Abstract
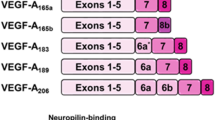
VEGF is an approximately 45 kDa homodimeric glycoprotein in the VEGF family, which includes more than seven proteins. Five of the polypeptides are encoded by distinct genes in the human genome: VEGF-A (VEGF), VEGF-B, VEGF-C, VEGF-D, and PGF (placenta growth factor) (Carmeliet, Oncology 69:4–10, 2005; Shibuya, Vascular permeability/vascular endothelial growth factor. In: Figg WD, Folkman J (eds) Angiogenesis. Springer, New York, pp 89–98, 2008). VEGF is considered to play a key role in regulating angiogenesis both in normal and malignant cells. VEGF-A exists in many different isoforms as a result of alternative exon splicing; the most frequent subtypes are VEGF121, VEGF165, VEGF189, and VEGF206. The shorter amino acid sequence isoform VEGF121 is soluble, in contrast to VEGF165, VEGF189, and VEGF206, which are heparin bound with varying affinity. VEGF121 and VEGF165, which also have the propensity to be unbound, are believed to have a central role in tumor angiogenesis (Kerbel and Ellis, Angiogenesis. In: DeVita, Hellman, Rosenberg (eds) Cancer. LWW, Philadelphia, pp 101–112, 2011).
Access provided by CONRICYT-eBooks. Download reference work entry PDF
Similar content being viewed by others
Keywords
- Bevacizumab
- Neuropilin-1
- Pazopanib and axitinib
- Sorafenib
- Sunitinib
- Vascular endothelial growth factor (VEGF)
- Anti-VEGF agents
- Biomarkers
- Clinical studies
- Endothelial functions
- In cancer
- Isoforms
- Preclinical models
- Receptors
- Regulator in angiogenesis
- Tyrosine kinase inhibitors (TKIs)
- Vascular permeability factor (VPF)
- VEGF-A gene
Target: Vascular Endothelial Growth Factor (VEGF)
VEGF is an approximately 45 kDa homodimeric glycoprotein in the VEGF family, which includes more than seven proteins. Five of the polypeptides are encoded by distinct genes in the human genome: VEGF-A (VEGF), VEGF-B, VEGF-C, VEGF-D, and PGF (placenta growth factor) (Carmeliet 2005; Shibuya 2008). VEGF is considered to play a key role in regulating angiogenesis both in normal and malignant cells. VEGF-A exists in many different isoforms as a result of alternative exon splicing; the most frequent subtypes are VEGF121, VEGF165, VEGF189, and VEGF206. The shorter amino acid sequence isoform VEGF121 is soluble, in contrast to VEGF165, VEGF189, and VEGF206, which are heparin bound with varying affinity. VEGF121 and VEGF165, which also have the propensity to be unbound, are believed to have a central role in tumor angiogenesis (Kerbel and Ellis 2011). Three VEGF receptors have been identified, VEGFR1 (Flt-1, Fms-like tyrosine kinase 1), VEGFR2 (KDR, kinase insert domain-containing receptor in humans/Flk1, fetal liver kinase 1 in mice), and VEGFR3 (Flt4). VEGFR3 has mainly been associated with lymphatic vessel growth and binds to the ligands VEGF-C and VEGF-D. VEGF-A binds to VEGFR1 and VEGFR2; both are expressed on vascular endothelial cells. The receptors have common characteristics and contain seven immunoglobulin-like domains (extra cellular ligand-binding domain), a tyrosine kinase domain, and the carboxy terminal. VEGFR2 bound to its ligand leads to receptor dimerization and triggers a cascade of signaling pathways that are believed to be essential in activating endothelial cells and promoting formation of new vessels, angiogenesis. Neuropilin-1 is a membrane protein and functions as a co-receptor, by increasing the affinity of VEGF165 for its receptor VEGFR2. The association between neuropilin-1 and VEGF165 is crucial for embryogenesis, if one of the proteins is missing; life is not sustained (Shibuya 2008, 2011).
Biology of the Target
VEGF is overexpressed in a majority of malignant tumors, and elevated VEGF has been shown repeatedly to be associated with poorer prognosis. VEGF stimulates a variety of endothelial functions inducing bone marrow mobilization of endothelial cells, migration, proliferation, survival, and vascular permeability. VEGF has also been shown to increase synthesis of nitric oxide, and one of the main side effects seen with anti-VEGF agents is hypertension (Kerbel and Ellis 2011). Two major pathways activated by the VEGF-VEGFR complex are PLCγ (phospholipase C gamma)-PKC-MAPK cascade resulting in proliferation and P13K-Akt pathway endorsing survival (Kawamuara et al. 2008). In addition to endothelial cells, VEGF influences other cells including monocytes and neurons (Ferrara 1999, 2008). Emerging data illuminates the immunosuppressive role of VEGF, by inducing production of inhibitory cytokines (IL-10 and IL-13), modulating dendritic cells, and stimulating regulatory T cells resulting in termination of T- and B-cell-mediated immune response (Correale et al. 2011; Alfaro et al. 2009).
The VEGF-A gene on chromosome 6 consists of 8 exons and is essential for embryonic vasculogenesis; deletion of one allele is not compatible with life. In adult life, VEGF-A is important in angiogenesis associated with female menstrual cycling and reproduction. VEGF gene expression is stimulated by various signals, hypoxia being a main candidate; others include acidic microenvironment, inflammatory cytokines, growth factors, androgens, and estrogens. VEGF upregulation is also influenced by an imbalance between the activation of oncogenes and inactivation of tumor suppressor genes (Ferrara 2008; Kerbel and Ellis 2011).
Target Assessment
Many biomarkers have been evaluated but none validated in prospective randomized trials, at this time. Several biomarkers have shown promise. VEGF, basic FGF, intercellular adhesion molecule (ICAM), and E-selectin were measured and evaluated pre- and posttreatment in the E4599 trial (leading to approval in lung cancer). Low-baseline ICAM showed significant association with improved response to treatment with or without bevacizumab and also overall survival. Decreased VEGF levels correlated to tumor response but not overall survival. VEGF and VEGFR2 showed correlation with progression-free survival (PFS) in the AVADO trial (breast cancer). In contrast there are trials which have failed to find VEGF levels to be predictive. Neuropilin-1 has indicated predictive value in metastatic colorectal cancer and metastatic gastric cancer. VEGF-D has been implicated to be of importance predicting response, resistance, and disease progression. Clinically, the development of hypertension is evaluated as a surrogate marker of efficacy in patients treated with bevacizumab (Ulahannan and Brahmer 2011; Meadows and Hurvitz 2012).
Role of the Target in Cancer
Rank: “unknown” to 10.
Unknown to 1–10: 10.
High-Level Overview
Diagnostic, Prognostic, and Predictive
There are no validated serum biomarkers available on the market to predict response to anti-VEGF therapy (Meadows and Hurvitz 2012).
Therapeutics
Bevacizumab is a humanized monoclonal antibody targeting circulating VEGF-A, subsequently inhibiting the ligand from binding to VEGFR. It was the first anti-VEGF therapy approved by the FDA in 2004 for the treatment of metastatic colorectal cancer in combination with irinotecan and 5-FU, based on a phase III trial, showing an increase in overall survival (15.6 months vs. 20.3 months) with a hazard ratio (HR) of 0.65. Improvements were also seen in progression-free survival and response rate (Hurvitz et al. 2004). Bevacizumab in combination with cytotoxic chemotherapy has been approved for the treatment of a number of different solid tumors including colorectal cancer, NSCLC (non-small cell lung cancer), and renal cell cancer. Glioblastoma has FDA approval for bevacizumab as a single agent. In January 2013, bevacizumab in combination with chemotherapy (FOLFOX or FOLFIRI) was approved in metastatic colon cancer patients, who had progressed on a first-line bevacizumab-containing regimen. This was based on a randomized phase III study demonstrating statistical OS benefit (9.8 months vs. 11.2 months) with an HR of 0.81, in the arm continuing to receive bevacizumab beyond progression.
Targeting the VEGFR is another approach for anti-VEGF therapy. Small-molecule tyrosine kinase inhibitors (TKIs), compete with ATP, binding to the active site of the VEGFR and thereby inhibiting activation. Sunitinib is a TKI approved for the treatment of renal cell cancer and GIST (gastrointestinal stromal tumors). Sorafenib, another TKI, has shown clinical activity in renal cell and hepatocellular carcinoma and is FDA approved for these malignancies. Pazopanib and axitinib are TKIs, which are FDA approved for renal cell cancer. Another recently FDA-approved anti-VEGF agent is regorafenib for colorectal cancer. In contrast to bevacizumab, the mentioned TKIs are approved as single agents for their indications and have several targets. VEGF inhibition by a different mechanism is through VEGF trap, a recombinant fusion protein, which contains the VEGF-binding site and thus binds the VEGF ligand, preventing binding to VEGFR. Ziv-aflibercept is an example of a VEGF trap drug, approved in combination with irinotecan for colorectal cancer (Ulahannan and Brahmer 2011; Meadows and Hurvitz 2012; FDA website). See Table 1.
Preclinical Summary
Vascular permeability factor (VPF) was discovered in 1983 by Senger and Dvorak. A few years later, VEGF was sequenced by Ferrara, and, when compared, the two proteins turned out to be the same (Folkman 2008). VEGF is a key regulator in angiogenesis , which is a necessary process for cancer cell proliferation beyond microscopic size, further invasion, and metastasis. Tumor angiogenesis causes abnormal structure and function of the vessels; in fact they can be so altered, making them hard to identify as blood vessels. Mouse monoclonal antibodies were found to inhibit VEGF in several cancer cell lines (1993); this discovery consequently led to the development of the first anti-VEGF agent in clinic, bevacizumab (Aragon-Ching et al. 2008; McDonald 2008).
In preclinical models, it has been shown that if anti-VEGF therapy is terminated, the tumor regains neo-angiogenesis rapidly. In one tumor model, during therapy, vascular density was reduced by 60–75% but, after withdrawing the drug, returned to baseline after 7 days (McDonald 2008).
Preclinical models have found inhibition of tumor growth when combining anti-VEGF therapy with tumor vaccination but only when the anti-VEGFR2 therapy was given at 25% of the dose. The lower anti-VEGF dose was also associated with increased distribution of functional blood vessels compared to higher doses. Hence lower dose of anti-VEGF therapy in these studies were linked to normalized vasculature structure and decreased immunosuppression (Huang et al. 2012).
Clinical Summary
Angiogenesis in tumors stimulated by VEGF is associated with abnormal vessels that are poorly organized and hyperpermeable, with consequent abnormal microenvironment characterized by interstitial hypertension, hypoxia, and acidosis. Preclinical data indicate synergy when anti-VEGF agents are combined with chemotherapy. Anti-VEGF agents inhibit growth of new blood vessels, cause regression of existing vasculature, and transiently “normalize” leaky tumor vasculature, which may increase the delivery of oxygen necessary to optimize radiation therapy and transport chemotherapy to the tumor. Additional effects observed with anti-VEGF therapy are decreased amount of ascites in ovarian cancer and reduced brain tumor edema in glioblastoma. The presence of anti-VEGF agents in between cycles of cytotoxic chemotherapy may lead to sustained tumor suppression. These may be contributing factors why there seems to be a synergistic effect when VEGF inhibitors are used in conjunction with chemotherapy (Jain 2005; Folkman 2008; Kerbel and Ellis 2011). In a clinical phase II trial with an anti-VEGF agent (TKI) used to treat glioblastoma patients, advanced MRI technique indicated normalization of the vasculature upon starting treatment; when the drug was discontinued so was the effect on the vasculature. Clinically, while on the drug, there was less brain edema and decreased need of steroids (Jain et al. 2008).
Anti-VEGF agents have been fairly well tolerated compared to cytotoxic chemotherapy. Adverse effects have been postulated to be mainly class specific and secondary to its mechanism of action. The inhibition of VEGF results in decreased synthesis of nitrous oxide with subsequent increase of vascular tone, which leads to hypertension. Severe hypertension is rare (<0.1%), but hypertension requiring medical treatment seems to range from 10% to 20%. Additional less common adverse effects include arterial thromboembolic events, GI perforation, and wound healing complications (Meadows and Hurvitz 2012).
Anticipated High-Impact Results
-
Validated predictive and prognostic biomarkers to individualize treatment, and select subgroups of patients who will have the greatest benefit and least toxicity from anti-VEGF treatment.
-
Surrogate markers to evaluate response and resistance, and adjust drug dosage to a given anti-VEGF treatment.
-
The optimal time in the course of malignancy to treat with anti-VEGF therapy
-
Immunologic effects of VEGF treatment, finding the right dose and combinations, to optimize antitumor effect
References
Alfaro C, et al. Influence of bevacizumab, sunitinib and sorafenib as single agents or in combination on the inhibitory effects of VEGF on human dendritic cell differentiation from monocytes. BJC. 2009;100:1111–9.
Aragon-Ching JB, et al. The clinical utility of bevacizumab. In: Figg WD, Folkman J, editors. Angiogenesis. New York: Springer; 2008. p. 375–85.
Carmeliet P. VEGF as a key mediator of angiogenesis in cancer. Oncology. 2005;69 Suppl 3:4–10.
Correale P, et al. Immunomodulatory properties of anticancer monoclonal antibodies: is the ‘magic bullet’ still a reliable paradigm? Immunotherapy. 2011;3:1–4.
FDA website: http://www.fda.gov/Drugs/InformationOnDrugs/ApprovedDrugs
Ferrara N. Role of vascular endothelial growth factor in regulation of angiogenesis. In: Teicher BA, editor. Antiangiogenic agents in cancer therapy. Totawa: Humana Press; 1999. p. 119–41.
Ferrara N. Overview and clinical applications of VEGF-A. In: Figg WD, Folkman J, editors. Angiogenesis. New York: Springer; 2008. p. 345–35.
Folkman J. History of angiogenesis. In: Figg WD, Folkman J, editors. Angiogenesis. New York: Springer; 2008. p. 1–14.
Huan Y, et al. Vascular normalizing doses of antiangiogenic treatment reprogram he immunosuppressive tumor microenvironment and enhance immunotherapy. Proc Natl Acad Sci U S A. 2012;109:17561–6.
Hurvitz H, et al. Bevacizumab plus Irinotecan, fluorouracil and leucovorin for metastatic colorectal cancer. NEJM. 2004;350:2335–42.
Jain RK. Normalization of tumor vasculature: an emerging concept in antiangiogenic therapy. Science. 2005;307:58–62.
Jain RK, et al. Normalization of tumor vasculature and microenvironment. In: Figg WD, Folkman J, editors. Angiogenesis. New York: Springer; 2008. p. 273–81.
Kawamuara H, et al. VEGF signal transduction in angiogenesis. In: Figg WD, Folkman J, editors. Angiogenesis. New York: Springer; 2008. p. 205–16.
Kerbel RS, Ellis L. Angiogenesis. In: DeVita, Hellman, Rosenberg, editors. Cancer. Philadelphia: LWW; 2011. p. 101–12.
McDonald D. Angiogenesis and vascular remodeling in inflammation and cancer: biology and architecture of the vasculature. In: Figg WD, Folkman J, editors. Angiogenesis. New York: Springer; 2008. p. 17–33.
Meadows K, Hurvitz H. Anti-VEGF therapies in the clinic. Cold Spring Harb Perspect Med. 2012;2:1–27.
Shibuya M. Vascular permeability/vascular endothelial growth factor. In: Figg WD, Folkman J, editors. Angiogenesis. New York: Springer; 2008. p. 89–98.
Shibuya M. VEGF and its receptor VEGFR signaling in angiogenesis: a crucial target for anti- and pro-angiogenic therapies. Genes Cancer. 2011;2:1097–105.
Ulahannan SV, Brahmer JR. Antiangiogenic agents in combination with chemotherapy in patients with advanced non-small cell cancer. Cancer Invest. 2011;29:325–37.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer Science+Business Media, New York (outside the USA)
About this entry
Cite this entry
Ulahannan, S. (2017). VEGF. In: Marshall, J. (eds) Cancer Therapeutic Targets. Springer, New York, NY. https://doi.org/10.1007/978-1-4419-0717-2_71
Download citation
DOI: https://doi.org/10.1007/978-1-4419-0717-2_71
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4419-0716-5
Online ISBN: 978-1-4419-0717-2
eBook Packages: Biomedical and Life SciencesReference Module Biomedical and Life Sciences