Abstract
Background: Very long chain acyl CoA dehydrogenase (VLCAD) deficiency (OMIM#201475) is an autosomal recessive disorder of fatty acid beta oxidation caused by defect in the ACADVL. The aim of this study was to analyze the clinical, biochemical, and molecular features of VLCAD deficiency in Saudi Arabia, including the treatment and outcome.
Methods: We carried out a retrospective chart review analysis of 37 VLCAD deficiency patients from two tertiary centers in Saudi Arabia, over a 14-year period (2002–2016). Twenty-three patients were managed at King Abdul-Aziz Medical City and fourteen patients at King Fahad Medical City.
Results: Severe early onset VLCAD deficiency is the most frequent phenotype in our patients, caused by four different mutations in ACADVL; 31 patients (83.7%) had a homozygous nonsense mutation in exon 2 of ACADVL c.65C>A;p. Ser22X. Twenty-three patients died before the age of 2 years, despite early detection by newborn screening and implementation of treatment, including supplementation with medium chain triglycerides.
Conclusion: This study reports the clinical, biochemical, molecular findings, treatment, and outcome of patients with VLCAD deficiency over the last 14 years. We identified the most common variant and one new variant in ACADVL. Despite early diagnosis and treatment, the outcome of VLCAD deficiency in this Saudi Arabian population remains poor. Preventive measures, such as prenatal diagnosis, could be implemented.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
Background
Very long chain acyl CoA dehydrogenase deficiency (VLCAD) is an autosomal recessive disorder of fatty acid beta oxidation, caused by a defect in ACADVL gene encoding the VLCAD enzyme, which catalyzes the initial step in the mitochondrial fatty acid beta oxidation pathway (Leslie et al. 1993). This process is essential for energy production during prolonged fasting or periods of increased energy need, such as with intercurrent infection. Dietary long chain fatty acids, or those released from fat stores, are transported into the mitochondria and undergo progressive shortening by a series of chain-length specific enzymes to produce acetyl CoA and beta-hydroxybutyrate (ketones) and reducing equivalents for the mitochondrial respiratory chain, providing an alternate energy source, primarily for the brain and other critical tissues, heart, liver, and skeletal muscle (Vockley and Whiteman 2002; Spiekerkoetter 2010).
VLCAD deficiency was first described in 1985 by Hale et al., and thought to be due to long chain acyl-CoA dehydrogenase deficiency (LCAD) (Hale et al. 1985). In 1993, Aoyama et al. described VLCAD deficiency (Aoyama et al. 1993), and patients previously diagnosed as LCAD were reclassified as VLCAD deficiency. The disease has three heterogeneous clinical phenotypes: severe early onset cardiac and multi-organ failure presenting in the first months of life with dilated or hypertrophic cardiomyopathy, arrhythmia, hepatomegaly, hypoglycemia, and is often lethal; a childhood onset phenotype with hypoketotic hypoglycemia, hepatic dysfunction, and rhabdomyolysis (cardiomyopathy is unlikely); a late onset phenotype, which presents with episodic myopathy and rhabdomyolysis (Andresen et al. 1999).
The diagnosis is established initially by detecting elevations of the C14:1, C14:2, C14, or C12 acylcarnitines (McHugh et al. 2011) on newborn screening or at clinical presentation and may be confirmed by molecular analysis of ACADVL. This gene was first cloned in 1995 (Aoyama et al. 1995). Subsequently, hundreds of pathogenic mutations have been discovered. Andresen et al. reviewed potential genotype/phenotype correlation, with a general classification of the pathological mutations: null mutations with no VLCAD enzyme activity, such as truncating variants with severe presentation; missense or single amino acid deletions with residual enzyme activity and milder presentation (Andresen et al. 1999). Diekman et al. reported a strong correlation between LC-FAO flux in fibroblasts and the clinical severity of VLCAD deficiency, suggesting that this assay may have better predictive value compared to enzyme activity or plasma acylcarnitine accumulation (Diekman et al. 2015). There are likely ethnic differences in disease presentation. Most of the reported cases in Andresen et al. were European, with a mild phenotype; however, the cases initially reported by Aoyama et al. from Japan were all of the severe phenotype (Aoyama et al. 1993; Andresen et al. 1999). With the implementation of newborn screening programs, early identification of severe cases has allowed for early management and improved outcomes in some patients. Milder phenotypes may also be detected early, some of whom may remain asymptomatic, but which may reflect the true incidence of the disease (Touma et al. 2001; Spiekerkoetter 2010).
In general, treatment of VLCAD is avoidance of triggers of acute decompensation, such as prolonged fasting and intercurrent infections (catabolic stressors), early intervention for acute symptoms and dietary management, including restriction of long chain fat and supplementation with medium chain triglycerides (MCT) that can diffuse directly into the mitochondria and bypass the enzyme deficiency. Controversially, carnitine supplementation maybe used to help eliminate accumulated organic acid metabolites and prevent a secondary deficiency. Management also requires regular follow up to manage the diet, periodic monitoring of cardiac function and growth parameters (McHugh et al. 2011).
Although Saudi Arabia ranks second globally in the prevalence of genetic diseases (Christianson et al. 2006), this is the first report of clinical outcomes for VLCAD deficiency.
Methods
We carried out a retrospective chart review of 37 cases of VLCAD deficiency identified and followed at two tertiary centers in Saudi Arabia from 2002 to 2016. Twenty-three patients were from King Abdul-Aziz Medical City (KAMC) and 14 patients from King Fahad Medical City (KFMC).
Ethics approval for clinical and laboratory data collection was obtained from the King Abdullah International Medical Research Center (KAIMRC) in Riyadh, Saudi Arabia (RC16/189/R). All patients were detected early by tandem mass spectrometry newborn screening and subsequently treatment with a special metabolic formula containing MCT in addition to carnitine supplementation, with close monitoring and follow up. The diagnosis was confirmed by molecular analysis, including parental carrier testing.
ACADVL was analyzed by PCR and sequencing of coding exon and highly conserved intronic spice sites. The reference sequence of ACADVL is NM_000018.3.
Result
Clinical Features
All patients were products of consanguineous marriages. The oldest patient was 6 years old (Table 1). There were 23 female patients and 14 male patients. The female to male ratio was approximately 2:1. The family history of unexplained fetal death was positive in 31 patients (83.7%). Early onset cardiac and multi-organ failure VLCAD deficiency was detected in 27 patients (73%); the childhood hepatic and hypoglycemic form in 8 patients (21.6%); and the periodic myopathic form in 2 patients (5.5%).
Twenty-one patients (56.7%) were found to have a variable degree of hypertrophic cardiomyopathy and one (2%) had dilated cardiomyopathy. Eleven patients (29.7%) had structural heart disease (ventricular and atrial septal defect, pulmonary stenosis, patent ductus arteriosus, or persistent foramen oval). All patients who underwent echocardiogram had normal ejection fraction with a total average at 70.5%. Twelve patients (32.4%) developed hepatomegaly; five patients (13.5%) had hypotonia. Twenty-three (62.1%) died between the ages of 2 days and 3 years. Most deaths were preceded by frequent admissions for metabolic acidosis and rhabdomyolysis. Twenty of them died with multiple organ failure, cardiomyopathy, and arrhythmias. One patient developed acute kidney injury secondary to rhabdomyolysis and three patients (8.1%) died of sudden unexplained death in the first few days of life. Muscular hypotonia was detected in eight patients (21.6%), one of whom also had microcephaly, dysmorphic features, and seizure disorder.
Biochemical Features
All of our cases had high long chain C14 acylcarnitines. Thirty-four (91.9%) had variable elevation of liver enzymes. Five patients (13.5%) had abnormal coagulation profile and twelve patients (32.4%) had mild-to-moderate hypoalbuminemia. Hypoketotic hypoglycemia was detected in 17 patients (46%). Creatine phosphokinase (CPK) was high in 18 cases (48.6%). Recurrent metabolic acidosis was also observed. Most of the biochemical markers increased during metabolic crises.
Molecular Features
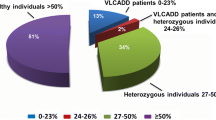
Our results showed that the mutational spectrum is narrow with four different mutations in ACADVL; 31 patients (83.7%) had a homozygous stop codon nonsense mutation in exon 2 c.65C>A; p.Ser22X (Table 2).
Clinical Outcome
Although all patients received standard treatment regimen mentioned above, including the MCT oil immediately following the diagnosis, the outcome was still poor, with recurrent admission for metabolic decompensation, resulting in death in 23 patients (>75% of patients) within first 2 years of life. Two sisters (28 and 18 months) are still alive with good metabolic stability and no cardiomyopathy, and found to have a pathogenic homozygous variant in exon 3 c.134 C>A; p.Ser45x.
A 3-year-old female patient with good metabolic stability was found to have c.1349G>A; p.Arg450His. A new variant in exon 7 c.494T>C; p.Phe165Ser was detected by whole exome sequencing in one 4-year-old female patient who is still alive with severe global developmental delay, generalized hypotonia, and dysmorphic features. This patient had another homozygous probably pathogenic variant in ZNF423 c.3250G>A; p.Val1084Ile. Both variants detected in this patient were also found in heterozygous state in each parent.
Two of the patients who died early had a positive newborn screen and clinical features of VLCAD deficiency and a positive family history but mutation analysis was not obtained.
Discussion
Very long chain Acyl CoA dehydrogenase deficiency is a severe life-threatening metabolic disorder of mitochondrial fatty acid beta-oxidation, which is one of the major metabolic pathways in eukaryotic energy production (Watanabe et al. 2000). The incidence of VLCAD deficiency is between 1:100,000 and 1:120,000 live births (Zytkovicz et al. 2001; Chace et al. 2002) which increased to 1:42,500 after the introduction of tandem MS for expanded newborn screening (Spiekerkoetter et al. 2003). In Saudi Arabia, however, a recent publication reported an incidence of 1:37,000, consistent with other reports of high frequency of metabolic disorders in Saudi Arabia (Alfadhel et al. 2016). The high consanguinity rate among Saudi population (Al-Gazali et al. 2006) could explain the high incidence of the disease.
It is apparent from our study and previous reports that VLCAD deficiency is a clinically heterogeneous disease that can be divided into three major phenotypes as previously described (Ogilvie et al. 1994; Andresen et al. 1999). Most of our patients presented with a severe early onset cardiac and multi-organ failure phenotype in the first few months of life, mainly in the neonatal period. Despite dietary modification and frequent monitoring, the mortality rate was 62%. The overall mortality rate of VLCAD deficiency was reported previously to reach up to 75% (Andresen et al. 1999) in clinically diagnosed patients, pre-newborn screening. The poor outcome in our study is likely related to the severe null mutations in a consanguineous population. The majority of the severe cases in our cohort were cardiomyopathic; however, there was no correlation between the degree of cardiomyopathy and the ejection fraction, and death. It is possible that arrhythmias played important role in sudden death of our patients. Arrhythmias have been previously reported in VLCAD deficiency patients. These include QT prolongation, polymorphic ventricular tachycardia, and ventricular fibrillation, sometimes without cardiomyopathy (Bonnet et al. 1999; Gelinas et al. 2011; Yamamoto et al. 2013).
A stop codon variant c.65C>A; p.Ser22X was found in 84% of our patients. This null mutation was initially described by Watanabe et al. and encodes a truncated protein leading to a complete deficiency of the VLCAD enzyme (Andresen et al. 1999; Watanabe et al. 2000).
The null mutation, reported by Touma et al., with a relatively milder cardiomyopathy phenotype, was also found in our population, but despite early diagnosis and treatment, the outcome was poor.
Interestingly, the c.134 C>A (p.Ser45X), nonsense mutation was detected in two patients with good metabolic control and no cardiomyopathy. As for the c.65C>A nonsense variant, the encoding VLCAD protein should be completely deficient. The relatively good metabolic health in the patient with the c.134C>A mutation is therefore probably explained by other genetic or environmental factors. The other previously reported mutation, c.1349G>A p.Arg450His, was detected in a 3-year-old patient. It was previously reported in a 14-year-old Japanese girl (Fukao et al. 2001) as a compound heterozygote, with residual activity and a milder phenotype, similar to our patient.
In this study we also report a new variant, which was identified by WES, the variant, c.494T>C (p.Phe165Ser) in exon 7 of ACADVL, affect a highly conserved amino acid, and introduce a large physiochemical deference. Indeed, in silico analysis predicted that this variant was pathogenic. Another variant in exon 4 of the ZNF423 c.3250G>A; p.Val1084Ile (associated with Joubert syndrome type 19 [OMIM # 614884]) was detected and could explain the unexpected phenotypes in this particular patient.
We did not detect any patient in this study with the variant c.848T>C; p.V283A, reported in the literature as the most frequent mutation in VLCAD deficient patients (Miller et al. 2015; Evans et al. 2016). This variant is often associated with residual enzyme activity and mild hepatopathic (hypoglycemia may occur) or episodic myopathic adult form of VLCAD deficiency that responds well to standard treatment (Andresen et al. 1999; Touma et al. 2001; Miller et al. 2015). The new variant detected in this study broadens the genetic spectrum of VLCAD deficiency; however, the detection of another homozygous variant in ZNF423 may indicate presence of another genetic disease in this patient which is not uncommon in our society. Al-Owain et al. discussed the concept of “Double hit” and reported many examples of patients with two or more concurrent genetic diseases as in our patient population, which was attributed to the high rate of consanguinity in Saudi society (Al-Owain et al. 2012).
The presence of a common null mutation in our patients and the poor outcome despite early diagnosis and treatment suggests that preventive measures may be an option. In our centers, in addition to thorough genetic counseling for affected families, we offer prenatal diagnosis for future pregnancies. With education and the philosophy that the “current patient is the last patient in the family,” most of the families accept the offered preventive measures.
Conclusion
In our retrospective study of 37 VLCAD deficiency patients over a 14-year period, the clinical outcomes and genotypes in our patients are different to that reported in the Caucasian population, with majority of cases having a severe early onset cardiac and multi-organ failure phenotype. Homozygosity for the c.65C>A nonsense mutation is the common with 83.7% of cases. Despite the early detection by newborn screening and early implementation of standard treatment, the outcome is fatal in most patients in the first 2 years of life. The prevention of this disease in our population may require pre-implantation genetic diagnosis, prenatal genetic testing, and carrier testing of high risk family members in addition to premarital genetic carrier testing for the known family mutation.
References
Alfadhel M, Benmeakel M, Hossain MA et al (2016) Thirteen year retrospective review of the spectrum of inborn errors of metabolism presenting in a tertiary center in Saudi Arabia. Orphanet J Rare Dis 11:126
Al-Gazali L, Hamamy H, Al-Arrayad S (2006) Genetic disorders in the Arab world. BMJ 333:831–834
Al-Owain M, Al-Zaidan H, Al-Hassnan Z (2012) Map of autosomal recessive genetic disorders in Saudi Arabia: concepts and future directions. Am J Med Genet A 158A:2629–2640
Andresen BS, Olpin S, Poorthuis BJ et al (1999) Clear correlation of genotype with disease phenotype in very-long-chain acyl-CoA dehydrogenase deficiency. Am J Hum Genet 64:479–494
Aoyama T, Uchida Y, Kelley RI et al (1993) A novel disease with deficiency of mitochondrial very-long-chain acyl-CoA dehydrogenase. Biochem Biophys Res Commun 191:1369–1372
Aoyama T, Souri M, Ueno I et al (1995) Cloning of human very-long-chain acyl-coenzyme a dehydrogenase and molecular characterization of its deficiency in two patients. Am J Hum Genet 57:273–283
Bonnet D, Martin D, De Pascale L et al (1999) Arrhythmias and conduction defects as presenting symptoms of fatty acid oxidation disorders in children. Circulation 100:2248–2253
Chace DH, Kalas TA, Naylor EW (2002) The application of tandem mass spectrometry to neonatal screening for inherited disorders of intermediary metabolism. Annu Rev Genomics Hum Genet 3:17–45
Christianson A, Howson CP, Modell B (2006) March of Dimes global report on birth defects: the hidden toll of dying and disabled children. In: March of Dimes global report on birth defects: the hidden toll of dying and disabled children. March of Dimes Birth Defects Foundation, White Plains, p 76
Diekman EF, Ferdinandusse S, van der Pol L et al (2015) Fatty acid oxidation flux predicts the clinical severity of VLCAD deficiency. Genet Med 17:989–994
Evans M, Andresen BS, Nation J, Boneh A (2016) VLCAD deficiency: follow-up and outcome of patients diagnosed through newborn screening in Victoria. Mol Genet Metab 118:282–287
Fukao T, Watanabe H, Orii K et al (2001) Myopathic form of very-long chain acyl-CoA dehydrogenase deficiency: evidence for temperature-sensitive mild mutations in both mutant alleles in a Japanese girl. Pediatr Res 49:227–231
Gelinas R, Thompson-Legault J, Bouchard B et al (2011) Prolonged QT interval and lipid alterations beyond beta-oxidation in very long-chain acyl CoA dehydrogenase null mouse hearts. Am J Physiol Heart Circ Physiol 301:H813–H823
Hale DE, Batshaw ML, Coates PM et al (1985) Long-chain acyl coenzyme a dehydrogenase deficiency: an inherited cause of nonketotic hypoglycemia. Pediatr Res 19:666–671
Leslie ND, Valencia CA, Strauss AW, Connor JA, Zhang K (1993) Very long-chain acyl-coenzyme A dehydrogenase deficiency. In: Pagon RA, Adam MP, Ardinger HH et al (eds) GeneReviews®. University of Washington, Seattle, Seattle
McHugh D, Cameron CA, Abdenur JE et al (2011) Clinical validation of cutoff target ranges in newborn screening of metabolic disorders by tandem mass spectrometry: a worldwide collaborative project. Genet Med 13:230–254
Miller MJ, Burrage LC, Gibson JB et al (2015) Recurrent ACADVL molecular findings in individuals with a positive newborn screen for very long chain acyl CoA dehydrogenase (VLCAD) deficiency in the United States. Mol Genet Metab 116:139–145
Ogilvie I, Pourfarzam M, Jackson S, Stockdale C, Bartlett K, Turnbull DM (1994) Very long-chain acyl coenzyme a dehydrogenase deficiency presenting with exercise-induced myoglobinuria. Neurology 44:467–473
Spiekerkoetter U (2010) Mitochondrial fatty acid oxidation disorders: clinical presentation of long-chain fatty acid oxidation defects before and after newborn screening. J Inherit Metab Dis 33:527–532
Spiekerkoetter U, Tenenbaum T, Heusch A, Wendel U (2003) Cardiomyopathy and pericardial effusion in infancy point to a fatty acid b-oxidation defect after exclusion of an underlying infection. Pediatr Cardiol 24:295–297
Touma EH, Rashed MS, Vianey-Saban C et al (2001) A severe genotype with favourable outcome in very long chain acyl CoA dehydrogenase deficiency. Arch Dis Child 84:58–60
Vockley J, Whiteman DA (2002) Defects of mitochondrial beta-oxidation: a growing group of disorders. Neuromuscul Disord 12:235–246
Watanabe H, Orii KE, Fukao T et al (2000) Molecular basis of very long chain acyl CoA dehydrogenase deficiency in three Israeli patients: identification of a complex mutant allele with P65L and K247Q mutations, the former being an exonic mutation causing exon 3 skipping. Hum Mutat 15:430–438
Yamamoto A, Nakamura K, Matsumoto S et al (2013) VLCAD deficiency in a patient who recovered from ventricular fibrillation, but died suddenly of a respiratory syncytial virus infection. Pediatr Int 55:775–778
Zytkovicz TH, Fitzgerald EF, Marsden D et al (2001) Tandem mass spectrometric analysis for amino, organic, and fatty acid disorders in newborn dried blood spots: a two-year summary from the New England Newborn Screening Program. Clin Chem 47:1945–1955
Acknowledgments
The authors would like to thank the patients and their families. The authors would also like to extend their acknowledgment to Ms. Rasha Al-kindi for her support in data collection.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Additional information
Communicated by: Verena Peters
Appendices
Learning Point
Truncating null mutations was the most common genotype in our VLCAD deficiency patients, with poor outcome despite early diagnosis and proper management. Prenatal diagnosis be a preferable strategy for managing this disorder in our population.
Details of the Contributions of Individual Authors
AO: performed the majority of work associated with preparing, writing, and submitting the manuscript and contributed to the clinical diagnosis and management of the patient. MN: performed work associated with preparing, writing, and intellectual discussion. MF, AAS, and FM: contributed to the diagnosis and management of the patient at KAMC and edited the manuscript. AAA, EF, and AM: contributed to the clinical diagnosis and management of the patient at KFMC and edited the manuscript. DM: Study design, manuscript writing, and final revision. MAB and MAA: Data collection and manuscript revision. WE: contributed to the clinical diagnosis and management of the patient and performed the work related to study design, conceptual discussion, and manuscript writing and revision. All authors read and approved the final manuscript.
Guarantor Author
Wafaa Eyaid.
Compliance with Ethics Guidelines
Conflict of Interest
Abdulrahman Obaid, Marwan Nashabat, Majid Alfadhel, Ali Alasmari, Fuad Al Mutairi, Abdulrahman Alswaid, Eissa Faqeih, Aziza Mushiba, Deborah Marsden, Marwah Albanyan, Maryam Alalwan, and Wafaa Eyaid declare that they have no conflict of interest.
Informed Consent
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000 (5). Informed consent was obtained from all parents and available upon request.
Details of Ethics Approval
This study was approved by King Abdullah International Medical Research Center IRB (RC16/189/R).
Details of Funding
This study received no specific funding from any financial support agency either public or commercial and not-for-profit sectors.
Rights and permissions
Copyright information
© 2017 Society for the Study of Inborn Errors of Metabolism (SSIEM)
About this chapter
Cite this chapter
Obaid, A. et al. (2017). Clinical, Biochemical, and Molecular Features in 37 Saudi Patients with Very Long Chain Acyl CoA Dehydrogenase Deficiency. In: Morava, E., Baumgartner, M., Patterson, M., Rahman, S., Zschocke, J., Peters, V. (eds) JIMD Reports, Volume 40. JIMD Reports, vol 40. Springer, Berlin, Heidelberg. https://doi.org/10.1007/8904_2017_58
Download citation
DOI: https://doi.org/10.1007/8904_2017_58
Received:
Revised:
Accepted:
Published:
Publisher Name: Springer, Berlin, Heidelberg
Print ISBN: 978-3-662-57879-7
Online ISBN: 978-3-662-57880-3
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)