Abstract
Advances in mobile technology constitute a promising and evolving trend that enables better access to health care especially for the elderly, disabled, and chronically ill. It overcomes geographical, temporal, and organizational barriers at low and affordable costs. The aim of the study was to evaluate the needs and expectations of Polish citizens and their attitudes toward mobile health (mHealth) services using mobile phones and communication devices in medical care and also to evaluate the sociodemographic factors affecting such behavioral processes. A total of 1000 adults were selected from the Polish population by random sampling. The assessment was made with the use of computer-assisted telephone interview (CATI). Approximately 78% of the study participants were proficient mobile phone users with a predominance of young people. Forty-seven percent of them expressed the desire to obtain information about their health via their mobile phone if they had the opportunity to do so. Important factors associated with the aforementioned statement included younger age, being still in education, or unemployed. Among the mHealth supporters, the vast majority of people (84%) would like to receive SMS (short message service) reminders for appointments and prescribed medicines. Other favorable mHealth activities were e-registration (77.9%), viewing test results online (80.6%), or receiving basic medical recommendations (75.7%). Only 30% of the respondents had a positive attitude toward teleconsultation, while 17.8% of them were willing to pay for this option. Further research on emerging new and beneficial mHealth solutions needs to be conducted.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
Digital transformation has revolutionized almost every aspect of our lives and has the potential to increase health-care quality across the globe. Mobile health technology, commonly known as mHealth, is a relatively recent development in the digital world. It includes using devices such as cell phones, iPads, tablets, laptops, and similar devices in order to obtain access to health information networks. Using a smartphone or tablet for health management has now become as important as the traditional use of websites with a computer. The results of a worldwide survey including 7905 consumers published in 2018 by Accenture showed that for health management, 50% of respondents used websites and 48% used smartphones or tablets (Accenture Consumer Survey 2018).
Advances in mobile technology constitute a promising and evolving trend. They enable better access to health care, especially for the elderly, disabled, and chronically ill. They overcome geographical, temporal, and organizational barriers at low and affordable costs. Given their inexpensiveness, these devices are becoming increasingly available. The number of mobile phone users worldwide is growing rapidly. In 2010, 296 million smartphones were sold worldwide (Gartner 2011). In 2013, more than one billion smartphones were delivered to global markets. In the same year, there was a higher sale of smartphones than traditional cell phones (Business Wire 2014). According to a US national study, 95% of Americans own a mobile phone of some kind. In 2011, just 35% of Americans had a smartphone, while in 2018 this percentage was 77%. The ownership of a mobile phone is common across a wide range of demographic groups. By contrast, smartphone ownership depends on a greater variation of factors based on age, household income, and educational attainment (Pew Research Center 2018).
Smartphones allow real-time and on-demand communication, they store and exchange large amounts of personal information, and – through their multimedia-rich touch displays – they facilitate the lives of their owners. Thanks to the possibility of data storage in smartphones, mHealth applications enable the collection of substantial amounts of medical data, data on physiology, lifestyle, and daily activities. Typical examples of such applications include medical education materials and motivational tools such as reminding about taking medications or offering advice on exercises and diets (Boulos et al. 2014). A smartphone with Internet access and other built-in features like text messaging, e-mailing, web browsing, camera, GPS, audio, and video is crucial for the operation of mHealth services. These built-in devices provide additional possibilities of the implementation of mHealth applications. As a result, mHealth solutions may improve the efficiency of health protection both in the area of therapy and in the management of the health system. Telemonitoring in chronic diseases and issuing e-prescriptions during remote consultations are becoming more and more popular. Thanks to such solutions, users have easier access to information on their health at any place and time (Gensini et al. 2017).
Mobile devices and applications (apps) provide numerous benefits to the health-care system. These increasingly sophisticated tools could be a solution in favor of supporting and promoting patient care. In order to maximize the value and proper incorporation of these tools into health-care systems, their impact on their users must be well known. Therefore, the aim of this study was to evaluate the attitudes, needs, and expectations of Polish citizens with regard to selected mHealth services and to determine the sociodemographic factors affecting such behavioral processes.
2 Methods
2.1 Participants
A random sample of 1000 Polish adults was chosen nationwide to be included in the survey carried out between December 2017 and January 2018. The attitude toward mHealth services using mobile phones and communication devices in medical care was assessed by means of computer-assisted telephone interview (CATI). To make sure that the study group was representative, the province and town/city size were considered for the determination of the geographical distribution of respondents, who were further selected based on sociodemographic characteristics. On average, 5.2% of subjects agreed to participate in the study. Those who refused to do so, who did not answer the phone, who were too sick to participate, or whose phone number was incorrect fell into the nonresponders’ group. The majority of the nonresponders did not give any reason for their refusal. As a result, they were replaced by another household from the same region or town/city until 1000 participants completed the questionnaire.
2.2 Questionnaire
A questionnaire was designed to identify and determine diverse aspects related to the use of the Internet for health-related purposes and general opinion on telemedicine applications. In this study, we only focused on questions concerning consumer attitudes to, and views on, mobile health apps and associations between them and sociodemographic characteristics, including health status. First, the respondents were asked whether they had a mobile phone and were proficient in the use of a smartphone. Among those who gave a positive answer to this question, the respondents were further divided into two groups: supporters and non-supporters of mHealth use. In the supporters’ group, the opinion on the following mHealth services was measured: SMS (short message service) reminders about medical appointments or taking medications, teleconsultation, telemonitoring, medical test results reporting on cell phones, online registration, obtaining simple medical recommendations, and others. In addition, the participants were asked about their general opinion on the remote consultation and willingness to pay for it. The questionnaire also included items related to sociodemographic characteristics and health conditions such as respondent’s age, gender, education, and place of residence.
2.3 Data Analysis
In order to notice significant correlations between sociodemographic factors of the participants and their attitude toward mobile health apps, both descriptive and statistical analyses were incorporated. The Shapiro–Wilk test was used to check quantitative variables for normality of distribution which none of them displayed. Therefore, only nonparametric tests were used to carry out the analysis. The Wilcoxon multiple comparison test was conducted to compare the distribution of quantitative variables between the groups. For qualitative variables, the Chi-squared and Fisher’s independence tests were used to determine statistically significant dependencies. For all tests, the significance level was assumed to be 0.05. The R statistical package (version 3.5.1) was used for calculations.
3 Results
3.1 Characteristics of Respondents
The study included 558 women and 442 men randomly selected from among the Polish population. The median age was 53 (min–max, 18–88) years. There were 957 persons who declared that they used a mobile phone, mostly smartphones, but only 778 (77.8%) of them were proficient in its use. Six hundred and thirteen (61.3%) of respondents lived in cities/towns and 387 (38.7%) in rural areas. The majority of 856 (85.6%) respondents lived with someone else, while another 144 (14.4%) lived alone. As for employment status, 594 (59.4%) of respondents were professionally active, 317 (31.7%) were retirees or chronically ill/disabled, and 44 (4.4%) were still in education. Three hundred thirty-nine (33.9%) of respondents completed primary, 373 (37.3%) secondary, and 288 (28.8%) higher education. More than half of respondents were in good/very good health (n = 570; 57.5%), less in fair health (n = 347; 35%), and only 74 (7.5%) in poor/very poor health.
3.2 Factors Affecting Mobile Phone Use
Persons who were dexterous in using mobile phone devices were usually younger (p < 0.0001), better educated (p < 0.0001), and in better health (p < 0.0001). Those who were professionally active or still in education fully embraced this technology more frequently compared to those who were retired or chronically ill (p < 0.0001). What is more, a significantly greater percentage of mobile phone users lived in cities/towns (p = 0.002) and with their families or with someone else but not alone (p = 0.002). According to the questionnaire, women and men equally benefit from mobile devices. For more information, see Table 1.
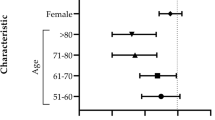
3.3 Support for Mobile Health (mHealth) Activities
Forty-seven percent of mobile phone users (n = 366) supported mHealth and 53% (n = 412) did not. Younger age increased the probability of having a positive attitude toward mHealth services (p < 0.00001). Further, people who were still in education or unemployed were more willing to support it (p < 0.0001) (Table 2). The most common mHealth activity was SMS reminders. In the group of SMS-reminder supporters, those who more frequently lived with their families (p < 0.05) and those who were still students, professionally active, or unemployed prevailed significantly (p < 0.05). People who opted for online registration were younger (p < 0.05), more often students or with completed higher education (p = 0.01), professionally active or unemployed (p = 0.01), and in better health status (p < 0.05). The same sociodemographic factors influenced the attitude toward mobile phone teleconsultation. Younger age had a positive effect on receiving test results on mobile phones (p = 0.01). There was no statistically significant correlation between telemonitoring, getting simple medical recommendations, and sociodemographic factors. For more details, see Table 3.
3.4 Opinion About Teleconsultation
Merely a third (29.7%) of respondents adopted a positive attitude toward mobile phone remote consultations. There were 61.3% of the proficient mobile phone users and 84.5% of the mHealth supporters who expressed their willingness for mobile phone teleconsultations (Fig. 1). Only 17.8% of respondents were ready to pay €10 for it. Compared to the other groups, the attitude of mHealth supporters toward paying for mobile phone teleconsultations was the most positive. The highest rate of a favorable attitude toward mobile phone teleconsultations was most frequently noticed among young people (p < 0.0001), with a high level of education (p < 0.0001), who lived in cities/towns (p < 0.03), and who were still in the process of education (p = 0.004) and in good health (p < 0.03). The willingness to pay for teleconsultation was correlated with younger age (p < 0.0001), a high level of education (p < 0.0001), being unemployed or professionally active (p < 0.0001), and being in good health (p < 0.0001) (Table 4).
4 Discussion
Over the years, mobile technology has witnessed many improvements that made mobile phones available for anyone everywhere. Due to the advanced computing and communication capability, which includes Internet access and global positioning systems, there is a great potential for application development. These technological innovations are implemented to improve access to, quality, and experience concerning just about every social, entertainment, and educational area of our lives. It is inevitable that we would also turn to digital solutions in the face of medical problems.
mHealth devices and telehealth platforms are increasingly used to complement medical care for patients who are proficient in the use of the Internet and other electronic communication tools. To use them accurately and appropriately, it is necessary for patients to be competent in digital and mobile technology. In the present study, over three fourths of the people were proficient mobile phone users. Nearly half of them were interested in mHealth. For the comparison of our current results to some prior studies, a 2012 Pew Research Center survey found that only 19% of mobile phone users had at least one health app (Fox and Duggan 2012). In turn, a German population-based survey conducted in 2017 revealed that among mobile phone users, around 20% used health apps (Ernsting et al. 2017). This study indicates a growing interest in various mHealth services. It is young people who were professionally active, with higher education, or still in education who were especially willing to use health apps for cell phones. Young age, a high level of education, and higher earnings were the key sociodemographic factors that were positively correlated with mHealth support in other studies (Carroll et al. 2017; Bhuyan et al. 2016; Krebs and Duncan 2015). However, there are still obstacles to a widespread use of mHealth technology. Technical systems may be poorly adapted to some groups of recipients. As this study showed, people who are old, retired, or chronically ill and lived alone and in rural areas were the least willing to use mobile devices. Nevertheless, it seems that it is these very groups that should reap the greatest benefits of telemedicine such us easier access to specialists, remote monitoring, and providing quick actions in case of emergency (van Houwelingen et al. 2018; Kaambwa et al. 2017; Bujnowska–Fedak 2015). A positive correlation was observed between living with the family and the willingness to use cell phones. This may indicate that when it comes to technology efficiency, it is beneficial for older generations to live with younger people. People are glad to ask their relatives for help in using the latest technologies (Zickuhr 2013). However, training in the field of using mobile technologies is required to allow them to take full advantage of benefits of mHealth.
The development and adoption of new methods of communication provide new opportunities for delivering health services. Due to the ubiquity of text messaging, rapid and automated delivery, and its relatively low cost, SMS has become recommended for use by leading organizations in various health-care fields (Schwebel and Larimer 2018). SMS reminders were primarily focused on outcomes such as appointment attendance and medication adherence (Berrouiguet et al. 2016; Kannisto et al. 2014). Currently, they may also serve as coaching tips or simple medical recommendations to support the desirable change of behavior (Prochaska et al. 1994; Fjeldsoe et al. 2009). This study confirmed the highest willigness of mobile phone users toward this service (88% of the mHealth supporters), which is very encouraging. A recent meta-analysis of randomized controlled trials demonstrates that medication adherence among patients with chronic conditions increases twofold with mobile phone text messaging (Thirumurthy and Lester 2012). A particular advantage of SMS services lies in that that they usually do not contain sensitive personal data. As it is well known, the security and confidentiality of data are a big concern for users (Suslo et al. 2018). Online registration and medical test results reporting also received a highly positive feedback in the current study (77.9% and 80.6% of the mHealth supporters, respectively). Medical appointment scheduling may improve the operation of the health-care system by improving access to it, decreasing waiting time, and decreasing staff labor (Zhao et al. 2017). Consequently, medical test results reporting makes it possible to provide a seamless exchange of information between the doctor and the patient. Using an app is faster and easier than downloading and printing lab results (Dullabh et al. 2014).
Teleconsultations and remote monitoring tools met with cautious response (43.7% and 55.7% of the mHealth supporters, respectively). People are still unwilling to change direct face-to-face communication with the doctor. Young age significantly affected the likelihood of using teleconsultation. According to a study by Zocdoc (2015), people who are raised in the digital era are less likely to visit the doctor and more naturally are inclined to make contact online instead. As reported by Krebs and Duncan (2015), a financial aspect is also of considerable importance in terms of the use of health apps. Approximately half of the app users stop using certain health apps due to hidden costs, which is consistent with the results of the current study. We noticed that a mere 17.8% of the entire cohort was willing to pay for teleconsultation. Yet the rate of people who were prepared to pay for the service significantly increased (42%) in the group of the proficient mHealth users. This is an important finding as it offers the opportunity to increase the profitability of mHealth due to cost-effective telemedical solutions.
This study has several limitations. The response rate was low (5.2% on average), albeit that is a rather usual finding in this type of study. Nonetheless, a nonresponse bias could have occurred and affected the estimates. In addition, the December–January time of the audit, which includes a holiday season and a winter break, might have influenced the low response rate. Moreover, due to the nature and high speed of the telephone conversation in CATI, the respondents were deprived of the possibility of thinking about and giving the most appropriate answer. The question about the financial status of respondents was also missing. On the other hand, it seems inappropriate to ask about earnings during a telephone interview, which might have given unreliable answers. Lastly, it is worth mentioning that this study focused on the attitudes of users rather than on patients’ outcomes. Therefore, the exact rate of the use of particular mHealth services is unknown. Further studies are necessary to assess the actual use of health apps rather than the attitudes and perceptions of their users.
5 Conclusions
Mobile technology has the potential to make the health-care system more efficient, less expensive, and more accessible. mHealth devices and telehealth platforms support disease management for patients who are proficient in the use of these tools. As with any new technology, the adaptation to mHealth services is a work in progress. Those who are young, with higher education, and who are professionally active are more drawn to digital technology than the rest of the population. Those who are older, retired, and chronically ill or disabled struggle to adapt to digital technology. Initial fears and the lack of willingness to use it at the beginning do not mean that it is ineffective. Even if the implementation of mHealth services is difficult to do well in certain environments, it is crucial to provide advice and to encourage potential users to benefit from it. The article demonstrates the need for further research to be performed to show the effects of numerous innovative uses of mobile technology on health outcomes.
References
Accenture Consumer Survey (2018) on Digital Health. https://www.accenture.com/t20180306T103559Z_w_/us-en/_acnmedia/PDF-71/accenture-health-2018-consumer-survey-digital-health.pdf. Accessed on 25 Oct 2018
Berrouiguet S, Baca–García E, Brandt S, Walter M, Courtet P (2016) Fundamentals for future mobile–health (mHealth): a systematic review of mobile phone and web–based text messaging in mental health. J Med Internet Res 18(6):e:135
Bhuyan SS, Lu N, Chandak A, Kim hM Wyant D, Bhatt J, Kedia S, Chang CF (2016) Use of mobile health applications for health–seeking behavior among US adults. J Med Syst 40(6):153
Boulos MNK, Brewer AC, Karimkhani C, Buller DB, Dellavalle RP (2014) Mobile medical and health apps: state of the art, concerns, regulatory control and certification. Online J Public Health Inform 5(3):229
Bujnowska–Fedak MM (2015) Trends in the use of the Internet for health purposes in Poland. BMC Public Health 15:194
Business Wire (2014) worldwide smartphone shipments top one billion units for the first time, according to IDC. http://www.businesswire.com/news/home/20140127006506/en/worldwide-smartphone-shipments-top-billion-units-time. Accessed on 25 Oct 2018
Carroll JK, Moorhead A, Bond R, LeBlanc WG, Petrella RJ, Fiscella K (2017) Who uses mobile phone health apps and does use matter? A secondary data analytics approach. J Med Internet Res 19(4):e125
Dullabh PM, Sondheimer N, Katsh E, Evans MA (2014) How patients can improve the accuracy of their medical records. EGEMS 2(3):1080
Ernsting C, Dombrowski SU, Oedekoven M, O Sullivan JL, Kanzler M, Kuhlmey A, Gellert P (2017) Using smartphones and health apps to change and manage health behaviors: a population–based survey. J Med Internet Res 19(4):e101
Fjeldsoe BS, Marshall AL, Miller YD (2009) Behavior change interventions delivered by mobile telephone short–message service. Am J Prev Med 36(2):165–173
Fox S, Duggan M (2012) Pew Research Center. Washington, DC: Pew Internet & American Life Project Mobile Health 2012. http://www.pewinternet.org/2012/11/08/mobile-health-2012/. Accessed on 25 Oct 2018
Gartner (2011) Gartner says worldwide mobile device sales to end users reached 1.6 billion units in 2010; Smartphone sales grew 72 percent in 2010. http://www.gartner.com/newsroom/id/1543014. Accessed on 25 Oct 2018
Gensini GR, Alderighi C, Rasoini R, Mazzanti M, Casolo G (2017) Value of telemonitoring and telemedicine in heart failure management. Card Fail Rev 3(2):116–121
Kaambwa B, Ratcliffe J, Shulver W, Killington M, Taylor A, Crotty M, Carati C, Tieman J, Wade V, Kidd MR (2017) Investigating the preferences of older people for telehealth as a new model of health care service delivery: a discrete choice experiment. J Telemed Telecare 23(2):301–313
Kannisto KA, Koivunen MH, Välimäki MA (2014) Use of mobile phone text message reminders in health care services: a narrative literature review. J Med Internet Res 16(10):e222
Krebs P, Duncan DT (2015) Health app use among US mobile phone owners: a national survey. JMIR Mhealth Uhealth 3(4):e101
Pew Research Center (2018) Mobile fact sheet. http://www.pewinternet.org/fact-sheet/mobile/. Accessed on 25 Oct 2018
Prochaska JO, Norcross JC, DiClemente CC (1994) Changing for good. A revolutionary program that explains the six stages of change and teaches you how to free yourself from bad habits. William Morrow & Co, New York. ISBN: 9780380725724
Schwebel FJ, Larimer ME (2018) Using text message reminders in health care services: a narrative literature review. Internet Interv 13:82–104
Suslo R, Paplicki M, Dopierala K, Drobnik J (2018) Fostering digital literacy in the elderly as a means to secure their health needs and human rights in the reality of the twenty–first century. Fam Med Prim Care Rev 20(3):271–275
Thirumurthy H, Lester RT (2012) M–health for health behaviour change in resource–limited settings: applications to HIV care and beyond. Bull World Health Organ 90:390–392
van Houwelingen CT, Ettema RG, Antonietti MG, Kort HS (2018) Understanding older people’s readiness for receiving telehealth: mixed–method study. J Med Internet Res 20(4):e123
Zhao P, Yoo I, Lavoie J, Javoie BJ, Simgoes E (2017) Web–based medical appointment systems: a systematic review. J Med Internet Res 19(4):e134
Zickuhr K (2013) Who’s not online and why? http://www.pewinternet.org/2013/09/25/main-report-2/. Accessed on 25 Oct 2018
Zocdoc (2015) New study: why Americans are dropping out of healthcare. https://www.zocdoc.com/about/news/new-study-why-americans-are-dropping-out-of-healthcare/. Accessed on 26 Oct 2018
Acknowledgments
This article forms a part of national surveys on the use of the Internet and e-health services in Poland conducted by Wroclaw Medical University in Wroclaw, Poland (statutory activity ST.C290.17.040/2017). The authors would like to thank Tomasz Kujawa for his methodological and statistical help.
Conflicts of Interest
The authors declare no conflicts of interest in relation to this article.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Respondents were provided with comprehensive information on the objectives and scope of survey and gave their informed consent. The survey was approved by the Bioethics Committee of Wroclaw Medical University in Poland.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Waligóra, J., Bujnowska–Fedak, M.M. (2019). Online Health Technologies and Mobile Devices: Attitudes, Needs, and Future. In: Pokorski, M. (eds) Medical Science and Research. Advances in Experimental Medicine and Biology(), vol 1153. Springer, Cham. https://doi.org/10.1007/5584_2019_335
Download citation
DOI: https://doi.org/10.1007/5584_2019_335
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-19058-3
Online ISBN: 978-3-030-19059-0
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)