Abstract
Adherence to therapy plays a key role in treatment optimization and clinical outcome in patients with chronic obstructive pulmonary disease (COPD). The adherence to inhaled medications is poor, ranging from 20% to 60%. In this study we searched Medline and PubMed literature regarding factors that could have an impact on therapy adherence in COPD patients, using the key words “COPD” or “chronic obstructive pulmonary disease” and “adherence”. The search was limited to the English language article published between January 2013 and December 2019. Review papers, study protocols, and meta-analyses were excluded. The final material included 25 articles. The evaluation was performed using the Cochrane Review Manager guidelines. The 25 articles represented 29 countries from 5 continents. We assessed adherence to therapy and the impact of selected factors on the adherence in 27,660 COPD patients (60.9% of whom were male, mean age 64 years). The factors affecting adherence were broken down into three categories: sociodemographic, clinical, and psychological. There were two standardized instruments used in the analyzed studies: Test of Adherence to Inhalers (TAI) and self-reported Morisky Medication Adherence Scale (MMAS-8). We found that 46.3% of patients had a moderately good level of adherence to inhaled therapy (TAI range around 50 points), while 41.6% of patients had a high level of adherence to oral therapy. The nature of non-adherence was in most cases inadvertent rather than an erratic or deliberate demeanor (48.5% vs. 38.9% vs. 42.4%, respectively). We conclude that standardized instruments enable the prediction of adherence to therapy and should be used in clinical practice. The assessment of adherence is essential for undertaking interventions to counteract plausible non-adherence. Collaboration between an educator and a psychologist is required to evaluate the patient’s motivation and to ensure his comprehension of treatment prescribed.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
Adherence to treatment plays a key role in the course of chronic obstructive pulmonary disease (COPD). Non-adherence is rather common, as adherence ranges between 20% and 60% of COPD patients. Non-adherence results in symptom exacerbation, frequent hospitalizations, and poor quality of life. COPD was the fourth most common cause of death in 2000. It is estimated that 4.7 million people will die from COPD by 2020, making the disease the third most common cause of death worldwide. Human and economic losses due to non-adherence in COPD have been estimated at $300 billion per year (DiMatteo 2004).
The WHO has identified non-adherence to treatment as one of the most serious health problems. Non-adherence is a fundamental barrier to achieving the expected outcomes of evidence-based treatment. The consequences for non-adherent patients range from health deterioration to death. At the same time, non-adherence has serious health-related and economic ramifications for the entire society. To date, hundreds of factors that affect treatment adherence have been described. Their classification by the WHO comprises five broad categories: (1) socioeconomic factors, (2) healthcare system-related factors, (3) illness-related factors, (4) treatment-related factors, and (5) patient-dependent factors (WHO 2003).
Factors associated with satisfaction and technique of inhaled therapy have been identified as the most significant for COPD treatment adherence, while sociodemographic factors are considered the least significant. The main problem associated with inhaled therapy is a lack of the patients’ savvy to use this treatment option. Other substantial predictors of adherence include psychological factors. Beliefs about medication and treatment satisfaction are the most common causes of treatment discontinuation. Chronically treated patients collect experiences and develop their own beliefs regarding the use of specific medications, sometimes also considering the experience of their friends or family members. Another major determinant of adherence is concern about the use of complex inhalers or other devices. In the literature, differences in adherence have been reported between inhaled and oral treatments. Thus, factors that would influence adherence should be considered when selecting specific treatment.
The available reports present contradictory findings regarding the impact of sociodemographic and clinical factors on adherence in COPD patients. In general, there are few studies that include the assessment of the impact of psychosocial factors on adherence to treatment in chronically ill patients. There is also an apparent shortage of the literature describing non-adherence risk factors in COPD patients. Therefore, this study was undertaken to present and evaluate the available literature findings on the influence of sociodemographic, clinical, and psychosocial factors on adherence to therapy in COPD patients.
2 Methods
2.1 Search Strategy
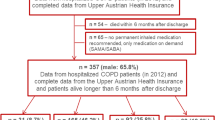
In this study, we searched Medline and PubMed databases for the articles addressing factors that could have an impact on therapy adherence in COPD patients, using the key words “COPD” or “chronic obstructive pulmonary disease” and “adherence” or “MMAS” or “TAI”. The search was limited to the English language article published between January 2013 and December 2019. Review papers, study protocols, and meta-analyses were excluded. The final material included 25 articles comprising a total of 27,660 COPD patients. Of this cohort, 16,844 (60.9%) were men of the mean age of 64 years. The evaluation was performed using the Cochrane Review Manager guidelines. Subsequent analyses were performed using the Cochrane Review Manager guidelines (Lutje 2019). The search scheme is presented in detail in Fig. 1.
2.2 Statistical Elaboration
Statistical analysis was performed using a fixed effect or random effect model, depending on the heterogeneity of results. For the latter model, the DerSimonian–Laird estimator was used. A p-value <0.05 defined statistically significant associations. The analysis was performed using R software v3.6.1 (R Core Team 2019).
3 Results
There were two main standardized instruments used in the analyzed studies: Test of Adherence to Inhalers (TAI) and self-reported Morisky Medication Adherence Scale (MMAS-8). TAI consists of 10 (short version) or 12 (full version) items. In the 10-item version of the test, each item was scored between 1 (worst) and 5 (best) possible score, yielding a total ranging from 10 to 50 points. The 12-item TAI includes additional two items addressing the healthcare professional, which are scored 1 (bad) and 2 (good), adding the maximum of 4 points. These two items were designed to unravel the inadvertent non-adherent pattern. This pattern was identified when the score for item 11 or 12 was 1. The erratic or deliberate non-adherent behavior pattern was identified when the score for items either 1–5 or 6–10 was ≤24, respectively (Plaza et al. 2016a).
The Morisky Medication Adherence Scale (MMAS-8) is a self-reported questionnaire to assess adherence to medication. The scale comprises eight items that assess behaviors and barriers related to the long-term adherence to medication. MMAS-8 score may range between 0 and 8, with the scores <6, 6–7, and 8 corresponding to low, medium, and high adherence, respectively (Morisky et al. 2008).
3.1 Test of Adherence to Inhalers (TAI): Five Studies Included in the Analysis
3.1.1 TAI: % of Good Scores of Adherence to Therapy
The analysis shows that 46.3% of patients in the analyzed studies obtained good scores of adherence to therapy (95%CI; 39.9–52.8). The test for heterogeneity demonstrated a considerable heterogeneity of data, with the heterogeneity coefficient of I2 = 84.8% (p < 0.001). The random effects model was applied in the data elaboration (Fig. 2).
3.1.2 TAI: % of Inadvertent Non-adherence to Therapy
The analysis shows that 48.5% of patients in the analyzed studies showed inadvertent non-adherence to therapy (95%CI: 21.3–75.7). The test for heterogeneity demonstrated considerable heterogeneity of data, with the heterogeneity coefficient of I2 = 99.4% (p < 0.001). The random effects model was applied in the data elaboration (Fig. 3).
3.1.3 TAI: % of Erratic Non-adherence to Therapy
The analysis shows that 38.9% of patients in the analyzed studies showed erratic non-adherence to therapy (95%CI: 18.3–59.4). The test for heterogeneity demonstrated considerable heterogeneity of data, with the heterogeneity coefficient of I2 = 98.9% (p < 0.001). The random effects model was applied in the data elaboration (Fig. 4).
3.1.4 TAI: % of Deliberate Non-adherence to Therapy
The analysis shows that 42.5% of patients in the analyzed studies showed erratic non-adherence to therapy (95%CI: 12.0–72.9). The test for heterogeneity demonstrated considerable heterogeneity of data, with the heterogeneity coefficient of I2 = 99.6% (p < 0.001). The random effects model was applied in the data elaboration (Fig. 5).
3.2 Morisky Medication Adherence Scale (MMAS-8): Six Studies Included in the Analysis
3.2.1 MMAS-8: % of High Scores of Adherence to Therapy
The analysis shows that 41.6% of patients in the analyzed studies obtained high adherence scores (95%CI: 26.7–56.4). The test for heterogeneity demonstrated considerable heterogeneity of data, with the heterogeneity coefficient of I2 = 99.3% (p < 0.001). The random effects model was applied in the data elaboration (Fig. 6).
3.3 Factors Affecting Adherence to Therapy in COPD Patients
Table 1 shows sociodemographic, clinical, and psychological factors contributing to non-adherence to therapy in COPD patients. The most commonly reported factors having a negative connotation were those of sociodemographic (low income), clinical (disease duration, severity, and medication), and psychological nature (coping with disease stress, depression, or negative beliefs concerning curability).
Among the factors contributing to better adherence to COPD therapy, age ≥ 60 years and male gender are the most commonly reported sociodemographic factors (Table 2). On the clinical side, frequency of hospitalization and the knowledge about the number and type of medications and the use of inhalers also had a positive influence on adherence to therapy. Satisfaction with inhalation treatment was commonly reported as a strong predictor of better adherence as well.
4 Discussion
This article is a review of recent studies on factors affecting adherence to COPD treatment. Most of the analyzed studies used self-reported measures. The findings demonstrate that COPD patients have lower adherence to therapy than those with other chronic diseases, such as cardiovascular disorders, hypercholesterolemia, osteoporosis, or diabetes. In COPD, adherence rates ranged between 20% and 60%. George et al. (2005), using a patient-reported medication adherence scale, have found a good adherence in 37% of patients. Ágh et al. (2011) have reported that 58.2% of patients had optimum adherence, based on MMAS-8 scores. Plaza et al. (2016b) have found that adherence to inhaled therapy was present in 49% of COPD patients. Referring to the causes of non-adherence, authors report a variety of factors, and the issue is yet debatable in the literature. In the present review, we broke down the factors associated with adherence to COPD therapy into the sociodemographical, clinical, and psychological category, akin to the classification used by WHO (2003).
In screening tests performed in daily clinical practice, the level of adherence in patients treated for asthma and COPD rarely exceeds 50%. In a study by Wiśniewski et al. (2014), only 67% of patients adhered to treatment 30 days after discharge from the hospital. COPD treatment is primarily based on inhalation therapy, although most patients prefer oral medications. In the studies included in this review, the rate of satisfactory adherence ranged between 46.3% for inhalation and 41.6% for oral therapy. This may be exemplified by the findings of Montes de Oca et al. (2017) who reported the scores for 10-item TAI and MMAS-8 questionnaires of 47.4 ± 4.9 vs. 6.8 ± 1.6, i.e., high vs. medium adherence, respectively. In that study, however, the incorrect use of inhalers could influence the adherence level. Patients who adhere better to inhalation than oral therapy usually have a better savvy in using inhalers, and use a variety of inhaler devices and inhaled drugs. Among factors contributing to better adherence, the ones associated with taking medication using an inhaler have been assessed most frequently. In a GAPP study, 23% of patients reported that no time was devoted to discuss with them the use of proper treatment techniques for successful asthma management (Canonica et al. 2007). The literature demonstrates that as many as 90% of patients may inhale medication incorrectly, although the estimate varies depending on the selection of a study sample and on the type of inhaler used. Multiple studies clearly demonstrate the efficacy of education performed by a pharmacist, nurse, or physician in increasing the adherence rate (Broadbent et al. 2018; Dudvarski Ilic et al. 2016; Moy et al. 2016; Poureslami et al. 2016; Tommelein et al. 2014). Broadbent et al. (2018) have shown that patients who receive training from a pharmacist perform a greater number of puffs per day compared to the non-trained subjects; mean 48.5% vs. 29.5%, respectively; p = 0.03.
Referring to non-adherence, the present review shows that a substantial number of patients (42.5%) purposely chose not to take their medication, which was deliberate non-adherence. On the other side, 48.5% of patients failed to follow the instructions received from medical personnel, which demonstrated inadvertent non-adherence, and 38.9% of patients failed to adhere to treatment due to their lifestyle, which was erratic non-adherence. We also found that psychological factors, such as a belief in the effectiveness of treatment, satisfaction with one’s physician, and the ease and training in the inhaler use, count significant for having good adherence. In a study by Olszanecka-Glinianowicz and Almgren-Rachtan (2014), non-adherence is inversely proportional to the sense of control over one’s disease and the opinion on the effectiveness of treatment. In another study, a strong correlation has been reported between adherence to pharmaceutical treatment and patient’s perceived health (Wiśniewski et al. 2014). According to Sanduzzi et al. (2014), adverse consequences of non-adherence include a gradual deterioration of quality of life, a sense of the disease being out of control, a greater number of exacerbations, and a higher mortality. Observations from a 3-year-long TORCH study demonstrate a greater than twofold increase in the risk of death and a nearly twofold increase in the risk of rehospitalization in non-adherent patients (Vestibo et al. 2009). These findings were confirmed in the present review, where the number of hospitalizations was a predictor of lower adherence.
The studies reviewed in this article differed in terms of COPD severity. The effect of disease severity on adherence to therapy is a contentious issue. Most studies show a better adherence with increasing severity of disease. Some other studies, however, show the opposite trend, a better adherence when the disease runs a mild course (Liao and Chen 2019; Leiva-Fernández et al. 2014). The discrepancy might be explained by the strength of motivation to continue treatment, associated with persistent symptoms that interfere with the patient’s daily functioning. Another consideration concerns the adverse effects of medications, which may affect the patient’s willingness to take them. In the GAPP study, patients who categorized their asthma as severe, and those who were treated by specialists, were most likely to discuss the knowledgeable aspects of their condition (Canonica et al. 2007).
The influence of sociodemographical factors on adherence to therapy in COPD patients is yet another debatable issue. In this review, we show that better adherence associates with older age, male gender, and daily functioning. The reason could be that pensioners have more time for regular living, exercising, and following dietary guidelines. On the other side, older patients may have a difficulty to adhere to treatment due to the presence of comorbidities. In contrast, younger patients are more likely to oppose medical advice and tend not to accept their illness, which may lead to non-adherence (Świątoniowska et al. 2018). In the studies reviewed herein male gender predominated among patients. That is in line with a study by Liao and Chen (2019) who have shown that adherence is outstandingly greater in men than women (87.3% vs. 12.7%, respectively). Other studies also show that men are more likely to adhere to therapy than women (Vestibo et al. 2009). The issue is somehow contentious as in a study by Dhamane et al. (2017), 59% of COPD patients are women, but the authors do not show any influence of gender on adherence. Other authors point out that low income and a lack of professional activity undermine adherence to COPD treatment (Liao and Chen 2019; Plaza et al. 2016b), although the underlying reasons for that are not full well clear. In patients experiencing economic difficulties, adherence to disease monitoring may be improved by addressing modifiable barriers such as cost and access (Campbell et al. 2014). There are, however, studies that put into question the association between sociodemographical factors and adherence to therapy (Khadour et al. 2012; Bourbeau and Bartlett (2008).
In conclusion, standardized questionnaire tools enable the prediction of adherence to therapy in COPD patients and should be used in clinical practice. The assessment of adherence is essential for undertaking interventions to counteract plausible non-adherence. Collaboration between an educator and a psychologist is needed to evaluate the patient’s motivation and to ensure he comprehends the treatment prescribed.
References
Ágh T, Inotai A, Mészáros Á (2011) Factors associated with medication adherence in patients with chronic obstructive pulmonary disease. Respiration 82(4):328–334
Barja-Martínez E, Casas-González S, Simón-López AF, Mancheño-Ovejero C, Padial-de la Cruz MLG (2019) Adherence to inhaled therapy in the outpatient setting. Enferm Clin 29(1):34–38. (Article in Spanish)
Bourbeau J, Bartlett SJ (2008) Patient adherence in COPD. Thorax 63(9):831–838
Broadbent E, Garrett J, Jepsen N, Li Ogilvie V, Ahn HS, Robinson H, Peri K, Kerse N, Rouse P, Pillai A, MacDonald B (2018) Using robots at home to support patients with chronic obstructive pulmonary disease: pilot randomized controlled trial. J Med Internet Res 20(2):e45
Campbell DJ, Ronksley PE, Manns BJ, Tonelli M, Sanmartin C, Weaver RG, Hennessy D, King-Shier K, Campbell T, Hemmelgarn BR, Interdisciplinary Chronic Disease Collaboration (2014) The association of income with health behavior change and disease monitoring among patients with chronic disease. PLoS One 9(4):e94007
Canonica GW, Baena-Cagnani CE, Blaiss MS, Dahl R, Kaliner MA, Valovirta EJ, GAPP Survey Working Group (2007) Unmet needs in asthma: Global Asthma Physician and Patient (GAPP) Survey: global adult findings. Allergy 62(6):668–674
Chrystyn H, Small M, Milligan G, Higgins V, Gil EG, Estruch J (2014) Impact of patients’ satisfaction with their inhalers on treatment compliance and health status in COPD. Respir Med 108(2):358–365
Dhamane AD, Schwab P, Hopson S, Moretz C, Annavarapu S, Burslem K, Renda A, Kaila S (2017) Association between adherence to medications for COPD and medications for other chronic conditions in COPD patients. Int J Chron Obstruct Pulmon Dis 12:115–122
DiMatteo MR (2004) Variations in patients’ adherence to medical recommendations: a quantitative review of 50 years of research. Med Care 42(3):200–209
Dudvarski Ilic A, Zugic V, Zvezdin B, Kopitovic I, Cekerevac I, Cupurdija V, Perhoc N, Veljkovic V, Barac A (2016) Influence of inhaler technique on asthma and COPD control: a multicenter experience. Int J Chron Obstruct Pulmon Dis 11:2509–2517
George J, Kong DC, Thoman R, Stewart K (2005) Factors associated with medication nonadherence in patients with COPD. Chest 128(5):3198–3204
Ivanov Y, Nikolaev I, Nemeth I (2018) Real-life evaluation of COPD treatment in a Bulgarian population: a 1-year prospective, observational, noninterventional study. Int J Chron Obstruct Pulmon Dis 13:653–663
Jouleh B, Erdal M, Eagan TM, Bakke P, Gulsvik A, Nielsen R (2018) Guideline adherence in hospital recruited and population-based COPD patients. BMC Pulm Med 18(1):195
Khadour MR, Hawwa AF, Kidney JC, Smyth BM, McElnay JC (2012) Potential risk factors for medication non-adherence in patients with chronic obstructive pulmonary disease (COPD). Eur J Clin Pharmacol 68(10):1365–1373
Kokturk N, Polatli M, Oguzulgen IK, Saleemi S, Al Ghobain M, Khan J, Doble A, Tariq L, Aziz F, El Hasnaoui A (2018) Adherence to COPD treatment in Turkey and Saudi Arabia: results of the ADCARE study. Int J Chron Obstruct Pulmon Dis 13:1377–1388
Leiva-Fernández J, Leiva-Fernández F, García-Ruiz A, Prados-Torres D, Barnestein-Fonseca P (2014) Efficacy of a multifactorial intervention on therapeutic adherence in patients with chronic obstructive pulmonary disease (COPD): a randomized controlled trial. BMC Pulm Med 14:70
Liao KM, Chen CY (2019) The association between adherence and dementia in chronic obstructive pulmonary disease. Medicine (Baltimore) 98(20):e15646
Lutje V (2019) Guide to the search strategy. https://cidg.cochrane.org. Accessed on 02 Jan 2019
Mısırlıgil Z, Çımrın A, Günen H, Özlü T, Çilli A, Akyıldız L, Bayram H, Gemicioğlu B, Uzaslan E, Abadoğlu Ö, Suerdem M (2017) Real life profile of asthma and chronic obstructive pulmonary disease patients in Turkey. Tuberk Toraks 65(3):169–179
Montes de Oca M, Menezes A, Wehrmeister FC, Lopez Varela MV, Casas A, Ugalde L, Ramirez-Venegas A, Mendoza L, López A, Surmont F, Miravitlles M (2017) Adherence to inhaled therapies of COPD patients from seven Latin American countries: the LASSYC study. PLoS One 12(11):e0186777
Morisky DE, Ang A, Krousel-Wood M, Ward HJ (2008) Predictive validity of a medication adherence measure in an outpatient setting. J Clin Hypertens (Greenwich) 10(5):348–354
Moy ML, Martinez CH, Kadri R, Roman P, Holleman RG, Kim HM, Nguyen HQ, Cohen MD, Goodrich DE, Giardino ND, Richardson CR (2016) Long-term effects of an internet-mediated pedometer-based walking program for chronic obstructive pulmonary disease: randomized controlled trial. J Med Internet Res 18(8):e215
Müllerová H, Landis SH, Aisanov Z, Davis KJ, Ichinose M, Mannino DM, Maskell J, Menezes AM, van der Molen T, Oh YM, Tabberer M, Han MK (2016) Health behaviors and their correlates among participants in the continuing to confront COPD International Patient Survey. Int J Chron Obstruct Pulmon Dis 11:881–890. Erratum in: Int J Chron Obstruct Pulmon Dis 12:859
Ngo CQ, Phan DM, Vu GV, Dao PN, Phan PT, Chu HT, Nguyen LH, Vu GT, Ha GH, Tran TH, Tran BX, Latkin CA, Ho CSH, Ho RCM (2019) Inhaler technique and adherence to inhaled medications among patients with acute exacerbation of chronic obstructive pulmonary disease in Vietnam. Int J Environ Res Public Health 16(2):pii: E185
Nguyen TS, Nguyen TLH, Pham TTV, Hua S, Ngo QC, Li SC (2019) Impact of pharmaceutical care in the improvement of medication adherence and quality of life for COPD patients in Vietnam. Respir Med 153:31–37
Olszanecka-Glinianowicz M, Almgren-Rachtan A (2014) The adherence and illness perception of patients diagnosed with asthma or chronic obstructive pulmonary disease treated with polytherapy using new generation cyclohaler. Postepy Dermatol Alergol 31(4):235–246
Pinnock H, Hanley J, McCloughan L, Todd A, Krishan A, Lewis S, Stoddart A, van der Pol M, MacNee W, Sheikh A, Pagliari C, McKinstry B (2013) Effectiveness of telemonitoring integrated into existing clinical services on hospital admission for exacerbation of chronic obstructive pulmonary disease: researcher blind, multicentre, randomised controlled trial. BMJ 347:f6070
Plaza V, Fernández-Rodríguez C, Melero C, Cosío BG, Entrenas LM, de Llano LP, Gutiérrez-Pereyra F, Tarragona E, Palomino R, López-Viña A, TAI Study Group (2016a) Validation of the ‘Test of the Adherence to Inhalers’ (TAI) for asthma and COPD patients. J Aerosol Med Pulm Drug Deliv 29(2):142–152
Plaza V, López-Viña A, Entrenas LM, Fernández-Rodríguez C, Melero C, Pérez-Llano L, Gutiérrez-Pereyra F, Tarragona E, Palomino R, Cosio BG (2016b) Differences in adherence and non-adherence behaviour patterns to inhaler devices between COPD and asthma patients. COPD 13(5):547–554
Poureslami I, Kwan S, Lam S, Khan NA, FitzGerald JM (2016) Assessing the effect of culturally specific audiovisual educational interventions on attaining self-management skills for chronic obstructive pulmonary disease in Mandarin- and Cantonese-speaking patients: a randomized controlled trial. Int J Chron Obstruct Pulmon Dis 11:1811–1822
R Core Team (2019) R: a language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. https://www.R-project.org/. Accessed on 22 Jan 2019
Sanduzzi A, Balbo P, Candoli P, Catapano GA, Contini P, Mattei A, Puglisi G, Santoiemma L, Stanziola AA (2014) COPD: adherence to therapy. Multidiscip Respir Med 9:60
Świątoniowska N, Dudek K, Szymczyk A, Jankowska-Polańska B (2018) Factors associated with adherence in patients with type 2 diabetes mellitus. J Educ Health Sport 8(12):192–209
Tommelein E, Mehuys E, Van Hees T, Adriaens E, Van Bortel L, Christiaens T, Van Tongelen I, Remon JP, Boussery K, Brusselle G (2014) Effectiveness of pharmaceutical care for patients with chronic obstructive pulmonary disease (PHARMACOP): a randomized controlled trial. Br J Clin Pharmacol 77(5):756–766
Toyama T, Kawayama T, Kinoshita T, Imamura Y, Yoshida M, Takahashi K, Fujii K, Higashimoto I, Hoshino T (2019) Differences In adherence barriers to inhaled medicines between Japanese patients with chronic obstructive pulmonary disease and asthma evaluated using the ‘Adherence Starts with Knowledge 20’ (ASK-20) questionnaire. Intern Med 58(2):175–185
Tran M, Xiang P, Rascati KL, Stock EM, Godley PJ, Coleman A, Bogart MR, Stanford RH (2016) Predictors of appropriate pharmacotherapy management of COPD exacerbations and impact on 6-month readmission. J Manag Care Spec Pharm 22(10):1186–1193
van der Palen J, Cerveri I, Roche N, Singh D, Plaza V, Gonzalez C, Patino O, Scheepstra I, Safioti G, Backer V (2019) DuoResp® Spiromax® adherence, satisfaction and ease of use: findings from a multi-country observational study in patients with asthma and COPD in Europe (SPRINT). J Asthma 11:1–9
Vestibo J, Anderson JA, Calverley P, Celli B, Ferguson GT, Jenkins C, Knobil K, Willits LR, Yates JC, Jones PW (2009) Adherence to inhaled therapy, mortality and hospital admission in COPD. Thorax 64(11):939–943
WHO (2003) Adherence to long-term therapies – evidence for action. Essential medicines and health products information portal. A World Health Organization resource. https://apps.who.int/medicinedocs/en/d/Js4883e/8.5.4.html. Accessed on 22 Oct 2019
Wiśniewski D, Porzezińska M, Gruchała-Niedoszytko M, Niedoszytko M, Slominski JM, Jassem E (2014) Factors influencing adherence to treatment in COPD patients and its relationship with disease exacerbations. Pneumonol Alergol Pol 82(2):96–104
Conflicts of Interest
The authors declare no conflicts of interest in relation to this article.
Ethical Approval
This is a literature review article that does not contain any current studies or experiments with human participants or animals performed by any of the authors. The writing of this article was accepted by the scientific Review Board of Wroclaw Medical University in Poland.
Informed Consent
There are no individual participants included in this review article. Therefore, there was no requirement to obtain individual informed consent.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Świątoniowska, N., Chabowski, M., Polański, J., Mazur, G., Jankowska-Polańska, B. (2020). Adherence to Therapy in Chronic Obstructive Pulmonary Disease: A Systematic Review. In: Pokorski, M. (eds) Medical Research and Development. Advances in Experimental Medicine and Biology(), vol 1271. Springer, Cham. https://doi.org/10.1007/5584_2019_477
Download citation
DOI: https://doi.org/10.1007/5584_2019_477
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-50497-7
Online ISBN: 978-3-030-50498-4
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)