Abstract
Pancreatic carcinoma is the fourth most deadly cancer in the United States and was responsible for 36.800 deaths in 2010. The incidence is 11/100,000 per year, and in about 80 %, the cancer is located in the pancreas’ head. Together with ampullary carcinoma, distal common bile duct carcinoma, and duodenal carcinoma, they are referred to as periampullary carcinomas. After radical resection the 5-year survival is currently 20-25 % and up to 50 % is found in ampullary tumors. With increasing experience and improved , .perioperative care, mortality rate is reduced to less than 5 % in high-volume centers. Unfortunately the procedure is still accompanied by substantial morbidity rates ranging from 40 to 60 %
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Duodeno pancreatic head surgery
- Biliary anastomosis
- Whipple procedure
- Postoperative bleeding
- Pancreatic leakage
- Biliary leakage
- Angiography
Pancreatic carcinoma is the fourth most deadly cancer in the United States and was responsible for 36.800 deaths in 2010. The incidence is 11/100,000 per year, and in about 80 %, the cancer is located in the pancreas’ head. Together with ampullary carcinoma, distal common bile duct carcinoma, and duodenal carcinoma, they are referred to as periampullary carcinomas [1, 2].
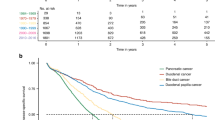
When diagnosed the overall 5-year survival rate is around 5 %. While prognosis is poor and survival low, surgical resection remains the only potential curative procedure for periampullary carcinomas. After radical resection the 5-year survival is currently 20–25 % and up to 50 % is found in ampullary tumors [3]. However in 80 % of patients with pancreatic cancer, curative procedure is infeasible, because of local vascular ingrowth or metastatic disease [4]. For patients with a resectable lesion partial pancreatoduodenectomy is the procedure of choice as introduced by Kausch and Whipple, currently modified for a pylorus-preserving pancreatoduodenectomy (PPPD) [5].
In the early years mortality rates of 10–40 % have been reported, but after increasing experience and improved perioperative care, mortality rate reduced to less than 5 % in high-volume centers [6, 7]. With improved results pancreatoduodenectomy (PD) is now widely accepted as treatment of choice for malignant tumors and even used for some benign lesions such as chronic pancreatitis with radiological signs of a mass in the pancreatic head region.
Unfortunately, the procedure is still accompanied by substantial morbidity rates ranging from 40 to 60 % [8–11]. The enormous difference in morbidity is partly due to a wide variety of definitions of complications used in the past. Fortunately the most common complications such as pancreatic anastomotic leakage, hemorrhage, and delayed gastric emptying now have been defined by the International Study Group of Pancreatic Surgery (ISGPS) [12–14]. A more general classification of surgical complication was introduced by Clavien in 2004 in which complications are graded following the invasiveness of their therapeutic interventions [15].
In this chapter we will discuss the diagnoses, grading, and management of the most important complications such as postpancreatectomy hemorrhage, anastomotic leakage, delayed gastric emptying, and chylous leakage as well as prevention and risk factors.
Complications
Anastomotic Leakage
Pancreatic Anastomosis
Incidence and Definition
Leakage of the pancreatic anastomosis is a key determinant in postoperative outcome and the most important complication after pancreatic surgery. It is associated with other complications such as intra-abdominal abscesses, sepsis, bleeding, and delayed gastric emptying that prolong hospital stay and are responsible for up to 88 % of postoperative mortality [9]. Due to a wide range in definitions, highly variable incidence rates between 2 and 30 % are reported in studies on pancreatic anastomotic leakage [16, 17]. The different definitions prevent a validated comparison of incidence and outcomes in different clinical trials. The International Study Group for Pancreatic Fistula (ISGPF) therefore developed a grading system for an objective and universally accepted definition of postoperative pancreatic fistula (POPF). It represents a “failure of healing/sealing of a pancreatic-enteric anastomosis, or it may represent a parenchymal leak not directly related to an anastomosis such as one originating from the raw pancreatic surface” [12].
Diagnosis and Grading
M. Trede reported many years ago the early clinical signs of POPF being abdominal tenderness, a slightly drier tongue, a rise in temperature and pulse, dyspnea, oliguria, and barely perceptible agitation [10]. These simple clinical changes are still the first step in early recognition of this complication. Pancreatic anastomosis leakage is generally recognized between the third and seventh POD (postoperative day).
When POPF is suspected, intra-abdominal drain effluent is tested on amylase contents. Amylase contents higher than three times the upper normal serum value associated with the symptoms mentioned above set the diagnosis POPF. Most patients generally will have a thorax X-ray examination because of the dyspnea showing pleural effusion due to the intra-abdominal collections. Computed tomography (CT) will confirm the diagnosis and identify the presence of intra-abdominal collections, see Fig. 14.1a.
Since the definition mentioned above will include clinically well patients with minor complaints, POPF is graded based on its clinical impact and therapeutic consequences following the ISGPF definition (Table 14.1) [12, 18].
Management and Outcome
Depending on the severity of POPF conservative management is adequate in up to 90 % of all patients and includes maintenance of perioperatively placed abdominal drains, supportive intravenous fluid and antibiotics, abstention of oral feeding, and nutritional support preferably by enteral feeding tube. Radiological intervention such as percutaneous drainage (Fig. 14.1b) is performed when conservative measures are unsuccessful and intra-abdominal collections or abscesses are found indicating a grade B POPF.
The incidence rate of grade B is widely variable, 13–63 %, and so is the frequency of radiological interventions ranging from 7 % up to 17 % in patients with POPF [19–21].
In the case of repeated unsuccessful percutaneous drainage or complications seen in POPF grade C such as sepsis, surgical intervention is almost mandatory. Like grade B POPF, the incidence rate of grade C and its subsequent surgical treatment is variable, ranging from 5.5 % up to 66 % of patients who undergo surgery [22]. The minimal approach during relaparotomy is extensive lavage and drainage. For a total dehiscent anastomosis, a more radical approach is needed. The anastomosis is discontinued, the jejunostomy closed by a stapler, and the pancreatic remnant can be closed and left behind with drainage of the pancreatic duct to create a controlled fistula, or even removed, a so called salvage pancreatectomy. This measure is under debate since definitive endocrine insufficiency is inevitable. More recently some advocate performing a new anastomosis into the stomach, a pancreaticogastrostomy.
In a study conducted in our institute surgical drainage was performed in 20 % of all patients with severe pancreatic leakage and completion pancreatectomy was performed in 22 %. This study also showed a significant reduction in the overall relaparotomy rate of 16.1–7.7 % (P = 0.005) in the period 1992–2002, despite a stable leakage rate, which has been further reduced during the past 10 years, indicating improvement of the nonsurgical management [22].
Radiological interventions have gained a more prominent role in the management of complications in most recent studies. These minimal-invasive techniques will shorten hospital stay and lower mortality rates and hospital costs by preventing extensive surgical procedures.
Risk Factors and Prevention
Many factors influence the incidence of POPF after PD as depicted in Table 14.2 [23]. Some factors are more significant than others. Generally accepted to be the most important risk factors are disease and pancreas-related factors as well as surgeons’ experience and hospital volume.
Yeo et al. reported the strongest predictors of POPF being ampullary or duodenal disease and surgical volume [24]. Others reported additional risk factors in their multivariate analyses: coronary artery disease (OR 3.7; 95 % CI 1.2–12.1), a soft gland (OR 10.0; 95 % CI 2.1–47.6), and pancreatic duct diameter ≤3 mm (RR 2.5; 95 % CI 1.05–9.5). Similar predictive factors were found in our study: pancreatic duct size ≤2 mm (P = 0.002), operating time ≥285 min (P = 0.031), and ampullary adenocarcinoma (P = 0.035) [22, 25].
Several surgical techniques have been described in order to find the optimal reconstruction after PD and prevent high rates of POPF. Two randomized controlled trials (RCT) compared the two most common techniques: pancreaticojejunostomy (PJ) versus pancreaticogastrostomy (PG). However, no superiority of either PJ or PG was reported [24, 26].
New techniques different from the conventional anastomotic techniques have been described in two other RCTs. A significant decrease in clinically relevant POPF from 18 % to 4 % was reported after comparing pancreaticogastrostomy with gastric partition versus conventional PJ, in favor of the PG with gastric partition (P = 0.01) [27]. A new pancreaticojejunostomy binding technique compared with conventional PJ reported leakage rates in 0 % versus 7.2 %, respectively (OR 1.08; 95 % CI 1.02–1.14; P = 0.014) [28].
The most optimal technique for the PJ reconstruction is still under debate ranging from end-to-side, duct-to-mucosa, to invagination, but only two randomized trials were performed. One study showed fewer POPF cases after the invagination technique compared with the duct-to-mucosa PJ (12 % vs. 24 %, P = 0.04), though another study revealed no significant differences in POPF rates in patients with soft pancreatic texture when duct-to-mucosa was compared to end-to-side PJ. Another ongoing debate is one- or two-layer reconstruction with continuous or interrupted sutures, but no differences are reported. The experience of the surgeon with one of these techniques is the most important determinant [29].
Procedures to avoid a pancreatic anastomosis and thereby avoiding POPF have also been described. Occlusion of pancreatic duct after PD showed no difference in postoperative complications [30]. Total pancreatectomy will of course avoid anastomotic leakage but is associated with endocrine pancreatic insufficiency.
Drainage of the pancreatic duct as a preventive measure was studied in three RCTs. They compared drainage versus no drainage after PD. Internal pancreatic duct drainage did not reduce the POPF rate; however two studies reported a significantly lower rate after external drainage (26 % vs. 42 %, P = 0.034; 6.7 % vs. 20 %, P = 0.032) [20, 25, 31]. The role of fibrin glue was also evaluated but no decrease in POPF rates was reported [32].
Pharmacological intervention is another major preventive measure. Lai et al. reviewed 11 RCTs in which 6 showed a decreased postoperative complication rate after the use of perioperative somatostatin, but the other 5 did not. Two studies reported significantly less POPF cases in the somatostatin group (P < 0.05). Though, due to the contradictory outcomes, the use of somatostatin remains controversial [9].
In conclusion, many different aspects to prevent leakage have been analyzed, and so far none have been proven superior in meta-analyses or large RCTs. The surgeon’s experience in performing the anastomosis might be the most important factor, but new techniques/modifications as pancreaticogastrostomy with gastric partition, the invagination procedure, as well as stenting of the anastomosis are promising, but more research is necessary to prove superiority of any of those procedures.
Biliary Anastomosis
Incidence and Definition
Leakage of the hepaticojejunostomy is reported between 0.4 and 10 % of the patients after pancreatic surgery. It can initiate a biliary peritonitis and is associated with concomitant complications such as intra-abdominal abscesses, bleeding, and wound infection. This prolongs hospital stay and decreases quality of life. Unlike pancreatic leakage, it is a rare complication with very low mortality rates ranging from 1 to 3 % [33].
The International Study Group of Liver Surgery (ISGLS) recently developed a uniform definition and grading system of biliary leakage. It is defined as bile-stained fluid in the abdominal drain or biliary collections in the abdominal cavity in need for radiological or surgical intervention. Bilirubin concentration of the drained fluid is at least three times the serum bilirubin concentration [34].
Diagnosis and Grading
Biliary leakage is suspected when bile-stained fluid is present in the abdominal drain. Other anastomotic leakages have to be ruled out and ultrasonography and CT can detect any intra-abdominal perihepatic collections. Diagnostic aspiration of the collection will establish the diagnosis of biliary leakage. Magnetic resonance cholangiopancreatography (MRCP) can be used to detect the location of the leak.
In patients with biliary leakage, typical laboratory abnormalities are seen: isolated hyperbilirubinemia with normal Gamma-glutamyl transpeptidase and alkaline phosphatase due to the lack of obstruction.
The clinical characteristics and grading parameters are summarized in Table 14.3 [34].
Management and Outcome
Maintenance of preoperatively placed drains is the first step in managing biliary leakage. However in the case of an insufficiently drained leakage, percutaneous transhepatic biliary drainage (Fig. 14.2) is the treatment of choice and is performed in nearly 70 % of patients. A catheter is placed into the biliary system and preferably through the anastomosis into the jejunal loop which facilitates external and internal drainage.
This procedure changed the aggressive management of early relaparotomy in which the leakage was drained externally and abdominal lavage was performed. Anastomotic repair was performed when necessary but is currently avoided by the percutaneous approach. Surgical management is now only performed in less than 20 % of patients after drainage is unsuccessful or patients’ clinical status asks for an immediate aggressive approach seen in grade C.
Prevention and Risk Factors
In a multivariate analysis, we found three independent predictors of biliary leakage: obesity BMI ≥ 35 (OR 11.32, 95 % CI 1.71–75, P = 0.012), no preoperative endoscopic biliary drainage (OR 2.43, 95 % CI 1.03–5.78, P = 0.044), and segmental anastomosis (OR 13.56, 95 % CI 4.23–43.49, P < 0.001) [33].
Preventing leakage of the hepaticojejunostomy can be achieved by placing a stent in the common bile duct during operation providing the bile to leak through the stent into the jejunum or drained externally.
Enteric Anastomosis
Incidence and Definition
Enteric anastomotic leak is very rarely seen after pancreatic surgery. Only one article solely describes duodenojejunostomy (DJ) or gastrojejunostomy (GJ) leakage after PPPD or standard PD, respectively [35]. The clinical symptoms might be the same as leakage of the PJ or HJ. Most large studies do not report DJ or GJ leak separately, simply because the complication did not occur, or in a low incidence rate ranging from 0.4 % to 1.2 %. The incidence is comparable with rates reported in other upper gastrointestinal operations. DJ or GJ leakage was defined as radiographic or visual evidence of the anastomotic defect [30, 35].
Diagnosis and Grading
DJ or GJ leakage can present within the first 10 days after surgery with one or more of the following clinical signs: an acute abdomen, fever, or enterocutaneous fistula or loss of bowel contents via the abdominal drain. Laboratory results will often reveal a leukocytosis. Radiological signs that indicate anastomotic failure will reveal free air on X-ray and fluid collections on CT (Fig. 14.3).
DJ or GJ leakage has been graded in a study previously mentioned according to the Clavien complication grading system [15].
Management and Outcome
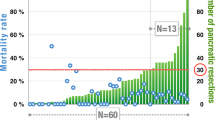
DJ or GJ leakage is a potentially fatal complication, it can prolong hospital stay with up to 25 days and surgical management is often required. In a study mentioned above, 12 out of 13 patients underwent relaparotomy. In >80 % of these patients, a distal gastrectomy had to be performed followed by new reconstruction. Only one patient was treated radiological with percutaneous drainage. Mortality rate reported in this study was substantial (38 %) [35].
Prevention and Risk Factors
Due to the low incidence, multivariate models of risk factors are unavailable. Furthermore the causes of these complications are unknown, but impaired perfusion of the anastomosis and a poorly vascularized duodenal stump might be causative factors in particular for the pylorus-preserving pancreatoduodenectomy.
Postpancreatectomy Hemorrhage
Incidence and Definition
Postoperative hemorrhage is another serious complication after pancreatic resection with incidence rates varying from 2 to 20 % and mortality rates exceeding 50 % [36]. The variability in incidence and mortality is partly caused by the many different definitions that are being used. Furthermore, substantial differences are seen in onset, cause, bleeding site, intensity, and clinical impairment of postoperative hemorrhage.
To enable a comparison between different surgical techniques in pancreatic surgery and the consequential incidence rate of postoperative hemorrhage and its mortality, one widely accepted definition is needed. The International Study Group of Pancreatic Surgery (ISGPS) developed a definition and proposed the term postpancreatectomy hemorrhage (PPH) [13]. They classified postoperative bleeding based on three criteria: time of onset, early PPH occurring within 24 h postoperatively and late PPH >24 h; location, intraluminal or extraluminal; and severity and impact, mild PPH with a similar clinical impairment and severe PPH with sequential blood transfusions and radiological and/or surgical interventions.
Since the introduction of the ISGPS hemorrhage classification, a number of studies validated the scoring system which is currently generally accepted [36, 37].
Diagnosis and Grading
Patients who develop PPH may present with hypotension, tachycardia, decreasing hemoglobin concentration, clinical deterioration, or blood loss through the gastrointestinal tract or abdominal drains depending on the site of the bleeding: intraluminal or extraluminal.
Intraluminal bleedings are seen near the anastomotic site, vessels in that area, the surface of the pancreas, or near a gastric ulcus. They generally present with blood loss through the gastrointestinal tract being hematemesis, melaena, and blood loss through the nasogastric tube. Intraluminal bleeding will usually manifest as an early hemorrhage. Consensus has been reached considering the cause of early hemorrhage which is likely due to technical failures during the index operation. In the case of intraluminal hemorrhage, endoscopy can be very useful since diagnosing and managing an anastomotic bleeding can be performed simultaneously. Angiography can be used to embolize bleeding from vessels. A recent analysis showed that angiography was performed in over 50 % of patients with PPH after pancreatic surgery and 18 % was subjected to an endoscopy. Both procedures were initially performed to detect the bleeding site [38]. All diagnostic interventions were performed provided that the patient was in a stable hemodynamic condition.
Extraluminal bleedings are seen in the abdominal cavity and may be evident by blood loss through the abdominal drain. The bleedings are caused by vascular erosion, anastomotic ulceration, arterial pseudoaneurysm, or disrupted suture line caused by POPF, biliary leakage, or intra-abdominal infections and generally present as late PPH. When PPH is suspected, ultrasonography and CT can detect intra-abdominal collections (hematoma as well as abscesses) seen in 70–80 % in late PPH. Furthermore, both procedures can detect pseudoaneurysms. The diagnosis is confirmed by angiography [39].
Blood loss through abdominal drains or nasogastric tubes is called a sentinel bleed and can be seen hours or even days before massive hemorrhage. Jagad et al. reviewed several studies and showed that in 30–100 %, a sentinel bleed resulted in PPH hours or days later [36]. A study performed in our institute reported that in 78 % of patients, a sentinel bleed was detected prior to late PPH and 74 % of patients with late PPH had septic complications [39].
When PPH is diagnosed, the clinical grading system proposed by the ISGPS classification, summarized in Table 14.4, can be used to state the severity of the hemorrhage [13].
Management and Outcome
Severe PPH asks for immediate treatment through either radiological intervention, e.g., angiography with embolization (Figs. 14.4a and b, 14.5a and b) or endoscopy with clips or sclerotherapy, or surgical intervention when the patients’ condition is deteriorating rapidly or radiological interventions are unsuccessful or infeasible.
Patient presenting with hematemesis after pancreatoduodenectomy was performed. Angiography reveals an aberrant arteria hepatica communis (AHC) originating from the arteria mesenterica superior (AMS) and a pseudoaneurysm of the arteria gastroduodenalis shown in (a) (arrow). A covered stent is placed in the arteria hepatica communis to manage the pseudoaneurysm shown in (b) (arrow)
In a recent study on PPH, 38 % of patients underwent primary surgery, 57 % underwent primary radiological intervention, and 5 % were treated conservatively. More than half of the radiological interventions (54 %) were unsuccessful and a rescue laparotomy still had to be performed. The success rate of radiological coiling in terms of hemostasis was 80 % [38]. In this study endoscopic intervention was used in patients with early intraluminal bleeding realizing that a PJ bleeding generally is outside the reach of endoscopy but can also be managed by interventional angiography. Intraluminal bleeding can disrupt the anastomosis, causing a “false” extraluminal bleed since blood is then seen in the abdominal cavity. Early extraluminal PPH (within 24 h after surgery) is generally managed immediately with relaparotomy.
Management of late PPH is different since it is often caused by pseudoaneurysms due to POPF or intra-abdominal infections. An earlier study conducted at the AMC showed that 69 % of patients with late PPH underwent primary surgery and only 9 % were managed by radiological embolization. In half of all the surgical procedures, a vessel ligation was performed. Completion pancreatectomy was performed because of persistent anastomotic leakage (Table 14.5) [39].
More recently embolization is performed in the majority of patients.
A meta-analysis regarding the management of late PPH after PD showed 20 small case series with 163 patients in which 47.2 % of patients underwent primary surgery, 44.8 % underwent primary radiological intervention, and 8 % were treated conservatively. No significant differences were found regarding the morbidity or mortality between relaparotomy and radiological intervention. Though late hemorrhage is often already associated with other complications, in particular leakage and sepsis, as mentioned earlier, this combination is associated with a poor prognosis [40].
The pathophysiology of early PPH makes its management less complicated with better outcomes compared to late PPH. Identifying the importance of a sentinel bleed and an adequate aggressive approach towards the patients’ clinical status will dictate the appropriate treatment. More research is needed to offer any standardized rules in the management of PPH.
Prevention and Risk Factors
The two most important predictive factors in PPH are sentinel bleed and pancreatic fistula [39]. A multivariate analysis reported three significant risk factors being pancreatic leakage (OR 3.5; 95 % CI 1.8–6.1), gastrojejunostomy leakage (OR 9.2; 95 % CI 1.5–56), and intra-abdominal abscess (OR 7.8; CI 4.2–14) [41]. Others suggest extended lymph node dissection being a risk factor [36]. PPH can be minimized by optimal preoperative preparation of the patient, exact attention to details during surgery, and close observation of the patient postoperatively.
Delayed Gastric Emptying
Incidence and Definition
The most common complication after pancreatoduodenectomy is delayed gastric emptying (DGE). Although DGE is not associated with a high mortality, it does have a severe impact on the postoperative course, hospital stay, and quality of life. It is most often found in patients with intra-abdominal complications. Although the pathogenesis of primary DGE, without intra-abdominal complications, still remains unclear disruption of the neural connections, ischemic injury to the muscle mechanism and low levels of circulating motilin are thought to be involved.
Due to the lack of a generally accepted definition, the reported incidence rates vary widely from 5 to 57 % [42]. More recently, the International Study Group of Pancreatic Surgery (ISGPS) developed an objective and generally applicable definition with different grades [14]. The definition takes several aspects into account:
-
Duration of nasogastric tube (NGT) and/or need for reinsertion of NGT
-
Ability to tolerate solid oral intake
-
Severity
-
Therapeutic consequences
Diagnosis and Grading
The different grades of DGE describe its severity and clinical impact (Table 14.6) [14].
DGE is an early complication seen after pancreatic surgery. Patients are unable to tolerate solid oral intake by POD 7 and NGT is required for 4 days or more. When DGE arises, the underlying cause and in particular intra-abdominal collections due to leakage have to be excluded and generally a CT scan is performed. Diagnostic procedures to assess the gastric emptying are not routinely used but scintigraphy is considered the most accurate method for measurement of DGE [43].
Management and Outcome
The required intervention depends on the severity of DGE. Grade A will have no interventional consequences, but in grade C DGE adequate management aimed at the cause is necessary. When DGE is caused by intra-abdominal complications, managing these complications will subsequently manage DGE.
Standard treatment of DGE is mainly supportive by maintenance of perioperatively placed nasogastric tube and nutritional support preferably by the enteral route despite the fact that enteral infusion can potentially impair gastric emptying. A randomized trial was conducted in our institute to assess the effect of cyclic versus continuous enteral feeding on DGE. Cyclic enteral feeding after PPPD was associated with a shorter period of enteral nutrition, faster return to a normal diet (P = 0.04), and a shorter hospital stay (P = 0.04) [44].
Massive production of the NGT might lead to electrolyte and body fluid disturbances, and in these circumstances parental supplementation is mandatory.
Therapeutic measures have been sought to minimize the incidence of DGE. The reduction in circulating motilin levels after PD is thought to be causing DGE. Motilin agonists, erythromycin, have been administered in order to improve gastric emptying. DGE was reported in 14.3 % of patients who were administered erythromycin versus 57.1 % of patients who did not received erythromycin (P < 0.04) [42].
Prevention and Risk Factors
Since the causes of DGE are unclear and likely to be multifactorial, it is difficult to take preventive measures. Various surgical techniques have been appointed to decrease the incidence of DGE.
Extended research has been conducted on the outcomes of standard PD versus pylorus-preserving PD (PPPD). A recently published RCT revealed that standard PD significantly reduces the incidence of DGE compared with PPPD (P = 0.02) [45]. However three systematic reviews failed to report this. They did report perioperative differences, PPPD was a faster procedure (95 % CI −105.70 to −30.83; P = 0.0004) with less intraoperative blood loss (95 % CI −0.96 to −0.56; P < 0.00001) [46–48].
Two meta-analyses compared standard PD with extended lymphadenectomy PD and revealed slightly higher DGE rates in the extended group [49, 50]. The largest RCT reported DGE in 6 % in the PD group and in 16 % in the extended PD group (P = 0.006) [51]. Explanation for this difference might be that more complex operations, with increased operation time and more blood loss, have a higher chance of DGE.
A more recently published study on DGE analyzed the effect of antecolic versus retrocolic reconstruction of the enterojejunostomy. DGE was seen in 30.9 % and no differences were found between the two techniques (antecolic 34 % vs. retrocolic 28 %, P = 0.6). Age was the only significant predictive factor found after multivariate analysis (P = 0.02) [52]. Another RCT did however show a significant difference. DGE was reported in 5 % in the antecolic group and in 50 % in the retrocolic group (P = 0.0014), but the study population was very limited (n = 40) [53]. Currently an RCT is being conducted in our own institute regarding DGE after retrocolic versus antecolic reconstruction of the duodenojejunostomy (registration number NTR1697).
The influence of prophylactic octreotide on DGE was analyzed in an RCT but failed to show an effect. They did however identify preoperative biliary drainage as an independent risk factor (OR 3.8; 95 % CI 0.98-14.9; P = 0.054) [54].
Chylous Leakage
Incidence and Definition
Chylous leakage is caused by injury to the lymphatic system. The cisterna chyli, a saccular dilatation which contains ascending lymphatic trunks, is located on the same level as the pancreas and injury to the cisterna chyli or its tributaries can occur during pancreatic dissection from the back site.
Chylous leakage is a rare complication; thus little is known about its incidence and management. Recent studies report a wide variation and incidence rates of 1.8, 5, 6.7, and 11 % [55–57]. In the absence of a uniform definition, our center proposed a grading system and a clear definition of chylous leakage. Chylous leakage was defined as a drain output of ≥275 mL with milky appearance and triglyceride level higher then 1.2 mmol/L in the absence of anastomotic leakage [57].
Diagnosis and Grading
Chylous leakage is usually seen on POD 1 or 2. It can appear as painless abdominal distension and respiratory embarrassment and can cause weight loss and fatigue. The appearance of the drain output and its high levels of triglycerides are sufficient to set the diagnosis. In some cases, CT can be helpful and some authors report more invasive diagnostic measures such as lymphangiography and lymphoscintigraphy [58]. However these techniques are very rarely used in daily practice.
Chylous leakage is graded in order to predict the severity and clinical impact (Table 14.7) [57].
Management and Outcome
In general, dietary therapy is the most frequently used conservative management. Enteral feeding with high protein and low fat with low or median-chain triglycerides is the treatment of choice. When enteral intake is impossible, total parenteral nutrition (TPN) is given. TPN is also given as an addition to enteral feeding when enteral feeding alone is insufficient [57]. The combination of dietary measures and somatostatin has been reported to be beneficial as well [55]. Paracentesis is performed when conservative measures alone are not adequate and is reported to be sufficient in up to 100 % [57]. Like the invasive diagnostic procedures, rigorous therapeutic measures for chylous leakage such as relaparotomy or a peritoneovenous shunt to close the leakage of the cisterna chyli are rarely performed [56].
Prevention and Risk Factors
Several factors were associated with a higher risk of chylous leakage. In a multivariate analysis, an increasing number of lymph nodes harvested (OR 1.07; 95 % CI 1.02–1.13; P = 0.007) and vascular resection at the time of surgery (OR 8.25; 95 % CI 1.99–34.6; P = 0.004) were two prognostic factors. Chronic pancreatitis was another independent-associated factor (OR 2.52; 95 % CI 1.19–5.32; P = 0.016) [56, 57].
Summary
Pancreatic surgery is associated with a high incidence of complications. The most severe combination of complications responsible for high mortality rates is anastomotic leakage and hemorrhage. Clinical observation and an adequate approach are important in the postoperative management. This postoperative management has shifted over the last decade, and a nonoperative management is seen more often in which radiological intervention plays an important role.
References
Jemal A, Siegel R, Xu J, Ward E. Cancer statistics, 2010. CA Cancer J Clin. 2010;60(5):277–300.
Sharma C, Eltawil KM, Renfrew PD, Walsh MJ, Molinari M. Advances in diagnosis, treatment and palliation of pancreatic carcinoma: 1990–2010. World J Gastroenterol. 2011;17(7):867–97.
Riall TS, Cameron JL, Lillemoe KD, Campbell KA, Sauter PK, Coleman J, et al. Pancreaticoduodenectomy with or without distal gastrectomy and extended retroperitoneal lymphadenectomy for periampullary adenocarcinoma–part 3: update on 5-year survival. J Gastrointest Surg. 2005;9(9):1191–204.
Kuhlmann KF, de Castro SM, Wesseling JG, ten Kate FJ, Offerhaus GJ, Busch OR, et al. Surgical treatment of pancreatic adenocarcinoma; actual survival and prognostic factors in 343 patients. Eur J Cancer. 2004;40(4):549–58.
Whipple AO, Parsons WB, Mullins CRTREATMENTOFCARCINOMAOFTHEAMPULLAOFVATER. Ann Surg. 1935;102(4):763–79.
van Heek NT, Kuhlmann KF, Scholten RJ, de Castro SM, Busch OR, van Gulik TM, et al. Hospital volume and mortality after pancreatic resection: a systematic review and an evaluation of intervention in the Netherlands. Ann Surg. 2005;242(6):781–8.
Finks JF, Osborne NH, Birkmeyer JD. Trends in hospital volume and operative mortality for high-risk surgery. N Engl J Med. 2011;364(22):2128–37.
DeOliveira ML, Winter JM, Schafer M, Cunningham SC, Cameron JL, Yeo CJ, et al. Assessment of complications after pancreatic surgery: A novel grading system applied to 633 patients undergoing pancreaticoduodenectomy. Ann Surg. 2006;244(6):931–7.
Lai EC, Lau SH, Lau WY. Measures to prevent pancreatic fistula after pancreatoduodenectomy: a comprehensive review. Arch Surg. 2009;144(11):1074–80.
Trede M, Schwall G. The complications of pancreatectomy. Ann Surg. 1988;207(1):39–47.
Gouma DJ, van Geenen RC, van Gulik TM, de Haan RJ, de Wit LT, Busch OR, et al. Rates of complications and death after pancreaticoduodenectomy: risk factors and the impact of hospital volume. Ann Surg. 2000;232(6):786–95.
Bassi C, Dervenis C, Butturini G, Fingerhut A, Yeo C, Izbicki J, et al. Postoperative pancreatic fistula: an international study group (ISGPF) definition. Surgery. 2005;138(1):8–13.
Wente MN, Veit JA, Bassi C, Dervenis C, Fingerhut A, Gouma DJ, et al. Postpancreatectomy hemorrhage (PPH): an International Study Group of Pancreatic Surgery (ISGPS) definition. Surgery. 2007;142(1):20–5.
Wente MN, Bassi C, Dervenis C, Fingerhut A, Gouma DJ, Izbicki JR, et al. Delayed gastric emptying (DGE) after pancreatic surgery: a suggested definition by the International Study Group of Pancreatic Surgery (ISGPS). Surgery. 2007;142(5):761–8.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240(2):205–13.
McKay A, Mackenzie S, Sutherland FR, Bathe OF, Doig C, Dort J, et al. Meta-analysis of pancreaticojejunostomy versus pancreaticogastrostomy reconstruction after pancreaticoduodenectomy. Br J Surg. 2006;93(8):929–36.
Wente MN, Shrikhande SV, Muller MW, Diener MK, Seiler CM, Friess H, et al. Pancreaticojejunostomy versus pancreaticogastrostomy: systematic review and meta-analysis. Am J Surg. 2007;193(2):171–83.
Shrikhande SV, D'Souza MA. Pancreatic fistula after pancreatectomy: evolving definitions, preventive strategies and modern management. World J Gastroenterol. 2008;14(38):5789–96.
Berger AC, Howard TJ, Kennedy EP, Sauter PK, Bower-Cherry M, Dutkevitch S, et al. Does type of pancreaticojejunostomy after pancreaticoduodenectomy decrease rate of pancreatic fistula? A randomized, prospective, dual-institution trial. J Am Coll Surg. 2009;208(5):738–47.
Pessaux P, Sauvanet A, Mariette C, Paye F, Muscari F, Cunha AS, et al. External Pancreatic Duct Stent Decreases Pancreatic Fistula Rate After Pancreaticoduodenectomy: Prospective Multicenter Randomized Trial. Ann Surg. 2011;253(5):879–85.
Prenzel KL, Holscher AH, Grabolle I, Fetzner U, Kleinert R, Gutschow CA, et al. Impact of duct-to-mucosa pancreaticojejunostomy with external drainage of the pancreatic duct after pancreaticoduodenectomy. J Surg Res. 2011;171:558–62.
de Castro SM, Busch OR, van Gulik TM, Obertop H, Gouma DJ. Incidence and management of pancreatic leakage after pancreatoduodenectomy. Br J Surg. 2005;92(9):1117–23.
Ramacciato G, Mercantini P, Petrucciani N, Nigri GR, Kazemi A, Muroni M, et al. Risk factors of pancreatic fistula after pancreaticoduodenectomy: a collective review. Am Surg. 2011;77(3):257–69.
Yeo CJ, Cameron JL, Maher MM, Sauter PK, Zahurak ML, Talamini MA, et al. A prospective randomized trial of pancreaticogastrostomy versus pancreaticojejunostomy after pancreaticoduodenectomy. Ann Surg. 1995;222(4):580–8.
Poon RT, Fan ST, Lo CM, Ng KK, Yuen WK, Yeung C, et al. External drainage of pancreatic duct with a stent to reduce leakage rate of pancreaticojejunostomy after pancreaticoduodenectomy: a prospective randomized trial. Ann Surg. 2007;246(3):425–33.
Duffas JP, Suc B, Msika S, Fourtanier G, Muscari F, Hay JM, et al. A controlled randomized multicenter trial of pancreatogastrostomy or pancreatojejunostomy after pancreatoduodenectomy. Am J Surg. 2005;189(6):720–9.
Fernandez-Cruz L, Cosa R, Blanco L, Lopez-Boado MA, Astudillo E. Pancreatogastrostomy with gastric partition after pylorus-preserving pancreatoduodenectomy versus conventional pancreatojejunostomy: a prospective randomized study. Ann Surg. 2008;248(6):930–8.
Peng SY, Wang JW, Lau WY, Cai XJ, Mou YP, Liu YB, et al. Conventional versus binding pancreaticojejunostomy after pancreaticoduodenectomy: a prospective randomized trial. Ann Surg. 2007;245(5):692–8.
Bassi C, Falconi M, Molinari E, Mantovani W, Butturini G, Gumbs AA, et al. Duct-to-mucosa versus end-to-side pancreaticojejunostomy reconstruction after pancreaticoduodenectomy: results of a prospective randomized trial. Surgery. 2003;134(5):766–71.
Tran K, Van Eijck C, Di Carlo V, Hop WC, Zerbi A, Balzano G, et al. Occlusion of the pancreatic duct versus pancreaticojejunostomy: a prospective randomized trial. Ann Surg. 2002;236(4):422–8.
Winter JM, Cameron JL, Campbell KA, Chang DC, Riall TS, Schulick RD, et al. Does pancreatic duct stenting decrease the rate of pancreatic fistula following pancreaticoduodenectomy? Results of a prospective randomized trial. J Gastrointest Surg. 2006;10(9):1280–90.
Lillemoe KD, Cameron JL, Kim MP, Campbell KA, Sauter PK, Coleman JA, et al. Does fibrin glue sealant decrease the rate of pancreatic fistula after pancreaticoduodenectomy? Results of a prospective randomized trial. J Gastrointest Surg. 2004;8(7):766–72.
de Castro SM, Kuhlmann KF, Busch OR, van Delden OM, Lameris JS, van Gulik TM, et al. Incidence and management of biliary leakage after hepaticojejunostomy. J Gastrointest Surg. 2005;9(8):1163–71.
Koch M, Garden OJ, Padbury R, Rahbari NN, Adam R, Capussotti L, et al. Bile leakage after hepatobiliary and pancreatic surgery: A definition and grading of severity by the International Study Group of Liver Surgery. Surgery. 2011;149(5):680–8.
Winter JM, Cameron JL, Yeo CJ, Lillemoe KD, Campbell KA, Schulick RD. Duodenojejunostomy leaks after pancreaticoduodenectomy. J Gastrointest Surg. 2008;12(2):263–9.
Jagad RB, Koshariya M, Kawamoto J, Chude GS, Neeraj RV, Lygidakis NJ. Postoperative hemorrhage after major pancreatobiliary surgery: an update. Hepatogastroenterology. 2008;55(82–83):729–37.
Puppala S, Patel J, McPherson S, Nicholson A, Kessel D. Hemorrhagic complications after Whipple surgery: imaging and radiologic intervention. AJR Am J Roentgenol. 2011;196(1):192–7.
Yekebas EF, Wolfram L, Cataldegirmen G, Habermann CR, Bogoevski D, Koenig AM, et al. Postpancreatectomy hemorrhage: diagnosis and treatment: an analysis in 1669 consecutive pancreatic resections. Ann Surg. 2007;246(2):269–80.
de Castro SM, Kuhlmann KF, Busch OR, van Delden OM, Lameris JS, van Gulik TM, et al. Delayed massive hemorrhage after pancreatic and biliary surgery: embolization or surgery? Ann Surg. 2005;241(1):85–91.
Limongelli P, Khorsandi SE, Pai M, Jackson JE, Tait P, Tierris J, et al. Management of delayed postoperative hemorrhage after pancreaticoduodenectomy: a meta-analysis. Arch Surg. 2008;143(10):1001–7.
Wei HK, Wang SE, Shyr YM, Tseng HS, Tsai WC, Chen TH, et al. Risk factors for post-pancreaticoduodenectomy bleeding and finding an innovative approach to treatment. Dig Surg. 2009;26(4):297–305.
Yeo CJ, Barry MK, Sauter PK, Sostre S, Lillemoe KD, Pitt HA, et al. Erythromycin accelerates gastric emptying after pancreaticoduodenectomy. A prospective, randomized, placebo-controlled trial. Ann Surg. 1993;218(3):229–37.
Abell TL, Camilleri M, Donohoe K, Hasler WL, Lin HC, Maurer AH, et al. Consensus recommendations for gastric emptying scintigraphy: a joint report of the American Neurogastroenterology and Motility Society and the Society of Nuclear Medicine. Am J Gastroenterol. 2008;103(3):753–63.
van Berge Henegouwen MI, Akkermans LM, van Gulik TM, Masclee AA, Moojen TM, Obertop H, et al. Prospective, randomized trial on the effect of cyclic versus continuous enteral nutrition on postoperative gastric function after pylorus-preserving pancreatoduodenectomy. Ann Surg. 1997;226(6):677–85.
Kawai M, Tani M, Hirono S, Miyazawa M, Shimizu A, Uchiyama K, et al. Pylorus ring resection reduces delayed gastric emptying in patients undergoing pancreatoduodenectomy: a prospective, randomized, controlled trial of pylorus-resecting versus pylorus-preserving pancreatoduodenectomy. Ann Surg. 2011;253(3):495–501.
Diener MK, Knaebel HP, Heukaufer C, Antes G, Buchler MW, Seiler CM. A systematic review and meta-analysis of pylorus-preserving versus classical pancreaticoduodenectomy for surgical treatment of periampullary and pancreatic carcinoma. Ann Surg. 2007;245(2):187–200.
Diener MK, Fitzmaurice C, Schwarzer G, Seiler CM, Antes G, Knaebel HP, et al. Pylorus-preserving pancreaticoduodenectomy (pp Whipple) versus pancreaticoduodenectomy (classic Whipple) for surgical treatment of periampullary and pancreatic carcinoma. Cochrane Database Syst Rev. 2011;5, CD006053.
Karanicolas PJ, Davies E, Kunz R, Briel M, Koka HP, Payne DM, et al. The pylorus: take it or leave it? Systematic review and meta-analysis of pylorus-preserving versus standard whipple pancreaticoduodenectomy for pancreatic or periampullary cancer. Ann Surg Oncol. 2007;14(6):1825–34.
Iqbal N, Lovegrove RE, Tilney HS, Abraham AT, Bhattacharya S, Tekkis PP, et al. A comparison of pancreaticoduodenectomy with extended pancreaticoduodenectomy: a meta-analysis of 1909 patients. Eur J Surg Oncol. 2009;35(1):79–86.
Michalski CW, Kleeff J, Wente MN, Diener MK, Buchler MW, Friess H. Systematic review and meta-analysis of standard and extended lymphadenectomy in pancreaticoduodenectomy for pancreatic cancer. Br J Surg. 2007;94(3):265–73.
Yeo CJ, Cameron JL, Lillemoe KD, Sohn TA, Campbell KA, Sauter PK, et al. Pancreaticoduodenectomy with or without distal gastrectomy and extended retroperitoneal lymphadenectomy for periampullary adenocarcinoma, part 2: randomized controlled trial evaluating survival, morbidity, and mortality. Ann Surg. 2002;236(3):355–66.
Gangavatiker R, Pal S, Javed A, Dash NR, Sahni P, Chattopadhyay TK. Effect of antecolic or retrocolic reconstruction of the gastro/duodenojejunostomy on delayed gastric emptying after pancreaticoduodenectomy: a randomized controlled trial. J Gastrointest Surg. 2011;15(5):843–52.
Tani M, Terasawa H, Kawai M, Ina S, Hirono S, Uchiyama K, et al. Improvement of delayed gastric emptying in pylorus-preserving pancreaticoduodenectomy: results of a prospective, randomized, controlled trial. Ann Surg. 2006;243(3):316–20.
Kollmar O, Moussavian MR, Richter S, de Roi P, Maurer CA, Schilling MK. Prophylactic octreotide and delayed gastric emptying after pancreaticoduodenectomy: results of a prospective randomized double-blinded placebo-controlled trial. Eur J Surg Oncol. 2008;34(8):868–75.
Aoki H, Takakura N, Shiozaki S, Matsukawa H. Milk-based test as a preventive method for chylous ascites following pancreatic resection. Dig Surg. 2010;27(5):427–32.
Assumpcao L, Cameron JL, Wolfgang CL, Edil B, Choti MA, Herman JM, et al. Incidence and management of chyle leaks following pancreatic resection: a high volume single-center institutional experience. J Gastrointest Surg. 2008;12(11):1915–23.
van der Gaag NA, Verhaar AC, Haverkort EB, Busch OR, van Gulik TM, Gouma DJ. Chylous ascites after pancreaticoduodenectomy: introduction of a grading system. J Am Coll Surg. 2008;207(5):751–7.
D'Hondt M, Foubert K, Penninckx F, Aerts R. Lymphangiography as a Treatment Method for Chylous Ascites Following Pancreaticoduodenectomy. Cancer: J Gastrointest; 2010.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer-Verlag London
About this chapter
Cite this chapter
Tol, J.A.M.G., van Gulik, T.M., Busch, O.R.C., Gouma, D.J. (2014). Prevention and Treatment of Major Complications After Duodeno-pancreatic Head Surgery. In: Cuesta, M., Bonjer, H. (eds) Treatment of Postoperative Complications After Digestive Surgery. Springer, London. https://doi.org/10.1007/978-1-4471-4354-3_14
Download citation
DOI: https://doi.org/10.1007/978-1-4471-4354-3_14
Published:
Publisher Name: Springer, London
Print ISBN: 978-1-4471-4353-6
Online ISBN: 978-1-4471-4354-3
eBook Packages: MedicineMedicine (R0)