Abstract
The ability to diagnose basic arrhythmias and conduction disorders in infants, children, adolescents, and adults with congenital heart disease is a fundamental of pediatric and adult congenital cardiovascular medicine. This chapter provides basic knowledge regarding the physiology of cardiac conduction, practical information on the diagnosis of common rhythm disturbances, and general instruction on the primary methods for acquisition of electrocardiographic data, including body surface electrocardiography, ambulatory monitoring, and provocative electrophysiology study. The knowledge obtained from this chapter will form a foundation for further understanding rhythm disturbances in even the most complex patients with congenital heart disease.
Access provided by Autonomous University of Puebla. Download reference work entry PDF
Similar content being viewed by others
Keywords
- Atrial fibrillation
- Atrial flutter
- Atrioventricular nodal reentrant tachycardia
- Atrioventricular reciprocating tachycardia
- Automaticity
- Bradycardia
- Bundle branch block
- Complete heart block
- Dysrhythmia
- Ectopic atrial tachycardia
- Electrocardiogram
- Electrophysiology
- First- and second-degree atrioventricular block
- Junctional ectopic tachycardia
- Reentry
- Signal-averaged electrocardiography
- Sinoatrial node dysfunction
- Supraventricular tachycardia
- Tachycardia
- Triggered activity
- Ventricular tachycardia
- Vectorcardiography
Introduction
The cardiac rhythm strip and multichannel electrocardiogram represent the summative contribution of structural, metabolic, hemodynamic, and electrical influences on the atrial and ventricular myocardia and on the specialized cardiac conduction system. The overarching intent of this chapter is to convey a practical approach toward diagnostic accuracy when confronted with cardiac arrhythmias and conductive disorders in children and all patients having congenital heart disease. However, most of the principles of arrhythmia interpretation are applicable to humans of all ages. This foundation will be augmented by more specific comments regarding certain arrhythmias, especially pediatric bradyarrhythmias and conduction defects, in an effort to supplement other chapters in this text. The remainder of this chapter is devoted to the technical acquisition of cardiac rhythm data in the youngster. To that end, noninvasive rhythm recording instruments will be emphasized, but an introduction to intracardiac electrophysiologic testing will also be included. This chapter will not emphasize electrocardiographic characteristics of specific pre- and postoperative congenital heart defects, rhythm strip interpretation from patients having implanted cardiac rhythm management devices, interpretation of immediate postoperative arrhythmias from temporary pacing wires, and arrhythmias related to orthotopic cardiac transplantation. Also, this chapter is not intended to be a primer for basic pediatric 12- or 15-lead electrocardiogram (ECG) interpretation.
Cardiac Electrophysiology
Cardiac electrogenesis is necessary for electromechanical coupling, and it initiates and proceeds in an anatomic sequence which optimizes hemodynamic performance. The primary molecular “parts” include plasma membrane-linked voltage- and ligand-gated channel proteins (and their interacting proteins) whose activities result in ionic flow according to their electrochemical gradients (e.g., the hyperpolarization-activated, cyclic nucleotide-gated (HCN) channels of the sinoatrial node and rapid and slow delayed rectifier potassium channels of cardiac muscle (Ikr and Iks)), cell-to-cell gap junction proteins for passive ion and other small molecule movement (e.g., connexin43 in working cardiac myocardium and connexin40 in the AV node), and energy-requiring ionic pumps and nonenergy-requiring exchangers for reestablishing cytoplasmic and organelle ion concentrations (e.g., the sodium/potassium ATPase pump, the sodium-calcium exchanger). Each cardiac cell type has its own constitution of these structures, especially of plasma membrane channels (Fig. 157.1). Tissue endowment of these fundamental structures changes through fetal and early postnatal development, under hypoxic and other metabolic stresses, and related to persistent electrical and mechanical (hemodynamic) changes.
Cardiac myocyte action potentials and the primary ion channels. In the top portion are illustrated idealized action potentials from cells from the major cardiac tissues: nodal (sinoatrial and atrioventricular) tissue, atrial myocardium, and ventricular myocardium (including His bundle, bundle branches, and Purkinje fibers). Voltages represent intra- versus extracellular potentials, and the numerals 0–4 represent the classical stages of the action potential: 4 is the resting membrane potential, 0 results from unopposed depolarization via inward currents, 1 and 2 result from competing inward depolarizing and outward repolarizing currents, and 3 results mostly from outward repolarizing currents. The specific currents and their time courses are depicted beneath each action potential. Each current results from specific ion flow along its electromotive gradient and through a (relatively) ion-specific channel. The channel pores, in turn, are formed from conformational changes that occur in multimeric channel proteins (listed to the left). Each channel protein multimer (usually tetramer) changes configuration based upon the voltage milieu, hence, resulting in channel pore “openness.” The orderly opening and closing of myocyte cell membrane channels result in the action potential. This accounts for the following critical phenomena: (a) spontaneous (phase 4) depolarization of those tissues having the property of automaticity (sinoatrial and atrioventricular nodes); (b) Achievement of activation threshold (onset of phase 0) in resting cells downstream from already depolarized cells via passive movement of sodium ions across gap junctions; (c) Initiation of excitation-contraction, as inward calcium current activates calcium-induced calcium release from the sarcoplasmic reticulum; and (d) tissue refractoriness to protect against tetany and inappropriate reentry. CHACNGC = cationic hyperpolarization-activated, cyclic nucleotide-gated (pacemaker) channel; dashed lines by IKACh imply variable influence of acetylcholine-gated potassium channel activity according to parasympathetic tone. Steeper negative slope enhances automaticity. Sinoatrial rate variability is influenced by this channel, the calcium clock (not pictured), and sympathetic nervous system influences on c-AMP gating portion of the HCN gene product
The tissue “parts” capable of cardiac conduction include what is euphemistically considered the specialized conduction system and working myocardium. The only cardiac tissues normally incapable of electrical conduction are the annulus fibrosis and AV valves and the semilunar valves and annuli. Critical to this discussion is the concept of anisotropic conduction, which refers to the influences on cardiac conduction by cell geometry, cell alignment, and density of cell-to-cell connections [1]. This phenomenon is especially vital in understanding the electrical properties of the right atrium, with its regions of smooth walls and dense pectinate muscles. In temporal order, according to fastest automaticity, the specialized conduction system normally “begins” with spontaneous discharge by the sinoatrial node (SAN), a comma-shaped structure, which is subepicardial and lies along the superior portion of the sulcus terminalis. Wavefronts emanating from the SAN were once thought to activate the right atrium and preferentially conduct to the AV node and left atrium via four specialized tracts (of Thoral, of Wenckebach, descending tract, and Bachmann’s bundle). Only Bachmann’s bundle, which is a tract of working atrial myocardium connecting the superomedial right atrium posterior to the ascending aorta to the anterior roof of the left atrium, has survived in modern parlance. As with all working myocardium, atrial muscle has relatively rapid conduction properties, which is enhanced or subdued according to principles of anisotropy. The AV node (AVN) is an oval-shaped structure, which lies on the right side of the atrial septum, just posterior to the hinge-point of the septal leaflet of the tricuspid valve, anterosuperior to the coronary sinus ostium, inferior to the tendon of Todaro, posterior to the membranous septum, and anterosuperior portion of the triangle of Koch. Like the SAN, the AVN has slow conduction properties and capacity for automaticity, though at a slower rate than the SAN. Anatomical approaches to the AVN, especially from superiorly and from postero-inferiorly, contain cell types (so-called transitional cells) which are intermediate between atrial myocardium and AVN cells with respect to histological appearance, channel constitution, and cell-to-cell connections [2]. These characteristics may be important in potentiation of the common form of supraventricular tachycardia, AVN reentrant tachycardia. The anterosuperior portion of the AVN transitions into tissue containing parallel bundles of cells having fast conduction properties, the penetrating bundle (or “bundle of His”). This well-insulated structure penetrates the central fibrous body, whereupon it splits within the crest of the muscular septum into the cord-like right bundle branch (RBB) and the fan-shaped left bundle branch (LBB). The RBB is subendocardial within the anterior right ventricular septum, traveling in the moderator band and terminating in the right ventricular free wall. The LBB is very superficial on the surface of the left ventricular septum, where it roughly divides into anterior and posterior (actually, superior and inferior) divisions. Critically, the terminal elements of the bundle branches continue as the rapidly conducting – and definitively endocardial – Purkinje cell network. The left side of the base of the ventricular septum is the site of earliest ventricular myocardial depolarization from this network. Depolarization is completed within the working ventricular myocardium. There are differences in action potential characteristics of the different layers of the ventricular walls (endocardial, m-cell, and epicardium) and between right and left ventricles, according to differences in repolarizing channel constitutions. An anatomical summary of the specialized conduction system appears as in Fig. 157.2.
Anatomical correlates of cardiac depolarization with the surface ECG. Note that AV nodal depolarization mostly occurs during the terminal portions of the P wave, and that the PR segment largely represents depolarization of the His-bundle branch-Purkinje system. cAVN compact AV node, F fast transitional cell inputs to the compact AV node, S slow transitional cell inputs to the compact AV node
The cardiac rhythm is determined by the influences of intrinsic automaticity and conduction and refractoriness properties (as determined by features of channel endowment and anisotropic conduction) and by external influences of the autonomic nervous system and of hemodynamic circumstances. Sympathetic nervous system influences enhance automaticity of automatic tissues and increase conduction velocity and shorten refractoriness of most tissues. Parasympathetic nervous system influences decrease automaticity of automatic tissues, slow conduction through sinoatrial and AV nodal tissues, and shorten refractoriness in working atrial myocardium. Arrhythmias occur related to congenital channel abnormalities, congenital abnormalities of elements of the specialized conduction system, congenital (or rarely acquired) accessory conducting pathways, abnormal automaticity or conduction in metabolically deranged tissue, or from mechanisms created by micro- or macroregions of fibrosis or artificial obstacles to conduction. Developmental changes that occur in channel properties, channel abundance, electrogenic pumps, channel interacting proteins, cell-to-cell connections, gross tissue and chamber structure, and autonomic innervation account for the normal changes in electrocardiographic intervals (especially heart rate, heart rate variability, PR interval, and QRS duration) and contribute to propensity to age-specific dysrhythmias. The remainder of this chapter is intended to serve as the foundation for other chapters in this textbook. Therefore, the definitions and concepts to follow are generic to the human cardiac conduction system; only the section on “Bradycardias” is specific to the pediatric age range.
Mechanisms of Tachyarrhythimia and of Improved Conduction
Reentry
When a conducting wavefront is capable of renegotiating a structure which it had just depolarized and it does so prior to (“faster than”) depolarization from the ambient pacemaker, reentry is said to have occurred. Traditional criteria necessary for reentry to occur include a tissue source (site A) which is electrically conductive and bypasses a region which is transiently not electrically available (site B), subsequent capacity for conduction through site B in a retrograde direction, and recovery (from refractoriness) of site A after the wavefront has retrogradely traversed site B (Fig. 157.3). Reentry is by far the most common mechanism of pathological tachycardias. The reentry circuit may be large (so-called macro-reentry), as in the case of AV reciprocating tachycardia (in which the critical circuit includes an accessory AV pathway, atrial muscle, the normal specialized AV conduction system, and ventricular muscle), or very small (so-called micro-reentry), involving a small region of atrial or ventricular muscle, some of which has altered conduction/refractoriness properties. In mathematical terms, reentry may only occur within an anatomical region whose net length is larger than the presenting electrical wavelength (λ), defined as the product of the conduction velocity (CV) times the functional refractory period (FRP) of that tissue [3]. (The FRP is defined as the minimum duration in milliseconds during which a particular structure can be depolarized twice.) Hence, structures having regions of slow conduction and having a net relatively short refractory period are conducive to reentry. This concept is also highly applicable to the mechanisms of antiarrhythmic and proarrhythmic drugs.
Schematic of the reentry mechanism in cardiac tissue. Sites A and B may represent widely separated structures (e.g., the specialized AV conduction system and an accessory AV pathway, in the case of orthodromic AV reciprocating tachycardia), regions separated by normal anatomic obstacles to conduction (e.g., the tricuspid valve annulus, in the case of typical atrial flutter), or regions separated by acquired conduction obstacles (e.g., the atriotomy scar, in the case of postoperative intraatrial reentry tachycardia)
Reentry may occur within any conductive cardiac structure. When there is a single reentrant event (i.e., the wavefront extinguishes after a single revolution), the surface electrogram will register a single extrasystole involving those structures depolarized by the reentrant wavefront. Such a premature event is then called a reciprocating beat or echo beat. This may be indistinguishable from atrial or ventricular premature beats using other mechanisms of impulse formation.
Enhanced Automaticity
When the channel milieu results in spontaneous phase 4 depolarization in a sufficient volume of cells to enable depolarization of surrounding tissues and at a rate faster than the SAN mechanism, enhanced automaticity is said to be present. Although any diseased tissue is capable of such a rhythm, common examples include junctional tachycardia postcongenital heart surgery (emanating from the penetrating bundle or AVN), idiopathic atrial ectopic tachycardia, and ventricular tachycardia immediate postmyocardial infarction. Enhanced automaticity may also result from mechanical stretching and from hypokalemia, and it is enhanced by catecholamines. This mechanism is the second most common cause of pathological tachycardias. Due to their incessant nature, idiopathic automatic tachycardias which are sufficiently slow that they do not cause initial symptoms are notorious for eventually causing tachycardia-induced cardiomyopathy.
Triggered Activity
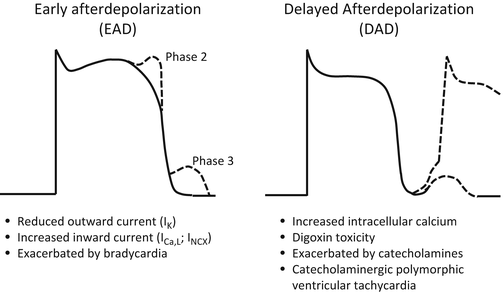
This term refers to early (EAD) or delayed afterdepolarizations (DAD) which result from very different action potential perturbations (Fig. 157.4). EADs result from action potential prolongation (phase 2 or 3 phenomenon) and are promoted by bradycardia, extracellular hypokalemia, and potassium channel blocking drugs. Mechanistically, EAD’s occur when there is reduced repolarization reserve due to limited outward potassium currents, and the countervailing depolarizing currents (such as L-type calcium current or sodium/calcium exchanger) are sufficiently strong to regenerate a full-action potential [4]. Some polymorphic ventricular tachycardias and torsades de pointes ventricular tachycardia are malignant arrhythmias caused by EADs. The pulmonary vein triggers for paroxysmal atrial fibrillation in adults likely also use this mechanism [5]. DADs result from excessive intracellular calcium loading during phase 4 of the action potential and are associated with digoxin toxicity and very serious genetic abnormalities of myocardial intracellular calcium trafficking, catecholaminergic polymorphic ventricular tachycardia (CPVT). In vulnerable patients, catecholamines contribute to DADs. Increased cytosolic calcium promotes DADs via the sodium/calcium exchanger. The hallmark tachycardia in digoxin toxicity and in CPVT is bidirectional ventricular tachycardia. In addition, less serious tachycardias thought to use triggered activity include some outflow tract monomorphic ventricular tachycardias and some focal atrial tachycardias.
Ventricular myocyte action potentials perturbated by after depolarizations (dashed lines). Illustrated on the left are early after depolarizations during phase 2 and phase 3 which do not result in fully regenerated action potentials. On the right are delayed afterdepolarizations, one of which results in a fully regenerated action potential
Other Mechanisms
Parasystole refers to an automatic rhythm which eminates from a protected focus; that is, it depolarizes adjacent tissue which has recovered excitability but cannot, itself, be depolarized or reset by neighboring wavefronts. This focus is said to demonstrate “entrance block” but not “exit block.” Although this phenomenon has been described in many cardiac tissues, ventricular premature beats caused by a ventricular parasystolic focus are best known. Classical parasytolic foci have a constant discharge rate, resulting in a rate of surface eletrocardiographic phenomena (e.g., wide complex QRS in the case of ventricular parasystole), which is a multiple of the underlying rate of discharge. Therefore, it is not associated with a regular coupling interval to normal electrical events from the same chamber (e.g., between the QRS of a sinus beat and the ventricular premature beat). Despite the presence of entrance block, electrotonic conduction from other ambient impulses may slightly delay the discharge rate of the parasystolic focus when that external influence occurs in the early portion of the parasystolic cycle and accelerate the discharge rate when it occurs in the latter portion, so-called modulated parasystole (Fig. 157.5). Some forms of the very common (and thought to be benign) automatic idioventricular rhythm (AIVR) may be due to a ventricular parasystolic focus, whose discharge rate is very similar to the ambient sinus rate.
A continuous rhythm strip illustrating “modulated parasystole.” Uniform premature ventricular contractions (PVCs) have a fundamental discharge cycle length of about 1,300 ms. In parasystole, due to entrance block but not exit block (meaning that normal tissue cannot reset the parasystolic focus), all inter-PVC intervals should be a multiple of 1,300 ms. In modulated parasystole, the inter-PVC intervals vary slightly from a multiple of the fundamental discharge cycle length likely due to electrotonic influences (i.e., spread of current without creation of action potential) by surrounding normal tissue. * illustrates that the coupling interval from the sinus QRS to PVCs is variable, typical of ventricular parasystole
Reflection is a potential form of reentry, in which a proximal area of tissue, usually electrically depressed, conducts to a distal area by slow electrotonic conduction, followed, in turn, by reactivation of the depressed region by normal depolarization (Fig. 157.6, left) [6]. Summation is a theoretical mechanism of improved conduction, wherein two wavefronts, each separately incapable of conduction through a depressed region, converge and successfully conduct across that zone (Fig. 157.6, right). Beyond the scope of this chapter, but worthy of mention, experimental evidence exists for the presence of relatively large and electrically stable spiral waves and rotors (Fig. 157.7) [7]. A kind of reentry in which involved tissue has a very short refractory period, these phenomena may be the source of some examples of atrial and ventricular fibrillations [7]. Depolarization of neighboring tissues which are repeatedly and irregularly terminated by wavebreaks due to their longer rectory periods results in the characteristic chaotic chamber electrograms.
“Reflection” has been demonstrated in ischemic canine Purkinje fibers. In this form of reentry, a spontaneous depolarization from partially depolarized ischemic tissue (a) conducts to healthy tissue by electrotonic influences (dotted arrow, b). The resulting action potential conducts back to the damaged tissue by normal cable conduction properties (c) after that tissue’s refractory period has expired. The stippled area represents ischemic myocardium (The top portion is reproduced with permission from Rosenthal et al [6]). “Summation” is a theoretical mechanism by which conduction over an electrically depressed region (cross-hatched in figure) may only occur secondary to convergence of wavefronts, each arising in a separate anatomic structure and each of which, separately, cannot conduct across the depressed tissue. This mechanism has been hypothesized to account for some examples of unidirectional conduction block. The double line (//) represents conduction block
Top: schematic example of a rotor, whose core has a very abbreviated action potential due to electrotonic effects, resulting in a very short wavelength (WL). The rotor’s peripheral spiral wave has a longer wavelength at its periphery (action potential having solid line at upper right) than at its inner curvature (more abbreviated action potential having dotted line at upper right). This results in functional reentry. Bottom: computer-generated rotor illustrating fibrillatory conduction due to wavebreaks. Wavebreaks, themselves, may result from anatomic obstacles, thus creating daughter spiral waves. Numbers represent time in ms (Both figures are reproduced with permission from Vaquero et al [7])
Supernormal conduction is said to exist when conduction occurs at a time when it is not expected to do so, that is, during the tissue’s refractory period. This phenomenon occurs when a wavefront encounters a tissue that is at the end of phase 3 of its repolarization and, therefore, nearing its activation threshold (from the opposite direction) (Fig. 157.8 top) [8]. A smaller than expected stimulus can elicit a depolarization at that time. This form of excitability has been demonstrated in the bundle branch-Purkinje fiber system, Bachmann’s bundle, and probably accessory AV connections. The gap phenomenon also represents improved conduction at a time when it does not seem like conduction should occur. It may be demonstrated in any portion of the heart beyond the sinoatrial node and occurs following wavefront delay in a structure (say, structure “A”) proximal to the tissue in question (say, structure “B”). That is, a less premature event delivered to structure “A” encounters “B” in its effective refractory period and cannot depolarize “B,” but a more premature event finds “A” in its relative refractory period, slowing the wavefront and allowing its presentation to a now recovered “B” (Fig. 157.8 bottom).
“Supernormal conduction” and “gap phenomenon” are two examples of improved conduction at times when conduction is expected to be worse. Top: an example of absent conduction through an accessory AV connection at sinus rate of 90 bpm, followed by alternating beats having pre-excitation once sinus rate increased to 95 bpm. This is explained at the top, right, with an idealized action potential from accessory pathway tissue. A faster wavefront (e) encounters the accessory pathway tissue closer to its activation threshold voltage (b) than a wavefront at a slower rate (d). Hence, a wavefront occurring during the supernormal period (c) allows depolarization of the accessory pathway tissue. (a) represents the resting membrane potential. (Top-right figure is reproduced with permission from Kinoshita et al [8].) Bottom: During electrophysiologic testing and single atrial extrastimulus (S2, resulting in P2) placement following a drivetrain of 8 beats at 600 ms (100 bpm) (S1-S1, resulting in P1-P1), a less prematurely delivered atrial beat (S1-S2 coupled to the last beat of drivetrain by 300 ms, resulting in P1-P2) does not propagate to the ventricles, whereas a more premature atrial beat (S1-S2 of 290 ms, resulting in P1-P2) does propagate to the ventricles (note QRS following P2 in right example but not in left example). In this example, the “gap phenomenon” occurs in the atria between the pacing site and the atrial tissue near the AV node. This is indicated by a longer P1-P2 (314 ms) following S1-S2 of 290 ms than the P1-P2 (303 ms) following S1-S2 of 300 ms. S stimulation artifact, // represents conduction block
Mechanisms of Bradyarrhythmia and of Impaired Conduction
Reduced Automaticity
Since the SAN is the natural cardiac pacemaker, reduced automaticity in this structure is most clinically relevant. Mechanistically, reduced automaticity results either from a reduced slope of phase 4 spontaneous depolarization or from a lower (less negative) activation threshold of the involved pacemaking tissue. Intrinsic channelopathic, inflammatory/infectious, mechanical (stretch), autonomic, pharmacologic, and metabolic causes may cause transient or permanent impairment of automaticity. In the case of the sinus node, sudden sinus pauses exceeding twice the prevailing sinus rate, or exaggerated sinus arrhythmia (in which there is slight sinus acceleration prior to any pause) should invoke consideration of sinoatrial exit block ahead of a defect in automaticity (see below).
Conduction Block
Although conduction block or delay may exist in any normally conductive cardiac tissue, the practical use of the term block is most commonly applied to structures of the specialized conduction system. However, the term delay may be applied to working myocardium. For example, when there is age-specific conduction delay in atrial depolarization, the surface ECG may or may not provide criteria for right or left atrial enlargement, and the intracardiac electrophysiologic study (EPS) may demonstrate specific regions of slow conduction in atrial muscle. Likewise, in the presence of age-specific QRS prolongation, if the ECG does not satisfy criteria for right or left bundle branch block, the term intra- or interventricular conduction delay applies. This is indicative of pharmacologic, fibrosis-related, hemodynamic, metabolic, or intrinsic channelopathic impairment of myocardial conduction. Irrespective of etiology, the mechanism of conduction delay or block may involve macrostructural fibrosis, impediment to cell-to-cell connectivity, functional molecular abnormality, or some combination thereof.
The concept of conduction block necessarily refers to cardiac structures which normally have a hierarchal sequence of conduction, that is, from a proximal to a distal structure. From the perspective of clinical relevance, the terms first-, second-, and third-degree conduction blocks are primarily applied to atrial-to-ventricular, or AV, conduction, although second-degree block may also be clinically applied to SAN-to-atrial muscle or sinoatrial conduction. First-degree block refers to delayed but persistent conduction from a proximal to a distal structure. Third-degree block implies complete absence of conduction between proximal and distal structures. Second-degree block can exist as “type I” and “type II.” The concept of second-degree block is abstractly illustrated at the top of Fig. 157.9. In that figure, the proximal structure (triangle) and distal structure (diamond) represent the SAN and atrial muscle (P wave), respectively, when considering sinoatrial block and the P wave and QRS, respectively, for AV block. For AV block, the precise structure exhibiting blocked conduction (i.e., AVN or His bundle-Purkinje system) may be determined during EPS, because a septal atrial electrogram (representing the proximal extent of the AVN) and a His bundle electrogram (representing the distal extent of the AVN and the His bundle proper) may be recorded. Because the SAN does not produce an easily recordable electronic signal, SAN conduction block must be determined by inference. Hence, first-degree SAN block cannot be diagnosed, and third-degree SAN block cannot be discriminated from impaired SAN automaticity. However, as illustrated in Fig. 157.9, middle, a rhythm strip which shows a shortening P-to-P interval prior to a pause suggests type I second-degree SAN block, and one that shows a pause equivalent to two prevailing P-to-P intervals suggest type II second-degree SAN block. Likewise, in the case of type I second-degree AV block, the progressive PR interval prolongs but relatively less so with subsequent beats (resulting in R-to-R interval shortening), prior to the nonconducted P wave, whereas, in type II second-degree AV block, the PR interval (and, therefore, R-to-R interval) is constant prior to the nonconducted P wave. Type I mostly occurs in the AV node, and it is not necessarily clinically important. Type II mostly occurs in the His-Purkinje system and is considered an unstable rhythm.
The phenomenon of “second-degree block” may exist in any cardiac tissue. The concepts of types I and II second-degree block are illustrated at the top, using a triangle as a surrogate for the proximal cardiac structure and a diamond as a surrogate for the distal cardiac structure. Numbers represent arbitrary conduction intervals between structures. See text for further explanation. Below: type I second-degree block in sinoatrial nodal (SAN) and AV nodal structures
Other Mechanisms
Concealed conduction refers to a limited depolarization within a portion of the specialized conduction system (or, theoretically, an accessory pathway) which then leaves a wake of relative or absolute refractoriness. The next wavefront either dies out or traverses that region more slowly than expected. This is a form of phase 3 block. Since the normal specialized conduction system does not provide an electrocardiographic signature per se, the only evidence for concealed conduction is poorer than expected conduction by the subsequent impulse, manifesting as PR interval prolongation, bundle branch block, or even a completely blocked P wave (Fig. 157.10) [9]. Phase 4 block (known as critical rate block) also manifests with poorer than expected conduction, usually within the bundle branches. These are structures which ordinarily maintain a stable phase 4 resting membrane potential. However, when diseased, they may spontaneously slowly depolarize. A normally occurring wavefront would then encounter a partially depolarized membrane, resulting in a phase 0 slope which is less steep (i.e., more slowly conducting) than had the normal wavefront encountered that membrane earlier in phase 4. Hence, bundle branch block would occur at a slower but not faster rate.
In top rhythm strip, example of “phase 3 block” in one and then the other bundle branch (*) or the AV node (†) following premature atrial contractions (note P waves altering previous T waves). In middle rhythm strip, there is “concealed conduction” in the AV conduction system. Premature ventricular contractions retrogradedly penetrate into the AV conduction system, making these structures partially depolarized (but not completely refractory); this results in reduced conduction velocity by the ensuing atrial wavefront and a longer than normal PR segment (*). This phenomenon is graphically depicted by a ladder diagram below the rhythm strip as lines having flatter slopes in the AV panel (†). The bottom rhythm strip shows sinus rhythm, sinus slowing, and a junctional escape rhythm. Because the junctional escape mechanism does not retrogradedly conduct to the atrium, the slower sinus P waves should eventually be capable of conducting to the ventricles as “sinus capture beats.” However, concealed retrograde conduction into portions of the AV junction that are proximal to the junctional escape focus (black dot in ladder diagram) renders that tissue entirely refractory (gray region in ladder diagram), an example of concealed conduction and phase 3 block. In this and all subsequent ladder diagrams, A atria, AV AV junctional structures, and V ventricles (Middle rhythm strip is reproduced with permission from Marriott & Conover [9])
Discriminating Supraventricular from Ventricular Tachycardia
Because this textbook includes separate chapters on the entities supraventricular tachycardia (SVT) and ventricular tachycardia (VT), this chapter will only provide diagnostic algorithms based upon the surface ECG and rhythm strip for discrimination of diagnoses within each entity. However, the ability to discriminate supraventricular from ventricular tachycardia is of paramount importance, due to the potential difference in hemodynamic consequences and to the differences in treatment; hence, this subject requires specific attention.
In the broadest sense, SVT refers to any nonsinus tachycardia that includes as a critical anatomic component of its substrate any structure between and inclusive of the atrial muscle and His bundle. Ventricular tachycardia, therefore, necessarily includes some portion of the bundle branches, Purkinje system, or ventricular myocardium, as its substrate. Normal pacemaking tissues (the sinus node and, potentially, the AVN) will always discharge unless they are depolarized by a faster rhythm. With the single possible exception of junctional ectopic tachycardia, SVT does indeed overdrive suppress the sinus node, but VT will only suppress the sinus and AV nodes if there is persistent retrograde (ventriculoatrial = VA) conduction from the VT substrate through the AV conduction system and into the atria. In the absence of VA conduction, sinus or junctional discharges during VT will occasionally penetrate the AV conduction system and depolarize a portion of or even the entire ventricular mass “between beats” of VT, resulting in what is referred to as “sinus capture beats” or “fusion beats” (Fig. 157.11). A relatively slow VT and/or rapid sinus rhythm improve the likelihood of this observation. This phenomenon strongly suggests the diagnosis of ventricular tachycardia (or junctional ectopic tachycardia). Frequent sinus capture or fusion beats can present a picture of a somewhat chaotic tachycardia. For completion’s sake, if the R-R interval varies and the QRS morphology varies from beat to beat, there are two other entities to consider: complex SVTs with variable bundle branch aberrancy or pre-excitation and nonsustained but frequently repetitive VT (or SVT with bundle branch aberrancy).
Ventricular tachycardia at a rate of about 200 bpm. There is a sinus capture beat in the middle of the tracing. Discrimination of sinus P waves from baseline artifact is difficult in this tracing, but variable morphology of ST segments and T waves, especially during the first three beats, strongly suggests absence of retrograde (ventricular-to-atrial) conduction
In the presence of a tachycardia with regular R-R interval and a QRS duration which is normal for age, SVT is the diagnosis, although VTs eminating from the ventricular septum may have a relatively short QRS duration. A nonsinus tachycardia having a prolonged QRS duration has its own differential diagnosis: VT, SVT with bundle branch aberrancy, and a pre-excited tachycardia. If a prior ECG during sinus rhythm is available from the patient, the presence of inherent bundle branch block (as may occur following congenital heart surgery) or pre-excitation (especially the Wolff-Parkinson-White pattern) provides the clinician a template of the patient’s baseline atrial-determined QRS morphology. That information notwithstanding, discriminating VT from SVT with bundle branch aberrancy is by far the most common dilemma. A 12-lead ECG during tachycardia with special attention to V1 is most helpful. Based upon nuances of the QRS morphology in either a basic right (RBBB) or left bundle branch blocklike (LBBB) pattern, the basic diagnosis can often be made (Fig. 157.12) [10, 11]. Pharmacological interventions may also be helpful. The use of a short-acting AV nodal blocking agent, such as adenosine, is diagnostic for a primary atrial tachyarrhythmia if it results in transient AV block but persistent of the atrial arrhythmia. Its ability to terminate a tachycardia suggests the presence of an AVN-dependent SVT, but some outflow tract VTs may also be terminated by these agents. Ultimately, intracardiac electrophysiological testing may be required. Algorithms such as the one in Fig. 157.12 are based upon adult data, and, unfortunately, analogous applications of electrocardiograms from infants and young children are not available. For example, a QRS duration of only 100 ms from a regular nonsinus tachycardia in a neonate would be considered ventricular tachycardia until proven otherwise.
Discrimination of supraventricular tachycardia (SVT) with bundle branch block from ventricular tachycardia (VT), based upon adult criteria. The intervals mentioned in this figure may not apply to infants and small children. †: This portion of figure is later referenced by Fig. 157.15 (“Diagnostic algorithm” is modified with permission from Brugada et al [10])
Regular Narrow Complex Tachycardias
These tachycardias are best analyzed from a rhythm strip or, preferably, from a multichannel ECG. If the R-R interval is irregular, a primary atrial tachyarrhythmia is assumed, especially atrial fibrillation or atrial flutter. Other entities such as junctional ectopic tachycardia with sinus capture beats, certain septal VTs with sinus capture beats, and non-reentrant AV nodal tachycardia rounds out the differential diagnosis. Comprising the vast majority of narrow complex tachycardias are those with a regular R-R interval, in which that interval only varies (often as alternating intervals) by less than 40 ms. Attention to the inter-R-R electrogram is then necessary. This interval is comprised of fusion of T waves and atrial depolarizations. Here, again, knowledge of the patient’s baseline ECG and T wave morphology may help inform that which is atrial. Likewise, the underlying ECG during sinus rhythm may provide clues about the SVT substrate, such as the delta wave of the Wolff-Parkinson-White pattern. The presence of two or more atrial depolarizations for every QRS nearly always makes the diagnosis of a primary atrial tachycardia. If there is a 1:1 QRS-to-P wave relationship, their temporal relationship becomes helpful. A “short R-P” interval (defined as QRS onset-to-onset of P wave being less than the P-to-next QRS) has a discrete differential diagnosis, as does a “long R-P” interval (defined conversely), though with significant overlap (Fig. 157.13). Tachycardias, which are incessant, show variations in rate according to autonomic nervous system milieu or show “warm-up” and “cooldown” behaviors most likely use enhanced automaticity as their mechanism. Nearly all others are paroxysmal, using either reentrant or, less commonly, triggered mechanisms. Following basic rhythm strip and multichannel ECG analysis and consideration of their spontaneous initiation and termination, pharmacologic maneuvers may be considered. A diagnostic algorithm of SVT subtypes within the broader context of all nonsinus tachycardias and considering some of the above principles appears as in Fig. 157.14. In many patients, intracardiac electrophysiological testing is required to make a definitive diagnosis.
Examples of short- and long-RP supraventricular tachycardia. The top tracing represents orthodromic AV reciprocating tachycardia from a 9-year-old male having a left lateral accessory pathway. The bottom tracing represents atypical variety of AV nodal reentrant tachycardia from an 18-year-old female
Diagnostic algorithm for diagnosing types of nonsinus tachycardias, specifically, narrow-complex tachycardias. aAVNRT atypical form of AV nodal reentrant tachycardia, AET atrial ectopic tachycardia, AFl atrial flutter, CAT chaotic atrial tachycardia, FAT focal atrial tachycardia, JET junctional ectopic tachycardia, OAVRT orthodromic form of AV reciprocating tachycardia, PJRT permanent form of junctional reciprocating tachycardia, tAVNRT typical form of AV nodal reentrant tachycardia, and *, ** these portions of figure are later referenced by Fig. 157.15
Regular Wide Complex Tachycardias
Discrimination of the three categories of wide complex tachycardia (VT, SVT with bundle branch aberrancy, and pre-excited tachycardias) is worthy of comment. Any form of SVT may exist in a patient coincidentally having pre-excitation and in which the accessory pathway alters the QRS but does not participate in the SVT mechanism. We say that the accessory pathway is an “innocent bystander.” The only pre-excited SVT which utilizes the accessory pathway as a necessary antegrade portion of the tachycardia mechanism is the antidromic form of atrioventricular reciprocating tachycardia (AVRT). Hence, most of the concepts described in the narrow complex tachycardia section apply to both SVT with bundle branch aberrancy and to pre-excited tachycardias. A diagnostic algorithm for wide complex tachycardias in children appears as in Fig. 157.15, with the same caveats as for Fig. 157.14.
Diagnostic algorithm for diagnosing types of nonsinus wide complex tachycardias. AET atrial ectopic tachycardia, AFl atrial flutter, ART antidromic reciprocating tachycardia, AVNRT AV nodal reentrant tachycardia, BBB bundle branch block, FAT focal atrial tachycardia, NSR normal sinus rhythm, PE pre-excitation, RVOT right ventricular outflow tract, VT ventricular tachycardia, † refers to portion of Fig. 157.12 also labeled with †, and * or ** refers to portions of Fig. 157.14 also labeled with * or **
Bradycardias
Sinoatrial Node Dysfunction
The synonymous terms “sinus node dysfunction,” “sinoatrial node dysfunction (SAND),” and “sick sinus syndrome” imply some combination of depressed SAN automaticity and sinoatrial conduction block. These terms are often used carelessly, depending upon the context: clinical signs and symptoms, rhythm strip observations, or observations in the electrophysiology laboratory. Most experts agree that the terms best apply when there is a combination of symptoms with electrocardiographic abnormalities. The term “tachy-brady syndrome” applies to the combination of SAND and paroxysmal atrial tachycardias, especially atrial flutter, which may occur long term following atrial surgery.
The symptoms associated with SAND in children relate to low cardiac output and may be paroxysmal and dramatic, such as syncope or presyncope or subtle and very nonspecific, such as persistent fatigue, nausea, irritability, daytime somnolence, behavior changes, declining school performance, and headaches. The electrocardiographic findings may be similarly nonspecific. These include persistent sinus bradycardia (with average heart rates < 2SD for age); excessive pauses (greater than twice the ambient sinus interval), especially in the presence of exaggerated sinus arrhythmia; wandering atrial pacemaker; and subsidiary escape rhythms, especially nonaccelerated junctional or low atrial rhythms (Fig. 157.16).
Rhythm strips from patients having sinoatrial node dysfunction following congenital heart surgery. The top strip shows sinus bradycardia and a sinus pause. The pause could be due to failure of sinoatrial node discharge (decreased automaticity) or to second-degree sinoatrial conduction block. The bottom strip is continuous and shows junctional bradycardia and nonsustained episodes of atrial flutter
Electrophysiologic features of sinoatrial node dysfunction may also be sought in the electrophysiology laboratory. Abnormally long sinus delays (relative to the ambient sinus rate) following >30-s periods of rapid atrial pacing, the so-called sinus node recovery time (SNRT), may indicate depressed sinus node automaticity [12]. It is even thought that the sinoatrial conduction time may be estimated by introducing progressively earlier single premature atrial events from the high right atrium into sinus rhythm (or a slow atrial-paced rhythm) and subtracting the prevailing sinus cycle length (or the slow-atrial-paced cycle length, S1-S1) from the – eventually stable – return cycle (S2-S3, with S2 representing the premature stimulus and S3 the subsequent recovery sinus node-produced electrogram) [13, 14]. These techniques require certain assumptions, and they suffer from poor positive predictive accuracy and reproducibility [15]. In the past, SNRT measurement during pharmacologic blockade of autonomic influences has been championed in children to help improve the value of this test [16]. Clinical application of these techniques has waned greatly in the last two decades. More recently, specialized filtering and frequency settings have permitted direct measurement of sinoatrial node depolarization [17], but this technique has also not been embraced by clinicians.
Sinoatrial node dysfunction is a condition of advancing age, and it is rare in infants, children, adolescents, and young adults except following congenital heart surgery. A list of associations in the young appears in Table 157.1 [18–26].
Atrioventricular Conduction System Block
First- and Second-Degree Atrioventricular Block
First-degree AV block is defined as a prolonged PR interval while in sinus rhythm. This interval normally prolongs with age. The PR interval, ordinarily defined as the electrocardiographic interval from the sinus P wave onset to the QRS onset, comprises the conduction time from the sinoatrial node transatrially to the AV node, the trans-AV nodal conduction time, and the conduction time through the His bundle, bundle branches, and Purkinje network. (A portion or the entirety of these structures may be bypassed by pathological accessory pathways, the subject of another chapter.) Hence, first-degree AV block may result from delay in any of these anatomic structures. Accordingly, the etiology and clinical significance of this common finding reflect the anatomic structure responsible for the delay. For example, first-degree AV block caused by right atrial volume overload due to an atrial septal defect does not predict progression to higher grades of AV block. However, the development of first-degree AV block, especially when combined with QRS axis change in a young person having a mitochondrial disease such as Kearns-Sayre syndrome, likely represents evolving HPS damage and is a harbinger of dangerous complete AV block. A nonexhaustive list of etiologies of all levels of AV block appears in Table 157.2. In the absence of congenital heart disease/surgery, acquired cardiac disease, metabolic or electrolyte disorder, acute infectious disease, neuromuscular disease, channelopathy, or drug/toxin effect, first-degree AV block in young people merely represents enhanced parasympathetic influences or is idiopathic and does not represent risk to the patient. It occurs in up to 12 % of ambulatory rhythm recordings from healthy teenagers [27] and in 0.65–1.1 % of random 12-lead ECGs in children [28]. Isolated first-degree AV block in young athletes is considered a normal variant, occurring in 23 % of ambulatory rhythm recordings from teenaged athletes [29]. Rarely, especially following surgery for congenital heart disease, very prolonged PR intervals result in ventricular contraction not yet being completed by the time of the next atrial contraction. Hence, atrial contraction against closed AV valves ensues, with possible symptoms of light-headedness, fatigue, and nausea, so-called pseudo-pacemaker syndrome [30].
Type I second-degree AV block usually results from blocked conduction in the AV conduction system, usually the AV node, and only requires therapy if clearly causing symptoms of dizziness, presyncope, or fatigue. This finding exists in up to 11 % of asymptomatic teenagers during sleep [27] and in up to 20 % of athletic teenagers [29], based upon ambulatory rhythm monitoring. Its presence during wakefulness is much less common and is probably worthy of long-term patient surveillance. Type II second-degree AV block usually represents infranodal AV conduction system disease and represents an unstable conduction system, but it too has been identified in apparently healthy young athletes [29]. It may be associated with bundle branch block. Knowledge of the underlying etiology or type of prior heart surgery also helps inform the anatomic level of block and attendant risk (Table 157.2). Treadmill exercise testing may be helpful in discriminating the anatomic level of second-degree AV block. As a rule, autonomic factors favor improved AV conduction at faster atrial rates when the disease is in the AV node and AV block worsens at faster atrial rates when the disease is infranodal.
Bundle Branch Block
Conduction abnormalities that manifest as perturbations in the QRS morphology and lengthening of the QRS duration represent abnormalities within the bundle branches, Purkinje fibers, and/or ventricular myocardium. In children, they are often components of an underlying condition, including many of those listed in Table 157.2. Progressive bundle branch block or nonspecific interventricular conduction delay is especially important, as it may represent disease progression to complete AV block (e.g., Kearns-Sayre syndrome). The coexistence of distal conduction system disease with other conditions appears in discussion of those underlying disorders. This section addresses isolated bundle branch disease.
Right bundle branch block (RBBB) is diagnosed by the electrocardiographic pattern of a dominant broad S wave in lead I (and often aVR) and R’ in lead V1. “Complete” RBBB requires that the QRS duration be sufficiently long for the patient’s age and that the conduction delay be concentrated in the terminal portions of the QRS. That is, if the QRS is uniformly prolonged, even with a dominant R versus S wave in V1, interventricular conduction delay with right ventricular hypertrophy is also possible. If the QRS duration is somewhat prolonged (but not having a z score of >2) and has a similar pattern as RBBB, “incomplete RBBB” (iRBBB) is diagnosed. Discriminating iRBBB from right ventricular hypertrophy in a youngster having a right ventricular volume overload condition may be impossible. These patterns are common in children, representing 2.9 % (iRBBB) and 0.16 % (RBBB) of healthy 6–17-year olds [31], with a female predominance. Incomplete RBBB having an rSr’ pattern in V1 is now considered a normal variant in physically conditioned teenagers [32].
Isolated familial complete RBBB (i.e., not coexisting with a cardiomyopathy) has been recognized for decades, but its clinical significance remains in dispute. If there is, in addition, left axis deviation of the initial 40 ms of the QRS (therefore, comprising one form of bifascicular block), progression to complete AV block has been reported in some series [33, 34] but not in others [35]. Even in the presence of a normal initial QRS axis, progression to AV block has been reported in some series [36, 37] but not in others [38]. It is reasonable to obtain ECGs in first-degree family members and grandparents, when isolated complete RBBB is first identified in a child. The role of long-term surveillance when the family history is negative and ECGs are normal is unknown.
Complete left bundle branch block (LBBB) is diagnosed when the QRS duration exceeds a z score of 2, and there is a pure S or rS in V1. This diagnosis may be confused with the Wolff-Parkinson-White pattern and a right free wall accessory pathway; the PR interval should always be carefully measured, as it will be very short in the presence of Wolff-Parkinson-White pattern. As an isolated finding, LBBB in a youngster is rare and always raises the concern of progressive conduction system disease, with or without cardiomyopathy. Affected youngsters require ambulatory rhythm monitoring and exercise testing in order to identify periods of AV block, especially at higher atrial rates. At minimum, long-term surveillance is required. LBBB may occur following left ventricular outflow tract surgery.
Congenital Complete Atrioventricular Block
Congenital complete atrioventricular block (CCAVB) occurs in 1 in 11,000 live births [39]. Approximately two-thirds of cases are considered immune mediated, related to transplacental passage of anti-ribonucleoprotein antibodies (anti-SSA, Ro (especially anti-Ro52 and anti-Ro60); or anti-SSB, La) from women who are ANA positive, though only a minority of these women have active systemic lupus erythematosus or Sjögren syndrome. These antibodies result in an immune-mediated fibroelastic destructive process starting at about 18 weeks of gestation and resulting in CAVB (>90 %) and/or SAND (10 %). The pathogenesis of CAVB (and, less commonly, SAND or endocardial fibroelastosis) is incompletely understood, although there are currently three active theories: [1] The calcium channel theory, in which cell surface L-type calcium channel proteins (Cav1.3) are targeted by maternal antibodies; [2] The apoptotic theory, in which the normally antibody-inaccessible ribonucleoproteins, Ro and La, are exteriorized during apoptosis, prompting an antibody-mediated inflammatory response with collateral damage to neighboring healthy myocytes; and [3] The serotoninergic theory, in which cross-reactivity between the 52 kD portion of the nuclear (and therefore unavailable) Ro antigen and cell surface 5-HT4 receptors, occurs. This causes reduction of L-type calcium channel proteins, because 5-HT4 receptor binding is important for L-type calcium channel activation. A combination of the first two theories is currently favored [40].
About 5 % of pregnancies in women having antibodies result in CCAVB, but after a first-affected infant, that incidence increases to about 18 % for subsequent pregnancies [39]. New data suggest that recurrences are more likely in older women and when the vulnerable portion of gestation (12–24 weeks) occurs during the months of January–March [41]. Affected newborns may also have transient rashes, hepatitis, or cytopenias, which may persist until about 6 months of age. The presence of isolated neonatal lupus rash is associated with a 6- to 10-fold increase risk of CCAVB in subsequent pregnancy [42]. Rarely, AV block does not occur until weeks to a few months postpartum.
Nonimmune CCAVB occurs with a higher than expected incidence in fetuses having certain structural congenital heart defects, especially congenitally corrected transposition and some forms of heterotaxy (particularly, left atrial isomerism, or “polysplenia”). Uncommon genetic etiologies, which may or may not have associated structural defects, include mutations in the Nkx2.5 transcription factor gene [43] or the Tbx5 transcription factor gene. When the latter is associated with Holt-Oram syndrome, sinoatrial node dysfunction may coexist or predominate [44].
CCAVB is a morbid condition, carrying a 20–30 % incidence of fetal or neonatal death. This risk is highest when there is associated SAND and endocardial fibroelastosis [45]. In the presence of hydrops fetalis, the mortality rate of immune-mediated CCAVB is 73–100 %. The diagnosis of congenital heart block is made during fetal ultrasound, and once identified, patients should be observed closely in utero for signs of heart failure and hydrops fetalis. Early delivery and immediate postbirth pacing may be indicated and weighed against the risks of prematurity. Among antibody-exposed fetuses, especially following a prior-affected infant, there are several ultrasound-guided methods of monitoring the mechanical AV interval. The goal is to identify progressive AV interval lengthening or development of second-degree AV block, in hopes of providing maternal therapy to prevent progression to CAVB. That said, there is still no conclusive proof that PR prolongation in these fetuses predicts progression to CAVB. Once CAVB is present, no therapies are effective. Several anecdotal series have championed the use of maternal steroids, plasmapheresis, and/or IVIG to prevent progression to CAVB and even reversal of second-degree AV block [46–49]. However, IVIG was shown not to be effective in a recent large experience [50], and the PRIDE study, in which dexamethasone was used in a randomized protocol, also failed to demonstrate efficacy [51]. For fetuses with CCAVB who have signs of hydrops or an excessively slow rate (<55 bpm) and in whom early delivery is felt to be highly undesirable, maternal administration of the beta-adrenergic agent, ritodrine, has been reported to be helpful [52].
Once an infant with heart failure is born, aggressive therapy is required for all other aggravating factors, including pleural and pericardial effusions, lung disease of prematurity, and coexisting structural heart defects. Duration of temporary transcutaneous pacing is limited by skin fragility, so placement of temporary transvenous or epicardial wires in the intensive care nursery may be necessary.
The rhythm strip from an affected patient demonstrates atrioventricular dissociation, usually with a normal sinus P wave rate (Fig. 157.17). However, in up to 10 % of infants having immune AV block, the sinus node will also be affected, resulting in sinus P wave bradycardia, as well. In the more common circumstance, the P wave rate is often coincidentally about twice that of the escape junctional pacemaker. This can result in the QRS having a relatively constant relationship with the preceding and following P waves, at least for brief periods of time. This can simulate second-degree AV block and 2:1 AV conduction. The true diagnosis will become evident after prolonged rhythm strip surveillance. Another interesting phenomenon is often observed in children having congenital AV block and periods of a relatively constant QRS and P wave relationship: The P-P interval bracketing the QRS is often slightly longer than the alternating P-P interval. Theories abound for this observation, including the mechanical effect of atrial stretch associated with right atrial contraction against a closed tricuspid valve and alterations in blood flow to the sinoatrial nodal artery.
Rhythm strip from a 6-year-old having congenital complete AV block. It illustrates AV dissociation, a faster P wave rate than QRS rate, and a regular R-R interval. The associated ladder diagram below illustrates blocked atrial impulses (symbol, //) in the upper portion of the AV node and an AV conduction system escape mechanism (symbol, •) from the more distal AV conduction system
Specific indications for permanent pacing in newborns and in children with congenital complete heart block are included in the 2008 guidelines for device-based therapy of cardiac rhythm abnormalities [53]. Even asymptomatic adults with CCAVB have a 5 % incidence of sudden death at long-term follow-up [54]. It has therefore become standard practice to permanently pace all such patients by their late teenage years. Among patients with congenital complete heart block who require pacing, perhaps up to 10 % will develop significant ventricular dysfunction [55]. Whether this is due to intrinsic muscle disease related to the initial immune-mediated process or whether this is purely due to dyssynchronous ventricular depolarization is unknown. Ventricular function benefits from ventricular resynchronization pacing in this patient group [56]. Lastly, an association between immune-mediated CCAVB, but not non-immune CCAVB, and aortic root dilatation has recently been discovered [57].
Interpreting the Rhythm Strip
Rhythm strip interpretation can be most daunting in the presence of irregular rhythms. By categorizing the pattern of irregularity, the clinician may then reduce the differential diagnosis to more manageable considerations. All available clinical information should be brought to bear when weighing the possibilities within each category. For example, when considering an infant having just undergone surgery for AV septal defect and who now has “group beating” and a normal P wave appearance and rate, second-degree AV block would move to the top of the list. Or, in a teenager who has Wolff-Parkinson-White pattern and narrow QRS complex “premature beats,” reciprocating beats related to the accessory pathway should come to mind. Based upon the classical textbook by Marriott and Conover, Advanced Concepts in Arrhythmias Second Edition [9], we have found certain sequential steps to be a good approach to complex arrhythmia interpretation. First, the clinician is advised to utilize as many leads as possible. This is critical for determining the origin of the atrial impulse, the type of bundle branch block, and the QRS axis and to identify events which may be isoelectric, and therefore not visible, in one lead or the other. Next, the QRS is identified, and even if the amplitude is very low, it is always followed by a T wave. One or the other is always visible. Third, the P wave should be sought. It may appear as only a distortion of the QRS, ST segment, or T wave. If available, the normal QRS, ST segment, and T wave will serve as an unaltered template. Finally, subtle changes in the rates of the P and QRS complexes should be measured, so that the perturbation of the rate of one can be related to that of the other; that is, depolarization of which chamber is dictating the rhythm? This provides mechanistic insight into the underlying arrhythmia. What follows is a summary of etiologies of various QRS arrhythmic patterns according to the arrhythmia phenotype, with some additional comments when appropriate. A “ladder diagram” is used to illustrate the anatomical electrical connections that account for some of these phenomena.
Etiologies of Premature QRS Complexes
Premature atrial complexes (PACs; often referred to as atrial premature beats, or APBs) result in early ventricular depolarizations only if the AV conduction system components have recovered from their refractory periods from the prior normal beat (Table 157.3). If not, a distortion of the prior T wave may be the only evidence that an atrial extrasystole has occurred. If only one or the other bundle branch has recovered from refractoriness, the resultant QRS will have a bundle branch block appearance. A rhythm strip showing both premature narrow and wide QRS complex beats should raise the suspicion of conducted PACs. Nonconducted PACs result in a QRS pause (see below) and may only be identified by distortion of the T wave corresponding the prior normal QRS. PACs are common in patients having an otherwise normal conduction system, especially in neonates, and usually do not require therapy. Premature junctional complexes (PJCs) are exceedingly rare, occur when there is abnormal automatic discharge from the AV node or His bundle, and are considered pathologic. Unapparent conducted PACs and low atrial PACs are sometimes miscategorized as PJCs. Premature ventricular complexes (PVCs; often referred to as ventricular premature beats, or VPBs) are also common normal variants and may eminate from any portion of the ventricular myocardium. The more septal their origin, the more narrow the QRS. PVCs are discriminated from PACs with bundle branch aberrancy, based upon the normal T wave associated with the prior sinus beat. If the PVC is available by full 12-lead ECG, the QRS morphology may also be useful (Fig. 157.12). When the PVC does not conduct retrogradedly through the specialized conduction system into the atria, sinus node discharges continue unabated. If the sinus discharge which occurs nearly contemporaneously with the PVC slows sufficiently in the AV conduction system, a propagated QRS may result. In that instance, the PVC is said to be interpolated. Otherwise, there is a post-PVC pause in the ventricular rhythm; the interval between the sinus-conducted QRS complexes which bracket the PVC would then be twice the ambient sinus rate, and the interval from the PVC to the next sinus conducted QRS is considered a “compensatory pause” (Fig. 157.18).
A 3-channel rhythm strip showing monomorphic ventricular trigeminy with its associated ladder diagram. The premature ventricular focus (symbol • in the ladder diagram) blocks retrogradedly in the AV conduction system (indicated by the symbol, //), a common characteristic of the human heart. Therefore, sinoatrial discharges continue uninterrupted but block in the distal AV conduction system, which is refractory (gray shaded regions), due to concealed conduction from the ventricular extrasystoles. This results in a compensatory pause, because the interval between conducted QRS complexes is twice the ambient sinus rate
“Capture beats” occur when there are competitive rhythms and on occasion they fail to suppress each other. For example, this is seen in patients having SAND, a predominantly slow junctional escape rhythm, the absence of retrograde conduction from the AVN up to the atrium, and an occasional sinus node discharge which enters the AVN prior to the next expected junctional depolarization. Similarly, changes in autonomic nervous system tone or other dynamic influences may cause sudden improvement in AV conduction such that 1:1 AV conduction briefly interrupts constant high-grade AV block. “Reciprocating beats” can be viewed as single beats of a reentrant SVT, classically occurring when a sinus node-driven QRS reenters the atria via conduction up an accessory AV connection, followed by normal AV conduction back to the ventricles (Fig. 157.19).
Examples of premature beats with associated ladder diagrams. The top rhythm strip shows primary junctional rhythm (the discharging focus is indicated by the symbol, •, in the ladder diagram), no evidence for retrograde conduction from the junction into the atria, and a brief period of a faster atrial rhythm. The fourth and fifth QRS complexes are premature and are sinus “capture beats,” which result from sinus P waves (*) conducting to the ventricles. The longer PR interval preceding the first of these two beats (and denoted by the dashed line in the ladder diagram) is due to slower antegrade conduction, because it is relatively refractory due to retrograde concealment from the prior junctional beat. // indicates conduction block. The bottom rhythm strip shows a single premature conducted P wave. The mechanism cannot be determined from this rhythm strip and, as indicated by the two ladder diagrams beneath it, could represent a true premature atrial contraction (top ladder diagram) or a reciprocating beat related to an accessory AV connection (bottom ladder diagram), among others
Etiologies of Pauses of the QRS Complex
Most entities in this category have been previously discussed. Nonconducted atrial bigeminy of the fetus and neonate probably represents the most common cause of sustained QRS bradycardia in young humans (Table 157.4). The only clue to this diagnosis in a brief rhythm strip may be the distorted T wave by the PACs. A longer period of surveillance will likely reveal either resumption of sinus rhythm without PACs or conducted PACs. Concealed junctional extrasystoles probably represent the most common manifestation of PJCs (see above). Using the mechanism of concealed conduction, as previously described, an early His bundle extrasystole may both find the distal conduction system refractory and leave its own wake of refractoriness; hence, it results in neither its own QRS nor AV conduction of the ensuing atrial depolarization (Fig. 157.20) [9]. This diagnosis is best made during intracardiac electrophysiologic testing.
In the differential diagnosis of QRS pauses, this rhythm strip illustrates the unusual diagnosis of “concealed junctional extrasystoles.” These discharges (indicated by the symbol, •, in the ladder diagram) most likely originate in the His bundle. Although they do not conduct antegradedly to the ventricles, they do leave a wake of refractoriness in the AV junction (indicated by the gray regions and representing another example of concealed conduction). When the sinoatrial impulse encounters the AV junction partially depolarized in its relatively refractory state (*), conduction slows, as indicated by PR interval prolongation (beats 1, 3, and 5). When the sinoatrial impulse encounters the AV junction in its absolute refractory period, there is no conduction, resulting in the QRS pause. If, as in this case, the junctional extrasystoles do not result in a depolarizing signal on the surface ECG, the diagnosis must be made by inference, unless intracardiac electrograms are available (Modified with permission from Marriott & Conover [9], p. 375)
Etiologies of Bigeminal QRS Complex Rhythm
A bigeminal rhythm implies a monotonous pattern of alternating QRS-to-QRS intervals (Table 157.5). Although the entities in this category overlap with “premature beats,” 3:2 conduction deserves further mention. Either second-degree sinoatrial or AV block in which conduction block occurs after every third depolarization of the proximal structure will give the appearance of bigeminy, because there will always be an alternating inter-R wave interval.
Etiologies of Group Beating of QRS Complexes
“Group beating” means that there are repetitive clusters of ventricular impulses separated by a beat or several beats of a normal or, at least, slower rhythm (Table 157.6). The only forms of SVT which may fall into this category are those in which the AV node is not a portion of the reentrant circuit, i.e., primary atrial tachycardias. Orthodromic AV reciprocating tachycardia and nearly all forms of AV nodal reentrant tachycardia have a 1:1 VA relationship and do not present with QRS group beating. The only exception is the permanent form of junctional reciprocating tachycardia (a form of orthodromic AVRT), in which the tachycardia may spontaneously terminate and restart (after brief sinus rhythm) incessantly.
Etiologies of Regular QRS Bradycardia
The practitioner should always be cognizant of the developmental changes in the sinus rate when considering the presence of bradycardia. The relevance of sinus bradycardia must take into account the clinical milieu, especially in older children and teenagers, when there is a high incidence of isolated heightened vagal tone. In addition to some of the manifestations of SAND (sinus bradycardia, junctional bradycardia, and regular type II second-degree sinoatrial block (which cannot be diagnosed from the surface rhythm strip)), this category includes persistent nonconducted atrial bigeminy and third-degree (complete) AV block.
Electrocardiography
Electrocardiography is the measurement and interpretation of voltages generated by the heart and recorded on the body surface. While clinical interpretation of the electrocardiogram may be based solely on the recognition of patterns across leads on the recorded page, this methodology may ultimately lead to a flawed diagnosis when the basic assumptions about the recording of a patient’s electrocardiogram are violated. Such can be the case in congenital heart disease, where anatomy and physiology vary vastly. Therefore, the interpretation of the electrocardiogram must be grounded in a basic understanding of its genesis.
Electrical Generator in a Volume Conductor
In the simplest form, the heart can be considered a battery within a bounded volume of electrically conductive fluid (the body). A battery in a conductive medium passes current from one pole to the other pole continuously, until exhausted, with the amount of current being determined by the resistance. The current is driven throughout the entire volume of the conductor. The direction and density of the current is determined by factors related to the uniformity of the conductive medium. The current density is highest close to the source and is less at farther points, such as the body surface. Nonuniformity of conductivity, the presence of nonconductive objects, or irregularities of the boundaries can all affect the path of the electric current. In the body, there are many influences on these current paths. These include the shape, position, and mass of the myocardium as well as the lungs, vessels, rib cage, musculature, and skin. The volume and location of blood, or fluid, within the thorax is also influential.
Body Surface Potentials
The myocardium generates current in complex patterns throughout the heterogeneous conductive structure of the body. If these patterns were visible on the skin, a unique and abstract line drawing would be present that would be a representation of the underlying system. A battery in the thorax would generate a static pattern that would remain unchanged as long as energy remained in the battery and there were no changes in the conductivity of the system, such as no breathing. However, the heart is not static. With each beat, an electrically active wavefront propagates throughout the myocardium. This wavefront acts as thin layer of electric bipoles with positive and negative sides. In fact, one can think of the activation wavefront as tiny batteries adjacent to each other in a curvilinear formation that moves through the myocardium in time. At an instant in time, the wavefront generates a particular pattern of current on the body surface. The pattern is determined by the position, shape, and density of the wavefront within the myocardium. As these change during the cardiac cycle, so does the body surface pattern. The purpose of electrocardiography is to record and reconstruct the body surface patterns throughout the cardiac cycle in order to make inferences about the characteristics of the electrical generator that produced them. For further detailed information regarding the generation of cardiac and body surface biopotentials, see reference [58].
Leads
The body surface patterns of electricity must be sampled extensively in order to characterize the underlying myocardium. However, instead of measuring the current flowing at each point, it is practical to measure the electric potential. The driving force for current flow is the difference in electrical potential between two points, better known as the voltage. Electrode pairs are placed on the skin surface in order to measure the voltage between two points. An electrode pair is a “lead.” The voltage recorded from a lead is one-dimensional. That is, without the knowledge of the positions of the electrodes, the measurement is only a value. However, in knowing the lead position on the body, two-dimensional information is obtained and more accurate inferences can be made regarding the source. With multiple leads, a three-dimensional picture can start to be constructed.
Yet, the cardiac cycle is not static. Therefore, the voltage from a lead must be recorded periodically over time at a sampling rate that is frequent enough to accurately measure and reproduce the continual changes in voltage. An electrogram is a tracing of how the voltage between two points on the body varies over time. Through the combination of spatial sampling by using multiple leads and temporal sampling by recording over time, a complete multidimensional representation of the cardiac cycle, as viewed from the body surface, is created.
Mapping the Cardiac Cycle
Since the inception of electrocardiography, there has been a quest for optimizing body surface measurements. The ultimate goal is to be able to fully infer the status of the cardiac electrical generator: its shape, function, position, and rhythm. The electrical potentials on the body, and within the body, are continuous. Therefore, there are an infinite number of electrode pairs that can be placed. From a mathematical standpoint, the equations that govern the flow of electrical current in time and space are known. Therefore, if the body shape and all of its contents and electrical characteristics were known, then a complete and accurate model of the myocardium could be recreated from measurements on the skin. This is known as the inverse solution – perhaps the Holy Grail of electrocardiography.
Body surface mapping has been performed using vests with hundreds of electrodes to measure as many sites as physically possible in order to create a three-dimensional rendition of the electrical potentials on the human torso [59]. Imagine a topographical map of a mountainous area showing elevations with peaks and valleys. A body surface map is an electrical “topo map.” Areas of negative or positive potential can be identified and tracked throughout the cardiac cycle. The time-dependent changes in the map can give diagnostic information. The increased number of lead sets and higher density of spatial sampling could potentially reveal more detailed information. However, both practical and clinical limitations are dominant and the standard approach is to use 12 leads.
Vectorcardiography
In vectorcardiography, changes in the body surface potentials are represented as a single vector centered in the chest in a three-dimensional coordinate system. The length of the vector represents the magnitude of the surface voltage. The direction and length of the vector changes with the cardiac cycle and the tip inscribes a loop during one cardiac cycle. The interpretation of the shape and direction of the loop in three dimensions is used to make diagnostic inferences. The benefit of the vectorcardiogram is that it incorporates both time and space to give a two-dimensional rendition of the cardiac cycle. In this manner, the activation wavefront in the myocardium is almost “visualized” as it propagates within the ventricles during the cardiac cycle. Alterations of the magnitude and direction of the vector loop can be used to identify abnormalities of conduction that could suggest the presence of cardiac structural abnormalities.
Standard Electrocardiogram
The mainstay of present day electrocardiography is the standard 12-lead electrocardiogram. The 12 leads are recorded using electrodes placed on each limb and across the chest in a reproducible pattern. The standardization is critical, since, from a practical standpoint, the interpreting physician is not typically performing the measurement. The interpreter is blind to the method of data collection and makes assumptions that the data are collected in the same manner each time. Correct electrode placement is critical in order to properly interpret the electrocardiogram.
For example, imagine that an object under frosted glass is photographed from multiple directions. You are handed a stack of pictures of the shadows on the glass created by the underlying object, and you are asked to draw the object in three-dimensions. Without knowledge of the direction from which the pictures were obtained, you would not be able to accurately perform the task. However, if you knew the positions of the camera, then you would have a chance. Furthermore, you would be able to perform the task repeatedly with different objects under the glass as long as the camera positions did not change with each instance.
Much like a camera lens having a field of view from which it gathers light, each set of electrodes has a lead field. A lead will be most sensitive to electrical events in the direction of its lead field. Therefore, to “reconstruct” the cardiac electrical cycle over time, multiple leads with different lead field directions are used. Lead sets are used in order to maximize recording sensitivity in two planes. In the frontal plane, lead fields most sensitive to measurement parallel to a coronal section of the body are used. In the horizontal plane, lead fields are used which are sensitive in a plane parallel to a transverse section.
For the frontal plane, the standard limb leads, labeled I, II, and III, (Fig. 157.21) are measured from the surface potentials recorded between electrodes placed on the distal extremities: lead I left arm(+)/right arm(-), lead II left leg (+)/right arm(-), lead III left arm(-)/left leg (+). A right-leg electrode is also placed and acts as a ground to reduce environmental electromagnetic noise. Note, there has been interest in moving the distal-limb electrodes to a proximal position on the torso. This is commonly employed in clinical settings with bedside monitoring or with ambulatory monitors. Although an electrocardiogram is obtained and may help with rhythm interpretation, these electrode positions are not standard and final diagnosis should always be made using the standardized electrode positions and lead sets.
Twelve ECG recording leads. The Einthoven’s triangle (shaded gray) and the hexaxial reference system depicting frontal plane ECG leads are shown in the top and middle panels. Direction of chest (precordial) lead axis with corresponding recording sites on the chest is shown at the bottom, with grounding to the Wilson Central Terminal (WCT). ICS intercostal space
By convention, a lead “points” in the positive direction. That is, if activation in the heart is propagating in the direction of the lead (i.e., the “positive” electrode), then the measured voltage will be positive as well. However, if activation proceeds in the exact opposite direction, just as much information will be obtained, albeit as a negative deflection of the recorded electrogram. Similarly, if two activation wavefronts are proceeding in opposite directions simultaneously, then there will be cancelation of voltages in the electrocardiogram, and the degree of positive or negative deflection will depend upon the dominance of voltage from one wavefront or the other. Lead I is sensitive along the horizontal axis in the frontal plane, pointing to the left side. Leads II and III add sensitivity along an axis tilted at 60° and 120° below the horizontal, respectively. To record from more directions in the frontal plane, the augmented leads, aVR, aVL, and aVF, are added. The lead fields for these leads are created using combinations of the standard limb leads. For example, aVF is measured between the left leg electrode and a combination of right-arm and left-arm electrodes. This combination yields a lead field which “points” nearly vertically and inferiorly. The leads aVL and aVR add recording sensitivity along an axis tilted at 30° and 150° above the horizontal, respectively. The six frontal leads (I, II, III, aVF, aVR, and aVL) provide lead fields with nearly 360° of sensitivity in the frontal plane. Of note, leads II, III, and aVF are called the inferior leads. Since the positive electrodes of these leads are positioned below the horizontal axis, the lead fields are particularly sensitive to activation in a superior to inferior, or top to bottom, direction. This directional information is valuable for determining the axis of activation and repolarization.
Measurements in the horizontal plane, orthogonal to the frontal plan, are accomplished using six leads created from precordial electrodes placed across the chest. Whereas the frontal lead fields are generated by measurements between physical electrodes, the horizontal lead fields are created by measuring between a single electrode on the skin surface and a reference point called the Wilson Central Terminal (WCT). The WCT is formed by connecting the right-arm, left-arm, and left-leg electrodes to each other via resistors. For the purpose of understanding the lead field directions, the WCT can be considered as an electrode centered in the heart in the thorax. Lead fields with differing directions of sensitivity are thereby created by measuring between an electrode on the chest surface and the WCT. The standard 12-lead electrocardiogram includes six positions for these electrodes on the chest, resulting in leads V1-V6.
The electrode placement for the precordial leads is standardized and specific with respect to landmarks on the thorax. The precordial electrodes are placed at the following positions: V1, 4th intercostal space at the right sternal border; V2, 4th intercostal space at the left sternal border; V3, the midpoint between electrodes V2 and V4; V4, 5th intercostal space aligned at the midclavicular line; V5, horizontally in line with V4 but at the anterior axillary line (or midway between V4 and V6); and V6, horizontally in line with V4 but at the midaxillary line.
Any deviation in placement of the electrodes (e.g., one interspace too high or too low) can result in significant changes of the signal and affect interpretation. This must be emphasized in training those who will be recording electrocardiograms. While hasty electrode placement and acquisition of signals may be desirable in a critical situation or with an uncooperative young child, attention to detail is critical since it is much more difficult for the interpreting individual to suspect abnormal precordial lead placement than inadvertent limb lead electrode reversal.
The lead fields for the precordial leads fan out in the horizontal plane. The lead field for V1 assumes more of an anterior and rightward direction. The remainder of the lead fields point to the left chest. In pediatric electrocardiography, additional precordial leads have been used with electrodes placed in mirror image positions on the right chest – such as lead V4r. Given the normal rotated position of the heart relative to the chest wall, the theoretical lead field axis for V4r, which points anterior and rightward, may deliver a better delineation of “right” and “left” cardiac electrical events compared to lead I, for example. In some institutions, lead V4r is added as a standard lead. Additionally, in dextrocardia, the right precordial leads may be used to record a “standard” set of the leads despite the abnormal cardiac position. In the presence of dextrocardia, some institutions have adopted variations of lead placement, including right-left mirror image placement of all leads (limb and precordial), right-left mirror image placement of the precordial leads only, or even sliding the precordial leads rightward (e.g., V1 placed in right fifth intercostal space in midaxillary line and V6 in left fourth intercostal space at left sternal border). These nonstandard arrangements may be confusing when viewed by clinicians unfamiliar with a particular institution’s conventions.
Signal Recording and Processing
Low-amplitude biopotential signals in the body are difficult to record. Careful signal acquisition techniques must be employed to obtain an adequate signal-to-noise ratio for electrocardiographic interpretation. Reduction of noise begins with proper electrical isolation of the patient. Attention should be given to ensure there is no contact with noise sources, such as other medical equipment. Artifacts that are introduced by other sources can appear as a periodic signal in the electrocardiogram baseline. These artifacts could easily be mistaken for signals generated by the patient and misinterpreted as an arrhythmia, such as atrial flutter or fibrillation, by the interpreting individual. If possible, heating or cooling blankets or other equipment near or attached to the patient should be turned off. Electric and magnetic fields, such as those created by electric lighting, are present throughout our environment. Electric fields create small differences of electric potential in space that could be detected when there is high electrode resistance and high amplification – such as in electrocardiography. In addition, magnetic fields can induce small, but detectable, electric current in lead wires. Consideration should be given to turning off overhead fluorescent lighting to reduce the field. In addition, the wires to individual electrodes attached to the body should be twisted together and bundled, if possible, to reduce magnetic and electric field-induced currents in the wires themselves. Noise control at the tissue-electrode interface is also essential. Electron transfer must occur between the skin, the electrolyte gel, and the Ag/AgCl metal electrode interface. Simple attention to cleaning the skin prior to electrode placement reduces electrical impedance at this interface and reduces noise. In addition, the electrodes must not overlap or have any electrical connection between electrodes on the skin surface – such as fluid or electrode gel. This may be especially difficult in small infants where infant-sized electrodes may not all fit on the chest surface. In this setting, it may be necessary to reduce the number of electrode sites on the chest wall (Fig. 157.22). The electrical shielding of lead wires and the grounding of equipment is paramount in the high-amplification environment of an electrocardiographic recording machine. The machines are manufactured with this noise protection in place. However, the ground for the machine is obtained through the wall socket power source. Yet, this ground may not be entirely adequate or “clean.” If there is substantial noise in the recordings, consideration should be given to plugging the machine into a different power source to obtain a different ground point.
Examples of electrocardiographic artifacts. Top: A rhythm strip generated during chest physiotherapy on an infant creates high-amplitude motion artifacts which simulate ventricular tachycardia. Narrow QRS complexes are seen marching through the artifact. Middle: A rhythm strip generated from a Holter’s magnetic tape illustrates drag of the recording medium, causing crowding of the signal and suggesting tachycardia. The nonphysiologic abbreviation of the T waves provides the clue that this is artifactual. Bottom: A 12-lead ECG from an infant in which merging contact gel from overlapping electrodes creates a nearly identical QRS complex among all leads
From a signal analysis standpoint, the electrocardiogram is complex and contains components having a variety of frequencies with varying periodicity. The challenge with signal processing of the electrocardiogram comes in being able to filter noise from the biological signal without removing clinically important wave frequencies. These range from the lower-frequency T wave to the higher-frequency QRS. Respiratory variation produces a low frequency baseline drift, generally slower (lower frequency) than that of the T wave. Electrical noise at higher frequencies can be present throughout the tracing. In the United States, the standard frequency for alternating current is 60 Hz. Unfortunately, this frequency falls in the range of useful frequencies obtained in the electrocardiogram. In addition to substantial noise that can alter the baseline, 60 Hz artifacts can alter the shape and amplitude of the QRS. Therefore, a combination of high-pass and low-pass filters in addition to “notch” filters (to remove specific frequencies such as 60 Hz) must be used to isolate the clinically useful frequencies from the recording. Filtering can be performed to make a very “clean” appearing signal. However, this may come at the expense of the fidelity of the cardiac waveform.
The electrocardiogram is classically presented on a printed page in a standard format with four columns and three leads per row in each column (4 × 3 format). The frontal leads are presented in the first two columns, and the precordial leads are presented in the last two columns. One or more rows of continuous tracings may be printed from left to right along the bottom of the paper as a rhythm strip. Tracings were originally only printed on thermal graph paper with gridlines having minor divisions every 1 mm and major divisions every 5 mm. At the standardized “paper speed” of 25 mm/s, the minor and major divisions represent 0.04 s (40 ms) and 0.2 s (200 ms), respectively. With 10 s of signal per page, each column in a 4 × 3 format presents 2.5 s of data. The amplitude of signals printed on the page is also standardized. At a “full standard” height, each 1 mm minor division (horizontal), represents 0.1 mV – or alternatively, as may be printed on the paper, 10 mm/mV. It is conventional for a rectangular wave to be printed at the edge of the printed page to act as a calibration mark. If the mark is a rectangle that is 10 mm in height (two major divisions), then full standard applies for the entire page. If the mark is a stair-step that is 10 mm initially, but “steps” down to 5 mm for the last half, then the first two columns (frontal leads) are at the full standard height, and the last two columns (precordial leads) are at a half-standard height of 5 mm/mV. Alternatively, the entire page may be presented at half standard. This is necessary when the lead voltages (especially the QRS) are so large that they overlap the tracings in a subjacent row. For proper interpretation, it is critical to recognize the format, paper speed, and amplitude calibration of the presented electrocardiogram. In the current age of paperless electronic recording and online interpretation, the presentation standards are preserved. However, at the user’s discretion, the format can be changed. This flexibility presents a distinct benefit given that leads can easily be rearranged on the page, for example, as a simultaneous 12-lead rhythm strip for improved interpretation and diagnosis of nonsustained arrhythmias.
International standards are established for the methodology of recording the electrocardiogram with respect to sampling rate, amplification, electrical filtering, and presentation of the information. A comprehensive review of the recommended standards for electrocardiography, and their scientific basis, are found in the 2007 consensus statement from the American College of Cardiology/American Heart Association/Heart Rhythm Society/and the International Society for Computerized Electrocardiology [60].
Signal-Averaged Electrocardiography (SAECG) and Microvolt T Wave Alternans
The acquired signals from the body surface contain more information than that which is presented in the standard 12-lead electrocardiogram. Extremely low-amplitude and high- or low-frequency signals that are generated by the myocardium are either filtered out of the final electrocardiogram or of such low amplitude that they are not readily apparent. The signal-averaged ECG (SAECG) and microvolt T wave alternans (mTWA) acquisition methods are aimed at detecting some of these component signals. SAECG focuses on depolarization with analysis of the QRS. mTWA focuses on repolarization with analysis of the T wave. With both methods, multiple QRST complexes are acquired during a stable, periodic rhythm and then analyzed with mathematical techniques that take advantage of the repetition of beats over time to detect the small amplitude signals. Without delving deeply into concepts of signal processing, a periodic signal can be thought of as a summation of sine waves of different frequencies and amplitudes. Through the Fourier transform, a time-based signal (such as an electrocardiogram) can be analyzed to determine the combination of sine waves that, if added together, would reconstruct the signal. The output is a transformation to a histogram of frequencies that make up the original time-based signal. The height of the histogram at a particular frequency represents the relative contribution of the sine wave at that particular frequency. With Fourier transformation to the frequency domain and with multibeat averaging in the time domain, extremely low-amplitude signals, in the microvolt range, can be detected.
SAECG is utilized to detect low-amplitude potentials that occur late during the QRS. These late potentials represent the terminal events of activation in the cardiac cycle and are ordinarily buried in the low-amplitude “noise” of a standard electrocardiogram. The presence of prolonged, low-amplitude potentials at the end of the QRS would suggest that late activation occurs in areas of diseased or scarred myocardium and would furthermore imply that an arrhythmogenic substrate may be present. In order to detect these late, high-frequency, low-amplitude signals, different recording techniques are employed than are used for standard electrocardiography, including different lead sets on the body surface and different signal filters. The acquisition is performed at rest with as much noise reduction as possible, including particular attention to skin preparation and room electrical noise. The output of the SAECG is a filtered QRS (fQRS) based on a composite of all recorded beats and a statistical determination of the amount of late activation present relative to the amplitude of the fQRS. Clinical criteria are used to declare the presence or absence of abnormal late potentials. These criteria include the duration of the fQRS (normal, <114 ms), the magnitude of signal in the last 40 ms of the fQRS (normal, >20uV), and the duration of the signal having magnitude less than 40 uV (normal, <38 ms). A late potential is thought to be present if one or more of those three measurements are abnormal. SAECG testing is relevant in pediatrics, particularly as a minor criterion for the diagnosis of arrhythmogenic right ventricular dysplasia/cardiomyopathy [61].
T wave alternans (TWA) is present when the amplitude and/or duration of the T wave oscillates on a beat-to-beat basis. Visible TWA is seen with severe abnormalities of repolarization, such as in long QT syndrome (LQTS) or severe electrolyte disturbances. Invisible TWA at the microvolt level (mTWA) may also be present and represent electrical instability. These tiny beat-wise changes may be detected with specialized recording techniques, as with SAECG. As with SAECG, specific body surface leads and lead sets are used. Over 100 beats are acquired at stable heart rates. Fourier transformation and frequency analysis are used to detect the minute oscillations of the T wave. Since the criteria for abnormal mTWA includes its development after reaching a particular threshold heart rate, signal acquisition is performed during gradual exercise testing using a treadmill or stationary cycle. The presence of mTWA above a particular amplitude, lasting for a particular duration and occurring at a low heart rate, is an indicator of repolarization instability in adults. The utility of mTWA in the pediatric population is undetermined.
Ambulatory Monitoring
Ambulatory monitoring is invaluable in the diagnosis of arrhythmias in pediatric patients. It is far more common for rhythm disturbances to occur sporadically than continuously. Common presenting symptoms of palpitations, “my heart is beeping” or “my heart hurts” in younger children, are unlikely to be occurring at the time of the office visit. Therefore, while the 12-lead electrocardiogram has the benefit of interrogating electrical activity in the myocardium from multiple vantage points, the recording period is limited. By sacrificing the advantage of many leads for prolonged recording time, ambulatory monitoring provides an opportunity to capture an arrhythmia “in the wild.”
Ambulatory monitoring can be categorized by type. Typically this division is between continuous and event monitors. In nearly all circumstances, monitoring is performed noninvasively from the body surface. However, specialized long-term monitoring, in the form of an implantable loop recorder may be necessary [62]. Technological advances continue to blur the distinction between continuous and event monitors, simply because there are fewer electrical and mechanical limitations to recording and storing electrocardiographic data over long periods of time. A critical component, unique to event monitoring, is the ability to “call in” or transmit data for review and interpretation of the electrocardiogram in the immediate aftermath of a symptomatic event.
Continuous (Holter) Monitoring
The Holter monitor is an externally worn device for continuous recording of electrocardiograms from, typically, 1–3 body surface leads. Holter monitor recording has the benefit of continuous recording and storage of all electrocardiogram tracings without user input. The clinical indications for monitoring of this type are numerous and supplying an exhaustive list of clinical scenarios is not practical. Common uses in the outpatient pediatric cardiology setting include: quantitative assessment of atrial or ventricular ectopy, rhythm surveillance in patients with daily or more frequent symptoms, rhythm surveillance for conduction defects or ectopy in asymptomatic patients with congenital heart disease, and rhythm surveillance for pacing or sensing abnormalities in patients with pacemakers. Other uses take advantage of the modern age of sophisticated quantitative software analysis of the electrocardiogram. These include beat-wise QT interval analysis, heart rate variability, and beat-wise ST segment analysis.
Recording electrodes are adhered to the skin of the chest. As with the standard ECG, attention to detail regarding skin preparation and electrode adhesion is important for success. This is especially the case if the patient will be physically active while being monitored. Critical information may be missed if one or more electrodes become dislodged during the recording period. Typically, five electrodes are used: right and left “arms,” right and left “legs,” and a single precordial position. However, for practical purposes of patient comfort, the arm and leg positions are in a “proximal” position where all electrodes are placed on the torso. This allows lead wires to be worn completely under clothing – important for compliance in the adolescent concerned about appearance and in the young child. Since interpretation of the recordings is focused on the rhythm, conforming to the electrode position standards of the 12-lead ECG is not critical. Despite the thoracic location of all of the electrodes, lead field differences are still satisfactory.
Historically, Holter monitors were battery-powered devices slightly larger than a paperback book, and they had a shoulder strap for wearing, much like a purse or satchel. The recorded data from the electrodes were stored on an analog magnetic cassette tape. In these devices, at the end of the recording period, the tape was removed from the device and “played” back to obtain the recorded signals. Analog to digital conversion was performed at the time of playback. Computer software was then used to analyze the recordings. Holter monitoring in the current age has benefitted greatly from solid-state miniaturized electronics. Current monitors are a fraction of the size of prior devices and can be worn clipped to a belt or even worn as a necklace. The device is silent, and there are no moving parts. The electronic circuitry now allows for direct digital sampling of the signals with high fidelity. The recordings are stored digitally on “flash” memory chips or inserted cards. While the most common Holter recording period is 24 h, perhaps dictated historically by electromechanical limitations, some of the newest devices allow continuous recordings for up to 14 days or more. At the end of the recording period, data from the memory card can be uploaded to a computer for analysis either using local software or by having the data sent remotely to the monitoring company via the internet.
Holter monitors provide a wealth of information. Automated analysis is performed for the entire recording period. Typical summary data include heart rate maximum, minimum, and average, in addition to histograms of heart rate and RR intervals. Following automatic creation of the individual’s normal QRS template, detection of premature beats and discrimination of supraventricular versus ventricular beats is performed. A complete tabular and graphical summary of ectopic beats, couplets, and runs is provided as a function of time of day. This is critical for determining diurnal variation of arrhythmias or other influences on ectopy frequency, such as activity. Other data are also commonly available, such as heart rate variability analysis or QT interval measurement. Although less commonly relevant to pediatric populations, beat-wise ST analysis may also be performed. Following computerized data analysis, manual over-reading by a technician is then performed. The technician manually scans the data for rhythm disturbances and flags sections of data for further review by the clinician. This is especially important when a patient has maintained a diary of symptoms during the recording period. These periods of the recorded data can be evaluated closely for findings that may correlate with the patient’s symptoms. Finally, at the clinician user level, “full disclosure” can be requested and the entirety of the recorded sample can be visually scanned for abnormalities.
Event Monitoring
There are two types of event monitors, loop and handheld. Loop monitors are similar to their Holter counterpart in that body surface recording is performed for a prolonged period. However, loop monitors are generally worn for up to 1 month as opposed to 24 h. Loop monitors utilize continual recording and storage of signals in a limited amount of memory. When the memory space is filled with data, then signals are saved to the beginning of the memory and overwrite the earliest recordings. In this manner, a “loop” is made, with only the most recent information being available. The continuous looping of the recording allows essentially endless monitoring periods, only limited by battery life.
The main value of these monitors is based upon the ability to save an event. If a patient experiences a symptom, then a button can be pressed on the monitor to signify an “event.” When an event is signaled, the recorder stores a timed segment of the data in memory outside of the “loop.” A period of time preceding the button press and a period after the press are stored. This allows the possibility of capturing a short-lived rhythm change that ended prior to the physical button push. Automation within the monitoring device also exists and can allow for auto-triggered event capture based upon predetermined rate and rhythm criteria. The utility of auto-triggered event capture in the pediatric population must take into account the fact that an active child’s sinus tachycardia can easily exceed preset rates that would trigger an event capture for an adult. Once event data are stored, these data must then be “uploaded” or transmitted to a receiving facility for evaluation. For many monitors, this is accomplished via transduction of the stored data to an audible signal. The audio signal is then transmitted to the receiving company simply by calling in, holding the monitor to the phone, and pressing a button for playback. At the receiving end, the audio signal is recorded and converted to an electrical signal for analysis and presentation as an electrocardiographic tracing. Newer monitors perform this task using cellular transmitters within the device; they automatically transmit the data to the receiving company immediately after an event has been signaled. Typically, the data from an event are reviewed by company technicians, and then, based upon established criteria that stratify an urgent versus nonurgent event, the ordering clinician is notified and can review the electrocardiographic recording.
Handheld event monitors are a type of ambulatory monitor that is not worn continually. The monitor is generally a thin, small device, approximately the size of a cellular phone, with two electrode contacts on the back of the casing. If an event is occurring and ongoing, the user places the monitor against the skin somewhere on the chest and then presses an event button on the device. The monitor records the electrocardiogram measured between the two external electrodes. Depending on the storage capabilities of the device, a number of event recordings can be saved. Then, as with the loop monitor, the data are uploaded via the telephone to the receiving company.
The decision regarding which type of monitor to recommend for a patient is not always straightforward. A short list of benefits, drawbacks, and general indications are given in Table 157.7 for each type of monitor. Holter monitors have a clear benefit of recording continually from multiple leads. Therefore, there is no dependence on the patient to “capture” an event, except to document symptoms if they occur. Holter monitors can be used for all ages, including infants. Event monitors require user input, and, as such, a decision must be made as to whether a child is mature enough to perform the task. For school-age children who are willing and capable, a loop monitor may be preferable, given that it is worn at all times and will not likely get lost or damaged. For children and teens who are self-conscious about a continuously attached “piece of medical equipment,” a handheld device may be preferable. Nonetheless, the decision is also determined by the suspected cause of symptoms. If the patient is only experiencing symptoms for less than 30 s, then the likelihood of successfully capturing the event using a handheld device is low.
In general, the use of implantable loop recorders is limited, due to the need for surgical implantation and ultimate explantation. However, in the case of rare events with severe symptoms, such as syncope with concern for an arrhythmia mechanism in patients in whom it is impractical to record an event using other noninvasive means, an implantable loop recorder may be needed.
Exercise Testing
The exercise “stress” test is an important tool for the pediatric cardiologist. Testing may be useful in patients who present with symptoms that are only elicited during exertion, such as chest pain, light-headedness, or palpitations; all of which may be related to cardiac arrhythmias. However, exercise testing has many applications beyond the cardiac conduction system: patients having hypertrophic cardiomyopathy to determine if left ventricular outflow obstruction worsens or if the blood pressure response is normal, patients having exertional chest pain to determine the presence of exercise-induced reactive airway disease (requiring pre-/postexercise pulmonary function testing), and a general assessment of cardiopulmonary-neuromuscular function in patients with congenital heart disease or cardiomyopathy. In the latter example, full metabolic exercise testing is performed. This combines standard exercise testing with continuous measurement of respiratory gas exchange. The metabolic exercise test is a powerful tool for helping determine if symptoms are due to cardiac, pulmonary, or neuromuscular limitations or due to deconditioning. A complete description of exercise testing in children appears elsewhere in this textbook.
The remaining comments in this section will be directed toward the use of exercise testing for suspected or known cardiac arrhythmias or conduction abnormalities. In the presence of atrial or ventricular ectopic beats, exercise testing may be indicated for determining if increased levels of endogenous catecholamines exacerbate the arrhythmia. This may indicate the presence of a channelopathy, such as CPVT or certain forms of long QT syndrome. Exercise testing may be useful for sudden death risk stratification in asymptomatic patients with ventricular pre-excitation (Wolff-Parkinson-White syndrome [63]). A list of arrhythmias or conduction abnormalities for which exercise testing in children is considered valuable appears in Table 157.8.
The standard exercise test is performed in a clinic or hospital setting with resuscitation equipment available using a motorized treadmill or stationary cycle ergometer. At minimum, 12-lead electrocardiograms, pulse oximetry, and automated noninvasive blood pressure data are measured. The patient is asked to wear comfortable athletic clothing. Electrocardiographic leads are attached after the skin is prepared to gain maximal adhesion and decrease the chance of electrode displacement during exercise due to perspiration. Typically, baseline measurements of blood pressure, heart rate, and ECG are recorded at rest in the supine and standing positions. Exercise is then begun in a graded fashion. The machine is typically programmed to perform a standard protocol where, for a treadmill, the rate and angle of incline are increased or, for a cycle ergometer, the load is increased, in a stepwise fashion after a specified amount of time. Coincident with these changes in loading conditions for the patient, 12-lead electrocardiograms are recorded as well as other vital signs including heart rate and blood pressure. Multiple protocols exist, including the Bruce or Balke protocols for treadmill and the James, McMaster, and Strong protocols for cycle ergometer [64]. The standard or a modified form of the Bruce protocol is commonly used in the pediatric cardiac population. For example, in a modified Bruce protocol, there are seven incremental stages, starting with a slow, walking rate and zero incline in stage one. The stages are changed every 3 min until an end point is reached: The patient reaches a goal heart rate (typically over 80 % of maximum predicted rate based on age), reproduction of symptoms, and occurrence of concerning changes in the electrocardiogram or blood pressure or the patient becomes too fatigued and cannot proceed. In the recovery stage, monitoring is continued, while the patient rests and recovers to baseline. While some arrhythmias may be induced during the initial or peak phases of exercise, others may appear during recovery. Therefore, ongoing observation is important during this stage.
Transesophageal Electrophysiology Testing
An esophageal, or transesophageal, electrophysiology study is a useful diagnostic test when noninvasive electrocardiography or ambulatory monitoring is not adequate for diagnostic purposes. An esophageal EP study is less invasive than an intracardiac catheter EP study. Among practitioners who use this modality, indications for esophageal EP testing include [1] in patients having recurrent symptoms suggestive of paroxysmal supraventricular tachycardia that occur too infrequently for practical ambulatory monitoring; [2] in patients having recurrent symptoms suggestive of paroxysmal supraventricular tachycardia and who are not able to successfully use an event recorder; [3] in infants having known supraventricular tachycardia in order to prove antiarrhythmic drug efficacy; [4] for risk assessment in asymptomatic patients with Wolff-Parkinson-White syndrome, in whom exercise testing and/or Holter monitoring show persistent pre-excitation [63], [5] therapeutically, for entrainment and termination of atrial flutter and its subtypes in newborns and in older children following congenital heart surgery; and [6] in currently asymptomatic toddlers who had had SVT as an infant. In the latter example, esophageal testing would be performed with the patient off medications to determine inducibility of SVT and the need for further treatment. The esophageal electrophysiology study is not useful for induction of ventricular tachycardia, since stimulation is supraventricular. The lone exception is fascicular left ventricular tachycardia, in which atrial pacing alone may induce the arrhythmia.
Esophageal electrophysiology studies are primarily performed in a cardiac catheterization laboratory setting. This is for both safety and practical reasons, given that sedation is typically necessary, there is a potential need for resuscitation, and electophysiologic recording equipment is present. To perform the study, intravenous sedation is given. Medications for this purpose include propofol, fentanyl, midazolam, ketamine, or some combination. If ketamine is selected, the addition of glycopyrrolate will reduce the associated increase in airway secretions. Once the patient is moderately sedated and electrocardiographic monitoring is underway, a 10-French bipolar esophageal catheter is lubricated with lidocaine jelly and is passed from the nares to the esophagus. A 5-French catheter is available for use in infants. The neck should be sharply flexed in order to avoid passage to the larynx. Ideally, the older child should be coached to swallow the catheter down, once they feel it in their hypopharynx. As the catheter is passed, the electrocardiogram recorded from the esophageal catheter is monitored. Typically, given the position of the esophagus posterior to the left atrium, an atrial and a ventricular electrocardiogram are visualized. Brief fluoroscopy may be helpful to verify position but is not always necessary. The catheter electrodes are then connected to an electrophysiologic stimulator. The stimulator must be capable of delivering at least 20 mA of current at a pulse width of 10 ms, since capture of the atrial myocardium from the esophagus requires high current output. This is partly due to the requirement of passing current through the esophageal wall and across a distance to the left atrium. The electrodes on an esophageal pacing catheter should be much larger than those on an intracardiac electrode catheter. Larger electrodes allow the delivered pacing current to be dispersed, thus, reducing the current density. This avoids potential esophageal damage, reduces capture of esophageal smooth muscle, and reduces discomfort.
Pacing is first performed during sinus rhythm to establish the output current necessary to capture and activate the left atrium. Subsequently, single, double, and triple atrial premature beats can be delivered during sinus rhythm to attempt arrhythmia induction. We prefer this strategy to extra-stimulation following drivetrains, in order to limit pacing and reduce patient discomfort. However, rapid atrial pacing can also be performed. In the case of WPW, atrial fibrillation can be induced for risk stratification purposes. Once atrial fibrillation is induced, the rhythm is recorded continually, and the patient is closely monitored for deterioration to ventricular fibrillation. The shortest R-R interval between consecutively pre-excited QRS complexes during atrial fibrillation is measured and is used to determine risk of sudden death. If supraventricular tachycardia is induced during testing, the relationship of the atrial and ventricular electrograms from the esophageal catheter provide helpful diagnostic clues as to the mechanism of the arrhythmia. Diagnostic information is also obtained when the tachycardia terminates – with or without intervention with intravenous adenosine or with atrial burst pacing. If no arrhythmias are induced with the initial round of pacing, isoproterenol, followed by isoproterenol plus atropine, can be infused and the testing repeated. Typically, if no arrhythmias are induced under these conditions, the study is considered negative and terminated. Sedation is discontinued and after recovery, the patient is discharged, within 2 h of completion of the procedure. This type of procedure is well tolerated in all age groups.
Experts believe that esophageal electrophysiology testing is thought to have high positive and negative predictive values for supraventricular tachycardia, although there is no rigorous proof of this belief.
Intracardiac Electrophysiology Testing
The intracardiac catheter electrophysiology (EP) study is an invasive diagnostic and potentially therapeutic procedure when combined with catheter ablation. Consensus and nonconsensus indications for this procedure in children appear in Table 157.9. To summarize this exhaustive list, the most common indications in children with structurally normal hearts include [1] exertional syncope, [2] nonsustained or sustained wide complex tachycardias, [3] symptomatic Wolff-Parkinson-White syndrome, [4] asymptomatic WPW when prior tests suggest that the accessory pathway may confer a high risk of sudden death, and [5] persistently symptomatic children (having palpitations) when other noninvasive diagnostic methods fail to document arrhythmia. In the case of supraventricular or ventricular tachycardia, indications for catheter-based EP study when combined with possible ablation are discussed in a separate chapter dedicated to ablative therapies in children. In patients with congenital heart disease, the threshold for intracardiac EP study is lowered. Patients with repaired or palliated congenital heart disease with unexplained syncope usually warrant electrophysiologic study. In addition, strong consideration of study should be given to patients with single ventricle physiology and who have a history of supraventricular or atrial tachycardia prior to their final staged repair, because catheter access to the heart will be severely limited following Fontan-style operations. Similarly, patients with Ebstein’s anomaly of the tricuspid valve should be considered for electrophysiology study prior to valvular operations, given the high incidence of atrioventricular accessory pathways in this form of congenital heart disease.
Catheter EP studies are performed in the cardiac catheterization laboratory with availability of fluoroscopy, resuscitation equipment, a multichannel electrophysiology recording system, an electrophysiology stimulator, and, in the current age, a nonfluoroscopic catheter tracking system. The planning of each case considers the child’s size, type of arrhythmia (if known), coexisting structural heart disease, prior cardiac surgery, potential limitations of vascular access, current cardiac function, and other comorbidities. Antiarrhythmic drugs are generally stopped at least five half-lives prior to testing. Although procedures may be performed under moderate sedation and local anesthesia (with bupivacaine/procaine combination), there has been a trend toward the use of general anesthesia, especially if ablative therapy is being contemplated. The electrophysiological effects of anesthetic agents have been well described, and contemporary pediatric cardiac anesthesiologists provide superb sedation/anesthesia with minimal perturbation of electrophysiologic phenomena.
Multiple electrode catheter placement is required for electrogram recording and cardiac pacing. As in hemodynamic cardiac catheterizations, the femoral vessels are the preferred access sites. Femoral venous capacity is thought to accommodate up to a total of 5 Fr in infants weighing <2 kg, 6 Fr if 2–3 kg, 7 Fr if 3–5 kg, 9 Fr if 5–10 kg, 11 Fr if 10–25 kg, and 14 Fr if >25 kg. Currently, decapolar electrode catheters down to only 4 Fr diameter are available. In small children or those otherwise having limited vascular access, useful data can be obtained by creative combinations of electrogram acquisition, including the esophagus, trans-hepatic access, internal jugular vein, and subclavian vein. For the typical youngster undergoing basic intracardiac EP study, the methodology is similar across institutions with minor variations based on practice preference. Multipolar catheters are advanced within the venous system and placed at multiple sites within the heart for the purpose of recording atrial, His bundle, and ventricular activations simultaneously. Typically, a quadripolar electrode catheter is placed in contact with the endocardium along the superior and lateral portion of the right atrium near the sinus node. A second quadripolar catheter is placed along the midportion of the atrial septum spanning the tricuspid valve annulus, at the location of the tricuspid valve septal commissure, in order to record a His bundle electrogram. Given the position of this catheter, atrial, His bundle, and ventricular electrograms are recorded from this channel (Figs. 157.23 and 157.24). A third quadripolar catheter is placed in the cavity of the right ventricle. These catheters record signals from the right heart. However, in order to obtain left-sided signals, a multipole (usually, decapolar) catheter can be inserted in the coronary sinus via the coronary sinus ostium. By spanning the length of the coronary sinus and much of the great cardiac vein at the level of the atrioventricular groove, the bipole pairs of electrodes on this catheter record both left atrial and left ventricular electrograms. These electrograms are important for determining arrhythmia mechanism as well as for the diagnosis of left-sided accessory pathways (Figs. 157.25–157.27).
Body surface and intracardiac tracings during sinus rhythm. Catheter labels at the left side of the image: HRA (high right atrium), HIS (His bundle location at mid septum), and CS (coronary sinus, electrode 5 is proximal at ostium, electrode 1 is distal at lateral left atrial margin). This demonstrates a normal right to left and superior to inferior atrial (A) activation sequence. Right atrial conduction time (PA interval), AV nodal conduction time (AH interval), and His-Purkinje system conduction time (HV interval) are normal
Body surface and intracardiac tracings during supraventricular tachycardia, specifically orthodromic atrioventricular reciprocating tachycardia (ORT). The QRS is normal, without pre-excitation. The HV interval is normal. Earliest atrial activation is located at the CS3 electrode site. The VA interval (or RP interval) is shorter than the AV (or PR) interval, demonstrating a short RP tachycardia
Simultaneous recording and display of the catheter signals allows for precise measurement of timing at each site as well as “visualization” of activation as it proceeds past each recording site. The surface electrocardiogram is also recorded and displayed. Key timing intervals are measured, including the PA interval (conduction time from the sinus node to the AV node), the AH interval (conduction time within the AV node), and the HV interval (conduction time from the beginning of the His bundle through the Purkinje network). Programmed stimulation is performed to assess electrophysiologic characteristics of the atrial myocardium, the AV node, the His bundle/bundle branches/Purkinje network, the right ventricular myocardium, and, if present, accessory pathways. The chamber of interest is paced at a constant rate for approximately 8–10 beats. This sequence is then followed at a specific interval by a single premature paced beat. This sequence is repeated with the premature beat being delivered progressively earlier until the site no longer responds. This technique allows determination of “refractory periods” of the various cardiac structures. In addition, conduction characteristics may be investigated by pacing the cardiac structure of interest incrementally faster until a defined event occurs. To aid the nonelectrophysiologist in becoming conversant with intracardiac EP testing reports, a glossary of terms appears in Table 157.10 [65]. Just as there are developmental changes in the surface ECG intervals, so, too, do the intracardiac conduction intervals show changes with age. Some of these appear in Table 157.10. If inducibility of a tachyarrhythmia does not occur with single extrastimulus testing as described above, stimulation with multiple premature beats or bursts of pacing is performed. As with esophageal electrophysiology studies, if provocative testing under baseline conditions does not induce the expected tachycardia, testing is repeated during adrenergic stimulation with isoproterenol infusion, isoproterenol plus atropine, or epinephrine infusion.
The goals of the EP study are to assess the electrophysiologic characteristics of the myocardium, to determine if an arrhythmia substrate is present, to determine if a clinically relevant arrhythmia is inducible, to determine the mechanism of the arrhythmia, and occasionally to evaluate the pharmacological response of a tachyarrhythmia. Accurate diagnosis of the arrhythmia mechanism is important to help determine therapeutic approaches, including potential antiarrhythmic medications, ablation strategies, or need for an implantable defibrillator. Typically, the diagnostic EP study is performed in a setting where the ability to proceed with therapeutic ablation is seamless.
References
Spach MS, Kootsey JM, Sloan JD (1982) Active modulation of electrical coupling between cardiac cells of the dog. A mechanism for transient and steady state variations in conduction velocity. Circ Res 51:347–362
Greener ID, Monfredi O, Inada S, Chandler NJ, Tellez JO, Atkinson A, Taube MA, Billeter R, Anderson RH, Efimov IR, Molenaar P, Sigg DC, Sharma V, Boyett MR, Dobrzynski H (2011) Molecular architecture of the human specialised atrioventricular conduction axis. J Mol Cell Cardiol 50:642–651
Smeets JL, Allessie MA, Lammers WJ, Bonke FI, Hollen J (1986) The wavelength of the cardiac impulse and reentrant arrhythmias in isolated rabbit atrium. The role of heart rate, autonomic transmitters, temperature, and potassium. Circ Res 58:96–108
James N, Weiss JN, Garfinkel A, Karagueuzian HS, Chen PS, Qu Z (2010) Early afterdepolarizations and cardiac arrhythmias. Heart Rhythm 7:1891–1899
Burashnikov A, Antzelevitch C (2003) Reinduction of atrial fibrillation immediately after termination of the arrhythmia is mediated by late phase 3 early afterdepolarization-induced triggered activity. Circulation 107:2355
Rosenthal JE (1988) Reflected reentry in depolarized foci with variable conduction impairment in 1 day old infarcted canine cardiac tissue. J Am Coll Cardiol 12:404–411
Vaquero M, Calvo D, Jalife J (2008) Cardiac fibrillation: from ion channels to rotors in the human heart. Heart Rhythm 5:872–879
Kinoshita S, Katoh T, Hagisawa K, Kimura K (2007) Accessory-pathway block on alternate beats in the Wolff-Parkinson-White syndrome: supernormal conduction as the mechanism. J Electrocardiol 40:442–447
Marriott HJL, Conover M (1989) Advanced concepts in arrhythmias, 2nd edn. Mosby, St Louis, p 316
Brugada P, Brugada J, Mont L, Smeets J, Andries EW (1991) A new approach to the differential diagnosis of a regular tachycardia with a wide QRS complex. Circulation 83:1649
Wellens HJ, Bar FW, Lie KI (1978) The value of the electrocardiogram in the differential diagnosis of a tachycardia with a widened QRS complex. Am J Med 64:27–33
Narula OS, Samet P, Javier RP (1972) Significance of the sinus-node recovery time. Circulation 45:140–158
Strauss HC, Bigger JT, Saroff AL, Giardina EG (1976) Electrophysiologic evaluation of sinus node function in patients with sinus node dysfunction. Circulation 53:763–776
Narula OS, Shantha N, Vasquez M, Towne WD, Linhart JW (1978) A new method for measurement of sinoatrial conduction time. Circulation 58:706–714
de Marneffe M, Jacobs P, Englert M (1986) Reproducibility of electrophysiologic parameters of extrinsic sinus node function in patients with and without sick sinus syndrome. Pacing Clin Electrophysiol 9:482–489
Marcus B, Gillette PC, Garson A Jr (1991) Electrophysiologic evaluation of sinus node dysfunction in postoperative children and young adults utilizing combined autonomic blockade. Clin Cardiol 14:33–40
Hluchý J, Milovský V, Sámel M, Pavlovic M (1989) Comparison of indirect and direct methods for determination of sinoatrial conduction time. Eur Heart J 10:256–267
Schulze-Bahr E, Neu A, Friederich P, Kaupp UB, Breithardt G, Pongs O, Isbrandt D (2003) Pacemaker channel dysfunction in a patient with sinus node disease. J Clin Invest 111:1537–1545
Benson DW, Wang DW, Dyment M, Knilans TK, Fish FA, Strieper MJ, Rhodes TH, George AL (2003) Congenital sick sinus syndrome caused by recessive mutations in the cardiac sodium channel gene (SCN5A). J Clin Invest 112:1019–1028
Makita N, Sasaki K, Groenewegen WA, Yokota T, Yokoshiki H, Murakami T, Tsutsui H (2005) Congenital atrial standstill associated with coinheritance of a novel SCN5A mutation and connexin 40 polymorphisms. Heart Rhythm 2:1128–1134
Ratnasamy C, Idriss SF, Carboni MP, Kanter RJ (2009) Arrhythmias in children having a single left superior vena cava and minimal structural heart disease. J Cardiovasc Electrophysiol 20:182–186
Pasquali SK, Marino BS, Kaltman JR, Schissler AJ, Wernovsky G, Cohen MS, Spray TL, Tanel RE (2008) Rhythm and conduction disturbances at midterm follow-up after the ross procedure in infants, children, and young adults. Ann Thorac Surg 85:2072–2078
Salerno JC, Chun TU, Rutledge JC (2008) Sinus bradycardia, Wolff Parkinson White, and left ventricular noncompaction: an embryologic connection? Pediatr Cardiol 29:679–682
Weese-Mayer DE, Silvestri JM, Menzies LJ, Morrow-Kenny AS, Hunt CE, Hauptman SA (1992) Congenital central hypoventilation syndrome: diagnosis, management, and long-term outcome in thirty-two children. J Pediatr 120:381–387
Østergaard JR, Rasmussen TB, Mølgaard H (2011) Cardiac involvement in juvenile neuronal ceroid lipofuscinosis (Batten disease). Neurology 76:1245–1251
Sumitomo N, Karasawa K, Taniguchi K, Ichikawa R, Fukuhara J, Abe O, Miyashita M, Kanamaru H, Ayusawa M, Harada K (2008) Association of sinus node dysfunction, atrioventricular node conduction abnormality and ventricular arrhythmia in patients with Kawasaki disease and coronary involvement. Circ J 72:274–280
Dickinson DF, Scott O (1984) Ambulatory electrocardiographic monitoring in 100 healthy teenage boys. Br Heart J 51:179–183
Bexton RS, Camm AJ (1984) First degree atrioventricular block. Eur Heart J 5 (Suppl A):107–109
Viitasalo MT, Kala R, Eisalo A (1984) Ambulatory electrocardiographic findings in young athletes between 14 and 16 years of age. Eur Heart J 5:2–6
Kim YH, Onunain S, Trouton T, Sosa-Suarez G, Levine RA, Garan H, Ruskin JN (1993) Pseudo-pacemaker syndrome following inadvertent fast pathway ablation for atrioventricular nodal reentrant tachycardia. J Cardiovasc Electrophysiol 4:178–182
Yamakawa Y, Ishikawa T, Uchino K, Mochida Y, Ebina T, Sumita S, Kobayashi T, Matsushita K, Matsumoto K, Ohkusu Y, Nishizawa T, Takigiku K, Iwamoto M, Kimura K, Umemura S (2004) Prevalence of right bundle-branch block and right precordial ST-segment elevation (Brugada-type electrocardiogram) in Japanese children. Circ J 68:275–279
Corrado D, Pelliccia A, Heidbuchel H, Sharma S, Link M, Basso C, Biffi A, Buja G, Delise P, Gussac I, Anastasakis A, Borjesson M, Bjørnstad HH, Carre F, Deligiannis A, Dugmore D, Fagard R, Hoogsteen J, Mellwig KP, Panhuyzen-Goedkoop N, Solberg E, Vanhees L, Drezner J, Estes NAM III, Iliceto S, Maron BJ, Peidro R, Schwartz PJ, Stein R, Thiene G, Zeppilli P, McKenna WJ (2010) Recommendations for interpretation of 12-lead electrocardiogram in the athlete. Eur Heart J 31:243–259
Stéphan E (1979) Hereditary bundle branch system defect. A new genetic entity? Am Heart J 97:708–718
Schaal SF, Seidensticker J, Goodman R, Wooley CF (1973) Familial right bundle-branch block, left axis deviation, complete heart block, and early death. A heritable disorder of cardiac conduction. Ann Intern Med 79:63–66
Palitzsch D, Scheffzek A (1981) Familial right bundle branch block and left axis deviation without cardiac disorders. Monatsschr Kinderheilkd 129:300–302
Stéphan E, de Meeus A, Bouvagnet P (1997) Hereditary bundle branch defect: right bundle branch blocks of different causes have different morphologic characteristics. Am Heart J 133:249–256
Simonsen EE, Madsen EG (1970) Four cases of right-sided bundle-branch block and one case of atrioventricular block in three generations of a family. Br Heart J 32:501–504
Esscher E, Hardell LI, Michaëlsson M (1975) Familial, isolated, complete right bundle-branch block. Br Heart J 37:745–747
Buyon JP, Hiebert R, Copel J, Craft J, Friedman D, Katholi M, Lee LA, Provost TT, Reichlin M, Rider L, Rupel A, Saleeb S, Weston WL, Skovron ML (1998) Autoimmune-associated congenital heart block: demographics, mortality, morbidity and recurrence rates obtained from a national neonatal lupus registry. J Am Coll Cardiol 31:1658–1666
Karnabi E, Boutjdir M (2010) Role of calcium channels in congenital heart block. Scand J Immunol 72:226–234
Ambrosi A, Salomonsson S, Eliasson H, Zeffer E, Skog A, Dzikaite V, Bergman G, Fernlund E, Tingström J, Theander E, Rydberg A, Skogh T, Öhman A, Lundström U, Mellander M, Winqvist O, Fored M, Ekbom A, Alfredsson L, Källberg H, Olsson T, Gadler F, Jonzon A, Kockum I, Sonesson SE, Wahren-Herlenius M (2012) Development of heart block in children of SSA/SSB-autoantibody-positive women is associated with maternal age and displays a season-of-birth pattern. Ann Rheum Dis 71:334–340
Izmirly PM, Llanos C, Lee LA, Askanase A, Kim MY, Buyon JP (2010) Cutaneous manifestations of neonatal lupus and risk of subsequent congenital heart block. Arthritis Rheum 62:1153–1157
Jay PY, Harris BS, Buerger A, Rozhitskaya O, Maguire CT, Barbosky LA, McCusty E, Berul CI, O’brien TX, Gourdie RG, Izumo S (2004) Function follows form: cardiac conduction system defects in Nkx2-5 mutation. Anat Rec A Discov Mol Cell Evol Biol 280:966–972
Bossert T, Walther T, Gummert J, Hubald R, Kostelka M, Mohr FW (2002) Cardiac malformations associated with the Holt-Oram syndrome–report on a family and review of the literature. Thorac Cardiovasc Surg 50:312–314
Chockalingam P, Jaeggi ET, Rammeloo LA, Haak MC, Adama van Scheltema PN, Breur JMPJ, Bartelings MM, Clur SB, Blom NA (2011) Persistent fetal sinus bradycardia associated with maternal anti-SSA/Ro and anti-SSB/La antibodies. J Rheumatol 38:2682–2685
Ruffatti A, Milanesi O, Chiandetti L, Cerutti A, Gervasi MT, De Silvestro G, Pengo V, Punzi L (2012) A combination therapy to treat second-degree anti-Ro/La-related congenital heart block: a strategy to avoid stable third-degree heart block? Lupus 21:666–671
Routsias JG, Kyriakidis NC, Friedman DM, Llanos C, Clancy R, Moutsopoulos HM, Buyon J, Tzioufas AG (2011) Association of the idiotype:antiidiotype antibody ratio with the efficacy of intravenous immunoglobulin treatment for the prevention of recurrent autoimmune-associated congenital heart block. Arthritis Rheum 63:2783–2789
Raboisson M, Fouron J, Sonesson S, Nyman M, Proulx F, Gamache S (2005) Fetal Doppler echocardiographic diagnosis and successful steroid therapy of Luciani-Wenckebach phenomenon and endocardial fibroelastosis related to maternal anti-Ro and anti-La antibodies. J Am Soc Echocardiog 18:375–380
Jaeggi ET, Silverman ED, Yoo S, Kingdon J (2004) Is immune-mediated complete fetal atrioventricular block reversible by transplacental dexamethasone therapy? Ultrasound Obst Gynecol 23:602–605
Pisoni CN, Brucato A, Ruffatti A, Espinosa G, Cervera R, Belmonte-Serrano M, Sánchez-Román J, García-Hernández FG, Tincani A, Bertero MT, Doria A, Hughes GRV, Khamashta MA (2010) Failure of intravenous immunoglobulin to prevent congenital heart block: findings of a multicenter, prospective, observational study. Arthritis Rheum 62:1147–1152
Friedman DM, Kim MY, Copel JA, Llanos C, Davis C, Buyon JP (2009) Prospective evaluation of fetuses with autoimmune-associated congenital heart block followed in the PR Interval and Dexamethasone Evaluation (PRIDE) Study. Am J Cardiol 103:1102–1106
Matsubara S, Morimatsu Y, Shiraishi H, Kuwata T, Ohkuchi A, Izumi A, Takeda S, Suzuki M (2008) Fetus with heart failure due to congenital atrioventricular block treated by maternally administered ritodrine. Arch Gynecol Obstet 278:85–88
Epstein AE, Chair (2008) ACC/AHA/HRS 2008 guidelines for device-based therapy of cardiac rhythm abnormalities: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the ACC/AHA/NASPE 2002 Guideline Update for Implantation of Cardiac Pacemakers and Antiarrhythmia Devices) developed in collaboration with the American Association for Thoracic Surgery and Society of Thoracic Surgeons. Am Coll Cardiol 51:e1–e62
Michaëlsson M, Jonzon A, Riesenfeld T (1995) Isolated congenital complete atrioventricular block in adult life. A prospective study Circulation 92:442–449
Moak JP, Barron KS, Hougen TJ, Wiles HB, Balaji S, Sreeram N, Cohen MH, Nordenberg A, Van Hare GF, Friedman RA, Perez M, Cecchin F, Schneider DS, Nehgme RA, Buyon JP (2001) Isolated congenital complete atrioventricular block in adult life. A prospective study. J Am Coll Cardiol 37:238–242
Cecchin F, Frangini PA, Brown DW, Flynn-Thompson F, Alexander ME, Triedman JK, Gauvreau K, Walsh EP, Berul CI (2009) Cardiac resynchronization therapy (and multisite pacing) in pediatrics and congenital heart disease: five years experience in a single institution. J Cardiovasc Electrophysiol 20:58–65
Davey DL, Bratton SL, Bradley DJ, Yetman AT (2011) Relation of maternal anti-Ro/La antibodies to aortic dilation in patients with congenital complete heart block. Am J Cardiol 108:561–564
Plonsey R, Barr RC (2007) Bioelectricity: a quantitative approach, 3rd edn. Springer, New York
Robinson MR, Curzen N (2009) Electrocardiographic body surface mapping: potential tool for the detection of transient myocardial ischemia in the 21st century? Ann Noninvasive Electrocardiol 14:201–210
Kligfield P, Gettes LS, Bailey JJ et al (2007) Recommendations for the standardization and interpretation of the electrocardiogram: part I: the electrocardiogram and its technology a scientific statement from the American Heart Association Electrocardiography and Arrhythmias Committee, Council on Clinical Cardiology; the American College of Cardiology Foundation; and the Heart Rhythm Society endorsed by the International Society for Computerized Electrocardiology. J Am Coll Cardiol 49:1109–1127
Marcus FI, McKenna WJ, Sherrill D et al (2010) Diagnosis of arrhythmogenic right ventricular cardiomyopathy/dysplasia: proposed modification of the task force criteria. Circulation 6(121):1533–1541
Gass M, Apitz C, Salehi-Gilani S et al (2006) Use of the implantable loop recorder in children and adolescents. Cardiol Young 16:572–578
Cohen MI, Triedman JK, Cannon BC et al (2012) PACES/HRS expert consensus statement on the management of the asymptomatic young patient with a Wolff-Parkinson-White (WPW, ventricular pre-excitation) electrocardiographic pattern: developed in partnership between the Pediatric and Congenital Electrophysiology Society (PACES) and the Heart Rhythm Society (HRS). Endorsed by the governing bodies of PACES, HRS, the American College of Cardiology Foundation (ACCF), the American Heart Association (AHA), the American Academy of Pediatrics (AAP), and the Canadian Heart Rhythm Society (CHRS). Heart Rhythm 6:1006–1024
Paridon SM, Alpert BS, Boas SR et al (2006) Clinical stress testing in the pediatric age group: a statement from the American Heart Association Council on Cardiovascular Disease in the Young, Committee on Atherosclerosis, Hypertension, and Obesity in Youth. Circulation 113:1905–1920
Gillette PC, Garson A Jr (eds) (1990) Pediatric arrhythmias: electrophysiology and pacing. WB Saunders, Philadelphia
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer-Verlag London
About this entry
Cite this entry
Idriss, S.F., Kanter, R.J. (2014). Diagnosis of Arrhythmias and Conductive Disorders. In: Da Cruz, E., Ivy, D., Jaggers, J. (eds) Pediatric and Congenital Cardiology, Cardiac Surgery and Intensive Care. Springer, London. https://doi.org/10.1007/978-1-4471-4619-3_136
Download citation
DOI: https://doi.org/10.1007/978-1-4471-4619-3_136
Published:
Publisher Name: Springer, London
Print ISBN: 978-1-4471-4618-6
Online ISBN: 978-1-4471-4619-3
eBook Packages: MedicineReference Module Medicine