Abstract
Pompe disease (OMIM 232300), a glycogen storage disorder caused by deficiency in the lysosomal enzyme acid alpha-glucosidase (EC 3.2.1.20), results in weakness and cardiomyopathy in infants affected with the classic form. Although the primary disease manifestations are due to glycogen accumulation in skeletal and cardiac muscle, glycogen also accumulates in a variety of additional tissues. To improve our understanding of disease pathogenesis in long-term survivors, we reviewed postmortem results for three infants with the classic form of Pompe disease. We have observed a number of new complications in long-term survivors of infantile-onset Pompe disease, and we focused this postmortem study on pathological correlates. Findings in survivors include cardiac arrhythmias, which may be related to glycogen accumulation in cardiac conduction tissue; urinary incontinence, likely due to glycogen accumulation in smooth muscle; and refractory errors, possibly related to accumulation in ocular structures. These observations provide potential pathophysiologic correlates for complications in long-term survivors of infantile Pompe disease.
Competing interests: None declared
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Acid alpha-glucosidase deficiency
- Autopsy
- Cardiomyopathy
- Glycogen storage disorder
- Lysosomal storage disorder
- Pompe disease
Introduction
Pompe disease (glycogen storage disease type II) is an autosomal recessive disorder due to deficiency of the lysosomal enzyme acid alpha-glucosidase (GAA). Infantile-onset Pompe disease (IPD) presents in the first few days to weeks of life with hypotonia, developmental delay, and cardiomyopathy. Enzyme replacement therapy (ERT) with recombinant acid alpha-glucosidase (rhGAA) improves survival in IPD (van den Hout et al. 2000; Kishnani et al. 2006). While the disorder was described decades ago, our understanding of disease complications continues to evolve, particularly as ERT has improved survival.
Recent publications highlight the need for a better understanding of disease complications in long-term survivors of IPD. Some of the complications, such as bowel and urinary incontinence, arterial aneurysms, and dysphagia, overlap with known complications in late-onset Pompe disease (LOPD) (El-Gharbawy et al. 2011; Prater et al. 2012; Hobson-Webb et al. 2012; Laforêt et al. 2008). Additional findings, such as cardiac arrhythmias and ocular refractory errors, are emerging (Prakalapakorn et al. 2014). In addition, cognitive abnormalities have been observed in long-term survivors (Spiridigliozzi et al. 2012).
We analyzed autopsy findings in three deceased individuals with IPD, diagnosed 5–14 years ago, to explore the pathophysiology of clinical findings in long-term survivors with IPD. These observations were compared with postmortem findings in the published literature. We placed particular emphasis on glycogen accumulation in tissue with few or no previous observations, such as central and peripheral nervous system, cardiac conduction tissue, ocular structures, and smooth muscle. This knowledge expands our current understanding of complications observed among long-term survivors of infantile Pompe disease and offers additional knowledge that can guide health care supervision.
Materials and Methods
We conducted a retrospective chart review of clinical and postmortem data in three deceased individuals with infantile Pompe disease. Chart review included notes from clinical care, radiology results, and autopsy results. The study received exempt status by the Duke Medicine Institutional Review Board for Clinical Investigations. Literature review included articles generated by a PubMed database search using the terms “Pompe disease and autopsy,” “Pompe disease and postmortem,” “glycogen storage disease type II and autopsy,” and “glycogen storage disease type II and postmortem.”
Results
Patient 1
This female African American infant had hypotonia and feeding difficulties at 2 months of age. She was diagnosed with Pompe disease at 6 months of age, when a diagnostic evaluation was initiated on the observation of cardiomegaly noted during a respiratory illness. Her diagnosis was made by muscle biopsy findings, reduced GAA enzyme activity, and homozygosity for the c.2560C>T mutation in the GAA gene. She was determined to be cross-reactive immunological material (CRIM)-negative by Western blot. Recombinant alglucosidase-alpha infusions were initiated at 6 months of age at 20 mg/kg every week. Due to CRIM-negative status, she received a course of immunomodulation therapy using rituximab, methotrexate, and intravenous immunoglobulin (IVIG) when ERT was initiated. She developed peak IgG titers of 12,800 at eight weeks after initiation of ERT. She received a second round of immunomodulation, and peak titers were 25,600 after this intervention.
She had a history of poor feeding, gastroesophageal reflux, reduced diaphragmatic muscle movement, and respiratory insufficiency and received a tracheostomy and gastrostomy tube at 7 months of age. This child was diagnosed with dysphagia at 15 months of age. Gross and fine motor development remained delayed throughout life, with scores less than 5th percentile at 15 and 22 months of age on the Alberta Infant Motor Scale (AIMS). She had osteopenia, as evidenced by a Z-score of −4.4 in lumbar vertebrae on a DEXA scan at 16 months of age. Cardiac function and left ventricular mass improved with enzyme replacement therapy (Table 1). However, she had electrocardiographic evidence of accelerated cardiac conduction throughout her life. She had a sudden death at 21 months of age from a presumed arrhythmia.
Postmortem Examination
Autopsy findings are summarized in Table 2.
Smooth Muscle
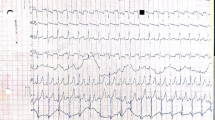
Glycogen accumulation in smooth muscle was severe in the iris sphincter muscle of the eyes and in the urinary bladder and mild in the distal esophagus (Fig. 1a, b), stomach, small intestine, and colon.
(a, b) There was mild vacuolar myopathy of smooth muscle (*) and moderate vacuolar myopathy of skeletal muscle (**) in the mid esophagus of patient 1 (hematoxylin and eosin; magnification bars = 500 μm in a and 100 μm in (b). (c, d) The sinoatrial node (*) of patient 1 had severe vacuolation of the specialized myocytes comprising this structure, along with severe vacuolar myopathy of the right atrial cardiac myocytes (hematoxylin and eosin, magnification bars = 500 μm in c and 50 μm in d). (e, f) Smooth muscle cells and some neurons within ganglia of the myenteric plexus (*; Auerbach’s plexus) of the small intestine of patient 2 were laden with glycogen (e: periodic acid-Schiff stain and f: periodic acid-Schiff stain after diastase digestion of glycogen; magnification bar = 50 μm). (g, h) Anterior horn neurons (*) of the spinal cord of patient 2 exhibited prominent glycogen accumulation (a: periodic acid-Schiff stain and b: periodic acid-Schiff stain after diastase digestion of glycogen; magnification bar = 50 μm for both g and h). (i, j) The bundle of His (*) in patient 3 had moderate vacuolation of its specialized myocytes (hematoxylin and eosin; magnification bars = 100 μm in I and 50 μm in j)
Cardiac Muscle
There was glycogen accumulation in the cardiac conduction system, with severe vacuolization of cells at the sinoatrial node (Fig. 1c, d), atrioventricular node, and the bundle of His.
Nervous System
Unfixed brain weight was 1,165 g (normal for age is 1,026.6–1,154.1 g, Stocker and Dehner 2001). There was moderate ventricular dilatation. Glycogen accumulation was evident in neurons of the cortex, midbrain, pons, medulla, cerebellum, and spinal cord. There was cytoplasmic storage material in glial cells of white matter, in the temporal neocortex, and in neurons and glia of the basal ganglia and internal capsule, caudate, and thalamus. The patient also had ballooned neurons in the substantia nigra, the dorsal raphe nuclei, the pontine nuclei, and in the inferior olivary nuclei with periodic acid-Schiff (PAS) staining of the material in the cytoplasm. There were also ballooned neurons with positive PAS staining in the dentate nucleus, neurons, glial cells, and white matter of the cerebellum. Purkinje cells in the cerebellum were relatively spared of glycogen accumulation. The patient had large ballooned neurons in the anterior horns of the spinal column. There were vacuolar changes consistent with glycogen accumulation in the sural nerve and ganglia of the small intestine and colon.
Eyes
The patient had severe vacuolation in lens epithelial cells, moderate glycogen accumulation in retinal ganglion cells, and mild accumulation in corneal endothelial cells.
Other Findings
Moderate vertebral osteoporosis was present.
Patient 2
This African American female was noted to have hypotonia and poor feeding at 3 months of age. She was diagnosed with cardiomyopathy and subsequently with CRIM-negative infantile Pompe disease after presentation with a respiratory illness at 4 months of age. Her diagnosis was established by deficiency in GAA enzyme activity in muscle and fibroblasts and compound heterozygosity for mutations in the GAA gene: c.766_785del_ins_C (p.Tyr256fsX6) and c.2432delT (p.Leu811fsX37). As this child received a diagnosis of Pompe disease prior to regulatory approval of ERT, treatment was started at 8 months, without immunomodulation. The patient developed inhibitory antibodies four weeks after initiation of therapy and had peak titers of 102,400 at 12 weeks after initiation of ERT. She had left ventricular hypertrophy and decreased function at initiation of treatment, with minimal short-term improvement while receiving ERT (Table 1). She was diagnosed with obstructive apnea and hypoventilation and required noninvasive ventilation at 11 months of age. She had aspiration on a swallow study at 11 months of age and required nasogastric feedings. She died at almost 12 months of age after an episode of emesis and subsequent cardiopulmonary arrest.
Postmortem Examination
Smooth Muscle
Glycogen was present in the smooth muscle of blood vessels, gastrointestinal (Fig. 1e, f) and respiratory tracts, myometrium, iris sphincter, and ciliary body.
Nervous System
Unfixed brain weight was 733 g (mean for age 886 g, standard deviation 64 g, Stocker and Dehner 2001). She had unremarkable ventricles without evidence of dilatation. PAS-positive material had accumulated in the glial cells and astrocytes within the white matter and in the cytoplasm of neurons of multiple brainstem nuclei, including the oculomotor, pontine, and inferior olivary nuclei. There was glycogen accumulation in astrocytes of the cerebellar white matter, although the Purkinje cells were relatively spared. The child also had glycogen accumulation in ganglion cells of the GI tract, adrenal glands, pancreas, and anterior horn of the spinal cord (Fig. 1g, h).
Eyes
There was prominent vacuolization and PAS staining of the iris sphincter and lens epithelial cells, as previously described by Yanovitch et al. (2010). There was also PAS-positive material in the corneal endothelium, iris pigment and lens epithelium, retinal ganglion cells, and inner plexiform layer of the retina. Transmission electron microscopy demonstrated glycogen accumulation within lysosomes of scleral fibroblasts, retinal ganglion cells, and cells of the retinal inner nuclear layer. In addition, glycogen accumulation was more prominent in bipolar and Müller cells than in amacrine and horizontal cells of the inner retinal nuclear layer.
Patient 3
This African American male infant was diagnosed at 5 months of age with Pompe disease during a hospitalization for respiratory symptoms. He was homozygous for the c.2560C>T mutation in the GAA gene and was determined to be CRIM-negative by Western blot. Enzyme replacement therapy at 20 mg/kg every other week and immune modulation with rituximab and methotrexate were started shortly after diagnosis. Hypertrophic cardiomyopathy and severe decrease in fractional shortening were present at diagnosis, and fractional shortening had some improvement with ERT (Table 1). Swallow study at 6 months of age demonstrated severe oropharyngeal dysphagia and aspiration with all consistencies. The child had delayed motor milestones, with an AIMS score less than 1st percentile at initial evaluation at 5.5 months of age. IgG titers remained negative during ERT. He was diagnosed with subglottic stenosis at 7 months of age and had a cardiopulmonary arrest at 7.5 months of age.
Postmortem Examination
Smooth Muscle
Glycogen accumulation was observed in smooth muscle of blood vessels and the respiratory and gastrointestinal tracts.
Cardiac Muscle
Moderate vacuolation in the specialized myocytes of the bundle of His was present (Fig. 1i, j).
Nervous System
Unfixed brain weighted 796 g (mean for age 767 g, standard deviation 32 g, Stocker and Dehner 2001). There was no evidence of ventricular dilatation. Glycogen accumulation was observed within cranial nerve nuclei of the mid pons and neurons of the dorsal raphe of the medulla. There was also glycogen accumulation in ganglion cells of the gastrointestinal tract and in the spinal cord. Vacuolation was present in the sural nerve.
Other Findings
The child had severe subglottic stenosis due to a circumferential tracheal fibrotic ridge. Glycogen accumulation in the urothelium and the eccrine glands of the skin was noted.
Discussion
We reviewed postmortem data in three patients with infantile Pompe disease as a method to correlate pathology in deceased individuals with complications observed in long-term survivors. Postmortem findings are summarized in Table 2. Our current understanding of the natural history of infantile Pompe disease is somewhat limited by lack of pathophysiological correlates, and autopsy findings can inform clinical observations. A sample of autopsy findings in past publications is summarized in Table 3. All decedents presented in our case series were CRIM-negative, diagnosed in the first six months of life, and treated with ERT. It is unclear if ERT modified glycogen accumulation throughout the body, as serial sampling from pre-mortem tissue was not available. The cause of death varied but appeared to be a sudden cardiac death in at least two.
All of the individuals had a clinical history of oropharyngeal dysfunction and gastroesophageal reflux. Glycogen accumulation was observed in skeletal muscle of the tongue and proximal and mid esophagus in the three cases. We note a previous report of glycogen accumulation in the tongue (Araoz et al. 1974) and of tongue weakness in individuals with IPD and LOPD (Jones et al. 2010; Dubrovsky et al. 2011; Maggi et al. 2013) as a likely contributor to oropharyngeal dysfunction in the current cases. There was also glycogen accumulation in the smooth muscle of the mid and distal esophagus, and we posit that weakness of the lower esophageal sphincter could contribute to gastroesophageal reflux.
The three cases presented in this series had glycogen accumulation throughout the smooth muscle of the gastrointestinal and genitourinary tracts. This finding could provide a pathophysiologic mechanism for small and large intestinal dysmotility and bowel control in this cohort. Bowel dysfunction and urinary incontinence have been reported in adults with LOPD, likely related to decreased anal sphincter pressure and fatty infiltration of pelvic floor musculature (Remiche et al. 2012; McNamara et al. 2015), along with glycogen accumulation in smooth muscle of the bladder (Hobson-Webb et al. 2012), and within neurons of the submucosal (Meissner’s) and myenteric (Auerbach’s) plexuses of the small and large intestines (Bernstein et al. 2010). We have observed urinary and bowel incontinence in several long-term survivors with infantile Pompe disease, an area that would benefit from long-term follow-up studies (Tan et al. 2013).
Glycogen accumulation in the smooth muscle of blood vessels was noted in the three decedents. Dilated arteriopathy has been reported in adults with LOPD (Quenardelle et al. 2014; El-Gharbawy et al. 2011), and very recently in a long-term survivor of infantile Pompe disease (Patel et al. 2013), in addition to dolichoectasia of the basilar artery and ectasia of the internal carotids (Sacconi et al. 2010; Laforêt et al. 2008). Glycogen accumulation in smooth muscle may affect cellular contractility and thus weaken blood vessel walls.
Glycogen accumulation in the cardiac conduction system in cases 1 and 3 is an interesting observation in Pompe disease that has only been reported once before (Bharati et al. 1982). A potential clinical correlate is evidence of preexcitation on electrocardiograms for case 1 and shortened conduction time in a postmortem electrogram on bundle of His tissue (Nakamura et al. 1979). Several long-term survivors have experienced arrhythmias (McDowell et al. 2008; Prater et al. 2012), and we propose that cardiac conduction is affected by glycogen accumulation within the conduction system. Glycogen accumulation in the cardiac conduction system is present in glycogen storage disease type III and in the mouse model for PRKAG2-caused hypertrophic cardiomyopathy (Austin et al. 2012; Arad et al. 2003). Persistence of glycogen in cardiac conduction tissue, despite ERT, suggests poor penetration and a potential cardiac cause for sudden death in cases 1 and 3.
We observed glycogen accumulation in various ocular structures. We have recently described a high prevalence of myopia and astigmatism in long-term survivors with IPD and posited various ways that glycogen accumulation in ocular tissues may contribute to these issues (Prakalapakorn et al. 2014).
There was extensive glycogen accumulation in the central and peripheral nervous systems. The pattern of accumulation included neurons and glial cells of the white matter, brainstem, and cerebellum, with relative sparing of cerebellar Purkinje cells. Glycogen accumulation has previously been reported throughout the central nervous system (Araoz et al. 1974; Sakurai et al. 1974; Asukata et al. 1976; Nakamura et al. 1979; Teng et al. 2004; Thurberg et al. 2006). The decedents also had extensive accumulation in anterior horn cells of the spinal cord and in intestinal ganglion cells, as described previously (Thurberg et al. 2006; Martini et al. 2001; Teng et al. 2004). Glycogen accumulation has also been observed in peripheral nerves in LOPD (Fidziańska et al. 2011). A clinical correlate for this observation is a reduction in amplitudes and absent motor units on nerve conduction studies in a case of infantile-onset Pompe disease (Burrow et al. 2010). Glycogen accumulation in the peripheral nervous system raises the possibility that the weakness observed in affected individuals may be partly neurogenic.
While none of our three patients had pre-mortem MRI of brain, patient two in this case series had mild, diffuse volume loss on CT scan of the head at 8 months of age, and there was blurring of the gray-white differentiation for patient 3 at 5 months of age. Neuronal loss in brain and spinal cord has been described in postmortem examination (Martini et al. 2001). A recent publication noted parenchymal volume loss on brain MRI in a child with infantile Pompe disease at 2 years of age (Burrow et al. 2010). Interestingly, the oldest patient in the current case series, patient 1, had dilatation of the ventricles on postmortem examination. Ventricular dilatation was also observed in brain MRI in three of five participants who had serial MRI scanning (Chien et al. 2006). Finally, serial MRI in a CRIM-negative patient demonstrated white matter abnormalities despite normal myelination (Rohrbach et al. 2010). Glycogen accumulation in central and peripheral nervous system in the GAA knockout mouse model 6neo(−)/6neo(−) was extensive, but varied in distribution and intensity. Accumulation was progressive and included neurons, glia, and pericytes of the cerebral cortex, portions of the basal ganglia, and the brainstem. Early glycogen accumulation was present in the spinal cord, particularly in motor neurons (Sidman et al. 2008).
It is unclear whether the observed brain abnormalities can impact cognitive development in individuals affected with infantile Pompe disease. Spiridigliozzi et al. (2012) noted differences in intellectual functioning between classic and atypical Pompe disease in a CRIM-positive cohort followed prospectively. Similar data for CRIM-negative individuals, however, is lacking, and it is unclear whether the differences observed in intellectual achievement are related to glycogen accumulation in the CNS.
Conclusion
This report expands our current understanding of pathologic correlates of clinical observations among long-term survivors (Table 4). Although limited to retrospective data, such review is nevertheless valuable in providing additional insight into potential complications in long-term survivors of infantile Pompe disease and may provide information for health care supervision. This study also highlights the value of postmortem analysis in understanding the pathophysiology of disease manifestations.
Abbreviations
- AIMS:
-
Alberta infant motor scale
- CRIM:
-
Cross-reactive immunological material
- ERT:
-
Enzyme replacement therapy
- GAA:
-
Acid alpha-glucosidase
- GSD:
-
Glycogen storage disease
- H&E:
-
Hematoxylin and eosin stain
- IPD:
-
Infantile Pompe disease
- IVIG:
-
Intravenous immunoglobulin
- LOPD:
-
Late-onset Pompe disease
- PAS:
-
Periodic acid-Schiff
- PASD:
-
Periodic acid-Schiff followed by diastase digestion
References
Arad M, Moskowitz IP, Patel VV, Ahmad F, Perez-Atayde AR, Sawyer DB et al (2003) Transgenic mice overexpressing mutant PRKAG2 define the cause of Wolff–Parkinson–White syndrome in glycogen storage cardiomyopathy. Circulation 107:2850–2856
Araoz C, Sun CN, Shenefelt R, White HJ (1974) Glycogenosis type II (Pompe’s disease): ultrastructure of peripheral nerves. Neurology 24:739–742
Asukata I, Aizawa S, Kosakai M, Kirino Y, Ishikawa E (1976) An autopsy case of type II glycogenosis. Acta Path Jpn 26:629–635
Austin SL, Proia AD, Spencer-Manzon MJ, Butany J, Wechsler SB, Kishnani PS (2012) Cardiac pathology in glycogen storage disease type III. JIMD Rep 31:65–72
Bernstein DL, Bialer MG, Mehta L, Desnick RJ (2010) Pome disease: dramatic improvement in gastrointestinal function following enzyme replacement therapy. A report of three later-onset patients. Mol Genet Metab 101:130–133
Bharati S, Serratto M, DuBrow I et al (1982) The conduction system in Pompe’s disease. Pediatr Cardiol 2:25–32
Burrow TA, Bailey LA, Kinnett DG, Hopkin RJ (2010) Acute progression of neuromuscular findings in infantile Pompe disease. Pediatr Neurol 42:455–458
Chien YH, Lee NC, Peng SF, Hwu WL (2006) Brain development in infantile-onset Pompe disease treated by enzyme replacement therapy. Pediatr Res 60:349–352
Dubrovsky A, Corderi J, Lin M, Kishnani PS, Jones HN (2011) Expanding the phenotype of late-onset Pompe disease: tongue weakness: a new clinical observation. Muscle Nerve 44:897–901
El-Gharbawy AH, Bhat G, Murillo JE et al (2011) Expanding the clinical spectrum of late-onset Pompe disease: dilated arteriopathy involving the thoracic aorta, a novel vascular phenotype uncovered. Mol Genet Metab 103:362–366
Fidziańska A, Ługowska A, Tylki-Szymańska A (2011) Late form of Pompe disease with glycogen storage in peripheral nerves axons. J Neurol Sci 301:59–62
Hobson-Webb LD, Proia AD, Thurberg BL, Banugaria S, Prater SN, Kishnani PS (2012) Autopsy findings in late-onset Pompe disease: a case report and systematic review of the literature. Mol Genet Metab 106:462–469
Jones HN, Muller CW, Lin M et al (2010) Oropharyngeal dysphagia in infants and children with infantile Pompe disease. Dysphagia 25:277–283
Kishnani PS, Nicolino M, Voit T et al (2006) Chinese hamster ovary cell-derived recombinant human acid alpha-glucosidase in infantile-onset Pompe disease. J Pediatr 149:89–97
Laforêt P, Petiot P, Nicolino M et al (2008) Dilative arteriopathy and basilar artery dolichoectasia complicating late-onset Pompe disease. Neurology 70:2063–2066
Maggi L, Salerno F, Bragato C et al (2013) Familial adult-onset Pompe disease associated with unusual clinical and histological features. Acta Myol 32:v85–v90
Martini C, Ciana G, Benettoni A et al (2001) Intractable fever and cortical neuronal glycogen storage in glycogenosis type 2. Neurology 57:906–908
McDowell R, Li JS, Benjamin DK et al (2008) Arrhythmias in patients receiving enzyme replacement therapy for infantile Pompe disease. Genet Med 10:758–762
McNamara ER, Austin S, Case L, Wiener JS, Peterson AC, Kishnani PS (2015) Expanding our understanding of lower urinary tract symptoms and incontinence in adults with Pompe disease. JIMD Rep [Epub ahead of print]
Nakamura Y, Tanimura A, Yasuoka C, Kato H (1979) An autopsy case of type II glycogenosis. Kurume Med J 26:349–354
Patel TT, Banugaria SG, Frush DP, Enterline DS, Tanpaiboon P, Kishnani PS (2013) Basilar artery aneurysm: a new finding in classic infantile Pompe disease. Muscle Nerve 47:613–615
Prakalapakorn SG, Proia AD, Yanovitch TL et al (2014) Ocular and histologic findings in a series of children with infantile Pompe disease treated with enzyme replacement therapy. J Pediatr Ophthalmol Strabismus 20:1–8
Prater SN, Banugaria SG, DeArmey SM et al (2012) The emerging phenotype of long-term survivors with infantile Pompe disease. Genet Med 14:800–810
Quenardelle V, Bataillard M, Bazin D, Lannes B, Wolff V, Echaniz-Laguna A (2014) Pompe disease presenting as an isolated generalized dilative arteriopathy with repeated brain and kidney infracts. J Neurol 262:473–475
Remiche G, Herbaut AG, Ronchi D et al (2012) Incontinence in late-onset Pompe disease: an underdiagnosed treatable condition. Eur Neurol 68:75–78
Rohrbach M, Klein A, Kohli-Wiesner A et al (2010) CRIM-negative infantile Pompe disease: 42-month treatment outcome. J Inherit Metab Dis 33:751–757
Sacconi S, Bocquet JD, Chanalet S, Tanant V, Salviati L, Desnuelle C (2010) Abnormalities of cerebral arteries are frequent in patients with late-onset Pompe disease. J Neurol 257:1730–1733
Sakurai I, Tosaka A, Mori Y, Imura S, Aoki K (1974) Glycogenosis type II (Pompe) – the fourth autopsy case in Japan. Acta Pathologica Japonica 24:829–846
Sidman RL, Taksir T, Fidler J et al (2008) Temporal neuropathologic and behavioral phenotype of 6neo/6neo Pompe disease mice. J Neuropathol Exp Neurol 67:803–818
Spiridigliozzi GA, Heller JH, Kishnani PS (2012) Cognitive and adaptive functioning of children with infantile Pompe disease treated with enzyme replacement therapy: long-term follow up. Am J Med Genet Part C 160C:22–29
Stocker JT, Dehner LP (eds) (2001) Pediatric pathology, 2nd edn. Lippincott Williams & Wilkins, Philadelphia, pp. 1444–1446, p. 1451
Tan QK, Cheah SM, DeArmey SM, Kishnani PS (2013) Low anal sphincter tone in infantile-onset Pompe disease: an emerging clinical issue in enzyme replacement therapy patients requiring special attention. Mol Genet Metab 108:142–144
Temple JK, Dunn DW, Blitzer MG, Shapira E (1985) The “muscular variant” of Pompe disease: clinical, biochemical and histologic characteristics. Am J Med Genet 21:597–604
Teng Y-T, Su W-J, Hou J-W, Huang S-F (2004) Infantile-onset glycogen storage disease type II (Pompe disease): report of a case with genetic diagnosis and pathological findings. Chang Gung Med J 27:379–384
Thurberg BL, Lynch Maloney C, Vaccaro C et al (2006) Characterization of pre- and post-treatment pathology after enzyme replacement therapy for Pompe disase. Lab Invest 86:1208–1220
Yanovitch TL, Banugaria SG, Proia AD, Kishnani PS (2010) Clinical and histologic ocular findings in Pompe disease. J Pediatr Ophthalmol Strabismus 47:34–40
Van den Hout H, Reuser AJ, Vulto AG, Loonen MC, Cromme-Dijkhuis A, Van der Ploeg AT (2000) Recombinant human alpha-glucosidase from rabbit milk in Pompe patients. Lancet 356:397–398
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Additional information
Communicated by: Carla E. Hollak, MD
Appendices
Synopsis
Pompe disease leads to generalized glycogen accumulation that may lead to with multi-organ complications in long-term survivors.
Compliance with Ethics Guidelines
Conflict of Interest
Loren Pena declares that she has no conflict of interest.
Alan Proia declares that he has no conflict of interest.
Priya Kishnani has received research/grant support and honoraria from Genzyme Corporation and is a member of the Pompe Disease Advisory Board for Genzyme Corporation.
Informed Consent
This study has been reviewed and granted exempt status by the Duke Medicine Institutional Review Board for Clinical Investigations as decedent research; hence the requirement for informed consent was waived.
Contributions by Individual Authors
Loren Pena wrote the protocol and manuscript with guidance from Alan Proia regarding tissue findings and from Priya Kishnani regarding clinical course.
Rights and permissions
Copyright information
© 2015 SSIEM and Springer-Verlag Berlin Heidelberg
About this chapter
Cite this chapter
Pena, L.D.M., Proia, A.D., Kishnani, P.S. (2015). Postmortem Findings and Clinical Correlates in Individuals with Infantile-Onset Pompe Disease. In: Zschocke, J., Baumgartner, M., Morava, E., Patterson, M., Rahman, S., Peters, V. (eds) JIMD Reports, Volume 23. JIMD Reports, vol 23. Springer, Berlin, Heidelberg. https://doi.org/10.1007/8904_2015_426
Download citation
DOI: https://doi.org/10.1007/8904_2015_426
Received:
Revised:
Accepted:
Published:
Publisher Name: Springer, Berlin, Heidelberg
Print ISBN: 978-3-662-47466-2
Online ISBN: 978-3-662-47467-9
eBook Packages: MedicineMedicine (R0)