Abstract
Despite recent advances in the surgical techniques and equipment available for the management of urinary lithiasis, the prevalence of this condition continues to increase in the North American population. Associated costs are estimated to exceed 5.3 billion US dollars each year.
Epidemiological studies have implicated a range of contributory dietary, medical, environmental, and genetic factors in the pathophysiology of this disease. Many of these factors are consistent internationally. Despite this, the North American population, with its associated racial, environmental, and socioeconomic diversity, provides unique epidemiological insights. This chapter provides an overview of the risk factors for stone disease as well as incidence and prevalence patterns in a North American context using contemporary data.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Incidence
- Urinary stones
- Oxalates
- Urates
- Prevalence
- Geographical variation
- Stone composition
- Urine composition
- Staghorn stones
- Calcium oxalate stones
- Calcium phosphate stones
- Infection stones
- Uric acid stones
- Cystine stones
- Practice patterns
- Pediatric stones
- Age-related stone formation
- Recurrence
- Stone site
Introduction
Despite recent advances in the surgical techniques and equipment available for the management of urinary lithiasis, the prevalence of this condition continues to increase in the North American population. Associated costs are estimated to exceed 5.3 billion US dollars each year [1].
Epidemiological studies have implicated a range of contributory dietary, medical, environmental, and genetic factors in the pathophysiology of this disease. Many of these factors are consistent internationally. Despite this, the North American population, with its associated racial, environmental, and socioeconomic diversity, provides unique epidemiological insights. This chapter provides an overview of the risk factors for stone disease as well as incidence and prevalence patterns in a North American context using contemporary data.
Incidence
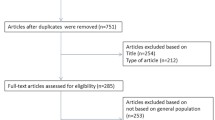
Information with regard to incident stone events affecting the North American population in the second half of the twentieth century may be extrapolated from a large population-based study conducted in Rochester, Minnesota [2]. Despite contradictory results in studies from other developed Western nations [3] suggesting a recent increased incidence of urinary lithiasis, these large studies show that the incidence of stone disease has plateaued in North America since the early 1970s.
Although stone disease appears to have declined among males since 1970 (Table2.1), the overall incidence of stone disease has remained stable. This is explained by an increased incidence in females of all ages (Fig.2.1). The male-to-female ratio reflects this, having declined from 3.1:1 in 1970 to 1.3:1 in 2000 [2]. Peak incidence in females has been shown to occur at a younger age of 20–29 years, compared with 60–69 years for males (see Table2.1and Fig.2.1)
Incident symptomatic stone rates 1950–2000.Solid linesdepict data from the current Rochester, MN, study (1970–2000). For comparison, thedotted linesindicate data from the previous Rochester, MN, USA, study by Johnson et al. (1950–1974) [5]. To facilitate comparison between the two studies, as in the earlier report, all rates are age adjusted to the 1960 US white population (Adapted with permission from Macmillan Publishers Ltd: Kidney International. Lieske et al. [2])
Prevalence
The lifetime risk of stone disease for individuals residing in the USA has been estimated to be 10–15 % and is influenced by racial and environmental factors as well as gender [4,5]. The United States National Health and Nutrition Examination Survey (NHANES) examined the prevalence of stone disease in a total of 31,479 individuals over two time periods between 1976–1980 and 1988–1994. By incorporating data from a large community-based survey, the study provides representative information with regard to temporal trends in the prevalence of stone disease. In comparing the two study periods, the prevalence in the United States was noted to have increased from 3.8 to 5.7 % [6]. Such results should be interpreted with a degree of caution, given the emergence of improved technologies for detection and treatment of stone disease between the two periods.
Differences in prevalence according to geographical location have been linked to dehydration and an associated increase in the concentration of lithogenic substances in the urine resulting from warmer climates [7]. Accordingly, the highest rates of stone disease are seen in the Southeastern United States, [8,9] with the lowest rates in the West and Midwest (Fig.2.2).
Age-adjusted prevalence of kidney stones in the 1988–1994 United States adult population by gender within regions (Adapted with permission from Stamatelou et al. [6])
A higher prevalence of stone disease in males is consistent across all age ranges, with a gradual increase in prevalence with age for both male and female patients (see Table2.2). With regard to ethnicity, African Americans display less than half the prevalence of stone disease when compared with Caucasians [8,10].
Practice Patterns/Methods of Treatment
The proportion of health care expenditure allocated to the management of urolithiasis continues to increase in North America. In 2000, direct treatment costs were estimated to exceed 2.1 billion dollars [11]. This reflects both an increase in the prevalence of the condition and the emergence of novel minimally invasive treatment options.
Practice patterns within the United States have been captured by several databases, including HCUP (Healthcare Cost and Utilization Project), CMS (Centers for Medicare & Medicaid Services), CHCPE (Centre for Health Care Policy and Evaluation), and NAMS (National Hospital Ambulatory Medical Care Survey).
A total of 617,647 individuals presented to an emergency room with a listed primary diagnosis of urolithiasis in 2000 [11]. This amounts to an estimated rate of 226 cases per 100,000 individuals. The increased availability and acceptance of minimally invasive techniques such as shock wave lithotripsy (SWL) and ureteroscopy led to an increase in ambulatory surgery between 1994 and 1998, with rates of 123/100,000 and 199/100,000, respectively. Accordingly, the mean length of hospital stay decreased for upper tract stones from 2.6 to 2.3 days during the same time period [11].
A reduction in open surgical procedures corresponded with a 60 % increase in ureteroscopic procedures for the period between 1992 and 2000. The rates of percutaneous nephrolithotomy (PCNL) (3–6 %) and SWL (49–54 %) remained essentially unchanged [12]. Although more recent data are lacking, it is likely that the proportion of cases performed ureteroscopically has continued to increase with the advent and dissemination of improved optical systems and ancillary devices.
Stone Composition
Evidence from studies in industrialized countries suggests a significant change in the chemical composition of renal stones during the second half of the twentieth century [13–15]. Calcium oxalate (monohydrate and dihydrate) now accounts for more than 60 % of all stones. This is likely a reflection of alterations in diet, in particular an increase in consumption of foods high in sodium and animal protein. Although many of the larger studies have been conducted in Europe, the results are likely to be representative in a North American context.
Table2.3summarizes the distribution of the most frequently encountered stones. While female patients are more likely to form phosphate stones, calcium oxalate stones are more common in male patients [16,17].
Urinary Parameters
Twenty-four-hour urine analysis remains an important part of the evaluation of the recurrent stone former. Low urine volume (defined as less than 2 L/day) has been implicated in the formation of both calcium- and non-calcium-containing stones, and the inverse relationship between stone formation and urine volume has been proven in observational studies [18]. Up to 92 % of patients with uric acid stones demonstrate low urine output [19]. Although not traditionally recommended, the consumption of caffeinated beverages (tea/coffee) and alcohol (wine/beer) has been shown in observational studies to reduce the subsequent risk of stone formation [20,21].
Up to 40 % of patients with calcium stone disease have associated hypercalciuria [22]. Hypercalciuria may also be seen in association with uric acid and struvite stones, with rates of 23 and 50 %, respectively [19]. Hyperoxaluria (>45 mg/day; 0.5 mmol/day) is more commonly seen in male calcium stone formers and may affect up to 40 % of such patients. In the North American population, hypocitraturia (<320 mg/day; 1.67 mmol/day) is seen in 5–11 % of patients and in association with all stone types [18,19].
Predisposing Factors
Medical
Results from the NHANES demonstrated an 80 % increase in the rate of extreme obesity in the USA between 1994 and 2000 [23]. This trend has continued through the first part of the twenty-first century. In addition to increasing the difficulty and complications associated with the treatment of existing stones, comorbid health conditions such as diabetes mellitus, hypertension, and metabolic syndrome have been implicated in the increased prevalence of stones in the North American population [24–27].
Obesity has been shown to negatively impact on urinary parameters, with an increase in the excretion of lithogenic substances, including calcium, oxalate, sodium, and uric acid [28,29]. The magnitude of this effect is more marked in females, which may account for a recent increased incidence of stone disease in this cohort of patients.
The formation of uric acid stones is commonly seen in those with obesity [30]. Insulin resistance may interfere with renal ammonium production and decrease urine pH [31]. In addition, a diet high in animal protein and purines is often seen in association with obesity and contributes to increased urinary acidity.
A range of other medical conditions, such as gout, inflammatory bowel disease, hyperparathyroidism, and renal tubular acidosis, have a well-established role in the formation of renal stones.
Surgical
In association with the increase in morbid obesity in North America and a frequent failure of individuals to lose weight with lifestyle interventions alone, there was a fivefold increase in the rate of bariatric surgery between 1998 and 2002 [32]. Although weight loss confers significant cardiovascular benefit and reduces the likelihood of metabolic syndrome, modern bariatric surgery has been linked to high rates of hyperoxaluria [33–35]. This has been found to be associated with a significant increase in the formation of calcium oxalate calculi within 5 years of surgery [36]. The mechanism for this remains elusive; however, it is likely to result from a combination of malabsorption and alterations in gut flora.
Genetic
While a clear genetic basis exists for cysteine urolithiasis, the genetic contribution to more common forms of stone disease remains less well defined.
A positive family history confers a 2.5 times increased risk of urolithiasis [37]. The relative contribution of environmental factors such as diet and climate in such families as compared with genetic influence alone requires further investigation.
Dietary/Environmental
As evidenced by the geographic variation in the prevalence of urolithiasis in North America, [8,9] rates of stone disease are higher in hot, dry climates due to associated dehydration and low urine volumes.
Between the time periods 1976–1980 and 1988–1994, the mean annual temperature (MAT) increased by 0.5 ° C in the United States. The prevalence of stone disease increased during the same time period. The effect of climate change on rates of urolithiasis remains to be precisely defined. Using climate change modeling data, which suggests that mean annual temperatures (MAT) will continue to rise in much of the United States, [38] a 7–10 % increase in the prevalence in stone disease is predicted by 2050 [39]. Figures2.3and2.4demonstrate predicted changes in the geographical distribution of stone disease, with an expansion of the “stone belt” from the Southeast to the Midwest of the United States.
Predicted warming and linear model nephrolithiasis risk change by 2050 for the USA. Strongest warming is in the midcontinent and upper Midwest.Heavy linesshow the four US census regions, andlight gray linesshow National Oceanic and Atmospheric Administration (NOAA) climate divisions (Adapted with permission from Brikowski et al. [39]. Copyright 2008, National Academy of Sciences, U.S.A.)
Predicted growth in high-risk stone area (stone belt; risk ratio ≥1.2) vs. time, for 2000 (yellow), 2050 (orange), and 2095 (red), linear model. At 2000, 41 % of the population is within a high-risk zone, 56 % at 2050, and 70 % at 2095, based on year 2000 population distribution (Adapted with permission from Brikowski et al. [39]. Copyright 2008, National Academy of Sciences, U.S.A.)
Several dietary constituents have been implicated in the formation of stones. These are particularly relevant in a North American context, where the diet is generally high in both sodium and animal protein. Animal proteins have been shown to reduce urinary citrate excretion and increase calcium excretion [40]. Likewise, dietary sodium has been shown to induce hypercalciuria [41].
Consumption of high-sugar carbonated beverages has been implicated in the rapid increase in rates of metabolic syndrome, obesity, diabetes, and cardiovascular disease seen within North America. Of all food types, soda is currently the greatest contributor to caloric intake in the United States [42]. Given the overwhelming evidence that obesity predisposes to urolithiasis, it is likely that soda indirectly contributes to stone disease. In addition, such beverages may contribute directly via the metabolism of fructose (the main sweetener used in soda), which increases serum uric acid [43].
The use of vitamin supplements has increased markedly over recent years in Western countries [44–46]. It has been estimated that approximately 40 % of Canadian adults regularly take supplements [47]. A proportion of these preparations contain high doses of vitamin C (ascorbic acid). Due to the metabolism of vitamin C to oxalate, supplementation in excess of the recommended daily intake (90 mg) has been associated with increased oxalate excretion [48] and a 40 % increase in stone formation [24]. In light of these results, patients with a history of calcium oxalate stone disease should be advised to avoid supplements containing vitamin C.
The importance of adequate dietary calcium in the prevention of osteoporosis for postmenopausal women is well established. In the knowledge that up to 80 % of stones in North America are calcium-containing, the contribution of dietary and supplemental calcium to stone formation has been thoroughly investigated [51]. Contrary to initial beliefs, several studies have convincingly demonstrated an inverse relationship between dietary calcium and risk of stone formation [24,49,50]. In light of these results, there appears to be no role for calcium restriction in the context of urolithiasis.
Conclusion
Although the incidence appears to have stabilized in North America over the past three decades, urolithiasis remains a significant health issue, with associated high costs and morbidity. Epidemiological studies have identified new challenges specific to the North American population, particularly in relation to an association between obesity and stone disease.
References
Saigal CS, Joyce G, Timilsina AR. Direct and indirect costs of nephrolithiasis in an employed population: opportunity for disease management? Kidney Int. 2005;68:1808–14.
Lieske JC, de la Pena Vega LS, Slezak JM, et al. Renal stone epidemiology in Rochester, Minnesota: an update. Kidney Int. 2006;69(4):760–4.
Hesse A, Brandle E, Wilbert D, et al. Study on the prevalence and incidence of urolithiasis in Germany comparing the years 1979 vs. 2000. Eur Urol. 2003;44:709–13.
Johnson CM, Wilson DM, O’Fallon WM, et al. Renal stone epidemiology: a 25-year study in Rochester, Minnesota. Kidney Int. 1979;16:624–31.
Sierakowski R, Finlayson B, Landes RR, et al. The frequency of urolithiasis in hospital discharge diagnoses in the united states. Invest Urol. 1978;15:438–41.
Stamatelou KK, Francis ME, Jones C, et al. Time trends in reported prevalence of kidney stones in the United States: 1976–1994. Kidney Int. 2003;63:1817–23.
Pak CY. Etiology and treatment of urolithiasis. Am J Kidney Dis. 1991;18:624–37.
Soucie JM, Thun MJ, Coates RJ, et al. Demographic and geographic variability of kidney stones in the United States. Kidney Int. 1994;46:893–9.
Curhan GC, Rimm EB, Willett WC, et al. Regional variation in nephrolithiasis incidence and prevalence among United States men. J Urol. 1994;151:838–41.
Sarmina I, Spirnak JP. Urinary lithiasis in the black population: an epidemiological study and review of the literature. J Urol. 1987;138:14–7.
Pearle MS, Calhoun EA, Curhan GC, et al. Urologic diseases in America project: urolithiasis. J Urol. 2005;173:848–57.
Kerbl K, Rehman J, Landman J, et al. Current management of urolithiasis; progress or regress? J Endourol. 2002;16:281–8.
Leusmann DB, Blaschke R, Schmandt W. Results of 5035 stone analysis: a contribution to epidemiology of stone disease. Scand J Urol Nephrol. 1990;24:205–10.
Daudon M, Donsimoni R, Hennequin C, et al. Sex- and age-related composition of 10617 calculi analyzed by infrared spectroscopy. Urol Res. 1995;23:319–26.
Asper R. Epidemiology and socioeconomic aspects of urolithiasis. Urol Res. 1984;12:1–5.
Gault MH, Chafe L. Relationship of frequency, age and sex, stone weight and composition in 15,624 stones: comparison of results for 1980 to 1983 and 1995 to 1998. J Urol. 2000;164:302–7.
Robertson WG, Peacock M, Heyburn PJ. Clinical and metabolic aspects of urinary stone disease in Leeds. Scand J Urol Nephrol Suppl. 1980;53(suppl):199–206.
Curhan GC, Willett WC, Speizer FE, et al. Twenty-four-hour urine chemistries and the risk of kidney stones among women and men. Kidney Int. 2001;59:2290–8.
Kourambas J, Aslan P, Teh CL, et al. Role of stone analysis in metabolic evaluation and medical treatment of nephrolithiasis. J Endourol. 2001;15:181–6.
Curhan GC, Willett WC, Spiezer FE, et al. Beverage use and risk for kidney stones in women. Ann Intern Med. 1998;128:534–40.
Curhan GC, Willett WC, Rimm EB, et al. Prospective study of beverage use and the risk of kidney stones. Am J Epidemiol. 1996;143:240–7.
Curhan GC. Epidemiology of stone disease. Urol Clin North Am. 2007;34:287–93.
Flegal KM, Carroll MD, Ogden CL, et al. Prevalence and trends in obesity among US adults, 1999–2000. JAMA. 2002;288:1723–7.
Taylor EN, Stampfer MJ, Curhan GC. Dietary factors and the risk of incident kidney stones in men: new insights after 14 years of follow-up. J Am Soc Nephrol. 2004;15:3225–32.
Taylor EN, Stampfer MJ, Curhan GC. Diabetes mellitus and the risk of nephrolithiasis. Kidney Int. 2005;68:1230–5.
Taylor EN, Stampfer MJ, Curhan GC. Obesity, weight gain, and the risk of kidney stones. JAMA. 2005;293:455–62.
Cappuccino FP, Strazzullo P, Mancini M. Kidney stones and hypertension: population based study of an independent clinical association. BMJ. 1990;12:1234–6.
Taylor EN, Curhan GC. Body size and 24-hour urine composition. Am J Kidney Dis. 2006;48:905–15.
Ekeruo WO, Tan YH, Young MD, et al. Metabolic risk factors and the impact of medical therapy on the management of nephrolithiasis in obese patients. J Urol. 2004;172:159–63.
Daudon M, Lacour B, Jungers P. Influence of body size on urinary stone composition in men and women. Urol Res. 2006;34:193–9.
Abate N, Chandalia M, Cabo-Chan Jr AV, et al. The metabolic syndrome and uric acid nephrolithiasis: novel features of renal manifestation of insulin resistance. Kidney Int. 2004;65:386–92.
Santry HP, Gillen DL, Lauderdale DS. Trends in bariatric surgical procedures. JAMA. 2005;294:1909–17.
Nelson WK, Houghton SG, Milliner DS, et al. Enteric hyperoxaluria, nephrolithiasis, and oxalate nephropathy: potentially serious and unappreciated complications of Roux-en-Y gastric bypass. Surg Obes Relat Dis. 2005;1:481–5.
Asplin JR, Coe FL. Hyperoxaluria in kidney stone formers treated with modern bariatric surgery. J Urol. 2007;177:565–9.
Sinha MK, Collazo-Clavell ML, Rule A, et al. Hyperoxaluric nephrolithiasis as a complication of Roux-en-Y gastric bypass surgery. Kidney Int. 2007;72:100–7.
Matlaga BR, Shore AD, Magnuson T, et al. Effect of gastric bypass surgery on kidney stone disease. J Urol. 2009;181:2573–7.
Curhan GC, Willett W, Rimm E, et al. Family history and risk of kidney stones. J Am Soc Nephrol. 1997;8:1568–73.
IPCC4. Climate change 2007: the physical science basis, summary for policy-makers. Fourth climate assessment report (UN Intergovernmental Panel on Climate Change, Geneva), 2007, p. 1–18.
Brikowski TH, Lotan Y, Pearle MS. Climate-related increase in the prevalence of urolithiasis in the United States. Proc Natl Acad Sci USA. 2008;105:9841–6.
Breslau N, Brinkley L, Hill K, et al. Relationship of animal protein-rich diet to kidney stone formation and calcium metabolism. J Clin Endocrinol Metab. 1998;66:140–6.
Muldowney FP, Freaney R, Moloney MF. Importance of dietary sodium in the hypercalciuria syndrome. Kidney Int. 1982;22:292–6.
Block G. Foods contributing to energy intake in the US: data from NHANES III and NHANES 1999–2000. J Food Compost Anal. 2004;17:439–47.
Nakagawa T, Hu H, Zharikov S, et al. A causal role for uric acid in fructose-induced metabolic syndrome. Am J Physiol Renal Physiol. 2006;290:F625–31.
Millen AE, Dodd KW, Subar AF. Use of vitamin, mineral, nonvitamin, and nonmineral supplements in the United States: the 1987, 1992, and 2000 National Health Interview Survey results. J Am Diet Assoc. 2004;104:942–50.
Ervin RB, Wright JD, Kennedy-Stephenson J. Use of dietary supplements in the United States, 1988–94. Vital Health Stat 11. 1999;244:1–14.
Slesinski MJ, Subar AF, Kahle LL. Trends in use of vitamin and mineral supplements in the United States: the 1987 and 1992 National Health Interview Surveys. J Am Diet Assoc. 1995;95:921–3.
Guo X, Willows N, Kuhle S, et al. Use of vitamin and mineral supplements among Canadian adults. Can J Public Health. 2009;1004:357–60.
Traxer O, Huet B, Poindexter J, et al. Effect of ascorbic acid consumption on urinary stone risk factors. J Urol. 2003;170:397–400.
Curhan GC, Willett WC, Rimm EB, et al. A prospective study of dietary calcium and other nutrients and the risk of symptomatic kidney stones. N Engl J Med. 1993;328:833–8.
Curhan GC, Willett W, Speizer F, et al. Comparison of dietary calcium with supplemental calcium and other nutrients as factors affecting the risk for kidney stones in women. Ann Intern Med. 1997;126:497–504.
Curhan GC, Willett W, Knight EL, et al. Dietary factors and the risk of incident kidney stones in younger women (Nurses’ Health Study II). Arch Intern Med. 2004;164:885–91.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2012 Springer-Verlag London
About this chapter
Cite this chapter
Denstedt, J.D., Fuller, A. (2012). Epidemiology of Stone Disease in North America. In: Talati, J., Tiselius, HG., Albala, D., YE, Z. (eds) Urolithiasis. Springer, London. https://doi.org/10.1007/978-1-4471-4387-1_2
Download citation
DOI: https://doi.org/10.1007/978-1-4471-4387-1_2
Published:
Publisher Name: Springer, London
Print ISBN: 978-1-4471-4383-3
Online ISBN: 978-1-4471-4387-1
eBook Packages: MedicineMedicine (R0)