Abstract
Introduction
Despite being a major physical protective barrier, the human skin is also a major source of several immune cells that participate in innate and adaptive immune responses therefore, it is described as “first line of immune defence”. The involvement of heat shock proteins (HSP) in skin immune responses has been demonstrated by their expression in response to skin stressors such as UV irradiation, heat, environmental, microbial invasion and in several inflammatory-autoimmune skin disorders, which ultimately present them as potential therapeutic targets. The loss of immunological tolerance to the critical self-antigens which leads to dysregulation of immune responses and amplified inflammatory reactions are the major characteristic features underlying most inflammatory-autoimmune diseases. In spite of the recent successes recorded with novel immunosuppressive biological therapies and the use of atopic medications in the treatment of inflammatory/autoimmune skin diseases, their use remains a burden because they neither provide permanent solution to the interaction between pathogenic and protective immune responses nor offer permanent state of medicine-free disease remission. Our aim is to better understand the key players in the pathophysiology of various inflammatory-autoimmune skin disorders, which would have significant impact towards improved therapy.
Methods
We reviewed all the relevant literatures on the therapeutic potential of heat shock proteins in human inflammation/autoimmune skin diseases.
Result
Several studies have reported the therapeutic potential of HSP in inflammatory/autoimmune skin diseases owing to their ability to induce the regulation of regulatory T-cells, which play critical role in induction and dysregulation of immune response leading to the progression of several inflammatory/autoimmune diseases.
Conclusions
Despite the progress made in determining the key players in pathophysiology of various inflammatory/autoimmune skin disorders, therapeutic treatment remain burdensome as most of these treatments are restricted to conventional immunosuppressive methods. These therapies however, do not provide permanent solution to the interaction between pathogenic and protective immune responses. With HSP being one of the key regulators of immune response to autoimmune inflammatory diseases, targeting HSP or HSP inhibitors in these diseases could provide a novel therapeutic approach in the treatment of autoimmune/inflammatory diseases.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Atopic dermatitis
- Autoimmune diseases
- Bullous pemphigoid
- Heat shock proteins (HSP)
- Inflammation
- Psoriasis
- Skin
1 Introduction
The skin is the largest external organ that provides both physical and microbial protection to the human body. It is composed of two main layers: epidermis and dermis [1]. The epidermis, being the outermost layer of the skin creates a waterproof barrier and plays an important role in the skin tone. This layer is composed of keratinized, stratified-squamous epithelium, closely packed with 95% of cells called keratinocytes, which produces keratin: a fibrous structural protein with an important role in hardness and water-resistance properties of the skin [2]. The dermis on the other hand, is considered the core integumentary system of the skin, and a layer lying beneath the epidermis, consisting of blood vessels, nerves, sweat glands, hair follicles, as well as tough connective tissues such as collagen and elastin fibres which provide structural support to the human skin [3]. Apart from protecting against physical barriers and external injuries (such as UV radiation, environmental stresses and microbial invasion), the skin like other parts of body is actively involved in immune responses and dynamic cellular interactions in order to maintain and regulate several key processes such as wound healing, angiogenesis, disease prevention and inflammation [4]. In addition, it has been hypotheiszed that the skin is the first line of immune defence and functions in immune surveillance. This is supported by the skin immunity and skin-associated lymphoid tissue (SALT) concept, which reveals the skin houses several types of immune cells (such as T and B cells, dendritic cells, mast cells, langerhan’s cells) that participate in both innate and adaptive immune responses [5].
Inflammation of the skin is described as an irritation of the skin from internal or external causes characterized by pain, itching, redness and dryness. Inflammation works to detect and neutralize invading pathogens including cancer cells and infectious agents that stimulate or triggers an immune response, hence playing a prominent role in the maintenance of the overall body health, as well as regulation of skin homeostasis. Additionally, when short-lived, inflammatory responses are said to be beneficial to the human body because it helps clear invading pathogens and initiates the process of healing and repair. However, long term inflammation has been associated with several inflammatory diseases of the skin including psoriasis, dermatitis and bullous pemphigoid [6].
As a result of constant exposure of the skin to microbial pathogens and other stressful stimuli (such as UV irradiation, cold, allergens, heat and reactive oxygen species), the skin frequently produces larger number of heat shock proteins (HSP), which enables its response to these stressors. These proteins are broadly classified into various groups according to their molecular weight, function, cellular location and sequence homology. They include ATP-dependent HSP (Hsp110, Hsp100, Hsp90, Hsp70, Hsp60/65 and Hsp40) and ATP-independent HSP (small heat shock proteins-Hsp27 to Hsp10) [7]. The expression and synthesis of heat shock proteins or otherwise known as stress proteins is a universal phenomena taking place in all living cells studied including humans [8]. The study and identification of heat-inducible proteins date back to the early days of Ritossa in 1962, when he observed the dramatic increase in the expression of HSP in the salivary gland of the fruit fly Drosophila melanogaster in response to elevated temperature [9, 10]. Following the discovery of HSP, it was thought their functions were restricted to inducible signals such as heat, viral and bacterial infections, exercise, heavy metals, ischemia, gravity, oxidative stress, nutrient deficiency, inflammatory diseases and cancer [11]. Subsequent studies have however demonstrated that some of these proteins are constitutively expressed in different cellular compartments to perform various cellular functions ranging from protein folding, degradation of misfolded peptides, transportation of organelles across cellular membrane to signal transduction, hence giving them the less complimentary name of “molecular chaperones” [12, 13]. Although their expression pattern varies, it is noteworthy to state that these proteins do not work in isolation but are dependent on co-chaperoning activities or oligomerization to execute their biological functions [14].
Since discovery till date, it is not surprising that HSP have been the subject of huge strides in biological research, owing to their ever-present, abundant expression and diverse effects in the pathology of many diseases, especially human inflammatory diseases and cancer [15]. The roles of HSP in human skin inflammatory diseases, most especially psoriasis, atopic dermatitis, bullous pemphigoid and in other skin diseases, has been well documented. In fact, HSP has been reported to form part of the immune response capable of modulating inflammatory cascades through the inhibition of pro-inflammation mediators, hence encouraging its crucial role in the pathophysiology of several skin inflammatory disorders. Primarily, HSP are intracellular proteins involved in protein folding, refolding, degradation and translocation of organelles, however, their ubiquitous nature in the pathogenesis of several human diseases have escalated their therapeutic applications, Thus, herein the therapeutic potential of heat shock proteins in the following skin inflammatory diseases: psoriasis, atopic dermatitis and bullous pemphigoid is discussed.
1.1 Roles of HSP in Skin Inflammatory Diseases
Unresolved inflammatory reactions have been linked to various clinical manifestations, immunopathology and pathogenesis of several human inflammatory diseases. As a result, many studies have been oriented towards understanding and resolving the mechanisms of inflammatory reactions. These mechanisms include: apoptosis of inflammatory leukocytes, production of lipid mediators, macrophage repolarization and production of specific cytokines. In addition, proper regulation of these mechanisms are very important in controlling and managing inflammatory diseases, hence any powerful immune-modulator that regulates propagation of these mechanisms can be seriously considered as potential therapy in human inflammatory diseases. The roles of HSP in modulating immune cascades leading to inflammatory reactions via inhibition of pro-inflammatory cytokines or mediators has been elucidated [11, 16]. For instance, most chronic inflammatory diseases are autoimmune diseases caused by the dysregulation and inappropriate stimulation of the immune system leading to a loss of tolerance to self-antigens, which degenerates into the immune system attacking its own cells.
1.2 Atopic Dermatitis
Atopic dermatitis (AD) is a common, chronic inflammatory skin disease characterized by intense itching or highly pruritic and inflammatory eczematous lesions that often leads to substantial sleep disturbance, as well as skin trauma, with significant impact on the quality of life of the affected persons and care givers [17]. Recently, AD has become one of the most common chronic skin disorders that affects nearly 5% of the population in developed countries and an increase in the life-time prevalence of AD has been reported in the last 30 years. In fact, it is estimated that about 10–20% of children and 1–2% of adults suffers from this skin illness in the Western countries [18]. Furthermore, it is noteworthy to mention that children with AD are very susceptible to developing asthma, food allergies (eggs and peanut) and allergic rhinitis, the latter is more likely to cause severe form of the disease [19, 20].
Although the pathogenesis of AD is still unclear, it has been reported that the complex interactions between subvert skin barrier function, infectious agents, environmental factors and immune dysregulations contribute immensely to the pathology of AD [21]. A genetic defect in the gene that codes for filaggrin, a filament aggregating protein known to bind keratin fibres in epithelial cells has been associated with the disruption of the epidermal layer, which is a hallmark of AD pathogenesis and its clinical manifestation [22]. Filaggrin protein is a protective barrier that plays an important role in structural organization, as well as in the maintenance of skin homeostatic balance in general [23]. A disrupted filaggrin layer allows for the entering of allergens and microbes into the dermis, thus provoking systemic allergic responses such as immunoglobulin E (IgE) reaction, leading to a direct interaction between antigens (specifically Staphylococcus aureus, which is predominantly present in nearly 90% of AD patients) from the external environment and the dermis’ immune cells (such as Th2 & Th1 cells, chemokines and cytokines), which intensifies scratching, itching and inflammation: the characteristic features of AD [21, 24, 25]. In addition, AD can emanate as a result of imbalance or interaction disturbance between Th2 and regulatory T cells leading to disruption of epidermal cells and complex interaction of skin immune cells, perpetuating the itchy-scratch cycle as proposed by Hägermark and Wahlgren [26], which result in the loss of skin barrier integrity causing dryness of the skin [27] as shown in Fig. 1.
The skin of atopic dermatitis patients (ranging from acute atopic dermatitis in its weeping, blistering form; eczema herpeticum in a young girl; close-up photograph of the skin demonstrating dramatic xerosis to subacute atopic dermatitis in its dry, scaly, papular form; leg of an infant with atopic dermatitis demonstrating xerosis). Diagram taken from Berke et al. [24]
Interestingly, AD skin diseased are prone to similar stressful signals such as infection, UV irradiation, mechanical injuries, miscellaneous topic medications and environmental stimuli, which also enhances the induction of HSP expression, of which their cytoprotective functions in inflammatory diseases are well documented ([28]). More so, the heat shock protein family HSP60 in particular has been reported to act as bystander antigen due to its wide expression in the inflammation sites and recognition by immune-competent T cells. Evidence from skin lesions of patients suffering from Behcet’s disease, atherosclerosis, juvenile idiopathic arthritis and diabetes mellitus, present Hsp60 as a potential candidate in the management of various inflammatory diseases ([29, 30]). In almost all the AD skin lesions studied, infiltrating cells and keratinocytes expresses various heat shock proteins (Hsp65 and Hsp72/73) and the intensity of their expression seems to correlate with the severity of the disease lesions [28]. Taken together, these findings suggest roles for HSP in the pathogenesis of AD, although the exact mechanisms that mediate this relationship in AD skin lesions are poorly understood. However, based on the existing evidence of enhanced expression of HSP27 in response to environmental stress factors in AD patients [31] and considering the roles of HSP in the healing and repairing processes in general, it is safe to speculate that over-expression of these proteins in the skin of AD patients promotes the repairing processes through inflammatory and innate immune responses.
1.3 Psoriasis
Psoriasis is a common, multifactorial, chronic, autoimmune inflammatory skin disorder that can be triggered by a complex interaction between environmental factors (e.g. stress, physical trauma, cigarette smoking and infection), immunology and genetic factors, which sometimes lead to disfiguring features in affected individuals [32]. Generally, psoriasis affects approximately 1–3% of the world’s population, and is caused by different contributing factors, although these factors vary from individual to individual [33, 34]. While the actual cause of psoriasis is not fully understood, it believed that dyregulation of auto-immune T cells network, which include various cytokines (IL-17, IL-12, IL-22) resulting in abnormal proliferation and differentiation of keratinocytes leads to the “cellular immune confusion” with the immune system attacking its own cells. Consequently, the process of production and regulation of immune cells in the keratinocytes switches to overdrive, speeding up the abnormal production and regulation of the immune cells in that area of the skin [35]. This process, together with colonizing cells (in-flowing leucocytes-neutrophils) and several inflammatory cytokines secreted by the activated keratinocytes leads to the formation of psoriatic/scaly plaques characterised by pustular lesions [36, 37] as shown in Fig. 2; warmth and redness, which are the hallmarks of inflammatory response. There are several types of psoriasis, which include: inverse, guttate, erythrodermic and plague, with latter being the most severe and common form of psoriasis. The re-occurring, blistering red/pink spots, stigma and disfiguring nature of psoriatic infections often poses serious social, psychological and financial challenges on the infected individual [38, 39].
The psoriatic skin plaque (ranging from single plaque of psoriasis, well demarcated and heavily scaled, chronic plaque psoriasis to inverse psoriasis). Diagram taken from Griffiths and Barker [38]
Recently, growing knowledge of the role of innate and adaptive immunity in several inflammatory diseases including psoriasis exist. The roles of HSP in modulating immune response such as Th-1-type cytokine and Toll-like receptors (TLRs) as well as in psoriatic plaque have been well documented. These TLRs play crucial roles in mediating innate immune responses through the induction of proinflammatory cytokines production via the NF-kB mediated transduction pathways, as well as in recognizing numerous microbial-derived molecules [40, 41]. Furthermore, studies have shown that HSP are greatly expressed in psoriatic skin lesions and could have a huge role in the pathogenesis of psoriatic plaque ([42, 43, 44]). Although their exact function in psoriatic skin is not well known, it is believed that HSP could engage with innate immunity through the activation of IL-12, thereby contributing to Th1 cell that mediates the transition from symptomless to psoriatic skin lesion [45]. Similarly, in keratinocytes, binding of Hsp90 to CD91 receptor and activation of dendritic cells (DCs) results in antigen presentation, migration and production of proinflammatory cytokines. Considering the crucial role of activated DCs in the initiation of the psoriatic skin lesions, the secretion of Hsp90 by the stressed keratinocytes could play a prominent role in the mediation and pathogenesis of psoriasis [43]. Additionally, the chaperoning activities of Hsp90 promotes IL-17 signal, which induces proinflammatory cytokines such as tumor necrosis factor-α (TNF-α), contributing to the amplified loop of psoriatic lesion. A recent finding suggest Hsp90 involvement in the inflammation of the psoriatic lesion could provide a link between innate immune activation, keratinocytes stress and perpetuation of psoriatic inflammation therefore, inhibiting Hsp90 activities could be a promising therapeutic target towards improved psoriasis therapy [43]. Nevertheless, a result from topical treatment of alfalfa-derived Hsp70 (aHsp70) on mice psoriatic skin lesion suggests that its expression might decrease psoriasis pathogenesis through modulation of T cell activation, since psoriasis is an immune-related disease characterized by proliferation of keratinocytes, although exact mechanism needs to be elucidated in future studies [37].
1.4 Bullous Pemphigoid
Bullous Pemphigoid (BP) is the most common autoimmune and inflammatory skin disorder characterized by subepidermal blistering due to the disruption of dermal-epidermal junction by the binding of autoantibodies against the hemidesmosomal component of BP180 and BP230. Bullous Pemphigoid is an acquired autoimmune condition that mostly affects elderly people over the age of 60 years, even though the rare incidence at infancy and early childhood development has been reported. Additionally, BP occur evenly in men and in women, though the clinical manifestation and severity of the disease differ from person to person and individuals over the age of 80 years are at high risk of developing the severe of form of the disease.
Although what triggers the immune malfunction that leads to the development and pathogenesis of BP is not clearly understood. However, it is believed to arise from binding of the autoantibodies to hemidesmosomal component of BP180 and BP230 proteins, resulting in the activation of component complements at basement membrane zone (BMZ) or dermal-epidermal junction [46]. This binding results in the degranulation of mast cells and releasing of proinflammatory cytokines from keratinocytes together with immigrating eosinophils, macrophages and neutrophils into the skin. Additionally, the subsequent release of reactive oxygen species (ROS) and proteinases from the surrounding infiltrating inflammatory cells, enhances the separation of epidermis from dermis and the formation of blisters-filled fluid characterised by tense itchy-blisters and erosion, urticarial and pruritic plaques [47, 48] as seen in Fig. 3. Other factors such as drugs (some medications), bacterial or viral infections, physical and mechanical traumas, as well as other autoimmune/inflammatory diseases such as rheumatoid arthritis, thyroid disorders, malignancies and diabetes mellitus have been reported to associate with triggering BP in some patients [49].
The skin of Bullous Pemphigoid patient (showing large, tense bullae, and erythematous patches at dermal-epidermal junction filled with infiltrating inflammatory cells). Diagram taken from Fang et al. [46]
BP are predominantly malfunctions of autoantibodies or immune cells, dysregulation of inflammatory responses and stress, as such, any immunodulating and form of stress inducible molecules capable of eliciting these responses could play a role in the pathogenesis of BP. The roles of heat shock proteins in many chronic inflammation as well as in autoimmune diseases such rheumatoid arthritis, systematic lupus, psoriasis and BP, have been widely reported [28]. For instance, the high expression of Hsp90 in blistering lesions of BP patients has been documented, although its serum level expression did not correlate with autoantibodies against the BP180 NC16A enzyme complex [50]. It was hypothesised that anti-BP180 NC16A autoantibodies could induce intracellular expression of Hsp90 via the generation of ROS and cytokines proinflammatory mediators, which induces inflammatory response [49]. More so, studies have shown that the overexpression of Hsp90 in BP patients has been observed in both bullous skin lesion and serum treated with human keratinocytes (HaCaT), suggesting that Hsp90 could be an effective treatment target in an experimental epidermolysis bullosa acquisita-mouse model [51, 52]. Taken together, these findings are indications of the crucial role that heat shock proteins could play in the pathogenesis of BP, even though the exact mechanism of action is unclear at the moment and thus requires future studies.
1.5 Therapeutic Potential of Heat Shock Proteins in Human Inflammatory/Autoimmune Skin Diseases
Unresolved inflammation response and loss of tolerance to self-antigens caused by dysregulation and inappropriate stimulation of the immune system leading to an attack by its own cells are the hallmark of inflammatory and autoimmune diseases initiation. Although the actual causes of autoimmune dysregulation and its progression to chronic inflammation are still not fully understood. However, it has been reported that genetic mutation, lifestyle, environmental factors, persistence viral or bacterial infections, are the major contributing factors that cause these diseases [53]. In addition, these stress factors that mediate chronic inflammation or autoimmune diseases, also activate the synthesis of heat shock proteins. The roles of HSP in proinflammatory cytokines and signalling pathways that promote inflammatory or autoimmune diseases have been exploited and are still an ongoing area of research. In fact, overexpression of Hsp60 has been reported to induce the secretion of several cytokines (IL-6, IL-12 and IL-15), as well as increased expression of nitric oxide and TNF-α via CD14 and p38 MAPK signalling pathway in human monocytes [54]. Furthermore, an enhanced expression of Hsp60 in mammalian cell lines proved it could be a key for T cell and antibody responses in both chronic inflammatory diseases and atherosclerosis [55, 56]. In addition, considering that Hsp70 can mediate the induction of TNF-α, IL-1 and IL-6 via CD14-dependent pathway ultimately suggest a direct role of HSP in inflammatory propagation [57].
The concept of heat shock proteins in therapeutics initially arose from a study on cross-reactive immunity to human Hsp60, which revealed that T cells cross-reactivity with HSP60 could induce diabetes in mice. Subsequent study then found that the administration of Mycobacterium tuberculosis Hsp65 in mice could either induce or repress diabetes [58]. In addition, the findings that recombinant Hsp10 can inhibit the inflammatory changes induced by lipopolysaccharides (LPS) in mice and in macrophages prompted the attempt to commercialize Hsp10 as a therapeutic target and small-scale clinical trials for XToll, a modified form of Hsp10 [59, 60].
For instance, in patients with psoriasis plaque, short-term treatment with Hsp10 [recombinant chaperonin 10 (Cpn10)] led to a rapid reduction of the disease parameters. Probably, this was achieved through the modification of activity in chronic inflammatory and decrease in the release of inflammatory cytokines such as IL-1 and TNF-α, which play key roles in mediating inflammatory response and immune response in general [60, 61]. This finding suggests that Cpn10 may regulate a wide array of inflammatory responses in skin inflammatory diseases and may provide a range of therapeutic approaches in these diseases.
Furthermore, studies have shown overexpression of Hsp60 in peripheral blood mononuclear cell (PBMC) of children with AD skin lesion compare to that of non-lesional skin. The expression of Hsp60-reactive T cells in these children correlates with up-regulation of pro-inflammatory cytokine IFNγ and dowregulation of anti-inflammatory cytokine IL-10 [30]. This study together with the finding that demonstrates the expression of Hsp60 at site of inflammation and that Hsp60 can modulate the regulation of cytokines and Th1 phenotype in the skin lesion of dogs with atopic dermatitis [62], suggests the immunomodulating activities of Hsp60, as well as its contribution to the local inflammatory response in AD patients. Based on these findings, it is safe to speculate that Hsp60-reactive T cells plays a role in the pathogenesis of AD and future studies oriented towards investigating the immunomodulating properties and inflammatory response of Hsp60 in AD, could provide a novel therapeutic target in the management of the disease. Additionally, the expression of Hsp27 in the skin of AD and its correlation with environmental stress in human keratinocytes and in exercised skin, could be indicative of its cytoprotective role and biological defence responses to the disruption of skin barriers (filaggrin) in AD [31].
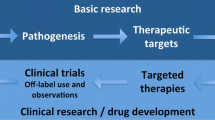
More so, the implication of Hsp90 in inflammation-associated immunological processes has been demonstrated by its essential role in various transcription factors and signalling molecules, which participate in cellular inflammation cascades such as induction of several pro-inflammatory cytokines, participation in auto-antigen presentation, as well as interaction with auto-antigenic proteins by acting as a potent promoter of the immune network outside of the cells [63]. The report that basement membrane-degrading matrix metalloproteinases (MMPs) released from surrounding cells also participates in blister formation and tissue injury in autoimmune bullous diseases rather than their initial role in tumour cellular invasion [64, 65], makes it an interesting aspect that inhibitors of Hsp90 could present therapeutic target in autoimmune diseases like BP. In fact, the growing pharmacological evidence of Hsp90 inhibitors in bullous autoimmune-inflammatory disorders has gained momentum as demonstrated by ameliorating effects of Hsp90 blockers in preclinical rodent experiments in other autoimmune inflammatory disorders such as systemic lupus erythematosus, encephalomyelitis and rheumatoid arthritis [66,67,68]. Although, it is largely unknown whether extracellular and intracellular dyregulation of Hsp90 in BP patients is primarily due to the pathogenesis or secondary changes induced by inflammation. However, for the fact that this chaperone is involved in many intracellular signalling which directly associated with production of inflammatory cytokines such as IL-6 and IL-8 (these cytokines play a major transcriptional factor role in the pathogenesis of BP) and this role in keratinocytes is believed to be of one the earliest stage of BP pathophysiology leading to the formation of blisters, thus suggests it may play a crucial role in the pathophysiology of BP [68,69,70]. Based on the aforementioned studies that highlight the important roles of HSP in modulating regulatory T cells (Tregs), which is critical in mediating inflammatory/autoimmune diseases, it can be hypothesized that studies targeting HSP or/and their inhibitors in inflammatory/autoimmune skin disorders could provide a good therapeutic approach in the treatment and management of these diseases as proposed in the model shown in Fig. 4.
Model proposing the disruption of skin epidermal layer, initiation, progression and pathogenesis of inflammatory/autoimmune diseases. (1) The stressors such UV irradiation, environmental factors, microbial invasion and other mechanical injuries that damages skin epidermal cells leading to cellular skin stress; (2) disruption of stratum corneum and environmental stressors such heat, UV radiation and microbial invasion induces expression of heat shock protein (Hsp90, Hsp70, Hsp60 and Hsp27); (3) these stressors causes skin injury/disruption of filaggrin protein; (4) microbial invasion and mechanical injuries to the skin provokes inflammatory response which aimed at clearing the invading pathogen and initiating cellular repair; (5) disruption of skin layers also induce the synthesis of cytoprotective heat shock proteins as well as inflammatory reaction which form part of immune response in general; (6) up-regulation of T cells (Tregs) which play critical roles in the initiation and progression of autoimmune diseases; (7) the interaction between immune response together with regulatory T cells can sometimes lead to “immune confusion” of immune system attacking its own cells which degenerates to autoimmune diseases; (8) pathogenesis of autoimmune diseases; (9) up-regulation and involvement of heat shock proteins in the pathogenesis and clinical manifestation of autoimmune disorders
2 Conclusions
Despite the progress made in determining the key players in pathophysiology of various inflammatory/autoimmune skin disorders, their therapeutic treatment remains a burden as most of these treatments are restricted to conventional immunosuppressive methods such as corticosteroid, atopic medications and more advanced biological methods that focus on supressing chronic inflammation. These therapies however, do not provide permanent solution to the interaction between pathogenic and protective immune responses and in most cases, patients are subjected to severe side effects. Therefore, there is a need for researchers to develop safe therapies with high efficacy to carefully balance this interaction in the complex environment. HSP are one of the key regulators of immune response to autoimmune inflammatory diseases and have been considered as potential therapeutic targets in the treatment of these diseases due to their ability to induce the production of immune regulatory T (Treg) cells, which plays critical role in the clinical manifestation of autoimmune-inflammatory disorders. Thus, targeting HSP or HSP inhibitors in these diseases could provide a novel therapeutic approach in the treatment of autoimmune-inflammatory skin disorders.
Abbreviations
- AD:
-
Atopic dermatitis
- BP:
-
Bullous Pemphigoid
- DCs:
-
dendritic cells
- HSP:
-
heat shock proteins
- IFN-γ:
-
interferon-γ
- IgE:
-
immunoglobulin E
- IL:
-
interleukins
- LPS:
-
lipopolysaccharides
- MMPs:
-
matrix metalloproteinases
- PBMC:
-
peripheral blood mononuclear cell
- ROS:
-
reactive oxygen species
- SALT:
-
skin-associated lymphoid tissue
- Th1:
-
T helper 1
- TLRs:
-
toll-like receptors
- TNF-α:
-
tumor necrosis factor-α
- Treg:
-
regulatory T cells
References
Oomens CW, van Vijven M, Peters GW (2017) Skin mechanics. In: Biomechanics of living organs. Academic, London, pp 347–357
Hendriks FM, Brokken D, Oomens CWJ, Bader DL, Baaijens FPT (2006) The relative contributions of different skin layers to the mechanical behavior of human skin in vivo using suction experiments. Med Eng Phys 28:259–266
Benítez JM, Montáns FJ (2017) The mechanical behavior of skin: structures and models for the finite element analysis. Comput Struct 190:75–107
Matejuk A (2018) Skin immunity. Arch Immunol Ther Exp 66:45–54
Quaresma JAS (2019) Organization of the skin immune system and compartmentalized immune responses in infectious diseases. Clin Microbiol Rev 32:00034–00018
Hotamisligil GS (2006) Inflammation and metabolic disorders. Nature 444(7121):860–867
Batulan Z, Pulakazhi Venu VK, Li Y, Koumbadinga G, Alvarez-Olmedo DG, Shi C, O’Brien ER (2016) Extracellular release and signaling by heat shock protein 27: role in modifying vascular inflammation. Front Immunol 7:285
Ikwegbue P (2019) Investigation of the interaction between heat shock protein 70.14 (Hsp 70.14) and RBBP6 RING finger domain. Master of Science Dissertation, University of Zululand, South Africa
Ritossa F (1962) A new puffing pattern induced by temperature shock and DNP in Drosophila. Experientia 18:571–573
Candido EPM (2001) Heat shock proteins A2-Brenner, Sydney. In: Miller JH (ed) Encyclopedia of genetic. Academic, New York, pp 914–915
Ikwegbue PC, Masamba P, Oyinloye BE, Kappo AP (2018) Roles of heat shock proteins in apoptosis, oxidative stress, human inflammatory diseases, and cancer. Pharmaceuticals 11:1–12
Alqarni AS, Ali H, Iqbal J, Owayss AA, Smith BH (2019) Expression of heat shock proteins in adult honey bee (Apis mellifera L.) workers under hot-arid subtropical ecosystems. Saudi J Biol Sci 26(7):1372–1376
Li Z, Srivastava P (2004) Heat-shock proteins. In: Coligan JE et al (eds) Current protocols in immunology, p Appendix 1: Appendix 1T. https://doi.org/10.1002/0471142735.ima01ts58
Zininga T, Ramatsui L, Shonhai A (2018) Heat shock proteins as immunomodulants. Molecules 23(11):E2846
Pockley AG (2002) Heat shock proteins, inflammation, and cardiovascular disease. Circulation 105(8):1012–1017
Edkins AL, Price JT, Pockley AG, Blatch GL (2017) Heat shock proteins as modulators and therapeutic targets of chronic disease: an integrated perspective. Philos Trans R Soc Lond Ser B Biol Sci 373(1738):20160521
Weidinger S, Klopp N, Rummler L, Wagenpfeil S, Novak N, Baurecht HJ, Groer W, Darsow U, Heinrich J, Gauger A, Schafer T (2005) Association of NOD1 polymorphisms with atopic eczema and related phenotypes. J Allergy Clin Immunol 116:177–184
Larsen FS, Hanifin J (2002) Epidemiology of atopic dermatitis. Immunol Allergy Clin N Am 22:1–24
Akdis CA, Akdis M, Bieber T, Bindslev-Jensen C, Boguniewicz M, Eigenmann P, Hamid Q, Kapp A, Leung DY, Lipozencic J, Luger TA (2006) Diagnosis and treatment of atopic dermatitis in children and adults: European Academy of Allergology and Clinical Immunology/American Academy of Allergy, Asthma and Immunology/PRACTALL Consensus Report. Allergy 61:969–987
Tsakok T, Marrs T, Mohsin M, Baron S, du Toit G, Till S, Flohr C (2016) Does atopic dermatitis cause food allergy? A systematic review. J Allergy Clin Immunol 137:1071–1078
Kapur S, Watson W, Carr S (2018) Atopic dermatitis. Allergy Asthma Clin Immunol 14:2–52
Avena-Woods C (2017) Overview of atopic dermatitis. Am J Manag Care 23(8 Suppl):S115–S123
Bandier J, Ross-Hansen K, Carlsen BC, Tanassi JT, Johansen JD, Heegaard NH (2016) Quantification of epidermal Filaggrin in human skin and its response to skin irritation. J Invest Dermatol 136:1296–1299
Berke R, Singh A, Guralnick M (2012) Atopic dermatitis: an overview. Am Fam Physician 86:35–42
Buske-Kirschbaum A, Geiben A, Hellhammer D (2001) Psychobiological aspects of atopic dermatitis: an overview. Psychother Psychosom 70:6–16
Hägermark Ö, Wahlgren CF (1995) Treatment of itch. Semin Dermatol 14(4):320–325
Yosipovitch G, Hundley JL (2004) Practical guidelines for relief of itch. Dermatol Nurs 16:325–332
Ghoreishi M, Yokozeki H, Hua WM, Nishioka K (2000) Expression of 27 KD, 65 KD and 72/73 KD heat shock protein in atopic dermatitis: comparison with those in normal skin and contact dermatitis. J Dermatol 27:370–379
Ergun T, İnce Ü, Ekşioğlu-Demiralp E, Direskeneli H, Gürbüz O, Gürses L, Aker F, Akoğlu T (2001) HSP 60 expression in mucocutaneous lesions of Behcet’s disease. J Am Acad Dermatol 45:904–909
Kapitein B, Aalberse JA, Klein MR, de Jager W, Hoekstra MO, Knol EF, Prakken BJ (2013) Recognition of self-heat shock protein 60 by T cells from patients with atopic dermatitis. Cell Stress Chaperones 18:87–95
Niiyama S, Yoshino T, Matsukuma S, Mukai H (2016) Heat shock protein 27 kDa content in stratum Corneum correlates with severity of atopic dermatitis. Acta Derm Venereol 96:976–977
Albanesi C, Madonna S, Gisondi P, Girolomoni G (2018) The interplay between keratinocytes and immune cells in the pathogenesis of psoriasis. Front Immunol 9:1549
Christophers E (2001) Psoriasis – epidemiology and clinical spectrum. Clin Exp Dermatol 26:314–320
Wu W, Debbaneh M, Moslehi H, Koo J, Liao W (2014) Tonsillectomy as a treatment for psoriasis: a review. J Dermatolog Treat 25:482–486
Buquicchio R, Foti C, Ventura MT (2018) The psoriasis pathogenesis and the metabolic risk. Open Dermatol J 12:70–79
Lowes MA, Suárez-Fariñas M, Krueger JG (2014) Immunology of psoriasis. Annu Rev Immunol 32:227–255
Seifarth FG, Lax JEM, Harvey J, DiCorleto PE, Husni ME, Chandrasekharan UM, Tytell M (2018) Topical heat shock protein 70 prevents imiquimod-induced psoriasis-like inflammation in mice. Cell Stress Chaperones 23(5):1129–1135
Griffiths CE, Barker JN (2007) Pathogenesis and clinical features of psoriasis. Lancet 370:63–271
Raho G, Koleva DM, Garattini L, Naldi L (2012) The burden of moderate to severe psoriasis. PharmacoEconomics 30:1005–1013
Heldwein KA, Fenton MJ (2002) The role of toll-like receptors in immunity against mycobacterial infection. Microbes Infect 4:937–944
Kaisho T, Akira S (2000) Critical roles of toll-like receptors in host defense. Crit Rev Immunol 20(5):393–405
Boehncke WH, Dahlke A, Zollner TM, Sterry W (1994) Differential expression of heat shock protein 70 (HSP70) and heat shock cognate protein 70 (HSC70) in human epidermis. Arch Dermatol Res 287:68–71
Kakeda M, Arock M, Schlapbach C, Yawalkar N (2014) Increased expression of heat shock protein 90 in keratinocytes and mast cells in patients with psoriasis. J Am Acad Dermatol 70:683–690
Wang WM, Jin HZ (2019) Heat shock proteins and psoriasis. Eur J Dermatol 29:121–125
Curry JL, Qin JZ, Bonish B, Carrick R, Bacon P, Panella J, Robinson J, Nickoloff BJ (2003) Innate immune-related receptors in normal and psoriatic skin. Arch Pathol Lab Med 127:178–186
Fang H, Zhang Y, Li N, Wang G, Liu Z (2018) The autoimmune skin disease bullous pemphigoid: the role of mast cells in autoantibody-induced tissue injury. Front Immunol 9:407
Schulze F, Kasperkiewicz M, Zillikens D, Schmidt E (2013) Bullöses Pemphigoid. Hautarzt 64:931–945
Okon L, Werth V (2014) Bullous Pemphigoid, mucous membrane Pemphigoid and pemphigus vulgaris: an update on pathobiology. Curr Oral Health Rep 1:180–189
Raveendran MN, Srinivasan SM (2017) Postpartum bullous pemphigoid-A case report. Our Dermatol Online/Nasza Dermatologia Online 8:2
Tukaj S, Kleszczyński K, Vafia K, Groth S, Meyersburg D, Trzonkowski P, Ludwig RJ, Zillikens D, Schmidt E, Fischer TW, Kasperkiewicz M (2013) Aberrant expression and secretion of heat shock protein 90 in patients with bullous pemphigoid. PLoS One 8:7–0496
Kasperkiewicz M, Tukaj S, Gembicki AJ, Silló P, Görög A, Zillikens D, Kárpáti S (2014) Evidence for a role of autoantibodies to heat shock protein 60, 70, and 90 in patients with dermatitis herpetiformis. Cell Stress Chaperones 19:837–843
Kasperkiewicz M, Müller R, Manz R, Magens M, Hammers CM, Somlai C, Westermann J, Schmidt E, Zillikens D, Ludwig RJ, Orosz A (2011) Heat-shock protein 90 inhibition in autoimmunity to type VII collagen: evidence that nonmalignant plasma cells are not therapeutic targets. Blood 117:6135–6142
Ikwegbue PC, Masamba P, Mbatha LS, Oyinloye BE, Kappo AP (2019) Interplay between heat shock proteins, inflammation and cancer: a potential cancer therapeutic target. Am J Cancer Res 9:2–242
Dubey A, Prajapati KS, Swamy M, Pachauri V (2015) Heat shock proteins: a therapeutic target worth to consider. Vet World 8(1):46–51
Grundtman C, Kreutmayer SB, Almanzar G, Wick MC, Wick G (2011) Heat shock protein 60 and immune inflammatory responses in atherosclerosis. Arterioscler Thromb Vasc Biol 31:960–968
Tukaj S, Kaminski M (2019) Heat shock proteins in the therapy of autoimmune diseases: too simple to be true? Cell Stress Chaperones 24:475–479
Lovett MC, Coates JR, Shu Y, Oglesbee MJ, Fenner W, Moore SA (2014) Quantitative assessment of hsp70, IL-1β and TNF-α in the spinal cord of dogs with E40K SOD1-associated degenerative myelopathy. Vet J 200:312–317
Elias D, Markovits D, Reshef T, van der Zee R, Cohen IR (1990) Induction and therapy of autoimmune diabetes in the non-obese diabetic (NOD/Lt) mouse by a 65-kDa heat shock protein. Proc Natl Acad Sci 87:1576–1580
Johnson BJ, Le TT, Dobbin CA, Banovic T, Howard CB, Flores FDML, Vanags D, Naylor DJ, Hill GR, Suhrbier A (2005) Heat shock protein 10 inhibits lipopolysaccharide-induced inflammatory mediator production. J Biol Chem 280:4037–4047
Pockley AG, Henderson B (2017) Extracellular cell stress (heat shock) proteins—immune responses and disease: an overview. Philos Trans R Soc B Biol Sci 373:20160–20522
Williams B, Vanags D, Hall S, McCormack C, Foley P, Weiss J, Johnson B, Latz E, Feeney D (2008) Efficacy and safety of chaperonin 10 in patients with moderate to severe plaque psoriasis: evidence of utility beyond a single indication. Arch Dermatol 144:683–685
Jassies-van der Lee A, Rutten V, Van Kooten P, Van der Zee R, Willemse T (2008) Intradermal injection of Hsp60 induces cytokine responses in canine atopic and healthy skin. Cell Stress Chaperones 13:387–391
Srivastava P (2002) Roles of heat-shock proteins in innate and adaptive immunity. Nat Rev Immunol 2(3):185–194
Schulz R, Dobbelstein M, Moll UM (2012) HSP90 inhibitor antagonizing MIF: the specifics of pleiotropic cancer drug candidates. Onco Targets Ther 1:1425–1426
Kasperkiewicz M, Zillikens D, Schmidt E (2012) Pemphigoid diseases: pathogenesis, diagnosis, and treatment. Autoimmunity 45:55–70
Rice JW, Veal JM, Fadden RP, Barabasz AF, Partridge JM, Barta TE, Dubois LG, Huang KH, Mabbett SR, Silinski MA, Steed PM (2008) Small molecule inhibitors of Hsp90 potently affect inflammatory disease pathways and exhibit activity in models of rheumatoid arthritis. Arthritis Rheum 58:3765–3775
Yun TJ, Harning EK, Giza K, Rabah D, Li P, Arndt JW, Luchetti D, Biamonte MA, Shi J, Lundgren K, Manning A (2011) EC144, a synthetic inhibitor of heat shock protein 90, blocks innate and adaptive immune responses in models of inflammation and autoimmunity. J Immunol 186:563–575
Tukaj S, Zillikens D, Kasperkiewicz M (2015) Heat shock protein 90: a pathophysiological factor and novel treatment target in autoimmune bullous skin diseases. Exp Dermatol 24:567–571
Van den Bergh F, Eliason SL, Burmeister BT, Giudice GJ (2012) Collagen XVII (BP 180) modulates keratinocyte expression of the proinflammatory chemokine, IL-8. Exp Dermatol 21:605–611
Tukaj S, Węgrzyn G (2016) Anti-Hsp90 therapy in autoimmune and inflammatory diseases: a review of preclinical studies. Cell Stress Chaperones 21:213–218
Acknowledgements
Authors will like to acknowledge Dr. Sesan John Owonubi for proofreading this manuscript. None of the authors received any kind of funding towards the work presented in this article.
Disclosure of Interests
All authors declare they have no conflict of interest.
Ethical Approval for Studies Involving Human
This article does not contain any studies with human participants performed by any of the authors.
Ethical Approval for Studies Involving Animals
This article does not contain any studies with animals performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Ikwegbue, P.C., Revaprasadu, N., Kappo, A.P. (2020). Therapeutic Potential of Heat Shock Proteins in Human Inflammation/Autoimmune Skin Diseases: Future Directions. In: Asea, A.A.A., Kaur, P. (eds) Heat Shock Proteins in Inflammatory Diseases. Heat Shock Proteins, vol 22. Springer, Cham. https://doi.org/10.1007/7515_2020_36
Download citation
DOI: https://doi.org/10.1007/7515_2020_36
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-85167-5
Online ISBN: 978-3-030-85168-2
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)