Abstract
The most important adverse effect of antithrombotic treatment is the occurrence of bleeding. Studies of patients receiving anticoagulant therapy indicate that the incidence of major bleeding is 0.5 %/year and intracranial bleeding 0.2 %/year, however, it is likely that in real life practice the incidence is even higher. In particular, combined anticoagulant and antiplatelet agents may markedly increase the risk of major hemorrhagic complications. The most important risk factors for bleeding in patients receiving anticoagulants are the intensity of the anticoagulation and some patient characteristics, including age and co-morbidities. In case of serious or even life-threatening bleeding in a patient who uses anticoagulant agents or when a patient on anticoagulants needs to undergo an urgent invasive procedure, anticoagulant treatment can be reversed by various specific strategies. Heparin and heparin derivatives can be counteracted by protamine sulphate, whereas the anticoagulant effect of vitamin K antagonists may be neutralized with the administration of vitamin K or prothrombin complex concentrates. The anti-hemostatic effect of aspirin and other anti-platelet agents can be corrected by the administration of platelet concentrate and/or desmopressin, if needed. For the new generation oral anticoagulants including specific inhibitors of factor IIa, or factor Xa reversing strategies are currently being evaluated. The effect of factor Xa inhibitors can probably be reversed by prothrombin complex concentrates or recombinant factor VIIa, whereas for anti-IIa agents no specific reversing agent has been identified so far.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Major Bleeding
- Disseminate Intravascular Coagulation
- Anticoagulant Effect
- Prothrombin Complex Concentrate
- Direct Thrombin Inhibitor
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Introduction
Anticoagulant agents are often used for prevention and treatment of a wide range of cardiovascular diseases, including acute coronary syndromes. The most frequently used anticoagulants are heparin or its derivatives, vitamin K antagonists (such as warfarin or coumadin) and antiplatelet agents, including aspirin and thienopyridine derivatives, such as clopidogrel or prasugrel. A myriad of clinical studies have demonstrated that these agents (alone or in combination) can prevent or treat acute or chronic thrombo-embolic complications, such as in patients with atrial fibrillation or prosthetic heart valves, after myocardial infarction, percutaneous coronary interventions, or ischemic stroke, and in patients with venous thrombosis or pulmonary embolism [1]. The most important complication of treatment with anticoagulants is hemorrhage, which may be serious, may cause long-term debilitating disease, or may even be life-threatening [2, 3]. In a very large series of 34,146 patients with acute ischemic coronary syndromes, anticoagulant-associated bleeding was associated with a 5-fold increased risk of death during the first 30 days and a 1.5-fold higher mortality between 30 days and 6 months [4]. Major bleeding was an independent predictor of mortality across all subgroups that were analyzed. In some clinical situations the incidence of serious bleeding complications may annihilate or even overwhelm the efficacy of antithrombotic agents, as has been shown in the secondary prevention of patients with ischemic stroke by vitamin K antagonists [5]. Nevertheless, in many situations clinical studies show a favorable balance between efficacy and safety in favor of anticoagulant treatment. However, if severe bleeding occurs or if a patient needs to undergo an urgent invasive procedure, such as emergency surgery, it may be necessary to reverse the anticoagulant effect of the various agents [6]. Depending on the clinical situation, i.e. the severity of the bleeding or the urgency and estimated risk of the invasive procedure, this reversal may take place in a few hours, but in some cases immediate reversal is necessary (Table 7.1) [7, 8]. Generally, each (immediate) reversal of anticoagulant treatment needs also to take into consideration the indication for the antithrombotic agents. For example, the interruption of combined aspirin and clopidogrel treatment in a patient in whom recently an intracoronary stent has been inserted will markedly increase the risk of acute stent thrombosis with consequent downstream cardiac ischemia or infarction. Likewise, in a patient with a prosthetic mitral valve and atrial fibrillation, interruption of vitamin K antagonists may increase the risk of valve thrombosis and cerebral or systemic embolism. Each of these specific clinical situations requires a careful and balanced assessment of the benefits and risks of reversing anticoagulants (and potential strategies to keep the period of reversal as short as possible). In this chapter, we will describe the various strategies to reverse the anticoagulant effect of currently most widely used antithrombotic agents and the new generation of anticoagulants.
Incidence and Risk Factors for Bleeding in Patients on Anticoagulants
In well-controlled patients in clinical trials treatment with heparin or vitamin K antagonists (VKA’s) increase the risk of major bleeding by 0.5 %/year and the risk of intracranial hemorrhage by about 0.2 %/year [9]. The most important risk factor for hemorrhage in users of anticoagulants is the intensity of the anticoagulant effect [9]. Studies indicate that with a target INR of >3.0 the incidence of major bleeding is twice as large as in studies with a target INR of 2.0–3.0 [10]. In a meta-analysis of studies in patients with prosthetic heart valves, a lower INR target range resulted in a lower frequency of major bleeding and intracranial hemorrhage with a similar antithrombotic efficacy [11]. A retrospective analysis of outpatients using warfarin who presented with intracranial hemorrhage demonstrated that the risk of this complication doubled for each 1 unit increment of the INR [12]. Patient characteristics constitute another important determinant of the bleeding risk bleeding. Elderly patients have a 2-fold increased risk of bleeding [13] and the relative risk of intracranial hemorage (in particular at higher intensities of anticoagulation) was 2.5 (95 % CI 2.3–9.4) in patients >85 years compared to patients 70–74 year old [14]. Recently, genetic factors have been identified that may affect the risk of bleeding. Common polymorphisms in the P450 CYP2C9 enzyme were found to be associated with slow metabolism of VKA’s and (possibly) a higher risk of bleeding [9, 15]. Other genetic factors that may influence the requirement of VKA’s are variants in the vitamin K epoxide reductase complex subunit 1 gene (VKORC1) [16]. Co-morbidity, such as renal or hepatic insufficiency, may also significantly increase the risk of bleeding. A case-control study in 1,986 patients on VKA’s showed that this comorbidity increased the risk of bleeding by about 2.5 [17]. Another very important determinant of the risk of bleeding is the use of other medication, in particular agents affecting platelet function. Two meta-analyses, comprising 6 trials with a total of 3,874 patients and 10 trials with a total of 5,938 patients, found a relative risk of major bleeding when VKA’s or heparin were combined with aspirin of 2.4 (95 % CI 1.2–4.8) and 2.5 (95 % CI 1.7–3.7), respectively [18, 19]. A population-based case-control study confirmed the high risk of upper gastro-intestinal bleeding in patients using VKA’s in combination with aspirin and/or clopidogrel [20]. Non-steroidal anti-inflammatory agents (NSAIDs) are also associated with an enhanced risk of gastro-intestinal bleeding. The combined use of VKA’s and NSAIDs may result in an 11-fold higher risk of hospitalization for gastro-intestinal bleeding as compared to the general population [21]. This risk is not significantly lower when using selective inhibitors of COX-2 [22].
Heparin and Low Molecular Weight (LMW) Heparin
Heparin and heparin derivatives act by binding to antithrombin and thereby about 1,000-fold potentiating the anticoagulant effect of this endogenous inhibitor towards thrombin and factor Xa (and some other coagulation factors). Heparin has a relatively short half life of about 60–90 min and therefore the anticoagulant effect of therapeutic doses of heparin will be mostly eliminated at 3–4 h after termination of continuous intravenous administration [23]. The anticoagulant effect of high dose subcutaneous heparin, however, will take a longer time to abolish. If a more immediate neutralization of heparin is required, intravenous protamine sulphate is the antidote of choice. Protamine, derived from fish sperm, binds to heparin to from a stable biologically inactive complex. Each mg of protamine will neutralize approximately 100 units of heparin. Hence, the protamine dose in a patient on a stable therapeutic heparin dose of 1,000–1,250 U/h should be about 25–30 mg (sufficient to block the amount of heparin given in the last 2–3 h). The maximum dose of protamine is 50 mg. Since the half-life of protamine is only about 10 min, the reversal of therapeutic dose subcutaneous heparin requires a repeated infusion of protamine sulphate (e.g. repeated after 1 h). The effect of protamine can be monitored by measuring the activated partial thromboplastin time (aPTT), which should normalize after its administration.
The reversal of LMW heparin is more complex, as protamine sulphate will only neutralize the anti-factor IIa activity and has no or only partial effect on the smaller heparin fragments causing the anti-factor Xa activity of the compound [24, 25]. The net effect of protamine reversal of LMW heparin is not completely clear. There are no clinical studies that have systematically studied this and small case series and experimental animal studies show contradictory results [25–27]. As the aPTT is not useful as a monitoring assay when using LMW heparin, it can also not be used for the monitoring of the neutralizing effect of protamine. Given the relatively long half-life of LMW heparin, the lack of an adequate strategy to reverse its anticoagulant action may sometimes cause a problem in clinical situations. A practical approach is to give 1 mg of protamine per 100 anti-factor Xa units of LMW heparin given in the last 8 h (whereas 1 mg of enoxaparin equals 100 anti-factor Xa units). If bleeding continues, a second dose of 0.5 mg per 100 anti-factor Xa units can be given.
The most important adverse effect of protamine is an allergic response, including hemodynamic and respiratory problems [28]. Most adverse reactions can be prevented or minimized by slowing the rate of administration of the drug or by pretreatment with steroids and antihistamines. Risk factors for an adverse reaction are sensitivity to fish (as may occur in traditional fishermen that are often exposed to fish proteins when cutting themselves), a history of vasectomy (which may demolish the blood-testis barrier with consequent formation of anti-semen antibodies) and a history of receiving protamine sulphate containing insulin. Initial reports that the use of protamine sulphate could lead to an increased risk of rebound thrombosis, in particular ischemic stroke [29, 30], were not confirmed in a recent randomized controlled study [31].
There are some other strategies to reverse (mostly unfractionated) heparin, such as platelet factor-4, heparanase, or extracorporeal heparin-removal devices, but none of these approaches have been properly evaluated and they are not currently approved for clinical use [32–34].
Pentasaccharides
Pentasaccharides are recently developed synthetic compounds that effectively bind and potentiate antithrombin to block factor Xa. Since they lack the additional glycosaminoglycan saccharide residues to bind to thrombin, it has an effect on factor Xa exclusively. The prototype pentasaccharide (and the only one approved for clinical use so far) is fondaparinux. Another pentasaccharide that is currently under study is idraparinux. The main difference between these two agents is the elimination half-life, which is 15–20 h for fondaparinux and 5½ days for idraparinux. This means that idraparinux can be administered once weekly, which renders the subcutaneous route of administration less cumbersome. Pentasaccharides were shown to be effective in the prophylaxis and treatment of venous thromboembolism and are currently evaluated in other types of thrombosis [35]. The (very) long half-life of pentasaccharides necessitates the availability of a suitable antidote if major bleeding complicates the treatment, which may especially occur in patients that are treated with therapeutic doses of this type of anticoagulation. So far, there is no antidote for pentasaccharides that has been studied in controlled clinical studies [36]. The only agent that has been systematically evaluated to reverse the anticoagulant effect of pentasaccharides is recombinant factor VIIa (rVIIa). Two randomized placebo-controlled studies in healthy volunteers have tested the hypothesis that rVIIa may be useful as a suitable antidote for pentasaccharide anticoagulation [37, 38]. In the first study 16 subjects were treated with therapeutic doses of the pentasaccharide fondaparinux and after 2 h (at the time of maximal anticoagulation) challenged with rVIIa or placebo. Injection of rVIIa (90 μg/kg) after fondaparinux normalized the prolonged aPTT and prothrombin time (PT) and reversed the decrease in prothrombin activation fragments 1 + 2 (F(1 + 2)), as observed with fondaparinux alone. Thrombin-generation time and endogenous thrombin potential, which were inhibited by fondaparinux, normalized up to 6 h after rVIIa injection. In the second study 12 subjects received a single s.c. dose of 7.5 mg idraparinux (which is 3 fold higher than the currently recommended dose). The inhibition of thrombin generation by idraparinux, as reflected by an increased thrombin generation time (TGT) and decreased level of prothrombin fragment 1 + 2 (F1+2), was partially reversed by injection of rVIIa 3 h after idraparinux administration. The administration of rVIIa 1 week after treatment with idraparinux (when much lower, though still therapeutic, doses of the pentasaccharide were present) resulted in an nearly complete reversal of anticoagulation, reflected by normalization of thrombin generation time and other markers of thrombin generation. As mentioned, there are no controlled trials in patients who present with pentasaccharide-induced bleeding but there is some anecdotal experience suggesting that rVIIa may indeed be able to stop bleeding in patients anticoagulated with fondaparinux.
Vitamin K Antagonists
When interrupting the administration of VKA’s important differences in the half-lives of the various agents (9 h for acenocoumarol, 36–42 h for warfarin, and 90 h for phenprocoumon, respectively) need to be taken into account [39]. The most straightforward intervention to counteract the effect of VKA’s is the administration of vitamin K [40]. There is quite some debate on the use of vitamin K in patients with a too high INR but no signs of bleeding. However, a recent randomized controlled trial did not find any difference in bleeding or other complications in nonbleeding patients with INR values of 4.5 to 10 that were treated with vitamin K or placebo [41]. In patients with clinically significant bleeding administration of vitamin K is crucial to reverse the anticoagulant effect of VKA’s. Vitamin K can be given orally and intravenously, whereas the parenteral route has the advantage of a more rapid onset of the treatment [42]. After the administration of i.v. vitamin K, within 2 h the INR will start to drop and will be completely normalized within 12–16 h [43], whereas after oral administration it will take up to 24 h to normalize the INR [40]. Intramuscular injections of vitamin K should be avoided in patients who are anticoagulated and subcutaneous administration of vitamin K results in a less predictable bioavailability [42]. A potential concern with the use of parenteral vitamin K is the occurrence of anaphylactic reactions, although the incidence of this complication is very low, in particular with the more modern micelle preparations [44].
In case of very serious or even life-threatening bleeding, immediate correction of the INR is mandatory and can be achieved by the administration of vitamin K-dependent coagulation factors. Theoretically, these factors are present in fresh frozen plasma, however, the amount of plasma that is required to correct the INR is very large, carries the risk of fluid overload, and will probably take hours to administer [45]. Therefore, prothrombin complex concentrates (PCC’s), containing all vitamin K-dependent coagulation factors, are more useful. Although PCC’s can indeed be given using fixed dose schemes, it has been shown that individualized dosing regimens based on INR at presentation and body weight are more effective [46]. In a prospective study in patients using VKA and presenting with bleeding also found that PCC’s resulted in at least satisfactory and sustained hemostasis in 98 % [47]. In recent years the safety of PCC’s, in particular regarding the transmission of blood-borne infectious diseases, has markedly improved owing to several techniques, such as pasteurization, nanofiltration, and addition of solvent detergent. The risk of disseminated intravascular coagulation (DIC) due to traces of activated coagulation factors in PCC’s comes from older literature and modern PCC’s seem not to be associated with eliciting DIC [48].
New Direct Factor Xa Inhibitors
In recent years a large number of new antithrombotic agents has been developed and tested in clinical trials and many of these new agents will become available for clinical practice in the very near future [49]. The need for new anticoagulant agents is quite obvious; Firstly, the current agents are insufficiently effective. For example 10–15 % of patients undergoing major orthopedic surgery develop venous thromboembolism, despite prophylaxis with low molecular weight (LMW) heparin [50]. Furthermore, the available anticoagulants are relatively unsafe, mostly due to the occurrence of bleeding as discussed hereabove. Lastly, current anticoagulant agents are often cumbersome with regards to their clinical use, requiring repeated laboratory control and frequent dose adjustments. Increasing knowledge on the function of the haemostatic system in vivo has resulted in a new generation of anticoagulant agents.
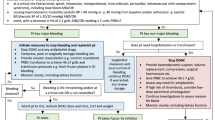
Some of these new class of anticoagulants are directed at factor Xa. Prototypes of these agents are rivaroxaban and apixaban, which have shown promising results in clinical studies [51, 52]. In trials in patients with acute venous thromboembolism rivaroxaban and apixaban were as effective as LMW heparin but rivaroxaban was associated with a lower incidence of bleeding complications (2.2 % versus 8.8 %) [53, 54]. Rivaroxaban was also studied in patients with acute coronary syndromes and showed a dose-dependent efficacy but also increased rates of major bleeding at higher doses [55]. Similarly, apixaban showed a similar pattern and exhibited 2.5 fold increased bleeding rates, in particular in patients using simultaneous anti-platelet agents [56]. Taken together, compared to LMW heparin direct factor Xa inhibitors result at doses achieving equivalent efficacy a lower bleeding risk and at doses achieving higher efficacy a similar bleeding risk. This means that for some clinical situations these drugs may represent an important improvement, however, the risk of (major) bleeding is still present. Recently it was shown that the administration of prothrombin complex concentrate (PCC) resulted in a correction of the prolonged prothrombin time and restored depressed thrombin generation after rivaroxaban treatment in a controlled trial in healthy human subjects (Fig. 7.1) [57]. The effect of PCC’s on reversal of the anticoagulant effect of oral factor Xa inhibitors was confirmed in a series of experiments in animals and human subjects [58–60]. The clinical efficacy in bleeding patients, however, needs to be established.
Restoration of rivaroxaban-induced impaired thrombin generation, measured by endogenous thrombin potential (ETP), by administration of prothrombin complex concentrates (squares) as compared to placebo (circles) in healthy volunteers. Mean ± SD are reported, the difference between the two groups is statistically significant (p < 0.001 Repeated Measures ANOVA)
Direct Thrombin Inhibitors
Another important group of new anticoagulants is the class of direct thrombin inhibitors. Thrombin is the central enzyme in the coagulation process, not only mediating the conversion of fibrinogen to fibrin, but also being the most important physiological activator of platelets and various other coagulation factors. Inhibition of thrombin can be achieved by administration of heparin, but in view of the limited capability of the heparin-antithrombin complex to inhibit surface-bound thrombin, new antithrombin-independent anticoagulants have been developed [61]. Prototype of these thrombin inhibitors is hirudin, originally derived from the saliva from leeches (hirudo medicinalis) and nowadays produced by recombinant technology. Melagatran is a synthetic thrombin inhibitor, which has predictable pharmacokinetic properties and can thus be used in a fixed dose [62]. Moreover, the pro-drug ximelagatran is relatively quickly absorbed after oral ingestion and results in a sufficient systemic availability, rendering this agent suitable for long-term use as oral anticoagulant. Despite clinical trials on prevention and treatment of venous thromboembolism and in patients with atrial fibrillation showing a promising efficacy of ximelagatran, the compound has been withdrawn by the manufacturer, due to the occurrence of enhanced liver enzymes in 6–7 % of patients. Recently, dabigatran, also a direct thrombin inhibitor with good and relatively stable bioavailability after oral ingestion, has been introduced and licensed for prevention of venous thromboembolism after orthopedic surgery. Indeed, clinical trials evaluating dabigatran against LMW heparin in patients undergoing major othropedic surgery show similar or slightly better efficacy of the direct thrombin inhibtor and similar bleeding rates [63, 64]. The largest group of patients using long-term anticoagulants, however, are those with atrial fibrillation. In these patients dabigatran (150 mg twice daily) showed a significantly lower rate of thromboembolic complications compared to warfarin (relative risk 0.66; 95 % confidence interval 0.53–0.82) but also a slightly lower risk of major hemorrhage (3.11 %/year in the dabigatran group versus 3.36 %/year in the warfarin group) [65]. Based on these findings and if confirmed by other ongoing major trials, it may be quite likely that in the future oral anticoagulant treatment with vitamin K antagonists is going to be replaced by treatment with directly acting anticoagulants, such as direct thrombin inhibitors. However, the risk of major bleeding is still relatively large and requires adequate management strategies.
For each of the direct thrombin inhibitors no established antidote is available in case of serious bleeding complicating the anticoagulant treatment. Again, the half-life of most of the agents is relatively short, hence in case of less serious bleeding interruption of treatment will be sufficient to reverse the anticoagulant effect. However, if immediate reversal is required, it is not clear which would be the best strategy. In a controlled clinical study in healthy subjects the melagatran-induced effects on aPTT, thrombin generation and platelet activation were not affected by the administration of rVIIa [66]. Also, in human subjects challenged with dabigatran there was no reversal of the anticoagulation by administration of prothrombin complex concentrates [57]. An experimental study of intracerebral hematoma in dabigatran-treated rats, however, demonstrated that relatively high doses of prothrombin complex concentrates were able to reduce hematoma volume [67].
Aspirin
Aspirin is effective in the secondary prevention of atherothrombotic disease, in particular coronary artery disease, cerebrovascular thromboembolism and peripheral arterial disease [68]. As a consequence, aspirin is one of the most widely used agents in the Western world. Aspirin increases the risk of bleeding, in particular gastro-intestinal bleeding, and has been associated with a small but consistent increase in intracerebral hemorrhage. In addition, it has been shown that the use of aspirin is associated with increased perioperative blood loss in major procedures, although this does not necessarily translates into clinically relevant endpoints, such as the requirement for transfusion or re-operation [69]. Over the last years the approach to the patient who uses aspirin and who presents with bleeding or needs to undergo an invasive procedure has changed considerably. In fact, in current clinical practice bleeding can almost always be managed with local hemostatic procedures or conservative strategies without interrupting aspirin and also most invasive procedures do not require the cessation of aspirin when adequate attention is given to local hemostasis. In contrast, interruption of aspirin has been associated with an increased risk of thromboembolic complications, potentially due to a rebound hypercoagulability. Obviously, in special clinical circumstances, such as intracranial bleeding or the need to undergo a neurosurgical or ophthalmic procedure, the anti-hemostatic effect of aspirin needs to be reversed immediately. The most rigorous measure to achieve that is the administration of platelet concentrate after cessation of aspirin. Another approach is the administration of de-amino d-arginin vasopressin (DDAVP, desmopressin). DDAVP is a vasopressin analogue that despite minor molecular differences has retained its antidiuretic properties but has much less vaso-active effects [70]. DDAVP induces release of the contents of the endothelial cell associated Weibel Palade bodies, including von Willebrand factor. Hence, the administration of DDAVP results in a marked increase in the plasma concentration of von Willebrand factor (and associated coagulation factor VIII) and (also by yet unexplained additional mechanisms) a remarkable augmentation of primary hemostasis as a consequence. DDAVP is effective in patients with mild hemophilia A or von Willebrand’s disease and in patients with qualitative platelet defects, such as in uremia or liver cirrhosis. DDAVP seems also capable of correcting the aspirin-induced platelet dysfunction, although large clinical studies employing relevant outcome parameters are missing [71]. The combined effect of platelet concentrate and subsequent administration of DDAVP has also been advocated to correct the aspirin effect on platelets. The standard dose of DDAVP is 0.3–0.4 μg/kg in 100 ml saline over 30 min and its effect is immediate.
Thienopyridine Derivatives
Clopidogrel, prasugrel and ticagrelor belong to the class of thienopyridine derivatives, which act by blocking the adenosine diphosphate (ADP) receptor on the platelet. Clinical studies have shown that clopidogrel is as good as aspirin in the secondary prevention of atherothrombotic events [72]. Importantly, the combination of aspirin and clopidogrel is vastly superior over aspirin alone in patients who have received intracoronary stents or in other patients with high risk coronary artery disease. There is ample evidence that dual platelet inhibition of aspirin plus clopidogrel has a significantly higher efficacy than aspirin alone in patients with acute coronary syndromes who have undergone coronary interventions for at least a year (and possibly longer) after the event. However, the increased efficacy of the combined use of aspirin and clopidogrel is also associated with a significantly higher bleeding risk [73]. Prasugrel is another thienopyridine derivative that after rapid and almost complete absorption after oral ingestion irreversibly binds to the ADP receptor. Prasugrel has a stronger anti-platelet effect than clopidogrel because of more effective metabolism and less dependence of cytochrome P450 enzymes that may be subject to genetic polymorphisms [74]. Prasugrel was shown to be more effective than clopidogrel in preventing ischemic events in patients with ST elevation myocardial infarction undergoing primary percutaneous coronary interventions (with or without stent) [75]. Rates of major bleeding were similar between clopidogrel and prasugrel, however, the rate of serious bleeding in patients requiring emergency coronary artery bypass grafting (CABG) was higher in the prasugrel group. In patients with acute coronary syndromes prasugrel was also more effective than clopidogrel in preventing cardiovascular death, myocardial infarction and stroke, however, major bleeding rates were higher in the prasugrel group (2.4 % versus 1.8 %) [76]. Of note, this disadvantage of prasugrel did not outweigh the efficacy benefit, and the net clinical benefit (defined as the efficacy gain minus the increased risk of major bleeding) was preserved in favour of prasugrel. Ticagrelor is a cyclopentyltriazolopyrimidine that differs from thienopyridines (ticlopidin, clopidogrel, prasugrel), as ticagrelor is not a prodrug requiring active biotransformation by cytochromes in the liver and thus is characterized by a more rapid, more effective and more consistent platelet inhibition than ticlopidin or clopidogrel [77]. The Platelet Inhibition and Patient Outcomes (PLATO) trial determined whether ticagrelor was superior to clopidogrel for the prevention of vascular events and death in a broad population of patients presenting with an acute coronary syndrome [78]. treatment with ticagrelor as compared with clopidogrel significantly reduced the rate of death from vascular causes, myocardial infarction, or stroke. The ticagrelor and clopidogrel groups did not differ significantly with regard to the rates of major bleeding as defined in the trial or according to the Thrombolysis in Myocardial Infarction (TIMI) criteria. The two treatment groups did not differ significantly in the rates of CABG-related major bleeding or bleeding requiring transfusion of red cells. However, in the ticagrelor group, there was a higher rate of non–CABG-related major bleeding according to the study criteria and the TIMI criteria. With ticagrelor as compared with clopidogrel, there were more episodes of intracranial bleeding, including fatal intracranial bleeding. However, there were fewer episodes of other types of fatal bleeding in the ticagrelor group. Recently, a fourth thienopyridine derivative has been introduced: cangrelor. The advantage of this compound over the other members of this group is the faster onset of action, which may be critical in acute coronary syndromes. However, two major clinical trials comparing cangrelor with clopidogrel in patients undergoing percutaneous coronary interventions did not show a higher efficacy of cangrelor but did demonstrate a significantly higher risk of bleeding [79, 80]. Taken together, dual platelet inhibition, in particular with clopidogrel or even more outspoken with prasugrel, is highly effective in high risk patients with coronary artery disease but the bleeding risk with dual platelet inhibition is something to take into account and strategies to reverse the antiplatelet effect may be warranted in case of serious bleeding.
The decision whether or not the interrupt or even reverse antithrombotic treatment with dual platelet inhibition in case of serious bleeding or the need to perform an invasive procedure will depend on the specific clinical situation but also on the indication for the antithrombotic treatment (see above). Especially in patients with recent implantation of an intracoronary stent (in the last 6–12 weeks), cardiologists will often not or only reluctantly agree with cessation of treatment [81]. In this period re-endothelization of the stent has not yet occurred and the patient is very vulnerable to acute thrombotic occlusion of the stent. In patients with drug-eluting stents this period may be even longer. If, however, the decision is made to stop and even reverse the treatment with aspirin and clopidogrel, administration of platelet concentrate is probably the best way to correct the hemostatic defect [82]. In addition, DDAVP was shown to correct the defect in platelet aggregation caused by clopidogrel, so this may be another option [83].
Conclusion
Conventional anticoagulant treatment can be reversed by specific interventions when the clinical situation requires immediate correction of hemostasis. For the new generation of anticoagulants, no specific antidotes are available, although some interventions are promising but need further evaluation. Antiplatelet therapy with aspirin, alone or in combination with thienopyridine derivatives, such as clopidogrel and prasugrel, can be reversed but this is often not required and sometimes not desirable in view of the indication for this treatment.
References
Hirsh J, Guyatt G, Albers GW, Harrington R, Schunemann HJ. Antithrombotic and thrombolytic therapy: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition). Chest. 2008;133(6 Suppl):110S–2.
Mannucci PM, Levi M. Prevention and treatment of major blood loss. N Engl J Med. 2007;356(22):2301–11.
Levi MM, Eerenberg E, Lowenberg E, Kamphuisen PW. Bleeding in patients using new anticoagulants or antiplatelet agents: risk factors and management. Neth J Med. 2010;68(2):68–76.
Eikelboom JW, Mehta SR, Anand SS, Xie C, Fox KA, Yusuf S. Adverse impact of bleeding on prognosis in patients with acute coronary syndromes. Circulation. 2006;114(8):774–82.
Algra A. Medium intensity oral anticoagulants versus aspirin after cerebral ischaemia of arterial origin (ESPRIT): a randomised controlled trial. Lancet Neurol. 2007;6(2):115–24.
Lip GY, Andreotti F, Fauchier L, Huber K, Hylek E, Knight E, Lane DA, Levi M, Marin F, Palareti G, Kirchhof P, Collet JP, Rubboli A, Poli D, Camm J. Bleeding risk assessment and management in atrial fibrillation patients: a position document from the European Heart Rhythm Association, endorsed by the European Society of Cardiology Working Group on Thrombosis. Europace. 2011;13(5):723–46.
Levi M. Emergency reversal of antithrombotic treatment. Intern Emerg Med. 2009;4(2):137–45.
Levi M, Eerenberg E, Kamphuisen PW. Bleeding risk and reversal strategies for old and new anticoagulants and antiplatelet agents. J Thromb Haemost. 2011:9(9)1705–12.
Schulman S, Beyth RJ, Kearon C, Levine MN. Hemorrhagic complications of anticoagulant and thrombolytic treatment: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition). Chest. 2008;133(6 Suppl):257S–98.
Saour JN, Sieck JO, Mamo LA, Gallus AS. Trial of different intensities of anticoagulation in patients with prosthetic heart valves. N Engl J Med. 1990;322(7):428–32.
Vink R, Kraaijenhagen RA, Hutten BA, van den Brink RB, de Mol BA, Buller HR, Levi M. The optimal intensity of vitamin K antagonists in patients with mechanical heart valves: a meta-analysis. J Am Coll Cardiol. 2003;42(12):2042–8.
Hylek EM, Singer DE. Risk factors for intracranial hemorrhage in outpatients taking warfarin. Ann Intern Med. 1994;120(11):897–902.
Hutten BA, Lensing AW, Kraaijenhagen RA, Prins MH. Safety of treatment with oral anticoagulants in the elderly. A systematic review. Drugs Aging. 1999;14(4):303–12.
Fang MC, Chang Y, Hylek EM, Rosand J, Greenberg SM, Go AS, Singer DE. Advanced age, anticoagulation intensity, and risk for intracranial hemorrhage among patients taking warfarin for atrial fibrillation. Ann Intern Med. 2004;141(10):745–52.
Higashi MK, Veenstra DL, Kondo LM, Wittkowsky AK, Srinouanprachanh SL, Farin FM, Rettie AE. Association between CYP2C9 genetic variants and anticoagulation-related outcomes during warfarin therapy. JAMA. 2002;287(13):1690–8.
Reitsma PH, van der Heijden JF, Groot AP, Rosendaal FR, Buller HR. A C1173T dimorphism in the VKORC1 gene determines coumarin sensitivity and bleeding risk. PLoS Med. 2005;2(10):e312.
Levi M, Hovingh GK, Cannegieter SC, Vermeulen M, Buller HR, Rosendaal FR. Bleeding in patients receiving vitamin K antagonists who would have been excluded from trials on which the indication for anticoagulation was based. Blood. 2008;111(9):4471–6.
Hart RG, Benavente O, Pearce LA. Increased risk of intracranial hemorrhage when aspirin is combined with warfarin: a meta-analysis and hypothesis. Cerebrovasc Dis. 1999;9(4):215–7.
Rothberg MB, Celestin C, Fiore LD, Lawler E, Cook JR. Warfarin plus aspirin after myocardial infarction or the acute coronary syndrome: meta-analysis with estimates of risk and benefit. Ann Intern Med. 2005;143(4):241–50.
Hallas J, Dall M, Andries A, Andersen BS, Aalykke C, Hansen JM, Andersen M, Lassen AT. Use of single and combined antithrombotic therapy and risk of serious upper gastrointestinal bleeding: population based case-control study. BMJ. 2006;333(7571):726.
Mellemkjaer L, Blot WJ, Sorensen HT, Thomassen L, McLaughlin JK, Nielsen GL, Olsen JH. Upper gastrointestinal bleeding among users of NSAIDs: a population-based cohort study in Denmark. Br J Clin Pharmacol. 2002;53(2):173–81.
Battistella M, Mamdami MM, Juurlink DN, Rabeneck L, Laupacis A. Risk of upper gastrointestinal hemorrhage in warfarin users treated with nonselective NSAIDs or COX-2 inhibitors. Arch Intern Med. 2005;165(2):189–92.
Hirsh J, Bauer KA, Donati MB, Gould M, Samama MM, Weitz JI. Parenteral anticoagulants: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition). Chest. 2008;133(6 Suppl):141S–59.
Lindblad B, Borgstrom A, Wakefield TW, Whitehouse Jr WM, Stanley JC. Protamine reversal of anticoagulation achieved with a low molecular weight heparin. The effects on eicosanoids, clotting and complement factors. Thromb Res. 1987;48(1):31–40.
Massonnet-Castel S, Pelissier E, Bara L, Terrier E, Abry B, Guibourt P, Swanson J, Jaulmes B, Carpentier A, Samama M. Partial reversal of low molecular weight heparin (PK 10169) anti-Xa activity by protamine sulfate: in vitro and in vivo study during cardiac surgery with extracorporeal circulation. Haemostasis. 1986;16(2):139–46.
Van Ryn-McKenna J, Cai L, Ofosu FA, Hirsh J, Buchanan MR. Neutralization of enoxaparine-induced bleeding by protamine sulfate. Thromb Haemost. 1990;63(2):271–4.
Bang CJ, Berstad A, Talstad I. Incomplete reversal of enoxaparin-induced bleeding by protamine sulfate. Haemostasis. 1991;21(3):155–60.
Caplan SN, Berkman EM. Letter: protamine sulfate and fish allergy. N Engl J Med. 1976;295(3):172.
Fearn SJ, Parry AD, Picton AJ, Mortimer AJ, McCollum CN. Should heparin be reversed after carotid endarterectomy? A randomised prospective trial. Eur J Vasc Endovasc Surg. 1997;13(4):394–7.
Mauney MC, Buchanan SA, Lawrence WA, Bishop A, Sinclair K, Daniel TM, Tribble CG, Kron IL. Stroke rate is markedly reduced after carotid endarterectomy by avoidance of protamine. J Vasc Surg. 1995;22(3):264–9.
Dellagrammaticas D, Lewis SC, Gough MJ. Is heparin reversal with protamine after carotid endarterectomy dangerous? Eur J Vasc Endovasc Surg. 2008;36(1):41–4.
D’Ambra M. Restoration of the normal coagulation process: advances in therapies to antagonize heparin. J Cardiovasc Pharmacol. 1996;27 Suppl 1:S58–62.
Despotis GJ, Summerfield AL, Joist JH, Goodnough LT, Santoro SA, Zimmermann JJ, Lappas DG. In vitro reversal of heparin effect with heparinase: evaluation with whole blood prothrombin time and activated partial thromboplastin time in cardiac surgical patients. Anesth Analg. 1994;79(4):670–4.
Tao W, Deyo DJ, Brunston Jr RL, Vertrees RA, Zwischenberger JB. Extracorporeal heparin adsorption following cardiopulmonary bypass with a heparin removal device–an alternative to protamine. Crit Care Med. 1998;26(6):1096–102.
Buller HR. Treatment of symptomatic venous thromboembolism: improving outcomes. Semin Thromb Hemost. 2002;28 Suppl 2:41–8.
Crowther MA, Warkentin TE. Bleeding risk and the management of bleeding complications in patients undergoing anticoagulant therapy: focus on new anticoagulant agents. Blood. 2008;111(10):4871–9.
Bijsterveld NR, Vink R, van Aken BE, Fennema H, Peters RJ, Meijers JC, Buller HR, Levi M. Recombinant factor VIIa reverses the anticoagulant effect of the long-acting pentasaccharide idraparinux in healthy volunteers. Br J Haematol. 2004;124:653–8.
Bijsterveld NR, Moons AH, Boekholdt SM, van Aken BE, Fennema H, Peters RJ, Meijers JC, Buller HR, Levi M. Ability of recombinant factor VIIa to reverse the anticoagulant effect of the pentasaccharide fondaparinux in healthy volunteers. Circulation. 2002;106(20):2550–4.
Ansell J, Hirsh J, Hylek E, Jacobson A, Crowther M, Palareti G. Pharmacology and management of the vitamin K antagonists: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition). Chest. 2008;133(6 Suppl):160S–98.
Dentali F, Ageno W, Crowther M. Treatment of coumarin-associated coagulopathy: a systematic review and proposed treatment algorithms. J Thromb Haemost. 2006;4(9):1853–63.
Crowther MA, Ageno W, Garcia D, Wang L, Witt DM, Clark NP, Blostein MD, Kahn SR, Vesely S, Schulman S, Kovacs MJ, Rodger MA, Wells P, Anderson D, Ginsberg JS, Selby R, Siragusa S, Silingardi M, Dowd MB, Kearon C. Oral vitamin K versus placebo to correct excessive anticoagulation in patients receiving warfarin. Ann Intern Med. 2009;150:293–300.
Crowther MA, Douketis JD, Schnurr T, Steidl L, Mera V, Ultori C, Venco A, Ageno W. Oral vitamin K lowers the international normalized ratio more rapidly than subcutaneous vitamin K in the treatment of warfarin-associated coagulopathy. A randomized, controlled trial. Ann Intern Med. 2002;137(4):251–4.
Lubetsky A, Yonath H, Olchovsky D, Loebstein R, Halkin H, Ezra D. Comparison of oral vs intravenous phytonadione (vitamin K1) in patients with excessive anticoagulation: a prospective randomized controlled study. Arch Intern Med. 2003;163(20):2469–73.
Dentali F, Ageno W. Management of coumarin-associated coagulopathy in the non-bleeding patient: a systematic review. Haematologica. 2004;89(7):857–62.
Aguilar MI, Hart RG, Kase CS, Freeman WD, Hoeben BJ, Garcia RC, Ansell JE, Mayer SA, Norrving B, Rosand J, Steiner T, Wijdicks EF, Yamaguchi T, Yasaka M. Treatment of warfarin-associated intracerebral hemorrhage: literature review and expert opinion. Mayo Clin Proc. 2007;82(1):82–92.
van Aart L, Eijkhout HW, Kamphuis JS, Dam M, Schattenkerk ME, Schouten TJ, Ploeger B, Strengers PF. Individualized dosing regimen for prothrombin complex concentrate more effective than standard treatment in the reversal of oral anticoagulant therapy: an open, prospective randomized controlled trial. Thromb Res. 2006;118(3):313–20.
Pabinger I, Brenner B, Kalina U, Knaub S, Nagy A, Ostermann H. Prothrombin complex concentrate (Beriplex P/N) for emergency anticoagulation reversal: a prospective multinational clinical trial. J Thromb Haemost. 2008;6(4):622–31.
Levi M. Disseminated intravascular coagulation. Crit Care Med. 2007;35:2191–5.
Levi M. New antithrombotics in the treatment of thromboembolic disease. Eur J Intern Med. 2005;16(4):230–7.
Strebel N, Prins M, Agnelli G, Buller HR. Preoperative or postoperative start of prophylaxis for venous thromboembolism with low-molecular-weight heparin in elective hip surgery? Arch Intern Med. 2002;162(13):1451–6.
Agnelli G, Gallus A, Goldhaber SZ, Haas S, Huisman MV, Hull RD, Kakkar AK, Misselwitz F, Schellong S. Treatment of proximal deep-vein thrombosis with the oral direct factor Xa inhibitor rivaroxaban (BAY 59–7939): the ODIXa-DVT (Oral Direct Factor Xa Inhibitor BAY 59–7939 in Patients With Acute Symptomatic Deep-Vein Thrombosis) study. Circulation. 2007;116(2):180–7.
Shantsila E, Lip GY. Apixaban, an oral, direct inhibitor of activated Factor Xa. Curr Opin Investig Drugs. 2008;9(9):1020–33.
Bauersachs R, Berkowitz SD, Brenner B, Buller HR, Decousus H, Gallus AS, Lensing AW, Misselwitz F, Prins MH, Raskob GE, Segers A, Verhamme P, Wells P, Agnelli G, Bounameaux H, Cohen A, Davidson BL, Piovella F, Schellong S. Oral rivaroxaban for symptomatic venous thromboembolism. N Engl J Med. 2010;363(26):2499–510.
Buller HR, Prins MH, Lensin AW, Decousus H, Jacobson BF, Minar E, Chlumsky J, Verhamme P, Wells P, Agnelli G, Cohen A, Berkowitz SD, Bounameaux H, Davidson BL, Misselwitz F, Gallus AS, Raskob GE, Schellong S, Segers A. Oral rivaroxaban for the treatment of symptomatic pulmonary embolism. N Engl J Med. 2012;366(14):1287–97.
Mega JL, Braunwald E, Mohanavelu S, Burton P, Poulter R, Misselwitz F, Hricak V, Barnathan ES, Bordes P, Witkowski A, Markov V, Oppenheimer L, Gibson CM. Rivaroxaban versus placebo in patients with acute coronary syndromes (ATLAS ACS-TIMI 46): a randomised, double-blind, phase II trial. Lancet. 2009;374(9683):29–38.
Alexander JH, Becker RC, Bhatt DL, Cools F, Crea F, Dellborg M, Fox KA, Goodman SG, Harrington RA, Huber K, Husted S, Lewis BS, Lopez-Sendon J, Mohan P, Montalescot G, Ruda M, Ruzyllo W, Verheugt F, Wallentin L. Apixaban, an oral, direct, selective factor Xa inhibitor, in combination with antiplatelet therapy after acute coronary syndrome: results of the Apixaban for Prevention of Acute Ischemic and Safety Events (APPRAISE) trial. Circulation. 2009;119(22):2877–85.
Eerenberg ES, Kamphuisen PW, Sijpkens MK, Meijers JC, Buller HR, Levi M. Reversal of rivaroxaban and dabigatran by prothrombin complex concentrate: a randomized, placebo-controlled, crossover study in healthy subjects. Circulation. 2011;124:1573–9.
Fukuda T, Honda Y, Kamisato C, Morishima Y, Shibano T. Reversal of anticoagulant effects of edoxaban, an oral, direct factor Xa inhibitor, with haemostatic agents. Thromb Haemost. 2012;107(2):253–9.
Zhou W, Zorn M, Nawroth P, Butehorn U, Perzborn E, Heitmeier S, Veltkamp R. Hemostatic therapy in experimental intracerebral hemorrhage associated with rivaroxaban. Stroke. 2013;44(3):771–8.
Marlu R, Hodaj E, Paris A, Albaladejo P, Cracowski JL, Pernod G. Effect of non-specific reversal agents on anticoagulant activity of dabigatran and rivaroxaban: a randomised crossover ex vivo study in healthy volunteers. Thromb Haemost. 2012;108(2):217–24.
Weitz JI, Buller HR. Direct thrombin inhibitors in acute coronary syndromes: present and future. Circulation. 2002;105(8):1004–11.
Wahlander K, Lapidus L, Olsson CG, Thuresson A, Eriksson UG, Larson G, Eriksson H. Pharmacokinetics, pharmacodynamics and clinical effects of the oral direct thrombin inhibitor ximelagatran in acute treatment of patients with pulmonary embolism and deep vein thrombosis. Thromb Res. 2002;107(3–4):93–9.
Eriksson BI, Smith H, Yasothan U, Kirkpatrick P. Dabigatran etexilate. Nat Rev Drug Discov. 2008;7(7):557–8.
Eriksson BI, Dahl OE, Rosencher N, Kurth AA, van Dijk CN, Frostick SP, Prins MH, Hettiarachchi R, Hantel S, Schnee J, Buller HR. Dabigatran etexilate versus enoxaparin for prevention of venous thromboembolism after total hip replacement: a randomised, double-blind, non-inferiority trial. Lancet. 2007;370(9591):949–56.
Connolly SJ, Ezekowitz MD, Yusuf S, Eikelboom J, Oldgren J, Parekh A, Pogue J, Reilly PA, Themeles E, Varrone J, Wang S, Alings M, Xavier D, Zhu J, Diaz R, Lewis BS, Darius H, Diener HC, Joyner CD, Wallentin L. Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med. 2009;361(12):1139–51.
Woltz M, Levi M, Sarich TC, Bostrom SL, Ericksson UG, Erikkson M, Svensson M, Weitz JI, Elg M, Wahlander K. Effect of recombinant factor VIIa on melagatran-induced inhibition of thrombin generation and platelet activation in healthy volunteers. Thromb Haemost. 2004;91:1090–6.
Zhou W, Schwarting S, Illanes S, Liesz A, Middelhoff M, Zorn M, Bendszus M, Heiland S, Van RJ, Veltkamp R. Hemostatic therapy in experimental intracerebral hemorrhage associated with the direct thrombin inhibitor dabigatran. Stroke. 2011;42(12):3594–9.
Patrono C, Baigent C, Hirsh J, Roth G. Antiplatelet drugs: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition). Chest. 2008;133(6 Suppl):199S–233.
Merritt JC, Bhatt DL. The efficacy and safety of perioperative antiplatelet therapy. J Thromb Thrombolysis. 2004;17(1):21–7.
Richardson DW, Robinson AG. Desmopressin. [Review] [165 refs]. Ann Intern Med. 1985;103(2):228–39.
Reiter RA, Mayr F, Blazicek H, Galehr E, Jilma-Stohlawetz P, Domanovits H, Jilma B. Desmopressin antagonizes the in vitro platelet dysfunction induced by GPIIb/IIIa inhibitors and aspirin. Blood. 2003;102(13):4594–9.
Anonymous. A randomised, blinded, trial of clopidogrel versus aspirin in patients at risk of ischaemic events (CAPRIE). CAPRIE Steering Committee [see comments]. Lancet. 1996;348(9038):1329–39.
Yusuf S, Zhao F, Mehta SR, Chrolavicius S, Tognoni G, Fox KK. Effects of clopidogrel in addition to aspirin in patients with acute coronary syndromes without ST-segment elevation. N Engl J Med. 2001;345(7):494–502.
Bhatt DL. Prasugrel in clinical practice. N Engl J Med. 2009;361(10):940–2.
Montalescot G, Wiviott SD, Braunwald E, Murphy SA, Gibson CM, McCabe CH, Antman EM. Prasugrel compared with clopidogrel in patients undergoing percutaneous coronary intervention for ST-elevation myocardial infarction (TRITON-TIMI 38): double-blind, randomised controlled trial. Lancet. 2009;373(9665):723–31.
Wiviott SD, Braunwald E, McCabe CH, Montalescot G, Ruzyllo W, Gottlieb S, Neumann FJ, Ardissino D, De SS, Murphy SA, Riesmeyer J, Weerakkody G, Gibson CM, Antman EM. Prasugrel versus clopidogrel in patients with acute coronary syndromes. N Engl J Med. 2007;357(20):2001–15.
Giannitsis E, Katus A. Antiplatelet therapy – ticagrelor. Hamostaseologie. 2012;32:177–85.
Wallentin L, Becker RC, Budaj A, Cannon CP, Emanuelsson H, Held C, et al. Ticagrelor versus clopidogrel in patients with acute coronary syndromes. N Engl J Med. 2009;361:1045–57.
Bhatt DL, Lincoff AM, Gibson CM, Stone GW, McNulty S, Montalescot G, Kleiman NS, Goodman SG, White HD, Mahaffey KW, Pollack Jr CV, Manoukian SV, Widimsky P, Chew DP, Cura F, Manukov I, Tousek F, Jafar MZ, Arneja J, Skerjanec S, Harrington RA. Intravenous platelet blockade with cangrelor during PCI. N Engl J Med. 2009;361(24):2330–41.
Harrington RA, Stone GW, McNulty S, White HD, Lincoff AM, Gibson CM, Pollack Jr CV, Montalescot G, Mahaffey KW, Kleiman NS, Goodman SG, Amine M, Angiolillo DJ, Becker RC, Chew DP, French WJ, Leisch F, Parikh KH, Skerjanec S, Bhatt DL. Platelet inhibition with cangrelor in patients undergoing PCI. N Engl J Med. 2009;361(24):2318–29.
Grines CL, Bonow RO, Casey Jr DE, Gardner TJ, Lockhart PB, Moliterno DJ, O’Gara P, Whitlow P. Prevention of premature discontinuation of dual antiplatelet therapy in patients with coronary artery stents: a science advisory from the American Heart Association, American College of Cardiology, Society for Cardiovascular Angiography and Interventions, American College of Surgeons, and American Dental Association, with representation from the American College of Physicians. Catheter Cardiovasc Interv. 2007;69(3):334–40.
Vilahur G, Choi BG, Zafar MU, Viles-Gonzalez JF, Vorchheimer DA, Fuster V, Badimon JJ. Normalization of platelet reactivity in clopidogrel-treated subjects. J Thromb Haemost. 2007;5(1):82–90.
Leithauser B, Zielske D, Seyfert UT, Jung F. Effects of desmopressin on platelet membrane glycoproteins and platelet aggregation in volunteers on clopidogrel. Clin Hemorheol Microcirc. 2008;39(1–4):293–302.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer-Verlag London
About this chapter
Cite this chapter
Levi, M. (2014). Management of Bleeding Complications. In: Avanzas, P., Clemmensen, P. (eds) Pharmacological Treatment of Acute Coronary Syndromes. Current Cardiovascular Therapy. Springer, London. https://doi.org/10.1007/978-1-4471-5424-2_7
Download citation
DOI: https://doi.org/10.1007/978-1-4471-5424-2_7
Published:
Publisher Name: Springer, London
Print ISBN: 978-1-4471-5423-5
Online ISBN: 978-1-4471-5424-2
eBook Packages: MedicineMedicine (R0)