Abstract
Obesity in children and adolescents contributes to increased prevalence of metabolic and hemodynamic complications, which may impair endothelial function and structure. A high resolution B-mode ultrasound measurement of intima-media thickness (IMT) is a useful tool to assess early, preclinical stage of atherosclerosis. The objective of this study was to evaluate the carotid artery IMT in obese children and its association with insulin resistance and other traditional metabolic syndrome components. The study entailed 80 obese children, aged 5.3–17.9 year and a control group of 31 children. Obesity was defined using the International Obesity Task Force (IOTF) criteria. Metabolic syndrome was defined using the International Diabetes Federation (IDF) criteria of 2007. Each patient’s anthropometric measurements, blood parameters, and the carotid IMT were evaluated. Insulin resistance indices were calculated. We found that children with metabolic syndrome had a significantly increased IMT compared to children who did not meet the syndrome criteria (0.62 ± 0.09 mm vs. 0.55 ± 0.18 mm, p = 0.03) and compared to control group (0.62 ± 0.09 vs. 0.52 ± 0.14, p = 0.02). In a multivariable linear regression analysis, IMT correlated with systolic blood pressure (p = 0.005). The results did not show an association between IMT and insulin resistance. We conclude that abdominal obesity and the accompanying components of metabolic syndrome lead to increased carotid IMT. The enhanced systolic blood pressure plays a major role in changing the carotid IMT.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
Atherosclerotic process and fibrous plague formation are the most frequent causes of mortality worldwide. Atherosclerosis does not usually provoke any symptoms even for decades until a sudden onset of coronary events such as stroke, myocardial infarction, or peripheral vascular disease. It is well-known that obesity in children and adolescents can induce atherosclerotic vascular changes even at an early age. Furthermore, fat mass accumulation (mainly visceral) favors the occurrence of metabolic and hemodynamic disturbances, whose severity and coexistence also play a crucial role in the pathogenesis of atherosclerotic process (Hong 2010; Berenson et al. 1998). The risk of its occurrence increases with increasing body mass index (BMI). At least two risk factors for cardiovascular disease were found in 39% of children and adolescents with BMI ≥ 95th percentile (pc), and in 59% of those with BMI ≥ 99 percentile (Freedman et al. 2007).
Therefore, it is important to take action to promote a healthy lifestyle and to identify patients who are at a risk of developing atherosclerosis. Besides traditional risk factors for coronary artery disease (CAD), the measurement of intima-media thickness (IMT) of the carotid artery using high-resolution ultrasonography has been used to evaluate early changes in the endothelium structure, which reflect the severity and extent of atherosclerosis in other arteries. The IMT is a useful surrogate marker of subclinical atherosclerosis in a wide spectrum of age (Johnson et al. 2009). In adults, IMT correlates with severity and extent of CAD such as myocardial infarction and stroke. Increased IMT precedes the occurrence of cardiovascular events, irrespective of traditional risk factors (O’Leary et al. 1999). In children, increased carotid IMT has been found in patients with familiar hypercholesterolemia (Vijayasarathi and Goldberg 2014), primary hypertension (Bucher et al. 2013), chronic kidney disease (Brady et al. 2012), and type 1 diabetes (Rodriguez et al. 2007). A large body of evidence indicates that adiposity and obesity-related metabolic and hemodynamic disturbances adversely affect the endothelium. The results concerning the association between IMT and cardiometabolic risk factors in obese children vary and are not fully consistent (Elshorbagy et al. 2016; Fang et al. 2010; Giannini et al. 2008; Reinehr et al. 2006). Therefore, this study seeks to determine the IMT in obese children and adolescents and the IMT’s association with insulin resistance and other traditional components of metabolic syndrome.
2 Methods
The study included 80 obese children (50 boys and 30 girls) aged 5.3–17.9 years (mean age 11.4 ± 2.9 years) hospitalized at the Department of Pediatrics and Endocrinology of the Medical University of Warsaw in Poland. After excluding endocrine, hereditary, kidney and infectious diseases, obesity was defined using the BMI cutoff level for children according to the International Obesity Task Force (IOTF) (Cole et al. 2000). The metabolic syndrome (MetS) criteria for obesity in children aged ≥10 years were adopted according to the International Diabetes Federation (IDF) Consensus Statement (Zimmet et al. 2007). Hence, examined subjects were divided by age into two subgroups: children younger than 10 years and older than 10 years. The older children were further divided according to the presence or absence of MetS. The controls were 31 healthy non-obese children (mean age 13.1 ± 2.6 years). The study participants underwent physical examination, anthropometric measurements, blood tests, and their carotid intima media thickness was evaluated by ultrasonography. The study protocol was approved by the Bioethics Committee of the Medical University of Warsaw in Poland.
The anthropometric measurements consisted of body height (cm), body weight (kg), waist and hip circumference (cm), and thickness of skinfolds under the triceps brachii muscle and under the inferior scapular angle (mm). The results of these measurements were used to determine BMI, waist to hip ratio (WHR), and waist to height ratio (WHtR). The degree of obesity (expressed as SDS BMI) was quantified using the least mean square method of Cole (1990). Body fat percentage (FAT) was calculated using the Slaughter equations based on skinfold measurements (Slaughter et al. 1998) and additionally in obese children using the bioelectrical impedance analysis (BIA) (Body Fat Analyzer BF-905; Maltron International Ltd., Rayleigh, UK).
After a 12-h overnight fast, blood samples were taken to measure fasting glucose and lipid profile (total cholesterol - TC, high density lipoprotein cholesterol - HDL-C, triglycerides - TG) using a standard enzymatic method. Light-density lipoprotein cholesterol (LDL-C) was calculated using Friedewald’s formula. The oral glucose tolerance test (OGTT) was performed in obese children, but not in healthy controls. The obtained data were used to calculate indicators of insulin resistance: homoeostasis model assessment (HOMA), fasting glucose to insulin ratio (FGIR), quantitative insulin sensitivity check index (QUICKI), oral glucose insulin sensitivity index (OGIS), and Matsuda indices (Ten and Maclaren 2004). Hyperlipidemia was interpreted according to the American Heart Association (AHA) recommendations (Hayman et al. 2007). Glucose levels were interpreted in accordance with the Polish Diabetes Association guidelines (PDA 2016). Severe insulin resistance was defined as the HOMA value ≥3.
In obese children, blood pressure (BP) was measured using a sphygmomanometer. After 10 min of rest, BP was measured three times and the average was taken for analysis. Hypertension was diagnosed when the values of systolic (SBP) or diastolic blood pressure (DBP) were above the 95th percentile for the Polish population of children; mean blood pressure values between the 90th and 95th percentiles were defined as the border zone (Ostrowska-Nawarycz and Nawarycz 2007).
Carotid IMT was measured by a trained investigator using 12–15 MHz ultrasound high resolution linear vascular probe on ATL 3000 HDL (Bothell; Washington DC). IMT measurements were assessed three times on both sides at the far wall of common carotid artery about 1 cm from the bifurcation as the distance between the two parallel echogenic lines: between lumen-intima and media-adventitia interferences. The average of these measurements was considered as the final carotid IMT value.
Data were presented as means ± SD, and minimum and maximum values, unless otherwise indicated. Differences between study groups were analyzed by independent samples t-test or Mann-Whitney U test. Associations between carotid IMT and chosen anthropometric, biochemical variables, and blood pressure were determined by Spearman’s nonparametric correlation. Multivariable linear regression analysis was used to quantify the influence of chosen anthropometric parameters, metabolic factors, and blood pressure on IMT. A p-value <0.05 was assumed to define statistical significance of differences. Statistical analysis was performed using a commercial IBM SPSS 19 statistical packet (Armonk, NY).
3 Results
The mean BMI of the obese children was 29.2 ± 4.6 kg/m2, the mean BMI SDS was 2.8 ± 0.5. For most anthropometric parameters and lipids profile there were statistically significant differences between the study group and the control group (Table 1). Increased values of total cholesterol (TC ≥ 200 mg/dl) were found in 20.0% of obese children, raised low-density lipoprotein cholesterol concentrations (LDL-C ≥ 110 mg/dl) was detected in 41.3% of obese children. Triglycerides (TG) levels exceeding 110 mg% were observed in 52 obese children (65.0% of the group). Low levels of high-density lipoprotein cholesterol (HDL-C < 40 mg/dl) were found in 28 (35.0%) obese children. Impaired fasting glucose was diagnosed in 9 (11.3%) and impaired glucose tolerance in 22 (27.5%) obese children. Elevated fasting insulin levels ≥15 μIU/ml were found in 47.5% of the children. The mean value of the insulin resistance indicator HOMA was 3.4 ± 2.1, whereas 52.5% of the group had HOMA values showing severe insulin resistance ≥3. The percentage of obese children with SBP slightly above the 95th percentile was 7.5%, and for DBP the percentage was 17.5%. The anthropometric and laboratory characteristics for obese children disaggregated by age and the presence of MetS are presented in Table 2.
The MetS criteria were applied to obese children at the age of 10 years and older according to the International Diabetes Federation recommendations. Among the 54 obese children, 42 (77.8%), including 16 girls and 26 boys, had central obesity, 20 (37.0%) had elevated levels of TG (≥150 mg/dl), and 20 children (37.0%) had decreased levels of HDL-C (< 40 mg/dl). In 10 children (10.0%) increased levels of SBP (≥130 mg/dl) or decreased levels of DBP (< 85 mmHg) were found. Five obese children (9.3%) had impaired fasting glucose (≥100 mg/dl). Diagnosis of metabolic syndrome (presence of central obesity plus any two or more out of other four components) was made found in 12 (22.2%) obese patients. The MetS (+) and the MetS (−) subgroups did not demonstrate significant differences regarding anthropometric parameters describing obesity and insulin resistance indices, as shown in Table 2.
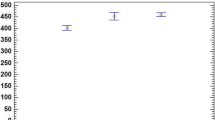
The mean carotid IMT measurement did not show significant differences between obese children and the normal-weight control group (0.55 ± 0.15 mm vs. 0.52 ± 0.14 mm; p = 0.4). When we compared the subgroup of obese children aged 10 years and older with control individuals of similar mean age, the differences in the mean value of IMT were somehow bigger (0.57 ± 0.17 vs. 0.52 ± 0.14; p = 0.2) and further increased for children with metabolic syndrome (0.62 ± 0.09 vs. 0.52 ± 0.14; p = 0.02) (Fig. 1). Carotid IMT did not differ significantly between obese girls and boys (0.58 ± 0.19 mm vs. 0.53 ± 0.11 mm; p = 0.17). Children aged 10 years and older had a slightly higher mean value of carotid IMT than younger children (0.57 ± 0.17 vs. 0.53 ± 0.10; p = 0.13). Higher carotid IMT values were found in children who met the IDF criteria of metabolic syndrome compared to those who did not have MetS diagnosis (0.62 ± 0.09 mm vs. 0.55 ± 0.18 mm; p = 0.03).
In the correlation analysis between carotid IMT and anthropometric parameters assessing nutritional status, biochemical parameters, and blood pressure it was found that IMT correlated positively with glucose at 90 min (r = 0.26, p = 0.02) and 120 min during OGTT (r = 0.23, p = 0.04), and also with systolic (SBP) (r = 0.30; p = 0.01) and diastolic blood pressure (DBP) (r = 0.24; p = 0.05). Linear regression analysis revealed the influence of blood pressure on carotid IMT (β = 0.006; p = 0.002, 95% CI: 0.002–0.009). Furthermore, this correlation remained significant in a multivariable linear regression analysis after adjustment for age, some anthropometric and biochemical parameters, and blood pressure as the independent variables (Table 3).
4 Discussion
The number of overweight and obese children and adolescents is currently growing worldwide. Obesity-related metabolic and hemodynamic disturbances such as dyslipidemia, insulin resistance, type 2 diabetes, and hypertension play a fundamental role in the pathogenesis of atherosclerosis. Atherosclerosis can begin in the pediatric population at all ages. Early accumulation of fatty streaks of lipid-engorged macrophages in the intima of an artery has no clinical symptoms but can be accessed via B-mode ultrasonography imaging of the thickness of intima-media space of carotid artery wall. Measurement of carotid IMT is an established non-invasive surrogate indicator for the evaluation of subclinical atherosclerosis (Hong 2010; Urbina et al. 2009). Some recent studies have confirmed that exposure to excess adiposity and some cardio-metabolic complications associated with overweight and obesity lead to increased thickness of carotid artery wall in children and adolescents (Reinehr and Wunsch 2011; Fang et al. 2010; Giannini et al. 2008; Iannuzzi et al. 2004).
In the present study we evaluated carotid IMT in several subgroups formed according to the following criteria: obese children under 10 years of age, obese children aged 10 years and older divided according to the presence of MetS criteria of IDF, and the control group of non-obese peers. We showed that obese children who fulfilled MetS criteria had the highest mean value of IMT, which differed significantly compared to obese children without MetS. Similar findings were obtained by Elshorbagy et al. (2016) based on a study of 60 obese children aged 8–16 years. In that study, significant differences of carotid IMT have also been reported between obese children and the control group, which we did not see in the present study. In another study, Vijayasarathi and Goldberg (2014) have demonstrated that children with metabolic syndrome had a higher mean value of IMT compared to patients with heterozygous familiar hypercholesterolemia and in both of these groups carotid IMT values were higher compared to non-obese patients. Also Reinehr et al. (2008), who studied a group of 264 Caucasian overweight children aged 7–16 years, have found significant correlations between carotid IMT values and metabolic syndrome defined by different MetS criteria established by Viner et al. (2005) and Weiss et al. (2004), but not those established by de Ferranti et al. (2004) and Cook et al. (1988). We did not find significant differences between the whole group of obese children and the control group, probably due to mismatched age of studied children; the difference in the mean age between obese children and the control group was 1.6 years. When we took into account the group of older obese children, whose mean age was similar to the mean age of the corresponding control group, the differences of mean carotid IMT between these groups became greater and statistically significant in relation to children with MetS. This confirms that structural endothelial changes appear to be dependent on coexisting vascular risk factors and their severity (Reinehr and Wunsch 2011).
The main abnormalities in MetS etiology are central obesity and insulin resistance. Giannini et al. (2008), who studied a group of 53 prepubertal obese children, have found correlations between IMT and insulin resistance indices (HOMA, WBISI – whole body insulin sensitivity index, glucose–insulin ratio). Elshorbagy et al. (2016) have shown that epicardial fat mass – an indirect marker reflecting visceral fat – is an independent predictor of carotid IMT in obese children with MetS. In the present study we did not find a link between carotid IMT and surrogate indices of body fat centralization and insulin resistance, nor did we find any differences regarding these parameters between groups of children with and without MetS diagnosis. Systolic blood pressure seems to be an important risk factor of early arterial structural changes in the present study. A linear correlation between carotid IMT and systolic hypertension has been demonstrated by Stabouli et al. (2012) in a study of 53 obese and 78 non-obese patients. In a study by Reinehr et al. (2006), including 96 obese children (mean age 11 years) carotid IMT values have been associated with hypertension and also with impaired glucose metabolism and inflammation. Another study (Aggoun et al. 2008) has shown that elevated blood pressure impairs endothelium function. Furthermore, Weberruß et al. (2016) have explained that non-significant differences in the value of carotid IMT SDS between obese patients and healthy patients could be due to the lack of additional cardiovascular risk factors, like hypertension accompanying obesity. We hypothesize that the lack of significant correlations between all obese children and the control group in our study is due to the small number of children with hypertension. Most of the children with elevated blood pressure belonged to the group with MetS diagnosis, which had the highest mean value of IMT.
Moreover, in this study we observed that older children had slightly higher mean values of IMT than younger ones, despite having a lower BMI SDS. Park et al. (2015) in their systemic review including 7366 children and adolescents have shown an association between IMT and adiposity in children with the mean age ≥ 12 years, but not in pre-adolescents. Although we did not find such a relationship, we found that duration of obesity is an important risk factor for endothelial alterations. Also, Reis et al. (2013) have shown in follow-up examinations that duration of overall and abdominal obesity is associated with coronary artery calcification and its progression, independent of the degree of adiposity. It cannot be ruled out that the higher values of IMT in older children are due to an adaptive response to sheer stress and tensile stress related to higher blood pressure. Probably pressure overload and the co-existence of metabolic risk factors, which are both characteristic of children with MetS, lead to pathological remodeling of artery wall and increased IMT.
In the literature there are only a few reports denying the existence of significantly higher values of carotid intima media wall thickness in obese pediatric population (Aggoun et al. 2008; Tounian et al. 2001). Despite the absence of differences in IMT between obese children and their normal-weight peers, Weberruβ et al. (2016) have shown that obese girls have significantly higher arterial stiffness parameters, which correlate with BMI. Early manifestations of atherosclerosis, such as alterations of endothelial and smooth muscle function, have also been demonstrated in 48 children with severe obesity (BMI z-score 4.4) in a study by Tounian et al. (2001) and in 48 prepubertal obese children in a study by Aggoun et al. (2008). These changes may precede remodeling process of the artery wall, yet they are not advanced enough to result in increased IMT. Presumably, changes in the morphology of carotid artery wall and significantly increased IMT could have appeared in the children from our study group with a longer time of followup. The Bogalusa Heart Study showed that childhood obesity contributes to elevated IMT in adults, independent of adult BMI (Freedman et al. 2008).
Silva et al. (2012), in their meta-analysis covering 16 articles published from 2005 to 2009 comparing IMT between obese and non-obese children, stress the importance of methodology of the IMT measurement. In 12 studies in which the differences in IMT were significant the value of IMT in obese children ranged widely from 0.37 to 0.74 mm. According to these authors, the inconsistency in the results may be explained by the fact that different segments were measured and the number of measurements varied. For example, Reinehr et al. (2006) have measured four values on each side near the bifurcation of the common carotid and have used maximum values for statistical calculations.
An increasing number of clinical studies emphasize the role of obesity in children and adolescents in the development of atherosclerosis in early childhood. Metabolic syndrome, defined as a cluster of interrelated risk factors that promote and enhance the risk of cardiovascular disease development, constitutes a particular risk for early remodeling of artery wall. As the obesity rate increases, the prevalence of metabolic syndrome grows in pediatric population and affects 16–44% of obese children (Friend et al. 2012). In the present study, MetS was diagnosed in 22.2% of patients. It is a global problem, because obesity with its concomitant cardiovascular disorder, and especially metabolic syndrome, can persist into adulthood and promote further growth of carotid IMT (Koskinen et al. 2009). Taking care of children with metabolic syndrome should be one of the methods of prevention of cardiovascular diseases in adulthood.
5 Conclusions
Abdominal obesity and the accompanying components of metabolic syndrome increases carotid intima-media thickness. High systolic blood pressure plays a major role in changing the carotid intima-media complex thickness. Early recognition and primary prevention in children with hypertension and other metabolic cardiovascular risk factors protect against the development of atherosclerosis and thus decrease the incidence of cardiovascular disease in adults. The measurement of IMT may be an additional tool to improve risk stratification of atherosclerosis in children and adolescents with obesity.
References
Aggoun Y, Farpour-Lambert NJ, Marchand LM, Golay E, Maggio AB, Beghetti M (2008) Impaired endothelial and smooth muscle functions and arterial stiffness appear before puberty in obese children and are associated with elevated ambulatory blood pressure. Eur Heart J 29(6):792–799
Berenson GS, Srinivascan SS, Bao W, Newman WP, Tracy RE, Wattigney WA (1998) Association between multiple cardiovascular risk factors and atherosclerosis in children and young adults. N Engl J Med 338:1650–1656
Brady TM, Schneider MF, Flynn JT, Cox C, Samuels J, Saland J, White CT, Furth S, Warady BA, Mitsnefes M (2012) Carotid intima – media thickness in children with CKD: results from the CKiD study. Clin J Am Soc Nephrol 7(12):1930–1937
Bucher BS, Ferrarini A, Weber N, Bullo M, Bianchetti MG, Simonetti GD (2013) Primary hypertension in childhood. Curr Hypertens Rep 15:444–452
Cole TJ (1990) The LMS method for constructing normalized growth standard. Eur J Clin Nutr 44:45–60
Cole TJ, Bellizzi MC, Flegal KM, Dietz WH (2000) Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ 320:1240–1243
Cook S, Weitzman M, Auinger P, Nguyen M, Dietz WH (1988) Prevalence of a metabolic syndrome phenotype in adolescents: findings from the third National Health and nutrition examination survey, 1988–1994. Arch Pediatr Adolesc Med 157:821–827
de Ferranti SD, Gauvreau K, Ludwig DS, Neufeld EJ, Newburger JW, Rifai N (2004) Prevalence of the metabolic syndrome in American adolescents: findings from the third National Health and nutrition examination survey. Circulation 110:2494–2497
Elshorbagy HH, Fouda ER, Kamal NM, Bassiouny MM, Fathi WM (2016) Evaluation of epicardial fat and carotid intima-media thickness in obese children. Iran J Pediatr 26(1):e2968
Fang J, Zhang JP, Luo CX, Yu XM, Lv LQ (2010) Carotid intima-media thickness in childhood and adolescent obesity relations to abdominal obesity, high triglyceride level and insulin resistance. Int J Med Sci 7(5):278–283
Freedman DS, Mei Z, Srinivasan SR, Berenson GS, Dietz WH (2007) Cardiovascular risk factors and excess adiposity among overweight children and adolescents: the Bogalusa Heart study. J Pediatr 150:12–17
Freedman DS, Patel DA, Srinivasan SR, Chen W, Tang R, Bond MG, Berenson GS (2008) The contribution of childhood obesity to adult carotid intima-media thickness: the Bogalusa Heart study. Int J Obes 32:749–756
Friend AJ, Craig LCA, Turner SW (2012) The prevalence of metabolic syndrome in children – a systematic review. Arch Dis Child 97:116–117
Giannini C, de Giorgis T, Scarinci A, Ciampani M, Marcovecchio ML, Chiarelli F, Mohn A (2008) Obese related effects of inflammatory markers and insulin resistance on increased carotid intima media thickness in pre-pubertal children. Atherosclerosis 197(1):448–456
Hayman LL, Meininger JC, Daniels SR, McCrindle BW, Helden L, Ross J, Dennison BA, Steinberger J, Williams CL, American Heart Association Committee on Atherosclerosis, Hypertension, and Obesity in Youth of the Council on Cardiovascular Disease in the Young.; American Heart Association Council on Cardiovascular Nursing.; American Heart Association Council on Epidemiology and Prevention.; American Heart Association Council on Nutrition, Physical Activity, and Metabolism (2007) Primary prevention of cardiovascular disease in nursing practice: focus on children and youth: a scientific statement from the American Heart Association Committee on atherosclerosis, hypertension, and obesity in youth of the council on cardiovascular disease in the young, council on cardiovascular nursing, council on epidemiology and prevention, and council on nutrition, physical activity, and metabolism. Circulation 116(3):344–357
Hong YM (2010) Atherosclerotic cardiovascular disease beginning in childhood. Korean Circ J 40(1):1–9
Iannuzzi A, Licenziati MR, Acampora C, Salvatore V, Auriemma L, Romano ML, Panico S, Rubba P, Trevisan M (2004) Increased carotid intima-media thickness and stiffness in obese children. Diabetes Care 27(10):2506–2508
Johnson RK, Appel LJ, Brands M, Howard BV, Lefevre M, Lustig RH, Sacks F, Steffen LM, Wylie-Rosett J, on behalf of the American Heart Association Nutrition Committee of the Council on Nutrition, Activity P, and Metabolism and the Council on Epidemiology and Prevention (2009) Dietary sugars intake and cardiovascular Health. A scientific statement from the American Heart Association. Circulation 120:1011–1020
Koskinen J, Kähönen M, Viikari JS, Taittonen L, Laitinen T, Rönnemaa T, Lehtimäki T, Hutri-Kähönen N, Pietikäinen M, Jokinen E, Helenius H, Mattsson N, Raitakari OT, Juonala M (2009) Conventional cardiovascular risk factors and metabolic syndrome in predicting carotid intima-media thickness progression in young adults: the cardiovascular risk in young Finns study. Circulation 120(3):229–236
O'Leary DH, Polak JF, Kronmal RA, Manolio TA, Burke GL, Wolfson SK (1999) Carotid artery intima and media thickness as a risk factor for myocardial infarction and stroke in older adults. Cardiovascular Health study collaborative research group. N Engl J Med 340(1):14–22
Ostrowska-Nawarycz L, Nawarycz T (2007) Norms of arterial blood pressure in children and adolescents – experience from the city of Lodz. Arterial Hyperten 2:138–150. (Article in Polish)
Park MH, Skow Á, De Matteis S, Kessel AS, Saxena S, Viner RM, Kinra S (2015) Adiposity and carotid-intima media thickness in children and adolescents: a systematic review. BMC Pediatr 15:161
PDA (2016) Polish Diabetes Association. Clinical recommendation for diabetic patients. Clin Diabetol 5(Suppl A) https://www.google.pl/webhp?sourceid=chrome-instant&ion=1&espv=2&ie=UTF-8#. Accessed 31 Jan 2017
Reinehr T, Kiess W, de Sousa G, Stoffel-Wagner B, Wunsch R (2006) Intima media thickness in childhood obesity. Relations to inflammatory marker, glucose metabolism and blood pressure. Metabolism 55:113–118
Reinehr T, Wunsch R, de Sousa G, Toschke AM (2008) Relationship between metabolic syndrome definitions for children and adolescents and intima-media thickness. Atherosclerosis 199:193–200
Reinehr T, Wunsch R (2011) Intima media thickness – related risk factors in childhood obesity. Int J Pediatr Obes 6(1):46–52
Reis JP, Loria CM, Lewis CE, Powell-Wiley TM, Wei GS, Carr JJ, Terry JG, Liu K (2013) Association between duration of overall and abdominal obesity beginning in young adulthood and coronary artery calcification in middle age. JAMA 310(3):280–288
Rodriguez RR, Gómez-Díaz RA, Haj JT, Avelar Garnica FJ, Soriano ER, Meguro EN, Carlos A, Aguilar-Salinas CA, Wacher NH (2007) Carotid intima-media thickness in pediatric type 1 diabetic patients. Diabetes Care 30(10):2599–2602
Silva LR, Stefanello JMF, Pizzi J, Timossi LS, Leite N (2012) Artherosclerosis subclinical and inflammatory markers in obese and nonobese children and adolescents. Braz J Epidemiol 15(4):804–816
Slaughter MH, Lohman TG, Boileau RA, Horswill CA, Stillman RJ, Van Loan MD, Bemben DA (1998) Skinfold equations for estimation of body fitness in children and youth. Hum Biol 60(5):709–723
Stabouli S, Kotsis V, Karagianni C, Zakopoulos N, Konstantopoulos A (2012) Blood pressure and carotid artery intima-media thickness in children and adolescents: the role of obesity. Hell J Cardiol 53(1):41–47
Ten S, Maclaren N (2004) Insulin resistance syndrome in children. J Clin Endocrinol Metab 89(6):2526–2539
Tounian P, Aggoun Y, Dubern B, Varille V, Guy-Grand B, Sidi D, Girardet JP, Bonnet D (2001) Presence of increased stiffness of common carotid artery and endothelial dysfunction in severely obese children: a prospective study. Lancet 358(9291):1400–1404
Urbina EM, Williams RV, Alpert BS, Collins RT, Daniels SR, Hayman L, Jacobson M, Mahoney L, Mietus-Snyder M, Rocchini A, Steinberger J, McCrindle B (2009) American Heart Association Atherosclerosis, Hypertension, and Obesity in Youth Committee of the Council on Cardiovascular Disease in the Young. Noninvasive assessment of subclinical atherosclerosis in children and adolescents: recommendations for standard assessment for clinical research: a scientific statement from the American Heart Association. Hypertension 54(5):919–950
Vijayasarathi A, Goldberg SJ (2014) Comparison of carotid intima-media thickness in pediatric patients with metabolic syndrome, heterozygous familial hyperlipidemia and normals. J Lipids 2014:546863. doi:10.1155/2014/546863
Viner RM, Segal TY, Lichtarowicz-Krynska E, Hidmarsh P (2005) Prevalence of the insulin resistance syndrome in obesity. Arch Dis Child 90:10–14
Weberruß H, Pirzer R, Böhm B, Dalla Pozza RD, Netz H, Oberhoffer R (2016) Intima-media thickness and arterial function in obese and non-obese children. BMC Obes 3:2. doi:10.1186/s40608-016-0081-9
Weiss R, Dziura J, Burgert TS, Tamborlane WV, Taksali SE, Yeckel CW, Allen K, Lopes M, Savoye M, Morrison J, Sherwin RS, Caprio S (2004) Obesity and the metabolic syndrome in children and adolescents. N Engl J Med 350:2362–2374
Zimmet P, Alberti K, Kaufman F, Tajima N, Silink M, Arslanian S, Wong G, Bennett P, Shaw J, Caprio S, IDF Consensus Group (2007) The metabolic syndrome in children and adolescents – an IDF consensus report. Pediatr Diabetes 8(5):299–306
Conflicts of Interest
The authors declare no conflicts of interest in relation to this article.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Rumińska, M. et al. (2017). Carotid Intima-Media Thickness and Metabolic Syndrome Components in Obese Children and Adolescents. In: Pokorski, M. (eds) Pulmonary Care and Clinical Medicine. Advances in Experimental Medicine and Biology(), vol 1021. Springer, Cham. https://doi.org/10.1007/5584_2017_29
Download citation
DOI: https://doi.org/10.1007/5584_2017_29
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-65468-3
Online ISBN: 978-3-319-65469-0
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)