Abstract
The search for biomarkers to aid in the diagnosis and prognosis of psychiatric conditions and predict response to treatment is a focus of twenty-first century medicine. The current lack of biomarkers in routine use is attributable in part to the existing way mental health conditions are diagnosed, being based upon descriptions of symptoms rather than causal biological evidence. New ways of conceptualizing mental health disorders together with the enormous advances in genetic, epidemiological, and neuroscience research are informing the brain circuits and physiological mechanisms underpinning behavioural constructs that cut across current diagnostic DSM-5 categories. Combining these advances with ‘Big Data’, analytical approaches offer new opportunities for biomarker development. Here we provide an introductory perspective to this volume, highlighting methodological strategies for biomarker identification; ranging from stem cells, immune mechanisms, genomics, imaging, network science to cognition. Thereafter we emphasize key points made by contributors on affective disorders, psychosis, schizophrenia, and autism spectrum disorder. An underlying theme is how preclinical and clinical research are informing biomarker development and the importance of forward and reverse translation approaches. In considering the exploitation of biomarkers we note that there is a timely opportunity to improve clinical trial design informed by patient ‘biological’ and ‘psychological’ phenotype. This has the potential to reinvigorate drug development and clinical trials in psychiatry. In conclusion, we are poised to move from the descriptive and discovery phase to one where biomarker panels can be evaluated in real-life cohorts. This will necessitate resources for large-scale collaborative efforts worldwide. Ultimately this will lead to new interventions and personalized medicines and transform our ability to prevent illness onset and treat complex psychiatric disorders more effectively.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Affective disorders
- Autism spectrum disorder
- Diagnostic biomarker
- Early intervention
- Forward and reverse translation
- Genetics
- Genomics
- Immune
- Inflammation
- Patient stratification
- Personalized medicines
- Predictive biomarker
- Prognosis biomarker
- Psychosis
- Schizophrenia
- Stem cells
1 Introduction
A quest of contemporary medicine is to provide improved patient care, through early intervention and personalized medicines. For conditions such as cancer and diabetes, the discovery and development of biomarkers has had a large impact on management and treatment. However, the development of biomarkers for psychiatric conditions has lagged behind that of other areas of medicine, with no biomarkers currently in routine use for the major psychiatric disorders. This lack of relevant biomarkers has represented a major impediment to improved care and the development of new treatments for these common and impactful conditions.
Whilst there are multiple reasons for this, a key factor is the current way mental health conditions are diagnosed (see Prata et al. 2014; Kalia et al. 2015; Scarr et al. 2015). Current diagnosis of these conditions through DSM-5 and ICD10 relies on descriptions of symptoms rather than utilizing causal biological evidence. As a consequence, broad syndromes encompassing a range of symptoms result in disorders being overtly heterogeneous in nature. Furthermore, traditional diagnostic methods lack reliability and at present the ability to predict prognosis and response to treatment are limited. Hence the ability to align broad-based disease domains with biomarker discovery is particularly challenging.
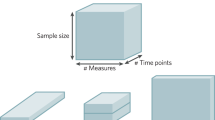
The launch of the Research Domain Criteria (RDoC) project by the National Institute of Mental Health (http://www.nimh.nih.gov/research-priorities/rdoc/index.shtml) some 10 years ago has led to new ways of conceptualizing mental health disorders out with DSM-5. In essence RDoC proposes that mapping the cognitive, circuit, and genetic aspects of mental disorders will yield new and better targets for treatment. This research framework provides opportunities to stratify patients for improved treatment options. Hence adopting an RDoC approach offers great opportunities for biomarker identification and development. Part of the ethos of RDoC is to align preclinical and clinical research, through forward and reverse translation. For example, it is envisaged that by assessing neural imaging and behavioural ‘biomarkers’ in preclinical models of disease risk (e.g. genetic risk variant) could assist in the discovery of new treatments and predict which treatments are likely to be most effective in a subset of patients.
In considering biomarkers, it is important to articulate their purpose; for Psychiatry, they can be considered broadly useful for
-
1.
Diagnosis – including identification of those at high risk.
-
2.
Prognosis – Assessment or prediction of the course of the disorder.
-
3.
Prediction of treatment response (therapeutic or adverse).
Understanding the neurobiology of neuropsychiatric disorders is key to the process of identifying and developing biomarkers. Given the complexity of psychiatric disorders, this will require a multidisciplinary approach. In recent years, enormous strides have been made in understanding the causes of mental health disorders. This has been driven in part from advances in genetics, epigenetics, omics, neurochemistry, physiology, imaging and behavioural technologies that enable the probing of the human brain with greater precision from early in neurodevelopment through to adolescence and adulthood.
2 Methodological Strategies for Biomarker Identification and Development
The initial chapters inform how technological advances are providing insights into the utility of biomarkers from the genetic and cellular level through to imaging and behaviour.
Johnstone et al. (2018) discuss recent advances in human induced pluripotent stem cell (hiPSC) technology for understanding neurodevelopmental disorders such as schizophrenia and autism, and also affective disorders. They highlight the promises and pitfalls of reprogramming cell fate for investigation of these disorders and provide recommendations for future directions which may lead to biomarker identification.
Herron et al. (2018) review the diverse range of pro-inflammatory mediators implicated in psychiatric disorders. Although the mechanisms through which altered inflammatory signaling impact on brain, mood and behaviour is unclear, several possible mechanisms have been proposed. For example, the enhanced levels of cytokines (released from brain microglia or by accessing the brain from the periphery through traversing the BBB or via vagus neural feedback) are hypothesized to impact on brain serotonin, dopamine and glutamate systems together with modifying BDNF expression. It is notable that several cytokines (IL-6, TNF alpha, IL-1beta) are altered in depression, schizophrenia and bipolar disorder, raising questions about a common role of inflammatory mediators in psychiatric illness. Interestingly in depression markers of inflammatory response are reported to reduce in response to treatment. Herron et al. conclude that notwithstanding the challenges of the heterogeneity of psychiatric disorders and the dynamic nature of the immune response, neuroimmune biomarkers hold the potential for stratification of illness, personalized treatments and may inform the development of immunologically targeted therapeutics.
Lydon-Staley and Bassett (2018) provide insight into how recent advances in the field of applied mathematics (specifically network science) provide a language to articulate how brain regions interact with each other at the structural and functional level. By analogy with, for example, social and transport networks, algorithms from network science enable the properties of a network to be interrogated. This work has enabled major advances in our understanding of brain connectivity during development and changes (dysconnectivity) arising from genetic and environmental factors that may lead to mental health conditions; particularly schizophrenia and depression. Lydon-Staley and Bassett note that the ‘applications of network analysis have revealed organizational principles of healthy brains that allow for efficient, flexible, and robust information processing and how this may deviate in psychiatric disorders’. Importantly these recent advances have moved the brain imaging field from one where local changes in structure and function are visualized to one where the dynamic interactions of brain structures can be characterized, which will be of particular value for the development of biomarkers.
MacQueen et al. (2018) highlight the utility of RDoC constructs as potential cognitive biomarkers which cross existing diagnostic categories. In particular, they focus on the constructs of attention, cognitive control, working memory, declarative memory, perception and language along with relevant subdomains. Consideration is given to linking neural processes to these constructs and the techniques available to measure these in human and preclinical models. By utilizing forward and reverse translation techniques to assess cognitive constructs it is argued that animal models can provide insight in dysfunction relevant to cognitive disorders and that potential treatments for a particular cognitive dysfunction can be tested similarly first in preclinical models and then in patient populations.
3 Preclinical and Clinical Research to Inform Biomarkers for Affective Disorders, Psychosis, Schizophrenia and Autism Spectrum Disorder
In subsequent chapters, there is a focus on how preclinical and clinical research are informing biomarker development for affective disorders, psychosis and autism.
Slaney et al. (2018) discuss the challenges of developing preclinical models relevant to depression, which can aid in biomarker identification. They note the limitations of conventional animal models of depression such as the forced swim/tail suspension test and reward sensitivity tests such as the sucrose preference test. For the latter, it is notable that patients with depression do not show similar deficits when tested using techniques which assess ‘in the moment’ pleasure. Clearly a major limitation is the challenge of developing animal models for disorders currently diagnosed by a description of symptoms. Slaney et al. provide persuasive evidence that neuropsychological deficits, specifically affective biases, (observed when emotional states affect cognitive function) evident in major depressive disorder, can inform the development of translational tasks in animals. In this regard, they review evidence that assessment of affective bias in rodents is feasible and has utility for predicting antidepressant efficacy as well as pro-depressant risk.
Battaglia and Khan (2018) focus on preclinical models for panic disorder and separation anxiety disorder involving early life interference with parental care. In common with the clinical conditions, CO2 hypersensitivity represents a common biomarker. In their review they discuss the possible mechanisms underpinning this pathophysiological readout, including gene–environment interactions and epigenetic changes and the implications for biomarker development.
Maron et al. (2018) emphasize the high prevelance rates of anxiety diosrders, their hetereogeneity and limitations in being treating successfully. In this review, they consider the large volume of data generated on clinical evidence from neuroimaging and genetic measurements as biomarkers in anxiety disorders, covering generalized anxiety disorder, panic disorder, social anxiety disorder, simple phobias as well as obsessive compulsive disorder and post-traumatic stress disorder, that are no longer part of the anxiety category in DSM-5. Although it is apparent that the amygdala is important in the expression of anxiety and the medial prefrontal cortex in restraining it, no biomarkers have yet to be associated with discrete anxiety disorders. Similarly genetic variants that are robustly associated with these particular disorders have yet to be confirmed. It is predicted that future research on gene-environmental factors combined with imaging and hormone biomarkers could lead to a panel of biomarkers for diagnosis and treatment management.
Notter (2018) provides a critical insight into immunological processes in schizophrenia pathology and their potential as biomarkers. Following an overview of immune system components, Notter reviews the results of immune dysfunctions along the clinical course of schizophrenia and discusses this in the context of their potential as predictive, trait or state biomarkers. On a negative note it appears that immune dysfunction in schizophrenia may be as heterogeneous as the condition itself. Nevertheless, this provides an opportunity for patient segregation based upon their immune profile. Clearly this type of stratification may help in the development and introduction of immune modulating drugs for specific groups of patients defined by their ‘immune biomarker’ profile. It is perhaps ironic that an association of schizophrenia with immune system dysfunction was postulated over a century ago, yet genetic evidence of genes that play an important role in immune functioning and neurodevelopment (e.g. complement component 4) was discovered very recently.
Reddaway et al. (2018) review advances in the genetic and genomic understanding of schizophrenia, and highlight the ways that this information may be used to better stratify patients to existing or new treatments. In addition they examine the way genetic information can be used to identify imaging markers associated with risk for disease through genomic imaging approaches. They particularly focus on studies examining the aggregated polygenic effect of common risk variants on brain structure and function, as well as the impact of rarer but more penetrant genetic variants such as chromosomal micro-deletions at 22q11.2. Overall the chapter highlights the value of integrating genetic information with imaging and other biomarker studies in order to define biologically relevant markers.
Hunter and Lawrie (2018) review the current status of imaging and genetic biomarkers predicting transition to psychosis. The early detection and intervention of high risk groups has been proposed as the most effective way of improving outcomes in individuals who transition to psychosis. Important advances in the understanding of dynamic brain changes that occur during the transition from health to a psychotic disorder have been obtained from longitudinal follow-up studies. Imaging studies have shown grey matter abnormalities in frontal, cingulate and temporal cortices, hippocampal structures and the cerebellum as being potentially predictive of those patients who will develop a psychotic disorder. Similarly, the development of polygenic risk scores (a measure of the cumulative genetic risk generated through the combination of many SNPs) is showing increased predictive power. Hunter and Lawrie emphasize the power of combining genetic and imaging data as being more effective than either biomarker alone. They note that continued advances in the genetics field along with ‘the application of machine learning techniques and imaging protocols in the context of every increasing computational power offer novel and exciting approaches to the development of tools that in their view likely, one day, offer clinicians a viable and acceptable method of assisting in complex diagnostic and treatment decisions’.
Pratt et al. (2018) discuss advancement in preclinical models for biomarker identification in schizophrenia. They note the importance of adopting a reciprocal forward and reverse translation approach as exemplified in RDoC for discovering panels of biomarkers for diagnosis, prognosis and treatment response. In particular, they emphasize that for preclinical biomarkers to translate to a clinically relevant outcome they should be measured in preclinical models of translational value and high validity. In this context, the review focusses on relevant imaging, electrophysiological, biochemical and cognitive behavioural modalities (informed by CNTRICS) in preclinical models based upon the glutamate hypofunction hypothesis, genetic and environmental risk factors for schizophrenia (reverse translation). Furthermore, the importance of forward translation is exemplified by the example that preclinical research has identified the thalamic reticular nucleus as a locus of brain dysfunction in schizophrenia which has recently been demonstrated in schizophrenia samples.
Andrews et al. (2018) provide an overview of the complex interactions between the many genetic and environmental factors implicated in autism spectrum disorder (ASD). They note that a major challenge in development of biomarkers for ASD is due to the aetiological and phenotypic complexity. In their review, they present evidence that new techniques, specifically combining neuroimaging with ‘machine learning’ based pattern classification methods may assist in making individual diagnostic predictions. Ultimately these ‘brain imaging’ biomarkers may not only assist in diagnosis but also help in the discovery and development of personalized treatments.
4 How Can Biomarkers Be Best Exploited?
Current research is shaping the way forward for the development of panels of biomarkers. This relies on the ever-increasing sophistication of ‘Big Data’ analytical approaches, whereby multifactorial, multidisciplinary findings can be integrated to reveal and test the sensitivity, specificity and reproducibility of biomarkers for early intervention, diagnosis and stratification.
The RDoC initiative, combined with fundamental advances in genetic, epidemiological and neuroscience research, is yielding new information on the circuits and physiological mechanisms underpinning particularly cognitive and behavioural constructs that cut across current diagnostic DSM-5 categories. Given that many disorders encompass a neurodevelopmental component and behavioural phenotypes (e.g. working memory deficits), that cross diagnostic categories, it is likely that ‘panels of biomarkers’ will be discovered that will enable the discovery and development of interventions suitable for treating particularly constructs (e.g. working memory) that cut across current diagnostic DSM-5 categories.
What are the prospects for Biomarkers in the twenty-first century Psychiatry? Notwithstanding, the existence of a small repertoire of biomarkers that already exist, namely a phamacogenetic biomarker for the side effects of clozapine along with a diagnostic biomarker to detect NMDA receptor antibodies in psychosis resulting from autoimmune limbic encephalitis, the closest biomarker for development is arguably an ‘early intervention in psychosis’ biomarker panel (incorporating genetic, imaging and behavioural biomarkers). The advanced status of research in this area supports ‘early intervention biomarker’ development as being ripe for translation into the clinic (see Hunter and Lawrie 2018). Ultimately, this would not only offer clinicians a method for assisting in complex diagnostic and treatment decisions, but importantly would have an enormous impact on patient care and society as a whole.
There is a timely opportunity to improve clinical trial design informed by patient phenotype. The availability of relevant biomarkers for psychiatric disorders, informed by advances in understanding of the underpinning biology, has the potential to reinvigorate drug development and clinical trials in psychiatry, which currently suffer from their reliance of “soft” endpoints. The assessment of therapeutic interventions is likely to yield richer data if patients are stratified according to their ‘biological’ and ‘psychological’ phenotypes. This would be the first step into the arena of personalized medicines.
From the reviews presented in this volume, it is clear that the journey towards the identification of biomarkers is poised to move from the descriptive and discovery phase to one where assessments of biomarker panels for diagnosis, patient stratification and treatment can be evaluated in real-life cohorts. This will require resources for large-scale collaborative efforts worldwide. In summary, we should view with optimism our capabilities to develop biomarkers that will ultimately lead to new interventions and transform our ability to prevent illness onset and treat complex psychiatric disorders more effectively.
References
Andrews DS, Marquand A, Ecker C, McAlonan G (2018) Using pattern classification to identify brain imaging markers in autism spectrum disorder. https://doi.org/10.1007/7854_2018_47
Battaglia M, Khan WU (2018) Reappraising preclinical models of separation anxiety disorder, panic disorder, and CO2 sensitivity: implications for methodology and translation into new treatments. https://doi.org/10.1007/7854_2018_42
Herron JW, Nerurkar L, Cavanagh J (2018) Neuroimmune biomarkers in mental illness. https://doi.org/10.1007/7854_2018_45
Hunter SA, Lawrie SM (2018) Imaging and genetic biomarkers predicting transition to psychosis. https://doi.org/10.1007/7854_2018_46
Johnstone M, Hillary RF, St Clair D (2018) Stem cells to inform the neurobiology of mental illness. https://doi.org/10.1007/7854_2018_57
Kalia M, Costa E, Silva J (2015) Biomarkers of psychiatric diseases: current status and future prospects. Metab Clin Exp. https://doi.org/10.1016/j.metabol.2014.10.026
Lydon-Staley DM, Bassett DS (2018) Network neuroscience: a framework for developing biomarkers in psychiatry. https://doi.org/10.1007/7854_2018_41
MacQueen DA, Young JW, Cope ZA (2018) Cognitive phenotypes for biomarker identification in mental illness: forward and reverse translation. https://doi.org/10.1007/7854_2018_50
Maron E, Lan C-C, Nutt D (2018) Imaging and genetic approaches to inform biomarkers for anxiety disorders, obsessive–compulsive disorders, and PSTD. https://doi.org/10.1007/7854_2018_49
Notter T (2018) Immunological processes in schizophrenia pathology: potential biomarkers? https://doi.org/10.1007/7854_2018_43
Prata D, Mechelli A, Kapur S (2014) Clinically meaningful biomarkers for psychosis: a systematic and quantitative review. Neurosci Biobehav Rev 45:134–141. https://doi.org/10.1016/j.neubiorev.2014.05.010
Pratt JA, Morris BJ, Dawson N (2018) Deconstructing schizophrenia: advances in preclinical models for biomarker identification. https://doi.org/10.1007/7854_2018_48
Reddaway JT, Doherty JL, Lancaster T, Linden DE, Walters J, Hall J (2018) Genomic and imaging biomarkers in schizophrenia. https://doi.org/10.1007/7854_2018_52
Scarr E et al (2015) Biomarkers for psychiatry: the journey from fantasy to fact, a report of the 2013 CINP think tank. Int J Neuropsychopharmacol 18(10):pyv042. https://doi.org/10.1093/ijnp/pyv042
Slaney C, Hinchcliffe JK, Robinson ESJ (2018) Translational shifts in preclinical models of depression: implications for biomarkers for improved treatments. https://doi.org/10.1007/7854_2018_44
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer International Publishing AG, part of Springer Nature
About this chapter
Cite this chapter
Pratt, J., Hall, J. (2018). Biomarkers in Neuropsychiatry: A Prospect for the Twenty-First Century?. In: Pratt, J., Hall, J. (eds) Biomarkers in Psychiatry. Current Topics in Behavioral Neurosciences, vol 40. Springer, Cham. https://doi.org/10.1007/7854_2018_58
Download citation
DOI: https://doi.org/10.1007/7854_2018_58
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-99641-7
Online ISBN: 978-3-319-99642-4
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)