Abstract
Patients with autoimmune pancreatitis (AIP) commonly present with vague abdominal pain, jaundice, or weight loss, and CT is often the first imaging study obtained. Characteristic CT findings of AIP include diffuse parenchymal enlargement of the pancreas and capsule-like rim. The pancreatic border commonly becomes featureless with effacement of the lobular contour of the pancreas. However, it may present as focal or segmental enlargement of the pancreas or low-density mass, and differentiation with pancreatic cancer may be difficult. Vascular involvement may be sometimes seen. Differentiation from pancreatic cancer can be difficult in such atypical cases. Enhancement pattern of pancreatic parenchyma (decreased enhancement during early phase and increased enhancement during delayed phase of contrast administration), lack of pancreatic duct dilatation, as well as presence of other organ (extrapancreatic) involvement are helpful findings in making the correct diagnosis of AIP. Other uncommon findings include pancreatic pseudocyst and calcification. FDG-PET and MRI with diffusion-weighted imaging may be helpful when CT findings are inconclusive.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Apparent Diffusion Coefficient
- Chronic Pancreatitis
- Pancreatic Duct
- Pancreatic Carcinoma
- Main Pancreatic Duct
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Introduction
Patients with autoimmune pancreatitis (AIP) commonly present with vague abdominal pain, jaundice, or weight loss, and contrast-enhanced computed tomography (CT) is often the first imaging study obtained. Radiological evaluation is crucial in making the correct diagnosis. Differentiating AIP from pancreatic cancer is the main goal to avoid unnecessary surgery or invasive intervention. One should be aware of various pancreatic and extrapancreatic manifestations of AIP in order to facilitate diagnosis.
Pancreatic Morphological Changes
Diffuse parenchymal enlargement of the pancreas is a characteristic feature of AIP seen in 24–73 % of patients (Figs. 5.1a, b, and 5.2) [1–5]. The pancreatic border becomes featureless with effacement of the lobular contour of the pancreas [2]. The pancreatic tail may become foreshortened [6]. On CT, the pancreas shows delayed enhancement during the late phase of contrast enhancement [1, 7]. On magnetic resonance imaging (MRI), the pancreas is diffusely hypointense on T1-weighted images, slightly hyperintense on T2-weighted images, and shows heterogeneous and diminished enhancement during the early phase with delayed increased enhancement during the late phase of contrast enhancement [1, 2, 8].
(a–d) A 68-year-old male with autoimmune pancreatitis. (a, b) Contrast-enhanced CT shows diffuse enlargement of the pancreas. Capsule-like rim is present around the tail of the pancreas. Enhancement of intrapancreatic portion of the bile duct is suggestive of biliary involvement. Note the intrahepatic biliary dilation. (c, d) Contrast-enhanced CT obtained after steroid treatment shows diffuse atrophy of the pancreas
Focal, mass-like enlargement of the pancreas is seen in 18–40 % of patients with AIP (Fig. 5.3) [2, 4, 5, 9]. Any portion of the pancreas can be involved, although involvement of the pancreatic head is more common [5, 10]. On CT, the enlarged segment of the pancreas typically demonstrates iso-attenuation compared to the non-enlarged segment of pancreatic parenchyma [2]. In a small number of cases, the focally enlarged segment is low attenuation compared to the uninvolved pancreatic parenchyma and may be indistinguishable from pancreatic cancer [2, 4, 9, 11]. The demarcation between the normal parenchyma tends to be sharp in such cases [11]. Atrophy of the pancreas upstream to the focally involved area is uncommon in patients with AIP in contrast to patients with pancreatic carcinoma. The pancreas may also appear as an area of segmental low density without mass-like enlargement. Multifocal pancreatic involvement is rare, but occasionally multiple low-attenuation lesions may be seen [12]. When the pancreas is focally enlarged, the normal appearing segment should be carefully examined, as the apparent normal area may cause biliary dilatation or may have abnormally decreased enhancement which are clues to the diagnosis.
The pancreas may appear normal in size or atrophic in 9–36 % of patients [3–5]. A normal-sized pancreas may result from a milder form of disease, but in such cases the enhancement pattern is usually altered [5]. Pancreatic atrophy is believed to represent a late burnt-out phase of the disease [2]. This appearance can also be seen after steroid therapy.
A capsule-like rim can been seen around the enlarged pancreas in 14–48 % of patients with AIP (Figs. 5.1a, and 5.2) [1, 2, 4, 5]. The capsule-like rim is low attenuation on contrast-enhanced CT and hypointense on both T1- and T2-weighted images and shows delayed enhancement on contrast-enhanced MR. The rim may diffusely surround the entire pancreas or only focal regions [5]. The rim is thought to represent peripancreatic extension of the characteristic inflammatory cell infiltration [1]. Mild peripancreatic stranding may also be present which is usually confined to the peripancreatic region with infrequent involvement of the mesentery and anterior pararenal fascia [2].
Enhancement Characteristics
The enhancement pattern is a useful adjunct to the morphological changes of the pancreas, which is assessed by contrast-enhanced CT or contrast-enhanced MRI using multiphasic technique. Irie et al. first described delayed enhancement in patients with diffuse changes of AIP; CT attenuation of the pancreas was higher at 6 min delayed scan compared to the 60 s delayed scan [1]. Qualitatively, CT attenuation of the pancreas in AIP is similar or higher than that of the liver and lower than that of spleen during the pancreatic phase and is similar or higher than that of the liver and higher than that of spleen in hepatic phase of biphasic CT [10, 13]. Quantitatively, mean CT attenuation value of the pancreatic parenchyma in AIP was significantly lower than that in normal controls during the pancreatic phase (AIP: 85 HU, normal pancreas: 104 HU; p < 0.05), but not significantly different in the hepatic phase (AIP: 96 HU, normal pancreas: 89 HU; p = 0.6) [7]. Similar enhancement pattern was observed on MR [8].
This enhancement pattern was also seen in patients with focal AIP: decreased enhancement during the pancreatic phase with delayed enhancement during the hepatic phase (Figs. 5.4a, b). On the other hand, pancreatic carcinoma shows decreased enhancement in the pancreatic phase with a minimal change in the enhancement in the hepatic phase (Figs. 5.5a, b). Wakabayashi et al. evaluated the CT enhancement pattern in 9 patients with focal AIP [9]. Of the 9 patients, 6 lesions were hypo-attenuating in the early phase but all were homogeneously iso-attenuating in the delayed phase. On the other hand, only 2 of 80 patients with pancreatic carcinoma had homogeneous enhancement in the delayed phase. Quantitatively, the mean CT attenuation value of focal AIP was not significantly different in the pancreatic phase (AIP: 71 HU, carcinoma: 59 HU; p = 0.06), but significantly higher than that in carcinoma in the hepatic phase (AIP: 90 HU, carcinoma: 64 HU; p < 0.001) [7]. Delayed enhancement of the mass or focally enlarged segment, defined as a 15-HU or greater increase from the pancreatic phase to the hepatic phase, was found in 7 of the 13 patients with focal AIP (54 %) and in 5 of 33 patients (15 %) with carcinoma (p = 0.02).
(a–c) A 30-year-old female with autoimmune pancreatitis, type II. (a, b) Contrast-enhanced MR images show segmental abnormality in the tail of the pancreas. The abnormal segment shows decreased enhancement during the early phase of contrast enhancement with delayed enhancement. (c) Diffusion-weighted images (ADC map) show restricted diffusion in abnormal segment
Diffusion-Weighted MR
Diffusion-weighted MR is a technique to evaluate the rate of microscopic water diffusion within tissues by using special magnetic gradients. Quantitative measurements of the diffusivity of water are described by the apparent diffusion coefficient. Kamisawa et al. showed that apparent diffusion coefficient values were significantly lower in AIP (1.01 ± 0.11 × 10(−3) mm(2)/s) than in pancreatic cancer (1.25 ± 0.11 × 10(−3) mm(2)/s) and normal pancreas (1.49 ± 0.16 × 10(−3) mm(2)/s) (P < 0.001) (Fig. 5.4c) [14]. Taniguchi et al. showed that apparent diffusion coefficient values were significantly lower in AIP (0.97 ± 0.18 × 10(−3) mm(2)/s) compared to other types of chronic pancreatitis (1.45 ± 0.10 × 10(−3) mm(2)/s) [15]. In addition, diffusion-weighted MR was helpful in reclassifying what appeared to be focal mass-forming AIP to diffuse AIP by showing diffusely decreased apparent diffusion coefficient values in the non-enlarged pancreatic segment.
Pancreatic Duct Changes
Diffuse or segmental narrowing of the main pancreatic duct is the characteristic ERCP finding [2, 16]. The pancreatic duct narrowing is often poorly seen on CT as the normal pancreatic duct is very small. MRCP is a preferred noninvasive method to assess the pancreatic ductal changes. Segmental narrowing of the main pancreatic duct may be seen as a poorly visualized segment on CT or MRCP compared to a normal-caliber pancreatic duct in uninvolved segments of pancreas [17, 18]. Mild pancreatic ductal dilation is commonly present upstream to the narrowed segment, and thus mild caliber changes of the main pancreatic duct are often detectable on CT or MR. The degree of main pancreatic duct dilation is usually milder than that seen in cases of pancreatic carcinoma. A relatively specific main pancreatic ductal change of AIP is multifocal narrowing, and this may be depicted on CT or MRCP [18, 19]. The duct-penetrating sign [20] may also be useful in differentiating AIP from pancreatic cancer. Secretin-stimulated MRCP may be helpful in the assessment of pancreatic duct-penetrating sign [19]. Enhancement of the pancreatic duct wall may be present in patients with AIP on portal phase or delayed phase CT [5].
Other Pancreatic and Peripancreatic Findings
Pancreatic pseudocyst and/or calcification is typically associated with alcohol-induced chronic pancreatitis [9]. However, calcifications are seen in 14–32 % and cysts are seen in 10–12 % of patients with AIP [4, 5], especially in the late or post-acute phase; therefore, presence of calcifications or cysts should not exclude the possibility of AIP [21, 22]. Pancreatic pseudocysts associated with AIP typically shrink after steroid therapy [22]. Vessels are commonly involved by the extension of peripancreatic soft tissue in patients with AIP (44–68 %). Vascular involvement may be either arterial such as superior mesenteric artery (10 %) or venous such as splenic vein or portal vein (58 %) [4, 5] . Involved veins are often narrowed but occlusion may occur [5].
Other Organ (Extrapancreatic) Involvement in the Abdomen
The most common site of extrapancreatic involvement is the biliary tree presenting with asy-mptomatic liver test abnormalities or jaundice [4]. On imaging, biliary involvement commonly appears as multifocal biliary strictures similar to primary sclerosing cholangitis. Rarely, it may form a mass which mimics cholangiocarcinoma. The kidneys are also commonly involved [23]. Radiographically, renal lesions are commonly bilateral and multiple, predominantly involving the renal cortex (Fig. 5.3b). Renal parenchymal lesions can be classified as small peripheral cortical nodules, round or wedge-shaped lesions, and diffuse patchy involvement. Renal lesions may present as a large solitary mass which mimic primary renal neoplasm. Retroperitoneal fibrosis is seen in 10 % of cases. Biliary or renal involvement and retroperitoneal fibrosis are exclusively seen in type 1 AIP. On the other hand, type 2 AIP is commonly associated with inflammatory bowel disease such as Crohn’s disease or ulcerative colitis [24].
Other Imaging Modalities
On PET, the pancreas shows increased 18F-fluorodeoxyglucose (FDG) uptake in almost all cases [25–29]. Although FDG uptake is commonly seen in pancreatic cancer (73–82 %), the pattern of uptake is usually different [26, 29]. FDG uptake in AIP is usually diffuse, segmental, or multifocal, while uptake in pancreatic carcinoma is usually focal. FDG uptake in extrapancreatic tissues such as the lacrimal gland, salivary gland, biliary tree, periaortic region, kidneys, prostate, and lymph nodes is common and specific for AIP [26, 27, 29]. On transabdominal US, the pancreas is diffusely or focally enlarged and hypoechoic. On contrast-enhanced US, the involved pancreatic segment commonly shows moderated to marked enhancement [30, 31].
Differentiating AIP from Pancreatic Malignancy and Other Types of Pancreatitis
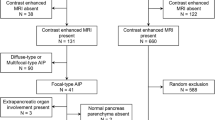
Differentiating AIP from pancreatic carcinoma on CT or MR can be difficult. AIP is one of the most common benign disease processes for which pancreatic resection is performed for suspected pancreatic carcinoma. AIP represents 31 % of tumefactive chronic pancreatitis patients who undergo pancreatic resection [32], and 2–6 % of patients who undergo pancreatic resection for suspected pancreatic cancer [32, 33]. Focal enlargement of the pancreas or low-attenuation mass formation is not uncommon in patients with AIP [2, 4, 9]. Moreover, pancreatic carcinoma may present as an iso-attenuating mass in approximately 10 % [34]. Findings that are useful in differentiating AIP from pancreatic carcinoma and its frequency are shown in Table 5.1 and Table 5.2 [35, 36]. Highly specific findings of AIP include diffuse pancreatic enlargement, capsule-like rim around the pancreas, other organ involvement (bile duct, kidney, retroperitoneum), and delayed enhancement of the pancreatic lesion. A low-density mass, distal pancreatic duct cutoff, or atrophy can be occasionally seen in AIP; given the much higher prevalence of pancreatic carcinoma, presence of such findings are highly suggestive of pancreatic carcinoma.
Although diffuse enlargement of the pancreas is highly suggestive of AIP, it is not without differential diagnosis. Diffuse infiltrating pancreatic malignancies such as lymphoma and pancreatic carcinoma should also be considered. While the pancreas of AIP typically shows delayed enhancement, lymphoma often shows washout of contrast on delayed scan [37]. A high-attenuation rim, which represents compressed normal parenchyma by carcinoma, is a helpful sign of diffuse infiltrating pancreatic carcinoma [38] (Figs. 5.5a, b). When the pancreas is focally enlarged but without findings suggestive of carcinoma (low-density mass, distal pancreatic duct cutoff, or atrophy), the finding is indeterminate and further investigation is necessary to make correct diagnosis (Fig. 5.3a) [35].
The morphology of the normal pancreas can vary even in subjects without pancreatic disease, thus assessing morphological changes in AIP such as diffuse enlargement is not always easy. In such cases, ancillary findings such as enhancement pattern (peak enhancement during pancreatic phase), lobulated contour, fatty marble, and absence of pancreatic duct irregularity are helpful to differentiate normal pancreas from AIP. Acute pancreatitis may present with diffuse enlargement of the gland with or without decreased enhancement. However, the clinical presentation is usually different. When pancreatic atrophy, calcifications, and/or pseudocyst formation is present, other forms of chronic pancreatitis must be considered in the differential diagnosis. These findings could be seen in the burnt-out phase of autoimmune pancreatitis.
Differences in Type 1 and Type 2 AIP
Little has been reported regarding the differences between type 1 and type 2 AIP on cross-sectional imaging (Fig. 5.4a–c). In a recent study, Deshpande et al. reviewed resected cases of type 1 (n = 11) and type 2 (n = 18) AIP [39]. Pancreatic tail cutoff sign was exclusively seen in type 2 disease (4/10). Other imaging features such as diffuse swelling of the pancreas, pancreatic stranding, capsule-like rim, and common bile duct strictures were seen in both types of AIP and were not helpful in distinguishing from one another. An international multicenter survey showed that diffuse swelling of the pancreas was more common in type 1 compared to type 2 AIP (40 % vs. 25 %) [24]. The pattern of extrapancreatic organ involvement is distinct between the two types and helpful when present [24]. Biliary or renal involvement and retroperitoneal fibrosis are seen in type 1 AIP, whereas inflammatory bowel disease is commonly associated with type 2 AIP.
Posttreatment Changes and Relapse
Steroid therapy often results in disease remission with resolution of clinical symptoms. Enlarged pancreatic parenchyma commonly normalizes or becomes atrophic (Figs. 5.1c, d) [8, 10]. Improvement of pancreatic duct stricture may be evident on CT or MR. Abnormal signal changes on T1, T2, or diffusion-weighted MR images improve completely or partially. Delayed enhancement changes on contrast-enhanced CT or MR usually normalize after steroid treatment. A pancreas with diffuse enlargement or capsule-like rim may respond to steroid more favorably [6].
Key Points
-
Diffuse parenchymal enlargement of the pancreas is a characteristic feature of AIP seen in 24–73 % of patients. However, it may present as focal or segmental enlargement of pancreas or low-density mass.
-
Capsule-like rim is a specific finding of AIP and seen in 14–48 % of patients with AIP.
-
The pancreatic parenchyma commonly shows decreased enhancement during the early phase contrast administration and shows increased enhancement during the delayed phase.
-
Presence of other organ (extrapancreatic) involvement is helpful in making the correct diagnosis of AIP.
-
FDG-PET and MRI with diffusion-weighted imaging may be helpful when CT findings are inconclusive.
References
Irie H, Honda H, Baba S, et al. Autoimmune pancreatitis: CT and MR characteristics. AJR Am J Roentgenol. 1998;170(5):1323–7.
Sahani DV, Kalva SP, Farrell J, et al. Autoimmune pancreatitis: imaging features. Radiology. 2004;233(2):345–52.
Church NI, Pereira SP, Deheragoda MG, et al. Autoimmune pancreatitis: clinical and radiological features and objective response to steroid therapy in a UK series. Am J Gastroenterol. 2007;102(11):2417–25.
Takahashi N, Fletcher JG, Fidler JL, Hough DM, Kawashima A, Chari ST. Dual-phase CT of autoimmune pancreatitis: a multireader study. AJR Am J Roentgenol. 2008;190(2):280–6.
Suzuki K, Itoh S, Nagasaka T, Ogawa H, Ota T, Naganawa S. CT findings in autoimmune pancreatitis: assessment using multiphase contrast-enhanced multisection CT. Clin Radiol. 2010;65(9):735–43.
Sahani DV, Sainani NI, Deshpande V, Shaikh MS, Frinkelberg DL, Fernandez-del CC. Autoimmune pancreatitis: disease evolution, staging, response assessment, and CT features that predict response to corticosteroid therapy. Radiology. 2009;250(1):118–29.
Takahashi N, Fletcher JG, Hough DM, et al. Autoimmune pancreatitis: differentiation from pancreatic carcinoma and normal pancreas on the basis of enhancement characteristics at dual-phase CT. AJR Am J Roentgenol. 2009;193(2):479–84.
Manfredi R, Frulloni L, Mantovani W, Bonatti M, Graziani R, Pozzi MR. Autoimmune pancreatitis: pancreatic and extrapancreatic MR imaging-MR cholangiopancreatography findings at diagnosis, after steroid therapy, and at recurrence. Radiology. 2011;260(2):428–36.
Wakabayashi T, Kawaura Y, Satomura Y, et al. Clinical and imaging features of autoimmune pancreatitis with focal pancreatic swelling or mass formation: comparison with so-called tumor-forming pancreatitis and pancreatic carcinoma. Am J Gastroenterol. 2003;98(12):2679–87.
Manfredi R, Graziani R, Cicero C, et al. Autoimmune pancreatitis: CT patterns and their changes after steroid treatment. Radiology. 2008;247(2):435–43.
Van Hoe L, Gryspeerdt S, Ectors N, et al. Nonalcoholic duct-destructive chronic pancreatitis: imaging findings. AJR Am J Roentgenol. 1998;170(3):643–7.
Kajiwara M, Kojima M, Konishi M, et al. Autoimmune pancreatitis with multifocal lesions. J Hepatobiliary Pancreat Surg. 2008;15(4):449–52.
Yang DH, Kim KW, Kim TK, et al. Autoimmune pancreatitis: radiologic findings in 20 patients. Abdom Imaging. 2006;31(1):94–102.
Kamisawa T, Takuma K, Anjiki H, et al. Differentiation of autoimmune pancreatitis from pancreatic cancer by diffusion-weighted MRI. Am J Gastroenterol. 2010;105(8):1870–5.
Taniguchi T, Kobayashi H, Nishikawa K, et al. Diffusion-weighted magnetic resonance imaging in autoimmune pancreatitis. Jpn J Radiol. 2009;27(3):138–42.
Horiuchi A, Kawa S, Hamano H, Hayama M, Ota H, Kiyosawa K. ERCP features in 27 patients with autoimmune pancreatitis. Gastrointest Endosc. 2002;55(4):494–9.
Kamisawa T, Tu Y, Egawa N, et al. Can MRCP replace ERCP for the diagnosis of autoimmune pancreatitis? Abdom Imaging. 2009;34(3):381–4.
Park SH, Kim MH, Kim SY, et al. Magnetic resonance cholangiopancreatography for the diagnostic evaluation of autoimmune pancreatitis. Pancreas. 2010;39(8):1191–8.
Carbognin G, Girardi V, Biasiutti C, et al. Autoimmune pancreatitis: imaging findings on contrast-enhanced MR, MRCP and dynamic secretin-enhanced MRCP. Radiol Med. 2009;114(8):1214–31.
Ichikawa T, Sou H, Araki T, et al. Duct-penetrating sign at MRCP: usefulness for differentiating inflammatory pancreatic mass from pancreatic carcinomas. Radiology. 2001;221(1):107–16.
Nishimura T, Masaoka T, Suzuki H, Aiura K, Nagata H, Ishii H. Autoimmune pancreatitis with pseudocysts. J Gastroenterol. 2004;39(10):1005–10.
Muraki T, Hamano H, Ochi Y, et al. Corticosteroid-responsive pancreatic cyst found in autoimmune pancreatitis. J Gastroenterol. 2005;40(7):761–6.
Takahashi N, Kawashima A, Fletcher JG, Chari ST. Renal involvement in patients with autoimmune pancreatitis: CT and MR imaging findings. Radiology. 2007;242(3):791–801.
Kamisawa T, Chari ST, Giday SA, et al. Clinical profile of autoimmune pancreatitis and its histological subtypes: an international multicenter survey. Pancreas. 2011;40(6):809–14.
Nakamoto Y, Saga T, Ishimori T, et al. FDG-PET of autoimmune-related pancreatitis: preliminary results. Eur J Nucl Med. 2000;27(12):1835–8.
Ozaki Y, Oguchi K, Hamano H, et al. Differentiation of autoimmune pancreatitis from suspected pancreatic cancer by fluorine-18 fluorodeoxyglucose positron emission tomography. J Gastroenterol. 2008;43(2):144–51.
Matsubayashi H, Furukawa H, Maeda A, et al. Usefulness of positron emission tomography in the evaluation of distribution and activity of systemic lesions associated with autoimmune pancreatitis. Pancreatology. 2009;9(5):694–9.
Nakajo M, Jinnouchi S, Fukukura Y, Tanabe H, Tateno R, Nakajo M. The efficacy of whole-body FDG-PET or PET/CT for autoimmune pancreatitis and associated extrapancreatic autoimmune lesions. Eur J Nucl Med Mol Imaging. 2007;34(12):2088–95.
Lee TY, Kim MH, Park do H, et al. Utility of 18F-FDG PET/CT for differentiation of autoimmune pancreatitis with atypical pancreatic imaging findings from pancreatic cancer. AJR Am J Roentgenol. 2009;193(2):343–8.
Numata K, Ozawa Y, Kobayashi N, et al. Contrast-enhanced sonography of autoimmune pancreatitis: comparison with pathologic findings. J Ultrasound Med. 2004;23(2):199–206.
D’Onofrio M, Zamboni G, Tognolini A, et al. Mass-forming pancreatitis: value of contrast-enhanced ultrasonography. World J Gastroenterol. 2006;12(26):4181–4.
Yadav D, Notahara K, Smyrk TC, et al. Idiopathic tumefactive chronic pancreatitis: clinical profile, histology, and natural history after resection. Clin Gastroenterol Hepatol. 2003;1(2):129–35.
Hardacre JM, Iacobuzio-Donahue CA, Sohn TA, et al. Results of pancreaticoduodenectomy for lymphoplasmacytic sclerosing pancreatitis. Ann Surg. 2003;237(6):853–8.
Prokesch RW, Chow LC, Beaulieu CF, Bammer R, Jeffrey Jr RB. Isoattenuating pancreatic adenocarcinoma at multi-detector row CT: secondary signs. Radiology. 2002;224(3):764–8.
Chari ST, Takahashi N, Levy MJ, et al. A diagnostic strategy to distinguish autoimmune pancreatitis from pancreatic cancer. Clin Gastroenterol Hepatol. 2009;7(10):1097–103.
Kamisawa T, Imai M, Yui Chen P, et al. Strategy for differentiating autoimmune pancreatitis from pancreatic cancer. Pancreas. 2008;37(3):e62–7.
Ishigami K, Tajima T, Nishie A, et al. MRI findings of pancreatic lymphoma and autoimmune pancreatitis: a comparative study. Eur J Radiol. 2010;74(3):e22–8.
Choi YJ, Byun JH, Kim JY, et al. Diffuse pancreatic ductal adenocarcinoma: characteristic imaging features. Eur J Radiol. 2008;67(2):321–8.
Deshpande V, Gupta R, Sainani N, et al. Subclassification of autoimmune pancreatitis: a histologic classification with clinical significance. Am J Surg Pathol. 2011;35(1):26–35.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2013 Springer Science+Business Media New York
About this chapter
Cite this chapter
Takahashi, N., Sahani, D.V. (2013). CT and MRI Features. In: Levy, M., Chari, S. (eds) Autoimmune (IgG4-related) Pancreatitis and Cholangitis. Springer, New York, NY. https://doi.org/10.1007/978-1-4419-6430-4_5
Download citation
DOI: https://doi.org/10.1007/978-1-4419-6430-4_5
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4419-6429-8
Online ISBN: 978-1-4419-6430-4
eBook Packages: MedicineMedicine (R0)