Abstract
The longer mean survival of oncological patients has led to an increased incidence of chemotherapy-induced cardiomyopathy. Anthracyclines and trastuzumab are the two most commonly implicated agents. Anthracyclines cause irreversible type I cardiomyopathy, where as, trastuzumab causes a potentially reversible type II cardiomyopathy. The most important risk factors are the total cumulative dose and pre-existing cardiovascular disease. MUGA scan and transthoracic echocardiogram are the most commonly used modalities to evaluate left ventricular function. Routine screening must be performed in all patients receiving cardiotoxic drugs. Early detection and treatment is critical for improved long-term cardiovascular prognosis. Patients with cardiomyopathy should be treated with standard heart failure therapy and treatment should be initiated as early as possible. Cardiac resynchronization therapy and heart transplant are viable options for patients with advanced heart failure. There is a great need for more research in this field with goals to develop drugs and protocols with lower cardiotoxicity, which still maintain antitumor efficacy; to develop biomarkers and imaging techniques for early detection of cardiac dysfunction; and to develop better management strategies of patients with cardiomyopathy. Creation of dedicated cardiac-oncology centers is essential for an improved future in this field.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
The survival of patients diagnosed with malignancy has improved drastically over the last few decades [1]. This has led to increased recognition of adverse events related to chemotherapeutic drugs, especially cardiovascular effects. Cardiovascular disease is the 2nd most common cause of mortality in these patients after the malignancy itself [2]. Cardiomyopathy is the most common cardiovascular side effect of chemotherapy. Various chemotherapeutic agents have been associated with the development of cardiomyopathy. A detailed list of these agents is provided in Table 13.1.
Chemotherapy-induced cardiomyopathy has been broadly classified into two types- Type I (non-reversible) and Type II (reversible) [3]. However, this distinction is not always mutually exclusive- type II dysfunction may not always be reversible and type I may reverse with cessation of the offending agent and heart failure (HF) therapy. Also, both types may co-exist, especially in patients receiving more than one cardiotoxic drug. Differences between type I and II cardiomyopathy are described in Table 13.2.
Definition
The definition of chemotherapy-induced cardiomyopathy has not been precisely defined. Various trials have employed different definitions of this entity. The Cardiac Review and Evaluation Committee (CRCE) has established the following criterion to diagnose chemotherapy induced cardiac dysfunction [4]:
-
1.
Decrease in left ventricular ejection fraction (LVEF), which is either global or worse in the septum
-
2.
Symptoms of congestive heart failure
-
3.
Signs of congestive heart failure, including but not limited to, S3 gallop, tachycardia or both
-
4.
A symptomatic decline in LVEF of at least 5 % or asymptomatic decline in LVEF of at least 10 % to an absolute LVEF of <55 %
Anthracyclines
Anthracyclines still remain the cornerstone of many modern chemotherapeutic regimens, with doxorubicin being the most widely used agent. These agents intercalate between specific bases in the DNA and inhibit DNA and RNA synthesis. Cardiotoxicity with these agents was recognized very early and found to be dose-dependent [5]. Initial studies, performed in 1970s, recommended a maximum total doxorubicin dose 550 mg/m2 [6]. However, these studies were limited by lack of evaluation for asymptomatic LV dysfunction. Recent studies report incidence of LV dysfunction to be as high as 50 % with long-term follow up [7]. Swain et al. [8] reported incidence of cardiomyopathy at 5 %, 16 % and 26 % respectively, with cumulative doses of 400, 500 and 550 mg/m2. Hence, currently the cumulative dose is usually limited to 400–450 mg/m2. However, there is no safe dose and cardiomyopathy has been reported with doses as low as 250 mg/m2, especially in children [9].
Three different manifestations of anthracycline-mediated cardiotoxicity have been described [10]:
-
1.
Acute — Acute cardiotoxicity is rare, occurring in <1 % patients and manifests within hours to weeks as arrhythmias, acute heart failure, myocardial ischemia, or pericarditis/myocarditis-like syndrome. Most patients recover completely from this acute cardiotoxicity. However, long terms effects are not known.
-
2.
Early-onset chronic — This manifestation occurs within the 1st year of treatment and incidence is reported at 1.6–2.1 %. It typically presents as dilated cardiomyopathy and may persist, or even progress, after discontinuation of the offending agent.
-
3.
Late-onset chronic — This is the most common form and is seen in about 1.6–5 % patients. It typically occurs years after chemotherapy and presents as progressive dilated cardiomyopathy, heart failure, or arrhythmias.
Various risk factors have been described for the development of anthracycline-mediated cardiomyopathy (Table 13.3) [11]. The most important risk factor is the total cumulative dose. Other major risk factors include extremes of age, pre-existing cardiovascular disease, concomitant use of other cardiotoxic drugs and chest irradiation.
Anthracyclines produce progressive and irreversible type I cardiomyopathy. Cardiac biopsy typically shows patchy areas of interstitial fibrosis, vacuolation and rarely frank necrosis [12]. The pathophysiology of anthracycline-medicated cardiomyopathy is not clearly understood and multiple mechanisms have been hypothesized [13]. The most commonly accepted hypothesis is generation of excessive reactive oxygen species (ROS) and free radical induced myocyte damage. Various mechanisms have been hypothesized for excess free radical production, including mitochondrial dysfunction, increased endothelial nitric oxide synthase production, iron dependent redox cycling, and NAD(P)H dependent mechanisms [13]. However, recent literature suggests that the ROS hypothesis may not fully explain the anthracycline-induced cardiotoxicity [13]. Other hypothesized mechanisms include inhibition of topoisomerase II, DNA cross-linking, decreased ATP production, direct damage to the mitochondria and cell membranes, and increased apoptosis.
Several attempts have been made to reduce doxorubicin cardiotoxicity:
-
1.
Structural modification of anthracyclines —
Many studies have focused on the development of chemotherapeutic agents, with reduced cardiotoxicty, while preserving antitumor efficacy. Unfortunately, thus far, the development of such an agent has remained unsuccessful. Epirubicin drew initial interest due to its reduced cardiotoxicity when compared mg-for-mg with doxorubicin. However, subsequent studies demonstrated epirubicin as a less potent chemotherapeutic agent compared to doxorubicin with similar cardiotoxicity at functionally equivalent doses of epirubicin [14].
-
2.
Different vehicle —
A liposomal-encapsulated doxorubicin remains restricted to the circulating blood and does not cross capillary junctions into normal organs. However, it easily penetrates into the tumor due to increased capillary permeability. It has been shown to reduce cardiotoxicity while still retaining its anti-neoplastic effects [15]. However, more data is still required and increased cost limits its use.
-
3.
Different protocols —
Continuous infusion reduces the risk of cardiotoxicity by decreasing the peak level of the drug [16]. However, it is associated with increased cost, need for an indwelling catheter and increased inconvenience to the patient. There is also a concern for reduction in antineoplastic effects.
Trastuzumab
Trastuzumab is a monoclonal antibody active against human epidermal growth factor (HER2) receptor, which is overexpressed in 25 % of breast cancers. However, trastuzumab significantly increases the risk of cardiomyopathy. A meta-analysis of randomized clinical trials with use of trastuzumab as an adjuvant chemotherapeutic agent showed a 1.6 % absolute increase in incidence of symptomatic heart failure and 7.2 % increase in LV systolic dysfunction [17]. Another trial in patients with metastatic breast cancer showed a 19 % increased risk of cardiomyopathy when trastuzumab was used in combination with anthracycline and cyclophosphamide, and a 12 % increased risk when added to paclitaxel [18]. Analysis of the SEER-Medicare database showed a 32.1 % incidence of cardiomyopathy in patients receiving trastuzumab and a 41.9 % incidence in patients receiving anthracycline plus trastuzumab, which is much higher than previously reported trials [19]. Most protocols recommend use of trastuzumab sequentially with anthracyclines. However, even sequential use is associated with an increased risk of cardiomyopathy, though much less than concomitant use [20] (See Table 13.4).
Trastuzumab produces type II cardiomyopathy, which is not dose dependent and potentially reversible. There is no visible myocyte damage on histology and changes are visible only on electron microscopy [21]. Some authors have re-challenged patients with trastuzumab without recurrence of cardiomyopathy in most patients [4]. However, many authors have questioned its reversible nature and reported a 20–40 % incidence of persistent LV dysfunction [22]. MRI studies have shown evidence of delayed gadolinium enhancement despite recovery of cardiac function, suggesting persistent myocardial damage [23]. Long-term studies are needed to better define the natural history of trastuzumab-induced cardiomyopathy.
The mechanism of trastuzumab-induced cardiomyopathy is not well understood, but inhibition of ErbB2 is thought to be the main mechanism. ErbB2 is a critical component of multiple anti-apoptotic pathways and is necessary for myocyte survival and repair. Trastuzumab binds to the ErbB2 on cardiac myocytes and blocks the cardioprotective ErbB2-ErbB4 signaling pathway [24]. Removal of trastuzumab leads of resumption of these pathways and recovery of cardiac damage. The synergistic cardiotoxic effects of anthracycline and trastuzumab can be explained by myocyte damage due to anthracyclines and blockage of repair mechanisms by trastuzumab [25].
A few approaches to reduce trastuzumab-induced cardiotoxicity are under investigation:
-
1.
Second generation monoclonal antibodies —
Lapatinib, a HER1 and HER2 receptor inhibitor, appears to be associated with much lower risk of cardiomyopathy than trastuzumab [26]. Other second-generation anti-HER2 therapies are being developed and three agents – neratinib, trastuzumab-DM1 and pertuzumab, are currently under investigation.
-
2.
Anthracycline-sparing protocols —
The BCIRG 006 trial demonstrated that the anthracycline-sparing chemotherapy protocols with trastuzumab alone were associated with significantly decreased risk of cardiomyopathy while preserving antitumor efficacy [27]. However, data regarding anti-neoplastic efficacy without anthracyclines is still conflicting [28].
-
3.
Shorter treatment duration —
Preliminary data shows that shorter regimens of trastuzumab are associated with a lower incidence of cardiomyopathy [29]. However, larger long-term studies are required to assess cardiotoxicity and anti-tumor efficacy.
Alkylating Agents
Cyclophosphamide is activated in the liver and its active metabolite crosslinks DNA, disrupting cell division. It has been associated with increased risk of cardiomyopathy, especially in combination with an anthracycline or cisplatin [30]. Other risk factors include advanced age and mediastinal irradiation. The mechanism of cardiotoxicity is not very well established and appears to be related to the strength of the individual dose, rather than cumulative dose [30]. Ifosamide has also been rarely associated with cardiomyopathy [31].
Antimicrotubule Agents
Paclitaxel, alone, has not been implicated as a cause of cardiomyopathy. However, it reduces the elimination of doxorubicin and increases its toxicity [32]. Paclitaxel should be avoided immediately before doxorubicin administration and within the next hour. The most common cardiovascular side-effect of paclitaxel is transient asymptomatic bradycardia [33].
Flouropyramidines
5-Flourouracil (5-FU) and its oral prodrug capecitabine have been associated with cardiotoxicity. The most common cardiac side effect is myocardial ischemia, likely related to coronary vasospasm [34]. Cardiomyopathy from these agents is rare and limited to a few case reports. It appears to have a type II pattern, with recovery of cardiac function in most cases after cessation of the agent [35].
Angiogenesis Inhibitors
Bevacizumab is a recombinant monoclonal antibody against the vascular endothelial growth factor (VEGF) receptor. It has primarily been associated with an increased risk of thrombotic events. The risk of cardiomyopathy is very low and follows the reversible type II pattern [36]. The most probable hypothesis is the loss of protective effects of VEGF against endothelial dysfunction caused by excess oxidative stress.
Tyrosine Kinase Inhibitors
The most common cardiovascular effect of tyrosine kinase inhibitors is hypertension. Sunitinib has been associated with a 6–8 % incidence of HF and up to a 19 % incidence of cardiomyopathy, especially in patients with pre-existing coronary artery disease and cardiac risk factors, like hypertension [37]. Imatinib, an inhibitor of the Bcr-Abl protein, is used in the treatment of chronic myelogenous leukemia and has been associated with HF as well [38]. It is hypothesized to induce cardiotoxicity by the activation of the endoplasmic reticulum stress response pathways. Electron microscopy of cardiac biopsies demonstrates membrane whorls, pleomorphic mitochondria, effaced cristae, glycogen accumulation, lipid droplets, and vacuoles [38]. However, data is limited to animal studies and a few small case series.
Diagnosis
Traditionally, the detection of cardiotoxicity has relied on detection of reduction in LVEF. Multiple-gated acquisition (MUGA) scan and transthoracic echocardiography are the two most commonly used modalities. Baseline LVEF should always be obtained before initiation of chemotherapy. The values obtained from different modalities are not interchangeable and, hence, the same modality should continually be used throughout the chemotherapy protocol for an assessment and comparison of LVEF.
MUGA Scan
Historically, MUGA scan has been the modality of choice to assess LVEF prior recent advances in echocardiography. MUGA scan has the advantage of lower inter-observer variability and generation of an exact LVEF number [39]. However, it exposes the patients to ionizing radiation (approximately 7.8 mSv/exam) [40] and does not provide any information regarding valvular disorders, pericardial diseases, and diastolic parameters. Currently, most centers use echocardiography as the primary modality for LVEF assessment. MUGA scan continues to be used at many centers due to the oncologists’ familiarity with the test and interpretation of its results. MUGA scan use should be limited in patients with poor acoustic windows or with pre-existing cardiomyopathy prior to the initiation of chemotherapy.
Transthoracic Echocardiography
Transthoracic echocardiography is the most commonly used modality for assessment of LVEF in patients receiving chemotherapy. Echocardiography is readily accessible, portable, inexpensive, and does not expose patients to ionizing radiation. It also provides additional information regarding valvular disorders, diastolic dysfunction, and pericardial disorders. Its disadvantages include larger inter-observer variability, dependence on complex geometric models and lack of good acoustic windows in many patients. Inter-observer variability and need for assumptions regarding ventricular geometry can be reduced by using 3D transthoracic echocardiography [41]. A small study with real time 3D transthoracic echocardiogram showed good correlation with MRI and MUGA scans in patients receiving chemotherapy [23]. Poor acoustic windows can be improved by the use of contrast agents, which better delineate the endocardial borders and reduce intra- and inter-observer variability [42]. Ideally, 3D echocardiography or contrast-enhanced echocardiography should be used as the modality of choice in screening patients for chemotherapy-induced cardiomyopathy.
Multiple indices of diastolic function have been evaluated in patients undergoing cardiotoxic chemotherapy [43]. Diastolic dysfunction usually precedes systolic dysfunction and early detection can potentially reduce the future risk of cardiomyopathy. However, none of the diastolic parameters have been found to have any significant association with development of future cardiac dysfunction [44].
Another modality used for early detection of cardiac dysfunction is the assessment of cardiac reserve by exercise or pharmacological stress echocardiography. Small studies have shown that reduction in cardiac reserve can be seen as early as after first cycle of chemotherapy and it can predict future cardiovascular events [45]. However, data regarding use of stress echocardiography are very limited.
The newest development in echocardiography is speckled and strain imaging. Multiple small trials have shown that these modalities can detect systolic dysfunction earlier than standard parameters and predict long term development of cardiomyopathy [46, 47]. Larger trials are still required before these modalities become standard of care. The major concern with these highly sensitive techniques is that many patients may never develop clinically significant cardiac dysfunction and life-saving therapies may be withheld unnecessarily.
Endomyocardial Biopsy
An endomyocardial biopsy can show typical features of cell damage from agents with type I cardiotoxicity. It was the gold standard to diagnose chemotherapy-induced cardiotoxicity. Billingham et al. [12] performed the pivotal trials assessing the histopathological changes following anthracycline exposure and developed a four point scoring system to characterize the extent of myocardial damage. However, it is an invasive procedure with significant risks and is not routinely used these days, especially with recent advances in other modalities of non-invasive imaging.
Cardiac MRI
Cardiac MRI (CMR) is currently the gold standard for assessment of LVEF [48]. CMR can also identify regions of non-transmural cardiac injury by delayed gadolinium enhancement. Anthracycline-induced cardiomyopathy characteristically demonstrates a delayed enhancement in the anterolateral wall and trastuzumab-induced cardiomyopathy shows a subepicardial delayed enhancement in the lateral wall [23]. CMR also provides detailed structural information, including right-sided chambers. However, CMR is not widely available and is expensive. CMR cannot be used in patients with metal devices or implants and gadolinium use is contraindicated in patients with reduced renal function.
Cardiac Biomarkers
Reduction in LVEF is a late development in the cascade of development of cardiomyopathy and early identification is critical. Several cardiac biomarkers have been studied to identify early cardiac damage. However, utmost caution must be exercised as a false positive result can withhold lifesaving therapy. A good biomarker must be easy to measure, accurate, reproducible, and most importantly, should have high specificity to limit likelihood of false positive results. Biomarkers should be used as an adjunct to the previously described modalities of cardiac assessment [49].
Troponin I is the most studied biomarker as a predictor of development of cardiomyopathy. Elevation of troponin I levels can predict cardiac damage earlier than currently used modalities [50]. One study involving 703 patients receiving anthracyclines showed a 30 % incidence of troponin I elevation and 9 % patients had persistent elevation even at 1 month [51]. Biomarker measurements were done before starting chemotherapy and immediately after. The testing was repeated at 12, 24, 36 and 72 h and again at 1 month. Cardiovascular endpoints were seen in 1 %, 37 % and 84 % patients, respectively, in troponin I negative, transient positive and persistent troponin I positive patients at 1 month. The positive and negative predictive value of troponin I was 84 % and 99 %, respectively. However, this has not been validated in repeated larger trials. A consensus regarding optimal timing of troponin I measurement has also not been reached.
Serum atrial natriuretic peptide (ANP), B-type natriuretic peptide (BNP) and N-terminal proBNP (NT-proBNP) have not been validated as a screening tool in patients receiving cardiotoxic drugs [52, 53]. The studies with these markers have been small, heterogeneous, single center trials and results have been conflicting. A few newer biomarkers have also shown promise in identification of cardiac damage, including, heart-type fatty acid-binding protein (H-FABP) [54] and glycogen phosphorylase BB (GPBB) [55].
Screening
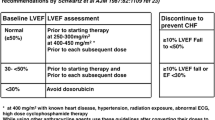
Screening guidelines have been published by various societies for anthracycline and trastuzumab-induced cardiomyopathy. However, there is a lack of consensus amongst various guidelines. Nuclear cardiology guidelines regarding screening for anthracycline-mediated cardiomyopathy are shown in Table 13.5 [56]. The Children’s Oncology Group’s Long-Term Follow-up Guidelines for Survivors of Childhood, Adolescent, and Young Adult Cancers (COG LTFU guidelines) recommend assessment of LV function by either echocardiogram or MUGA scan every 1–5 years (depending on the presence of risk factors for cardiotoxicity) [57].
The screening guidelines for trastuzumab-induced cardiomyopathy are slightly different. The National Comprehensive Cancer Network Guidelines recommend LVEF assessment at baseline and then every 3 months for the duration of chemotherapy [58]. The Cardiac Guideline Consensus Committee suggests that LVEF can be assessed every 3 months if EF is greater than 40 %. If the LVEF is less than 40 %, trastuzumab should be withheld and LVEF assessment should be done every month [59].
Cardiac Protection
All patients receiving chemotherapy are considered at risk for development of HF. The most useful method to reduce cardiotoxicity is by limiting the cumulative dose and avoiding the co-administration of multiple cardiotoxic drugs. Anthracycline-induced cardiomyopathy is thought to be primarily due to free radical production and many anti-oxidants have been studied to provide cardioprotection. However, data for most of these compounds have been discrepant and disappointing. Dexrazoxane, an iron chelator, is the only FDA approved agent for cardioprotection during anthracycline therapy [60]. A Cochrane meta-analysis showed significant benefit of dexrazoxane in prevention of cardiotoxicity with a hazard ratio of 0.29 (95 % CI 0.20–0.41) [61]. It has been shown to reduce subclinical myocyte damage during chemotherapy as well, as evidenced by reduced incidence of troponin I elevation. However, there are some concerns regarding the reduction of anti-tumor efficacy by anthracyclines, increased myelosuppression and higher risk of second malignancy [61]. Therefore, current guidelines recommend use of dexrazoxane only in patients who have already received ≥300 mg/m2 of doxorubicin and would benefit from further doses of doxorubicin. Dexrazoxane is not approved for use in children.
There has been limited data regarding role of standard HF drugs as cardioprotective agents. Small studies with use of carvedilol and valsartan have shown some cardioprotective effect [62, 63]. Cardinale et al. [64] randomized patients with positive troponin I levels at 1 month after chemotherapy to enalapril and placebo. The study found no reduction in LVEF in patients receiving enalapril, compared with a 43 % incidence in the control group. The recently published OVERCOME trial showed a small, but statistically significant benefit in preserving LVEF with prophylactic administration of enalapril and carvedilol [65]. However, larger multi-center trials are still needed. Many other agents are being evaluated as cardioprotective agents during chemotherapy.
Management
Data regarding management of chemotherapy-induced cardiomyopathy is limited and there are no well-defined recommendations. Most patients with cancer are excluded from major trials and, if included, they form a very small percentage of patients in most large trials. Traditionally, these patients were believed to respond poorly to standard HF therapy and had a very poor prognosis with 2-year mortality up to 60 % [66]. However, these historic beliefs were based on studies with diuretics and digitalis as the mainstay of HF therapy. Currently, patients with chemotherapy-induced cardiomyopathy should be treated with the same guidelines as other causes of cardiomyopathy. Although ACE inhibitors, ARBs and beta-blockers have never been systematically studied in these patients, these agents should be prescribed in every patient, if possible, and titrated up to the maximal tolerated dose. Recent trials show that the most critical variable for recovery of LVEF is the time to initiation of HF therapy. Cardinal et al. [67] showed the likelihood of LVEF recovery are highest if HF therapy is started within 2 months, compared to no chances of complete recovery if started after 6 months and not even partial recovery if started after 12 months. They found an approximately fourfold decrease in chances of complete recovery with doubling of time to initiation of HF therapy.
Small studies have shown significant benefit of cardiac resynchronization therapy (CRT) in patients meeting criterion [68]. A larger trial regarding use of CRT in these patients called MADIT-CHIC (Multicenter Automated Defibrillator Implantation Trial- Chemotherapy Induced Cardiomyopathy) is currently ongoing and will provide further information regarding benefit of CRT in these patients [69].
Orthotopic heart transplant (OHT) is also an option for these patients after confirmed complete remission. Between October 1987 and October 2011, only 0.8 % transplants (total 453 transplants) were performed in the United States for doxorubicin-induced cardiomyopathy [70]. However, the number of OHT performed per year for chemotherapy-induced cardiomyopathy has been constantly increasing. There was no difference in all-cause mortality or mortality from malignancy between patients receiving OHT for chemotherapy-induced cardiomyopathy and all other causes of cardiomyopathy [70]. However, data regarding recurrence of malignancy or development of new malignancy is very limited. Data from the International Society of Heart and Lung Transplantation (ISHLT) Registry between January 2000 and December 2008 showed an increased risk of malignancy in patients with chemotherapy-induced cardiomyopathy compared to other causes of non-ischemic cardiomyopathy (5 % vs 2 % respectively, p value = 0.006) [71]. There was no effect on short or long-term survival and only 5 % cases of malignancy occurred within the 1st year of OHT with only one case of recurrence of breast cancer.
Patients with trastuzumab-induced cardiomyopathy should be assessed for recovery of LV function, with concomitant increase of guideline-proven HF medications. Most patients recover their cardiac function within 1–2 months. If LV function recovers, patients can be rechallenged with trastuzumab with careful monitoring. If the EF falls again, trastuzumab should be stopped and not reinitiated again unless it is the only lifesaving therapy [20].
Takotsubo Cardiomyopathy
Stress induced cardiomyopathy, also known as Takotsubo cardiomyopathy, is an acute reversible cardiomyopathy triggered by an acute stress [72]. Recently, there have been multiple reports of Takotsubo cardiomyopathy after chemotherapy. It has been reported with use of rituximab [73], 5-Flourouracil (5-FU) [74], vascular endothelial growth factor receptor antagonists, especially bevacizumab [75] and the tubulin-depolymerization agent combrestatin [76]. The strongest association appears to be with administration of 5-FU [72].
Cardiac-Oncology
The early detection and management of chemotherapy-induced cardiomyopathy will define the future of field of cardiac-oncology. Both cardiology and oncology are highly specialized fields and management of these overlapping, complicated disease processes requires the coordination of both specialists. Many signs and symptoms of heart failure are similar to side effects of chemotherapy and radiation, including fatigue, shortness of breath, dyspnea on exertion, lower extremity edema, etc. The decreased activity of patients undergoing chemotherapy can lead to a delay in the detection of cardiovascular disease in this patient population [77]. The management of these patients becomes even more difficult when patients pursue oncological and cardiovascular care at different institutions. In addition, the screening and management guidelines are not streamlined and contribute to confusion along with poor adherence to recommendations leading to mismanagement of early asymptomatic cardiomyopathy [78]. The outcomes can be drastically improved by collaborative efforts between the oncologists and cardiologists in management of these disease processes [79].
The other major issue in cardiac-oncology is to maintain a fine balance between management of malignancy and cardiovascular outcomes. The aim is to provide adequate anti-cancer therapy with minimal cardiovascular risks. However, due to lack of data and absence of clear guidelines, the decision to continue or withhold chemotherapeutic agent has to be individualized and requires communication between the patient, the oncologist and the cardiologist.
There is an urgent need for development and widespread use of cardiac-oncology centers. These centers can result in better communication, better decision-making and hopefully, better outcomes. Cardiac-oncology centers may provide specialized care in the future and will aim to provide the best quality oncological care, as well as, early detection and management of cardiac dysfunction.
References
Siegel R, DeSantis C, Virgo K, et al. Cancer treatment and survivorship statistics, 2012. CA Cancer J Clin. 2012;62:220–41.
Ning Y, Shen Q, Herrick K, et al. Cause of death in cancer survivors. Cancer Res. 2012;72:LB-339.
Khawaja MZ, Cafferkey C, Rajani R, et al. Cardiac complications and manifestations of chemotherapy for cancer. Heart. 2014;100:1133–40.
Seidman A, Hudis C, Pierri MK, et al. Cardiac dysfunction in the trastuzumab clinical trials experience. J Clin Oncol. 2002;20(5):1215–21.
Van Hoff DD, Layard MW, Basa P, et al. Risk factors for doxorubicin-induced congestive heart failure. Ann Intern Med. 1979;91:710–7.
Lefrak EA, Pitha J, Rosenheim S, et al. A clinicopathologic analysis of adriamycin cardiotoxicity. Cancer. 1973;32:302–14.
Steinherz LJ, Steinherz PG, Tan CT, et al. Cardiac toxicity 4 to 20 years after completing anthracycline therapy. JAMA. 1991;266:1672–7.
Swain SM, Whaley FS, Ewer MS. Congestive heart failure in patients treated with doxorubicin: a retrospective analysis of three trials. Cancer. 2003;97:2869–79.
Mulrooney DA, Yeazel MW, Kawashima T, et al. Cardiac outcomes in a cohort of adult survivors of childhood and adolescent cancer: retrospective analysis of Childhood Cancer Survivor Study Cohort. Br Med Journal. 2009;339:b4606.
Yeh ET, Bickford CL. Cardiovascular complications of cancer therapy: incidence, pathogenesis, diagnosis and management. J Am Coll Cardiol. 2009;53(24):2231–47.
Raj S, Franco VI, Lipshultz SE. Anthracycline-induced cardiotoxicity: a review of pathophysiology, diagnosis and treatment. Curr Treat Options Cardio Med. 2014;16:315.
Billingham M, Bristow M. Evaluation of anthracycline cardiotoxicity: predictive ability and functional correlation of endomyocardial biopsy. Cancer Treat Symp. 1984;3:71–6.
Octavia Y, Tocchetti CG, Gabrielson KL, et al. Doxorubicin-induced cardiomyopathy: from molecular mechanisms to therapeutic strategies. J Mol Cell Cardiol. 2012;52:1213–25.
Ryberg D, Nielsen D, Skovsgaard T, et al. Epirubicin cardiotoxicity: an analysis of 469 patients with metastatic breast cancer. J Clin Oncol. 1998;16:3502–8.
Robert NJ, Vogel CL, Henderson IC, et al. The role of the liposomal anthracyclines and other systemic therapies in the management of advanced breast cancer. Semin Oncol. 2004;31(6 Suppl 13):106–46.
Van Dalen EC, Van Der Pal HJ, Caron HN, et al. Different dosage schedules for reducing cardiotoxicity in cancer patients receiving anthracycline chemotherapy. Cochrane Database Syst Rev 2006;(4):CD005008.
Bria E, Cuppone F, Fornier M, et al. Cardiotoxicity and incidence of brain metastases after adjuvant trastuzumab for early breast cancer: the dark side of the moon? A meta-analysis of the randomized trials. Breast Cancer Res Treat. 2008;109:231–9.
Slamon DJ, Leyland-Jones B, Shak S, et al. Use of chemotherapy plus a monoclonal antibody against HER2 for metastatic breast cancer that overexpresses HER2. N Engl J Med. 2001;344:783–92.
Chen J, Long JB, Hurria A, et al. Incidence of heart failure or cardiomyopathy after adjuvant trastuzumab therapy for breast cancer. J Am Coll Cardiol. 2012;60:2504–12.
Suter TM, Procter M, Van Veldhuisen DJ, et al. Trastuzumab-associated cardiac adverse effects in herceptin adjuvant trial. J Clin Oncol. 2007;25:3859–65.
Guarneri V, Lenihan DJ, Valero V, et al. Long-term cardiac tolerability of trastuzumab in metastatic breast cancer: the M.D. Anderson Cancer Center Experience. J Clin Oncol. 2006;24:4107–15.
Procter M, Suter TM, de Azambuja E, et al. Longer-term assessment of trastuzumab-related cardiac adverse events in the Herceptin Adjuvant (HERA) trial. J Clin Oncol. 2010;28:3422–8.
Walker J, Bhullar N, Fallah-Rad N, et al. Role of three-dimensional echocardiography in breast cancer: comparison with two-dimensional echocardiography, multiple-gated acquisition scans and cardiac magnetic resonance imaging. J Clin Oncol. 2010;28(21):3429–36.
Force T, Krause DS, Van Etten RA. Molecular mechanisms of cardiotoxicity of tyrosine kinase inhibition. Nat Rev Cancer. 2007;7:332–44.
Tocchetti CG, Ragone G, Coppola C, et al. Detection, monitoring and management of trastuzumab-induced left ventricular dysfunction: an actual challenge. Eur J Heart Fail. 2012;14:130–7.
Geyer CE, Forster J, Lindquist D, et al. Lapatinib plus capecitabine for HER2-positive advanced breast cancer. N Engl J Med. 2006;355:2733–43.
Slamon DJ, Eiermann W, Robert N, et al. Adjuvant trastuzumab in HER2-positive breast cancer. N Engl J Med. 2011;365(14):1273–83.
Castrellon AB, Gluck S. Adjuvant therapy for HER2 positive breast cancer: are anthracyclines still necessary? Clin Adv Hematol Oncol. 2008;6:666–72.
Joensuu H, Kellokumpu-Lehtinen PL, Bono P, et al. Adjuvant docetaxel or vinorelbine with or without trastuzumab for breast cancer. N Engl J Med. 2006;354:1260–6.
Dow E, Schulman H, Agura E. Cyclophosphamide cardiac injury mimicking acute myocardial infarction. Bone Marrow Transplant. 1993;12(2):169–72.
Quezado ZM, Wilson WH, Cunnion RE, et al. High-dose ifosfamide is associated with severe, reversible cardiac dysfunction. Ann Intern Med. 1993;118(1):31–6.
Biganzoli L, Cufer T, Bruning P, et al. Doxorubicin-paclitaxel: a safe regimen in terms of cardiac toxicity in metastatic breast carcinoma patients. Results from a European organization for research and treatment of cancer multicenter trial. Cancer. 2003;97:40–5.
Rowinsky EK, Donehower RC. Paclitaxel (taxol). N Engl J Med. 1995;332:1004–14.
Kosmas C, Kallistratos MS, Kopterides P, et al. Cardiotoxicity of flouropyrimidines in different schedules of administration: a prospective study. J Cancer Res Clin Oncol. 2008;134:75–82.
Sorrentino MF, Kim J, Foderaro AE, et al. 5-Flourouracil induced cardiotoxicity: review of the literature. Cartogr J. 2012;19(5):453–8.
Hawkes EA, Okines AFC, Plummer C, et al. Cardiotoxicity in patients treated with bevacizumab is potentially reversible. J Clin Oncol. 2011;29:e560–2.
Di Lorenzo G, Autorino R, Bruni G, et al. Cardiovascular toxicity follow sunitinib therapy in metastatic renal cell carcinoma: a multicenter analysis. Ann Oncol. 2009;20:1535–42.
Kerkela R, Grazette L, Yacobi R, et al. Cardiotoxicity of the cancer therapeutic agent imatinib mesylate. Nat Med. 2006;12(8):908–16.
Skrypniuk JV, Bailey D, Cosgriff PS, et al. UK audit of left ventricular ejection fraction estimation from equilibrium ECG gated blood pool images. Nucl Med Commun. 2005;26:205–15.
Mettler FA, Huda W, Yoshizumi TT, et al. Effective doses in radiology and diagnostic nuclear medicine: a catalog 1. Radiol. 248(1):254–63.
Sugeng L, Mor-Avi V, Weinert L, et al. Quantitative assessment of left ventricular size and function: side-by-side comparison of real-time three-dimensional echocardiography and computed tomography with magnetic resonance reference. Circulation. 2006;114:654–61.
Hoffman R, von Bardeleben S, Ten Cate F, et al. Assessment of systolic left ventricular function: a multi-center comparison of cineventriculography, cardiac magnetic resonance imaging, unenhanced and contrast-enhanced echocardiography. Eur Heart J. 2005;26:607–16.
Tjeerdsma G, Meinardi MT, WT v DG, et al. Early detection of anthracycline induced cardiotoxicity in asymptomatic patients with normal left ventricular systolic function: autonomic versus echocardiographic variables. Heart. 1999;81:419–23.
Radulescu D, Pripon S, Parv A, et al. Altered left ventricular diastolic performance in oncologic patients treated with epirubicin. Congest Heart Fail. 2007;13:215–20.
Civelli M, Cardinale D, Martinoni A, et al. Early reduction in left ventricular contractile reserve detected by dobutamine stress echo predicts high-dose chemotherapy-induced cardiac toxicity. Int J Cardiol. 2006;111:120–6.
Jurcut R, Wildiers H, Ganame J, et al. Strain rate imaging detects early cardiac effects of pegylated liposomal doxorubicin as adjuvant therapy in elderly patients with breast cancer. J Am Soc Echocardiogr. 2008;21:1283–9.
Sawaya H, Sebag I, Plana JC, et al. Early detection and prediction of cardiotoxicity in chemotherapy-treated patients. Am J Cardiol. 2011;107(9):1375–80.
Grothues F, Braun-Dullaeus R. Serial assessment of ventricular morphology and function. Heart Fail Clin. 2009;5(3):301–14.
Ky B, Carver JR. Biomarker approach to the detection and cardioprotective strategies during anthracycline chemotherapy. Heart Failure Clin. 2011;7:323–31.
Kilickap S, Barista I, Akgul E, et al. cTnT can be useful marker for early detection of anthracycline cardiotoxicity. Ann Oncol. 2005;16:798–804.
Cardinale D, Sandri MT, Colombo A, et al. Prognostic value of troponin I in cardiac risk stratification of cancer patients undergoing high-dose chemotherapy. Circulation. 2004;109:2749–54.
Horacek JM, Pudil R, Jebavy L, et al. Assessment of anthracycline-induced cardiotoxicity with biochemical markers. Exp Oncol. 2007;29(4):309–13.
Knobloch K, Tepe J, Lichtinghagen R, et al. Monitoring of cardiotoxicity during immunotherapy with Herceptin using simultaneous continuous wave Doppler depending on N-terminal pro-brain natriuretic peptide. Clio Med. 2007;7(1):88–9.
ElGhandour AH, ElSorady M, Azab S, et al. Human heart-type fatty acid-binding protein as an early diagnostic marker of doxorubicin cardiac toxicity. Hematology Rev. 2009;1:29–32.
Horacek JM, Tichy M, Pudil R, et al. Glycogen phosphorylase BB could be a new circulating biomarker for detection of anthracycline cardiotoxicity. Ann Oncol. 2008;19:1656–7.
Schwartz RG, McKenzie WB, Alexander I, et al. Congestive heart failure and left ventricular dysfunction complicating doxorubicin therapy: a seven year experience using serial radionuclide angiocardiography. Am J Med. 1987;82:1109–18.
Children’s Oncology Group. Long-term follow-up guidelines for survivors of childhood, adolescent, and young adult cancers. 2009, www.survivorshipguidelines.com.
National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology. Breast Cancer version 1. 2012.
Jones AL, Barlow M, Barrett-Lee PJ, et al. Management of cardiac health in trastuzumab treated patients with breast cancer: updated United Kingdom Nationa95l Cancer Research Institute recommendations for monitoring. Br J Cancer. 2009;100(5):684–92.
Lipshultz SE, Rifai N, Dalton VM, et al. The effect of dexrazoxane on myocardial injury in doxorubicin-treated children with acute lymphoblastic leukemia. N Engl J Med. 2004;351:145–53.
Van Dalen EC, Caron HN, Dickinson HO, et al. Cardioprotective interventions for cancer patients receiving anthracyclines. Cochrane Database Syst Rev 2008;(2):CD003917.
Kalay N, Basar E, Ozdogru I, et al. Protective effects of carvedilol against anthracycline-induced cardiomyopathy. J Am Coll Cardiol. 2006;48:2258–62.
Nakamae H, Tsumura K, Terada Y, et al. Notable effects of angiotension II receptor blocker, valsartan, on acute cardiotoxic changes after standard chemotherapy with cyclophosphamide, doxorubicin, vincristine, and prednisolone. Cancer. 2005;104:2492–8.
Cardinale D, Colombo A, Sandri MT, et al. Prevention of high-dose chemotherapy-induced cardiotoxicity in high-risk patients by angiotensin-converting enzyme inhibition. Circulation. 2006;114:2474–81.
Bosch X, Rovira M, Sitges M, et al. Enalapril and carvedilol for preventing chemotherapy-induced left ventricular systolic dysfunction in patients with malignant hemopathies. J Am Coll Cardiol. 2013;61:2355–62.
Felker GM, Thompson RE, Hare JM, et al. Underlying causes and long-term survival in patients with initially unexplained cardiomyopathy. N Engl J Med. 2000;342:1077–84.
Cardinale D, Colombo A, Lamantia G, et al. Anthracycline-induced cardiomyopathy. Clinical relevance and response to pharmacological therapy. J Am Coll Cardiol. 2010;55:213–20.
Rickard J, Kumbhani DJ, Baranowski B, et al. Usefulness of cardiac resynchronization therapy in patients with adriamycin-induced cardiomyopathy. Am J Cardiol. 2010;105(4):522–6.
Moss AJ. Multicenter Automated Defibrillator Implantation Trial- Chemotherapy Induced Cardiomyopathy (MADIT-CHIC). Clinicaltrials.gov/show/NCT02164721
Lenneman AJ, Wang L, Wigger M, et al. Heart transplant survival outcomes for adriamycin dilated cardiomyopathy. Am J Cardiol. 2013;111(4):609–12.
Oliveira GH, Hardaway BW, Kucheryavaya AY, et al. Characteristics and survival of patients with chemotherapy-induced cardiomyopathy undergoing heart transplantation. J Heart Lung Transplant. 2012;31:805–10.
Smith SA, Auseon AJ. Chemotherapy-induced Takotsubo cardiomyopathy. Heart Failure Clin. 2013;9:233–42.
Kanamori H, Tsutsumi Y, Mori A, et al. Delayed reduction in left ventricular function following treatment of non-Hodgkin’s lymphoma with chemotherapy and rituximab, unrelated to acute infusion reaction. Cardiology. 2006;105(3):184–7.
Grunwald MR, Howie L, Diaz Jr LA. Takotsubo cardiomyopathy and fluorouracil: case report and review of literature. J Clin Oncol. 2012;30(2):e11–4.
Franco TH, Khan A, Joshi V, et al. Takotsubo cardiomyopathy in two men receiving bevacizumab for metastatic cancer. Ther Clin Risk Manag. 2008;4(6):1367–70.
Bhakta S, Flick SM, Cooney MM, et al. Myocardial stunning following combined modality combrestatin-based chemotherapy: two case reports and review of literature. Clin Cardiol. 2009;32(12):e80–4.
Chen CL, Steingart R. Cardiac disease and heart failure in cancer patients: is our training adequate to provide optimal care? Heart Failure Clin. 2011;7:357–62.
Yoon GJ, Telli ML, Kao DP, et al. Left ventricular dysfunction in patients receiving cardiotoxic cancer therapies: are clinicans responding optimally? J Am Coll Cardiol. 2010;56:1644–50.
Albini A, Pennesi G, Donatelli F, et al. Cardiotoxicity of anticancer drugs: the need for cardio-oncology and cardio-oncological prevention. J Natl Cancer Inst. 2010;102(1):14–25.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer-Verlag London
About this chapter
Cite this chapter
Gupta, A., Eisen, H.J. (2017). Cardiac-Oncology: Management of the Patient with Heart Failure After Chemotherapy. In: Eisen, H. (eds) Heart Failure. Springer, London. https://doi.org/10.1007/978-1-4471-4219-5_13
Download citation
DOI: https://doi.org/10.1007/978-1-4471-4219-5_13
Published:
Publisher Name: Springer, London
Print ISBN: 978-1-4471-4218-8
Online ISBN: 978-1-4471-4219-5
eBook Packages: MedicineMedicine (R0)