Abstract
Myasthenia gravis is an autoimmune disorder with a highly variable clinical expression, course and prognosis. Although only moderate quality evidence is available, thymectomy is generally indicated in patients with early onset myasthenia gravis and positive acetylcholine receptor antibodies or in case of associated thymoma. Several surgical approaches to the thymus exist, the specific technique depending on the experience of the thoracic surgeon performing the procedure, also taking the preference of the patient into consideration. A multidisciplinary approach is advocated to ensure a high-quality level of preoperative, intraoperative and postoperative care. Due to the lack of large comparative or randomized trials no specific recommendations can be made regarding the best available approach to the thymus. Sternotomy remains the gold standard against which all other approaches should be evaluated and compared including thoracoscopic and robotic procedures. Despite the fact that available evidence is low, it seems that the less thymic tissue that has been left behind, the better the long-term results that are achieved.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
The thymus is associated with highly variable disease entities often related to autoimmune disorders. Pathologically, thymic hyperplasia, cysts and different kinds of tumors may occur. Their clinical behavior ranges from benign to aggressive with symptoms due to invasion of neighboring mediastinal structures or pericardial and pleural cavities.
In this chapter patients with myasthenia gravis are considered whether or not associated with a thymoma (patient population). Surgical treatment consists of thymectomy (intervention) which remains a highly controversial procedure, not only regarding the specific indications but also concerning the best surgical approach in order to obtain a complete thymectomy.
In this evidence-based approach we focus on three questions: What are the current indications for thymectomy in myasthenia gravis? The neurologist gives his point of view regarding the operative indications based on recent literature data. Secondly, we discuss the different ways to reach the thymus trying to answer the question “Which is the best surgical approach to the thymus?” (comparison). Lastly, the specific procedure of thymectomy is highlighted with the discussion centered on the question “Is extended thymectomy better than standard thymectomy?” (comparison). Remission of myasthenic symptoms is considered the main outcome parameter.
Search Strategy
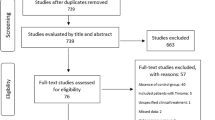
To retrieve relevant publications a PubMed search was performed with key words “myasthenia gravis” and “thymectomy”, current guidelines and major thoracic surgical text books were reviewed and references of included publications were screened for additional evidence.
Current Indications for Thymectomy in Myasthenia Gravis
Myasthenia gravis is an autoimmune disorder directed against the postsynaptic part of the neuromuscular junction. A wide variation in clinical severity is found ranging from occasional ptosis or diplopia with spontaneous remission to severe generalized weakness requiring temporary artificial ventilation. In some patients the symptoms remain limited to the extraocular muscles: these patients have ocular myasthenia in contrast to generalized myasthenia gravis. Most patients have antibodies against the acetylcholine receptor (AchR) itself, while a minority have antibodies against the receptor-like muscle-specific kinase (MUSK), low-density lipoprotein receptor-related protein 4 (LRP4) or no detectable antibodies with the currently available assays [1, 2].
AchR antibody positive myasthenia gravis is subdivided in early and late onset according to the initial diagnosis before or after age 50. While there is a predominance of women in the early onset group there is an increasing incidence of late onset patients with a predominance of men. About 10 % of myasthenic patients of all ages with positive AchR antibodies have a thymoma. Thymoma patients and late onset non-thymoma patients frequently have antibodies against titin or the ryanodine receptor, while these antibodies are rare in early onset non-thymoma myasthenia gravis. In contrast, thymic follicular hyperplasia is frequent in early onset non-thymoma patients and rare in late onset patients. There is evidence that the thymus is involved in the pathogenesis of all types of AchR myasthenia, while its role is unclear in MUSK myasthenia and unknown in LRP4 and seronegative myasthenia [3].
It is generally accepted that surgery is required when a thymoma has been diagnosed. It is common practice to recommend thymectomy in early onset non-thymoma patients with generalized myasthenic symptoms. This recommendation is supported by the pathogenetic mechanism of myasthenia gravis, observational studies and non-randomized trials, although a definite controlled randomized clinical trial is still lacking.
In formulating a practice parameter for the American Academy of Neurology, Gronseth and Barohn reviewed the evidence available until 2000 [4]. They concluded that all currently published studies had serious methodological flaws that prevented definite conclusions regarding the benefit of thymectomy. These flaws included the absence of randomized allocation to thymectomy and non-thymectomy treatment, the absence of standardized, blinded outcome determinations and confounding differences in enrollment in the surgical and non-surgical groups. Because most studies showed a positive association between thymectomy and remission or improvement of myasthenic symptoms, they recommended thymectomy as an option to increase the probability of remission or improvement in non-thymomatous autoimmune myasthenia gravis. This recommendation was supported in the guidelines for the treatment of autoimmune neuromuscular transmission disorders by the European Federation of Neurological Societies in 2010 [5]. Patients with AchR antibodies and generalized disease were most likely to improve. Thymectomy was also recommended for seronegative patients but not for patients with MUSK antibodies.
The presence of conflicting data concerning the effect of thymectomy in ocular myasthenia was confirmed in a Cochrane Review in 2012 [6]. According to a survey of the Thymic Working Group of the European Association for Cardio-Thoracic Surgery (EACTS) most surgeons do not operate on myasthenic patients with exclusively ocular symptoms [7].
A recent retrospective study of 98 thymectomies in myasthenic patients over a 12-year period confirmed the generally accepted chance of one out of three of complete stable remission after the procedure with a variable degree of improvement in the other patients [8].
In 2006 a “Multicenter, single-blind, randomized study comparing thymectomy to no thymectomy in non-thymomatous myasthenia gravis patients receiving prednisone” was initiated under impulse of the late John Newson-Davis [9]. In this ClinicalTrials.gov NCT00294658 study patients were recruited with an age range from 18 till 65, with onset of AchR antibody positive myasthenia gravis over the last 5 years, excluding patients with only ocular symptoms. Treatment with prednisone alone is compared to the combination of prednisone and thymectomy. Extended transsternal thymectomy is the only accepted surgical procedure. The last patient was enrolled in 2012, the first results are expected in 2015. This trial will answer the question whether thymectomy and steroids are better than steroids alone. The issue whether thymectomy only is better than no treatment, and which is the best surgical approach will remain unanswered. Current indications for thymectomy in myasthenia gravis are listed in Table 52.1.
Optimal Surgical Approach to the Thymus
The thymus originates from the third and fourth pharyngeal pouches which move towards the midline and subsequently descend into the mediastinum. The thymus has a typical H-shape with two cervical poles which are less developed, and two mediastinal poles which are broadly extending along the pericardium inferiorly as far as the anterior cardiophrenic recesses. A highly variable anatomy has been described which has profound surgical implications when discussing thymectomy and the most appropriate surgical approach [10]. Precise anatomical and pathological studies have demonstrated that additional ectopic thymic tissue may be discovered in 32–98 % of patients when an extended resection has been performed [10, 11]. Non-encapsulated lobules of thymus and microscopic foci of thymus may be present in the pretracheal and anterior mediastinal fat from the level of the thyroid to the diaphragm and bilaterally from beyond each phrenic nerve. Microscopic foci of thymus have also been found in subcarinal fat and in the aortopulmonary window.
Many different approaches exist to perform a thymectomy and these can be subdivided into open procedures, minimally invasive and combined interventions (Table 52.2). The different steps of these procedures have been described in detail [12–14]. The specific indication discussed within a multidisciplinary setting, the experience of the thoracic surgeon and the patient’s preference will determine the ultimate choice. In case of myasthenia a “maximal” thymectomy is advised removing as much thymic tissue as possible with surrounding mediastinal fat from the cervical region to the diaphragm extending laterally to both phrenic nerves, and also incorporating the mediastinal fat in the aortopulmonary window. In this way ectopic thymic tissue will be removed to a maximal extent.
In case of combined myasthenia and suspected or proven thymoma it is important to completely remove the thymic lesion. When present, its capsule should not be breached in order to avoid spilling of malignant cells into the mediastinum or pleural cavities.
Unfortunately, no randomized trials exist that compare the different surgical approaches to determine mortality, frequency of postoperative complications and evaluate long-term results. So, no high-quality evidence is available.
No doubt, sternotomy remains the current gold standard allowing an extended thymectomy by an anterior approach with complete removal of the thymus and surrounding fatty tissue, allowing opening of both pleural cavities, control of major mediastinal blood vessels and extensive dissection along the pericardium into the cardiophrenic recesses [14]. On the other hand, it requires a large incision necessitating an extensive osteotomy which may result in increased pain, higher morbidity, slower recovery and prolonged hospitalization time. However, a direct comparison of sternotomy with alternative incisions for similar patient groups is not available. A partial upper sternotomy provides good visualization of the upper mediastinum but evaluation of more caudal regions is not feasible [12]. Large mediastinal tumors invading major mediastinal structures may be approached by a lateral thoracotomy or combined incisions. The latter include hemi-clam shell or clam shell approaches, consisting of partial sternotomy combined with an anterolateral thoracotomy or bilateral anterior thoracotomy with transverse sternotomy, respectively. Especially for patients with myasthenia gravis and generalized complaints including respiratory problems, less invasive methods were developed to decrease morbidity in relation to the incision but still allowing an extended thymectomy.
By a cervicotomy it is possible to remove the entire thymus and surrounding fatty tissue, especially when a sternal retractor is used [13]. With the advent of video-assisted thoracic surgery (VATS), new methods became available to perform a thymectomy by small thoracoports. Recently, robotic-assisted thoracic surgery (RATS) was introduced providing optimal three-dimensional visualization facilitating dissection with the aid of highly flexible robotic arms [15–17].
Within the surgical community there is an ongoing discussion whether a right-sided, left-sided or bilateral thoracoscopic approach is indicated to perform a complete thymectomy. In some centers combined procedures are used as VATS in combination with a cervicotomy or a subxiphoid approach, in this way avoiding a scar in the cervical region [18]. The thymus may thus be approached from different angles allowing complete removal.
Regarding the incision no definite recommendations can be made due to the lack of randomized trials. Median sternotomy remains the gold standard. So, the experience of a surgeon and a specific center but also the preference of the patient after all relevant information has been provided, will determine the final approach.
Another controversial topic remains the role of a minimally invasive approach in patients with myasthenia and suspicion of thymoma. Depending on the location and size of the thymoma recent data indicate that well-encapsulated tumors without invasion into the mediastinum or large vessels can safely be removed by a thoracoscopic or especially, a robotic technique [15, 17, 18]. Invasion in large mediastinal vessels is a contra-indication for a VATS or robotic approach. The size limit is usually considered to be 4–5 cm [19]. However, as thymomas are slowly growing tumors, long-term results are still awaited for before definite conclusions will be reached regarding long-term oncological outcome.
Extended Thymectomy vs Standard Thymectomy
The role of thymectomy in the treatment of myasthenia gravis has not been elucidated yet [20]. Until recently, variable patient selection, timing and type of surgery and analytical methods rendered the conclusions of the most important retrospective studies inconsistent. Moreover, there are no controlled prospective studies and the unique randomized trial comparing thymectomy versus non-thymectomy in patients treated by steroids is still ongoing as outlined earlier [9].
Before dealing with the extent of the thymectomy to be performed for myasthenia gravis, it is crucial to emphasize that the thymus is a functional entity not limited to the gland itself and thymic cells may be found outside the main capsule. As outlined before, surgical and anatomical studies already showed many years ago that the thymus frequently consists of multiple lobes in the neck and mediastinum, often separately encapsulated and not necessarily contiguous [21, 22]. This results in the recommendation that as much mediastinal thymic tissue as possible should be removed for the treatment of non-thymomatous myasthenia gravis. This statement is supported by a review of published papers on the results of thymectomy [4, 20, 22–25]. Further proof comes from the presence of residual thymic tissue in most of the re-operations after previous transcervical and standard transsternal thymectomy, with improvement or remission of the myasthenic symptoms [26].
The original standard transsternal thymectomy used by Blalock was limited to removal of the thymic gland with its cervical and mediastinal lobes [27]. Unrelated to the surgical approach, the resection is currently more extensive than originally described and includes, at least, removal of all visible mediastinal thymic lobes and also part of the mediastinal and low cervical fat [4, 23–25].
The extended transsternal thymectomy also called “aggressive transsternal thymectomy” and “transsternal radical thymectomy” consists of en-bloc resection of all fat and thymic tissue in the neck and mediastinum. Dissection starts at the inferior part of the thyroid lobes proceeding caudally to the diaphragm and extending laterally from one phrenic to the contralateral one. Removing cervical tissue by a VATS or robotic procedure starting from below without a neck incision, may result in an incomplete resection which is less radical than a transcervical and transsternal thymectomy [20, 22]. However, because it is less invasive with low morbidity, this approach has been adopted by many thoracic surgeons dealing with myasthenia gravis. Retrospective studies comparing extended thymic resections with standard thymectomy, also supported the premise that the more thymic tissue is removed, the higher the remission rate will be [20].
However, we must consider that inappropriate statistical analysis has led in the past to incorrect conclusions about the relative merits of the extension of thymectomy. Unfortunately, uncorrected crude rates have been used in the most important retrospective series and this form of analysis did not include all relevant follow-up information including the median length of follow-up [4]. As a matter of fact, uncorrected crude data should not be used anymore in the comparative analysis of results of thymectomy for myasthenia gravis. Life table analysis using the Kaplan–Meier method, is currently the statistical technique of choice for the analysis of remissions following thymectomy [20].
Several other biases, such as the selection of patients for thymectomy, the different clinical classifications of myasthenia gravis, the lack of quantitative scoring systems and the different schedules of medications used in the preoperative and postoperative course make the comparative analysis based on existing published information unreliable [20].
From 2000 on, based on recommendations of the task force of the Myasthenia Gravis Foundation of America (MGFA), precise definitions of remission and life table analyses have been adopted in some but not all studies reporting the outcome of thymectomy in myasthenic patients.
Because of the lack of well-designed, controlled, prospective studies that compare thymectomy versus non-thymectomy, standard versus extended versus maximal thymectomy and finally, different surgical approaches to the thymus, we can only select and extrapolate data from well-performed observational trials. Despite the fact that the available evidence is of low quality, it seems that the less thymic tissue has been left behind, the better the long-term results are achieved.
We agree with Jaretzki and Sonett statements that the transcervical-transsternal maximal thymectomy should remain the benchmark against which all other thymectomy techniques have to be evaluated and that in the absence of controlled prospective studies comparing the various thymectomy techniques, it is not possible to define a procedure of choice [20]. Alternatively, in the hands of experienced surgeons, an extended transsternal thymectomy removes most of the thymic variations in the neck with less risk of injury to the recurrent laryngeal nerves. Good results have been reported and according to a recent European Survey, it is probably the most commonly performed procedure [7].
All thoracic surgeons should be convinced of the importance of complete removal of the thymus and commit the necessary time and care to achieve this goal safely. However, because the need for complete removal of all gross and microscopic thymus has not been definitively confirmed, it may be preferable to leave behind small amounts of suspected thymus than to cause injury to the recurrent laryngeal, left vagal or phrenic nerves, which can be devastating in a patient with myasthenia gravis.
As already mentioned, clearance of the neck region is a controversial point for most of the minimally invasive techniques (thoracoscopic or robotic-assisted) and this point needs to be addressed by further studies. Up to now the minimally invasive techniques proved to be feasible and safe but we must wait for a longer follow-up time and especially, high-quality comparative studies [24, 25].
Resections less than a standard thymectomy have never been considered for the treatment of non-thymomatous myasthenia gravis. Also for patients with encapsulated thymoma, non-invasive or microinvasive lesions, corresponding to Masaoka stages I and II, complete excision including an extended thymectomy is currently considered to be the procedure of choice, even in non-myasthenic patients. Recently, Onuki et al. conducted a retrospective comparative study of 79 patients and tested the hypothesis that limited thymectomy is not inferior to total thymectomy for stage I or II thymomas in terms of surgical outcome and postoperative complications [28]. The authors concluded that there were no statistical differences in the incidence of postoperative myasthenia gravis and disease-free survival between the two groups, but this was a retrospective historical comparative study and the neurologic inclusion criteria and outcome did not meet any MGFA recommendations.
Based on the low to moderate scientific evidence derived by the literature, thoracic surgeons should perform an extended thymectomy by the least invasive operation possible (Table 52.3).
Recommendations
Thymectomy is indicated in patients with early onset, generalized myasthenia gravis and positive acetylcholine receptor antibodies or in case of associated thymoma (evidence quality moderate; weak recommendation). Sternotomy is the best approach to perform a maximal, extended thymectomy (evidence quality low; weak recommendation). In case of myasthenia gravis with positive acetylcholine receptor antibodies extended thymectomy yields better long-term results than standard thymectomy (evidence quality low; weak recommendation).
A Personal View of the Data
In patients with early onset, generalized myasthenia gravis and positive acetylcholine receptor antibodies we favor an extended thymectomy. In case of thymic hyperplasia a robotic approach is preferred as it is feasible to perform a complete thymectomy. As the bulk of thymic tissue is usually located on the left side in front of the pericardium, most cases are approached from this side. In case of myasthenia gravis associated with thymoma, sternotomy remains our standard approach. Exceptions include tumors <5 cm without invasion of major vessels or structures which are resected with the robot from the left or right side depending on their precise location. The ultimate aim is complete excision without breaching the capsule.
Recommendations
-
Extended thymectomy yields better long-term results than standard thymectomy for management of myasthenia gravis. (Evidence quality low; weak recommendation)
-
Sternotomy is the best approach for performing an extended thymectomy. (Evidence quality low; weak recommendation)
References
Meriggioli MN, Sanders DB. Autoimmune myasthenia gravis: emerging clinical and biological heterogeneity. Lancet Neurol. 2009;8(5):475–90. Epub 2009/04/21.
Cossins J, Belaya K, Zoltowska K, Koneczny I, Maxwell S, Jacobson L, et al. The search for new antigenic targets in myasthenia gravis. Ann N Y Acad Sci. 2012;1275:123–8. Epub 2013/01/03.
Marx A, Pfister F, Schalke B, Saruhan-Direskeneli G, Melms A, Strobel P. The different roles of the thymus in the pathogenesis of the various myasthenia gravis subtypes. Autoimmun Rev. 2013;12(9):875–84. Epub 2013/03/29.
Gronseth GS, Barohn RJ. Practice parameter: thymectomy for autoimmune myasthenia gravis (an evidence-based review): report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology. 2000;55(1):7–15. Epub 2000/07/13.
Skeie GO, Apostolski S, Evoli A, Gilhus NE, Illa I, Harms L, et al. Guidelines for treatment of autoimmune neuromuscular transmission disorders. Eur J Neurol. 2010;17(7):893–902. Epub 2010/04/21.
Benatar M, Kaminski H. Medical and surgical treatment for ocular myasthenia. Cochrane Database Syst Rev. 2012;12, CD005081. Epub 2012/12/14.
Lucchi M, Van Schil P, Schmid R, Rea F, Melfi F, Athanassiadi K, et al. Thymectomy for thymoma and myasthenia gravis. A survey of current surgical practice in thymic disease amongst EACTS members. Interact Cardiovasc Thorac Surg. 2012;14(6):765–70. Epub 2012/03/01.
Spillane J, Hayward M, Hirsch NP, Taylor C, Kullmann DM, Howard RS. Thymectomy: role in the treatment of myasthenia gravis. J Neurol. 2013;260(7):1798–801. Epub 2013/03/20.
Newsom-Davis J, Cutter G, Wolfe GI, Kaminski HJ, Jaretzki 3rd A, Minisman G, et al. Status of the thymectomy trial for nonthymomatous myasthenia gravis patients receiving prednisone. Ann N Y Acad Sci. 2008;1132:344–7. Epub 2008/06/24.
Shields T. The thymus. In: Shields T, editor. Mediastinal surgery. Philadelphia: Lea & Febiger; 1991. p. 6–13.
Sonett J. Thymectomy for myasthenia gravis: optimal approach. In: F MK, editor. Difficult decisions in thoracic surgery an evidence-based approach. London: Springer; 2007. p. 469–73.
Trastek VP PC. Standard thymectomy. In: Shields T, editor. Mediastinal surgery. Philadelphia: Lea & Febiger; 1991. p. 365–8.
Kirby TG RJ, et al. Transcervical thymectomy. In: Shields T, editor. Mediastinal surgery. Philadelphia: Lea & Febiger; 1991. p. 369–71.
Jaretzki III A. Transcervical / trans-sternal “maximal” thymectomy for myasthenia gravis. Mediastinal surgery. Philadelphia: Lea & Febiger; 1991. p. 372–6.
Mussi A, Fanucchi O, Davini F, Lucchi M, Picchi A, Ambrogi MC, et al. Robotic extended thymectomy for early-stage thymomas. Eur J Cardiothorac Surg. 2012;41(4):e43–6; discussion e7. Epub 2012/03/01.
Ruckert JC, Sobel HK, Gohring S, Einhaupl KM, Muller JM. Matched-pair comparison of three different approaches for thymectomy in myasthenia gravis. Surg Endosc. 2003;17(5):711–5. Epub 2003/03/05.
Ruckert JC, Swierzy M, Ismail M. Comparison of robotic and nonrobotic thoracoscopic thymectomy: a cohort study. J Thorac Cardiovasc Surg. 2011;141(3):673–7. Epub 2011/02/22.
Zielinski M, Czajkowski W, Gwozdz P, Nabialek T, Szlubowski A, Pankowski J. Resection of thymomas with use of the new minimally-invasive technique of extended thymectomy performed through the subxiphoid-right video-thoracoscopic approach with double elevation of the sternum. Eur J Cardiothorac Surg. 2013;44(2):e113–9. Epub 2013/06/14.
Kimura T, Inoue M, Kadota Y, Shiono H, Shintani Y, Nakagiri T, et al. The oncological feasibility and limitations of video-assisted thoracoscopic thymectomy for early-stage thymomas. Eur J Cardiothorac Surg. 2013;44(3):e214–8. Epub 2013/06/14.
Sonett JR, Jaretzki 3rd A. Thymectomy for nonthymomatous myasthenia gravis: a critical analysis. Ann N Y Acad Sci. 2008;1132:315–28. Epub 2008/06/24.
Masaoka A, Nagaoka Y, Kotake Y. Distribution of thymic tissue at the anterior mediastinum. Current procedures in thymectomy. J Thorac Cardiovasc Surg. 1975;70(4):747–54. Epub 1975/10/01.
Jaretzki 3rd A, Wolff M. “Maximal” thymectomy for myasthenia gravis. Surgical anatomy and operative technique. J Thorac Cardiovasc Surg. 1988;96(5):711–6. Epub 1988/11/01.
Zielinski M, Kuzdzal J, Szlubowski A, Soja J. Comparison of late results of basic transsternal and extended transsternal thymectomies in the treatment of myasthenia gravis. Ann Thorac Surg. 2004;78(1):253–8. Epub 2004/06/30.
Meyer DM, Herbert MA, Sobhani NC, Tavakolian P, Duncan A, Bruns M, et al. Comparative clinical outcomes of thymectomy for myasthenia gravis performed by extended transsternal and minimally invasive approaches. Ann Thorac Surg. 2009;87(2):385–90; discussion 90-1. Epub 2009/01/24.
Mantegazza R, Baggi F, Bernasconi P, Antozzi C, Confalonieri P, Novellino L, et al. Video-assisted thoracoscopic extended thymectomy and extended transsternal thymectomy (T-3b) in non-thymomatous myasthenia gravis patients: remission after 6 years of follow-up. J Neurol Sci. 2003;212(1–2):31–6. Epub 2003/06/18.
Rosenberg M, Jauregui WO, De Vega ME, Herrera MR, Roncoroni AJ. Recurrence of thymic hyperplasia after thymectomy in myasthenia gravis. Its importance as a cause of failure of surgical treatment. Am J Med. 1983;74(1):78–82. Epub 1983/01/01.
Blalock A, Mason MF, Morgan HJ, Riven SS. Myasthenia gravis and tumors of the thymic region: report of a case in which the tumor was removed. Ann Surg. 1939;110(4):544–61. Epub 1939/10/01.
Onuki T, Ishikawa S, Iguchi K, Goto Y, Sakai M, Inagaki M, et al. Limited thymectomy for stage I or II thymomas. Lung Cancer. 2010;68(3):460–5. Epub 2009/09/01.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer-Verlag London
About this chapter
Cite this chapter
Van Schil, P.E., Mercelis, R., Lucchi, M. (2014). Extended Versus Standard Thymectomy for Myasthenia Gravis. In: Ferguson, M. (eds) Difficult Decisions in Thoracic Surgery. Difficult Decisions in Surgery: An Evidence-Based Approach, vol 1. Springer, London. https://doi.org/10.1007/978-1-4471-6404-3_52
Download citation
DOI: https://doi.org/10.1007/978-1-4471-6404-3_52
Published:
Publisher Name: Springer, London
Print ISBN: 978-1-4471-6403-6
Online ISBN: 978-1-4471-6404-3
eBook Packages: MedicineMedicine (R0)