhof KR, Nieuwenhuis S, Bashore TR (2003) Errors are foreshadowed in brain potentials associated with action monitoring in cingulate cortex in humans. Neurosci Lett 348(1):1–4
Ridderinkhof KR, Ullsperger M, Crone EA et al (2004) The role of the medial frontal cortex in cognitive control. Science 306(5695):443–447
Ritchie T, Noble EP (2003) Association of seven polymorphisms of the D2 dopamine receptor gene with brain receptor-binding characteristics. Neurochem Res 28(1):73–82
Roffman JL, Gollub RL, Calhoun VD et al (2008a) MTHFR 677C⇒T genotype disrupts prefrontal function in schizophrenia through an interaction with COMT 158Val⇒Met. Proc Natl Acad Sci U S A 105(45):17573–17578
Roffman JL, Weiss AP, Deckersbach T et al (2008b) Interactive effects of COMT Val108/158Met and MTHFR C677T on executive function in schizophrenia. Am J Med Genet B Neuropsychiatr Genet 5;147B(6):990–995
Roffman JL, Weiss AP, Purcell S et al (2008c) Contribution of methylenetetrahydrofolate reductase (MTHFR) polymorphisms to negative symptoms in schizophrenia. Biol Psychiatry 63(1):42–48
Roffman JL, Brohawn DG, Friedman JS et al (2011a) MTHFR 677C>T effects on anterior cingulate structure and function during response monitoring in schizophrenia: a preliminary study. Brain Imaging Behav 5(1):65–75
Roffman JL, Nitenson AZ, Agam Y et al (2011b) A hypomethylating variant of MTHFR, 677C>T, blunts the neural response to errors in patients with schizophrenia and healthy individuals. PLoS ONE 6(9):e25253
Ruchsow M, Spitzer M, Gron G et al (2005) Error processing and impulsiveness in normals: evidence from event-related potentials. Brain Res Cogn Brain Res 24(2):317–325
Russell J, Jarrold C (1998) Error-correction problems in autism: evidence for a monitoring impairment? J Autism Dev Disord 28(3):177–188
Sandrone S (2012) The brain as a crystal ball: the predictive potential of default mode network. Front Hum Neurosci 6:261
Santesso DL, Segalowitz SJ, Schmidt LA (2006) Error-related electrocortical responses are enhanced in children with obsessive-compulsive behaviors. Dev Neuropsychol 29(3):431–445
Santesso DL, Drmic IE, Jetha MK et al (2011) An event-related source localization study of response monitoring and social impairments in autism spectrum disorder. Psychophysiology:241–251
Scheffers MK, Coles MG (2000) Performance monitoring in a confusing world: error-related brain activity, judgments of response accuracy, and types of errors. J Exp Psychol Hum Percept Perform 26(1):141–151
Schmahmann JD, Pandya DN, Wang R et al (2007) Association fibre pathways of the brain: parallel observations from diffusion spectrum imaging and autoradiography. Brain 130(3):630–653
Schultz W (2002) Getting formal with dopamine and reward. Neuron 36(2):241–263
Schultz W, Dayan P, Montague PR (1997) A neural substrate of prediction and reward. Science 275:1593–1598
Shi J, Gershon ES, Liu C (2008) Genetic associations with schizophrenia: meta-analyses of 12 candidate genes. Schizophr Res 104(1–3):96–107
Sigmundsson T, Suckling J, Maier M et al (2001) Structural abnormalities in frontal, temporal, and limbic regions and interconnecting white matter tracts in schizophrenic patients with prominent negative symptoms. Am J Psychiatry 158(2):234–243
Simmonite M, Bates AT, Groom MJ et al (2012) Error processing-associated event-related potentials in schizophrenia and unaffected siblings. Int J Psychophysiol 84(1):74–79
Simon JR (1969) Reactions towards the source of stimulation. J Experimental Psychol 81:174–176
Smith BW, Mitchell DG, Hardin MG et al (2009) Neural substrates of reward magnitude, probability, and risk during a wheel of fortune decision-making task. Neuroimage 44(2):600–609
Sokhadze E, Baruth J, El-Baz A et al (2010) Impaired error monitoring and correction function in autism. J Neurother 14(2):79–95
Sokhadze EM, Baruth JM, Sears L et al (2012a) Prefrontal neuromodulation using rTMS improves error monitoring and correction function in autism. Appl Psychophysiol Biofeedback 37(2):91–102
Sokhadze EM, Baruth JM, Sears L et al (2012b) Event-related potential study of attention regulation during illusory figure categorization task in Adhd, autism spectrum disorder, and typical children. J Neurother 16(1):12–31
South M, Larson MJ, Krauskopf E et al (2010) Error processing in high-functioning autism spectrum disorders. Biol Psychol 85(2):242–251
Stroop JR (1935) Studies of interference in serial verbal reaction. J Exp Psychol 18:643–662
Summerfelt AT, Alphs LD, Wagman AM et al (1991) Reduction of perseverative errors in patients with schizophrenia using monetary feedback. J Abnorm Psychol 100(4):613–616
Sun Z, Wang F, Cui L et al (2003) Abnormal anterior cingulum in patients with schizophrenia: a diffusion tensor imaging study. NeuroReport 14(14):1833–1836
Suzuki M, Nohara S, Hagino H et al (2002) Regional changes in brain gray and white matter in patients with schizophrenia demonstrated with voxel-based analysis of MRI. Schizophr Res 55(1–2):41–54
Taj MJR, Viswanath B, Purushottam M et al (2013) DRD4 gene and obsessive compulsive disorder: do symptom dimensions have specific genetic correlates? Prog Neuropsychopharmacol Biol Psychiatry 41:18–23
Tan HY, Callicott JH, Weinberger DR (2008) Intermediate phenotypes in schizophrenia genetics redux: is it a no brainer? Mol Psychiatry 13(3):233–238
Taylor SF, Martis B, Fitzgerald KD et al (2006) Medial frontal cortex activity and loss-related responses to errors. J Neurosci 26(15):4063–4070
Taylor SF, Stern ER, Gehring WJ (2007) Neural systems for error monitoring: recent findings and theoretical perspectives. Neuroscientist 13(2):160–172
Thakkar KN, Polli FE, Joseph RM et al (2008) Response monitoring, repetitive behaviour and anterior cingulate abnormalities in autism spectrum disorders (ASD). Brain 131(Pt 9):2464–2478
Thorndike E (1911) Animal intelligence. Macmillan, New York
Tu P, Buckner RL, Zollei L et al (2010) Reduced functional connectivity in a right-hemisphere network for volitional ocular motor control in schizophrenia. Brain 133(2):625–637
Turetsky BI, Greenwood TA, Olincy A et al (2008) Abnormal auditory N100 amplitude: a heritable endophenotype in first-degree relatives of schizophrenia probands. Biol Psychiatry 64(12):1051–1059
Turken AU, Vuilleumier P, Mathalon DH et al (2003) Are impairments of action monitoring and executive control true dissociative dysfunctions in patients with schizophrenia? Am J Psychiatry 160(10):1881–1883
Ursu S, Stenger VA, Shear MK et al (2003) Overactive action monitoring in obsessive-compulsive disorder: evidence from functional magnetic resonance imaging. Psychol Sci 14(4):347–353
van Boxtel GJM, van der Molen MW, Jennings JR (2005) Differential involvement of the anterior cingulate cortex in performance monitoring during a stop-signal task. J Psychophysiol 19(1):1–10
van de Giessen E, de Win MM, Tanck MW et al (2009) Striatal dopamine transporter availability associated with polymorphisms in the dopamine transporter gene SLC6A3. J Nucl Med 50(1):45–52
van Dyck CH, Malison RT, Jacobsen LK et al (2005) Increased dopamine transporter availability associated with the 9-repeat allele of the SLC6A3 gene. J Nucl Med 46(5):745–751
van Hoesen GW, Morecraft RJ, Vogt BA (1993) Connections of the monkey cingulate cortex. In: Vogt BA, Gabriel M (eds) Neurobiology of cingulate cortex and limbic thalamus: a comprehensive handbook. Birkhauser, Boston, pp 249–284
van Schie HT, Mars RB, Coles MG et al (2004) Modulation of activity in medial frontal and motor cortices during error observation. Nat Neurosci 7(5):549–554
Van Tol HH, Wu CM, Guan HC et al (1992) Multiple dopamine D4 receptor variants in the human population. Nature 358(6382):149–152
van Veen V, Carter CS (2002) The timing of action-monitoring processes in the anterior cingulate cortex. J Cogn Neurosci 14(4):593–602
Van’t Ent D, Apkarian P (1999) Motoric response inhibition in finger movement and saccadic eye movement: a comparative study. Clin Neurophysiol 110(6):1058–1072
Vandenbergh DJ, Persico AM, Hawkins AL et al (1992) Human dopamine transporter gene (DAT1) maps to chromosome 5p15.3 and displays a VNTR. Genomics 14(4):1104–1106
Vlamings PH, Jonkman LM, Hoeksma MR et al (2008) Reduced error monitoring in children with autism spectrum disorder: an ERP study. Eur J Neurosci 28(2):399–406
Waltz JA, Gold JM (2007) Probabilistic reversal learning impairments in schizophrenia: further evidence of orbitofrontal dysfunction. Schizophr Res 93(1–3):296–303
Waltz JA, Frank MJ, Robinson BM et al (2007) Selective reinforcement learning deficits in schizophrenia support predictions from computational models of striatal-cortical dysfunction. Biol Psychiatry 62(7):756–764
Waltz JA, Schweitzer JB, Ross TJ et al (2010) Abnormal responses to monetary outcomes in cortex, but not in the Basal Ganglia, in schizophrenia. Neuropsychopharmacology
Wang F, Sun Z, Cui L et al (2004) Anterior cingulum abnormalities in male patients with schizophrenia determined through diffusion tensor imaging. Am J Psychiatry 161(3):573–575
Watt N, Wetherby AM, Barber A et al (2008) Repetitive and stereotyped behaviors in children with autism spectrum disorders in the second year of life. J Autism Dev Disord 38(8):1518–1533
Whalen PJ, Bush G, McNally RJ et al (1998) The emotional counting Stroop paradigm: a functional magnetic resonance imaging probe of the anterior cingulate affective division. Biol Psychiatry 44(12):1219–1228
Whalley HC, Simonotto E, Moorhead W et al (2006) Functional imaging as a predictor of schizophrenia. Biol Psychiatry 60(5):454–462
Whitfield-Gabrieli S, Ford JM (2012) Default mode network activity and connectivity in psychopathology. Annu Rev Clin Psychol 8:49–76
Willemssen R, Muller T, Schwarz M et al (2009) Response monitoring in de novo patients with Parkinson’s disease. PLoS One 4(3):e4898
Wittfoth M, Kustermann E, Fahle M et al (2008) The influence of response conflict on error processing: evidence from event-related fMRI. Brain Res 1194:118–129
Xiao Z, Wang J, Zhang M et al (2011) Error-related negativity abnormalities in generalized anxiety disorder and obsessive-compulsive disorder. Prog Neuropsychopharmacol Biol Psychiatry 35(1):265–272
Xing QH, Wu SN, Lin ZG et al (2003) Association analysis of polymorphisms in the upstream region of the human dopamine D4 receptor gene in schizophrenia. Schizophr Res 65(1):9–14
Yamasue H, Iwanami A, Hirayasu Y et al (2004) Localized volume reduction in prefrontal, temporolimbic, and paralimbic regions in schizophrenia: an MRI parcellation study. Psychiatry Res 131(3):195–207
Yan H, Tian L, Yan J et al (2012) Functional and anatomical connectivity abnormalities in cognitive division of anterior cingulate cortex in schizophrenia. PLoS One 7(9):e45659
Zald DH (2003) The human amygdala and the emotional evaluation of sensory stimuli. Brain Res Brain Res Rev 41(1):88–123
Zirnheld PJ, Carroll CA, Kieffaber PD et al (2004) Haloperidol impairs learning and error-related negativity in humans. J Cogn Neurosci 16(6):1098–1112
Acknowledgements
The chapter authors are grateful to Jordan Smoller and Daniel Z. Press for consultation.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer Science+Business Media LLC
About this chapter
Cite this chapter
Manoach, D.S., Agam, Y. (2016). Neural Markers of Errors as Endophenotypes in Neuropsychiatric Disorders. In: Jagaroo, V., Santangelo, S. (eds) Neurophenotypes. Innovations in Cognitive Neuroscience. Springer, Boston, MA. https://doi.org/10.1007/978-1-4614-3846-5_9
Download citation
DOI: https://doi.org/10.1007/978-1-4614-3846-5_9
Published:
Publisher Name: Springer, Boston, MA
Print ISBN: 978-1-4614-3845-8
Online ISBN: 978-1-4614-3846-5
eBook Packages: Behavioral Science and PsychologyBehavioral Science and Psychology (R0)