Abstract
Hyperornithinemia-hyperammonemia-homocitrullinuria (HHH) syndrome (OMIM 238970) is an autosomal recessive disorder that is caused by a deficiency of mitochondrial ornithine transporter 1, resulting in dysfunction of the urea cycle. HHH is the rarest of the urea cycle disorders, reported in fewer than 100 patients. It is characterized by extreme phenotypic variability, including diverse ages of onset and severity of phenotype. We report the first confirmed instance of HHH syndrome in a premature infant (31 2/7 weeks) with severe hyperammonemia (1,300 μmol/L).
This case highlights the importance of considering HHH in the differential diagnosis for neonatal hyperammonemia. Because HHH is not detected by newborn screening, and the characteristic biochemical triad may be subtle or even absent, it has the potential to be underdiagnosed; however, making the diagnosis has critical therapeutic implications as treatment is distinct from other urea cycle defects. For instance, lysine supplementation is a beneficial treatment unique to HHH. Therefore, we present here a review of previously reported cases in order to demonstrate the full spectrum of the disease and highlight potentially diagnostic features.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
The urea cycle, which converts ammonia to urea, is the major pathway for disposal of waste nitrogen. Functioning of the cycle involves the tightly regulated action of five enzymatic steps as well as membrane transporters which assure smooth integration of the mitochondrial and cytoplasmic components of the cycle. Mutations in either the constituent enzymes or the transporters can result in urea cycle defects, the clinical severity of which depends in part upon the completeness of the functional alteration. Urea cycle defects can present at virtually any age. Often an environmental stressor (typically infection) evokes hyperammonemia and clinical symptomatology by overwhelming an already compromised urea cycle (Lee et al. 2014).
Hyperornithinemia-hyperammonemia-homocitrullinuria (HHH) syndrome (mitochondrial ornithine transporter 1 deficiency) is an autosomal recessive disorder characterized by a failure of mitochondrial ornithine uptake (ORNT1/SLC25A15) and consequent inadequate supply of this amino acid to the mitochondrial ornithine transcarbamylase (OTC) reaction. The result is hyperammonemia and the accumulation of ornithine and lysine in the cytoplasm (Kim et al. 2012). Homocitrulline is thought to form from carbamylation of the increased cytoplasmic lysine pool. Patients manifest protein intolerance, episodic vomiting, growth failure, hepatomegaly, liver failure, and neurologic manifestations, including altered consciousness, seizures, pyramidal tract signs, and a variable degree of cognitive impairment with or without behavior problems. However, the clinical presentation can be highly variable (Lee et al. 2014; Lemay et al. 1992; Al-Hassnan et al. 2008; Gatfield et al. 1975).
Clinical Case Report
We present a male neonate born to a 27-year-old G2P0011 mother. Delivery was via Cesarean section at 31 2/7 weeks gestation due to maternal preeclampsia. Birth weight was 1.385 kg and the APGAR scores were 8 and 9. The mother received regular prenatal care. The patient was born to healthy non-consanguineous parents. The mother had electively terminated a prior pregnancy when she was 18 years. Family history was unremarkable with regard to intellectual disability, metabolic disease, dietary protein intolerance, or miscarriages. Both the mother and maternal grandmother described migraine headaches in association with menstruation. Prenatal laboratory tests and fetal ultrasounds were normal. Following delivery, he manifested periodic breathing that was treated with oxygen via nasal cannula and continuous positive airway pressure (CPAP) 6. He received a single dose of surfactant. On day of life (DOL) 4, worsening apnea and lethargy obliged intubation and controlled ventilation. A septic workup, including lumbar puncture, was performed because of deteriorating mental status and worsening apnea. Antibiotic therapy was initiated. Blood, urine, and CSF cultures were all negative. He initially received parenteral nutrition, but this was stopped when hyperammonemia (1,300 μmol/L) was discovered on DOL 5. The next day he was transferred to the Children’s Hospital of Philadelphia, where the initial blood ammonia was 623 μmol/L and treatment was started with intravenous acylation therapy (sodium phenylbutyrate and sodium benzoate; Ammonul) and intravenous arginine. Hyperammonemia rapidly resolved, and by DOL 9 he was successfully transitioned to oral therapy with arginine and sodium phenylbutyrate.
Although the patient’s ammonia levels quickly normalized with medical management, he remained critically ill and required dopamine and norepinephrine infusions for approximately 2 weeks. He had severe hepatic dysfunction and a coagulopathy reflected in an international normalized ratio (INR) that peaked at 2.31, prompting daily administration of vitamin K as well as multiple transfusions of fresh plasma, packed red cells, platelets, and cryoprecipitate for the first week of life. Neither multiple transfusions nor treatment with parenteral infusions of protein evoked hyperammonemia in our patient after his ammonia normalized. He also briefly required hydrocortisone for cardiovascular support, but steroid therapy did not cause recurrent hyperammonemia. Protein (0.25 g/day) was reintroduced into his TPN on DOL 9. His clinical picture was also notable for findings not associated with OTC deficiency such as small bilateral pleural effusions, a pericardial effusion, ascites, and generalized edema.
The Pennsylvania state newborn screening test was normal; detailed evaluation showed slight increases of phenylalanine and methionine. Urine organic acid quantitation and the blood acylcarnitine profile were normal. He never became acidotic. Blood lactate and pyruvate were not significantly elevated. Carbohydrate-deficient transferrin analysis was not suggestive of a congenital disorder of glycosylation.
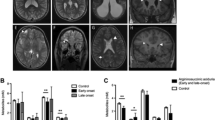
Plasma amino acid quantitation, initially obtained while the baby received parenteral nutrition, showed increased glutamine, ornithine, and citrulline. The glutamine/citrulline ratio was approximately 20 – in the expected range for OTC deficiency. The elevated ornithine was originally attributed to arginine supplementation; however, a repeat blood aminogram showed even more highly elevated ornithine (315 μmol/L; normal 26–164 μmol/L) and low blood lysine (56 μmol/L; normal 67–230 μmol/L) and relatively low citrulline (5.8 μmol/L; normal 0–35 μmol/L) (Fig. 1). Enteral lysine supplementation was initiated, and the infant was transitioned from arginine to citrulline. Urine orotic acid was initially (DOL 7) high at 12.5 mmol/mol creatinine (normal <4 mmol/mol creatinine); however this declined to a normal concentration after a few days (Table 1). Urine amino acid quantitation initially showed a generalized aminoaciduria, consistent with prematurity, but repeat analysis showed a disproportionate increase of urine ornithine. Urine homocitrulline was qualitatively present on retrospective analysis, but the concentration was within the “noise” of the test so was not initially remarked upon.
Single nucleotide polymorphism (SNP) chromosomal microarray was not consistent with the Xp11.4 gene deletion syndrome that includes a loss of ornithine transcarbamylase (Deardorff et al. 2008). The karyotype was a normal male, 46 XY without regions of homozygosity.
A next-generation sequencing urea cycle disorder panel (GeneDx, Maryland) showed two heterozygous pathogenic variants in the SLC25A15 gene (c.22 C>T with variant p.Gln8Ter (Q8X) and c.337 G>A with variant p.Gly113Ser (G113S)), which encodes the mitochondrial ornithine transporter, consistent with HHH syndrome. No other mutations were found.
Methods
For all standard runs, amino acids were analyzed using ultra-performance liquid chromatography, as described previously (Narayan et al. 2011). A standard column temperature of 43°C was used.
Discussion
HHH syndrome is an autosomal recessive disorder characterized by reduced ammonia clearance through the urea cycle due to mitochondrial ornithine deficiency. The basic defect is at the level of the mitochondrial ornithine transporter (ORNT1/SLC25A15), which has been mapped to chromosome 13q14. The clinical phenotype comprises protein intolerance, episodic vomiting, growth failure, hepatomegaly, and neurologic manifestations, including altered consciousness, seizures, pyramidal tract signs, and a variable degree of cognitive impairment with or without aberrant behaviors (Kim et al. 2012).
Impaired ornithine transport across the mitochondrial membrane causes ornithine accumulation in the cytoplasm and intramitochondrial ornithine deficiency. In four cases reported by Kim et al., patients all had elevated ornithine (200–1,400 μmol/L) and ammonia levels (up to 844 μmol/L) in blood and homocitrulline (~200 μmol/L) in urine (Kim et al. 2012). Our patient’s initial presentation was more severe with a blood ammonia of >1,300 μmol/L. He also had hepatic dysfunction that improved in tandem with resolution of the hyperammonemia. Our patient’s presentation is compared to other patients with HHH who presented in the neonatal period in Table 2 below.
Since the initial description by Shih et al., fewer than 100 patients with HHH syndrome have been reported (Shih et al. 1969; Sokoro et al. 2010). Most ethnic groups are represented, and there is no common mutation apart from a founder effect in the French-Canadian population of Quebec (Gatfield et al. 1975; Tessa et al. 2009).
The initial presentation and time of diagnosis in HHH is highly variable. In a retrospective review of 54 patients, there were 12 patients with a neonatal presentation (birth to 1 month), 13 with an infantile presentation (>1 month to 1 year), 24 with a childhood onset (>1 year to 12 years), and 5 with an adolescent to adult onset (>12 years). Only one patient was identified by newborn screen. Patients typically present acutely with intermittent hyperammonemia accompanied by vomiting, ataxia, lethargy, confusion, and coma, findings common to other urea cycle disorders. Some HHH patients have presented with fulminant liver failure (Fecarotta et al. 2006; Martinelli et al. 2015).
In most instances, HHH syndrome involves a chronic, progressive disease with protein intolerance, coagulation abnormalities, hypotonia, developmental delay, progressive encephalopathy with mental regression, and early signs of motor dysfunction. The vast majority of patients respond well to dietary and pharmacological therapy with a protein-limited diet and chronic ammonia scavenging therapy. The disorder is rarely lethal, with about 95% of patients surviving after diagnosis. By early adulthood, most patients develop signs of pyramidal tract dysfunction, often evolving into frank spastic paraparesis and lower limb stiffness. However, cognitive function is relatively preserved. Waisbren et al. found that in seven patients with HHH, IQs ranged 70–107 (Waisbren et al. 2016). Virtually all survivors had developmental disabilities that correlated with the number, severity, and duration of episodes of hyperammonemia (Msall et al. 1984, 1988).
Because HHH is a relatively rare urea cycle disorder that can be missed on newborn screen and has developmental outcomes that correlate with the number, severity, and duration of episodes of hyperammonemia, it is important to consider it in a differential diagnosis of any patient with hyperammonemia of unknown etiology. HHH also has the potential to be underdiagnosed since the classic biochemical triad may also be subtle or even absent. To our knowledge, this is the first instance of HHH in a premature neonate and illustrates the variability of the syndrome, including severe cardiovascular instability.
Abbreviations
- ASA:
-
Argininosuccinate
- CPS I:
-
Carbamoyl phosphate synthetase I
- CSF:
-
Cerebrospinal fluid
- DOL:
-
Day of life
- HHH:
-
Hyperornithinemia-hyperammonemia-homocitrullinuria
- INR:
-
International normalized ratio
- LP:
-
Lumbar puncture
- OTC:
-
Ornithine transcarbamylase
- TPN:
-
Total parenteral nutrition
References
Al-Hassnan ZN, Rashed MS, Al-Dirbashi OY, Patay Z, Rahbeeni Z, Abu-Amero KK (2008) Hyperornithinemia-hyperammonemia-homocitrullinuria syndrome with stroke-like imaging presentation: clinical, biochemical and molecular analysis. J Neurol Sci 264:187–194
Deardorff MA, Gaddipati H, Kaplan P et al (2008) Complex management of a patient with a contiguous Xp11.4 gene deletion involving ornithine transcarbamylase: a role for detailed molecular analysis in complex presentations of classical diseases. Mol Genet Metab 94(4):498–502
Fecarotta S, Parenti G, Vajro P et al (2006) HHH syndrome (hyperornithinaemia, hyperammonaemia, homocitrullinuria), with fulminant hepatitis-like presentation. J Inherit Metab Dis 29(1):186–189
Gatfield PD, Taller E, Wolfe DM, Haust MD (1975) Hyperornithinemia, hyperammonemia, and homocitrullinuria associated with decreased carbamyl phosphate synthetase I activity. Pediatr Res 9:488–497
Kim SZ, Song WJ, Nyhan WL, Ficicioglu C, Mandell R, Shih VE (2012) Long-term follow-up of four patients affected by HHH syndrome. Clin Chim Acta 413(13–14):1151–1155
Lee HH, Poon KH, Lai CK et al (2014) Hyperornithinaemia-hyperammonaemia-homocitrullinuria syndrome: a treatable genetic liver disease warranting urgent diagnosis. Hong Kong Med J 20(1):63–66
Lemay JF, Lambert MA, Mitchell GA et al (1992) Hyperammonemia-hyperornithinemia-homocitrullinuria syndrome: neurologic, ophthalmologic, and neuropsychologic examination of six patients. J Pediatr 121:725–730
Martinelli D, Diodato D, Ponzi E et al (2015) The hyperornithinemia-hyperammonemia-homocitrullinuria syndrome. Orphanet J Rare Dis 10:29
Msall M, Batshaw ML, Suss R, Brusilow SW, Mellits ED (1984) Neurologic outcome in children with inborn errors of urea synthesis. Outcome of urea-cycle enzymopathies. N Engl J Med 310(23):1500–1505
Msall M, Monahan PS, Chapanis N, Batshaw ML (1988) Cognitive development in children with inborn errors of urea synthesis. Acta Paediatr Jpn 30(4):435–441
Narayan SB, Ditewig-meyers G, Graham KS, Scott R, Bennett MJ (2011) Measurement of plasma amino acids by ultraperformance® liquid chromatography. Clin Chem Lab Med 49(7):1177–1185
Shih VE, Efron ML, Moser HW (1969) Hyperornithinemia, hyperammonemia, and homocitrullinuria. A new disorder of amino acid metabolism associated with myoclonic seizures and mental retardation. Am J Dis Child 117:83–92
Sokoro AA, Lepage J, Antonishyn N et al (2010) Diagnosis and high incidence of hyperornithinemia-hyperammonemia-homocitrullinuria (HHH) syndrome in northern Saskatchewan. J Inherit Metab Dis 33(Suppl 3):275–281
Tessa A, Fiermonte G, Dionisi-vici C et al (2009) Identification of novel mutations in the SLC25A15 gene in hyperornithinemia-hyperammonemia-homocitrullinuria (HHH) syndrome: a clinical, molecular, and functional study. Hum Mutat 30(5):741–748
Waisbren SE, Gropman AL, Batshaw ML (2016) Improving long term outcomes in urea cycle disorders-report from the urea cycle disorders consortium. J Inherit Metab Dis 39(4):573–584
Acknowledgments
The authors thank the family for their participation in this work.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Additional information
Communicated by: Bridget Wilcken, MBChB, MD
Appendices
Details of Funding
RDG received salary support from the National Institute of Diabetes and Digestive and Kidney diseases, K08-DK113250.
Details of Ethics Approval
Ethics approval was not required for this study.
Conflicts of Interest
None of the authors have any conflicts of interest to disclose.
Synopsis
Hyperornithinemia-hyperammonemia-homocitrullinuria is an important consideration in the evaluation of a neonate with hyperammonemia, even if the characteristic biochemical triad is not yet apparent.
Compliance with Ethics Guidelines
Conflict of Interest
The authors each declare that they have no conflict of interest.
Details of the contributions of individual authors: KTW performed clinical and biochemical evaluation of the patient and conceived and wrote the manuscript. RDG performed clinical and biochemical evaluation of the patient, conceived the manuscript, and provided oversight. MY performed clinical and biochemical evaluation of the patient and edited and conceived the manuscript. LIC performed clinical evaluation of the patient and edited and conceived the manuscript.
Ethics approval was not required for this study.
Rights and permissions
Copyright information
© 2018 Society for the Study of Inborn Errors of Metabolism (SSIEM)
About this chapter
Cite this chapter
Wild, K.T., Ganetzky, R.D., Yudkoff, M., Ierardi-Curto, L. (2018). Hyperornithinemia, Hyperammonemia, and Homocitrullinuria Syndrome Causing Severe Neonatal Hyperammonemia. In: Morava, E., Baumgartner, M., Patterson, M., Rahman, S., Zschocke, J., Peters, V. (eds) JIMD Reports, Volume 44. JIMD Reports, vol 44. Springer, Berlin, Heidelberg. https://doi.org/10.1007/8904_2018_132
Download citation
DOI: https://doi.org/10.1007/8904_2018_132
Received:
Revised:
Accepted:
Published:
Publisher Name: Springer, Berlin, Heidelberg
Print ISBN: 978-3-662-58616-7
Online ISBN: 978-3-662-58617-4
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)