Abstract
Sleep disorders are common in patients with chronic obstructive pulmonary disease (COPD) and are associated with greater disease severity, more frequent exacerbations, greater use of emergency health care, and higher mortality. They may contribute to worsening of COPD course by reducing patients’ adherence to treatment. The aim of this study was to evaluate quality of sleep in COPD patients and to assess the relationship between impaired sleep and adherence to inhalation therapy. The study included 106 COPD patients who were asked to answer the Pittsburgh Sleep Quality Index (PSQI), Epworth Sleepiness Scale (ESS), and Adherence to Refills and Medications Scale (ARMS). Clinical and demographic data were also collected. We found that over 60% of patients presented with sleep disorders (PSQI ≥5) and 75% with daytime sleepiness. None of the patients presented with optimal adherence to pharmacotherapy. Worse adherence was correlated with greater sleep disorders (r = 0.56; p < 0.001). ARMS questionnaire proved to be of high overall internal consistency (Cronbach’s alpha = 0.85). In conclusion, poor quality of sleep coexists with poor adherence to treatment among COPD patients. ARMS was proved to be a reliable tool for the assessment of adherence. Interventions aimed at improving sleep quality may be helpful to improve adherence to inhalation therapy in COPD patients.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Adherence to therapy
- Chronic obstructive pulmonary disease
- Daytime sleepiness
- Inhalation therapy
- Sleep disorders
1 Introduction
The Global Initiative for Chronic Obstructive Lung Disease (Mirza et al. 2018) defines chronic obstructive pulmonary disease (COPD) as “a common, preventable and treatable disease that is characterized by persistent respiratory symptoms and airflow limitation that is due to airway and/or alveolar abnormalities usually caused by significant exposure to noxious particles or gases”. COPD progresses with exacerbations and is associated with comorbidities (Vogelmeier et al. 2017). The disease not only decreases quality of life but it is also the leading cause of deaths from chronic respiratory diseases. In 2016, the number of deaths reached 2.93 million worldwide. COPD contributed 5.2% of non-communicable diseases in males and 3.9% in females in 2016. Mortality due to COPD is higher among the elderly. Mortality among women is lower than among men, but it is gradually increasing over time. COPD is the ninth leading cause of years of life lost globally, but the fifth in Western Europe (GBD 2016 Causes of Death Collaborators 2017).
Due to the chronic and progressive course, COPD is associated with many comorbidities. The disease primarily affects lungs, but systemic inflammation associated with COPD may serve as a possible causative factor responsible for the onset or deterioration of diseases such as ischemic heart disease, diabetes, and depression (Barnes and Celli 2009). Respiratory difficulties in the night-time and sleep apnea which are common among those patients contribute to changes in sleep pattern and result in daytime sleepiness. The percentage of COPD patients who report sleep problems is high; it is estimated between 16% and 75%. The most common sleep problems include insomnia, restless legs syndrome, and obstructive sleep apnea (Garrow et al. 2015). Complex and multi-dimensional sleep restriction, and consequently insufficient night rest, lead to problems with daily functioning and also may impact endocrine functions as well as metabolic and inflammatory responses (Banks et al. 2010).
In COPD patients, the occurrence of sleep disorders has a direct effect on the disease course. Coexistence of sleep problems is associated with disease severity, more frequent exacerbations, greater use of emergency health care, and higher mortality (Omachi et al. 2012). However, sleep disorders may reversely contribute to worsening of the course of COPD by reducing patient adherence to treatment. In this study, we attempted to shed more light on the association between sleep disorders and adherence to inhalation therapy. We believe that a better understanding of non-adherence among COPD patients can help improve both clinical and economic outcomes in this group of patients. Therefore, the aim of the study was to evaluate quality of sleep among patients with COPD and to assess the relationship between poor sleep quality and adherence to treatment with inhalation therapy.
2 Methods
The study included 106 patients with COPD (42 women and 64 men) with a mean age of 70.2 ± 5.9 (range 60–80) years of age, who were treated due to COPD at the Department of Internal Medicine in the Fourth Military Teaching Hospital in Wroclaw, Poland. Clinical and sociodemographic data were collected at the time of answering the questionnaires. Patients were classified into four categories according to the GOLD classification: GOLD 1 – mild; GOLD 2 – moderate; GOLD 3 – severe, and GOLD 4 – very severe (Vogelmeier et al. 2017). Additionally, patients were asked about their general feeling, the effect of the disease on daily activity, the quality of sleep, and the undertaking inhalation therapy such as short- and long-acting bronchodilators, theophylline, or glucocorticoids.
Quality of sleep was assessed using the Pittsburgh Sleep Quality Index (PSQI). This scale measures sleep quality in seven domains which are scored from 0 to 3 each. The total score ranges between 0 and 21. The result above 5 denotes poor sleep quality. The PSQI questionnaire has 89.6% sensitivity and 86.5% specificity for identifying cases with sleep disorders, using a cut-off score of 5. This questionnaire proved to have high internal consistency as indicated by Cronbach’s alpha of 0.83 and sufficient internal homogeneity (Mollayeva et al. 2016; Buysse et al. 1989).
The intensity of daytime sleepiness was assessed with Epworth Sleepiness Scale (ESS) (Johns 1991). The questionnaire consists of 8 items which described a possibility of falling asleep in particular situations. The probability was scored from 0 (no chances) to 3 (very high probability). The total score ranges from 0 to 24. The score above 10 denotes increased daytime sleepiness. For the purpose of this study, it was assumed that the score of 10 and below was normal, between 11 and 14 denoted mild sleepiness, between 15 and 18 moderate sleepiness, and above 18 severe sleepiness. The advantages of using ESS include its simplicity and high reliability for measuring persistent daytime sleepiness in adults. It also has a high level of internal consistency (Cronbach’s alpha of 0.88) (Johns 1992).
Adherence to pharmacotherapy was evaluated using the 12-item Polish version of Adherence to Refills and Medications Scale (ARMS). Possible score ranges from 12 (optimal adherence) to 48 (complete lack of adherence). Due to the fact that none of the patients investigated obtained an optimal result, the groups were classified as having moderate adherence level (13–30 scores) and poor adherence level (31–48 scores). The original version of ARMS has high internal consistency (Cronbach’s alpha of 0.81) and the results significantly correlate with those measured by the Morisky adherence scale (Kripalani et al. 2009).
2.1 Statistical Analysis
Nominal variables (sex, marital status, etc.) and ordinal variables (educations status, general feeling status, etc.) were presented as means and percentages. Comparison between groups with and without good and poor sleep quality (categorical variables) was conducted using contingency tables and assessed with the Pearson chi-squared test or in case of four-fold contingency tables with the chi-squared test with Yates correction or the Fisher exact test. Quantitative variables were presented as means ±SD. Conformity of distribution of continuous variables with the theoretical normal distribution in both groups of different sleep quality was verified with the Shapiro-Wilk test. Empirical distributions of body mass index (BMI) and age were other than normal (p < 0.05), so that their medians were compared with the non-parametric Mann-Whitney U test used. Differences were considered statistically significant at p < 0.05. All questionnaire data were collected in Microsoft Excel spreadsheet and statistically analyzed using the Statistica v12PL (StatSoft, Cracow, Poland).
The internal consistency and reliability of the Polish version of ARMS questionnaire were determined by computing Cronbach’s alfa and by calculating the correlation coefficient for scale items. The general assumption was made that a scale is considered of adequate internal consistency when alfa is ≥0.7 and items are of adequate similarity when a correlation coefficient is ≥0.3.
To evaluate the diagnostic importance of selected factors affecting adherence, the receiver operating characteristic (ROC) curve was used. The area under the curve (AUC) was used as a summary index for the discrimination of a test between patients with moderate and poor adherence.
3 Results
There were 65 (61.3%) patients with PSQI ≥5 which suggested poor sleep quality, while 41 (38.7%) did not present any signs of sleep problems. There were many differences between patients with and without sleep disorders. Patients who experienced sleep problems were older (p < 0.001), more often retired (p < 0.001), and more often lived alone (p < 0.001). There were more active smokers among them (p < 0.001). They also weighed 3 kg more on average (p = 0.011). Responders with sleep disorders experienced more problems with their health resulting in more frequent admissions to the hospital (p < 0.001) and longer hospitalizations (p < 0.001). They reported lower general feeling (p < 0.001) then respondents without sleep disorders. The comparison of clinical and social characteristics of the study group between respondents with and without sleep disorders is presented in Table 1.
Only did 26 (24.5%) patients report no daytime sleepiness. Out of the 80 (75.5%) patients with daytime sleepiness, a mild level of daytime sleepiness was observed in 30 (28.3%) patients, while moderate and severe in 25 (23.6%) each. Results of the ARMS questionnaire showed that there were no patients with optimal adherence to pharmacotherapy in the study group; 58 (54.7%) presented moderate adherence level and 48 (45.3%) poor adherence level. Details of daytime activities and sleep quality, the presence of daytime sleepiness and sleep disorders, and the level of adherence to treatment in the study group by the presence or lack of sleep disorders are presented in Table 2.
The assessment of the relationship between adherence to treatment and quality of sleep showed moderate relationship between those two variables (r = 0.562), which denotes that worse adherence was associated with greater sleep disorders. The graph of the correlation between adherence to treatment and quality of sleep is presented in Fig. 1.
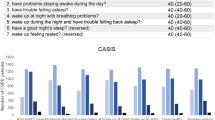
In the study groups of patients suffering from COPD, ARMS questionnaire proved to be of high overall internal consistency. Cronbach’s alpha for the scale was 0.85 and it satisfied Nunnally’s criterion of 0.7. The item-total correlation coefficient was 0.334. Item analysis of ARMS questionnaire is presented in Table 3. The ROC analysis showed that the number of previous hospitalizations below 4, ESS below 12 scores, and PSQI below 5 scores are the best discriminators that help identify patient adherence. Summary of ROC analysis is presented in Table 4.
4 Discussion
More than half (61.3%) of the COPD patients from our study experienced poor sleep quality as measured with PSQI. Additionally, patients classified as not having sleep disorders reported relatively high daytime sleepiness of the mean 9.5 scores as measured with ESS, while patients classified as having sleep disorders achieved a mean score of 17.3. The presence of sleep disorders translated into worse well-being. The study group presented with a low level of adherence to treatment; none of the patients had good adherence. The level of adherence correlated with the presence of sleep disorders.
The association of COPD and sleep disorders has been known for long (Klink and Quan 1987). The prevalence of sleep disorders in COPD patients reaches 60%. However, the quality of sleep is not routinely assessed by clinicians due to nonspecific complaints and as such, the coexistence of sleep disorders may be underestimated (Jen et al. 2016). Sleep profile differs between healthy controls and patients with COPD who report increased rate of symptoms such as insomnia; difficulty in initiating and maintaining sleep; obstructive sleep apnea; daytime sleepiness, and restless legs syndrome (Shawon et al. 2017; Budhiraja et al. 2015; Valipour et al. 2011). Patient-reported symptoms of impaired sleep are accompanied by biochemical changes responsible for nocturnal oxygen desaturation which manifest by reduced mean peripheral capillary oxygen saturation and increased sleep time spent with peripheral capillary oxygen saturation below 90% (Shawon et al. 2017). Our study confirms the high prevalence of sleep disorders among COPD patients. The mean score of PSQI was 9.9 which indicates poor overall quality of sleep. Only one fourth of our patients reported no daytime sleepiness. Patients with COPD complicated by sleep disorders had worse general health condition and more severe course of the disease than those without good sleep quality. Studies from the literature show that factors such as quality of sleep, acceptance of illness, and severity of COPD symptoms contribute to reduced quality of life (Uchmanowicz et al. 2016; Vardar–Yagli et al. 2015). As it has been known, concomitant sleep disorders in COPD patients are associated with severe symptoms and worse well-being. In the present study, we aimed to assess if they are also associated with poor adherence to treatment as follow doctors’ instructions is crucial for successful therapy.
Many efforts are undertaken to improve patient compliance because medication nonadherence jeopardizes outcomes and increases the costs of treatment (van Boven et al. 2016; van Boven et al. 2014). This is especially important in patients with severe chronic diseases such as COPD. Our study showed that none of the patients from the study group had optimal adherence to inhalation treatment. It is worth noting that in our study, ARMS showed high reliability among COPD patients (Cronbach’s alpha = 0.85). Reports from the literature show that about 40% of COPD patients present with sufficient level of adherence, but on the other hand, only 1 out of 10 patients use a metered dose inhaler correctly (Restrepo et al. 2008). Those findings are alarming and show that adherence to treatment in COPD patients is a complex process of cooperation between the patient and heath care providers.
Many factors may affect the level of adherence to prescribed medications among COPD patients. Researchers report various types of barriers to adherence. Intentional barriers include the lack of perception of the necessity of treatment and concerns about diagnosis and treatment. Nonintentional barriers include forgetting and technical problems with inhalers (improper medication use) (Horne et al. 2013; Drummond et al. 2008). There are also predictors that help to identify patients at risk of nonadherence. Fan et al. (2008) identified depressive and anxiety symptoms, lower education, and transportation issues as predictors for poor adherence to pulmonary rehabilitation among COPD patients. Rand et al. (1995) found better compliance in patients who were married, older, white, with more severe dyspnea, less shortness of breath, fewer hospitalizations, and those who were not confined to bed for respiratory illnesses. Turner et al. (1995) added nonsmoking status and stable lifestyle to the list of predictors for better adherence. A greater rate of comorbidity and greater polypharmacy also contribute to poor adherence. The coexistence of depression seems to play a major role in reducing adherence (Vetrano et al. 2017; Uchmanowicz et al. 2016). We found that sleep disorders were significantly correlated with worse adherence. Additional factors that help to identify problems with patient adherence are the number of previous hospitalizations, ESS score, and PSQI.
The link between sleep disorders and nonadherence has not been investigated. However, it was found that in patients with obstructive sleep apnea which often coexists with COPD, better sleep quality on the titration was related to better adherence to continuous positive airway pressure therapy (Somiah et al. 2012). The association between lower adherence and lower quality of sleep may possibly be rooted in poor overall condition of patients burdened with greater number of symptoms and comorbidities, similarly to conditions shown previously (Vetrano et al. 2017; Uchmanowicz et al. 2016). On the other hand, suboptimal control of COPD rooted in poor adherence to treatment results in further deterioration of sleep quality due to greater manifestation of pulmonary symptoms. We recommend further research on the relationship between adherences and sleep quality in COPD patients because an improvement in sleep quality may increase patient adherence and as a result, reduce cost of treatment and increase quality of life in this group of patients.
The study has several limitation. We found the relationship between poor medication adherence and poor sleep quality but causality remains to be studied. In COPD patients, many factors may worsen the quality of sleep such as dyspnea, cough, hypoxemia, and hypoventilation, which all also occur during the nighttime. A number of comorbidities can contribute to the development of sleep disorders such as cardiovascular diseases or mental problems. This study did not take into account possible causes of poor sleep quality. Additionally, adherence to medication has a multifactorial background, but we studied its relation to quality of sleep only.
5 Conclusions
This study showed the presence of a relationship between the quality of sleep and adherence to treatment among patients with COPD. The Adherence to Refills and Medications Scale (ARMS) was proved to be a reliable tool for the assessment of adherence to treatment among COPD patients. Interventions aimed at improving sleep quality may be helpful to improve adherence to inhalation therapy in this group of patients.
References
Banks S, Van Dongen HP, Maislin G, Dinges DF (2010) Neurobehavioral dynamics following chronic sleep restriction: dose–response effects of one night for recovery. Sleep 33(8):1013–1026
Barnes PJ, Celli BR (2009) Systemic manifestations and comorbidities of COPD. Eur Respir J 33(5):1165–1185
Budhiraja R, Siddiqi TA, Quan SF (2015) Sleep disorders in chronic obstructive pulmonary disease: etiology, impact, and management. J Clin Sleep Med 11(3):259–270
Buysse DJ, Reynolds CF 3rd, Monk TH, Berman SR, Kupfer DJ (1989) The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res 28(2):193–213
Drummond MB, Dasenbrook EC, Pitz MW, Murphy DJ, Fan E (2008) Inhaled corticosteroids in patients with stable chronic obstructive pulmonary disease: a systematic review and meta–analysis. JAMA 300(20):2407–2416
Fan VS, Giardino ND, Blough DK, Kaplan RM, Ramsey SD (2008) Costs of pulmonary rehabilitation and predictors of adherence in the National Emphysema Treatment Trial. COPD 5(2):105–116
Garrow AP, Yorke J, Khan N, Vestbo J, Singh D, Tyson S (2015) Systematic literature review of patient–reported outcome measures used in assessment and measurement of sleep disorders in chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis 10:293–307
GBD 2016 Causes of Death Collaborators (2017) Global, regional, and national age–sex specific mortality for 264 causes of death, 1980–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet 390(10100):1151–1210
Horne R, Chapman SC, Parham R, Freemantle N, Forbes A, Cooper V (2013) Understanding patients’ adherence–related beliefs about medicines prescribed for long–term conditions: a meta–analytic review of the necessity–concerns framework. PLoS One 8(12):e80633
Jen R, Li Y, Owens RL, Malhotra A (2016) Sleep in chronic obstructive pulmonary disease: evidence gaps and challenges. Can Respir J 2016:7947198
Johns MW (1991) A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep 14(6):540–545
Johns MW (1992) Reliability and factor analysis of the Epworth Sleepiness Scale. Sleep 15(4):376–381
Klink M, Quan SF (1987) Prevalence of reported sleep disturbances in a general adult population and their relationship to obstructive airways diseases. Chest 91(4):540–546
Kripalani S, Risser J, Gatti ME, Jacobson TA (2009) Development and evaluation of the Adherence to Refills and Medications Scale (ARMS) among low–literacy patients with chronic disease. Value Health 12(1):118–123
Mirza S, Clay RD, Koslow MA, Scanlon PD (2018) COPD guidelines: a review of the 2018 GOLD report. Mayo Clin Proc 93(10):1488–1502
Mollayeva T, Thurairajah P, Burton K, Mollayeva S, Shapiro CM, Colantonio A (2016) The Pittsburgh sleep quality index as a screening tool for sleep dysfunction in clinical and non–clinical samples: a systematic review and meta–analysis. Sleep Med Rev 25:52–73
Omachi TA, Blanc PD, Claman DM, Chen H, Yelin EH, Julian L, Katz PP (2012) Disturbed sleep among COPD patients is longitudinally associated with mortality and adverse COPD outcomes. Sleep Med 13(5):476–483
Rand CS, Nides M, Cowles MK, Wise RA, Connett J (1995) Long–term metered–dose inhaler adherence in a clinical trial. The Lung Health Study Research Group. Am J Respir Crit Care Med 152(2):580–588
Restrepo RD, Alvarez MT, Wittnebel LD, Sorenson H, Wettstein R, Vines DL, Sikkema–Ortiz J, Gardner DD, Wilkins RL (2008) Medication adherence issues in patients treated for COPD. Int J Chron Obstruct Pulmon Dis 3(3):371–384
Shawon MS, Perret JL, Senaratna CV, Lodge C, Hamilton GS, Dharmage SC (2017) Current evidence on prevalence and clinical outcomes of co–morbid obstructive sleep apnea and chronic obstructive pulmonary disease: a systematic review. Sleep Med Rev 32:58–68
Somiah M, Taxin Z, Keating J, Mooney AM, Norman RG, Rapoport DM, Ayappa I (2012) Sleep quality, short–term and long–term CPAP adherence. J Clin Sleep Med 8(5):489–500
Turner J, Wright E, Mendella L, Anthonisen N (1995) Predictors of patient adherence to long–term home nebulizer therapy for COPD. The IPPB Study Group. Intermittent positive pressure breathing. Chest 108(2):394–400
Uchmanowicz I, Jankowska–Polanska B, Motowidlo U, Uchmanowicz B, Chabowski M (2016) Assessment of illness acceptance by patients with COPD and the prevalence of depression and anxiety in COPD. Int J Chron Obstruct Pulmon Dis 11:963–970
Valipour A, Lavie P, Lothaller H, Mikulic I, Burghuber OC (2011) Sleep profile and symptoms of sleep disorders in patients with stable mild to moderate chronic obstructive pulmonary disease. Sleep Med 12(4):367–372
van Boven JF, Chavannes NH, van der Molen T, Rutten–van Molken MP, Postma MJ, Vegter S (2014) Clinical and economic impact of non–adherence in COPD: a systematic review. Respir Med 108(1):103–113
van Boven JF, Ryan D, Eakin MN, Canonica GW, Barot A, Foster JM (2016) Enhancing respiratory medication adherence: the role of health care professionals and cost–effectiveness considerations. J Allergy Clin Immunol Pract 4(5):835–846
Vardar–Yagli N, Saglam M, Savci S, Inal–Ince D, Calik–Kutukcu E, Arikan H, Coplu L (2015) Impact of sleep quality on functional capacity, peripheral muscle strength and quality of life in patients with chronic obstructive pulmonary disease. Expert Rev Respir Med 9(2):233–239
Vetrano DL, Bianchini E, Onder G, Cricelli I, Cricelli C, Bernabei R, Bettoncelli G, Lapi F (2017) Poor adherence to chronic obstructive pulmonary disease medications in primary care: role of age, disease burden and polypharmacy. Geriatr Gerontol Int 17(12):2500–2506
Vogelmeier CF, Criner GJ, Martinez FJ, Anzueto A, Barnes PJ, Bourbeau J, Celli BR, Chen R, Decramer M, Fabbri LM, Frith P, Halpin DM, Lopez Varela MV, Nishimura M, Roche N, Rodriguez–Roisin R, Sin DD, Singh D, Stockley R, Vestbo J, Wedzicha JA, Agusti A (2017) Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease 2017 report. GOLD executive summary. Am J Respir Crit Care Med 195(5):557–582
Conflicts of Interests
The authors declared no conflicts of interest in relation to this article.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This study was approved by the local Ethics Committee of Wroclaw Medical University in Poland.
Informed Consent
Written informed consent was obtained from all individual participants included in the study.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Chabowski, M., Łuczak, J., Dudek, K., Jankowska-Polańska, B. (2019). Sleep Disorders and Adherence to Inhalation Therapy in Patients with Chronic Obstructive Pulmonary Disease. In: Pokorski, M. (eds) Advances in Pulmonary Medicine: Research and Innovations. Advances in Experimental Medicine and Biology(), vol 1160. Springer, Cham. https://doi.org/10.1007/5584_2019_345
Download citation
DOI: https://doi.org/10.1007/5584_2019_345
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-21098-4
Online ISBN: 978-3-030-21099-1
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)